- New research shows an endovascular thrombectomy helps create new connections around dead brain tissue following a large ischemic stroke.
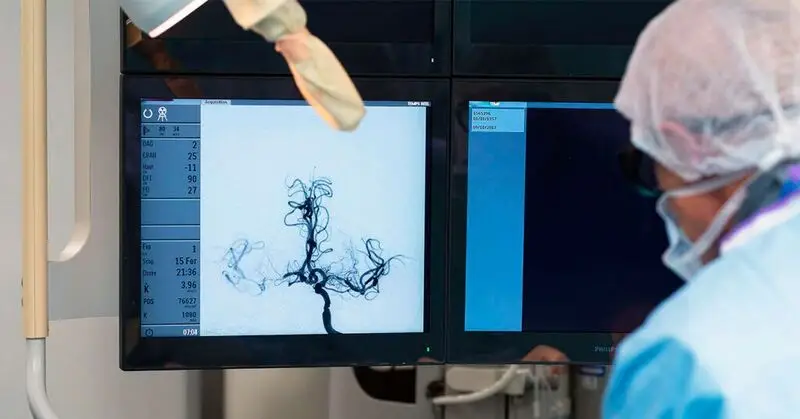
- The surgical procedure restores blood flow to large parts of the brain damaged by stroke.
- The findings demonstrate the potential for improved health and quality-of-life outcomes for stroke survivors.
In the United States, one person has a stroke every 40 seconds, while every 3 minutes and 14 seconds, another person dies of one, according to the
About 795,000 people have a stroke each year and 1 in 6 cardiovascular deaths is the result of a stroke. The CDC also reports that 87% of stroke cases are ischemic stroke, in which there is a blood clot blocking the flow of blood to the brain.
A new study finds that people who’ve had large ischemic strokes may experience better clinical outcomes when the blood clot, or thrombosis, that has damaged a large area of the brain is surgically removed with an endovascular thrombectomy (EVT).
In the study, the surgical procedure was accompanied by treatment with tissue plasmogen activator (tPA), which further breaks up clots.
The study is published in
Until now, EVT had been used for less severe strokes that produced smaller areas of dead brain tissue.
The new study, called “SELECT2 — A Randomized Controlled Trial to Optimize Patient’s Selection for Endovascular Treatment in Acute Ischemic Stroke,” followed patients for a year to document the long-term success of the procedure.
It took place at 31 hospitals in the United States, Canada, Spain, Switzerland, Australia, and New Zealand, and was a phase 3, open-label, international, randomized controlled trial with blinded endpoint assessment.
The 352 participants in the trial each had acute ischemic stroke with a large blood clot at its center, and were randomly assigned to receive either EVT with medical treatment or medical treatment alone, within 24 hours of the stroke.
All initially showed significant damage from the blood blockage, suggesting that they were likely to experience poor outcomes.
The findings show that after a 1-year followup, large-stroke patients who have received endovascular thrombectomy plus medication were 1.4 times more likely to achieve positive outcomes than those treated only medicinally.
These EVT patients were twice as likely to be able to walk without assistance, and three times more likely to lead completely independent lives. They also scored higher on quality-of-life surveys.
Neurologist Dr. Jason Tarpley, director of the Stroke & Neurovascular Center; Vascular and Interventional Neurology at the Pacific Neuroscience Institute in Santa Monica, CA, described a typical thrombectomy procedure for stroke for Medical News Today. Tarpley was not involved in the study.
First, he said a surgeon inserts a small catheter tube “about the size of an iPhone charging cable into the artery of the leg.” Then, the surgeon navigates a smaller catheter into the artery of the neck, followed by a smaller one.
Once at the stroke location, in some procedures, a “stent retriever” grabs the clot and pulls it out. Alternately, suction may remove the clot, he explained.
“We put the catheter right up to the surface of the clot, ‘kiss’ the clot and turn on suction that pulls the clot into the catheter,” Dr. Tarpley said.
What’s significant about this study is that it demonstrates — along with several other studies over the last few years — the potential value of addressing large areas of post-stroke dead brain tissue, instead of limiting the procedure to smaller ones.
Its finding suggests that even if the large area of dead brain tissue will never be resuscitated, returning blood flow to its general vicinity supplies the surrounding tissue with what it needs to leverage the brain’s remarkable plasticity.
With blood and oxygen flow restored, the brain can begin re-wiring itself around the dead tissue.
Dr. Tarpley was involved in a similar recent study, and noted while some patients may have good clinical outcomes during recovery, such outcomes are not guaranteed, with or without EVT. “Without the procedure, it’s dismal,” he said.
Cardiologist Dr. Jayne Morgan, executive director of Health and Community Education at the Piedmont Healthcare Corporation in Atlanta, GA, also not involved in the new study, told MNT the improved functional and quality-of-life outcomes resulting from thrombectomy among post-stroke survivors cannot be overstated.
“Not only are these indicators of higher functional independence and independent ambulation, but also lower mortality,” Dr. Morgan said.
“Moreover, the greater social benefits cannot be overstated, as the ability to remain connected in meaningful ways with the community for engagement and vitality will decrease depression, anxiety, and also death outcomes over time. This is especially important as poorer outcomes were noted in this study in those over the age of 70, and at great risk of social isolation that worsens with poor physical functioning.”
— Dr. Jayne Morgan, cardiologist
A stroke may occur from a blood clot or as the result of a rupturing brain aneurysm — such strokes can sometimes be surgically clamped to close the rupture.
There are many reasons a person might have a stroke. Dr. Morgan cited atrial fibrillation (AFib) — an irregular and frequently rapid heartbeat that can lead to blood clots — as well as the narrowing of arteries that occurs with carotid artery disease.
Dr. Morgan said high blood pressure (hypertension) is “the most significant factor because of the long-term damage that it can do to blood vessels.”
The risk of stroke also increases, said Dr. Morgan, with having had a previous stroke, a
“Blacks in the U.S. have a higher rate of strokes than any other ethnic group,” said Dr. Morgan. One factor is their unique susceptibility to
Other known risk factors for stroke include:
- smoking
- high cholesterol
- obesity (a risk factor for hypertension and diabetes)
In addition, noted Dr. Morgan, “Men have a higher rate of strokes, but women are more likely to die from strokes.”
Dr. Morgan also cited family history as a potential risk factor for stroke: “This should absolutely never be overlooked, as inherited disorders can be causative,” she said.
Managing one’s blood pressure is vitally important for stroke prevention, as is being physically active, Dr. Morgan said.
“Sedentary lifestyles increase the risk of many risk factors that increase the risk of stroke, such as obesity, cholesterol, hypertension, and diabetes,” she noted.
A Healthy diet and weight management help protect against stroke. Stress management is also key.
“Chronic stress is a risk factor for stroke,” Dr. Morgan said. “Don’t be hesitant to reach out to a therapist, or to engage in activities that increase pleasant socialization.”
To reduce stroke risk, experts also recommend:
- quitting or avoiding smoking
- limiting alcohol intake
- getting sufficient sleep
- taking any prescribed medications as directed