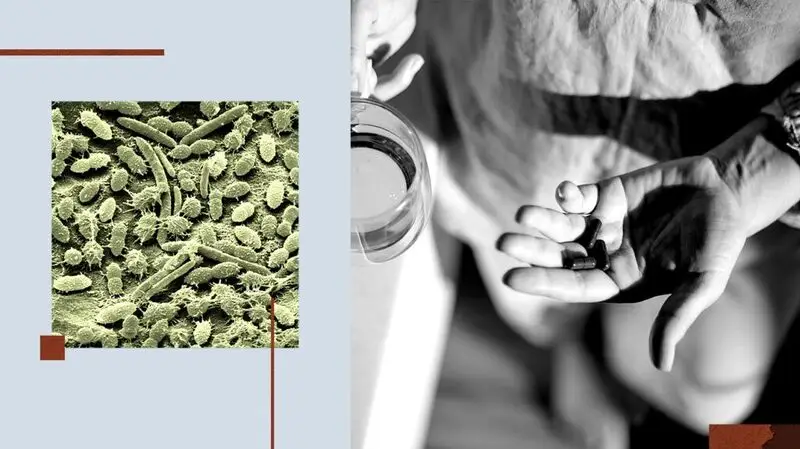
- Growing evidence shows that the gut microbiome is important for immune, digestive, and overall Health.
- Because antidepressants are taken orally, some of the active ingredients may make it to the large intestine, where the majority of microbes live.
- Medical News Today had spoken to three medical experts to find out more about how commonly prescribed antidepressants could shape and reshape our gut.
Recently, interest has been growing in how antidepressants could impact the gut microbiome — the trillions of microorganisms that inhabit the gut.
A recent study, for instance, concluded that antidepressants, among other drugs, impact the gut microbiome for years.
On the other side of the coin, scientists now know that connections between the gut microbiome and brain (the gut-microbiota-brain axis) can influence mental Health.
This raises the intriguing possibility that the makeup of the gut microbial community might influence how well antidepressant drugs work.
For this article, Medical News Today contacted three medical experts to explore how antidepressants might influence the microbiome. We also investigate how the gut microbiome influences the efficacy of antidepressant treatment.
In particular, we will focus on selective serotonin-reuptake inhibitors (SSRIs), which are the most commonly prescribed antidepressants.
It is crucial to note, however, that anyone taking antidepressants should not stop their medication or change their treatment regiment before speaking with their doctor. Doing so can be dangerous.
Although in some ways this seems like a relatively easy question to answer, there is an extra twist that makes it more challenging.
Existing research has shown that people with major depressive disorder have a different microbiome makeup than individuals without the condition.
This means that simply analyzing the gut microbiome of people who are taking SSRIs cannot tell you the full story: Their gut bacteria were probably different before they took the drugs.
Some studies have investigated the microbiomes of individuals taking SSRIs and other depression medications, identifying changes in the levels of certain species. However, these studies only looked at the microbiome at one point in time, so it is not possible to know whether these differences were present before the individual started taking SSRIs.
To make things more complex still, even though studies have identified differences between the microbiomes of individuals with and without depression, there is not yet a consensus on the precise differences.
Still, an innovative
The researchers took stool samples before the participants began treatment and after their symptoms began responding to treatment. This allowed them to chart the changes associated with the medication, specifically.
Overall, the researchers concluded that SSRIs did change the gut microbiome of people with depression. By the end of the study, their gut microbiome was more like the microbiome of healthy controls.
Although questions remain, this suggests that the changes in gut bacteria are not necessarily negative. The authors wrote: “[T]he gut microbiota tended to ‘normal’ gut microbiota structure under SSRIs treatment, thus indicating a positive effect of SSRIs on the change of gut microbiota.”
However, scientists need to continue investigating, as it is well-established that some SSRIs have an
Josh Lichtman, DO, a psychiatrist and medical director at Neuro Wellness Spa, told MNT that, while SSRIs may slightly shift the gut’s bacterial balance, “for most patients, the gut adjusts within a few weeks and returns to its normal baseline.”
He also told us that: “We don’t see evidence that SSRIs cause lasting microbiome damage. Diet and lifestyle tend to have a much bigger influence on gut health than the use of SSRIs.”
Along similar lines, Anoop Singh, MD, a board-certified psychiatrist and Regional Medical Director with Mindpath Health, said that:
“For most people, any SSRI-related changes appear modest and stabilize over time. It’s unlikely that SSRIs are doing lasting harm to the microbiome, and in some cases, they may even help restore the balance that chronic stress has disturbed.”
Although SSRIs can be a game-changer for some people with depression, they do not work for everyone. An estimated four out of 10 people with depression who take these drugs do not experience benefits.
Some evidence suggests that the makeup of an individual’s gut microbiome may help determine whether someone will respond well to SSRIs or not.
One study compared 62 antidepressant-naive people with major depressive disorder with 41 matched, Healthy controls. Once again, the researchers noted differences between the microbiomes of the two groups.
After those in the depression group had undergone 8 weeks of treatment with SSRIs, the scientists then divided them into responders who benefited and nonresponders who did not.
They found that some common genera of gut microbes were present at greater levels in those who did respond to treatment compared with nonresponders:
- Blautia—these are associated with health benefits and can kill certain disease-causing bacteria
- Bifidobacterium — these bacteria support a healthy gut and immune system
- Coprococcus — these produce a short-chain fatty acid called butyrate, which is associated with good overall health; interestingly, low levels of this genus of bacteria are
associated with depression .
“Emerging evidence suggests a real, two-way relationship. The microbiome doesn’t just respond to antidepressants; it may also help determine how well they work,“ Singh told MNT.
“Several studies have found that people with more diverse, balanced gut microbiomes tend to respond better to antidepressants. It’s an exciting area of research,” continued Singh, “and while we’re not yet at the point of choosing medications based on stool samples, the link between gut health and antidepressant response is becoming harder to ignore.”
As with every facet of the gut microbiome, its interaction with SSRIs is by no means straightforward. However, these are the main takeaways:
- people with depression tend to have markedly different microbiomes before drug treatment
- SSRIs change the makeup of the gut microbiome, but at least some of these changes are positive; however, SSRIs do show antibacterial properties, so some of the changes may be less favourable, but we need more research
- certain species of “good” gut bacteria are associated with better responses to SSRI treatment.
While many questions and mysteries still surround the gut microbiome and its links to health, it is growing increasingly clear that a healthy population of gut bacteria benefits overall health.
Although more studies are needed, it is possible that maintaining good gut health might reduce the risk of developing depression and enhance SSRI efficacy in those who take them.
Lastly, here is some advice from experts on how to nurture a healthy gut microbiome.
“The best way to support your gut microbiome is to eat a diverse, high-fiber, plant-filled diet,” explained Kristen Carli, MS, RD, a registered dietitian at WOWMD.
She told MNT that this should include “fiber-rich foods, which help feed the good bacteria in our guts. It’s also a good idea to include lots of probiotic-rich foods to replace some of the good bacteria whose growth may have been inhibited.”
Lichtman suggested following a “balanced, Mediterranean-style, plant-forward diet.” He also recommended staying active and learning to manage stress effectively.
“These habits support the ‘good’ gut bacteria that look after both digestive and mental health,” he concluded.
Continuing the theme, Singh suggested people “prioritize variety.“ He added that “a fiber-rich, plant-forward diet — including whole grains, legumes, vegetables, fruits, nuts, and seeds — encourages a more diverse microbiome.”
“Yogurt, kefir, kimchi, olive oil, and berries are excellent for feeding beneficial bacteria, but may not be right for everyone. Consult with your primary care provider or a nutritionist for specific advice, including the use of probiotics,” he concluded.