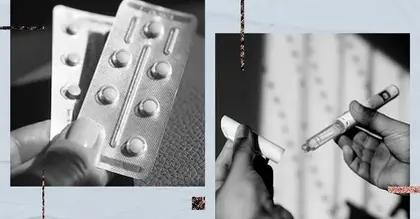
Drug Detail:Bionafem (Levonorgestrel emergency contraceptive [ lee-voe-nor-jes-trel ])
Drug Class: Contraceptives
Usual Adult Dose for Contraception
Intrauterine Device (IUD) insertion should be performed by a trained healthcare provider thoroughly familiar with product; product manufacturer labeling should be consulted:
Insert 1 IUD (13.5, 19.5 or 52 mg) into uterus
Timing of insertion:
- For women who are not currently using hormonal or intrauterine contraception: Insertion may occur at any time the woman is not pregnant; if inserted after the first 7 days of menstrual cycle, an additional method of contraception should be used for 7 days after insertion
- Switching from an oral, transdermal, or vaginal hormonal contraceptive: Insertion may occur at any time; if inserted during the hormone phase, continue use for 7 days after insertion or until the end of the current treatment cycle
- Switching from an injectable progestin contraceptive: Insertion may occur at any time; if inserted more than 3 months after the last injection, an additional method of contraception should be used for 7 days after insertion
- Switching from a contraceptive implant or another IUD: Insertion should occur on the same day the implant or IUD is removed
- Inserting after abortion or miscarriage:
- First trimester: May insert IUD immediately after a first trimester abortion or miscarriage
- Second trimester: Insertion of IUD should be delayed a minimum of 4 weeks or until the uterus is fully involuted; if involution is delayed, insertion should be delayed until involution is complete; consider the possibility of ovulation and conception occurring prior to insertion and advise patient on need for an additional method of contraception for 7 days after insertion
- After childbirth: Insertion of IUD should be delayed a minimum of 4 weeks after delivery, or until the uterus is fully involuted; if involution is delayed, insertion should be delayed until involution is complete; consider the possibility of ovulation and conception occurring prior to insertion and advise patient on need for an additional method of contraception for 7 days after insertion
Replacement: IUD should be replaced after the prescribed amount of time; a new IUD may be inserted for continued use
- Skyla(R): Replace after 3 years
- Kyleena(R), Mirena(R), and Liletta(R): Replace after 5 years
Comments:
- IUD may be removed at any time but must be removed by the end of the prescribed time; if continued use is desired, replace with a new IUD.
Uses: Prevention of pregnancy for up to 3 years (Skyla[R]) or 5 years (Kyleena[R], Mirena[R], and Liletta[R]); additionally, Mirena(R) is for the treatment of heavy menstrual bleeding in women who choose to use intrauterine contraception as their method of contraception.
Usual Adult Dose for Postcoital Contraception
Emergency Contraception:
Take 1.5 mg orally once or 0.75 mg orally 12 hours apart
Comments:
- Doses should be taken as soon as possible within 72 hours after unprotected intercourse or known/suspected contraception failure; the sooner it is taken the better.
- If vomiting occurs within 2 hours of taking dose, consider repeating the dose.
- This product is not intended for regular birth control.
Use: To reduce the chance or pregnancy after unprotected intercourse or a known/suspected contraceptive failure.
Usual Pediatric Dose for Contraception
Postpubertal adolescents:
Intrauterine Device (IUD) insertion should be performed by a trained healthcare provider thoroughly familiar with product; product manufacturer labeling should be consulted:
Insert 1 IUD (13.5, 19.5 or 52 mg) into uterus
Timing of insertion:
- For women who are not currently using hormonal or intrauterine contraception: Insertion may occur at any time the woman is not pregnant; if inserted after the first 7 days of menstrual cycle, an additional method of contraception should be used for 7 days after insertion
- Switching from an oral, transdermal, or vaginal hormonal contraceptive: Insertion may occur at any time; if inserted during the hormone phase, continue use for 7 days after insertion or until the end of the current treatment cycle
- Switching from an injectable progestin contraceptive: Insertion may occur at any time; if inserted more than 3 months after the last injection, an additional method of contraception should be used for 7 days after insertion
- Switching from a contraceptive implant or another IUD: Insertion should occur on the same day the implant or IUD is removed
- Inserting after abortion or miscarriage:
- First trimester: May insert IUD immediately after a first trimester abortion or miscarriage
- Second trimester: Insertion of IUD should be delayed a minimum of 4 weeks or until the uterus is fully involuted; if involution is delayed, insertion should be delayed until involution is complete; consider the possibility of ovulation and conception occurring prior to insertion and advise patient on need for an additional method of contraception for 7 days after insertion
- After childbirth: Insertion of IUD should be delayed a minimum of 4 weeks after delivery, or until the uterus is fully involuted; if involution is delayed, insertion should be delayed until involution is complete; consider the possibility of ovulation and conception occurring prior to insertion and advise patient on need for an additional method of contraception for 7 days after insertion
Replacement: IUD should be replaced after the prescribed amount of time; a new IUD may be inserted for continued use
- Skyla(R): Replace after 3 years
- Kyleena(R), Mirena(R), and Liletta(R): Replace after 5 years
Comments:
- IUD may be removed at any time but must be removed by the end of the prescribed time; if continued use is desired, replace with a new IUD.
Uses: Prevention of pregnancy for up to 3 years (Skyla[R]) or 5 years (Kyleena[R], Mirena[R], and Liletta[R]); additionally, Mirena(R) is for the treatment of heavy menstrual bleeding in women who choose to use intrauterine contraception as their method of contraception.
Usual Pediatric Dose for Postcoital Contraception
Emergency Contraception:
Postpubertal adolescents:
Take 1.5 mg orally once or 0.75 mg orally 12 hours apart
Comments:
- Doses should be taken as soon as possible within 72 hours after unprotected intercourse or known/suspected contraception failure; the sooner it is taken the better.
- If vomiting occurs within 2 hours of taking dose, consider repeating the dose.
- This product is not intended for regular birth control.
Use: To reduce the chance or pregnancy after unprotected intercourse or a known/suspected contraceptive failure.
Renal Dose Adjustments
Data not available
Liver Dose Adjustments
Intrauterine Device:
- Acute liver disease or liver tumor: Contraindicated
Precautions
CONTRAINDICATIONS:
- Hypersensitivity to the active component or any of the ingredients
- Known or suspected pregnancy
Intrauterine Device (IUD) is contraindicated if one or more of the following conditions exist:
- Acute liver disease or liver tumor (benign or malignant)
- Uterine bleeding of unknown etiology
- Known or suspected breast cancer or other progestin-sensitive cancer, now or in the past
- Congenital or acquired uterine anomaly, including fibroids, that distorts uterine cavity and would be incompatible with correct placement
- Acute pelvic inflammatory disease (PID) or a history of PID unless there has been subsequent intrauterine pregnancy
- Postpartum endometritis or infected abortion in past 3 months
- Known or suspected uterine or cervical neoplasia
- Untreated acute cervicitis or vaginitis, including bacterial vaginosis, known chlamydial or gonococcal cervical infection, or other lower genital tract infections until infection is controlled
- Conditions associated with increased susceptibility to pelvic infections
- Use as post-coital contraception
- A previously inserted intrauterine device that has not been removed
Safety and efficacy have been established in female patients of reproductive age; use prior to menarche is not indicated.
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
Emergency Contraception:
- Take as soon as possible up to 72 hours after unprotected sex; the sooner it is taken the better it will work.
- If vomiting occur within 2 hours after taking dose, dose should be repeated
Intrauterine Device (IUD):
- Insertion should be performed by a trained healthcare provider thoroughly familiar with product; product manufacturer labeling should be consulted
Timing of IUD Removal:
- If pregnancy is desired, the IUD may be removed at any time.
- If IUD is to be removed and pregnancy is not desired, a new contraception method should be started prior to removal of the IUD.
Storage requirements:
- IUD: For single use only; store pouch in outer carton until use to protect from light
Monitoring:
- IUD Follow-up: Re-examine patient 4 to 6 weeks following IUD insertion and once a year thereafter, or more frequently if clinically indicated.
- Emergency Contraception Follow-up: Physical or pelvic exam is recommended if there is any doubt concerning general health or pregnancy status of any woman after use for postcoital contraception.
Patient advice:
- Read the US FDA-approved patient labeling (Patient Information).
- Patients should understand that this drug does not protect against HIV infection and other sexually transmitted infections.
- Counsel patients on the risks of becoming pregnant if intercourse occurs in the 7-day period after insertion as well as before removal of IUD.
- Contact healthcare provider promptly if you become pregnant with IUD intact due to the risk of ectopic pregnancy.
- Report any signs/symptoms of lower abdominal pain, long-lasting or heavy bleeding, painful intercourse, chills, or fever.
- Report severe pain or fever following IUD insertion due to the risk of infection.
Frequently asked questions
- Can Plan B make your period late or cause bleeding?
- Can you drink alcohol after taking Plan B?
- How effective is Plan B and how late can you take it?
- What's the weight limit for Plan B?
- How many times can you take Plan B?
- Mirena, Kyleena, Skyla & Liletta - What's the difference?