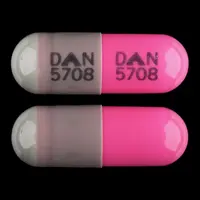
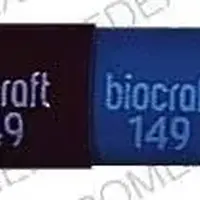
Generic name: cleocin hcl
Availability: Prescription only
Pregnancy & Lactation: Risk data available
Brand names: Clindamycin, Cleocin
What is Clindamycin (systemic) (monograph)?
Warning
- Diarrhea and Colitis
-
Clostridium difficile-associated diarrhea and colitis (CDAD; also known as antibiotic-associated diarrhea and colitis or pseudomembranous colitis) has been reported with nearly all anti-infectives, including clindamycin, and may range in severity from mild to life-threatening. Anti-infectives alter normal flora of the colon and may permit overgrowth of C. difficile.
-
Because clindamycin has been associated with severe colitis (potentially fatal), it should be reserved for treatment of serious infections when less toxic anti-infectives are inappropriate. Do not use for nonbacterial infections. (See Uses.)
-
C. difficile produces toxins A and B which contribute to development of CDAD. Hypertoxin-producing strains cause increased morbidity and mortality since they may be refractory to anti-infectives and may require colectomy. CDAD must be considered in all patients who present with diarrhea following anti-infective use. Careful medical history is necessary since CDAD has been reported to occur 2 months or longer after administration of anti-infectives.
-
If CDAD is suspected or confirmed, ongoing anti-infective use not directed against C. difficile may need to be discontinued. Institute appropriate fluid and electrolyte management, protein supplementation, anti-infective treatment of C. difficile, and surgical evaluation as clinically indicated. (See Superinfection/Clostridium difficile-associated Diarrhea and Colitis [CDAD] under Cautions.)
Introduction
Antibacterial; lincosamide antibiotic derived from lincomycin.
Uses for Clindamycin (Systemic)
Acute Otitis Media (AOM)
Alternative for treatment of AOM† [off-label].
When anti-infectives indicated, AAP recommends high-dose amoxicillin or amoxicillin and clavulanate as drugs of first choice for initial treatment of AOM; certain cephalosporins (cefdinir, cefpodoxime, cefuroxime, ceftriaxone) recommended as alternatives for initial treatment in penicillin-allergic patients without a history of severe and/or recent penicillin-allergic reactions.
AAP states clindamycin (with or without a third generation cephalosporin) is a possible alternative for treatment of AOM in patients who fail to respond to initial treatment with first-line or preferred alternatives.
May be effective in infections caused by penicillin-resistant Streptococcus pneumoniae; may not be effective against multidrug-resistant S. pneumoniae and usually inactive against Haemophilus influenzae. If used for retreatment of AOM, consider concomitant use of an anti-infective active against H. influenzae and Moraxella catarrhalis (e.g., cefdinir, cefixime, cefuroxime).
Bone and Joint Infections
Treatment of serious bone and joint infections (including acute hematogenous osteomyelitis) caused by susceptible Staphylococcus aureus or anaerobes.
Adjunct in the surgical treatment of chronic bone and joint infections caused by susceptible bacteria.
Gynecologic Infections
Treatment of serious gynecologic infections (e.g., endometritis, nongonococcal tubo-ovarian abscess, pelvic cellulitis, postsurgical vaginal cuff infection) caused by susceptible anaerobes.
Treatment of pelvic inflammatory disease (PID); used in conjunction with other anti-infectives. When a parenteral regimen is indicated for treatment of PID, IV clindamycin in conjunction with IV or IM gentamicin is one of several recommended regimens.
Intra-abdominal Infections
Treatment of serious intra-abdominal infections (e.g., peritonitis, intra-abdominal abscess) caused by susceptible anaerobes.
No longer routinely recommended for treatment of intra-abdominal infections because of increasing incidence of Bacteroides fragilis resistant to clindamycin.
Pharyngitis and Tonsillitis
Alternative for treatment of pharyngitis and tonsillitis† [off-label] caused by susceptible S. pyogenes (group A β-hemolytic streptococci; GAS) in patients who cannot receive β-lactam anti-infectives.
AAP, IDSA, and AHA recommend a penicillin regimen (10 days of oral penicillin V or oral amoxicillin or single dose of IM penicillin G benzathine) as treatment of choice for S. pyogenes pharyngitis and tonsillitis; other anti-infectives (oral cephalosporins, oral macrolides, oral clindamycin) recommended as alternatives in penicillin-allergic patients.
Respiratory Tract Infections
Treatment of serious respiratory tract infections (e.g., pneumonia, empyema, lung abscess) caused by susceptible S. aureus, S. pneumoniae, other streptococci, or anaerobes.
IDSA and ATS consider clindamycin an alternative for treatment of community-acquired pneumonia (CAP) caused by S. pneumoniae or S. aureus (methicillin-susceptible strains) in adults. IDSA also considers clindamycin an alternative for treatment of CAP caused by S. pneumoniae, S. pyogenes, or S. aureus in pediatric patients. For treatment of pneumonia caused by methicillin-resistant S. aureus (MRSA; also known as oxacillin-resistant S. aureus or ORSA), IDSA states clindamycin is one of several options, unless the strain is resistant to clindamycin.
For information on treatment of CAP, consult current IDSA clinical practice guidelines available at [Web].
Septicemia
Treatment of serious septicemia caused by S. aureus, streptococci, or anaerobes.
Skin and Skin Structure Infections
Treatment of serious skin and skin structure infections caused by susceptible staphylococci, S. pneumoniae, other streptococci, or anaerobes. One of several preferred drugs for treatment of staphylococcal and streptococcal skin and skin structure infections, including those known or suspected to be caused by susceptible MRSA.
Treatment of clostridial myonecrosis† [off-label] (gas gangrene) caused by Clostridium perfringens or other Clostridium; used in conjunction with or as alternative to penicillin G.
Alternative for treatment of infected human or animal (e.g., dog, cat, reptile) bite wounds; used in conjunction with either an extended-spectrum cephalosporin or co-trimoxazole. Purulent bite wounds usually are polymicrobial and broad-spectrum anti-infective coverage recommended. Nonpurulent infected bite wounds usually caused by staphylococci and streptococci, but can be polymicrobial.
For information on treatment of skin and skin structure infections, consult current IDSA clinical practice guidelines available at [Web].
Actinomycosis
Alternative to penicillin G or ampicillin for treatment of actinomycosis† [off-label], including infections caused by Actinomyces israelii.
Anthrax
Alternative for treatment of anthrax† [off-label].
Component of multiple-drug parenteral regimens recommended for treatment of inhalational anthrax that occurs as the result of exposure to B. anthracis spores in the context of biologic warfare or bioterrorism. Initiate treatment with IV ciprofloxacin or doxycycline and 1 or 2 other anti-infective agents predicted to be effective (e.g., chloramphenicol, clindamycin, rifampin, vancomycin, clarithromycin, imipenem, penicillin, ampicillin); if meningitis is established or suspected, use IV ciprofloxacin (rather than doxycycline) and chloramphenicol, rifampin, or penicillin.
Based on in vitro data, possible alternative for postexposure prophylaxis following a suspected or confirmed exposure to aerosolized anthrax spores† (inhalational anthrax) when drugs of choice (ciprofloxacin, doxycycline) not tolerated or cannot be used.
Babesiosis
Treatment of babesiosis† caused by Babesia microti or other Babesia.
Regimens of choice for babesiosis are clindamycin in conjunction with quinine or atovaquone in conjunction with azithromycin. Clindamycin and quinine regimen generally preferred for severe babesiosis caused by B. microti and infections caused by M. divergens, B. duncani, B. divergens-like organisms, or B. venatorum.
Also consider exchange transfusions in severely ill patients with high levels of parasitemia (>10%), significant hemolysis, or compromised renal, hepatic, or pulmonary function.
Bacterial Vaginosis
Treatment of bacterial vaginosis† (formerly called Haemophilus vaginitis, Gardnerella vaginitis, nonspecific vaginitis, Corynebacterium vaginitis, or anaerobic vaginosis).
CDC and others recommend treatment of bacterial vaginosis in all symptomatic women (including pregnant women).
Regimens of choice are 7-day regimen of oral metronidazole; 5-day regimen of intravaginal metronidazole gel; or 7-day regimen of intravaginal clindamycin cream. Alternative regimens are 2- or 5-day regimen of oral tinidazole; 7-day regimen of oral clindamycin; or 3-day regimen of intravaginal clindamycin suppositories. Preferred regimens for pregnant women are the oral or intravaginal metronidazole or clindamycin regimens.
Regardless of treatment regimen used, relapse or recurrence is common; retreatment with the same or an alternative regimen (e.g., oral therapy when topical was used initially) may be used in such situations.
Malaria
Treatment of uncomplicated malaria† caused by chloroquine-resistant Plasmodium falciparum or when plasmodial species not identified. Used in conjunction with oral quinine; not effective alone.
CDC and others state treatments of choice for uncomplicated chloroquine-resistant P. falciparum malaria or when plasmodial species not identified are the fixed combination of atovaquone and proguanil hydrochloride (atovaquone/proguanil); the fixed combination of artemether and lumefantrine (artemether/lumefantrine); or a regimen of oral quinine in conjunction with doxycycline, tetracycline, or clindamycin. When a quinine regimen used, concomitant doxycycline or tetracycline generally preferred over concomitant clindamycin (more efficacy data available regarding regimens that include a tetracycline); clindamycin preferred in young children or pregnant women who should not receive tetracyclines.
Treatment of severe malaria caused by P. falciparum†; used in conjunction with IV quinidine gluconate initially and then with oral quinine when an oral regimen tolerated. Severe malaria requires aggressive antimalarial treatment initiated as soon as possible after diagnosis.
Assistance with diagnosis or treatment of malaria is available from CDC Malaria Hotline at 770-488-7788 or 855-856-4713 from 9:00 a.m. to 5:00 p.m. Eastern Standard Time or CDC Emergency Operation Center at 770-488-7100 after hours and on weekends and holidays.
Pneumocystis jirovecii Pneumonia
Treatment of Pneumocystis jirovecii (formerly Pneumocystis carinii) pneumonia† (PCP); used in conjunction with primaquine. Designated an orphan drug by FDA for treatment of PCP associated with acquired immunodeficiency syndrome (AIDS).
Co-trimoxazole is drug of choice for treatment of mild, moderate, or severe PCP, including PCP in HIV-infected adults, adolescents, and children. Regimen of primaquine and clindamycin is an alternative for treatment of mild, moderate, or severe PCP in HIV-infected adults and adolescents who have had an inadequate response to co-trimoxazole or when co-trimoxazole is contraindicated or not tolerated. Although data not available regarding use in children, regimen of primaquine and clindamycin also can be considered an alternative to co-trimoxazole in HIV-infected children based on data in adults.
Regimen of primaquine and clindamycin not recommended for prevention of initial episodes (primary prophylaxis) or long-term suppressive or chronic maintenance therapy (secondary prophylaxis) of PCP. Co-trimoxazole is drug of choice for primary and secondary prophylaxis of PCP in HIV-infected adults, adolescents, and children.
Toxoplasmosis
Alternative for treatment of toxoplasmosis† caused by Toxoplasma gondii in immunocompromised adults, adolescents, and children (including HIV-infected patients); used in conjunction with pyrimethamine (and leucovorin). CDC, NIH, IDSA, and AAP recommend pyrimethamine (and leucovorin) used in conjunction with sulfadiazine as regimen of choice for initial treatment of toxoplasmosis in HIV-infected adults and adolescents, treatment of congenital toxoplasmosis, and treatment of acquired CNS, ocular, or systemic toxoplasmosis in HIV-infected children. Pyrimethamine (and leucovorin) used in conjunction with clindamycin is the preferred alternative in those unable to tolerate sulfadiazine or who fail to respond to initial regimen.
Alternative for long-term suppressive or chronic maintenance therapy (secondary prophylaxis) to prevent relapse of toxoplasmosis† in HIV-infected adults, adolescents, and children who have completed treatment for the disease; used in conjunction with pyrimethamine and leucovorin. Pyrimethamine (and leucovorin) used in conjunction with sulfadiazine is regimen of choice for secondary prophylaxis. Pyrimethamine (and leucovorin) used in conjunction with clindamycin is one of several alternatives in those who cannot tolerate sulfonamides.
Perioperative Prophylaxis
Alternative for perioperative prophylaxis† to reduce the incidence of infections in patients undergoing certain clean, contaminated surgeries when drugs of choice (e.g., cefazolin, cefuroxime, cefoxitin, cefotetan) cannot be used because of hypersensitivity to β-lactam anti-infectives.
Experts state clindamycin or vancomycin is a reasonable alternative for perioperative prophylaxis in patients allergic to β-lactam anti-infectives who are undergoing cardiac surgery (e.g., CABG, valve repairs, cardiac device implantation), neurosurgery (e.g., craniotomy, spinal and CSF-shunting procedures, intrathecal pump placement), orthopedic surgery (e.g., spinal procedures, hip fracture, internal fixation, total joint replacement), non-cardiac thoracic surgery (e.g., lobectomy, pneumonectomy, lung resection, thoracotomy), vascular surgery (e.g., arterial procedures involving a prosthesis, the abdominal aorta, or a groin incision), lower extremity amputation for ischemia, or certain transplant procedures (e.g., heart and/or lung). Clindamycin also a reasonable alternative for perioperative prophylaxis in such patients undergoing head and neck surgery (e.g., incisions through oral or pharyngeal mucosa).
For procedures that might involve exposure to enteric gram-negative bacteria, experts state that clindamycin or vancomycin used in conjunction with an aminoglycoside (e.g., amikacin, gentamicin, tobramycin), aztreonam, or a fluoroquinolone is a reasonable alternative in patients allergic to β-lactam anti-infectives. These procedures include certain GI and biliary tract procedures (e.g., esophageal or gastroduodenal procedures, appendectomy for uncomplicated appendicitis, surgery involving unobstructed small intestine, colorectal procedures), gynecologic and obstetric surgery (e.g., cesarean section, hysterectomy), urologic procedures involving an implanted prosthesis, and certain transplant procedures (e.g., liver, pancreas and/or kidney).
Prevention of Bacterial Endocarditis
Alternative to amoxicillin or ampicillin for prevention of α-hemolytic (viridans group) streptococcal bacterial endocarditis† in penicillin-allergic patients undergoing certain dental procedures (i.e., procedures that involve manipulation of gingival tissue, the periapical region of teeth, or perforation of oral mucosa) or certain invasive respiratory tract procedures (i.e., procedures involving incision or biopsy of respiratory mucosa) who have certain cardiac conditions that put them at highest risk of adverse outcomes from endocarditis.
Anti-infective prophylaxis solely for prevention of bacterial endocarditis no longer recommended by AHA for patients undergoing GU or GI procedures.
Cardiac conditions identified by AHA as associated with highest risk of adverse outcomes from endocarditis: Prosthetic cardiac valves or prosthetic material used for cardiac valve repair, previous infective endocarditis, certain forms of congenital heart disease, and cardiac valvulopathy after cardiac transplantation.
Consult most recent AHA recommendations for additional information on which cardiac conditions are associated with highest risk of adverse outcomes from endocarditis and specific recommendations regarding use of prophylaxis to prevent endocarditis in these patients.
Prevention of Perinatal Group B Streptococcal Disease
Alternative to penicillin G or ampicillin for prevention of perinatal group B streptococcal (GBS) disease† in penicillin-allergic pregnant women at high risk for anaphylaxis if they receive a β-lactam anti-infective.
Intrapartum anti-infective prophylaxis to prevent early-onset neonatal GBS disease is administered to women identified as GBS carriers during routine prenatal GBS screening performed at 35–37 weeks of gestation during the current pregnancy and to women who have GBS bacteriuria during the current pregnancy, a previous infant with invasive GBS disease, unknown GBS status with delivery at <37 weeks of gestation, amniotic membrane rupture for ≥18 hours, or intrapartum temperature of ≥38°C.
Penicillin G is drug of choice and ampicillin is the preferred alternative for anti-infective prophylaxis of GBS. Cefazolin is recommended for GBS prophylaxis in penicillin-allergic women who do not have immediate-type penicillin hypersensitivity; clindamycin or, alternatively, vancomycin is recommended for such prophylaxis in penicillin-allergic women at high risk for anaphylaxis (e.g., history of anaphylaxis, angioedema, respiratory distress, or urticaria after receiving a penicillin or cephalosporin).
Consider that S. agalactiae (group B streptococci; GBS) with in vitro resistance to clindamycin has been reported with increasing frequency; perform in vitro susceptibility tests of clinical isolates obtained during GBS prenatal screening. GBS isolates susceptible to clindamycin but resistant to erythromycin in vitro should be evaluated for inducible clindamycin resistance. If GBS isolate is intrinsically resistant to clindamycin, demonstrates inducible resistance to clindamycin, or if susceptibility to clindamycin and erythromycin are unknown, use vancomycin instead of clindamycin for GBS prophylaxis.
Consult most recent CDC and AAP guidelines for additional information on prevention of perinatal GBS disease.
Related/similar drugs
prednisone, amoxicillin, doxycycline, ciprofloxacin, cephalexin, metronidazole, azithromycinClindamycin (Systemic) Dosage and Administration
Administration
Administer orally, IM, or by intermittent or continuous IV infusion. Do not administer by rapid IV injection.
In the treatment of serious anaerobic infections, parenteral route usually used initially but may be switched to oral route when warranted by patient’s condition. In clinically appropriate circumstances, oral route may be used initially.
Clindamycin phosphate ADD-Vantage vials and commercially available premixed solutions of clindamycin phosphate in 5% dextrose should be used only for IV infusion.
For solution and drug compatibility information, see Compatibility under Stability.
Oral Administration
Clindamycin hydrochloride capsules and clindamycin palmitate hydrochloride oral solution can be administered without regard to food.
To avoid the possibility of esophageal irritation, administer clindamycin hydrochloride capsules with a full glass of water. Swallow capsules whole; do not use in pediatric patients unable to swallow capsules.
Reconstitution
Reconstitute clindamycin palmitate hydrochloride powder (granules) for oral solution by adding 75 mL of water to the 100-mL bottle. Add a large portion of the water initially and shake bottle vigorously; add remainder of the water and shake bottle until solution is uniform. The resulting oral solution contains 75 mg of clindamycin/5 mL.
IM Injection
For IM injection, administer clindamycin phosphate solution containing 150 mg of clindamycin per mL undiluted.
Single IM doses should not exceed 600 mg.
IV Infusion
Prior to IV infusion, clindamycin phosphate solutions (including solutions provided in ADD-Vantage vials) must be diluted with a compatible IV solution to a concentration ≤18 mg/mL.
Usually administered by intermittent IV infusion. Alternatively, may be given by continuous IV infusion in adults after first dose is given by rapid IV infusion. (See Table 1.)
Commercially available premixed solutions of clindamycin phosphate in 5% dextrose are administered only by IV infusion. Discard premixed solution if container seal is not intact or leaks are found or if the solution is not clear. Do not introduce additives into the container. Do not use flexible containers in series connections with other plastic containers; such use could result in air embolism from residual air being drawn from the primary container before administration of the fluid from the secondary container is complete.
Dilution
Clindamycin phosphate solution containing 150 mg of clindamycin per mL: Dilute appropriate dose in a compatible IV infusion solution and administer using the recommended rate of administration. (See Rate of Administration under Dosage and Administration.)
Clindamycin phosphate solution provided in ADD-Vantage vials: Dilute according to directions provided by the manufacturer. ADD-Vantage vials are for IV infusion only.
Clindamycin phosphate pharmacy bulk package: Dilute in a compatible IV infusion solution; not intended for direct IV infusion. Bulk package is intended for use only under a laminar flow hood. Entry into the vial should be made using a sterile transfer set or other sterile dispensing device, and the contents dispensed in aliquots using appropriate technique; multiple entries with a syringe and needle are not recommended because of the increased risk of microbial and particulate contamination. After entry into the bulk package vial, use entire contents promptly; discard any unused portion within 24 hours after initial entry.
Rate of Administration
Give intermittent IV infusions over a period of at least 10–60 minutes and at a rate ≤30 mg/minute. Give no more than 1.2 g by IV infusion in a single 1-hour period.
Dilute 300-mg doses in 50 mL of compatible diluent and infuse over 10 minutes; dilute 600-mg doses in 50 mL of diluent and infuse over 20 minutes; dilute 900-mg doses in 50–100 mL of diluent and infuse over 30 minutes; dilute 1.2-g doses in 100 mL of diluent and infuse over 40 minutes.
As an alternative to intermittent IV infusions in adults, the drug can be given by continuous IV infusion after an initial dose is given by IV infusion over 30 minutes. (See Table 1.)
|
Target Serum Clindamycin Concentrations |
Infusion Rate for Initial Dose |
Maintenance Infusion Rate |
|---|---|---|
|
>4 mcg/mL |
10 mg/minute for 30 minutes |
0.75 mg/minute |
|
>5 mcg/mL |
15 mg/minute for 30 minutes |
1 mg/minute |
|
>6 mcg/mL |
20 mg/minute for 30 minutes |
1.25 mg/minute |
Dosage
Available as clindamycin hydrochloride, clindamycin palmitate hydrochloride, and clindamycin phosphate; dosage expressed in terms of clindamycin.
Pediatric Patients
General Dosage in Neonates
Oral
Oral solution: Manufacturer recommends 8–12 mg/kg daily for serious infections, 13–16 mg/kg daily for severe infections, and 17–25 mg/kg daily for more severe infections. Give daily dosage in 3 or 4 equally divided doses. In children weighing ≤10 kg, manufacturer recommends a minimum dosage of 37.5 mg 3 times daily.
Neonates ≤7 days of age: AAP recommends 5 mg/kg every 12 hours in those weighing ≤2 kg or 5 mg/kg every 8 hours in those weighing >2 kg.
Neonates 8–28 days of age: AAP recommends 5 mg/kg every 8 hours in those weighing ≤2 kg or 5 mg/kg every 6 hours in those weighing >2 kg. In extremely low-birthweight neonates (<1 kg), consider 5 mg/kg every 12 hours until 2 weeks of age.
IV or IM
Neonates <1 month of age: Manufacturer recommends 15–20 mg/kg daily given in 3 or 4 equally divided doses. The lower dosage may be adequate for small, premature neonates.
Neonates ≤7 days of age: AAP recommends 5 mg/kg every 12 hours in those weighing ≤2 kg or 5 mg/kg every 8 hours in those weighing >2 kg.
Neonates 8–28 days of age: AAP recommends 5 mg/kg every 8 hours in those weighing ≤2 kg or 5 mg/kg every 6 hours in those weighing >2 kg. In extremely low-birthweight neonates (<1 kg), consider 5 mg/kg every 12 hours until 2 weeks of age.
General Dosage in Children 1 Month to 16 Years of Age
Oral
Capsules: Manufacturer recommends 8–16 mg/kg daily given in 3 or 4 equally divided doses for serious infections or 16–20 mg/kg daily given in 3 or 4 equally divided doses for more severe infections.
Oral solution: Manufacturer recommends 8–12 mg/kg daily for serious infections, 13–16 mg/kg daily for severe infections, or 17–25 mg/kg daily for more severe infections. Give daily dosage in 3 or 4 equally divided doses. In children weighing ≤10 kg, manufacturer recommends a minimum dosage of 37.5 mg 3 times daily.
AAP recommends 10–20 mg/kg daily given in 3 or 4 equally divided doses for mild to moderate infections or 30–40 mg/kg daily given in 3 or 4 equally divided doses for severe infections.
IV or IM
Manufacturer recommends 20–40 mg/kg daily given in 3 or 4 equally divided doses; use the higher dosage for more severe infections. Alternatively, manufacturer recommends 350 mg/m2 daily for serious infections or 450 mg/m2 daily for more severe infections.
AAP recommends 20–30 mg/kg daily given in 3 equally divided doses for mild to moderate infections or 40 mg/kg daily given in 3 or 4 equally divided doses for severe infections.
Acute Otitis Media† (AOM)
Oral
Children 6 months through 12 years of age: 30–40 mg/kg daily in 3 divided doses recommended by AAP. Use with or without a third generation cephalosporin. (See Acute Otitis Media under Uses.)
Pharyngitis and Tonsillitis†
Oral
AAP recommends 10 mg/kg 3 times daily (up to 900 mg daily) for 10 days.
IDSA recommends 7 mg/kg (up to 300 mg) 3 times daily for 10 days.
AHA recommends 20 mg/kg daily (up to 1.8 g daily) in 3 divided doses given for 10 days.
Respiratory Tract Infections
Oral
Children >3 months of age: IDSA recommends 30–40 mg/kg daily given in 3 or 4 divided doses.
IM or IV
Children >3 months of age: IDSA recommends 40 mg/kg daily given in divided doses every 6–8 hours.
Babesiosis†
Oral
IDSA recommends 7–10 mg/kg (up to 600 mg) every 6–8 hours for 7–10 days; used in conjunction with oral quinine sulfate (8 mg/kg [up to 650 mg] every 8 hours for 7–10 days). Others recommend 20–40 mg/kg (up to 600 mg) daily in 3 or 4 divided doses for 7–10 days; used in conjunction with oral quinine sulfate (24 mg/kg daily in 3 divided doses for 7–10 days).
IV
IDSA recommends 7–10 mg/kg (up to 600 mg) every 6–8 hours for 7–10 days; used in conjunction with oral quinine sulfate (8 mg/kg [up to 650 mg] every 8 hours for 7–10 days). Others recommend 20–40 mg/kg (up to 600 mg) daily in 3 or 4 divided doses for 7–10 days; used in conjunction with oral quinine sulfate (24 mg/kg daily in 3 divided doses for 7–10 days).
Malaria†
Treatment of Uncomplicated Chloroquine-resistant P. falciparum Malaria†
Oral20 mg/kg daily in 3 equally divided doses given for 7 days; used in conjunction with oral quinine sulfate (10 mg/kg 3 times daily given for 7 days if acquired in Southeast Asia or 3 days if acquired elsewhere).
Treatment of Severe P. falciparum Malaria†
Oral20 mg/kg daily in 3 equally divided doses given for 7 days; used in conjunction with IV quinidine gluconate (followed by oral quinine sulfate) given for a total duration of 3–7 days.
IV, then Oral10-mg/kg IV loading dose followed by 5 mg/kg IV every 8 hours; when oral therapy is tolerated, switch to oral clindamycin 20 mg/kg daily in 3 divided doses and continue for a total duration of 7 days.
Used in conjunction with IV quinidine gluconate (followed by oral quinine sulfate) given for a total duration of 3–7 days.
Pneumocystis jirovecii Pneumonia†
Treatment of Mild to Moderate Infections†
OralChildren: 10 mg/kg (up to 300–450 mg) every 6 hours given for 21 days; used in conjunction with oral primaquine (0.3 mg/kg once daily [up to 30 mg daily] for 21 days).
Adolescents: 450 mg every 6 hours or 600 mg every 8 hours given for 21 days; used in conjunction with oral primaquine (30 mg once daily for 21 days).
IVChildren: 10 mg/kg (up to 600 mg) every 6 hours given for 21 days; used in conjunction with oral primaquine (0.3 mg/kg once daily [up to 30 mg daily] for 21 days).
Adolescents: 600 mg every 6 hours or 900 mg every 8 hours given for 21 days; used in conjunction with oral primaquine (30 mg once daily for 21 days).
Toxoplasmosis†
Congenital Toxoplasmosis†
Oral or IV5–7.5 mg/kg (up to 600 mg) 4 times daily; used in conjunction with oral pyrimethamine (2 mg/kg once daily for 2 days followed by 1 mg/kg once daily) and oral or IM leucovorin (10 mg with each pyrimethamine dose).
Optimal duration not determined; some experts recommend continuing treatment for 12 months.
Treatment in Infants and Children†
Oral or IV5–7.5 mg/kg (up to 600 mg) 4 times daily; used in conjunction with oral pyrimethamine (2 mg/kg once daily for 2 days followed by 1 mg/kg once daily) and oral or IM leucovorin (10 mg with each pyrimethamine dose).
Continue acute treatment for ≥6 weeks; longer duration may be appropriate if disease is extensive or response incomplete at 6 weeks.
Treatment in Adolescents†
Oral or IV600 mg every 6 hours; used in conjunction with oral pyrimethamine (200-mg loading dose followed by 50 mg once daily in those <60 kg or 75 mg once daily in those ≥60 kg) and oral leucovorin (10–25 mg once daily; may be increased to 50 mg once or twice daily).
Continue acute treatment for ≥6 weeks; longer duration may be appropriate if disease is extensive or response incomplete at 6 weeks.
Prevention of Recurrence (Secondary Prophylaxis) in Infants and Children†
Oral7–10 mg/kg 3 times daily; used in conjunction with oral pyrimethamine (1 mg/kg or 15 mg/m2 [up to 25 mg] once daily) and oral leucovorin (5 mg once every 3 days).
Initiate long-term suppressive therapy or chronic maintenance therapy (secondary prophylaxis) in all patients after completion of acute treatment of toxoplasmosis.
Safety of discontinuing secondary toxoplasmosis prophylaxis in HIV-infected infants and children receiving potent antiretroviral therapy not extensively studied. Consider discontinuing secondary prophylaxis in HIV-infected children 1 to <6 years of age who have completed toxoplasmosis acute treatment, have received >6 months of stable antiretroviral therapy, are asymptomatic with respect to toxoplasmosis, and have CD4+ T-cell percentages that have remained >15% for >6 consecutive months. In HIV-infected children ≥6 years of age who have received >6 months of antiretroviral therapy, consider discontinuing secondary prophylaxis if CD4+ T-cell counts have remained >200/mm3 for >6 consecutive months. Reinitiate secondary prophylaxis if these parameters not met.
Prevention of Recurrence (Secondary Prophylaxis) in Adolescents†
OralDosage for secondary prophylaxis against toxoplasmosis in adolescents and criteria for initiation or discontinuance of such prophylaxis in this age group are the same as those recommended for adults. (See Adult Dosage under Dosage and Administration.)
Perioperative Prophylaxis†
IV
10 mg/kg given within 60 minutes prior to incision. Used with or without another anti-infective. (See Perioperative Prophylaxis under Uses.)
May give additional intraoperative doses every 6 hours during prolonged procedures; postoperative doses generally not recommended.
Prevention of Bacterial Endocarditis†
Patients Undergoing Certain Dental or Respiratory Tract Procedures†
Oral20 mg/kg as a single dose given 30–60 minutes prior to the procedure.
IM or IV20 mg/kg as a single dose given 30–60 minutes prior to the procedure.
Adults
General Adult Dosage
Serious Infections
Oral150–300 mg every 6 hours.
IV or IM600 mg to 1.2 g daily in 2–4 equally divided doses.
More Severe Infections
Oral300–450 mg every 6 hours.
IV or IM1.2–2.7 g daily in 2–4 equally divided doses.
For life-threatening infections, IV dosage may be increased up 4.8 g daily.
Gynecologic Infections
Pelvic Inflammatory Disease
IV, then OralInitially, 900 mg IV every 8 hours; used in conjunction with IV or IM gentamicin. After clinical improvement occurs, discontinue IV clindamycin and gentamicin and switch to oral clindamycin in a dosage of 450 mg 4 times daily to complete 14 days of therapy. Alternatively, oral doxycycline can be used to complete 14 days of therapy.
Pharyngitis and Tonsillitis†
Oral
IDSA recommends 7 mg/kg (up to 300 mg) 3 times daily for 10 days.
AHA recommends 20 mg/kg daily (up to 1.8 g daily) in 3 divided doses given for 10 days.
Respiratory Tract Infections
Oral
IDSA recommends 600 mg 3 times daily for 7–21 days.
IV
IDSA recommends 600 mg 3 times daily for 7–21 days.
Anthrax†
Treatment of Inhalational Anthrax†
IV900 mg every 8 hours.
Used in multiple-drug regimens that initially include IV ciprofloxacin or IV doxycycline and 1 or 2 other anti-infectives predicted to be effective.
Duration of treatment is 60 days if anthrax occurred as the result of exposure to anthrax spores in the context of biologic warfare or bioterrorism.
Babesiosis†
Oral
IDSA and others recommend 600 mg every 8 hours given for 7–10 days; used in conjunction with oral quinine sulfate (650 mg every 6 or 8 hours for 7–10 days).
IV
IDSA and others recommend 300–600 mg every 6 hours given for 7–10 days; used in conjunction with oral quinine sulfate (650 mg every 6 or 8 hours for 7–10 days).
Bacterial Vaginosis†
Treatment in Pregnant or Nonpregnant Women†
Oral300 mg twice daily given for 7 days.
Malaria†
Treatment of Uncomplicated Chloroquine-resistant P. falciparum Malaria†
Oral20 mg/kg daily in 3 equally divided doses given for 7 days; used in conjunction with oral quinine sulfate (650 mg 3 times daily given for 7 days if acquired in Southeast Asia or 3 days if acquired elsewhere).
Treatment of Severe P. falciparum Malaria†
Oral20 mg/kg daily in 3 equally divided doses given for 7 days; used in conjunction with IV quinidine gluconate (followed by oral quinine sulfate) given for a total duration of 3–7 days.
IV, then Oral10-mg/kg IV loading dose followed by 5 mg/kg IV every 8 hours; when oral therapy is tolerated, switch to oral clindamycin 20 mg/kg daily in 3 divided doses and continue for a total duration of 7 days.
Used in conjunction with IV quinidine gluconate (followed by oral quinine sulfate) given for a total duration of 3–7 days.
Pneumocystis jirovecii Pneumonia†
Treatment of Mild to Moderate Infections†
Oral450 mg every 6 hours or 600 mg every 8 hours given for 21 days; used in conjunction with oral primaquine (30 mg once daily for 21 days).
IV600 mg every 6 hours or 900 mg every 8 hours given for 21 days; used in conjunction with oral primaquine (30 mg once daily for 21 days).
Toxoplasmosis†
Treatment†
Oral or IV600 mg every 6 hours; used in conjunction with oral pyrimethamine (200-mg loading dose followed by 50 mg once daily in those <60 kg or 75 mg once daily in those ≥60 kg) and oral leucovorin (10–25 mg once daily; may be increased to 50 mg once or twice daily).
Continue acute treatment for ≥6 weeks; longer duration may be appropriate if disease is extensive or response incomplete at 6 weeks.
Prevention of Recurrence (Secondary Prophylaxis)†
Oral600 mg every 8 hours; used in conjunction with oral pyrimethamine (25–50 mg once daily) and oral leucovorin (10–25 mg once daily).
Initiate long-term suppressive therapy or chronic maintenance therapy (secondary prophylaxis) in all patients after completion of acute treatment of toxoplasmosis.
Consider discontinuing secondary prophylaxis in HIV-infected adults or adolescents who have successfully completed initial treatment for toxoplasmosis, are asymptomatic with respect to toxoplasmosis, and have CD4+ T-cell counts that have remained >200/mm3 for ≥6 months.
Reinitiate secondary prophylaxis if CD4+ T-cell count decreases to <200/mm3, regardless of plasma HIV viral load.
Perioperative Prophylaxis†
IV
900 mg given within 60 minutes prior to incision. Used with or without another anti-infective. (See Perioperative Prophylaxis under Uses.)
May give additional intraoperative doses every 6 hours during prolonged procedures; postoperative doses generally not recommended.
Prevention of Bacterial Endocarditis†
Patients Undergoing Certain Dental or Respiratory Tract Procedures†
Oral600 mg as a single dose given 30–60 minutes prior to the procedure.
IM or IV600 mg as a single dose given 30–60 minutes prior to the procedure.
Prevention of Perinatal Group B Streptococcal Disease†
Women at Risk Who Should Not Receive β-lactam Anti-infectives†
IV900 mg every 8 hours; initiate at time of labor or rupture of membranes and continue until delivery.
Special Populations
Hepatic Impairment
Dosage adjustments not usually necessary. Monitor hepatic function if used in those with severe hepatic disease.
Renal Impairment
Dosage adjustments not usually necessary.
Geriatric Patients
Dosage adjustments not usually necessary if used in geriatric patients with normal hepatic function and normal (age-adjusted) renal function.
Warnings
Contraindications
-
Hypersensitivity to clindamycin or lincomycin.
Warnings/Precautions
Warnings
Superinfection/Clostridium difficile-associated Diarrhea and Colitis (CDAD)
Possible emergence and overgrowth of nonsusceptible organisms, particularly yeasts. Institute appropriate therapy if superinfection occurs.
Treatment with anti-infectives alters normal colon flora and may permit overgrowth of Clostridium difficile. C. difficile infection (CDI) and C. difficile-associated diarrhea and colitis (CDAD; also known as antibiotic-associated diarrhea and colitis or pseudomembranous colitis) reported with nearly all anti-infectives, including clindamycin, and may range in severity from mild diarrhea to fatal colitis. C. difficile produces toxins A and B which contribute to development of CDAD; hypertoxin-producing strains of C. difficile are associated with increased morbidity and mortality since they may be refractory to anti-infectives and colectomy may be required.
Consider CDAD if diarrhea develops during or after therapy and manage accordingly. Obtain careful medical history since CDAD may occur as late as ≥2 months after anti-infective therapy discontinued.
If CDAD suspected or confirmed, discontinue anti-infectives not directed against C. difficile whenever possible. Initiate appropriate supportive therapy (e.g., fluid and electrolyte management, protein supplementation), anti-infective therapy directed against C. difficile (e.g., metronidazole, vancomycin), and surgical evaluation as clinically indicated.
Patients with Meningitis
Do not use for treatment of meningitis; clindamycin diffusion into CSF inadequate for treatment of CNS infections.
Sensitivity Reactions
Anaphylactic shock and anaphylactoid reactions with hypersensitivity reported.
Other severe hypersensitivity reactions, including severe skin reactions such as toxic epidermal necrolysis, drug reaction with eosinophilia and systemic symptoms (DRESS), and Stevens-Johnson syndrome, reported and have been fatal in some cases. Acute generalized exanthematous pustulosis and erythema multiforme also reported.
Generalized mild to moderate morbilliform-like (maculopapular) rash, vesiculobullous rash, urticaria, pruritus, angioedema, and rare instances of exfoliative dermatitis reported.
Some commercially available clindamycin capsules (e.g., Cleocin HCl 75- and 150-mg capsules) contain the dye tartrazine (FD&C yellow No. 5), which may cause allergic reactions including bronchial asthma in susceptible individuals. Although the incidence of tartrazine sensitivity is low, it frequently occurs in patients sensitive to aspirin.
Prior to initiation of clindamycin, make careful inquiry regarding prior hypersensitivity to drugs and other allergens. Use with caution in atopic individuals.
If anaphylactic or severe hypersensitivity reactions occur, permanently discontinue clindamycin and institute appropriate therapy as necessary.
General Precautions
Selection and Use of Anti-infectives
To reduce development of drug-resistant bacteria and maintain effectiveness of clindamycin and other antibacterials, use only for treatment or prevention of infections proven or strongly suspected to be caused by susceptible bacteria.
When selecting or modifying anti-infective therapy, use results of culture and in vitro susceptibility testing. In the absence of such data, consider local epidemiology and susceptibility patterns when selecting anti-infectives for empiric therapy.
Surgical procedures should be performed in conjunction with clindamycin therapy when indicated.
History of GI Disease
Use with caution in patients with a history of GI disease, particularly colitis. (See Superinfection/Clostridium difficile-associated Colitis under Cautions.)
Cardiovascular Effects
Rapid IV administration has caused cardiopulmonary arrest and hypotension.
Laboratory Monitoring
Monitor liver function, renal function, and CBCs periodically during prolonged therapy.
Specific Populations
Pregnancy
Reproduction studies in rats and mice have not revealed evidence of teratogenicity.
In clinical trials that included pregnant women, systemic clindamycin administered during second and third trimesters was not associated with increased frequency of congenital abnormalities. No adequate and well-controlled studies to date using clindamycin in pregnant women during first trimester of pregnancy.
Use during pregnancy only when clearly needed.
Clindamycin phosphate injection contains benzyl alcohol as a preservative; benzyl alcohol can cross the placenta. (See Pediatric Use under Cautions.)
Lactation
Distributed into milk; potentially can cause adverse effects on GI flora of breast-fed infants.
Manufacturer states clindamycin use in the mother is not a reason to discontinue breast-feeding; however, it may be preferable to use an alternate anti-infective.
If used in a breast-feeding mother, monitor infant for possible adverse effects on GI flora, including diarrhea and candidiasis (thrush, diaper rash) or, rarely, blood in the stool indicating possible antibiotic-associated colitis.
Consider benefits of breast-feeding and importance of clindamycin to the woman; also consider potential adverse effects on breast-fed child from the drug or from the underlying maternal condition.
Pediatric Use
Monitor organ system functions when used in pediatric patients (birth to 16 years of age).
Each mL of clindamycin phosphate injection contains 9.45 mg of benzyl alcohol. Large amounts of benzyl alcohol (i.e., 100–400 mg/kg daily) have been associated with toxicity (potentially fatal “gasping syndrome”) in neonates. Although amount of benzyl alcohol in recommended IM or IV clindamycin dosages are substantially lower than amounts reported in association with “gasping syndrome,” minimum amount of benzyl alcohol at which toxicity may occur unknown. Risk of benzyl alcohol toxicity depends on quantity administered and capacity of liver and kidneys to detoxify the chemical. Premature and low-birthweight infants may be more likely to develop toxicity.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether they respond differently than younger adults.
Clinical experience indicates that C. difficile-associated diarrhea and colitis seen in association with anti-infectives may occur more frequently and be more severe in geriatric patients (>60 years of age). Carefully monitor geriatric patients for development of diarrhea (e.g., changes in bowel frequency).
Hepatic Impairment
Moderate to severe liver disease may result in prolonged clindamycin half-life, but accumulation may not occur.
Periodically monitor liver enzymes in patients with severe hepatic impairment.
Common Adverse Effects
GI effects (nausea, vomiting, diarrhea, abdominal pain, tenesmus); rash; local reactions (pain, induration, sterile abscess with IM and thrombophlebitis, erythema, pain and swelling with IV).
How should I use Clindamycin (systemic) (monograph)
Administration
Administer orally, IM, or by intermittent or continuous IV infusion. Do not administer by rapid IV injection.
In the treatment of serious anaerobic infections, parenteral route usually used initially but may be switched to oral route when warranted by patient’s condition. In clinically appropriate circumstances, oral route may be used initially.
Clindamycin phosphate ADD-Vantage vials and commercially available premixed solutions of clindamycin phosphate in 5% dextrose should be used only for IV infusion.
For solution and drug compatibility information, see Compatibility under Stability.
Oral Administration
Clindamycin hydrochloride capsules and clindamycin palmitate hydrochloride oral solution can be administered without regard to food.
To avoid the possibility of esophageal irritation, administer clindamycin hydrochloride capsules with a full glass of water. Swallow capsules whole; do not use in pediatric patients unable to swallow capsules.
Reconstitution
Reconstitute clindamycin palmitate hydrochloride powder (granules) for oral solution by adding 75 mL of water to the 100-mL bottle. Add a large portion of the water initially and shake bottle vigorously; add remainder of the water and shake bottle until solution is uniform. The resulting oral solution contains 75 mg of clindamycin/5 mL.
IM Injection
For IM injection, administer clindamycin phosphate solution containing 150 mg of clindamycin per mL undiluted.
Single IM doses should not exceed 600 mg.
IV Infusion
Prior to IV infusion, clindamycin phosphate solutions (including solutions provided in ADD-Vantage vials) must be diluted with a compatible IV solution to a concentration ≤18 mg/mL.
Usually administered by intermittent IV infusion. Alternatively, may be given by continuous IV infusion in adults after first dose is given by rapid IV infusion. (See Table 1.)
Commercially available premixed solutions of clindamycin phosphate in 5% dextrose are administered only by IV infusion. Discard premixed solution if container seal is not intact or leaks are found or if the solution is not clear. Do not introduce additives into the container. Do not use flexible containers in series connections with other plastic containers; such use could result in air embolism from residual air being drawn from the primary container before administration of the fluid from the secondary container is complete.
Dilution
Clindamycin phosphate solution containing 150 mg of clindamycin per mL: Dilute appropriate dose in a compatible IV infusion solution and administer using the recommended rate of administration. (See Rate of Administration under Dosage and Administration.)
Clindamycin phosphate solution provided in ADD-Vantage vials: Dilute according to directions provided by the manufacturer. ADD-Vantage vials are for IV infusion only.
Clindamycin phosphate pharmacy bulk package: Dilute in a compatible IV infusion solution; not intended for direct IV infusion. Bulk package is intended for use only under a laminar flow hood. Entry into the vial should be made using a sterile transfer set or other sterile dispensing device, and the contents dispensed in aliquots using appropriate technique; multiple entries with a syringe and needle are not recommended because of the increased risk of microbial and particulate contamination. After entry into the bulk package vial, use entire contents promptly; discard any unused portion within 24 hours after initial entry.
Rate of Administration
Give intermittent IV infusions over a period of at least 10–60 minutes and at a rate ≤30 mg/minute. Give no more than 1.2 g by IV infusion in a single 1-hour period.
Dilute 300-mg doses in 50 mL of compatible diluent and infuse over 10 minutes; dilute 600-mg doses in 50 mL of diluent and infuse over 20 minutes; dilute 900-mg doses in 50–100 mL of diluent and infuse over 30 minutes; dilute 1.2-g doses in 100 mL of diluent and infuse over 40 minutes.
As an alternative to intermittent IV infusions in adults, the drug can be given by continuous IV infusion after an initial dose is given by IV infusion over 30 minutes. (See Table 1.)
|
Target Serum Clindamycin Concentrations |
Infusion Rate for Initial Dose |
Maintenance Infusion Rate |
|---|---|---|
|
>4 mcg/mL |
10 mg/minute for 30 minutes |
0.75 mg/minute |
|
>5 mcg/mL |
15 mg/minute for 30 minutes |
1 mg/minute |
|
>6 mcg/mL |
20 mg/minute for 30 minutes |
1.25 mg/minute |
Dosage
Available as clindamycin hydrochloride, clindamycin palmitate hydrochloride, and clindamycin phosphate; dosage expressed in terms of clindamycin.
Pediatric Patients
General Dosage in Neonates
Oral
Oral solution: Manufacturer recommends 8–12 mg/kg daily for serious infections, 13–16 mg/kg daily for severe infections, and 17–25 mg/kg daily for more severe infections. Give daily dosage in 3 or 4 equally divided doses. In children weighing ≤10 kg, manufacturer recommends a minimum dosage of 37.5 mg 3 times daily.
Neonates ≤7 days of age: AAP recommends 5 mg/kg every 12 hours in those weighing ≤2 kg or 5 mg/kg every 8 hours in those weighing >2 kg.
Neonates 8–28 days of age: AAP recommends 5 mg/kg every 8 hours in those weighing ≤2 kg or 5 mg/kg every 6 hours in those weighing >2 kg. In extremely low-birthweight neonates (<1 kg), consider 5 mg/kg every 12 hours until 2 weeks of age.
IV or IM
Neonates <1 month of age: Manufacturer recommends 15–20 mg/kg daily given in 3 or 4 equally divided doses. The lower dosage may be adequate for small, premature neonates.
Neonates ≤7 days of age: AAP recommends 5 mg/kg every 12 hours in those weighing ≤2 kg or 5 mg/kg every 8 hours in those weighing >2 kg.
Neonates 8–28 days of age: AAP recommends 5 mg/kg every 8 hours in those weighing ≤2 kg or 5 mg/kg every 6 hours in those weighing >2 kg. In extremely low-birthweight neonates (<1 kg), consider 5 mg/kg every 12 hours until 2 weeks of age.
General Dosage in Children 1 Month to 16 Years of Age
Oral
Capsules: Manufacturer recommends 8–16 mg/kg daily given in 3 or 4 equally divided doses for serious infections or 16–20 mg/kg daily given in 3 or 4 equally divided doses for more severe infections.
Oral solution: Manufacturer recommends 8–12 mg/kg daily for serious infections, 13–16 mg/kg daily for severe infections, or 17–25 mg/kg daily for more severe infections. Give daily dosage in 3 or 4 equally divided doses. In children weighing ≤10 kg, manufacturer recommends a minimum dosage of 37.5 mg 3 times daily.
AAP recommends 10–20 mg/kg daily given in 3 or 4 equally divided doses for mild to moderate infections or 30–40 mg/kg daily given in 3 or 4 equally divided doses for severe infections.
IV or IM
Manufacturer recommends 20–40 mg/kg daily given in 3 or 4 equally divided doses; use the higher dosage for more severe infections. Alternatively, manufacturer recommends 350 mg/m2 daily for serious infections or 450 mg/m2 daily for more severe infections.
AAP recommends 20–30 mg/kg daily given in 3 equally divided doses for mild to moderate infections or 40 mg/kg daily given in 3 or 4 equally divided doses for severe infections.
Acute Otitis Media† (AOM)
Oral
Children 6 months through 12 years of age: 30–40 mg/kg daily in 3 divided doses recommended by AAP. Use with or without a third generation cephalosporin. (See Acute Otitis Media under Uses.)
Pharyngitis and Tonsillitis†
Oral
AAP recommends 10 mg/kg 3 times daily (up to 900 mg daily) for 10 days.
IDSA recommends 7 mg/kg (up to 300 mg) 3 times daily for 10 days.
AHA recommends 20 mg/kg daily (up to 1.8 g daily) in 3 divided doses given for 10 days.
Respiratory Tract Infections
Oral
Children >3 months of age: IDSA recommends 30–40 mg/kg daily given in 3 or 4 divided doses.
IM or IV
Children >3 months of age: IDSA recommends 40 mg/kg daily given in divided doses every 6–8 hours.
Babesiosis†
Oral
IDSA recommends 7–10 mg/kg (up to 600 mg) every 6–8 hours for 7–10 days; used in conjunction with oral quinine sulfate (8 mg/kg [up to 650 mg] every 8 hours for 7–10 days). Others recommend 20–40 mg/kg (up to 600 mg) daily in 3 or 4 divided doses for 7–10 days; used in conjunction with oral quinine sulfate (24 mg/kg daily in 3 divided doses for 7–10 days).
IV
IDSA recommends 7–10 mg/kg (up to 600 mg) every 6–8 hours for 7–10 days; used in conjunction with oral quinine sulfate (8 mg/kg [up to 650 mg] every 8 hours for 7–10 days). Others recommend 20–40 mg/kg (up to 600 mg) daily in 3 or 4 divided doses for 7–10 days; used in conjunction with oral quinine sulfate (24 mg/kg daily in 3 divided doses for 7–10 days).
Malaria†
Treatment of Uncomplicated Chloroquine-resistant P. falciparum Malaria†
Oral20 mg/kg daily in 3 equally divided doses given for 7 days; used in conjunction with oral quinine sulfate (10 mg/kg 3 times daily given for 7 days if acquired in Southeast Asia or 3 days if acquired elsewhere).
Treatment of Severe P. falciparum Malaria†
Oral20 mg/kg daily in 3 equally divided doses given for 7 days; used in conjunction with IV quinidine gluconate (followed by oral quinine sulfate) given for a total duration of 3–7 days.
IV, then Oral10-mg/kg IV loading dose followed by 5 mg/kg IV every 8 hours; when oral therapy is tolerated, switch to oral clindamycin 20 mg/kg daily in 3 divided doses and continue for a total duration of 7 days.
Used in conjunction with IV quinidine gluconate (followed by oral quinine sulfate) given for a total duration of 3–7 days.
Pneumocystis jirovecii Pneumonia†
Treatment of Mild to Moderate Infections†
OralChildren: 10 mg/kg (up to 300–450 mg) every 6 hours given for 21 days; used in conjunction with oral primaquine (0.3 mg/kg once daily [up to 30 mg daily] for 21 days).
Adolescents: 450 mg every 6 hours or 600 mg every 8 hours given for 21 days; used in conjunction with oral primaquine (30 mg once daily for 21 days).
IVChildren: 10 mg/kg (up to 600 mg) every 6 hours given for 21 days; used in conjunction with oral primaquine (0.3 mg/kg once daily [up to 30 mg daily] for 21 days).
Adolescents: 600 mg every 6 hours or 900 mg every 8 hours given for 21 days; used in conjunction with oral primaquine (30 mg once daily for 21 days).
Toxoplasmosis†
Congenital Toxoplasmosis†
Oral or IV5–7.5 mg/kg (up to 600 mg) 4 times daily; used in conjunction with oral pyrimethamine (2 mg/kg once daily for 2 days followed by 1 mg/kg once daily) and oral or IM leucovorin (10 mg with each pyrimethamine dose).
Optimal duration not determined; some experts recommend continuing treatment for 12 months.
Treatment in Infants and Children†
Oral or IV5–7.5 mg/kg (up to 600 mg) 4 times daily; used in conjunction with oral pyrimethamine (2 mg/kg once daily for 2 days followed by 1 mg/kg once daily) and oral or IM leucovorin (10 mg with each pyrimethamine dose).
Continue acute treatment for ≥6 weeks; longer duration may be appropriate if disease is extensive or response incomplete at 6 weeks.
Treatment in Adolescents†
Oral or IV600 mg every 6 hours; used in conjunction with oral pyrimethamine (200-mg loading dose followed by 50 mg once daily in those <60 kg or 75 mg once daily in those ≥60 kg) and oral leucovorin (10–25 mg once daily; may be increased to 50 mg once or twice daily).
Continue acute treatment for ≥6 weeks; longer duration may be appropriate if disease is extensive or response incomplete at 6 weeks.
Prevention of Recurrence (Secondary Prophylaxis) in Infants and Children†
Oral7–10 mg/kg 3 times daily; used in conjunction with oral pyrimethamine (1 mg/kg or 15 mg/m2 [up to 25 mg] once daily) and oral leucovorin (5 mg once every 3 days).
Initiate long-term suppressive therapy or chronic maintenance therapy (secondary prophylaxis) in all patients after completion of acute treatment of toxoplasmosis.
Safety of discontinuing secondary toxoplasmosis prophylaxis in HIV-infected infants and children receiving potent antiretroviral therapy not extensively studied. Consider discontinuing secondary prophylaxis in HIV-infected children 1 to <6 years of age who have completed toxoplasmosis acute treatment, have received >6 months of stable antiretroviral therapy, are asymptomatic with respect to toxoplasmosis, and have CD4+ T-cell percentages that have remained >15% for >6 consecutive months. In HIV-infected children ≥6 years of age who have received >6 months of antiretroviral therapy, consider discontinuing secondary prophylaxis if CD4+ T-cell counts have remained >200/mm3 for >6 consecutive months. Reinitiate secondary prophylaxis if these parameters not met.
Prevention of Recurrence (Secondary Prophylaxis) in Adolescents†
OralDosage for secondary prophylaxis against toxoplasmosis in adolescents and criteria for initiation or discontinuance of such prophylaxis in this age group are the same as those recommended for adults. (See Adult Dosage under Dosage and Administration.)
Perioperative Prophylaxis†
IV
10 mg/kg given within 60 minutes prior to incision. Used with or without another anti-infective. (See Perioperative Prophylaxis under Uses.)
May give additional intraoperative doses every 6 hours during prolonged procedures; postoperative doses generally not recommended.
Prevention of Bacterial Endocarditis†
Patients Undergoing Certain Dental or Respiratory Tract Procedures†
Oral20 mg/kg as a single dose given 30–60 minutes prior to the procedure.
IM or IV20 mg/kg as a single dose given 30–60 minutes prior to the procedure.
Adults
General Adult Dosage
Serious Infections
Oral150–300 mg every 6 hours.
IV or IM600 mg to 1.2 g daily in 2–4 equally divided doses.
More Severe Infections
Oral300–450 mg every 6 hours.
IV or IM1.2–2.7 g daily in 2–4 equally divided doses.
For life-threatening infections, IV dosage may be increased up 4.8 g daily.
Gynecologic Infections
Pelvic Inflammatory Disease
IV, then OralInitially, 900 mg IV every 8 hours; used in conjunction with IV or IM gentamicin. After clinical improvement occurs, discontinue IV clindamycin and gentamicin and switch to oral clindamycin in a dosage of 450 mg 4 times daily to complete 14 days of therapy. Alternatively, oral doxycycline can be used to complete 14 days of therapy.
Pharyngitis and Tonsillitis†
Oral
IDSA recommends 7 mg/kg (up to 300 mg) 3 times daily for 10 days.
AHA recommends 20 mg/kg daily (up to 1.8 g daily) in 3 divided doses given for 10 days.
Respiratory Tract Infections
Oral
IDSA recommends 600 mg 3 times daily for 7–21 days.
IV
IDSA recommends 600 mg 3 times daily for 7–21 days.
Anthrax†
Treatment of Inhalational Anthrax†
IV900 mg every 8 hours.
Used in multiple-drug regimens that initially include IV ciprofloxacin or IV doxycycline and 1 or 2 other anti-infectives predicted to be effective.
Duration of treatment is 60 days if anthrax occurred as the result of exposure to anthrax spores in the context of biologic warfare or bioterrorism.
Babesiosis†
Oral
IDSA and others recommend 600 mg every 8 hours given for 7–10 days; used in conjunction with oral quinine sulfate (650 mg every 6 or 8 hours for 7–10 days).
IV
IDSA and others recommend 300–600 mg every 6 hours given for 7–10 days; used in conjunction with oral quinine sulfate (650 mg every 6 or 8 hours for 7–10 days).
Bacterial Vaginosis†
Treatment in Pregnant or Nonpregnant Women†
Oral300 mg twice daily given for 7 days.
Malaria†
Treatment of Uncomplicated Chloroquine-resistant P. falciparum Malaria†
Oral20 mg/kg daily in 3 equally divided doses given for 7 days; used in conjunction with oral quinine sulfate (650 mg 3 times daily given for 7 days if acquired in Southeast Asia or 3 days if acquired elsewhere).
Treatment of Severe P. falciparum Malaria†
Oral20 mg/kg daily in 3 equally divided doses given for 7 days; used in conjunction with IV quinidine gluconate (followed by oral quinine sulfate) given for a total duration of 3–7 days.
IV, then Oral10-mg/kg IV loading dose followed by 5 mg/kg IV every 8 hours; when oral therapy is tolerated, switch to oral clindamycin 20 mg/kg daily in 3 divided doses and continue for a total duration of 7 days.
Used in conjunction with IV quinidine gluconate (followed by oral quinine sulfate) given for a total duration of 3–7 days.
Pneumocystis jirovecii Pneumonia†
Treatment of Mild to Moderate Infections†
Oral450 mg every 6 hours or 600 mg every 8 hours given for 21 days; used in conjunction with oral primaquine (30 mg once daily for 21 days).
IV600 mg every 6 hours or 900 mg every 8 hours given for 21 days; used in conjunction with oral primaquine (30 mg once daily for 21 days).
Toxoplasmosis†
Treatment†
Oral or IV600 mg every 6 hours; used in conjunction with oral pyrimethamine (200-mg loading dose followed by 50 mg once daily in those <60 kg or 75 mg once daily in those ≥60 kg) and oral leucovorin (10–25 mg once daily; may be increased to 50 mg once or twice daily).
Continue acute treatment for ≥6 weeks; longer duration may be appropriate if disease is extensive or response incomplete at 6 weeks.
Prevention of Recurrence (Secondary Prophylaxis)†
Oral600 mg every 8 hours; used in conjunction with oral pyrimethamine (25–50 mg once daily) and oral leucovorin (10–25 mg once daily).
Initiate long-term suppressive therapy or chronic maintenance therapy (secondary prophylaxis) in all patients after completion of acute treatment of toxoplasmosis.
Consider discontinuing secondary prophylaxis in HIV-infected adults or adolescents who have successfully completed initial treatment for toxoplasmosis, are asymptomatic with respect to toxoplasmosis, and have CD4+ T-cell counts that have remained >200/mm3 for ≥6 months.
Reinitiate secondary prophylaxis if CD4+ T-cell count decreases to <200/mm3, regardless of plasma HIV viral load.
Perioperative Prophylaxis†
IV
900 mg given within 60 minutes prior to incision. Used with or without another anti-infective. (See Perioperative Prophylaxis under Uses.)
May give additional intraoperative doses every 6 hours during prolonged procedures; postoperative doses generally not recommended.
Prevention of Bacterial Endocarditis†
Patients Undergoing Certain Dental or Respiratory Tract Procedures†
Oral600 mg as a single dose given 30–60 minutes prior to the procedure.
IM or IV600 mg as a single dose given 30–60 minutes prior to the procedure.
Prevention of Perinatal Group B Streptococcal Disease†
Women at Risk Who Should Not Receive β-lactam Anti-infectives†
IV900 mg every 8 hours; initiate at time of labor or rupture of membranes and continue until delivery.
Special Populations
Hepatic Impairment
Dosage adjustments not usually necessary. Monitor hepatic function if used in those with severe hepatic disease.
Renal Impairment
Dosage adjustments not usually necessary.
Geriatric Patients
Dosage adjustments not usually necessary if used in geriatric patients with normal hepatic function and normal (age-adjusted) renal function.
What other drugs will affect Clindamycin (systemic) (monograph)?
Substrate of CYP isoenzyme 3A4 and, to a lesser extent, CYP3A5.
Moderate inhibitor of CYP3A4 in vitro; does not inhibit CYP1A2, 2C9, 2C19, 2E1, or 2D6.
Drugs Affecting Hepatic Microsomal Enzymes
CYP3A4 or 3A5 inhibitors: Possible increased plasma concentrations of clindamycin. Monitor for adverse effects if used with potent CYP3A4 inhibitor.
CYP3A4 or 3A5 inducers: Possible decreased plasma concentrations of clindamycin. Monitor for loss of clindamycin effectiveness if used with potent CYP3A4 inducer.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Neuromuscular blocking agents (tubocurarine, pancuronium) |
Potential for enhanced neuromuscular blocking action |
Use with caution in patients receiving neuromuscular blocking agents; closely monitor for prolonged neuromuscular blockade |
|
Rifampin |
Possible decreased clindamycin concentrations |
Monitor for clindamycin effectiveness |