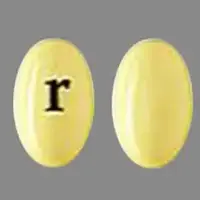
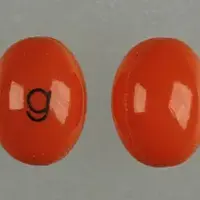
Generic name: hectorol
Availability: Prescription only
Pregnancy & Lactation: Risk data available
Brand names: Hectorol (oral/injection), Doxercalciferol (oral/injection)
What is Doxercalciferol (monograph)?
Introduction
A synthetic vitamin D analog.
Uses for Doxercalciferol
Hyperparathyroidism Secondary to Chronic Renal Disease
Treatment of secondary hyperparathyroidism in patients with chronic kidney disease (CKD) undergoing dialysis.
Oral doxercalciferol also used in the treatment of secondary hyperparathyroidism in patients with stage 3 or 4 CKD who do not yet require maintenance dialysis (predialysis patients).
Suppresses elevated serum or plasma parathyroid hormone (PTH) concentrations associated with secondary hyperparathyroidism in patients with CKD. Deficient production of biologically active vitamin D metabolites leads to secondary hyperparathyroidism, which contributes to the development of metabolic bone disease.
Doxercalciferol Dosage and Administration
Administration
Administration
Administer orally without regard to meals or by direct IV injection.
Dosage
Individualize doxercalciferol dosage based on serum or plasma intact PTH (iPTH) concentrations, with close monitoring of serum calcium and phosphorus concentrations.
In dialysis patients, measure serum iPTH, calcium, and phosphorus concentrations prior to initiation of the drug and weekly during first 12 weeks of therapy. Measure serum iPTH, calcium, phosphorus, and alkaline phosphatase concentrations periodically thereafter.
In predialysis patients, monitor serum calcium, serum phosphorus, and plasma iPTH concentrations at least every 2 weeks for 3 months after initiation of therapy or after subsequent dosage changes, then monthly for 3 months (once dosage is stabilized), and every 3 months thereafter.
Titrate dosage of doxercalciferol to reduce iPTH concentrations within a target range; specific target ranges recommended by manufacturer are based on the degree of renal impairment.
Manufacturer's recommendations based on National Kidney Foundation's 2003 KDOQI Clinical Practice Guidelines for Bone Metabolism and Disease in Chronic Kidney Disease.
|
CKD Stage |
GFR (mL/minute/1.73 m2) |
Target iPTH (pg/mL) |
|---|---|---|
|
3 |
30–59 |
35–70 |
|
4 |
15–29 |
70–110 |
|
5 |
<15 (or dialysis) |
150–300 |
Nephrology experts currently state that optimal iPTH concentration for predialysis patients with stage 3a (eGFR 45–59 mL/minute per 1.73 m2) to stage 5 CKD is unknown, but modest elevations may represent an appropriate adaptive response to declining renal function.
For patients with stage 5 CKD undergoing dialysis, some experts suggest maintaining iPTH concentrations within a range of approximately 2–9 times the assay's ULN (may correspond to range of approximately 130–600 pg/mL for commercial assays ). PTH assays exhibit substantial variability; previously recommended range of 150–300 pg/mL for patients with stage 5 CKD requiring dialysis was based on an assay that is no longer available. Avoid oversuppression of PTH, which may increase risk of adynamic bone disease.
Nephrology experts currently recommend using individual values for serum calcium and phosphorus (evaluated together) instead of the mathematical construct of calcium times phosphorus product to guide clinical practice.
Adults
Dialysis Patients
Hyperparathyroidism Secondary to Chronic Renal Disease
Oral|
Initial Dosing |
|
|---|---|
|
iPTH Concentrations |
Dosage |
|
>400 pg/mL |
10 mcg 3 times weekly at dialysis (approximately every other day) |
|
Dose Titration |
|
|
iPTH Concentrations |
Dosage |
|
>300 pg/mL |
Increase by 2.5 mcg at 8-week intervals as necessary; maximum recommended dosage is 20 mcg 3 times weekly (60 mcg weekly) |
|
150–300 pg/mL |
Maintain dosage |
|
<100 pg/mL |
Withhold for 1 week, reinitiate at a dose that is at least 2.5 mcg lower than the last dose |
If hypercalcemia, hyperphosphatemia, or a serum calcium (in mg/dL) times serum phosphorus (in mg/dL) product >55 mg2/dL2, decrease dosage or withhold therapy and/or adjust dosage of concomitant phosphate binders.
If serum calcium concentration >1 mg/dL above ULN, discontinue drug immediately, institute a low-calcium diet, withdraw calcium supplements, and measure serum calcium concentrations at least weekly; when normocalcemia ensues (generally in 2–7 days), reinstitute doxercalciferol at a reduced dose (at least 2.5 mcg lower than the prior dose).
IV|
Initial Dosing |
|
|---|---|
|
iPTH Concentrations |
Dosage |
|
> 400 pg/mL |
4 mcg 3 times weekly at end of dialysis (approximately every other day) |
|
Dose Titration |
|
|
iPTH Concentrations |
Dosage |
|
Decreased by <50% and exceeding 300 pg/mL |
Increase the dose given 3 times weekly by 1–2 mcg at 8-week intervals as necessary; IV dosages exceeding 18 mcg weekly have not been studied |
|
Decreased by >50% and exceeding 300 pg/mL |
Maintain dosage |
|
150–300 pg/mL |
Maintain dosage |
|
<100 pg/mL |
Withhold for 1 week, reinitiate at a dose at least 1 mcg lower than the last dose |
If hypercalcemia, hyperphosphatemia, or a serum calcium (in mg/dL) times serum phosphorus (in mg/dL) product >55 mg2/dL2, decrease dosage or withhold therapy and/or adjust dosage of concomitant phosphate binders.
If serum calcium concentration >1 mg/dL above ULN, discontinue drug immediately, institute a low-calcium diet, withdraw calcium supplements, and measure serum calcium concentrations at least weekly; when normocalcemia ensues (generally in 2–7 days), reinstitute doxercalciferol at a reduced dose (at least 1 mcg lower than the prior dose).
Predialysis Patients
Hyperparathyroidism Secondary to Chronic Renal Disease
Oral|
Initial Dosing |
|
|---|---|
|
iPTH Concentrations |
Dosage |
|
>70 pg/mL (Stage 3) and >110 pg/mL (Stage 4) |
1 mcg once daily |
|
Dose Titration |
|
|
iPTH Concentrations |
Dosage |
|
> 70 pg/mL (Stage 3) and >110 pg/mL (Stage 4) |
Increase by 0.5 mcg at 2-week intervals as necessary; maximum recommended dosage is 3.5 mcg once daily |
|
35–70 pg/mL (Stage 3) and 70–110 pg/mL (Stage 4) |
Maintain dosage |
|
<35 pg/mL (Stage 3) and <70 pg/mL (Stage 4) |
Withhold for 1 week, reinitiate at a dose that is at least 0.5 mcg lower than the last dose |
If hypercalcemia, hyperphosphatemia, or a serum calcium (in mg/dL) times phosphorus (in mg/dL) product >55 mg2/dL2, decrease dosage or withhold therapy and/or adjust dosage of concomitant phosphate binders.
If serum calcium concentration >10.7 mg/dL, discontinue drug immediately, institute a low-calcium diet, withdraw calcium supplements, and measure serum calcium concentrations at least weekly; when normocalcemia ensues (generally in 2–7 days), reinstitute doxercalciferol at a reduced dose (at least 0.5 mcg lower than the prior dose).
Prescribing Limits
Adults
Oral
Maximum: 20 mcg 3 times weekly (60 mcg weekly).
IV
Dosages >18 mcg weekly have not been studied.
Related/similar drugs
cinacalcet, Sensipar, paricalcitol, Zemplar, HectorolWarnings
Contraindications
Tendency toward hypercalcemia.
Evidence of vitamin D toxicity.
Doxercalciferol injection: Known hypersensitivity to doxercalciferol or any ingredient in the formulation. (See Hypersensitivity Reactions under Cautions.)
Warnings/Precautions
Sensitivity Reactions
Hypersensitivity Reactions
Serious, sometimes fatal, hypersensitivity reactions reported in hemodialysis patients receiving doxercalciferol injection. Reactions have included anaphylaxis with angioedema (involving the face, lips, tongue, and airways), hypotension, unresponsiveness, chest discomfort, shortness of breath, and cardiopulmonary arrest.
Monitor patients for hypersensitivity reactions upon initiation of IV doxercalciferol treatment. If hypersensitivity reactions occur, discontinue the drug and provide clinically appropriate treatment.
Hypercalcemia
Risk of vitamin D analog toxicity; may require emergency measures.
Acute hypercalcemia may increase risk of cardiac arrhythmias, seizures, and also synergistic inotropic and toxic effects in presence of cardiac glycosides.
Chronic hypercalcemia increases risk of soft-tissue calcification, including vascular calcification.
If hypercalcemia develops following initiation of doxercalciferol therapy, decrease dosage of doxercalciferol and/or calcium-containing phosphate binders.
Use radiographic evaluation of suspected areas for early detection of calcification.
Do not use vitamin D and its analogs during doxercalciferol therapy; possible additive effects.
Hyperphosphatemia
May occur with vitamin D analog toxicity.
In patients with CKD, use calcium-containing or other non-aluminum-containing phosphate binders and a low-phosphate diet to control serum phosphate concentrations.
If hyperphosphatemia develops following initiation of doxercalciferol therapy, decrease dosage of doxercalciferol and/or increase dosage of phosphate binder.
Hypermagnesemia
Do not use magnesium-containing antacids concomitantly with doxercalciferol.
Vitamin D Deficiency
Do not use doxercalciferol for treatment of nutritional vitamin D deficiency.
Evaluate patients for vitamin D deficiency prior to initiation of doxercalciferol therapy; if indicated, vitamin D deficiency should be treated prior to initiating doxercalciferol.
Metabolic Effects
Possible risk of hypercalcemia, hyperphosphatemia, hypercalciuria, and excessive suppression of iPTH concentrations; monitor and adjust dosages routinely to minimize risk of such effects.
Most patients require doxercalciferol dosage titration as well as adjustment of concomitant therapy (e.g., dietary phosphate binders) to optimize iPTH suppression while maintaining serum calcium and phosphorus within prescribed ranges. (See Dosage under Dosage and Administration.)
Specific Populations
Pregnancy
Category B.
Lactation
Not known if doxercalciferol is distributed into milk; discontinue nursing or drug because of potential risk (e.g., hypercalcemia) in nursing infants.
Pediatric Use
Safety and efficacy not established in pediatric patients.
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults.
Hepatic Impairment
Use with caution since doxercalciferol may not be metabolized appropriately. Monitor serum iPTH, calcium, and phosphorus concentrations more frequently.
Common Adverse Effects
In dialysis patients: Edema, headache, malaise, nausea/vomiting, dizziness, dyspnea, pruritus, bradycardia.
In predialysis patients with stage 3 or 4 CKD: Infection, chest pain, constipation, dyspepsia, anemia, dehydration, depression, hypertonia, insomnia, paresthesia, increased cough, dyspnea, rhinitis.
Excessive vitamin D intake (early manifestations): Weakness, headache, somnolence, nausea, vomiting, dry mouth, constipation, bone pain, metallic taste, anorexia.
Excessive vitamin D intake (late manifestations): Polyuria, polydipsia anorexia, weight loss, nocturia, calcific conjunctivitis, pancreatitis, photophobia, rhinorrhea, pruritus, hyperthermia, decreased libido, increased BUN, albuminuria, hypercholesterolemia, increased serum AST and ALT concentrations, ectopic calcification, hypertension, cardiac arrhythmias, sensory disturbances, dehydration, apathy, growth arrest, urinary tract infections.
How should I use Doxercalciferol (monograph)
Administration
Administration
Administer orally without regard to meals or by direct IV injection.
Dosage
Individualize doxercalciferol dosage based on serum or plasma intact PTH (iPTH) concentrations, with close monitoring of serum calcium and phosphorus concentrations.
In dialysis patients, measure serum iPTH, calcium, and phosphorus concentrations prior to initiation of the drug and weekly during first 12 weeks of therapy. Measure serum iPTH, calcium, phosphorus, and alkaline phosphatase concentrations periodically thereafter.
In predialysis patients, monitor serum calcium, serum phosphorus, and plasma iPTH concentrations at least every 2 weeks for 3 months after initiation of therapy or after subsequent dosage changes, then monthly for 3 months (once dosage is stabilized), and every 3 months thereafter.
Titrate dosage of doxercalciferol to reduce iPTH concentrations within a target range; specific target ranges recommended by manufacturer are based on the degree of renal impairment.
Manufacturer's recommendations based on National Kidney Foundation's 2003 KDOQI Clinical Practice Guidelines for Bone Metabolism and Disease in Chronic Kidney Disease.
|
CKD Stage |
GFR (mL/minute/1.73 m2) |
Target iPTH (pg/mL) |
|---|---|---|
|
3 |
30–59 |
35–70 |
|
4 |
15–29 |
70–110 |
|
5 |
<15 (or dialysis) |
150–300 |
Nephrology experts currently state that optimal iPTH concentration for predialysis patients with stage 3a (eGFR 45–59 mL/minute per 1.73 m2) to stage 5 CKD is unknown, but modest elevations may represent an appropriate adaptive response to declining renal function.
For patients with stage 5 CKD undergoing dialysis, some experts suggest maintaining iPTH concentrations within a range of approximately 2–9 times the assay's ULN (may correspond to range of approximately 130–600 pg/mL for commercial assays ). PTH assays exhibit substantial variability; previously recommended range of 150–300 pg/mL for patients with stage 5 CKD requiring dialysis was based on an assay that is no longer available. Avoid oversuppression of PTH, which may increase risk of adynamic bone disease.
Nephrology experts currently recommend using individual values for serum calcium and phosphorus (evaluated together) instead of the mathematical construct of calcium times phosphorus product to guide clinical practice.
Adults
Dialysis Patients
Hyperparathyroidism Secondary to Chronic Renal Disease
Oral|
Initial Dosing |
|
|---|---|
|
iPTH Concentrations |
Dosage |
|
>400 pg/mL |
10 mcg 3 times weekly at dialysis (approximately every other day) |
|
Dose Titration |
|
|
iPTH Concentrations |
Dosage |
|
>300 pg/mL |
Increase by 2.5 mcg at 8-week intervals as necessary; maximum recommended dosage is 20 mcg 3 times weekly (60 mcg weekly) |
|
150–300 pg/mL |
Maintain dosage |
|
<100 pg/mL |
Withhold for 1 week, reinitiate at a dose that is at least 2.5 mcg lower than the last dose |
If hypercalcemia, hyperphosphatemia, or a serum calcium (in mg/dL) times serum phosphorus (in mg/dL) product >55 mg2/dL2, decrease dosage or withhold therapy and/or adjust dosage of concomitant phosphate binders.
If serum calcium concentration >1 mg/dL above ULN, discontinue drug immediately, institute a low-calcium diet, withdraw calcium supplements, and measure serum calcium concentrations at least weekly; when normocalcemia ensues (generally in 2–7 days), reinstitute doxercalciferol at a reduced dose (at least 2.5 mcg lower than the prior dose).
IV|
Initial Dosing |
|
|---|---|
|
iPTH Concentrations |
Dosage |
|
> 400 pg/mL |
4 mcg 3 times weekly at end of dialysis (approximately every other day) |
|
Dose Titration |
|
|
iPTH Concentrations |
Dosage |
|
Decreased by <50% and exceeding 300 pg/mL |
Increase the dose given 3 times weekly by 1–2 mcg at 8-week intervals as necessary; IV dosages exceeding 18 mcg weekly have not been studied |
|
Decreased by >50% and exceeding 300 pg/mL |
Maintain dosage |
|
150–300 pg/mL |
Maintain dosage |
|
<100 pg/mL |
Withhold for 1 week, reinitiate at a dose at least 1 mcg lower than the last dose |
If hypercalcemia, hyperphosphatemia, or a serum calcium (in mg/dL) times serum phosphorus (in mg/dL) product >55 mg2/dL2, decrease dosage or withhold therapy and/or adjust dosage of concomitant phosphate binders.
If serum calcium concentration >1 mg/dL above ULN, discontinue drug immediately, institute a low-calcium diet, withdraw calcium supplements, and measure serum calcium concentrations at least weekly; when normocalcemia ensues (generally in 2–7 days), reinstitute doxercalciferol at a reduced dose (at least 1 mcg lower than the prior dose).
Predialysis Patients
Hyperparathyroidism Secondary to Chronic Renal Disease
Oral|
Initial Dosing |
|
|---|---|
|
iPTH Concentrations |
Dosage |
|
>70 pg/mL (Stage 3) and >110 pg/mL (Stage 4) |
1 mcg once daily |
|
Dose Titration |
|
|
iPTH Concentrations |
Dosage |
|
> 70 pg/mL (Stage 3) and >110 pg/mL (Stage 4) |
Increase by 0.5 mcg at 2-week intervals as necessary; maximum recommended dosage is 3.5 mcg once daily |
|
35–70 pg/mL (Stage 3) and 70–110 pg/mL (Stage 4) |
Maintain dosage |
|
<35 pg/mL (Stage 3) and <70 pg/mL (Stage 4) |
Withhold for 1 week, reinitiate at a dose that is at least 0.5 mcg lower than the last dose |
If hypercalcemia, hyperphosphatemia, or a serum calcium (in mg/dL) times phosphorus (in mg/dL) product >55 mg2/dL2, decrease dosage or withhold therapy and/or adjust dosage of concomitant phosphate binders.
If serum calcium concentration >10.7 mg/dL, discontinue drug immediately, institute a low-calcium diet, withdraw calcium supplements, and measure serum calcium concentrations at least weekly; when normocalcemia ensues (generally in 2–7 days), reinstitute doxercalciferol at a reduced dose (at least 0.5 mcg lower than the prior dose).
Prescribing Limits
Adults
Oral
Maximum: 20 mcg 3 times weekly (60 mcg weekly).
IV
Dosages >18 mcg weekly have not been studied.
Related/similar drugs
cinacalcet, Sensipar, paricalcitol, Zemplar, HectorolWhat other drugs will affect Doxercalciferol (monograph)?
Drugs Affecting Hepatic Microsomal Enzymes
Possible pharmacokinetic interaction with hepatic enzyme inducers (e.g., glutethimide, phenobarbital) or inhibitors (e.g., erythromycin, ketoconazole) affecting hepatic hydroxylation (activation) of doxercalciferol.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Cardiac glycosides |
Possible cardiac arrhythmias |
|
|
Cholestyramine |
Intestinal absorption of oral doxercalciferol may be decreased |
|
|
Erythromycin |
Serum concentrations of active moiety of doxercalciferol may be reduced |
|
|
Glutethimide |
Metabolism of doxercalciferol may be altered |
Dosage adjustment of doxercalciferol may be needed |
|
Ketoconazole |
Serum concentrations of active moiety of doxercalciferol may be reduced |
|
|
Magnesium-containing antacids |
Possible hypermagnesemia |
|
|
Mineral oil |
Possible decreased absorption of oral doxercalciferol |
|
|
Orlistat |
Possible decreased absorption of oral doxercalciferol |
|
|
Vitamin D and its analogs |
Potential additive pharmacologic effect resulting in increased adverse effects, including hypercalcemia |
|
|
Phenobarbital |
Metabolism of doxercalciferol may be altered |
Dosage adjustment of doxercalciferol may be needed |