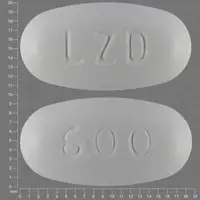
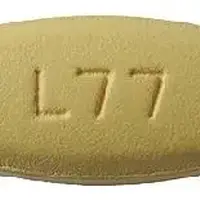
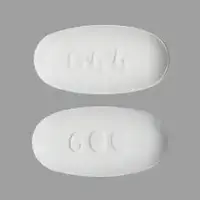
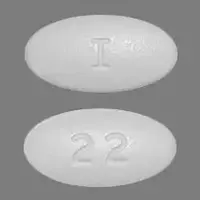
Generic name: zyvox
Availability: Prescription only
Pregnancy & Lactation: Risk data available
Brand names: Zyvox, Linezolid (oral/injection)
What is Linezolid (monograph)?
Introduction
Antibacterial; oxazolidinone.
Uses for Linezolid
Respiratory Tract Infections
Treatment of community-acquired pneumonia (CAP), including infections associated with concurrent bacteremia, caused by susceptible Streptococcus pneumoniae.
Treatment of CAP caused by susceptible Staphylococcus aureus (methicillin-susceptible [oxacillin-susceptible] strains only). Also recommended for treatment of CAP caused by methicillin-resistant S. aureus† [off-label] (MRSA; also known as oxacillin-resistant S. aureus or ORSA).
Treatment of nosocomial pneumonia caused by susceptible S. aureus (including MRSA) or S. pneumoniae.
Not indicated for treatment of respiratory tract infections caused by gram-negative bacteria. It is imperative that an anti-infective active against gram-negative bacteria be used concomitantly if documented or presumed pathogens include gram-negative bacteria.
For information regarding treatment of pneumonia, consult current IDSA clinical practice guidelines available at [Web].
Skin and Skin Structure Infections
Treatment of uncomplicated skin and skin structure infections caused by susceptible S. aureus (methicillin-susceptible [oxacillin-susceptible] strains only) or S. pyogenes (group A β-hemolytic streptococci, GAS).
Treatment of complicated skin and skin structure infections (including diabetic foot infections), without concurrent osteomyelitis, caused by susceptible S. aureus (including MRSA), S. pyogenes, or S. agalactiae (group B streptococci, GBS).
Not evaluated for use in the treatment of decubitus ulcers.
Not indicated for treatment of skin and skin structure infections caused by gram-negative bacteria. It is imperative that an anti-infective active against gram-negative bacteria be used concomitantly if the documented or presumed pathogens include gram-negative bacteria.
For information regarding treatment of skin and skin structure infections, consult current IDSA clinical practice guidelines available at [Web].
Vancomycin-resistant Enterococcus faecium Infections
Treatment of infections caused by susceptible vancomycin-resistant Enterococcus faecium, including infections associated with concurrent bacteremia.
Has been used for treatment of native valve or prosthetic valve infective endocarditis† [off-label] caused by vancomycin-resistant or multidrug-resistant E. faecium. AHA recommends that patients with infective endocarditis attributable to enterococci resistant to penicillins, aminoglycosides, and vancomycin be managed by a team of specialists in infectious disease, cardiology, cardiovascular surgery, clinical pharmacy, and, if necessary, pediatrics.
For information on diagnosis and management of infective endocarditis and its complications, including anti-infective treatment of enterococcal endocarditis, consult current AHA guidelines available at [Web].
Tuberculosis
Used in multiple-drug regimens for treatment of multidrug-resistant (MDR) tuberculosis† [off-label] caused by Mycobacterium tuberculosis (i.e., caused by M. tuberculosis resistant to isoniazid and rifampin). ATS, CDC, and IDSA state that linezolid is one of various options that can be considered for inclusion in multiple-drug regimens used for treatment of MDR tuberculosis. WHO recommends that linezolid be included in multiple-drug regimens used for longer-term treatment (≥18 months) of multidrug- or rifampin-resistant (MDR/RR) tuberculosis.
Used in a 3-drug combination regimen that includes bedaquiline and pretomanid for treatment of extensively drug resistant (XDR) pulmonary tuberculosis (i.e., caused by M. tuberculosis resistant to isoniazid, rifampin, any fluoroquinolone, and at least one injectable antituberculosis agent) or treatment-intolerant or non-responsive MDR pulmonary tuberculosis. WHO states that the 3-drug regimen of pretomanid, bedaquiline, and linezolid (also known as BPaL) may be used for treatment of MDR tuberculosis in patients who have not previously received either bedaquiline or linezolid (or received the drugs for ≤2 weeks) and have documented evidence that the MDR strain also is resistant to a fluoroquinolone.
Patients with MDR or XDR tuberculosis are at high risk for treatment failure and acquisition of further drug resistance. ATS, CDC, and IDSA recommend that such patients be referred to or that consultation be obtained from a specialized treatment center as identified by local or state health departments or the CDC.
For additional information on treatment of MDR and XDR tuberculosis, consult current guidelines from ATS/CDC/IDSA and WHO.
Linezolid Dosage and Administration
Administration
Administer orally or by IV infusion.
When clinically appropriate, IV route may be switched to oral without dosage adjustment.
Avoid large quantities of foods or beverages with high tyramine content during linezolid treatment. (See Monoamine Oxidase Inhibition under Cautions.)
Oral Administration
Administer orally without regard to meals.
Reconstitution
Reconstitute powder for oral suspension at time of dispensing by adding amount of water specified on bottle to provide a suspension containing 100 mg/5 mL. After tapping bottle gently to loosen the powder, add water in 2 portions and agitate well after each addition.
Prior to administration of each dose, gently mix suspension by inverting bottle 3–5 times; do not shake.
IV Administration
For solution and drug compatibility information, see Compatibility under Stability.
Single-use containers of linezolid injection for IV infusion should be administered without further dilution. Do not use the containers in series connections; do not introduce additives into the solution.
Rate of Administration
Administer by IV infusion over 30–120 minutes.
Dosage
Manufacturer states safety and efficacy of >28 days of linezolid treatment not evaluated in controlled clinical trials. The drug is administered for longer durations when used in multiple-drug regimens for treatment of MDR tuberculosis.
Pediatric Patients
General Dosage for Neonates
Oral or IV
Neonates: Manufacturer recommends 10 mg/kg every 12 hours initially in premature neonates <7 days of age; may consider 10 mg/kg every 8 hours in those with inadequate response. Manufacturer recommends 10 mg/kg every 8 hours in all neonates ≥7 days of age.
Neonates ≤7 days of age: AAP recommends 10 mg/kg every 12 hours in those with gestational age <34 weeks and 10 mg/kg every 8 hours in those with gestational age ≥34 weeks.
Neonates 8–28 days of age: AAP recommends 10 mg/kg every 8 hours, regardless of gestational age.
Respiratory Tract Infections
Community-acquired or Nosocomial Pneumonia
Oral or IVChildren 7 days through 11 years of age: 10 mg/kg every 8 hours for 10–14 days.
Adolescents ≥12 years of age: 600 mg every 12 hours for 10–14 days.
Skin and Skin Structure Infections
Uncomplicated Skin and Skin Structure Infections
OralChildren 7 days through 4 years of age: 10 mg/kg every 8 hours for 10–14 days.
Children 5 through 11 years of age: 10 mg/kg every 12 hours for 10–14 days.
Adolescents ≥12 years of age: 600 mg every 12 hours for 10–14 days.
Complicated Skin and Skin Structure Infections
Oral or IVChildren 7 days through 11 years of age: 10 mg/kg every 8 hours for 10–14 days.
Adolescents ≥12 years of age: 600 mg every 12 hours for 10–14 days.
Vancomycin-resistant Enterococcus faecium Infections
Oral or IV
Children 7 days through 11 years of age: 10 mg/kg every 8 hours for 14–28 days.
Adolescents ≥12 years of age: 600 mg every 12 hours for 14–28 days.
Adults
Respiratory Tract Infections
Community-acquired or Nosocomial Pneumonia
Oral or IV600 mg every 12 hours for 10–14 days.
Skin and Skin Structure Infections
Uncomplicated Skin and Skin Structure Infections
Oral400 mg every 12 hours for 10–14 days.
Complicated Skin and Skin Structure Infections
Oral or IV600 mg every 12 hours for 10–14 days.
Vancomycin-resistant Enterococcus faecium Infections
Oral or IV
600 mg every 12 hours for 14–28 days.
Active Tuberculosis
XDR or Treatment-intolerant or Non-responsive MDR Pulmonary Tuberculosis
Oral1.2 g daily for 26 week. Adjustment of dosage to 600 mg daily with further reductions to 300 mg daily or interruption of linezolid therapy may be required if myelosuppression, peripheral neuropathy, or optic neuropathy occurs.
Must administer in conjunction with oral pretomanid (200 mg once daily for 26 weeks) and bedaquiline (400 mg once daily for 2 weeks followed by 200 mg 3 times weekly [with at least 48 hours between doses] for 24 weeks).
The 3-drug combination regimen should be continued for 26 weeks, but may be extended beyond 26 weeks if necessary.
Special Populations
Hepatic Impairment
Mild to moderate hepatic impairment (Child-Pugh class A or B): Dosage adjustments not needed.
Severe hepatic impairment: Pharmacokinetics not evaluated.
Renal Impairment
Dosage adjustments not needed. Consider that linezolid metabolites may accumulate in patients with renal impairment; clinical importance unknown. (See Renal Impairment under Cautions.)
Hemodialysis patients: Administer linezolid doses after dialysis session.
Geriatric Patients
Dosage adjustments not needed.
Warnings
Contraindications
-
Known hypersensitivity to linezolid or any ingredient in the formulation.
-
Current or recent (within the last 2 weeks) treatment with drugs that inhibit MAO A or B (e.g., isocarboxazid, phenelzine). (See Specific Drugs under Interactions.)
Warnings/Precautions
Hematologic Effects
Myelosuppression (anemia, leukopenia, pancytopenia, thrombocytopenia) reported.
Toxicity studies in adult and juvenile dogs and rats indicate myelosuppression (bone marrow hypocellularity/decreased hematopoiesis; decreased extramedullary hematopoiesis in spleen and liver; decreased levels of circulating erythrocytes, leukocytes, and platelets) and lymphoid depletion in thymus, lymph nodes, and spleen.
Monitor CBCs weekly during linezolid treatment, especially in those receiving the drug for >2 weeks and in those who have preexisting myelosuppression, are receiving concomitant drugs associated with bone marrow suppression, or have a chronic infection that was or is being treated with concomitant anti-infective therapy.
Consider discontinuing linezolid if myelosuppression develops or worsens. Hematologic parameters generally have increased toward pretreatment values following discontinuance of the drug.
Peripheral and Optic Neuropathy
Peripheral and optic neuropathies reported in adults and children receiving linezolid, principally in those receiving the drug for >28 days. Optic neuropathy progressing to loss of vision reported when linezolid used for >28 days. Blurred vision reported in some patients who received the drug for <28 days.
If patient experiences symptoms of visual impairment (e.g., changes in visual acuity or color vision, blurred vision, visual field defect), promptly perform an ophthalmic evaluation. Monitor visual function in all patients receiving linezolid for extended periods of time (i.e., ≥3 months). In addition, monitor visual function in all patients reporting a new visual symptom, regardless of length of linezolid treatment.
If peripheral or optic neuropathy occurs, weigh potential benefits versus risks of continued linezolid treatment.
Serotonin Syndrome
Serotonin syndrome (including some fatalities) reported in patients receiving linezolid concomitantly with serotonergic drugs. Signs and symptoms of serotonin syndrome include mental changes (confusion, hyperactivity, memory problems), muscle twitching, excessive sweating, shivering, shaking, diarrhea, loss of coordination, and/or fever.
Most reported cases occurred in patients receiving linezolid concomitantly with SSRIs or SNRIs. FDA has not concluded whether concomitant use of linezolid with other drugs with lesser degrees of serotonergic activity (e.g., tricyclic antidepressants, MAO inhibitors) is associated with a risk comparable to that reported with SSRIs or SNRIs.
Unless considered clinically appropriate and patients can be carefully monitored for signs and/or symptoms of serotonin syndrome or neuroleptic malignant syndrome-like (NMS-like) reactions, do not use linezolid in patients with carcinoid syndrome or in patients receiving SSRIs, tricyclic antidepressants, serotonin 5-HT1 receptor agonists (triptans), meperidine, bupropion, or buspirone. (See Specific Drugs under Interactions.)
In cases when patient is already receiving a serotonergic antidepressant or buspirone and urgent treatment with linezolid is required (e.g., life-threatening infection caused by MRSA or vancomycin-resistant E. faecium) and alternatives to linezolid are not available and potential benefits of the drug outweigh risks of serotonin syndrome or NMS-like reactions, stop the serotonergic antidepressant promptly and administer linezolid. Monitor for manifestations of serotonin syndrome or NMS-like reactions (e.g., hyperthermia, rigidity, myoclonus, autonomic instability, mental status changes that include extreme agitation progressing to delirium and coma) for 2 weeks (5 weeks if fluoxetine was taken) or until 24 hours after last linezolid dose, whichever comes first. Also monitor for symptoms associated with discontinuance of the antidepressant.
Mortality
In an investigational study in seriously ill patients with intravascular catheter-related infections† [off-label], mortality was higher in patients receiving linezolid than in patients receiving a comparator anti-infective (vancomycin, oxacillin, dicloxacillin); patients also could receive concomitant therapy for gram-negative infection. There was no difference in mortality between linezolid and comparator regimens in patients with only gram-positive bacteria identified in the baseline culture; mortality was higher in linezolid-treated patients with gram-negative bacterial infections, mixed gram-positive and gram-negative infections, or no pathogen identified at baseline. Causality not established.
Not approved by FDA for treatment of catheter-related bacteremia or catheter-site infections; not approved for treatment of gram-negative bacterial infections.
Monoamine Oxidase Inhibition
Linezolid is a weak, nonselective, reversible inhibitor of MAO, and potentially may interact with MAO inhibitors and adrenergic and serotonergic agents. (See Specific Drugs under Interactions.)
Significant pressor response reported when tyramine doses >100 mg were used in adults receiving linezolid. Instruct patients to avoid large quantities of foods or beverages with high tyramine content during linezolid treatment. Foods high in tyramine content include those that may have undergone protein changes by aging, fermentation, pickling, or smoking to improve flavor (e.g., aged cheeses, fermented or air-dried meat, sauerkraut, soy sauce, tap beer, red wine). Consider that tyramine content of any protein-rich food may be increased if stored for long periods or improperly refrigerated.
Risk of Hypertension
Unless monitored for potential increases in BP, do not use linezolid in patients with uncontrolled hypertension, pheochromocytoma, or thyrotoxicosis or in patients receiving direct- or indirect-acting sympathomimetic agents (e.g., pseudoephedrine), vasopressor agents (e.g., epinephrine, norepinephrine), or dopaminergic agents (e.g., dopamine, dobutamine). (See Specific Drugs under Interactions.)
Lactic Acidosis
Lactic acidosis, characterized by recurrent nausea and vomiting, reported. Patients who develop recurrent nausea and vomiting, unexplained acidosis, or a low bicarbonate concentration while receiving linezolid should undergo immediate medical evaluation.
Seizures
Seizures reported; history of seizures or risk factors for seizures noted in some cases.
Hypoglycemia
Symptomatic hypoglycemia reported in patients with diabetes mellitus receiving linezolid concomitantly with insulin or oral hypoglycemic agents.
Although causal relationship between linezolid and hypoglycemia not established, caution patients with diabetes mellitus about potential for hypoglycemia during linezolid treatment.
If hypoglycemia occurs, dosage reduction of insulin or oral antidiabetic agents or discontinuance of linezolid, insulin, or oral antidiabetic agents may be necessary.
Sensitivity Reactions
Anaphylaxis, angioedema, and bullous skin disorders, including severe cutaneous adverse reactions (SCAR) such as toxic epidermal necrolysis and Stevens-Johnson syndrome, reported.
Tooth Discoloration
Superficial tooth discoloration and tongue discoloration reported. In cases with known outcome, tooth discoloration was removable with professional dental cleaning (manual descaling).
Phenylketonuria
Oral suspension contains aspartame, which is metabolized in the GI tract to provide 20 mg of phenylalanine per 5 mL of suspension.
Linezolid tablets do not contain aspartame and should be used in individuals with phenylketonuria (i.e., homozygous genetic deficiency of phenylalanine hydroxylase) and other individuals who must restrict their intake of phenylalanine.
Superinfection/Clostridioides difficile-associated Diarrhea and Colitis (CDAD)
Possible emergence and overgrowth of nonsusceptible organisms. Monitor carefully; institute appropriate therapy if superinfection occurs.
Treatment with anti-infectives alters normal colon flora and may permit overgrowth of Clostridioides difficile (formerly Clostridium difficile).
C. difficile infection (CDI) andC. difficile-associated diarrhea and colitis (CDAD; also known as antibiotic-associated diarrhea and colitis or pseudomembranous colitis) reported with nearly all anti-infectives, including linezolid, and may range in severity from mild diarrhea to fatal colitis. C. difficile produces toxins A and B which contribute to the development of CDAD; hypertoxin-producing strains of C. difficile are associated with increased morbidity and mortality since they may be refractory to anti-infectives and colectomy may be required.
Consider CDAD if diarrhea develops during or after therapy and manage accordingly. Obtain careful medical history since CDAD may occur as late as ≥2 months or longer after anti-infective therapy is discontinued.
If CDAD is suspected or confirmed, discontinue anti-infectives not directed against C. difficile whenever possible. Initiate appropriate anti-infective therapy directed against C. difficile (e.g., fidaxomicin, vancomycin, metronidazole), supportive therapy (e.g., fluid and electrolyte management, protein supplementation), and surgical evaluation as clinically indicated.
Selection and Use of Anti-infectives
Linezolid is indicated only for treatment of certain infections caused by certain gram-positive bacteria. The drug has no clinical activity against gram-negative bacteria and is not indicated for treatment of infections caused by gram-negative bacteria.
It is imperative that an anti-infective active against gram-negative bacteria be used concomitantly if documented or presumptive pathogens also include gram-negative bacteria. (See Uses.)
Safety and efficacy of linezolid given for >28 days not evaluated in controlled clinical trials. (See Dosage under Dosage and Administration.)
To reduce development of drug-resistant bacteria and maintain effectiveness of linezolid and other antibacterials, use only for treatment of infections proven or strongly suspected to be caused by susceptible bacteria.
When selecting or modifying anti-infective therapy, use results of culture and in vitro susceptibility testing. In the absence of such data, consider local epidemiology and susceptibility patterns when selecting anti-infectives for empiric therapy.
Information on test methods and quality control standards for in vitro susceptibility testing of antibacterials and specific interpretive criteria for such testing recognized by FDA is available at [Web]. For most antibacterials, including linezolid, FDA recognizes the standards published by the Clinical and Laboratory Standards Institute (CLSI).
Specific Populations
Pregnancy
Available data from published and postmarketing case reports regarding use of linezolid in pregnant women have not identified a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes
In mice, rats, and rabbits, linezolid was not teratogenic; however, embryofetal toxicities reported (e.g, post-implantational embryo death, decreased fetal body weights, increased incidence of costal cartilage fusion, reduced ossification).
Lactation
Distributed into human milk; not known whether the drug affects the breast-fed infant or affects milk production.
Consider benefits of breast-feeding and the importance of linezolid to the woman along with potential adverse effects on the breast-fed child from the drug or from the underlying maternal condition.
If used in a nursing woman, manufacturer recommends monitoring breast-fed infant for diarrhea and vomiting since these are the most common adverse reactions reported in infants being treated with linezolid.
Males of Reproductive Potential
Based on findings from animal studies, linezolid may reversibly impair fertility in males.
In adult male rats, reversible decrease in fertility and reproductive performance reported. The effects on fertility were mediated through altered spermatogenesis; affected spermatids contained abnormally formed and oriented mitochondria and were nonviable. Epithelial cell hypertrophy and hyperplasia in the epididymis observed in conjunction with decreased fertility.
Pediatric Use
Safety and efficacy for treatment of CAP, nosocomial pneumonia, complicated skin and skin structure infections, and vancomycin-resistant E. faecium infections in pediatric patients are supported by adequate and well-controlled studies in adults, pharmacokinetic studies in pediatric patients, and additional data from a comparator-controlled study of gram-positive infections in neonates and children through 11 years of age. Safety and efficacy for treatment of CAP in pediatric patients also is supported by evidence from an uncontrolled study in patients 8 months through 12 years of age.
Safety and efficacy for treatment of uncomplicated skin and skin structure infections in pediatric patients established in a comparator-controlled study in pediatric patients 5–17 years of age.
In children with a suboptimal response to linezolid, especially those with infections caused by pathogens with linezolid MICs of 4 mcg/mL, consider inadequate systemic exposure, site and severity of infection, and underlying medical conditions.
Manufacturer states not recommended for empiric treatment of CNS infections in pediatric patients. (See Distribution under Pharmacokinetics.)
Geriatric Use
Pharmacokinetic, safety, and efficacy profiles similar to those in younger adults. Possibility of greater sensitivity in some older individuals cannot be ruled out.
Hepatic Impairment
Mild or moderate hepatic impairment (Child-Pugh class A or B): Pharmacokinetics not altered.
Severe hepatic impairment: Pharmacokinetics not evaluated.
Renal Impairment
Although clinical importance not determined, the 2 principal metabolites of linezolid may accumulate in patients with impaired renal function; amount of accumulation increases with severity of renal impairment. Weigh potential benefits against potential risks of accumulation of linezolid metabolites. (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
GI effects (diarrhea, nausea, vomiting, localized or generalized abdominal pain, loose stools), headache, rash, dizziness, anemia, thrombocytopenia.
How should I use Linezolid (monograph)
Administration
Administer orally or by IV infusion.
When clinically appropriate, IV route may be switched to oral without dosage adjustment.
Avoid large quantities of foods or beverages with high tyramine content during linezolid treatment. (See Monoamine Oxidase Inhibition under Cautions.)
Oral Administration
Administer orally without regard to meals.
Reconstitution
Reconstitute powder for oral suspension at time of dispensing by adding amount of water specified on bottle to provide a suspension containing 100 mg/5 mL. After tapping bottle gently to loosen the powder, add water in 2 portions and agitate well after each addition.
Prior to administration of each dose, gently mix suspension by inverting bottle 3–5 times; do not shake.
IV Administration
For solution and drug compatibility information, see Compatibility under Stability.
Single-use containers of linezolid injection for IV infusion should be administered without further dilution. Do not use the containers in series connections; do not introduce additives into the solution.
Rate of Administration
Administer by IV infusion over 30–120 minutes.
Dosage
Manufacturer states safety and efficacy of >28 days of linezolid treatment not evaluated in controlled clinical trials. The drug is administered for longer durations when used in multiple-drug regimens for treatment of MDR tuberculosis.
Pediatric Patients
General Dosage for Neonates
Oral or IV
Neonates: Manufacturer recommends 10 mg/kg every 12 hours initially in premature neonates <7 days of age; may consider 10 mg/kg every 8 hours in those with inadequate response. Manufacturer recommends 10 mg/kg every 8 hours in all neonates ≥7 days of age.
Neonates ≤7 days of age: AAP recommends 10 mg/kg every 12 hours in those with gestational age <34 weeks and 10 mg/kg every 8 hours in those with gestational age ≥34 weeks.
Neonates 8–28 days of age: AAP recommends 10 mg/kg every 8 hours, regardless of gestational age.
Respiratory Tract Infections
Community-acquired or Nosocomial Pneumonia
Oral or IVChildren 7 days through 11 years of age: 10 mg/kg every 8 hours for 10–14 days.
Adolescents ≥12 years of age: 600 mg every 12 hours for 10–14 days.
Skin and Skin Structure Infections
Uncomplicated Skin and Skin Structure Infections
OralChildren 7 days through 4 years of age: 10 mg/kg every 8 hours for 10–14 days.
Children 5 through 11 years of age: 10 mg/kg every 12 hours for 10–14 days.
Adolescents ≥12 years of age: 600 mg every 12 hours for 10–14 days.
Complicated Skin and Skin Structure Infections
Oral or IVChildren 7 days through 11 years of age: 10 mg/kg every 8 hours for 10–14 days.
Adolescents ≥12 years of age: 600 mg every 12 hours for 10–14 days.
Vancomycin-resistant Enterococcus faecium Infections
Oral or IV
Children 7 days through 11 years of age: 10 mg/kg every 8 hours for 14–28 days.
Adolescents ≥12 years of age: 600 mg every 12 hours for 14–28 days.
Adults
Respiratory Tract Infections
Community-acquired or Nosocomial Pneumonia
Oral or IV600 mg every 12 hours for 10–14 days.
Skin and Skin Structure Infections
Uncomplicated Skin and Skin Structure Infections
Oral400 mg every 12 hours for 10–14 days.
Complicated Skin and Skin Structure Infections
Oral or IV600 mg every 12 hours for 10–14 days.
Vancomycin-resistant Enterococcus faecium Infections
Oral or IV
600 mg every 12 hours for 14–28 days.
Active Tuberculosis
XDR or Treatment-intolerant or Non-responsive MDR Pulmonary Tuberculosis
Oral1.2 g daily for 26 week. Adjustment of dosage to 600 mg daily with further reductions to 300 mg daily or interruption of linezolid therapy may be required if myelosuppression, peripheral neuropathy, or optic neuropathy occurs.
Must administer in conjunction with oral pretomanid (200 mg once daily for 26 weeks) and bedaquiline (400 mg once daily for 2 weeks followed by 200 mg 3 times weekly [with at least 48 hours between doses] for 24 weeks).
The 3-drug combination regimen should be continued for 26 weeks, but may be extended beyond 26 weeks if necessary.
Special Populations
Hepatic Impairment
Mild to moderate hepatic impairment (Child-Pugh class A or B): Dosage adjustments not needed.
Severe hepatic impairment: Pharmacokinetics not evaluated.
Renal Impairment
Dosage adjustments not needed. Consider that linezolid metabolites may accumulate in patients with renal impairment; clinical importance unknown. (See Renal Impairment under Cautions.)
Hemodialysis patients: Administer linezolid doses after dialysis session.
Geriatric Patients
Dosage adjustments not needed.
What other drugs will affect Linezolid (monograph)?
Minimally metabolized; possibly by CYP isoenzymes.
Does not inhibit CYP1A2, 2C9, 2C19, 2D6, 2E1, or 3A4. Does not induce CYP isoenzymes.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Potent inducers of hepatic enzymes: Possible reduced linezolid concentrations.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Aminoglycosides |
Gentamicin: No effect on pharmacokinetics of linezolid or gentamicin Gentamicin or streptomycin: In vitro evidence of additive or indifferent antibacterial effects |
|
|
Ampicillin |
In vitro evidence of additive or indifferent antibacterial effects |
|
|
Antidiabetic agents, oral |
Potential for hypoglycemia |
Dosage reduction of antidiabetic agent or discontinuance of linezolid or antidiabetic agent may be necessary |
|
Aztreonam |
No effect on pharmacokinetics of either drug In vitro evidence of additive or indifferent antibacterial effects |
|
|
Carbamazepine |
Possible decreased linezolid concentrations |
|
|
Carbapenems |
Imipenem: In vitro evidence of additive or indifferent antibacterial effects |
|
|
Insulin |
Potential for hypoglycemia |
Dosage reduction of insulin or discontinuance of linezolid or insulin may be necessary |
|
MAO inhibitors (isocarboxazid, phenelzine, selegiline, tranylcypromine) |
Potential pharmacologic interaction Increased risk of CNS toxicity, including serotonin syndrome |
Do not use linezolid in patients who are receiving (or have received within the last 2 weeks) an MAO inhibitor (see Serotonergic Drugs under Specific Drugs) |
|
Phenobarbital |
Possible decreased linezolid concentrations |
|
|
Phenytoin |
Effect on phenytoin pharmacokinetics unlikely; possible decreased linezolid concentrations |
Dosage adjustments not needed |
|
Rifampin |
Decreased peak plasma concentration and AUC of linezolid In vitro evidence of additive or indifferent antibacterial effects |
Mechanism of the interaction and clinical importance unknown |
|
Serotonergic drugs (SSRIs, SNRIs, tricyclic antidepressants, amoxapine, bupropion, buspirone, maprotiline, meperidine, mirtazapine, nefazodone, trazodone, vilazodone) |
Increased risk of serotonin syndrome, particularly with SSRIs and SNRIs; unclear whether risk associated with other serotonergic drugs is comparable to that reported with SSRIs and SNRIs |
Do not use concurrently unless considered clinically appropriate and patient can be carefully monitored for manifestations of serotonin syndrome or NMS-like reactions If urgent linezolid treatment necessary (e.g., life-threatening infections caused by MRSA or vancomycin-resistant E. faecium), promptly discontinue the serotonergic antidepressant and administer linezolid with close monitoring (see Serotonin Syndrome under Cautions) Serotonergic drug may be initiated or resumed 24 hours after last linezolid dose |
|
Sympathomimetic agents |
Reversible enhancement of pressor response may occur if linezolid used concomitantly with indirect-acting sympathomimetic agents (e.g., phenylpropanolamine, pseudoephedrine), vasopressor agents (e.g., epinephrine, norepinephrine), or dopaminergic agents (e.g., dopamine, dobutamine) |
Do not use concomitantly unless patient monitored for potential BP increases If adrenergic agent (e.g., dopamine, epinephrine) initiated in patient receiving linezolid, use lower initial doses of the adrenergic agent and titrate dosage to achieve desired response |
|
Vancomycin |
In vitro evidence of additive or indifferent antibacterial effects |
|
|
Vitamins (ascorbic acid, vitamin E) |
Ascorbic acid or vitamin E: Concomitant use slightly increases linezolid AUC |
Ascorbic acid or vitamin E: Dosage adjustments not needed |
|
Warfarin |
No substantial effect on warfarin pharmacokinetics |
Dosage adjustments not needed |