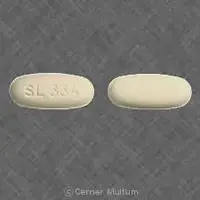
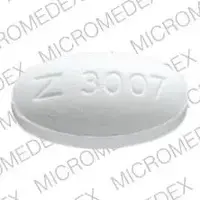
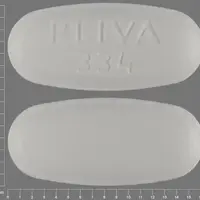
Generic name: metronidazole (oral/injection)
Drug class: Amebicides, Miscellaneous antibiotics
Availability: Prescription only
Pregnancy & Lactation: Risk data available
Brand names: Flagyl, Metronidazole (systemic) (monograph), Likmez
What is Metronidazole?
Metronidazole is an antibiotic that is used to treat bacterial infections of the vagina, stomach, liver, skin, joints, brain and spinal cord, lungs, heart, or bloodstream.
Metronidazole is also used to treat trichomoniasis, a sexually transmitted disease caused by a parasite. Usually both sexual partners are treated at the same time, even if one has no symptoms.
Do not use metronidazole to treat any condition that has not been checked by your doctor.
Warnings
You should not use metronidazole if you recently drank alcohol, or have taken disulfiram (Antabuse) within the past 2 weeks.
Do not drink alcohol or consume foods or medicines that contain propylene glycol while you are taking metronidazole and for at least 3 days after you stop taking it.
Seizures and other nervous system abnormalities have been reported in patients treated with metronidazole. You should stop using this medicine immediately if you experience any neurological symptoms such as seizures, headaches, visual changes, weakness, numbness, or tingling.
This medicine will not treat a viral infection such as the common cold or flu.
In animal studies (mice and rats), this medicine caused certain types of cancers or tumors. It is not known whether these effects would occur in people using this medicine. Ask your doctor about your risk
Before taking this medicine
You should not use this medicine if you are allergic to metronidazole, secnidazole, or tinidazole, or if:
-
you drank alcohol in the past 3 days;
-
you consumed foods or medicines that contain propylene glycol in the past 3 days; or
-
you took disulfiram (Antabuse) within the past 14 days.
May harm an unborn baby. Do not use metronidazole to treat trichomoniasis during the first trimester of pregnancy. Tell your doctor if you become pregnant.
Not all uses of metronidazole are approved for treating children and teenagers. Metronidazole is not approved to treat vaginal infections in girls who have not begun having menstrual periods.
To make sure you can safely take this medicine, tell your doctor if you have ever had:
-
liver disease;
-
kidney disease (or if you are on dialysis);
-
a heart rhythm disorder;
-
a stomach or intestinal disease such as Crohn's disease;
-
a blood cell disorder such as anemia (lack of red blood cells) or low white blood cell (WBC) counts;
-
a fungal infection anywhere in your body; or
-
a nerve disorder.
Metronidazole has caused cancer in animal studies. However, it is not known whether this would occur in humans. Ask your doctor about your risk.
You should not breastfeed within 24 hours after using metronidazole. If you use a breast pump during this time, throw out the milk and do not feed it to your baby.
How should I take Metronidazole
Metronidazole comes as a tablet, an extended-release tablet, and as a capsule to take by mouth. Metronidazole capsules and tablets are usually taken as a one-time dose (or divided into two doses on 1 day) or two to four times daily for up to 10 days or longer. Metronidazole extended-release tablets are usually taken once daily at least 1 hour before or 2 hours after a meal for 7 days. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take metronidazole exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Swallow the extended-release tablets whole; do not split, chew, or crush them.
Continue to take this medication even if you feel well. Do not stop taking it without talking to your doctor. If you stop taking this medication too soon or skip doses, your infection may not be completely treated and the bacteria may become resistant to antibiotics.
Dosing information
Take metronidazole exactly as prescribed by your doctor. Follow all directions on your prescription label and read all medication guides or instruction sheets.
Metronidazole oral is taken by mouth. The injection is given as an infusion into a vein. A healthcare provider will give you the injection if you are unable to take the medicine by mouth.
Shake the oral suspension (liquid). Measure a dose with the supplied measuring device (not a kitchen spoon).
Swallow the extended-release tablet whole and do not crush, chew, or break it.
If you are treating a vaginal infection, your sexual partner may also need to take metronidazole so you don't become reinfected.
Metronidazole is usually given for up to 10 days in a row. You may need to repeat this dosage several weeks later.
Keep using this medicine even if your symptoms quickly improve. Skipping doses could make your infection resistant to medication. This medicine will not treat a viral infection (flu or a common cold).
Metronidazole will not treat a vaginal yeast infection. You may even develop a new vaginal yeast infection, which may need to be treated with antifungal medication. Tell your doctor if you have symptoms such as itching or discharge during or after treatment with this medicine.
Do not share this medicine with another person, even if they have the same symptoms you have.
This medicine can affect the results of certain medical tests. Tell any doctor who treats you that you are using this medicine.
Store at room temperature away from moisture and heat.
Before Taking
You should not use this medicine if you are allergic to metronidazole, secnidazole, or tinidazole, or if:
-
you drank alcohol in the past 3 days;
-
you consumed foods or medicines that contain propylene glycol in the past 3 days; or
-
you took disulfiram (Antabuse) within the past 14 days.
May harm an unborn baby. Do not use metronidazole to treat trichomoniasis during the first trimester of pregnancy. Tell your doctor if you become pregnant.
Not all uses of metronidazole are approved for treating children and teenagers. Metronidazole is not approved to treat vaginal infections in girls who have not begun having menstrual periods.
To make sure you can safely take this medicine, tell your doctor if you have ever had:
-
liver disease;
-
kidney disease (or if you are on dialysis);
-
a heart rhythm disorder;
-
a stomach or intestinal disease such as Crohn's disease;
-
a blood cell disorder such as anemia (lack of red blood cells) or low white blood cell (WBC) counts;
-
a fungal infection anywhere in your body; or
-
a nerve disorder.
Metronidazole has caused cancer in animal studies. However, it is not known whether this would occur in humans. Ask your doctor about your risk.
You should not breastfeed within 24 hours after using metronidazole. If you use a breast pump during this time, throw out the milk and do not feed it to your baby.
Related/similar drugs
prednisone, omeprazole, amoxicillin, doxycycline, pantoprazole, ciprofloxacin, cephalexinWhat happens if I miss a dose?
Take the medicine as soon as you can, but skip the missed dose if it is almost time for your next dose. Do not take two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
Overdose symptoms may include nausea, vomiting, numbness, tingling, or problems with balance or muscle movement.
What should I know about storage and disposal of this medication?
Keep this medication in the container it came in, tightly closed, and out of reach of children. Store it at room temperature and away from light, excess heat and moisture (not in the bathroom).
It is important to keep all medication out of sight and reach of children as many containers (such as weekly pill minders and those for eye drops, creams, patches, and inhalers) are not child-resistant and young children can open them easily. To protect young children from poisoning, always lock safety caps and immediately place the medication in a safe location – one that is up and away and out of their sight and reach. http://www.upandaway.org
Unneeded medications should be disposed of in special ways to ensure that pets, children, and other people cannot consume them. However, you should not flush this medication down the toilet. Instead, the best way to dispose of your medication is through a medicine take-back program. Talk to your pharmacist or contact your local garbage/recycling department to learn about take-back programs in your community. See the FDA's Safe Disposal of Medicines website (http://goo.gl/c4Rm4p) for more information if you do not have access to a take-back program.
What should I avoid while using Metronidazole?
While taking metronidazole and for 3 days after your last dose: Do not drink alcohol or consume foods, medicines, or other products that contain alcohol or propylene glycol. You may have unpleasant effects such as headaches, nausea, vomiting, stomach cramps, and warmth or tingling under your skin.
Metronidazole side effects
Get emergency medical help if you have signs of an allergic reaction to metronidazole (hives, itching, warmth or tingling; fever, joint pain; dry mouth, dry vagina; stuffy nose, difficult breathing, swelling in your face or throat) or a severe skin reaction (fever, sore throat, burning eyes, skin pain, red or purple skin rash with blistering and peeling).
Call your doctor at once if you have:
-
new or worsening symptoms of infection;
-
painful or difficult urination;
-
confusion;
-
a light-headed feeling (like you might pass out);
-
vaginal itching or discharge; or
-
blisters or ulcers in your mouth, red or swollen gums, trouble swallowing.
Stop taking the medicine and call your doctor right away if you have neurologic side effects (more likely to occur while taking metronidazole long term):
-
numbness, tingling, or burning pain in your hands or feet;
-
vision problems, pain behind your eyes, seeing flashes of light;
-
muscle weakness, problems with speech or coordination;
-
trouble speaking or understanding what is said to you;
-
a seizure; or
-
fever, neck stiffness, and increased sensitivity to light.
Metronidazole can cause life-threatening liver problems in people with Cockayne syndrome. If you have this condition, stop taking this medicine and contact your doctor if you have signs of liver failure--nausea, stomach pain (upper right side), dark urine, clay-colored stools, or jaundice (yellowing of the skin or eyes).
Side effects may be more likely in older adults.
Common metronidazole side effects may include:
-
depression, trouble sleeping, feeling irritable;
-
headache, dizziness, weakness;
-
nausea, vomiting, loss of appetite, stomach pain;
-
diarrhea, constipation;
-
unpleasant metallic taste;
-
rash, itching;
-
vaginal itching or discharge, pain during sex;
-
mouth sores; or
-
swollen, red, or "hairy" tongue.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
See more: Metronidazole Side EffectsWhat other drugs will affect Metronidazole?
Sometimes it is not safe to use certain medicines at the same time. Some drugs can affect your blood levels of other drugs you use, which may increase side effects or make the medicines less effective.
Tell your doctor about all your current medicines. Many drugs can affect metronidazole, especially:
-
an antidepressant;
-
asthma medication;
-
busulfan or other cancer medicine;
-
heart or blood pressure medication;
-
lithium or other antipsychotic medicine;
-
medicine to treat malaria, HIV, or other infection; or
-
a blood thinner - warfarin, Coumadin, Jantoven.
This list is not complete and many other drugs may interact with metronidazole. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
What other information should I know?
Keep all appointments with your doctor and the laboratory. Your doctor will order certain lab tests to check your response to metronidazole.
Before having any laboratory test, tell your doctor and the laboratory personnel that you are taking metronidazole.
Do not let anyone else take your medication. Your prescription is probably not refillable. If you still have symptoms of infection after you finish the metronidazole, call your doctor.
It is important for you to keep a written list of all of the prescription and nonprescription (over-the-counter) medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.
What to Expect
You should feel better after using metronidazole for a few days, but this will depend on the type of infection you have.
Let your doctor know if you don’t improve two to three days after you finish your treatment or if you feel worse while taking this medicine.
Additional Dosage Information
Your dosage will depend on the type of infection you have, the formulation of metronidazole you use, and other factors.
Be sure to finish taking all the medicine your doctor prescribes, even if you feel better. If you stop this medicine too soon your infection may not be treated completely.
Secondary Uses
Metronidazole may be used to treat other types of infections that aren’t listed in this guide.