Drug Detail:Adbry (Tralokinumab-ldrm)
Drug Class: Interleukin inhibitors
Highlights of Prescribing Information
ADBRY® (tralokinumab-ldrm) injection, for subcutaneous use
Initial U.S. Approval: 2021
Indications and Usage for Adbry
ADBRY is an interleukin-13 antagonist indicated for the treatment of moderate-to-severe atopic dermatitis in adult patients whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable. ADBRY can be used with or without topical corticosteroids. (1)
Adbry Dosage and Administration
- Prior to ADBRY initiation, complete all age appropriate vaccinations as recommended by current immunization guidelines (2.1)
- The recommended dosage of ADBRY is an initial dose of 600 mg (four 150 mg injections), followed by 300 mg (two 150 mg injections) administered every other week. A dosage of 300 mg every 4 weeks may be considered for patients below 100 kg who achieve clear or almost clear skin after 16 weeks of treatment. (2.2)
- Administer by subcutaneous injection. (2.2)
Dosage Forms and Strengths
Injection: 150 mg/mL solution in a single-dose prefilled syringe with needle guard. (3)
Contraindications
Known hypersensitivity to tralokinumab-ldrm or any excipients in ADBRY. (4)
Warnings and Precautions
- Hypersensitivity: Hypersensitivity reactions, including anaphylaxis, and angioedema have occurred after administration of ADBRY. Discontinue ADBRY in the event of a hypersensitivity reaction. (5.1)
- Conjunctivitis and Keratitis: Patients should report new onset or worsening eye symptoms to their healthcare provider. (5.2)
- Parasitic (Helminth) Infections: Treat patients with pre-existing helminth infections before initiating treatment with ADBRY. If patients become infected while receiving ADBRY and do not respond to anti-helminth treatment, discontinue treatment with ADBRY until the infection resolves. (5.3)
- Risk of Infection with Live Vaccines: Avoid use of live vaccines. (5.4)
Adverse Reactions/Side Effects
Most common adverse reactions (incidence ≥ 1%) are upper respiratory tract infections, conjunctivitis, injection site reactions, and eosinophilia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact LEO Pharma Inc. at 1-877-494-4536 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 3/2023
Full Prescribing Information
1. Indications and Usage for Adbry
ADBRY is indicated for the treatment of moderate-to-severe atopic dermatitis in adult patients whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable. ADBRY can be used with or without topical corticosteroids.
2. Adbry Dosage and Administration
2.1 Vaccination Prior to Treatment
Complete all age-appropriate vaccinations as recommended by current immunization guidelines prior to initiating treatment with ADBRY [see Warnings and Precautions (5.4)].
2.2 Recommended Dosage
The recommended dosage of ADBRY is:
- An initial dose of 600 mg (four 150 mg injections), followed by 300 mg (two 150 mg injections) administered every other week.
- After 16 weeks of treatment, for patients with body weight below 100 kg who achieve clear or almost clear skin, a dosage of 300 mg every 4 weeks may be considered.
ADBRY is administered by subcutaneous injection [see Dosage and Administration (2.5, 2.6)].
2.3 Concomitant Topical Therapies
ADBRY can be used with or without topical corticosteroids. Topical calcineurin inhibitors may be used, but should be reserved for problem areas only, such as the face, neck, intertriginous and genital areas.
2.4 Missed Doses
If a dose is missed, administer the dose as soon as possible. Thereafter, resume dosing at the regular scheduled time.
2.5 Preparation for Use
- Before injection, remove ADBRY prefilled syringes from the refrigerator and allow to reach room temperature (30 minutes for the 150 mg/mL prefilled syringes) without removing the needle cap.
- After removal from the refrigerator, prefilled syringes may be kept at room temperature up to 30°C (86°F) and must be used within 14 days or discarded.
- Inspect ADBRY visually for particulate matter and discoloration prior to administration. ADBRY injection is a clear to opalescent, colorless to pale yellow solution. Do not use if the liquid contains visible particulate matter, is discolored or cloudy (other than clear to opalescent, colorless to pale yellow).
- ADBRY does not contain preservatives; therefore, discard any unused product.
2.6 Important Administration Instructions
- ADBRY is intended for use under the guidance of a healthcare provider. A patient may self-inject ADBRY after training in subcutaneous injection technique. Provide proper training to patients and/or caregivers on the preparation and administration according to the "Instructions for Use" [see Instructions for Use].
- For the initial 600 mg dose, administer each of the four ADBRY 150 mg injections at different injection sites within the same body area.
- For the subsequent 300 mg doses, administer the two ADBRY 150 mg injections at different injection sites within the same body area.
- Administer subcutaneous injection into the thigh or abdomen, except for the 2 inches (5 cm) around the navel. The upper arm can also be used if a caregiver administers the injection.
- Rotate the body area with each subsequent set of injections. DO NOT inject ADBRY into skin that is tender, damaged, bruised, or scarred.
3. Dosage Forms and Strengths
Injection: 150 mg/mL clear to opalescent, colorless to pale yellow solution in a single-dose prefilled syringe with needle guard
4. Contraindications
ADBRY is contraindicated in patients who have known hypersensitivity to tralokinumab-ldrm or any excipients in ADBRY [see Warnings and Precautions (5.1)].
5. Warnings and Precautions
5.1 Hypersensitivity
Hypersensitivity reactions including anaphylaxis and angioedema, have been reported with use of ADBRY.
If a serious hypersensitivity reaction occurs, discontinue ADBRY immediately and initiate appropriate therapy.
5.2 Conjunctivitis and Keratitis
Conjunctivitis and keratitis occurred more frequently in atopic dermatitis subjects who received ADBRY. Conjunctivitis was the most frequently reported eye disorder. Most subjects with conjunctivitis or keratitis recovered or were recovering during the treatment period [see Adverse Reactions (6.1)].
Advise patients to report new onset or worsening eye symptoms to their healthcare provider.
5.3 Parasitic (Helminth) Infections
Patients with known helminth infections were excluded from participation in clinical studies. It is unknown if ADBRY will influence the immune response against helminth infections by inhibiting IL-13 signaling.
Treat patients with pre-existing helminth infections before initiating treatment with ADBRY. If patients become infected while receiving ADBRY and do not respond to antihelminth treatment, discontinue treatment with ADBRY until the infection resolves.
5.4 Risk of Infection with Live Vaccines
ADBRY may alter a patient's immunity and increase the risk of infection following administration of live vaccines. Prior to initiating therapy with ADBRY, complete all age appropriate vaccinations according to current immunization guidelines. Avoid use of live vaccines in patients treated with ADBRY. Limited data are available regarding coadministration of ADBRY with non-live vaccines [see Clinical Pharmacology (12.2)].
6. Adverse Reactions/Side Effects
The following adverse reactions are discussed in greater detail elsewhere in the labeling:
- Hypersensitivity [see Warnings and Precautions (5.1)]
- Conjunctivitis and Keratitis [see Warnings and Precautions (5.2)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of ADBRY was evaluated in a pool of 5 randomized, double-blind, placebo-controlled trials in subjects with moderate-to-severe atopic dermatitis including three phase 3 Eczema Tralokinumab trials (ECZTRA 1, ECZTRA 2, and ECZTRA 3), a dose-finding trial, and a vaccine response trial. The safety population had a mean age of 37 years; 43% of subjects were female, 67% were White, 21% were Asian, and 9% were Black. In terms of co-morbid conditions, 39% of the subjects had asthma, 49% had hay fever, 36% had food allergy, and 21% had allergic conjunctivitis at baseline.
In these 5 atopic dermatitis trials, 1964 subjects were treated with subcutaneous injections of ADBRY, with or without concomitant topical corticosteroids (TCS). A total of 807 subjects were treated with ADBRY for at least 1 year.
ECZTRA 1 and ECZTRA 2 compared the safety of ADBRY monotherapy to placebo through Week 52. ECZTRA 3 compared the safety of ADBRY + TCS to placebo + TCS through Week 32.
6.2 Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity with ADBRY. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors, including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies in the studies described below with the incidence of antibodies in other studies or to other tralokinumab products may be misleading.
In ECZTRA 1, ECZTRA 2, and ECZTRA 3, and the vaccine-response trial, the incidence of Anti-Drug-Antibodies (ADA) during the initial 16-week treatment period was 1.4% for subjects treated with ADBRY 300 mg every other week and in 1.3% for subjects treated with placebo; neutralizing antibodies were seen in 0.1% of subjects treated with ADBRY and 0.2% of subjects treated with placebo.
Across all trial periods, the ADA incidence for subjects who received ADBRY was 4.6%; 0.9% had persistent ADA and 1.0% had neutralizing antibodies.
No clinically meaningful differences in the pharmacokinetics, safety, or efficacy of tralokinumab-ldrm were observed in patients who tested positive for anti-tralokinumab-ldrm antibody (including neutralizing antibodies).
8. Use In Specific Populations
8.4 Pediatric Use
The safety and effectiveness of ADBRY have not been established in pediatric patients.
8.5 Geriatric Use
Of the 1605 subjects exposed to ADBRY in 5 atopic dermatitis trials in the initial treatment period of up to 16 weeks, 77 subjects were 65 years or older. Clinical studies did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects [see Clinical Pharmacology (12.3)].
10. Overdosage
There is no specific treatment for ADBRY overdose. In the event of overdosage, contact Poison Control (1-800-222-1222) for latest recommendations and monitor the patient for any signs or symptoms of adverse reactions and institute appropriate symptomatic treatment immediately.
11. Adbry Description
Tralokinumab-ldrm, an interleukin-13 antagonist, is a human IgG4 monoclonal antibody. Tralokinumab-ldrm is produced in mouse myeloma cells by recombinant DNA technology, consists of 1326 amino acids, and has a molecular weight of approximately 147 kilodaltons.
ADBRY (tralokinumab-ldrm) injection is a sterile, preservative-free, clear to opalescent, colorless to pale yellow solution for subcutaneous use supplied as a single-dose prefilled syringe with needle guard in a siliconized Type-1 clear glass syringe. None of the components of the prefilled syringe or the needle guard are made with natural rubber latex.
Each prefilled syringe delivers 150 mg tralokinumab-ldrm in 1 mL and the inactive ingredients: acetic acid (0.3 mg), polysorbate 80 (0.1 mg), sodium acetate trihydrate (6 mg), sodium chloride (5 mg), and Water for Injection, at an approximate pH of 5.5.
12. Adbry - Clinical Pharmacology
12.1 Mechanism of Action
Tralokinumab-ldrm is a human IgG4 monoclonal antibody that specifically binds to human interleukin-13 (IL-13) and inhibits its interaction with the IL-13 receptor α1 and α2 subunits (IL-13Rα1 and IL-13Rα2). IL-13 is a naturally occurring cytokine of the Type 2 immune response. Tralokinumab-ldrm inhibits the bioactivity of IL-13 by blocking IL-13 interaction with IL-13Rα1/IL-4Rα receptor complex. Tralokinumab-ldrm inhibits IL-13-induced responses including the release of proinflammatory cytokines, chemokines and IgE.
12.2 Pharmacodynamics
ADBRY was associated with decreased concentrations of Th2 and Th22 immunity biomarkers in the blood, such as thymus and activation-regulated chemokine (TARC/CCL17), periostin, IL-22, lactate dehydrogenase (LDH) and serum IgE. ADBRY decreased expression of keratin 16 and Ki-67 in AD skin, and upregulated protein expression of loricrin. ADBRY suppressed expression of genes in the Th2 pathway, including CCL17, CCL18 and CCL26 as well as markers of Th17- and Th22-regulated genes in lesional skin. The clinical relevance of these biomarkers is not fully understood.
12.3 Pharmacokinetics
The mean (SD) steady-state trough concentration of tralokinumab-ldrm ranged from 98.0 (41.1) mcg/mL to 101.4 (42.7) mcg/mL following administration of ADBRY at 300 mg every other week. Tralokinumab-ldrm exposure increased proportionally over a dosage range up to 2100 mg for a 70 kg subject (30 mg/kg IV) (3.5 times the maximum approved recommended dosage). Steady-state tralokinumab-ldrm concentrations were achieved by week 16 following a 600 mg starting dose and 300 mg every other week.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Animal studies have not been conducted to evaluate the carcinogenic or mutagenic potential for tralokinumab-ldrm.
No effects on fertility parameters such as reproductive organs, menstrual cycle and sperm analysis were observed in male or female sexually mature cynomolgus monkeys that were subcutaneously administered tralokinumab-ldrm at doses up to 350 mg/animal (10 times the MRHD on a mg/kg basis of 10 mg/kg/week) in females once a week for three consecutive menstrual cycles (maximum of 15 doses) or 600 mg/animal (10 times the MRHD on a mg/kg basis of 10 mg/kg/week) in males once a week for 13 weeks. The monkeys were not mated to evaluate fertility.
14. Clinical Studies
The efficacy of ADBRY was assessed in three randomized, double-blind, placebo-controlled trials [ECZTRA 1 (NCT03131648), ECZTRA 2 (NCT03160885), and ECZTRA 3 (NCT03363854)]. Efficacy was assessed in a total of 1934 subjects 18 years of age and older with moderate-to-severe atopic dermatitis (AD) not adequately controlled by topical medication(s). Disease severity was defined by an Investigator's Global Assessment (IGA) score ≥ 3 in the overall assessment of AD lesions on a severity scale of 0 to 4, an Eczema Area and Severity Index (EASI) score ≥16 on a scale of 0 to 72, and a minimum body surface area (BSA) involvement of ≥10%. At baseline, 58% of subjects were male, 69% of subjects were White, 50% of subjects had a baseline IGA score of 3 (moderate AD), and 50% of subjects had a baseline IGA score of 4 (severe AD). The baseline mean EASI score was 32 and the baseline weekly averaged Worst Daily Pruritus Numeric Rating Scale (NRS) was 8 on a scale of 0-10.
In all three trials, subjects received subcutaneous injections of ADBRY 600 mg or placebo on Day 0, followed by 300 mg every other week or placebo for 16 weeks. Responders were defined as achieving an IGA 0 or 1 ("clear" or "almost clear") or EASI-75 (improvement of at least 75% in EASI score from baseline) at Week 16.
To evaluate maintenance of response in the monotherapy trials (ECZTRA 1 and ECZTRA 2), subjects responding to initial treatment with ADBRY 300 mg every other week were re-randomized to ADBRY 300 mg every other week, ADBRY 300 mg every 4 weeks or placebo every other week for another 36 weeks following first dose administration. Subjects randomized to placebo in the initial treatment period who achieved a clinical response at Week 16 continued to receive placebo every other week for another 36 weeks. Non-responders at Week 16, and subjects who lost clinical response during the maintenance period were placed on open-label treatment with ADBRY 300 mg every other week and optional use of TCS.
In the combination therapy trial (ECZTRA 3), subjects received either ADBRY 300 mg every other week with TCS or placebo with TCS and as needed topical calcineurin inhibitors (TCI) until Week 16. Subjects in the ADBRY 300 mg with TCS group who achieved clinical response at Week 16 were re-randomized to ADBRY 300 mg every other week with TCS or ADBRY every 4 weeks with TCS for another 16 weeks following first dose administration. Subjects in the placebo with TCS group who achieved clinical response at Week 16 continued on placebo with TCS for another 16 weeks. Subjects who did not achieve clinical response at Week 16 received ADBRY 300 mg every other week for another 16 weeks. A mid-potency TCS (i.e., mometasone furoate 0.1% cream) was dispensed at each dosing visit. Subjects were instructed to apply a thin film of the dispensed TCS as needed once daily to active lesions from Week 0 to Week 32 and were to discontinue treatment with TCS when control was achieved. An additional, lower potency TCS or TCI could be used at the investigator's discretion on areas of the body where use of the supplied TCS was not advisable, such as areas of thin skin.
All three trials assessed the primary endpoints of the proportion of subjects with an IGA 0 or 1 at Week 16 and the proportion of subjects with EASI-75 at Week 16. Secondary endpoints included the reduction of Worst Daily Pruritus NRS (weekly average) of at least 4 points on the 11-point itch NRS from baseline to Week 16.
17. Patient Counseling Information
Advise the patients to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
INSTRUCTIONS FOR USE
ADBRY® [ad'-bree]
(tralokinumab-ldrm)
injection, for subcutaneous use
This Instructions for Use contains information on how to inject ADBRY.
Read this Instructions for Use before you start using ADBRY prefilled syringes and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment.
Keep this Instructions for Use and refer to it as needed.
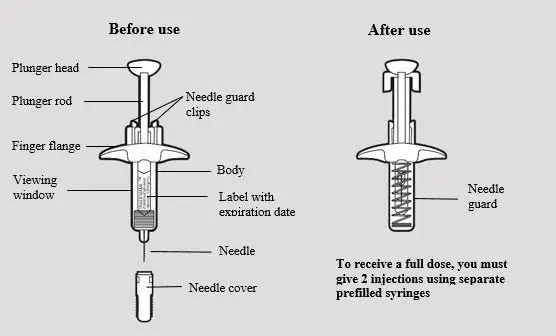
Each single-dose prefilled syringe contains 150 mg of ADBRY. The ADBRY prefilled syringes are for single-dose only.
Important Information You Need to Know Before Injecting ADBRY:
- Your healthcare provider should show you how to prepare and inject ADBRY using the prefilled syringes before you inject ADBRY for the first time.
- Do not inject yourself or someone else until you have been shown how to inject ADBRY the right way.
- Talk to your healthcare provider if you have any questions about how to inject ADBRY the right way.
-
To receive your full prescribed dose, you will need to give more than 1 ADBRY injection.
- To get your full prescribed initial dose of 600 mg, you will need to give 4 injections at different injection sites within the same body area.
- To get your full prescribed dose of 300 mg, you will need to give 2 injections at different injection sites within the same body area.
- It is recommended to rotate the body area with the next set of injections.
- The ADBRY prefilled syringes have a needle guard that will be activated to cover the needle after the injection is finished.
- For subcutaneous injection only (inject directly into fatty layer under the skin).
- Do not remove the needle cover until just before you give the injection.
- Do not share or reuse your ADBRY prefilled syringes.
- Do not inject through clothes.
ADBRY prefilled syringe parts (see Figure A):
Storing ADBRY
- Store ADBRY prefilled syringes in a refrigerator between 36°F to 46°F (2°C to 8°C).
- Store ADBRY prefilled syringes in the original carton and protect from light until you are ready to use them.
- ADBRY can be stored in the original carton at room temperature up to 86°F (30°C) for up to 14 days. Throw away (dispose of) syringes if left out of the refrigerator for more than 14 days.
- Do not freeze ADBRY prefilled syringes. Do not use if they have been frozen.
- Do not shake the ADBRY prefilled syringe.
- Do not heat the ADBRY prefilled syringe.
- Do not put the ADBRY prefilled syringe into direct sunlight.
- Keep ADBRY prefilled syringes and all medicines out of the reach of children.
Step 1: Setting up ADBRY injection
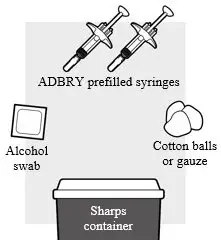
1a: Gather the supplies needed for your injection. For each ADBRY dose you will need (see Figure B):
- A clean flat, well-lit work surface, like a table
- 1 ADBRY carton that contains 2 ADBRY prefilled syringes
- An alcohol swab (not included in the carton)
- Clean gauze pads or cotton balls (not included in the carton)
- A puncture-resistant sharps disposal container (not included in the carton)
See Step 5 "Disposing of ADBRY" at the end of this Instructions for Use.
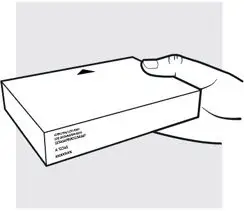
1b: Take the ADBRY prefilled syringe carton out of the refrigerator
- Check the expiration date (EXP) on the carton (see Figure C). Do not use if the expiration date on the carton has passed.
- Check to make sure the seal on the ADBRY carton is intact. Do not use the ADBRY prefilled syringes if the seal on the carton is broken.

1c: Let the ADBRY prefilled syringes warm up to room temperature (see Figure D)
Set the ADBRY carton on the flat surface and wait 30 minutes before you inject ADBRY to let the prefilled syringes warm up to room temperature 68°F to 86°F (20°C to 30°C). This will help to reduce discomfort and make it easier to inject ADBRY.
- Do not microwave the prefilled syringes, run hot water over them, or leave them in direct sunlight.
- Do not shake the syringes.
- Do not remove the needle cover on the prefilled syringes until you have reached Step 3 and are ready to inject.
- Do not put the syringes back in the refrigerator once they have reached room temperature.
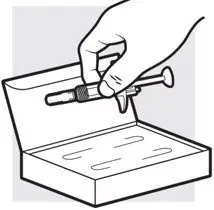
1d: Remove the ADBRY prefilled syringes from the carton
- Remove the 2 ADBRY prefilled syringes one by one from the carton by grasping the body (not the plunger rod) of the ADBRY prefilled syringes (see Figure E).
- Do not touch the needle guard clips to keep from activating the safety device (needle guard) too soon.
- Do not remove the needle cover on the prefilled syringes until you have reached Step 3 and are ready to inject.
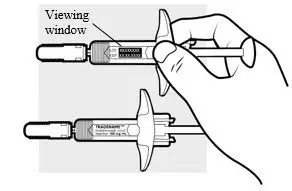
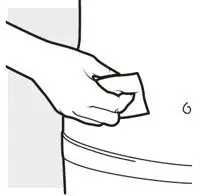
1e: Inspect the 2 ADBRY prefilled syringes (see Figure F)
- Make sure the ADBRY appears on the labels.
- Check the expiration date printed on the syringes.
- Check the medicine through the viewing windows. The medicine inside should be clear to slightly pearly and colorless to pale yellow.
- Do not use the ADBRY prefilled syringes, throw away and get new ones if:
- the expiration date printed on the syringes has passed
- the medicine is cloudy, discolored, or has particles in it
- they look damaged or have been dropped
- You may see small air bubbles in the liquid. This is normal. You do not need to do anything about it.
Step 2: Choosing and preparing injection area
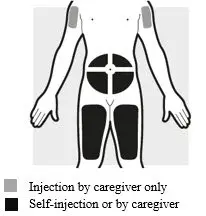
2a: Choose the area for your injections (see Figure G)
- You may inject into:
- your stomach area (abdomen)
- your thighs
- your upper arm. To inject into your upper arm, you will need a caregiver to give you the injections.
- Do not inject within 2 inches (5 cm) of your belly button (navel).
- Rotate the body area with each following set of injections. Do not use the same body area 2 times in a row.
- Do not inject where the skin is tender, damaged, bruised or scarred.
2b: Wash your hands and prepare your skin
- Wash your hands with soap and water.
- Clean the injection area for the 2 injections with an alcohol swab using a circular motion (see Figure H).
- Let the area dry completely.
- Do not blow or touch the cleaned area before injecting.
Step 3: Injecting ADBRY
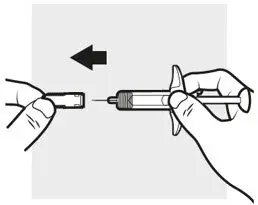
3a: Pull off the ADBRY needle cover
Hold the ADBRY prefilled syringe body with one hand, pull the needle cover straight off with your other hand (see Figure I) and throw it away in the sharps container.
- Do not try to recap the ADBRY prefilled syringes.
- Do not hold the plunger rod or plunger head while removing the needle cover.
- You may see a drop of liquid at the end of the needle. This is normal.
- Do not touch the needle, or let it touch any surface. If either of these occur, throw away the syringe and get a new one.

3b: Insert the needle
With one hand, gently pinch and hold a fold of skin where you cleaned the injection area. With the other hand, insert the needle completely at about a 45 degree angle into your skin (see Figure J).

3c: Inject the medicine
Use your thumb to firmly push down the plunger head all the way down (see Figure K). All the medicine is injected when you cannot push the plunger head any further.

3d: Release and remove
Lift your thumb off the plunger head. The needle will automatically move back inside the syringe body and lock into place (see Figure L).
- Place a dry cotton ball or gauze pad over the injection site for a few seconds. Do not rub the injection site. If needed, cover the injection site with a small bandage.
- There may be a small amount of blood or liquid where you injected. This is normal.
Throw away the used ADBRY prefilled syringe in the sharps disposal container. See Step 5 "Disposing of ADBRY".
Step 4: Injecting the next syringe
To get your full prescribed dose, you will need to give more than 1 injection.
- To get your full prescribed initial dose of 600 mg, you will need to give 4 injections.
- To get your full prescribed dose of 300 mg, you will need to give 2 injections.
Get a new ADBRY prefilled syringe and repeat Steps 3 and 5 (see Figure M) for each injection you need to give for your full prescribed dose.
Note
Make sure each injection is at least 1 inch (3 cm) from the prior injection site and within the same body area.

- Put the used ADBRY prefilled syringes in an FDA-cleared sharps disposal container right away after use (see Figure N). Do not throw away the ADBRY prefilled syringes in your household trash.
- If you do not have an FDA-cleared sharps disposal container, you may use a household container that is:
- made of heavy-duty plastic,
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out,
- upright and stable during use,
- leak-resistant, and
- properly labeled to warn of hazardous waste inside the container.
- When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and syringes. For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA's website at: http://www.fda.gov/safesharpsdisposal.
- Do not recycle your used sharps disposal container.
For more information go to www.ADBRY.com or call 1-844-692-3279. If you still have questions, call your healthcare provider.
Manufactured by: LEO Pharma A/S Industriparken 55, DK-2750 Ballerup, Denmark
Distributed by: LEO Pharma Inc., Madison, NJ 07940, USA
U.S. License No. 2169
ADBRY® is a registered trademark of LEO Pharma A/S.
© 2023 LEO Pharma Inc. All rights reserved.
This "Instructions for Use" has been approved by the U.S. Food and Drug Administration.
Approved March 2023
| ADBRY
tralokinumab-ldrm injection, solution |
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
| Labeler - LEO Pharma Inc. (832692615) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Catalent Indiana, LLC. | 172209277 | LABEL(50222-346) , PACK(50222-346) , MANUFACTURE(50222-346) , ANALYSIS(50222-346) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Astra Zeneca Pharmaceuticals LP | 968459953 | API MANUFACTURE(50222-346) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| LEO Pharma A/S | 306218108 | MANUFACTURE(50222-346) | |