Generic name: ibrutinib
Drug class: BTK inhibitors
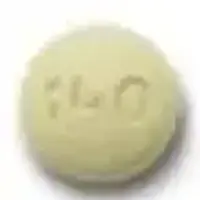
Dosage form: capsule
Availability: Prescription only
Pregnancy & Lactation: Risk data available
Brand names: Ibrutinib
What is Imbruvica?
Imbruvica (ibrutinib) is an oral targeted treatment that may be used alone or in combination with other medications to treat adults with the following types of blood cancers:
- Chronic lymphocytic leukemia (CLL)/ small lymphocytic lymphoma (SLL)
- Chronic lymphocytic leukemia (CLL)/Small lymphocytic lymphoma (SLL) with 17p deletion
- Waldenström’s macroglobulinemia (WM).
It may also be used to treat adults and children aged 1 year and older with chronic graft versus host disease (cGVHD) after failure of one or more lines of systemic therapy.
The accelerated approval status for Imbruvica for Mantle Cell Lymphoma (MCL) and Marginal Zone Lymphoma (MZL) was voluntarily withdrawn on April 6, 2023. This was because, although the Phase 3 SHINE study for MCL met its primary endpoint of progression-free survival (PFS), it was associated with an increased rate of adverse reactions. For MZL, the phase 3 SELENE study did not meet its primary endpoint of PFS.
Imbruvica works by directly inhibiting an enzyme, called Bruton’s tyrosine kinase (BTK). It forms a covalent bond with a cysteine residue on the enzyme, preventing its activity. BTK works as a signaling molecule for the B-cell antigen receptor (BCR) and cytokine receptor pathways. Activation of these pathways causes the proliferation of B cells and other interactions, and inhibition has been shown to reduce the growth and spread of malignant B cells. It belongs to the class of medicines known as BTK inhibitors.
Imbruvica was first FDA-approved on November 13, 2013.
Warnings
Serious hemorrhage, including intracranial or gastrointestinal hemorrhage, hematuria, and post-procedural hemorrhage has occurred in people receiving Imbruvica, 0.4% have been fatal. 39% of people reported bleeding of any grade, including purpura and petechiae. Coadministration with antiplatelet or anticoagulants may increase the risk. Your doctor will monitor for signs and symptoms of bleeding and discontinue if serious bleeding occurs. They may consider withholding Imbruivca for 3 to 7 days pre and post surgery depending on the risk of bleeding. Call your doctor at once if you have signs of bleeding inside your body, such as dizziness, confusion, headache, speech problems, black or bloody stools, pink or brown urine, or coughing up blood or vomit that looks like coffee grounds.
Imbruvica affects your immune system. Serious bacterial, viral, or fungal infections have been reported with Imbruvica; 21% were Grade 3 or higher. Cases of progressive multifocal leukoencephalopathy (PML) and Pneumocystis jirovecii pneumonia (PJP) have occurred, in addition to reactivation of hepatitis B. Consider prophylaxis for herpes simplex virus, pneumocystis jirovecii pneumonia, and other infections in patients who are at increased risk for infections. Tell your doctor if you have a fever, chills, cough, mouth sores, or other signs of infection.
Serious cardiac arrhythmias, including Atrial fibrillation and atrial flutter, have been reported in patients treated with Imbruvica. The risk is more likely in those with cardiac risk factors, high blood pressure, and acute infections. High blood pressure occurred in 19% of people prescribed Imbruvica in clinical trials. Monitor yourself for signs and symptoms of cardiac arrhythmias (such as palpitations, dizziness, dizziness when standing, and shortness of breath) and report these to your doctor immediately. Your doctor will check your blood pressure regularly.
Blood count abnormalities, including neutropenia, thrombocytopenia, and anemia, have occurred in people receiving Imbruvica. Your doctor will perform regular blood counts and interrupt treatment, reduce the dose, or discontinue treatment as warranted.
Using Imbruvica may increase your risk of developing other cancers, such as non-melanoma skin cancer. Ask your doctor about this risk and what skin symptoms to watch for. Wear protective clothing and use sunscreen (SPF 30 or higher) when you are outdoors.
Tumor Lysis syndrome has been reported infrequently with Imbruvica. Symptoms include nausea and vomiting, diarrhea, and muscle cramps. If you have any symptoms like these, report them to your doctor.
Imbruvica can cause fetal harm when administered to a pregnant woman, including malformations. Women should use effective contraception and avoid becoming pregnant while taking Imbruivca and for 1 month after the last dose. Men should avoid fathering a child during treatment and for 1 month after the last dose.
How should I take Imbruvica
Take Imbruvica exactly as prescribed by your doctor. Follow all directions on your prescription label and read all medication guides or instruction sheets.
Take this medicine with a full glass of water, at the same time each day. Drink plenty of liquids while you are taking Imbruvica.
Swallow the Imbruvica tablet or capsule whole and do not crush, chew, break, or open it.
Shake the oral suspension (liquid). Measure a dose with the supplied measuring device (not a kitchen spoon).
Tell your healthcare providers if you have a planned surgery.
You may get dehydrated during prolonged illness. Call your doctor if you are sick with vomiting or diarrhea.
You may get infections or bleed more easily. You will need frequent blood and medical tests.
Dosing information
The dose of Imbruvica varies depending on the condition being treated:
Dosage for Adults with CLL/SLL and WM
- 420mg once daily
Dosage for cGVHD
- Patients 12 years and older: 420mg once daily
- Patients 1 year old to less than 12 years old: 240mg/m2 once daily (up to a maximum dosage of 420mg once daily).
Before Taking
To make sure Imbruvica is safe for you, tell your doctor if you have ever had:
- an infection
- bleeding problems
- take a blood thinner such as warfarin
- a heart rhythm disorder
- risk factors for heart disease (such as diabetes, smoking, being overweight, having high blood pressure or high cholesterol)
- low blood cell counts
- recent surgery or plan to have surgery, medical or dental procedure or
- liver disease.
Taking Imbruvica may increase your risk of developing other cancers. Ask your doctor about this risk.
Ibrutinib can harm an unborn baby if the mother or the father is using Imbruvica.
If you are a woman, you may need a pregnancy test to make sure you are not pregnant. Use birth control while using Imbruvica and for at least 1 month after your last dose. If you are a man, use birth control if your sex partner can get pregnant. Keep using birth control for at least 1 month after your last dose. Tell your doctor right away if a pregnancy occurs.
Do not breastfeed while using Imbruvica, and for at least 1 week after your last dose.
What happens if I miss a dose?
Take the missed dose on the same day you remember it. Take your next dose at the regular time and stay on your once-daily schedule. Do not take 2 doses on the same day.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
What should I avoid while using Imbruvica?
Grapefruit and Seville oranges may interact with ibrutinib and cause side effects. Avoid consuming grapefruit products and orange marmalades.
Imbruvica side effects
Get emergency medical help if you have signs of an allergic reaction to Imbruvica: hives, difficulty breathing, swelling of your face, lips, tongue, or throat.
Imbruvica may cause a brain infection that can lead to disability or death. Tell your doctor if you have problems with speech, thought, vision, or muscle movement. These symptoms can get worse quickly.
You may get infections more easily, even serious or fatal infections. Call your doctor right away if you have signs of infection such as:
- fever, chills, sore throat
- mouth sores, red or swollen gums
- pale skin, easy bruising, unusual bleeding or
- chest discomfort, wheezing, dry cough or hack, rapid weight loss.
Imbruvica can cause you to bleed more easily. Call your doctor or seek emergency medical attention if you have:
- easy bruising, unusual bleeding, or any bleeding that will not stop
- bleeding inside your body - weakness, dizziness; pink or brown urine; abnormal vaginal bleeding; bloody or tarry stools, coughing up blood or vomit that looks like coffee grounds or
- bleeding in your brain - sudden weakness (especially on one side of the body), severe headache, problems with speech or vision.
Imbruvica may cause serious side effects. Call your doctor at once if you have:
- severe or ongoing diarrhea
- heart problems - swelling, rapid weight gain, feeling short of breath
- heart rhythm disorders - dizziness, chest pain, shortness of breath, fast or irregular heart rate, feeling light-headed
- high blood pressure - severe headache, blurred vision, pounding in your neck or ears
- low blood cell counts - fever, chills, tiredness, mouth sores, skin sores, easy bruising, unusual bleeding, pale skin, cold hands and feet, feeling light-headed or short of breath
- kidney problems - swelling, urinating less, feeling tired or short of breath or
- signs of tumor cell breakdown - tiredness, weakness, muscle cramps, nausea, vomiting, diarrhea, fast or slow heart rate, tingling in your hands and feet or around your mouth.
Your cancer treatments may be delayed or permanently discontinued if you have certain side effects.
Common Imbruvica side effects reported by more than 30% of people taking Imbruvica include:
- diarrhea, nausea, stomach pain
- fever, cough, trouble breathing
- mouth sores
- feeling tired
- low blood cell counts
- muscle spasms
- bruising, rash or
- muscle, joint, or bone pain.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
See more: Imbruvica Side EffectsWhat other drugs will affect Imbruvica?
Sometimes it is not safe to use certain medicines at the same time. Some drugs can affect your blood levels of other drugs you use, which may increase side effects or make the medicines less effective.
- Moderate to strong CYP3A Inhibitors, such as clarithromycin, nefazodone, itraconazole, ketoconazole, atazanavir, ritonavir, grapefruit juice, erythromycin, or verapamil
- Moderate to strong CYP3A inducers, such as glucocorticoids, rifampin, carbamazepine, phenobarbital, and phenytoin. Avoid coadministration.
Other drugs may interact with ibrutinib, including prescription and over-the-counter medicines, vitamins, and herbal products. Tell your doctor about all other medicines you use.