Generic name: fentanyl
Drug class: Opioids (narcotic analgesics)
Dosage form: injection, nasal spray, transdermal patch, sublingual tablet, sublingual spray, transmucosal lozenge (lollipop)
Availability: Prescription only
Pregnancy & Lactation: Risk data available
Brand names: Duragesic skin patch, Duragesic-100 (skin patch), Fentora, Ionsys, Onsolis
What is Fentanyl?
Fentanyl is a synthetic opioid medicine used to treat moderate to severe pain, it is up to 100 times stronger than other opioids like morphine, heroin or oxycodone. Fentanyl is from the class of medicines called narcotic analgesics.
What is Fentanyl used for?
- Fentanyl patches are used for long lasting pain relief for constant, around the clock cancer pain.
- Fentanyl nasal sprays, lollipops, injections, sublingual tablets and sprays are immediate acting and used for breakthrough pain. Breakthrough pain is when you have a flare up of pain, even though you are taking regular pain medicine for chronic or persistent pain.
Because fentanyl is a powerful prescription opioid it can be misused, abused and cause overdose deaths.
Fentanyl is classified as schedule 2 under the controlled substances act (CSA).
Warnings
Fentanyl can slow or stop your breathing, and may be habit-forming. MISUSE OF NARCOTIC MEDICINE CAN CAUSE ADDICTION, OVERDOSE, OR DEATH, especially in a child or other person using the medicine without a prescription.
Using this medicine during pregnancy may cause life-threatening withdrawal symptoms in the newborn.
Fatal side effects can occur if you use this medicine with alcohol, or with other drugs that cause drowsiness or slow your breathing.
How should I take Fentanyl
Fentanyl comes as a lozenge on a handle (Actiq), a sublingual (underneath the tongue) tablet (Abstral), a film (Onsolis), and a buccal (between the gum and cheek) tablet (Fentora) to dissolve in the mouth. Fentanyl is used as needed to treat breakthrough pain but not more often than four times a day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand.
Your doctor will probably start you on a low dose of fentanyl and gradually increase your dose until you find the dose that will relieve your breakthrough pain. If you still have pain 30 minutes after using fentanyl films (Onsolis), your doctor may tell you to use another pain medication to relieve that pain, and may increase your dose of fentanyl films (Onsolis) to treat your next episode of pain . Talk to your doctor about how well the medication is working and whether you are experiencing any side effects so that your doctor can decide whether your dose should be adjusted.
Do not use fentanyl more than four times a day. Call your doctor if you experience more than four episodes of breakthrough pain per day. Your doctor may need to adjust the dose of your other pain medication(s) to better control your pain.
Swallow the buccal tablet whole; do not split, chew, or crush. Also do not chew or bite the lozenge on a handle; only suck on this medication as directed.
Do not stop using fentanyl without talking to your doctor. Your doctor may decrease your dose gradually. If you suddenly stop using fentanyl, you may experience unpleasant withdrawal symptoms.
To use fentanyl lozenges (Actiq), follow these steps:
- Check the blister package and the handle of the lozenge to make sure the lozenge contains the dose of medication you have been prescribed.
- Use scissors to cut open the blister package and remove the lozenge. Do not open the blister package until you are ready to use the medication.
- Place the lozenge in your mouth, between your cheek and gum. Actively suck on the lozenge, but do not chew, crush, or bite it. Move the lozenge around in your mouth, from one side to the other, using the handle. Twirl the handle often.
- Do not eat or drink anything while the lozenge is in your mouth.
- Finish the lozenge in about 15 minutes.
- If you begin to feel dizzy, very sleepy, or nauseated before you have finished the lozenge, remove it from your mouth. Dispose of it immediately as described below or put it in the temporary storage bottle for later disposal.
- If you finish the entire lozenge, throw the handle away in a garbage can that is out of the reach of children. If you did not finish the entire lozenge, hold the handle under hot running water to dissolve all the medication, and then throw the handle away in a garbage can that is out of the reach of children and pets.
To use fentanyl buccal tablets (Fentora), follow these steps:
- Separate one blister unit from the blister card by tearing along the perforations. Peel back the foil to open the blister unit. Do not try to push the tablet through the foil. Do not open the blister unit until you are ready to use the tablet.
- Place the tablet in your mouth above one of your upper back teeth between your cheek and your gum.
- Leave the tablet in place until it dissolves completely. You may notice a gentle bubbling feeling between your cheek and gum as the tablet dissolves. It may take 14 to 25 minutes for the tablet to dissolve. Do not split, chew, bite, or suck the tablet.
- If any of the tablet is left in your mouth after 30 minutes, swallow it with a drink of water.
- If you begin to feel dizzy, very sleepy, or nauseated before the tablet dissolves, rinse your mouth with water and spit the remaining pieces of tablet into the sink or toilet. Flush the toilet or rinse the sink to wash away the tablet pieces.
To use fentanyl sublingual tablets (Abstral), follow these steps:
- Take a sip of water to moisten your mouth if it is dry. Spit out or swallow the water. Make sure your hands are dry before handling the tablet.
- Separate one blister unit from the blister card by tearing along the perforations. Peel back the foil to open the blister unit. Do not try to push the tablet through the foil. Do not open the blister unit until you are ready to use the tablet.
- Place the tablet under your tongue as far back as you can. If more than 1 tablet is needed for your dose, spread them around on the floor of your mouth under your tongue.
- Leave the tablet in place until it dissolves completely. Do not suck, chew, or swallow the tablet.
- Do not eat or drink anything until the tablet is completely dissolved and you no longer feel it in your mouth.
To use fentanyl films (Onsolis), follow these steps:
- Use scissors to cut along the arrows of the foil package to open it. Separate the layers of the foil package and remove the film. Do not open the foil package until you are ready to use the medication. Do not cut or tear the film.
- Use your tongue to wet the inside of your cheek, or if needed, rinse your mouth with water to wet the area where you will place the film.
- Hold the film on a clean, dry finger, with the pink side facing up. Place the film in your mouth, with the pink side against the inside of your moistened cheek. With your finger, press the film against your cheek for 5 seconds. Then remove your finger and the film will stick to the inside of your cheek. If more than one film is needed for your dose, do not put the films on top of each other. You may place the films on either side of your mouth.
- Leave the film in place until it dissolves completely. The film will release a minty flavor as it dissolves. It may take 15 to 30 minutes for the film to dissolve. Do not chew or swallow the film. Do not touch or move the film while it dissolves.
- You may drink liquids after 5 minutes, but do not eat anything until the film dissolves completely.
Dosing information
- Do not use fentanyl unless you are already being treated with a similar opioid pain medicine and your body is tolerant to it. Talk with your doctor if you are not sure you are opioid-tolerant.
- Take fentanyl exactly as prescribed by your healthcare provider. Follow the directions on your prescription label and read all medication guides. Never use fentanyl in larger amounts, or for longer than prescribed. Tell your doctor if you feel an increased urge to use more fentanyl.
- Never share opioid medicine with another person, especially someone with a history of drug abuse or addiction. MISUSE CAN CAUSE ADDICTION, OVERDOSE, OR DEATH. Keep the medication in a place where others cannot get to it. Selling or giving away opioid medicine is against the law.
- Do not replace one form of fentanyl with any other form of fentanyl, such as injection, skin patch, nasal spray, under the tongue spray, sublingual tablet or "lollipop" device).
- Store fentanyl in its original packaging at room temperature.
- Keep fentanyl out of the reach of children or pets. A small amount of fentanyl can be fatal to a child or pet who accidentally ingests or absorbs it. Seek emergency medical attention if this happens.
- Do not keep leftover opioid medication. Just one dose can cause death in someone using this medicine accidentally or improperly. Ask your pharmacist where to locate a drug take-back disposal program. If there is no take-back program, dispose of any unused skin patches in the same folded manner. Do not flush the fentanyl patch foil pouch or patch liners; place them in a trash container out of the reach of children and pets. For sublingual tablets, sublingual sprays, nasal sprays, lozenges carefully follow disposal instructions when this medicine is no longer needed.
Before Taking
You should not use fentanyl unless you are already being treated with a similar opioid pain medicine and your body is tolerant to it. Talk with your doctor if you are not sure you are opioid-tolerant.
You should only use or take fentanyl if you have your own personal prescription for this medicine. You should not use fentanyl if you are allergic to it, or if you have:
- severe asthma or other breathing problems; or
- a stomach or bowel obstruction (including paralytic ileus).
To make sure fentanyl is safe for you, tell your doctor if you have ever had:
- breathing problems, sleep apnea;
- a head injury, brain tumor, or mental illness;
- alcoholism or drug addiction;
- urination problems;
- a seizure disorder;
- liver or kidney disease; or
- problems with your gallbladder, pancreas, or thyroid.
If you are using fentanyl patches, tell your doctor if you have been sick with a fever. Having a high temperature can increase the amount of drug you absorb through your skin.
If you use opioid medicine while you are pregnant, your baby could become dependent on the drug. This can cause life-threatening withdrawal symptoms in the baby after it is born. Babies born dependent on opioids may need medical treatment for several weeks.
Do not breastfeed while you are using fentanyl.
Do not change to another form of fentanyl eg injection, skin patch, dissolving film, or "lollipop" device. If you switch from another form of fentanyl, you will not use the same dose.
Fentanyl products
Long acting fentanyl:
- fentanyl patches
Immediate acting fentanyl:
- fentanyl lozenge on a plastic handle - lollipop (Actiq)
- fentanyl nasal spray (Lazanda)
- fentanyl sublingual tablet (Fentora)
- fentanyl sublingual spray (Subsys)
- fentanyl injection
What is a fentanyl patch?
Fentanyl patches are applied to the skin to treat moderate to severe chronic pain around the clock. Fentanyl patches are used when other pain treatments such as non-opioid pain medicines or immediate-release opioid medicines do not treat your pain well enough or you cannot tolerate them.
Fentanyl patches are not for treating mild or occasional pain or pain from surgery. The patches are only used to treat constant around-the-clock pain.
One patch is applied to the skin and left on for 72 hours, then you remove the patch and apply a new patch straightaway.
Discontinue all other extended-release opioids when beginning therapy.
Due to the risk of respiratory depression, the transdermal patch is for use in opioid-tolerant patients only; opioid tolerant patients have been taking at least: morphine 60 mg daily, oral oxycodone 30 mg daily, oral hydromorphone 8 mg daily, or an equianalgesic dose of another opioid for 1 week or longer.
Comments
- Do not begin a patient on a fentanyl transdermal patch as their first opioid.
- A small number of patients may require a 48-hour dosing interval; an increase in dose should be evaluated before changing dosing intervals.
What is a fentanyl sublingual spray?
Fentanyl sublingual spray (brand name: Subsys) is used to treat breakthrough cancer pain that is not controlled by other medicines. Fentanyl sublingual spray is sprayed under the tongue when required for pain. Hold the liquid under the tongue for 30 to 60 seconds. Do not spit, swallow, or rinse your mouth during this time.
Fentanyl sublingual spray should be used together with other non-fentanyl narcotic pain medicines that are used around the clock.
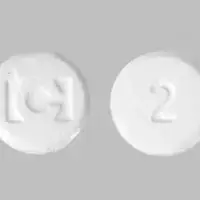
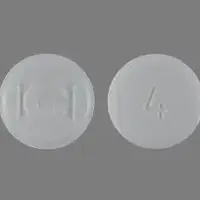
What are fentanyl buccal tablets?
Fentanyl buccal tablets (brand name: Fentora) are used to treat short episodes of "breakthrough" cancer pain that is not controlled by other medicines. The sublingual tablets are used in the mouth but not swallowed whole, instead the tablet is placed inside the mouth between the cheek and gum (buccal) or on the floor of your mouth under your tongue (sublingual) then allowed to dissolve.
Wait 30 minutes after using this medicine. If there is any of the tablet left in your mouth, you may drink a glass of water to help you swallow the leftover medicine.
Do not crush, split, suck, or chew fentanyl tablets, or swallow the tablets whole. You will get less relief for your breakthrough cancer pain.
It is important for you to keep taking your around-the-clock opioid pain medicine while using Fentora.
What are fentanyl ‘lollipops’ or lozenges?
Fentanyl lozenges (brand name: Actiq) are a lozenge containing fentanyl citrate that is attached to a plastic handle (lollipop), they are used to treat breakthrough cancer pain. They can be used by cancer patients 16 years of age and older who are already receiving and who are tolerant to around-the-clock opioid pain medicine for their background cancer pain.
Place the medicine in your mouth between your cheek and gum, and hold the handle with your fingers. Twirl the handle to move the medicine around in your mouth while sucking on it.
If you switch from using lozenge to using other forms of fentanyl, you will need to use a different dose. Many forms of fentanyl are given at lower doses than the lozenges. If you use the same dose of each medication, you may have life-threatening overdose symptoms.
What is fentanyl nasal spray?
Fentanyl nasal spray (brand name: Lazanda) is a nasal spray that contains fentanyl and is used to treat "breakthrough" pain for cancer patients.
The usual starting dose of fentanyl nasal spray (brand name: Lazanda) is 1 single spray into 1 nostril. Your doctor may change your dose. Follow all directions on your prescription label. Fentanyl can slow or stop your breathing. Never use fentanyl nasal spray in larger amounts, or for longer than prescribed. Tell your doctor if the medicine seems to stop working as well in relieving your pain.
Patients should also be using around the clock non-fentanyl narcotic pain medicine.
If you switch to fentanyl nasal spray from another form of fentanyl, you will not use the same dose. You must start with the lowest dose (100 micrograms).
What are fentanyl injections used for?
Fentanyl injections are used in a hospital setting as an analgesic or anesthetic premedication for surgery.
What happens if I miss a dose?
For fentanyl patches if you are using the skin patches on a schedule, apply the missed patch as soon as you remember. Continue wearing the patch for up to 72 hours and then apply a new one if needed for pain. Do not wear extra patches to make up a missed dose.
For fentanyl lollipops, nasal spray, sublingual tablets or spray since they are used for acute pain, you are not likely to miss a dose of this medicine. Skip any missed dose if it is almost time for your next scheduled dose. Do not use extra medicine to make up the missed dose.
Fentanyl overdose and abuse
Although fentanyl is a legal prescription drug used for pain control during surgery and for chronic or breakthrough cancer pain it is also being manufactured illegally or legal prescriptions are diverted and fentanyl is misused and abused as it is sold for its euphoric effects.
- Street drugs like heroin, cocaine and methamphetamine can also be laced with fentanyl, also counterfeit drugs including hydrocodone tablets or Xanax.
- Users may not realize the street drug they are buying from a dealer contains this potentially lethal compound.
- Fentanyl test strips can be used to test if drugs have been laced with fentanyl.
- Fentanyl is extremely potent, this means just 2 to 3 milligrams of this drug can lead to death due to respiratory depression (decreased breathing) which can quickly lead to coma and death.
- In 2021 there were 71,238 fentanyl overdose deaths in the United States.
What happens if I overdose?
Naloxone (Narcan nasal spray, Kloxxado nasal spray, Zimhi injection, Naloxone injection) is a safe and easily accessible medication used to reverse an opioid overdose and help restore breathing by blocking or reversing the opioid effects.
If an overdose is due to fentanyl then multiple bolus injections of naloxone or even continuous infusions may be needed to reverse the opioid action. Learn how to use naloxone before it is needed.
- If you believe someone has overdosed, administer naloxone, and then immediately call emergency personnel, such as 911.
- Naloxone can be life-saving for patients who overdose on narcotics, although in patients dependent upon opioids, it can also cause a severe withdrawal effect.
- If symptoms return, give another dose of naloxone in 2 to 3 minutes. Larger or repeat naloxone doses may be required until emergency responders arrive.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. A fentanyl overdose can be fatal, especially in a child or other person using the medicine without a prescription. Overdose symptoms may include extreme drowsiness, weak pulse, fainting, and slow breathing (breathing may stop).
What should I know about storage and disposal of this medication?
Keep this medication in the packaging it came in, tightly closed, and out of reach of children. Store fentanyl in a safe place so that no one else can use it accidentally or on purpose. Use the child-resistant locks and other supplies provided by the manufacturer to keep children away from the lozenges. Keep track of how much fentanyl is left so you will know if any is missing. Store fentanyl at room temperature and away from excess heat and moisture (not in the bathroom). Do not freeze fentanyl.
You must immediately dispose of any medication that is outdated or no longer needed through a medicine take-back program.. If you do not have a take-back program nearby or one that you can access promptly, then flush the fentanyl down the toilet so that others will not take it. Dispose of unneeded lozenges by removing each lozenge from the blister package, holding the lozenge over the toilet, and cutting off the medicine end with wire cutters so that it falls into the toilet. Throw away the remaining handles in a place that is out of the reach of children and pets, and flush the toilet twice when it contains up to five lozenges. Dispose of unneeded tablets or films by removing them from the packaging and flushing them down the toilet. Throw the remaining fentanyl packaging or cartons into a trash container; do not flush these items down the toilet. Call your pharmacist or the manufacturer if you have questions or need help disposing of unneeded medication.
It is important to keep all medication out of sight and reach of children as many containers (such as weekly pill minders and those for eye drops, creams, patches, and inhalers) are not child-resistant and young children can open them easily. To protect young children from poisoning, always lock safety caps and immediately place the medication in a safe location – one that is up and away and out of their sight and reach. http://www.upandaway.org
What special dietary instructions should I follow?
Do not eat grapefruit or drink grapefruit juice while using this medication.
What should I avoid while using Fentanyl?
Do not drink alcohol. Dangerous side effects or death could occur.
Fentanyl may impair your thinking or reactions. Avoid driving or operating machinery until you know how this medicine will affect you. Dizziness or severe drowsiness can cause falls or other accidents.
Grapefruit and grapefruit juice may interact with fentanyl and lead to unwanted side effects. Discuss the use of grapefruit products with your doctor.
Fentanyl side effects
Get emergency medical help if you have signs of an allergic reaction to fentanyl: hives; difficulty breathing; swelling of your face, lips, tongue, or throat.
Like other narcotic medicines, fentanyl can slow your breathing. Death may occur if breathing becomes too weak. A person caring for you should seek emergency medical attention if you have slow breathing with long pauses, blue colored lips, or if you are hard to wake up.
Fentanyl may cause serious side effects. Call your doctor at once if you have:
- slow heart rate, sighing, shallow breathing, breathing that stops during sleep;
- severe drowsiness, feeling like you might pass out;
- confusion, extreme fear, unusual thoughts or behavior; or
- low cortisol levels - nausea, vomiting, loss of appetite, dizziness, worsening tiredness or weakness.
Seek medical attention right away if you have symptoms of serotonin syndrome, such as: agitation, hallucinations, fever, sweating, shivering, fast heart rate, muscle stiffness, twitching, loss of coordination, nausea, vomiting, or diarrhea.
Serious side effects may be more likely in older adults and those who are malnourished or debilitated.
Long-term use of opioid medication may affect fertility (ability to have children) in men or women. It is not known whether opioid effects on fertility are permanent.
Common fentanyl side effects may include:
- headache, dizziness, drowsiness, pale skin, feeling weak or tired
- constipation, nausea, vomiting, stomach pain or
- sleep problems (insomnia)
- swelling in your hands or feet
- increased sweating, or cold feeling
- for patches itching, redness, or rash where a patch was worn.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
See more: Fentanyl Side EffectsWhat other drugs will affect Fentanyl?
You may have breathing problems or withdrawal symptoms if you start or stop taking certain other medicines. Tell your doctor if you also use an antibiotic, antifungal medication, heart or blood pressure medication, seizure medication, or medicine to treat HIV or hepatitis C.
Fentanyl can interact with many other drugs and cause dangerous side effects or death. Be sure your doctor knows if you also use:
- other narcotic medications - opioid pain medicine or prescription cough medicine;
- a sedative like Valium - diazepam, alprazolam, lorazepam, Ativan, Klonopin, Restoril, Tranxene, Versed, Xanax, and others;
- drugs that make you sleepy or slow your breathing - a sleeping pill, muscle relaxer, tranquilizer, antidepressant, or antipsychotic medicine;
- cold or allergy medicines, bronchodilator asthma/COPD medication, or a diuretic ("water pill");
- medicines for motion sickness, irritable bowel syndrome, or overactive bladder;
- drugs that affect serotonin levels in your body - medicine for depression, Parkinson's disease, migraine headaches, serious infections, or prevention of nausea and vomiting.
This list is not complete. Other drugs may interact with fentanyl, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed in this medication guide.
What other information should I know?
Keep all appointments with your doctor.
Do not let anyone else use your medication, even if he or she has the same symptoms that you have. Selling or giving away this medication may cause severe harm or death to others and is against the law.
This prescription is not refillable. Be sure to schedule appointments with your doctor on a regular basis so that you do not run out of medication.
It is important for you to keep a written list of all of the prescription and nonprescription (over-the-counter) medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.