Generic name: medically reviewed
Availability: Prescription only
Pregnancy & Lactation: Risk data available
What is Betaxolol (systemic) (monograph)?
Introduction
A β1-selective adrenergic blocking agent (β-blocker).
Uses for Betaxolol (Systemic)
Hypertension
Management of hypertension (alone or in combination with other classes of antihypertensive agents).
β-Blockers generally not preferred for first-line therapy of hypertension according to current evidence-based hypertension guidelines, but may be considered in patients who have a compelling indication (e.g., prior MI, ischemic heart disease, heart failure) for their use or as add-on therapy in those who do not respond adequately to the preferred drug classes (ACE inhibitors, angiotensin II receptor antagonists, calcium-channel blockers, or thiazide diuretics). A 2017 ACC/AHA multidisciplinary hypertension guideline states that β-blockers used for ischemic heart disease that are also effective in lowering BP include bisoprolol, carvedilol, metoprolol succinate, metoprolol tartrate, nadolol, propranolol, and timolol.
Individualize choice of therapy; consider patient characteristics (e.g., age, ethnicity/race, comorbidities, cardiovascular risk) as well as drug-related factors (e.g., ease of administration, availability, adverse effects, cost).
The 2017 ACC/AHA hypertension guideline classifies BP in adults into 4 categories: normal, elevated, stage 1 hypertension, and stage 2 hypertension. (See Table 1.)
Source: Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-115.
Individuals with SBP and DBP in 2 different categories (e.g., elevated SBP and normal DBP) should be designated as being in the higher BP category (i.e., elevated BP).
|
Category |
SBP (mm Hg) |
DBP (mm Hg) |
|
|---|---|---|---|
|
Normal |
<120 |
and |
<80 |
|
Elevated |
120–129 |
and |
<80 |
|
Hypertension, Stage 1 |
130–139 |
or |
80–89 |
|
Hypertension, Stage 2 |
≥140 |
or |
≥90 |
The goal of hypertension management and prevention is to achieve and maintain optimal control of BP. However, the BP thresholds used to define hypertension, the optimum BP threshold at which to initiate antihypertensive drug therapy, and the ideal target BP values remain controversial.
The 2017 ACC/AHA hypertension guideline generally recommends a target BP goal (i.e., BP to achieve with drug therapy and/or nonpharmacologic intervention) <130/80 mm Hg in all adults regardless of comorbidities or level of atherosclerotic cardiovascular disease (ASCVD) risk. In addition, an SBP goal of <130 mm Hg generally is recommended for noninstitutionalized ambulatory patients ≥65 years of age with an average SBP of ≥130 mm Hg. These BP goals are based upon clinical studies demonstrating continuing reduction of cardiovascular risk at progressively lower levels of SBP.
Other hypertension guidelines generally have based target BP goals on age and comorbidities. Guidelines such as those issued by the JNC 8 expert panel generally have targeted a BP goal of <140/90 mm Hg regardless of cardiovascular risk and have used higher BP thresholds and target BPs in elderly patients compared with those recommended by the 2017 ACC/AHA hypertension guideline.
Some clinicians continue to support previous target BPs recommended by JNC 8 due to concerns about the lack of generalizability of data from some clinical trials (e.g., SPRINT study) used to support the 2017 ACC/AHA hypertension guideline and potential harms (e.g., adverse drug effects, costs of therapy) versus benefits of BP lowering in patients at lower risk of cardiovascular disease.
Consider potential benefits of hypertension management and drug cost, adverse effects, and risks associated with the use of multiple antihypertensive drugs when deciding a patient's BP treatment goal.
For decisions regarding when to initiate drug therapy (BP threshold), the 2017 ACC/AHA hypertension guideline incorporates underlying cardiovascular risk factors. ASCVD risk assessment is recommended by ACC/AHA for all adults with hypertension.
ACC/AHA currently recommend initiation of antihypertensive drug therapy in addition to lifestyle/behavioral modifications at an SBP ≥140 mm Hg or DBP ≥90 mm Hg in adults who have no history of cardiovascular disease (i.e., primary prevention) and a low ASCVD risk (10-year risk <10%).
For secondary prevention in adults with known cardiovascular disease or for primary prevention in those at higher risk for ASCVD (10-year risk ≥10%), ACC/AHA recommend initiation of antihypertensive drug therapy at an average SBP ≥130 mm Hg or an average DBP ≥80 mm Hg.
Adults with hypertension and diabetes mellitus, chronic kidney disease (CKD), or age ≥65 years are assumed to be at high risk for cardiovascular disease; ACC/AHA state that such patients should have antihypertensive drug therapy initiated at a BP ≥130/80 mm Hg. Individualize drug therapy in patients with hypertension and underlying cardiovascular or other risk factors.
In stage 1 hypertension, experts state that it is reasonable to initiate drug therapy using the stepped-care approach in which one drug is initiated and titrated and other drugs are added sequentially to achieve the target BP. Initiation of antihypertensive therapy with 2 first-line agents from different pharmacologic classes recommended in adults with stage 2 hypertension and average BP >20/10 mm Hg above BP goal.
Black hypertensive patients generally tend to respond better to monotherapy with calcium-channel blockers or thiazide diuretics than to β-blockers. However, diminished response to β-blockers is largely eliminated when administered concomitantly with a thiazide diuretic.
Related/similar drugs
amlodipine, lisinopril, metoprolol, losartan, aspirin, furosemide, hydrochlorothiazideBetaxolol (Systemic) Dosage and Administration
General
-
Individualize dosage according to patient response and tolerance.
-
If long-term therapy is discontinued, reduce dosage gradually over a period of about 2 weeks. (See Abrupt Withdrawal of Therapy under Cautions.)
BP Monitoring and Treatment Goals
-
Monitor BP regularly (i.e., monthly) during therapy and adjust dosage of the antihypertensive drug until BP controlled.
-
If unacceptable adverse effects occur, discontinue drug and initiate another antihypertensive agent from a different pharmacologic class.
-
If adequate BP response not achieved with a single antihypertensive agent, either increase dosage of single drug or add a second drug with demonstrated benefit and preferably a complementary mechanism of action (e.g., ACE inhibitor, angiotensin II receptor antagonist, calcium-channel blocker, thiazide diuretic). Many patients will require ≥2 drugs from different pharmacologic classes to achieve BP goal; if goal BP still not achieved, add a third drug.
Administration
Oral Administration
Administer orally; absorption does not appear to be affected by food or alcohol.
Dosage
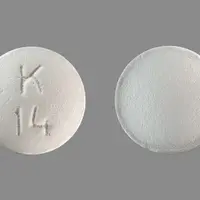
Available as betaxolol hydrochloride; dosage expressed in terms of the salt. Commercially available tablets containing 10 or 20 mg of betaxolol hydrochloride contain 8.94 or 17.88 mg of betaxolol, respectively.
Adults
Hypertension
Oral
Initially, 5–10 mg once daily, either alone or in combination with a diuretic. May double dosage after 7–14 days up to 20 mg daily.
Usual dosage range: Some experts state 5–20 mg once daily.
Prescribing Limits
Adults
Hypertension
Oral
Maximum 40 mg daily.
Special Populations
Hepatic Impairment
Dosage reductions are not routinely necessary. Use with caution; monitor patients carefully.
Renal Impairment
Initially, 5 mg once daily in those with severe impairment or undergoing dialysis. Increase dosage in increments of 5 mg daily, no more frequently than at 2-week intervals, up to a maximum of 20 mg daily.
Geriatric Patients
Initially, 5 mg daily.
Bronchospastic Disease
Use the lowest possible dosage (5–10 mg once daily).
If dosage must be increased, consider divided administration of the daily dose to avoid the higher peak plasma concentrations associated with once-daily dosing.
Warnings
Contraindications
-
Known hypersensitivity to betaxolol.
-
Patients with sinus bradycardia, heart block greater than first degree, cardiogenic shock, or overt cardiac failure.
Warnings/Precautions
Warnings
Heart Failure
Possible precipitation of heart failure.
Avoid use in patients with decompensated heart failure; may use cautiously in patients with inadequate myocardial function and, if necessary, in patients with well-compensated heart failure (e.g., those controlled with cardiac glycosides and/or diuretics).
Adequate treatment (e.g., with a cardiac glycoside and/or diuretic) and close observation recommended if signs or symptoms of impending heart failure occur; if heart failure continues, discontinue therapy, gradually if possible.
Abrupt Withdrawal of Therapy
Abrupt discontinuance of therapy is not recommended as it may exacerbate angina symptoms or precipitate MI in patients with CAD.
Gradually decrease dosage over a period of about 2 weeks and monitor patients carefully; advise patients to temporarily limit their physical activity during Withdrawal of therapy.
If exacerbation of angina occurs or acute coronary insufficiency develops, reinstitute therapy promptly and initiate appropriate measures for the management of unstable angina pectoris.
Bronchospastic Disease
Possible bronchoconstriction.
Generally should not be used in patients with bronchospastic disease, but may be used with caution in such patients who do not respond to or cannot tolerate alternative treatment.
Administer the lowest effective dosage (5–10 mg once daily); a bronchodilator (e.g., a β2-adrenergic agonist) should be available.
Major Surgery
Possible risks associated with general anesthesia (e.g., severe hypotension, difficulty maintaining heart beat) due to decreased ability of the heart to respond to reflex β-adrenergic stimuli. Use with caution in patients undergoing major surgery involving general anesthesia; anesthetics used should not cause myocardial depression.
Diabetes and Hypoglycemia
Possible decreased signs and symptoms of hypoglycemia (e.g., may mask tachycardia but not sweating or dizziness).
Use with caution in patients with diabetes mellitus receiving hypoglycemic drugs.
Thyrotoxicosis
Signs of hyperthyroidism (e.g., tachycardia) may be masked. Possible thyroid storm if therapy is abruptly withdrawn; carefully monitor patients having or suspected of developing thyrotoxicosis.
Sensitivity Reactions
Anaphylactic Reactions
Possible increased reactivity to repeated, accidental, diagnostic, or therapeutic challenges with a variety of allergens while taking β-blocking agents. Such patients may be unresponsive to usual doses of epinephrine.
General Precautions
Intraocular Pressure
Possible reduction in intraocular pressure. May interfere with glaucoma screening test; Withdrawal of therapy may cause return to increased intraocular pressure. (See Interactions.)
Specific Populations
Pregnancy
Category C.
Lactation
Distributed into milk. Use with caution.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
Possible increased incidence of bradycardia in patients >65 years of age compared with younger adults. Bradycardia (possibly dose related) may respond to dosage reduction. (See Geriatric Patients under Dosage and Administration.)
Hepatic Impairment
Although elimination half-life may be increased, clearance may remain unchanged, resulting in little change in the AUC. (See Hepatic Impairment under Dosage and Administration.)
Renal Impairment
Clearance may be decreased. Dosage adjustment may be needed based on degree of renal impairment. (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
Bradycardia, edema, headache, dizziness, fatigue, lethargy, insomnia, nervousness, bizarre dreams, impotence, dyspnea, pharyngitis, rhinitis, upper respiratory infection, dyspepsia, nausea, diarrhea, chest pain, arthralgia, rash.
How should I use Betaxolol (systemic) (monograph)
General
-
Individualize dosage according to patient response and tolerance.
-
If long-term therapy is discontinued, reduce dosage gradually over a period of about 2 weeks. (See Abrupt Withdrawal of Therapy under Cautions.)
BP Monitoring and Treatment Goals
-
Monitor BP regularly (i.e., monthly) during therapy and adjust dosage of the antihypertensive drug until BP controlled.
-
If unacceptable adverse effects occur, discontinue drug and initiate another antihypertensive agent from a different pharmacologic class.
-
If adequate BP response not achieved with a single antihypertensive agent, either increase dosage of single drug or add a second drug with demonstrated benefit and preferably a complementary mechanism of action (e.g., ACE inhibitor, angiotensin II receptor antagonist, calcium-channel blocker, thiazide diuretic). Many patients will require ≥2 drugs from different pharmacologic classes to achieve BP goal; if goal BP still not achieved, add a third drug.
Administration
Oral Administration
Administer orally; absorption does not appear to be affected by food or alcohol.
Dosage
Available as betaxolol hydrochloride; dosage expressed in terms of the salt. Commercially available tablets containing 10 or 20 mg of betaxolol hydrochloride contain 8.94 or 17.88 mg of betaxolol, respectively.
Adults
Hypertension
Oral
Initially, 5–10 mg once daily, either alone or in combination with a diuretic. May double dosage after 7–14 days up to 20 mg daily.
Usual dosage range: Some experts state 5–20 mg once daily.
Prescribing Limits
Adults
Hypertension
Oral
Maximum 40 mg daily.
Special Populations
Hepatic Impairment
Dosage reductions are not routinely necessary. Use with caution; monitor patients carefully.
Renal Impairment
Initially, 5 mg once daily in those with severe impairment or undergoing dialysis. Increase dosage in increments of 5 mg daily, no more frequently than at 2-week intervals, up to a maximum of 20 mg daily.
Geriatric Patients
Initially, 5 mg daily.
Bronchospastic Disease
Use the lowest possible dosage (5–10 mg once daily).
If dosage must be increased, consider divided administration of the daily dose to avoid the higher peak plasma concentrations associated with once-daily dosing.
What other drugs will affect Betaxolol (systemic) (monograph)?
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
β-Blockers (ophthalmic solution) |
Possible additive effects on intraocular pressure or systemic β blockade |
|
|
Calcium-channel blocking agents |
Potential hypotension, AV conduction disturbances, and left ventricular failure |
Avoid concomitant use in patients with impaired cardiac function |
|
Chlorthalidone |
Pharmacokinetic interaction unlikely |
|
|
Cimetidine |
Pharmacokinetic interaction unlikely |
|
|
Clonidine |
β-Adrenergic blockade may exacerbate rebound hypertension following discontinuance of clonidine |
Discontinue β-blockers several days before initiating gradual Withdrawal of clonidine If replacing clonidine, delay initiation of the β-blocker for several days after stopping clonidine |
|
Hydrochlorothiazide |
Pharmacokinetic interaction unlikely |
|
|
Nifedipine |
Pharmacokinetic interaction unlikely |
|
|
Reserpine |
Additive effects |
Monitor for signs of hypotension and bradycardia (e.g., vertigo, syncope, postural hypotension) |
|
Warfarin |
No potentiation of anticoagulant effect |