- Scientists have known for some time now that the eyes can also help doctors see signs of non-eye-related health conditions.
- Through the blood vessels in the retina, eye doctors can detect signs of conditions such as high blood pressure and high cholesterol.
- A new study found that the retina’s blood vessels may also be used to help predict a person’s heart disease risk and see how fast they are biologically aging.
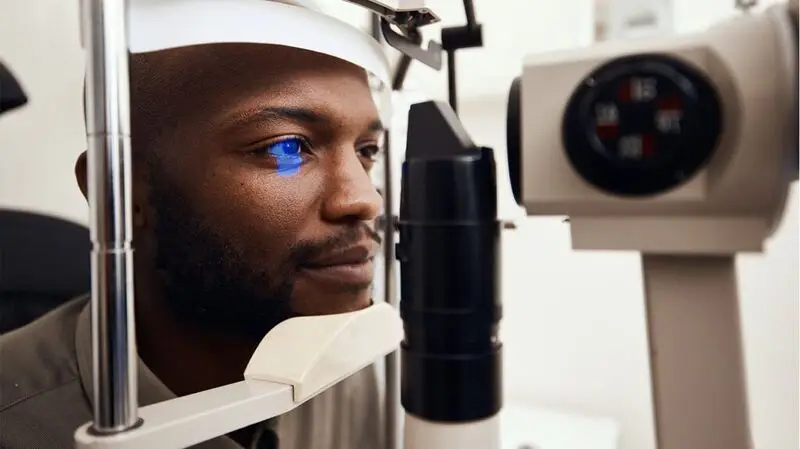
They say the eyes are in the window to the soul; however, scientists have known for some time now that the eyes can also help doctors see signs of non-eye-related health conditions.
For example, uveitis — inflammation of the eye — can be a sign that a person has an autoimmune disease. Through the blood vessels in the retina, or the back of the eye, eye doctors can detect signs of high blood pressure, high cholesterol, diabetes, and early stages of heart disease.
For this study, researchers analyzed retinal scans, genetic information, and blood samples from more than 74,000 participants across four major studies: the Canadian Longitudinal Study on Aging (CLSA), the Genetics of Diabetes Audit and Research in Tayside Scotland (GoDARTS), the U.K. Biobank, and the PHRI Prospective Urban and Rural Epidemiological (PURE) study.
“We chose to study the eye, and specifically the retina, because it provides a unique, noninvasive view of the body’s microvasculature (network of small blood vessels), which can reflect overall vascular health,” Marie Pigeyre, MD, PhD, associate professor in the Endocrinology Division of the Department of Medicine at McMaster University in Ontario, Canada, and senior author of this study, told Medical News Today.
“Retinal imaging can capture subtle changes linked to aging, inflammation, and heart disease, and with advances in AI, these scans can reveal early biological aging and help assess cardiovascular risk, as heart disease often develops silently.”
— Marie Pigeyre, MD, PhD
Upon analysis, researchers found that study participants who had simpler, less branched retinal blood vessels had a higher chance of developing cardiovascular disease. These participants also showed signs of biological aging, including higher inflammation and a shorter life span.
“The finding that simpler, less branched retinal blood vessels are linked to higher heart disease risk and shorter lifespan shows that retinal vascular complexity is a measurable indicator of systemic inflammation and vascular aging. This highlights the retina’s potential as an early, noninvasive biomarker to identify at-risk individuals, track vascular health over time, and enable personalized prevention and treatment strategies.”
— Marie Pigeyre, MD, PhD
Additionally, scientists unveiled potential biological causes for the changes to the eye’s blood vessels, including specific proteins — most notably MMP12 and
“Identifying proteins like MMP12 and IgG-Fc receptor IIb connects retinal vascular changes to specific inflammatory and tissue-remodeling pathways that can drive aging and cardiovascular disease,” Pigeyre said. “This discovery bridges microvasculature changes with underlying molecular mechanisms, highlighting potential therapeutic targets to slow vascular aging and prevent related diseases.”
MNT spoke with Benjamin Bert, MD, a board certified ophthalmologist at MemorialCare Orange Coast Medical Center in Fountain Valley, CA, about this study, who commented that this is an excellent study demonstrating the power of using the retinal microvasculature to diagnose other systemic diseases.
“The retinal microvasculature is the only microvasculature that we can see in a non-invasive manner, but is the same vasculature that is seen in the brain and the kidneys,” Bert explained.
“For that reason,
dilated eye exams have for years provided a way to examine this vasculature and allow clinicians to diagnose patients with underlying cardiovascular diseases like diabetes or hypertension. Studies like this may provide ways for us to be able to predict these diseases from a photograph of the eye earlier than we may be able to do now.”
— Benjamin Bert, MD
“There have been other studies, like this study, that have used artificial intelligence to interpret different forms of retinal imaging,” he continued. “These studies have been able to identify age and sex just from the retinal image and no other information. Other studies have been able to diagnose dementia from retinal scans. Thus, there is a lot more information that we can utilize from these noninvasive tests to tell us a lot about ourselves and our Health status.”
“I would definitely like to see this research continue as it can supplement blood tests, radiologic studies, and physical exam findings that we currently use to monitor our health status,” Bert added.
MNT also spoke with Craig Basman, MD, FACC, FSCAI, Associate Director, Structural & Congenital Heart Program, and director of the Adult Congenital Heart Disease at Hackensack University Medical Center in New Jersey, about this research.
“For individuals who are mindful of their cardiovascular health or how quickly their body is aging, the initial reaction to this study is a mix of apprehension and optimism,” Basman said.
“The study suggests that a lower complexity in the retinal blood vessel network is genetically linked to a higher risk of cardiovascular disease, stroke, and a shorter life span. It suggests that our genes may predispose some of us to a less robust microvascular system, which could have systemic implications,” he explained.
“However, this research also brings a significant wave of hope,” he continued. “The eye provides a unique, noninvasive window into the body’s vascular health.”
“The prospect of a quick, painless retinal scan giving early warnings about cardiovascular risk and biological aging is a powerful one. As our preventative treatment of cardiovascular pathology continues to evolve, it could empower individuals to make proactive lifestyle changes and seek preventative care long before symptoms of heart disease appear.”
— Craig Basman, MD, FACC, FSCAI
While promising, Basman said, this study is merely a foundational step and still requires clinical validation, refinement of predictive models, and investigation into potential causal mechanisms.
“In conclusion, this





