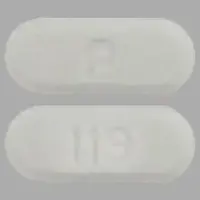
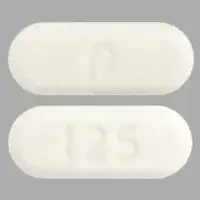
Generic name: everolimus
Drug class: MTOR inhibitors, Selective immunosuppressants
Dosage form: oral tablet, tablet for oral suspension
Availability: Prescription only
Pregnancy & Lactation: Risk data available
Brand names: Afinitor, Zortress, Afinitor disperz
What is Everolimus?
Everolimus (Afinitor, Afinitor Disperz, Zortress) belongs to a class of drugs called kinase inhibitors. It is used to prevent organ transplant rejection and treat certain benign (noncancerous) and cancerous tumors.
Different brandnames and tablet strengths of everolimus are used for different conditions:
- Afinitor (2.5 mg, 5 mg, 7.5 mg and 10 mg tablets), Afinitor Disperz (2 mg, 3 mg and 5 mg tablets for oral suspension) and generic versions of these are used to treat certain benign (noncancerous) and cancerous tumors.
- Zortress (0.25 mg, 0.5 mg, 0.75 mg and 1 mg tablets) and generic versions of it are used to prevent organ transplant rejection.
Everolimus is an inhibitor of a kinase called mammalian target of rapamycin (mTOR), which plays an important role in a pathway that regulates things such as how cells in your body multiply, form new blood vessels and use nutrients.
In people with tumors, everolimus works by reducing the blood flow to the tumor, which slows down the growth of tumors. Everolimus does this my binding to a protein called FKBP-12 and forming a complex, which blocks the activity of mTOR.
In people with a transplanted liver or kidney, everolimus acts as an immunosuppressant to prevent your body from attacking or rejecting the transplanted organ. Everolimus works by stopping a type of white blood cell called lymphocytes from activating and multiplying. These cells usually help our bodies fight off invading organisms, but after an organ transplant you don't want your immune system cells attacking or rejecting the new organ. Everolimus inhibits both antigenic and interleukin (IL-2 and IL-15) stimulation of lymphocytes.
Everolimus was approved by the US Food and Drug Administration (FDA) in 2009.
What is everolimus used for?
The Afinitor brand of everolimus is a prescription medicine used to treat:
- advanced hormone receptor-positive, HER2-negative breast cancer, along with the medicine exemestane, in postmenopausal women who have already received certain other medicines for their cancer.
- adults with a type of pancreatic cancer known as pancreatic neuroendocrine tumor (PNET), that has progressed and cannot be treated with surgery.
- adults with a type of cancer known as neuroendocrine tumor (NET) of the stomach and intestine (gastrointestinal), or lung that has progressed and cannot be treated with surgery.
It is not for use in people with carcinoid tumors that actively produce hormones. - adults with advanced kidney cancer (renal cell carcinoma or RCC) when certain other medicines have not worked.
- people with the following types of tumors that are seen with a genetic condition called tuberous sclerosis complex (TSC):
- adults with a kidney tumor called angiomyolipoma, when their kidney tumor does not require surgery right away.
- adults and children 1 year of age and older with a brain tumor called subependymal giant cell astrocytoma (SEGA) when the tumor cannot be removed completely by surgery.
The Afinitor Disperz brand of everolimus is a prescription medicine used to treat:
- adults and children 1 year of age and older with a genetic condition called tuberous sclerosis complex (TSC) who have a brain tumor called subependymal giant cell astrocytoma (SEGA) when the tumor cannot be removed completely by surgery.
- adults and children 2 years of age and older with a genetic condition called tuberous sclerosis complex (TSC) who have certain types of seizures (epilepsy), as an added treatment to other antiepileptic medicines.
The Zortress brand of everolimus is a prescription medicine used to:
- prevent transplant rejection (antirejection medicine) in people who have received a kidney transplant or liver transplant.
- it is used with other medicines called cyclosporine, corticosteroids and certain other transplant medicines to prevent rejection of your transplanted kidney. It is used with other medicines called tacrolimus and corticosteroids to prevent rejection of your transplanted liver.
It is not known if everolimus:
- is safe and effective in children to treat:
- hormone receptor-positive, HER-2 negative breast cancer
- a type of cancer called neuroendocrine tumors (NET)
- kidney cancer (renal cell carcinoma)
- a kidney tumor called angiomyolipoma, that can happen in children with a genetic condition called tuberous sclerosis complex (TSC)
- is safe and effective in transplanted organs other than the kidney and liver.
- sold under the Zortress brand is safe and effective in children under 18 years of age
Warnings
Important information you should know if you are taking everolimus to treat a tumor
This medication can cause serious side effects, including:
1. You may develop lung or breathing problems. In some people lung or breathing problems may be severe and can lead to death. Tell your healthcare provider right away if you have any of these symptoms:
- New or worsening cough
- Shortness of breath
- Chest pain
- Difficulty breathing or wheezing
2. You may be more likely to develop an infection, such as pneumonia, or a bacterial, fungal or viral infection. Viral infections may include active hepatitis B in people who have had hepatitis B in the past (reactivation). In some people (including adults and children) these infections may be severe and can lead to death. You may need to be treated as soon as possible.
Tell your healthcare provider right away if you have a temperature of 100.5˚F or above, chills, or do not feel well.
Symptoms of hepatitis B or infection may include the following:
- Fever
- Chills
- Skin rash
- Joint pain and swelling
- Tiredness
- Loss of appetite
- Nausea
- Pale stools or dark urine
- Yellowing of the skin
- Pain in the upper right side of the stomach
3. Severe allergic reactions. Call your healthcare provider or get medical help right away if you get signs and symptoms of a severe allergic reaction, including: rash, itching, hives, flushing, trouble breathing or swallowing, chest pain or dizziness.
4. Possible increased risk for a type of allergic reaction called angioedema, in people who take an Angiotensin-Converting Enzyme (ACE) inhibitor medicine during treatment with everolimus. Talk with your healthcare provider before taking this medication if you are not sure if you take an ACE inhibitor medicine. Get medical help right away if you have trouble breathing or develop swelling of your tongue, mouth, or throat during treatment with this medications.
5. Mouth ulcers and sores. Mouth ulcers and sores are common during treatment with everolimus but can also be severe. When you start treatment with one of this medication, your healthcare provider may tell you to also start a prescription mouthwash to reduce the likelihood of getting mouth ulcers or sores and to reduce their severity. Follow your healthcare provider’s instructions on how to use this prescription mouthwash. If you develop pain, discomfort, or open sores in your mouth, tell your healthcare provider. Your healthcare provider may tell you to restart this mouthwash or to use a special mouthwash or mouth gel that does not contain alcohol, peroxide, iodine, or thyme.
6. You may develop kidney failure. In some people this may be severe and can lead to death. Your healthcare provider should do tests to check your kidney function before and during your treatment.
If you have any of the serious side effects listed above, you may need to stop taking everolimus for a while or use a lower dose. Follow your healthcare provider’s instructions.
Important information you should know if you are taking everolimus to prevent transplant rejection
This medication can cause serious side effects, including:
- Increased risk of getting certain cancers. People who take this medication have a higher chance of getting lymphoma and other cancers, especially skin cancer. Talk to your doctor about your risk for cancer.
- Increased risk of serious infections. This medication weakens the body’s immune system and affects your ability to fight infections. Serious infections can happen with this medication that may lead to death. People taking this medication have a higher chance of getting infections caused by viruses, bacteria, and fungi (yeast).
- Call your doctor if you have symptoms of infection, including fever or chills.
- Blood clot in the blood vessels of your transplanted kidney. If this happens, it usually occurs within the first 30 days after your kidney transplant. Tell your doctor right away if you:
- have pain in your groin, lower back, side or stomach (abdomen)
- make less urine or you do not pass any urine
- have blood in your urine or dark colored urine (tea-colored)
- have fever, nausea, or vomiting
- Serious problems with your transplanted kidney (nephrotoxicity). You will need to start with a lower dose of cyclosporine when you take it with everolimus. Your doctor should do regular blood tests to check your levels of both everolimus and cyclosporine.
- Increased risk of death that can be related to infection, in people who have had a heart transplant. You should not take everolimus without talking to your doctor if you have had a heart transplant.
See the section below “What are the side effects of everolimus?” for information about other serious side effects.
How should I take Everolimus
Everolimus comes as a tablet to take by mouth and as a tablet to suspend in water and take by mouth. When everolimus is taken to treat kidney tumors, SEGA, or seizures in people who have TSC; RCC; or breast, pancreatic, stomach, intestine, or lung cancer, it is usually taken once a day. When everolimus is taken to prevent transplant rejection, it is usually taken twice a day (every 12 hours) at the same time as cyclosporine. Everolimus should either always be taken with food or always without food. Take everolimus at around the same time(s) every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take everolimus exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Everolimus tablets come in individual blister packs that can be opened with scissors. Do not open a blister pack until you are ready to swallow the tablet it contains.
You should take either everolimus tablets or everolimus tablets for oral suspension. Do not take a combination of both of these products.
Swallow the tablets whole with a full glass of water; do not split, chew, or crush them. Do not take tablets that have been crushed or broken. Tell your doctor or pharmacist if you are not able to swallow the tablets whole.
If you are taking the tablets for oral suspension (Afinitor Disperz), you must mix them with water before use. Do not swallow these tablets whole, and do not mix them with juice or any liquid other than water. Do not prepare the mixture more than 60 minutes before you plan to use it, and dispose of the mixture if it is not used after 60 minutes. Do not prepare the medication on a surface that you use to prepare or eat food. If you will be preparing the medication for someone else, you should wear gloves to prevent contact with the medication. If you are pregnant or plan to become pregnant, you should avoid preparing the medication for someone else, because contact with everolimus may harm your unborn baby.
You can mix the tablets for oral suspension in an oral syringe or in a small glass. To prepare the mixture in an oral syringe, remove the plunger from a 10-mL oral syringe and place the prescribed number of tablets in the barrel of the syringe without breaking or crushing the tablets. You can prepare up to 10 mg of everolimus in a syringe at one time, so if your dose is greater than 10 mg, you will need to prepare it in a second syringe. Replace the plunger in the syringe and draw about 5 mL of water and 4 mL of air into the syringe and place the syringe into a container with the tip pointing up. Wait 3 minutes to allow the tablets to go into suspension. then pick up the syringe and gently turn it up and down it five times. Place the syringe into the patient's mouth and push the plunger to administer the medication. After the patient has swallowed the medication, refill the same syringe with 5 mL of water and 4 mL of air and swirl the syringe to rinse out any particles that are still in the syringe. Give this mixture to the patient to be sure that he or she receives all of the medication.
To prepare the mixture in a glass, place the prescribed number of tablets into a small drinking glass that holds no more than 100 mL (about 3 ounces) without crushing or breaking the tablets. You can prepare up to 10 mg of everolimus in a glass at one time, so if your dose is greater than 10 mg, you will need to prepare it in a second glass. Add 25 mL (about 1 ounce) of water to the glass. Wait 3 minutes and then gently stir the mixture with a spoon. Have the patient drink the entire mixture immediately. Add another 25 mL of water to the glass and stir with the same spoon to rinse out any particles that are still in the glass. Have the patient drink this mixture to be sure that he or she receives all of the medication.
Your doctor may adjust your dose of everolimus during your treatment depending on the results of your blood tests, your response to the medication, side effects you experience, and changes in other medications that you take with everolimus. If you are taking everolimus to treat SEGA or seizures, your doctor will adjust your dose not more often than once every 1 to 2 weeks, and if you are taking everolimus to prevent transplant rejection, your doctor will adjust your dose not more often than once every 4 to 5 days. Your doctor may stop your treatment for a time if you experience severe side effects. Talk to your doctor about how you are feeling during your treatment with everolimus.
Dosing information
- Your healthcare provider will prescribe the dose of everolimus that is right for you.
- Take everolimus exactly as your healthcare provider tells you to.
- Do not stop taking everolimus or change your dose unless your doctor tells you to.
-
If you are taking everolimus to treat a tumor:
- Your healthcare provider may change your dose of everolimus or tell you to temporarily interrupt dosing, if needed.
- Take only the tablets or the tablets for oral suspension. Do not mix the two together.
- Use scissors to open the blister pack.
- Take everolimus 1 time each day at about the same time.
- Take everolimus the same way each time, either with food or without food.
- You should have blood tests before you start everolimus and as needed during your treatment. These will include tests to check your blood cell count, kidney and liver function, cholesterol, and blood sugar levels.
- If you take everolimus to treat SEGA or to treat certain types of seizures with TSC, you will also need to have blood tests regularly to measure how much medicine is in your blood. This will help your healthcare provider decide how much everolimus you need to take.
- Swallow everolimus tablets whole with a glass of water. Do not take any tablet that is broken or crushed.
- If your healthcare provider prescribes everolimus tablets for oral suspension, see the “Instructions for Use” that comes with your medicine for instructions on how to prepare and take your dose.
- Each dose of everolimus tablets for oral suspension must be prepared as a suspension before it is given.
- Everolimus tablets for oral suspension can cause harm to an unborn baby. When possible, the suspension should be prepared by an adult who is not pregnant or planning to become pregnant.
- Wear gloves to avoid possible contact with everolimus when preparing the suspensions of everolimus tablets for oral suspension for another person.
-
If you are taking everolimus to prevent transplant rejection:
- Take everolimus at the same time as your dose of cyclosporine medicine.
- Do not stop taking or change your dose of cyclosporine or tacrolimus medicine unless your doctor tells you to.
- If your doctor changes your dose of cyclosporine, your dose of everolimus may change.
- Take everolimus 2 times a day about 12 hours apart.
- Swallow everolimus tablets whole with a glass of water. Do not crush or chew everolimus tablets.
- Take everolimus tablets with or without food. If you take everolimus tablets with food, always take everolimus tablets with food. If you take everolimus tablets without food, always take everolimus tablets without food.
- Your doctor will do regular blood tests to check your kidney function while you take everolimus. It is important that you get these tests done when your doctor tells you to. Blood tests will monitor how your kidneys are working and make sure you are getting the right dose of everolimus and other transplant medications they may be on (cyclosporine and tacrolimus).
Before Taking
Do not take everolimus if you have had a severe allergic reaction to everolimus.
Do not take everolimus if you are allergic to any of the ingredients in it. See below for a complete list of ingredients.
Talk to your healthcare provider before taking this medicine if you are allergic to:
- a medicine that contains sirolimus
- a medicine that contains temsirolimus
Ask your healthcare provider if you do not know.
What should I tell my doctor before taking everolimus?
Before taking everolimus, tell your healthcare provider about all of your medical conditions, including if you:
- Have or have had kidney problems
- Have or have had liver problems
- Have diabetes or high blood sugar
- Have high blood cholesterol or triglyceride levels (fat in your blood)
- Have any infections
- Previously had hepatitis B
- Have skin cancer or it runs in your family
- have Lapp lactase deficiency or glucose-galactose malabsorption. You should not take everolimus to prevent transplant organ rejection if you have this disorder.
- Are scheduled to receive any vaccinations. You should not receive a “live vaccine” or be around people who have recently received a “live vaccine” during your treatment with everolimus. If you are not sure about the type of immunization or vaccine, ask your healthcare provider. For children with TSC and SEGA or certain types of seizures, work with your healthcare provider to complete the recommended childhood series of vaccines before your child starts treatment with everolimus.
- Are planning to have surgery or if you have had a recent surgery. You should stop taking everolimus if you are being treated for a tumor at least 1 week before planned surgery. See “What are the side effects of everolimus?” below.
- Have received radiation therapy or are planning to receive radiation therapy in the future. See “What are the side effects of everolimus?” below.
What happens if I miss a dose?
If you are taking everolimus to treat a tumor and you miss a dose, you may take it if it is less than 6 hours after the time you normally take it. If it is more than 6 hours after you normally take your everolimus, skip the dose for that day. The next day, take everolimus at your usual time. Do not take 2 doses to make up for a missed dose. If you are not sure about what to do, call your healthcare provider.
What happens if I overdose?
If you are taking everolimus to treat a tumor and you take too much, contact your healthcare provider or go to the nearest hospital emergency room right away. Take the pack of everolimus with you.
If you are taking everolimus to prevent transplant rejection, call your doctor or go to the nearest hospital emergency room right away.
What should I know about storage and disposal of this medication?
Keep this medication in the blister pack it came in, tightly closed, and out of reach of children. Store it at room temperature and away from light and excess heat and moisture (not in the bathroom). Keep the blister packs and tablets dry.
Unneeded medications should be disposed of in special ways to ensure that pets, children, and other people cannot consume them. However, you should not flush this medication down the toilet. Instead, the best way to dispose of your medication is through a medicine take-back program. Talk to your pharmacist or contact your local garbage/recycling department to learn about take-back programs in your community. See the FDA's Safe Disposal of Medicines website (http://goo.gl/c4Rm4p) for more information if you do not have access to a take-back program.
What special dietary instructions should I follow?
Do not eat grapefruit or drink grapefruit juice while taking this medication.
What should I avoid while using Everolimus?
- You should not drink grapefruit juice or eat grapefruit during your treatment with everolimus. It may make the amount of everolimus in your blood increase to a harmful level.
- Avoid receiving any live vaccines while taking everolimus. Some vaccines may not work as well while you are taking this medication.
- Avoid becoming pregnant. See the section Pregnancy and breastfeeding below.
- If you are taking everolimus to prevent transplant rejection, limit the amount of time you spend in the sunlight. Avoid using tanning beds or sunlamps. People who take everolimus have a higher risk of getting skin cancer. See the section “Important information” Wear protective clothing when you are in the sun and use a sunscreen with a high protection factor (SPF 30 and above). This is especially important if you have fair skin or if you have a family history of skin cancer.
Everolimus side effects
If you are taking everolimus to treat a tumour:
Everolimus can cause serious side effects, including:
- See “Important informtion” above for more information.
- Risk of wound healing problems. Wounds may not heal properly during everolimus treatment. Tell your healthcare provider if you plan to have any surgery before starting or during treatment with everolimus.
- You should stop taking everolimus at least 1 week before planned surgery.
- Your healthcare provider should tell you when you may start taking everolimus again after surgery.
- Increased blood sugar and fat (cholesterol and triglyceride) levels in the blood. Your healthcare provider should do blood tests to check your fasting blood sugar, cholesterol, and triglyceride levels in the blood before you start and during treatment with everolimus.
- Decreased blood cell counts. Everolimus can cause you to have decreased red blood cells, white blood cells, and platelets. Your healthcare provider should do blood tests to check your blood cell counts before you start and during treatment with everolimus.
- Worsening side effects from radiation treatment, that can sometimes be severe. Tell your healthcare provider if you have had or are planning to receive radiation therapy.
The most common side effects of everolimus in people with advanced hormone receptor-positive, HER2-negative breast cancer, advanced neuroendocrine tumors of the pancreas, stomach and intestine (gastrointestinal) or lung, and advanced kidney cancer include:
- Infections
- Rash
- Feeling weak or tired
- Diarrhea
- Swelling of arms, hands, feet, ankles, face, or other parts of the body
- Stomach-area (abdominal) pain
- Nausea
- Fever
- Cough
- Headache
- Decreased appetite
The most common side effects of everolimus in people who have SEGA, renal angiomyolipoma, or certain types of seizures with TSC include respiratory tract infections.
Other side effects that may occur with everolimus:
- Absence of menstrual periods (menstruation). You may miss 1 or more menstrual periods. Tell your healthcare provider if this happens.
- Everolimus may affect fertility in females and may affect your ability to become pregnant. Talk to your healthcare provider if this is a concern for you.
- Everolimus may affect fertility in males and may affect your ability to father a child. Talk to your healthcare provider if this is a concern for you.
If you are taking everolimus to prevent transplant rejection:
Everolimus may cause serious side effects, including:
- See “Important information" above.
- swelling under your skin especially around your mouth, eyes and in your throat (angioedema). Your chance of having swelling under your skin is higher if you take everolimus along with certain other medicines. Tell your doctor right away or go to the nearest emergency room if you have any of these symptoms of angioedema:
- sudden swelling of your face, mouth, throat, tongue or hands
- hives or welts
- itchy or painful swollen skin
- trouble breathing
- delayed wound healing. Everolimus can cause your incision to heal slowly or not heal well. Call your doctor right away if you have any of the following symptoms:
- your incision is red, warm or painful
- blood, fluid, or pus in your incision
- your incision opens up
- swelling of your incision
- lung or breathing problems. Tell your doctor right away if you have new or worsening cough, shortness of breath, difficulty breathing or wheezing. In some patients lung or breathing problems have been severe, and can even lead to death. Your doctor may need to stop everolimus or lower your dose.
- increased cholesterol and triglycerides (fat in your blood). If your cholesterol and triglyceride levels are high your doctor may want to lower them with diet, exercise and certain medicines.
- protein in your urine (proteinuria).
- change in kidney function. Everolimus may cause kidney problems when taken along with a standard dose of cyclosporine medicine instead of a lower dose.
Your doctor should do blood and urine tests to monitor your cholesterol, triglycerides and kidney function. - viral infections. Certain viruses can live in your body and cause active infections when your immune system is weak. Viral infections that can happen with everolimus include BK virus-associated nephropathy. BK virus can affect how your kidney works and cause your transplanted kidney to fail.
- blood clotting problems.
- diabetes. Tell your doctor if you have frequent urination, increased thirst or hunger.
- infertility, male. Everolimus can affect fertility in males and may affect your ability to father a child. Talk with your doctor if this is a concern for you.
- infertility, female. Everolimus can affect fertility in females and may affect your ability to become pregnant. Talk to your doctor if this is a concern for you.
The most common side effects of everolimus in people who have had a kidney or liver transplant include:
These common side effects have been reported in both kidney and liver transplant patients:
- nausea
- swelling of the lower legs, ankles and feet
- high blood pressure
The most common side effects of everolimu in people who have had a kidney transplant include:
- constipation
- low red blood cell count (anemia)
- urinary tract infection
- increased fat in the blood (cholesterol and triglycerides)
The most common side effects of everolimus in people who have had a liver transplant include:
- diarrhea
- headache
- fever
- abdominal pain
- low white blood cells
Tell your healthcare provider if you have any side effect that bothers you or does not go away.
These are not all the possible side effects of everolimus. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
See more: Everolimus Side EffectsWhat other drugs will affect Everolimus?
Tell your healthcare provider about all of the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Everolimus may affect the way other medicines work, and other medicines can affect how everolimus works. Taking everolimus with other medicines can cause serious side effects.
Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine. Especially tell your healthcare provider if you take:
- St. John's Wort (Hypericum perforatum)
- Medicine for:
- Fungal infections
- Bacterial infections
- Tuberculosis
- Seizures
- HIV-AIDS
- Heart conditions or high blood pressure
- High cholesterol or triglycerides
- Medicines that weaken your immune system (your body’s ability to fight infections and other problems) such as:
- cyclosporine (Sandimmune, Gengraf, Neoral)
Ask your healthcare provider or pharmacist if you are not sure if your medicine is one of those taken for the conditions listed above. If you are taking any medicines for the conditions listed above, your healthcare provider might need to prescribe a different medicine or your dose of everolimus may need to be changed. You should also tell your healthcare provider before you start taking any new medicine.
What other information should I know?
Do not let anyone else take your medication. Ask your pharmacist any questions you have about refilling your prescription.
It is important for you to keep a written list of all of the prescription and nonprescription (over-the-counter) medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.