Drug Detail:Alora (skin patch) (Estradiol transdermal (skin patch) [ es-tra-dye-ole-tranz-derm-al ])
Drug Class: Estrogens
Highlights of Prescribing Information
ALORA (estradiol transdermal system)
Initial U.S. Approval: 1975
WARNING: ENDOMETRIAL CANCER, CARDIOVASCULAR DISORDERS, PROBABLE DEMENTIA and BREAST CANCER
See full prescribing information for complete boxed warning.
Estrogen-Alone Therapy
• There is an increased risk of endometrial cancer in a woman with a uterus who uses unopposed estrogens (5.2)
• Estrogen-alone therapy should not be used for the prevention of cardiovascular disease or dementia (5.1, 5.3)
• The Women’s Health Initiative (WHI) estrogen-alone substudy reported increased risks of stroke and deep vein thrombosis (DVT) (5.1)
• The WHI Memory Study (WHIMS) estrogen-alone ancillary study of WHI reported an increased risk of probable dementia in postmenopausal women 65 years of age and older (5.3)
Estrogen Plus Progestin Therapy
• Estrogen plus progestin therapy should not be used for the prevention of cardiovascular disease or dementia (5.1, 5.3)
• The WHI estrogen plus progestin substudy reported increased risks of stroke, DVT, pulmonary embolism (PE), and myocardial infarction (MI) (5.1)
• The WHI estrogen plus progestin substudy reported increased risks of invasive breast cancer (5.2)
• The WHIMS estrogen plus progestin ancillary study of WHI reported an increased risk of probable dementia in postmenopausal women 65 years of age and older (5.3)
Recent Major Changes
Boxed Warning 03/2020
Indications and Usage for Alora
ALORA is an estrogen indicated for:
• Treatment of Moderate to Severe Vasomotor Symptoms due to Menopause (1.1)
• Treatment of Moderate to Severe Symptoms of Vulvar and Vaginal Atrophy due to Menopause (1.2)
• Treatment of Hypoestrogenism due to Hypogonadism, Castration or Primary Ovarian Failure (1.3)
• Prevention of Postmenopausal Osteoporosis (1.4)
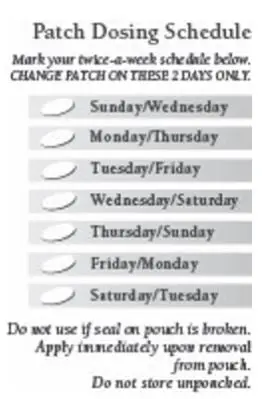
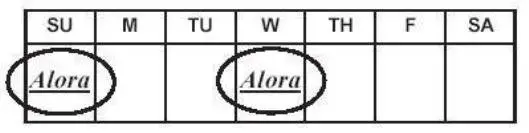
Alora Dosage and Administration
• Start therapy with ALORA 0.05 mg/day applied to the skin twice weekly for treatment of moderate to severe vasomotor symptoms, vulvar and vaginal atrophy symptoms due to menopause, hypoestrogenism due to hypogonadism, castration, or primary ovarian failure. Dosage adjustment should be guided by the clinical response (2.1, 2.2, 2.3, 2.4)
• Start therapy with ALORA 0.025 mg/day applied to the skin twice weekly for the prevention of postmenopausal osteoporosis. Dosage adjustment should be guided by the clinical response and adverse events (2.5)
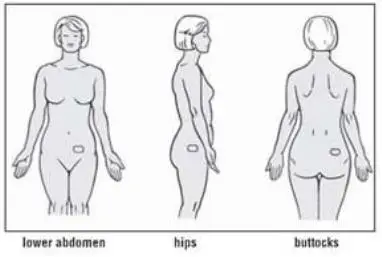
• ALORA should be placed on a clean, dry area of the lower abdomen (below the umbilicus) or upper quadrant of the buttock, or outer aspect of the hip. ALORA should not be applied to the breasts (2.6)
Dosage Forms and Strengths
Transdermal System 0.025 mg/day, 0.05 mg/day, 0.075 mg/day, and 0.1 mg/day (3)
Contraindications
• Undiagnosed abnormal genital bleeding. (4)
• Breast cancer or a history of breast cancer. (4, 5.2)
• Estrogen-dependent neoplasia. (4, 5.2)
• Active DVT, PE or a history of these conditions. (4, 5.1)
• Active arterial thromboembolic disease (e.g., stroke and MI) or a history of these conditions (4, 5.1)
• Known anaphylactic reaction or angioedema or hypersensitivity with ALORA (4)
• Hepatic impairment or disease (4, 5.10)
• Protein C, protein S, or antithrombin deficiency, or other known thrombophilic disorders (4)
Warnings and Precautions
• Estrogens increase the risk of gallbladder disease (5.4)
• Discontinue estrogens if severe hypercalcemia, loss of vision, severe hypertriglyceridemia or cholestatic jaundice occurs (5.5, 5.6, 5.9, 5.10)
• Monitor thyroid function in women on thyroid hormone replacement therapy (5.11, 5.18)
Adverse Reactions/Side Effects
Most common adverse reactions (≥10 percent) in the clinical study is breast pain (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Allergan at 1-800-678-7605 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
• Inducers and/or inhibitors of CYP3A4 may affect estrogen drug metabolism (7)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 3/2020
Full Prescribing Information
1. Indications and Usage for Alora
2. Alora Dosage and Administration
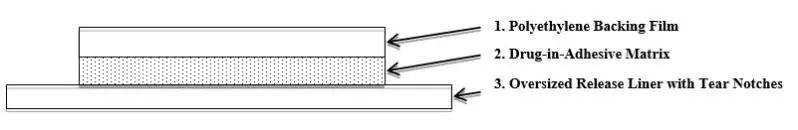
Administer Alora twice weekly, as instructed. Place the adhesive side of the Alora system on a clean, dry area of skin. The recommended application site is the lower abdomen. In addition, Alora may be used on the upper quadrant of the buttocks or outer aspect of the hip. Do not apply Alora to the breasts. Rotate the application sites of Alora , with an interval of at least 1 week allowed between applications to a particular site. Do not apply to oily, damaged, or irritated skin. Avoid the waistline, since tight clothing may rub the system off. Apply the system immediately after opening the pouch and removing the protective liner. Press the system firmly in place with the palm of the hand for about 10 seconds, making sure there is good contact, especially around the edges. Reapply the same system, in the event that a system should fall off. If necessary, a new system may be applied to another site. Maintain the original treatment schedule.
2.1 Important Instructions Including Administration with a Progestin
- Generally, when estrogen is prescribed for a postmenopausal woman with a uterus, consider addition of a progestin to reduce the risk of endometrial cancer. A woman who takes estrogen but does not have a uterus, generally does not need a progestin. In some cases, however, hysterectomized women who have a history of endometriosis may need a progestin [see Warnings and Precautions (5.2, 5.14)].
- Use estrogen-alone, or in combination with a progestin at the lowest effective dose and for the shortest duration consistent with treatment goals and risks for the individual woman. Re-evaluate postmenopausal women periodically as clinically appropriate to determine if treatment is still necessary.
2.2 Treatment of Moderate to Severe Vasomotor Symptoms due to Menopause
Start therapy with 0.05 mg per day applied to the skin twice weekly. Start therapy at the lowest effective dose and for the shortest duration consistent with treatment goals. Attempt to taper or discontinue the medication at 3 to 6-month intervals.
2.3 Treatment of Moderate to Severe Symptoms of Vulvar and Vaginal Atrophy due to Menopause
Start therapy with 0.05 mg per day applied to the skin twice weekly. Start therapy at the lowest effective dose and for the shortest duration consistent with treatment goals. Attempt to taper or discontinue the medication at 3 to 6-month intervals.
2.4 Treatment of Hypoestrogenism due to Hypogonadism, Castration, or Primary Ovarian Failure
Start therapy with 0.05 mg per day applied to the skin twice weekly. Adjust the dose as necessary to control symptoms. Use the clinical responses (relief of symptoms) at the lowest effective dose to guide administration of the Alora transdermal system, especially in women with an intact uterus.
2.5 Prevention of Postmenopausal Osteoporosis
Start therapy with 0.025 mg per day applied to the skin twice weekly. Use bone mineral density measurements to monitor treatment efficacy. Increase the dosage as necessary, depending on bone mineral density and adverse events. No studies have been conducted using an intermittent regimen for the prevention of postmenopausal osteoporosis.
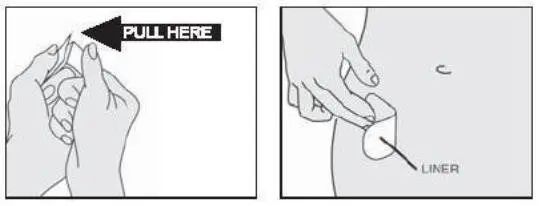
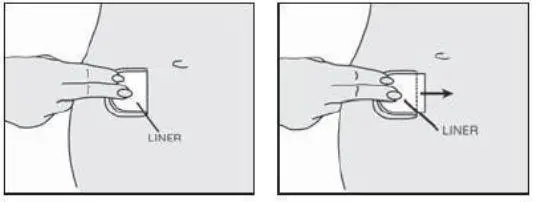
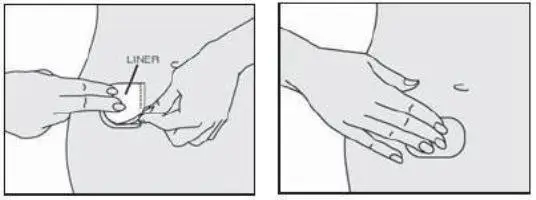
2.6 Application of the Alora Transdermal System
Site Selection
- Place the adhesive side of Alora on a clean, dry area of skin that is not oily, damaged or irritated.
- Apply Alora to the lower abdomen or the upper quadrant of the buttocks or the outer aspect of the hip.
- Never apply Alora to the breast.
- Do not apply Alora to the waistline since tight clothing may rub Alora off.
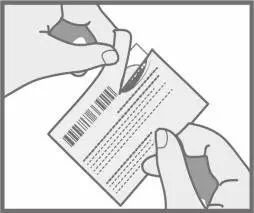
Application
- Apply Alora immediately after opening the pouch and remove the protective liner.
- Press Alora firmly in place with the palm of the hand for about 10 seconds. Make sure there is good contact with the skin, especially around the edges of Alora.
- If Alora falls off soon after application, the same Alora may be reapplied to a different site. If the original Alora cannot be reapplied, a new Alora may be applied to another site maintaining the same treatment schedule.
- Rotate the application sites with at least 1 week between applications to the same site.
4. Contraindications
Alora is contraindicated in women with any of the following conditions:
- Undiagnosed abnormal genital bleeding [see Warnings and Precautions (5.2)].
- Breast cancer or a history of breast cancer [see Warnings and Precautions (5.2)].
- Estrogen-dependent neoplasia [see Warnings and Precautions (5.2)].
- Active DVT, PE or a history of these conditions [see Warnings and Precautions (5.1)].
- Active arterial thromboembolic disease (e.g., stroke and MI) or a history of these conditions [see Warnings and Precautions (5.1)].
- Known anaphylactic reaction or angioedema or hypersensitivity with estradiol transdermal system
- Hepatic impairment or disease
- Protein C, protein S, or antithrombin deficiency, or other known thrombophilic disorders
5. Warnings and Precautions
5.1 Cardiovascular Disorders
Increased risk of stroke and DVT are reported with estrogen-alone therapy. Increased risk of PE, DVT, stroke, and MI are reported with estrogen plus progestin therapy. Immediately discontinue estrogens with or without progestin therapy if any of these occur or is suspected.
Manage appropriately any risk factors for arterial vascular disease (for example, hypertension, diabetes mellitus, tobacco use, hypercholesterolemia, and obesity) and/or venous thromboembolism (VTE) (for example, personal history or family history of VTE, obesity, and systemic lupus erythematosus).
Stroke
The WHI estrogen-alone substudy reported a statistically significant increased risk of stroke in women 50 to 79 years of age receiving daily CE (0.625 mg)-alone compared to women in the same age group receiving placebo (45 versus 33 strokes per 10,000 women-years, respectively). The increase in risk was demonstrated in year 1 and persisted [see Clinical Studies (14.4)]. Immediately discontinue estrogen-alone therapy if a stroke occurs or is suspected.
Subgroup analyses of women 50 to 59 of age suggest no increased risk of stroke for those women receiving CE (0.625 mg)-alone versus those receiving placebo (18 versus 21 per 10,000 women-years).1
The WHI estrogen plus progestin substudy reported a statistically significant increased risk of stroke in women 50 to 79 years of age receiving CE (0.625 mg) plus MPA (2.5 mg) compared to women in the same age group receiving placebo (33 versus 25 per 10,000 women-years) [see Clinical Studies (14.4)]. The increase in risk was demonstrated after the first year and persisted. Immediately discontinue estrogen plus progestin therapy if a stroke occurs or is suspected.
Coronary Heart Disease
The WHI estrogen-alone substudy reported no overall effect on coronary heart disease (CHD) events (defined as nonfatal MI, silent MI, or CHD death) in women receiving estrogen-alone compared to placebo2 [see Clinical Studies (14.4)].
Subgroup analyses of women 50 to 59 years of age suggest a statistically nonsignificant reduction in CHD events reported in women receiving daily CE (0.625 mg)-alone compared to placebo in women less than 10 years since menopause (8 versus 16 per 10,000 women-years).1
The WHI estrogen plus progestin substudy reported a statistically nonsignificant increased risk of CHD events in women receiving daily CE (0.625 mg) plus MPA (2.5 mg) compared to women receiving placebo (41 versus 34 per 10,000 women-years).1 An increase in relative risk was demonstrated in year 1, and a trend toward decreasing relative risk was reported in years 2 through 5 [see Clinical Studies (14.4)].
In postmenopausal women with documented heart disease (n=2,763, average 66.7 years of age) a controlled clinical trial of secondary prevention of cardiovascular disease [Heart and Estrogen/Progestin Replacement (HERS) Study] treatment with daily CE (0.625 mg) plus MPA (2.5 mg) demonstrated no cardiovascular benefit. During an average follow-up of 4.1 years, treatment with CE plus MPA did not reduce the overall rate of CHD events in postmenopausal women with established CHD. There were more CHD events in the CE plus MPA-treated group than in the placebo group in year 1, but not during the subsequent years. Two thousand three hundred and twenty-one (2,321) women from the original HERS trial agreed to participate in an open label extension of HERS, HERS II. Average follow-up in HERS II was an additional 2.7 years, for a total of 6.8 years overall. Rates of CHD events were comparable among women in the CE/MPA group and the placebo group in HERS, HERS II, and overall.
Venous Thromboembolism
In the WHI estrogen-alone substudy, the risk of VTE (DVT and PE) was increased for women receiving daily CE (0.625 mg)-alone compared to placebo (30 versus 22 per 10,000 women-years), although only the increased risk of DVT reached statistical significance (23 versus 15 per 10,000 women-years). The increase in VTE risk was demonstrated during the first 2 years 3 [see Clinical Studies (14.4)]. Immediately discontinue estrogen-alone therapy if a VTE occurs or is suspected.
In the WHI estrogen plus progestin substudy, a statistically significant 2-fold greater rate of VTE was reported in women receiving daily CE (0.625 mg) plus MPA (2.5 mg) compared to women receiving placebo (35 versus 17 per 10,000 women-years). Statistically significant increases in risk for both DVT (26 versus 13 per 10,000 women-years) and PE (18 versus 8 per 10,000 women-years) were also demonstrated. The increase in VTE risk was demonstrated during the first year and persisted 4 [see Clinical Studies (14.4)]. Immediately discontinue estrogen plus progestin therapy if a VTE occurs or is suspected.
If feasible, discontinue estrogens at least 4 to 6 weeks before surgery of the type associated with an increased risk of thromboembolism, or during periods of prolonged immobilization.
5.2 Malignant Neoplasms
Endometrial Cancer
An increased risk of endometrial cancer has been reported with the use of unopposed estrogen therapy in a woman with a uterus. The reported endometrial cancer risk among unopposed estrogen users is about 2 to 12-fold greater than in non-users and appears dependent on duration of treatment and on estrogen dose. Most studies show no significant increased risk associated with use of estrogens for less than one year. The greatest risk appears associated with prolonged use, with increased risks of 15 to 24-fold for 5 to 10 years or more. This risk has been shown to persist for at least 8 to 15 years after estrogen therapy is discontinued.
Clinical surveillance of all women taking estrogen/progestin combinations is important. Undertake adequate diagnostic measures, including directed or random endometrial sampling when indicated, to rule out malignancy in postmenopausal women with persistent or recurring abnormal genital bleeding with unknown etiology.
There is no evidence that the use of natural estrogens results in a different endometrial risk profile than synthetic estrogens of equivalent estrogen dose. Adding a progestin to estrogen therapy has been shown to reduce the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer.
Breast Cancer
The WHI substudy of daily CE (0.625 mg)-alone provided information about breast cancer in estrogen alone users. In the WHI estrogen-alone substudy, after an average follow-up of 7.1 years, daily CE-alone was not associated with an increased risk of invasive breast cancer [relative risk (RR) 0.80] compared to placebo5 [see Clinical Studies (14.4)].
After a mean follow-up of 5.6 years, the WHI substudy of daily CE (0.625 mg) plus MPA (2.5 mg) reported an increased risk of invasive breast cancer in women who took daily CE plus MPA compared to placebo. In this substudy, prior use of estrogen-alone or estrogen plus progestin therapy was reported by 26 percent of the women. The relative risk of invasive breast cancer was 1.24, and the absolute risk was 41 versus 33 cases per 10,000 women-years, for CE plus MPA compared with placebo. Among women who reported prior use of hormone therapy, the relative risk of invasive breast cancer was 1.86, and the absolute risk was 46 versus 25 cases per 10,000 women-years for CE plus MPA compared with placebo [see Clinical Studies (14.4)]. Among women who reported no prior use of hormone therapy, the relative risk of invasive breast cancer was 1.09, and the absolute risk was 40 versus 36 cases per 10,000 women-years for CE plus MPA compared with placebo. In the same substudy, invasive breast cancers were larger, were more likely to be node positive, and were diagnosed at a more advanced stage in the CE (0.625 mg) plus MPA (2.5 mg) group compared with the placebo group. Metastatic disease was rare, with no apparent difference between the two groups. Other prognostic factors, such as histologic subtype, grade and hormone receptor status did not differ between the groups6 [see Clinical Studies (14.4)].
Consistent with the WHI clinical trial, observational studies have also reported an increased risk of breast cancer with estrogen plus progestin therapy, and a smaller increase in the risk for breast cancer with estrogen-alone therapy, after several years of use. The risk increased with duration of use and appeared to return to baseline over about 5 years after stopping treatment (only the observational studies have substantial data on risk after stopping). Observational studies also suggest that the risk of breast cancer was greater, and became apparent earlier, with estrogen plus progestin therapy as compared to estrogen-alone therapy.
These studies have not generally found significant variation in the risk of breast cancer among different estrogen plus progestin combinations, doses, or routes of administration. The use of estrogen-alone and estrogen plus progestin has been reported to result in an increase in abnormal mammograms requiring further evaluation.
All women should receive yearly breast examinations by a healthcare provider and perform monthly breast self-examinations. In addition, mammography examinations should be scheduled based on patient age, risk factors, and prior mammogram results.
Ovarian Cancer
The CE plus MPA substudy of WHI reported that estrogen plus progestin increased the risk of ovarian cancer. After an average follow-up of 5.6 years, the relative risk for ovarian cancer for CE plus MPA vs. placebo was 1.58 (95% confidence interval 0.77-3.24) but was not statistically significant. The absolute risk for CE plus MPA versus placebo was 4.2 versus. 2.7 cases per 10,000 women-years.
A meta-analysis of 17 prospective and 35 retrospective epidemiology studies found that women who used hormonal therapy for menopausal symptoms had an increased risk for ovarian cancer. The primary analysis, using case-control comparisons, included 12,110 cancer cases from the 17 prospective studies. The relative risks associated with current use of hormonal therapy was 1.41 (95% confidence interval [CI] 1.32 to 1.50); there was no difference in the risk estimates by duration of the exposure (less than 5 years [median of 3 years] vs. greater than 5 years [median of 10 years] of use before the cancer diagnosis). The relative risk associated with combined current and recent use (discontinued use within 5 years before cancer diagnosis) was 1.37 (95% CI 1.27-1.48) and the elevated risk was significant for both estrogen-alone and estrogen plus progestin products. The exact duration of hormone therapy use associated with an increased risk of ovarian cancer, however, is unknown.
5.3 Probable Dementia
In the WHI Memory Study (WHIMS) estrogen-alone ancillary study, a population of 2,947 hysterectomized women 65 to 79 years of age was randomized to daily CE (0.625 mg)-alone or placebo.
After an average follow-up of 5.2 years, 28 women in the estrogen-alone group and 19 women in the placebo group were diagnosed with probable dementia. The relative risk of probable dementia for CE alone versus placebo was 1.49 (95 percent CI, 0.83-2.66). The absolute risk of probable dementia for CE-alone versus placebo was 37 versus 25 cases per 10,000 women-years8 [see Use in Specific Populations (8.5), and Clinical Studies (14.5)].
In the WHIMS estrogen plus progestin ancillary study, a population of, 4,532 postmenopausal women 65 to 79 years of age was randomized to daily CE (0.625 mg) plus MPA (2.5 mg) or placebo. After an average follow-up of 4 years, 40 women in the CE plus MPA group and 21 women in the placebo group were diagnosed with probable dementia. The relative risk for CE plus MPA versus placebo was 2.05 (95% confidence interval 1.21 – 3.48). The absolute risk of probable dementia for CE plus MPA versus placebo was 45 versus 22 cases per 10,000 women-years8 [see Use in Specific Populations (8.5), and Clinical Studies (14.5)].
When data from the two populations in the WHIMS estrogen-alone and estrogen plus progestin ancillary studies were pooled as planned in the WHIMS protocol, the reported overall relative risk for probable dementia was 1.76 (95 percent CI, 1.19-2.60). Since both ancillary studies were conducted in women 65 to 79 years of age, it is unknown whether these findings apply to younger postmenopausal women8 [see Use in Specific Populations (8.5), and Clinical Studies (14.5)].
5.4 Gallbladder Disease
A 2 to 4-fold increase in the risk of gallbladder disease requiring surgery in postmenopausal women receiving estrogens has been reported.
5.5 Hypercalcemia
Estrogen administration may lead to severe hypercalcemia in women with breast cancer and bone metastases. Discontinue estrogens, including Alora if hypercalcemia occurs, and take appropriate measures to reduce the serum calcium level.
5.6 Visual Abnormalities
Retinal vascular thrombosis has been reported in women receiving estrogens. Discontinue Alora pending examination if there is sudden partial or complete loss of vision, or a sudden onset of proptosis, diplopia, or migraine. Discontinue estrogens, including Alora, if examination reveals papilledema or retinal vascular lesions.
5.9 Exacerbation of Hypertriglyceridemia
In women with pre-existing hypertriglyceridemia, estrogen therapy may be associated with elevations of plasma triglycerides leading to pancreatitis. Consider discontinuation of Alora if pancreatitis occurs.
5.10 Hepatic Impairment and/or Past History of Cholestatic Jaundice
Estrogens may be poorly metabolized in women with hepatic impairment. For women with a history of cholestatic jaundice associated with past estrogen use or with pregnancy, exercise caution in prescribing Alora, and in the case of recurrence of cholestatic jaundice, discontinue Alora.
5.11 Exacerbation of Hypothyroidism
Estrogen administration leads to increased thyroid-binding globulin (TBG) levels. Women with normal thyroid function can compensate for the increased TBG by making more thyroid hormone, thus maintaining free T4 and T3 serum concentrations in the normal range. Women dependent on thyroid hormone replacement therapy who are also receiving estrogens may require increased doses of their thyroid replacement therapy. Monitor thyroid function in these women during treatment with Alora to maintain their free thyroid hormone levels in an acceptable range.
5.14 Exacerbation of Endometriosis
A few cases of malignant transformation of residual endometrial implants have been reported in women treated post-hysterectomy with estrogen-alone therapy. Consider the addition of a progestin for women known to have residual endometriosis post-hysterectomy.
5.18 Drug/Laboratory Test Interactions
- Accelerated prothrombin time, partial thromboplastin time, and platelet aggregation time; increased platelet count; increased factors II, VII antigen, VIII antigen, VIII coagulant activity, IX, X, XII, VII-X complex, II-VII-X complex, and beta- thromboglobulin; decreased levels of anti-factor Xa and antithrombin III, decreased antithrombin III activity; increased levels of fibrinogen and fibrinogen activity; increased plasminogen antigen and activity.
- Increased thyroid-binding globulin (TBG) leading to increased circulating total thyroid hormone, as measured by protein-bound iodine (PBI), T4 levels (by column or by radioimmunoassay) or T3 levels by radioimmunoassay. T3 resin uptake is decreased, reflecting the elevated TBG. Free T4 and free T3 concentrations are unaltered. Women on thyroid replacement therapy may require higher doses of thyroid hormone.
- Other binding proteins may be elevated in serum, for example, corticosteroid binding globulin (CBG), sex hormone-binding globulin (SHBG), leading to increased circulating corticosteroids and sex steroids, respectively. Free hormone concentrations, such as testosterone and estradiol, may be decreased. Other plasma proteins may be increased (angiotensinogen/renin substrate, alpha-1-antitrypsin, ceruloplasmin).
- Increased plasma high-density lipoprotein (HDL) and HDL2 subfraction concentrations, reduced low-density lipoprotein (LDL) cholesterol concentration, increased triglycerides levels.
- Impaired glucose tolerance.
6. Adverse Reactions/Side Effects
The following serious adverse reactions are discussed elsewhere in the labeling:
- Cardiovascular Disorders [see Boxed Warning and Warnings and Precautions (5.1)].
- Malignant Neoplasms [see Boxed Warning and Warning and Precautions (5.2)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reactions rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adverse reactions for Alora 0.025 mg/day, 0.05 mg/day, and 0.075 mg/day transdermal systems versus placebo, each applied twice weekly, were evaluated in a 2-year randomized, parallel-group, double-blind, double-dummy, placebo-controlled multicenter trial for the prevention of osteoporosis in 355 hysterectomized postmenopausal women [see Clinical Studies (14.3)]. Adverse reactions with an incidence greater than 2% and greater than placebo, are shown in Table 1.
| Placebo | Alora | Alora | Alora | |
| Body System | 0.025 mg/day | 0.05 mg/day | 0.075 mg/day | |
| (N = 87) | (N = 89) | (N = 90) | (N = 89) | |
| Preferred Term | n(%) | n(%) | n(%) | n(%) |
| Body As A Whole | ||||
| Asthenia | 4 (4.6) | 7 (7.9) | -- | -- |
| Cyst | 3 (3.4) | -- | 6 (6.7) | -- |
| Infection Fungal | 1 (1.1) | 3 (3.4) | 9 (10) | 4 (4.5) |
| Pain Abdominal | 4 (4.6) | 7 (7.9) | 5 (5.6) | -- |
| Pain Back | 5 (5.7) | -- | -- | 7 (7.9) |
| Cardiovascular | ||||
| Hypertension | 3 (3.4) | -- | -- | 6 (6.7) |
| Migraine | 2 (2.3) | 6 (6.7) | -- | -- |
| Digestive | ||||
| Dyspepsia | 1 (1.1) | 8 (9) | 4 (4.4) | 3 (3.4) |
| Gastroenteritis | 2 (2.3) | 3 (3.4) | 4 (4.4) | 3 (3.4) |
| Nausea | 3 (3.4) | 6 (6.7) | 5 (5.6) | -- |
| Nervous | ||||
| Dizziness | 0 (0) | -- | 7 (7.8) | 4 (4.5) |
| Skin | ||||
| Hirsutism | 0 (0) | 2 (2.2) | 2 (2.2) | 4 (4.5) |
| Pruritus | 4 (4.6) | -- | -- | 6 (6.7) |
| Rash | 5 (5.7) | 6 (6.7) | 8 (8.9) | -- |
| Urogenital | ||||
| Breast Enlargement | 3 (3.4) | -- | -- | 6 (6.7) |
| Leukorrhea | 1 (1.1) | 3 (3.4) | 2 (2.2) | 4 (4.5) |
| Pain Breast | 7 (8) | 13 (14.6) | 16 (17.8) | 31 (34.8) |
| -- represents exclusion of data that was less than 2% or less than placebo. | ||||
7. Drug Interactions
In vitro and in vivo studies have shown that estrogens are metabolized partially by cytochrome P450 3A4 (CYP3A4). Therefore, inducers or inhibitors of CYP3A4 may affect estrogen drug metabolism. Inducers of CYP3A4 such as St. John's Wort preparations (Hypericum perforatum), phenobarbital, phenytoin, carbamazepine, rifampin and dexamethasone may reduce plasma concentrations of estrogens, possibly resulting in a decrease in therapeutic effects and/or changes in the uterine bleeding profile. Inhibitors of CYP3A4 such as cimetidine, erythromycin, clarithromycin, ketoconazole, itraconazole, ritonavir and grapefruit juice may increase plasma concentrations of estrogens and may result in adverse reactions.
8. Use In Specific Populations
8.5 Geriatric Use
There have not been sufficient numbers of geriatric women involved in clinical studies utilizing Alora to determine whether those over 65 years of age differ from younger subjects in their response to Alora.
The Women’s Health Initiative Studies
In the WHI estrogen-alone substudy (daily CE [0.625 mg]-alone versus placebo), there was a higher relative risk of stroke in women greater than 65 years of age [see Warnings and Precautions (5.1), and Clinical Studies (14.5)].
In the WHI estrogen plus progestin substudy (daily CE [0.625 mg] plus MPA [2.5 mg] versus placebo), there was a higher relative risk of nonfatal stroke and invasive breast cancer in women greater than 65 years of age [see Warnings and Precautions (5.1), and Clinical Studies (14.5)].
The Women’s Health Initiative Memory Study
In the WHIMS ancillary studies of postmenopausal women 65 to 79 years of age, there was an increased risk of developing probable dementia in women receiving estrogen-alone or estrogen plus progestin when compared to placebo [see Warnings and Precautions (5.3), and Clinical Studies (14.5)]. Since both ancillary studies were conducted in women 65 to 79 years of age, it is unknown whether these findings apply to younger postmenopausal women [see Warnings and Precautions (5.3), and Clinical Studies (14.5)].
12. Alora - Clinical Pharmacology
12.3 Pharmacokinetics
The apparent mean (SD) serum half-life of estradiol is 1.75 ± 2.87 hours following Alora application.
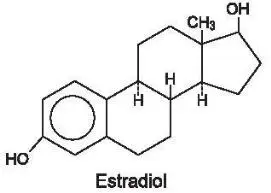
Absorption
Estradiol is transported across intact skin and into the systemic circulation by a passive diffusion process, the rate of diffusion across the stratum corneum being the principal factor. Alora maintains continuous transport of estradiol to the surface of the skin over the 3 to 4 day dosing interval.
Direct measurement of total absorbed dose of estradiol through analysis of residual estradiol content of systems worn over a continuous 4-day interval during 251 separate occasions in 123 postmenopausal women demonstrated that the average daily dose absorbed from Alora was 0.003 ± 0.001 mg estradiol per cm2 active surface area. The nominal mean in vivo daily delivery rates of estradiol calculated from these data are 0.027 mg/day, 0.054 mg/day, 0.081 mg/day, and 0.11 mg/day for the 9 cm2, 18 cm2, 27 cm2, and 36 cm2 Alora, respectively.
In another study, 20 women also were treated with three consecutive doses of Alora 0.05 mg/day, Alora 0.075 mg/day and Alora 0.1 mg/day administered in a twice weekly regimen for three weeks to the abdominal application sites. Mean steady-state estradiol serum concentrations observed over the dosing interval are shown in Figure 1 and a summary of estradiol pharmacokinetic parameters is provided in Table 2.
Figure 1
Mean Steady-State Estradiol Serum Concentration During the Third Twice Weekly Dose of Alora 0.1 mg/day, Alora 0.075 mg/day, and Alora 0.05 mg/day in 20 Postmenopausal Women.
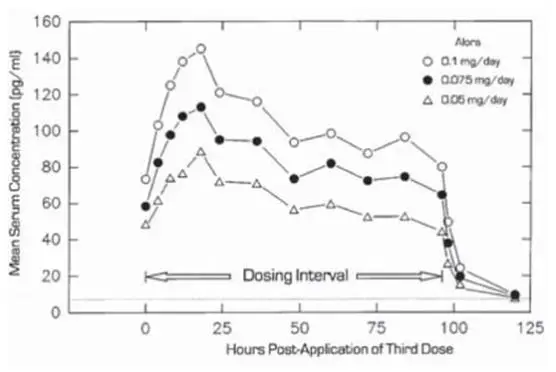
Table 2 Mean (SD) Pharmacokinetic Profile of Estradiol Over an 84-hour Dosing Interval following the Third Twice Weekly Dose of Alora 0.1 mg/day, Alora 0.075 mg/day, and Alora 0.05 mg/day in Postmenopausal Women.

In a single-dose randomized crossover study conducted to compare the effect of site of Alora application, 31 postmenopausal women wore single Alora 0.05 mg/day for 4-day periods on the lower abdomen, upper quadrant of the buttocks, and outside aspect of the hip. The estradiol serum concentration profiles are shown in Figure 2 and a summary of estradiol pharmacokinetic parameters is provided in Table 3.
Figure 2
Mean Estradiol Serum Concentrations During a Single 4-Day Wearing of Alora 0.05 mg/day Applied by 31 Postmenopausal Women to the Lower Abdomen, Upper Quadrant of the Buttocks or Outer Aspect of the Hip.
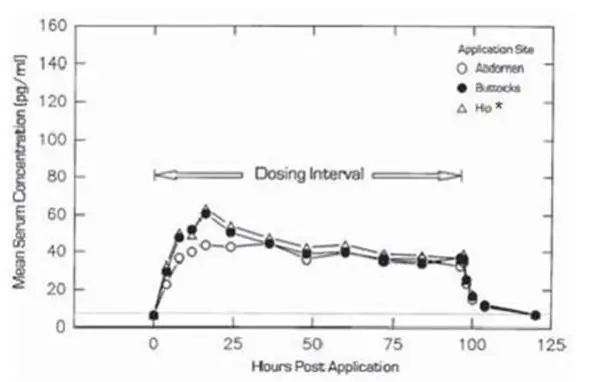
*Cmax and Cavg statistically different from abdomen
| Alora (mg/day) | Application Site | N | Dosing | Cmax (pg/mL) | Cmin (pg/mL) | Cavg (pg/mL) | CL (L/hr) |
| 0.05 | Abdomen | 31 | Single | 53 (23) | - | 41 (18) | 69 (22) |
| Buttock | 31 | Single | 67 (45) | - | 45 (21) | 66 (23) | |
| Hip* | 31 | Single | 69 (30) | - | 48 (17) | 62 (18) |
*Cmax and Cavg statistically different from abdomen
Steady-state estradiol serum concentrations were measured in two well-controlled clinical trials in the treatment of menopausal symptoms of 3 month duration (Studies 1 and 2), and one trial in the prevention of postmenopausal osteoporosis of 2 year duration (Study 3).
Table 4 provides a summary of these data.
| Alora (mg/day) | Study 1 | Study 2 | Study 3 |
| 0.025 | - | - | 24.5 (12.4) |
| 0.05 | 46.9 (38.5) | 38.8 (38.0) | 42.6 (23.7) |
| 0.075 | - | - | 56.7 (36.8) |
| 0.1 | 99.2 (77.0) | 97.0 (87.5) | - |
In a 2-year, randomized, double-blind, placebo-controlled, prevention of postmenopausal osteoporosis study in 355 hysterectomized women, the average baseline-adjusted steady-state estradiol serum concentrations were 18.6 pg/mL (45 patients) for the 0.025 mg/day dose, 35.9 pg/mL (47 patients) for the 0.05 mg/day dose, and 50.1 pg/mL (46 patients) for the 0.075 mg/day dose. These values were linearly related and dose proportional.
Distribution
No specific investigation of the tissue distribution of estradiol absorbed from Alora in humans has been conducted. The distribution of exogenous estrogens is similar to that of endogenous estrogens. Estrogens are widely distributed in the body and are generally found in higher concentrations in the sex hormone target organs. Estrogens circulate in the blood largely bound to sex hormone binding globulin (SHBG) and albumin.
Metabolism
Exogenous estrogens are metabolized in the same manner as endogenous estrogens. Circulating estrogens exist in a dynamic equilibrium of metabolic interconversions. These transformations take place mainly in the liver. Estradiol is converted reversibly to estrone, and both can be converted to estriol, which is the major urinary metabolite. Estrogens also undergo enterohepatic recirculation via sulfate and glucuronide conjugation in the liver, biliary secretion of conjugates into the intestine, and hydrolysis in the gut followed by reabsorption. In postmenopausal women a significant portion of the circulating estrogens exists as sulfate conjugates, especially estrone sulfate, which serves as a circulating reservoir for the formation of more active estrogens.
Excretion
Estradiol, estrone and estriol are excreted in the urine along with glucuronide and sulfate conjugates.
14. Clinical Studies
14.4 Women’s Health Initiative Studies
The WHI enrolled a total of 27,000 predominantly healthy postmenopausal women in two substudies to assess the risks and benefits of daily oral CE (0.625 mg)-alone or in combination with MPA (2.5 mg) compared to placebo in the prevention of certain chronic diseases. The primary endpoint was the incidence of CHD (defined as nonfatal MI, silent MI and CHD death), with invasive breast cancer as the primary adverse outcome studied. A “global index” included the earliest occurrence of CHD, invasive breast cancer, stroke, PE, endometrial cancer (only in the CE plus MPA substudy), colorectal cancer, hip fracture, or death due to other cause. The substudies did not evaluate the effects of CE-alone or CE plus MPA on menopausal symptoms.
WHI Estrogen-Alone Substudy
The WHI estrogen-alone substudy was stopped early because an increased risk of stroke was observed, and it was deemed that no further information would be obtained regarding the risk and benefits of estrogen-alone in predetermined primary endpoints.
Results of the estrogen-alone substudy, which included 10,739 women (average 63 years of age, range 50 to 79: 75.3 percent White, 15.1 percent Black, 6.1 percent Hispanic, 3.6 percent Other) after an average follow-up of 7.1 years, are presented in Table 6.
| Event | Relative Risk
CE vs. Placebo (95% nCIb) | CE
n = 5,310 | Placebo
n = 5,429 |
| Absolute Risk per 10,000
Women-years |
|||
| CHD eventsc | 0.95 (0.78-1.16) | 54 | 57 |
| Non-fatal MIc | 0.91 (0.73-1.14) | 40 | 43 |
| CHD deathc | 1.01 (0.71-1.43) | 16 | 16 |
| All strokesc | 1.33 (1.05-1.68) | 45 | 33 |
| Ischemic strokec | 1.55 (1.19-2.01) | 38 | 25 |
| Deep vein thrombosisc,d | 1.47 (1.06-2.06) | 23 | 15 |
| Pulmonary embolismc | 1.37 (0.9-2.07) | 14 | 10 |
| Invasive breast cancerc | 0.80 (0.62-1.04) | 28 | 34 |
| Colorectal cancerc | 1.08 (0.75-1.55) | 17 | 16 |
| Hip fracturec | 0.65 (0.45-0.94) | 12 | 19 |
| Vertebral fracturesc,d | 0.64 (0.44-0.93) | 11 | 18 |
| Lower arm/wrist fracturesc,d | 0.58 (0.47-0.72) | 35 | 59 |
| Total fracturesc,d | 0.71 (0.64-0.80) | 144 | 197 |
| Death due to other causese,f | 1.08 (0.88-1.32) | 53 | 50 |
| Overall mortalityc,d | 1.04 (0.88-1.22) | 79 | 75 |
| Global Indexg | 1.02 (0.92-1.13) | 206 | 201 |
a) Adapted from numerous WHI publications. WHI publications can be viewed at www.nhlbi.nih.gov/whi.
b) Nominal confidence intervals unadjusted for multiple looks and multiple comparisons.
c) Results are based on centrally adjudicated data for an average follow-up of 7.1 years.
d) Not included in “global index”.
e) Results are based on an average follow-up of 6.8 years.
f) All deaths, except from breast or colorectal cancer, definite or probable CHD, PE or cerebrovascular disease.
g) A subset of the events was combined in a "global index", defined as the earliest occurrence of CHD events, invasive breast cancer, stroke, pulmonary embolism, endometrial cancer, colorectal cancer, hip fracture, or death due to other causes.
For those outcomes included in the WHI "global index" that reached statistical significance, the absolute excess risks per 10,000 women-years in the group treated with CE-alone was 12 more strokes, while the absolute risk reduction per 10,000 women-years was 7 fewer hip fractures.9 The absolute excess risk of events included in the "global index" was a non-significant 5 events per 10,000 women-years. There was no difference between the groups in terms of all-cause mortality.
No overall difference for primary CHD events (nonfatal MI, silent MI and CHD death) and invasive breast cancer incidence in women receiving CE-alone compared with placebo was reported in final centrally adjudicated results from the estrogen-alone substudy, after an average follow-up of 7.1 years. See Table 6.
Centrally adjudicated results for stroke events from the estrogen-alone substudy, after an average follow-up of 7.1 years, reported no significant difference in the distribution of stroke subtype and severity, including fatal strokes, in women receiving estrogen-alone compared to placebo. Estrogen-alone increased the risk of ischemic stroke, and this excess risk was present in all subgroups of women examined.10
Timing of initiation of estrogen-alone therapy relative to the start of menopause may affect the overall risk-benefit profile. The WHI estrogen-alone substudy stratified by age showed in women 50 to 59 years of age a non-significant trend toward reduced risk for CHD [hazard ratio (HR) 0.63 (95 percent CI, 0.36-1.09)] and overall mortality [HR 0.71 (95 percent CI, 0.46-1.11)].
WHI Estrogen Plus Progestin Substudy
The WHI estrogen plus progestin substudy was stopped early. According to the predefined stopping rule, after an average follow-up of 5.6 years of treatment, the increased risk of invasive breast cancer and cardiovascular events exceeded the specified benefits included in the “global index.” The absolute excess risk of events included in the “global index” was 19 per 10,000 women-years.
For those outcomes included in the WHI “global index” that reached statistical significance after 5.6 years of follow-up, the absolute excess risks per 10,000 women-years in the group treated with CE plus MPA were 7 more CHD events, 8 more strokes, 10 more PEs, and 8 more invasive breast cancers, while the absolute risk reduction per 10,000 women-years were 6 fewer colorectal cancers and 5 fewer hip fractures.
Results of the CE plus MPA substudy, which included 16,608 women (average age of 63 years, range 50 to 79; 83.9% White, 6.8% Black, and 5.4% Hispanic, 3.9% Other), are presented in Table 7.
| Event | Relative Risk
CE/MPA vs. placebo (95% nCIc) | CE/MPA
n = 8,506 | Placebo
n = 8,102 |
| Absolute Risk per 10,000 Women-years | |||
| CHD events | 1.23 (0.99-1.53) | 41 | 34 |
| Non-fatal MI | 1.28 (1.00-1.63) | 31 | 25 |
| CHD death | 1.10 (0.70-1.75) | 8 | 8 |
| All strokes | 1.31 (1.03-1.68) | 33 | 25 |
| Ischemic stroke | 1.44 (1.09-1.90) | 26 | 18 |
| Deep vein thrombosisd | 1.95 (1.43-2.67) | 26 | 13 |
| Pulmonary embolism | 2.13 (1.45-3.11) | 18 | 8 |
| Invasive breast cancere | 1.24 (1.01-1.54) | 41 | 33 |
| Colorectal cancer | 0.61 (0.42-0.87) | 10 | 16 |
| Endometrial cancerd | 0.81 (0.48-1.36) | 6 | 7 |
| Cervical cancerd | 1.44 (0.47-4.42) | 2 | 1 |
| Hip fracture | 0.67 (0.47-0.96) | 11 | 16 |
| Vertebral fracturesd | 0.65 (0.46-0.92) | 11 | 17 |
| Lower arm/wrist fracturesd | 0.71 (0.59-0.85) | 44 | 62 |
| Total fracturesd | 0.76 (0.69-0.83) | 152 | 199 |
| Overall mortalityf | 1.00 (0.83-1.19) | 52 | 52 |
| Global Indexg | 1.13 (1.02-1.25) | 184 | 165 |
a) Adapted from numerous WHI publications. WHI publications can be viewed at www.nhlbi.nih.gov/whi.
b) Results are based on centrally adjudicated data.
c) Nominal confidence intervals unadjusted for multiple looks and multiple comparisons.
d) Not included in “global index”.
e) Includes metastatic and non-metastatic breast cancer, with the exception of in situ breast cancer.
f) All deaths, except from breast or colorectal cancer, definite or probable CHD, PE or cerebrovascular disease.
g) A subset of the events was combined in a "global index", defined as the earliest occurrence of CHD events, invasive breast cancer, stroke, pulmonary embolism, endometrial cancer, colorectal cancer, hip fracture, or death due to other causes.
Timing of initiation of estrogen plus progestin therapy relative to the start of menopause may affect the overall risk benefit profile. The WHI estrogen plus progestin substudy stratified by age showed in women 50 to 59 years of age, a non-significant trend toward reduced risk for overall mortality [HR 0.69 (95 percent CI, 0.44-1.07)].
14.5 Women’s Health Initiative Memory Study
The WHIMS estrogen-alone ancillary study of WHI enrolled 2,947 predominantly healthy hysterectomized postmenopausal women 65 to 79 years of age (45 percent were 65 to 69 years of age; 36 percent were 70 to 74 years of age; 19 percent were 75 years of age and older) to evaluate the effects of daily CE (0.625 mg)-alone on the incidence of probable dementia (primary outcome) compared to placebo.
After an average follow-up of 5.2 years, the relative risk of probable dementia for CE-alone versus placebo was 1.49 (95 percent CI, 0.83-2.66). The absolute risk of probable dementia for CE-alone versus placebo was 37 versus 25 cases per 10,000 women-years. Probable dementia as defined in the study included Alzheimer’s disease (AD), vascular dementia (VaD) and mixed types (having features of both AD and VaD). The most common classification of probable dementia in the treatment group and the placebo group was AD. Since the ancillary study was conducted in women 65 to 79 years of age, it is unknown whether these findings apply to younger postmenopausal women [see Warnings and Precautions (5.3), and Use in Specific Populations (8.5)].
The WHIMS estrogen plus progestin ancillary study enrolled 4,532 predominantly healthy postmenopausal women 65 years of age and older (47 percent were 65 to 69 years of age; 35 percent were 70 to 74 years of age; and 18 percent were 75 years of age and older) to evaluate the effects of daily CE (0.625 mg) plus MPA (2.5 mg) on the incidence of probable dementia (primary outcome) compared to placebo.
After an average follow-up of 4 years, the relative risk of probable dementia for CE plus MPA versus placebo was 2.05 (95 percent CI, 1.21-3.48). The absolute risk of probable dementia for CE plus MPA versus placebo was 45 versus 22 cases per 10,000 women-years. Probable dementia as defined in the study included AD, VaD and mixed types (having features of both AD and VaD). The most common classification of probable dementia in the treatment group and the placebo group was AD. Since the ancillary study was conducted in women 65 to 79 years of age, it is unknown whether these findings apply to younger postmenopausal women [see Warnings and Precautions (5.3), and Use in Specific Populations (8.5)].
When data from the two populations were pooled as planned in the WHIMS protocol, the reported overall relative risk for probable dementia was 1.76 (95 percent CI, 1.19-2.60). Differences between groups became apparent in the first year of treatment. It is unknown whether these findings apply to younger postmenopausal women [see Warnings and Precautions (5.3), and Use in Specific Populations (8.5)].
15. References
- Rossouw JE, et al. Postmenopausal Hormone Therapy and Risk of Cardiovascular Disease by Age and Years Since Menopause. JAMA. 2007;297:1465-1477.
- Hsia J, et al. Conjugated Equine Estrogens and Coronary Heart Disease. Arch Int Med. 2006;166:357-365.
- Curb JD, et al. Venous Thrombosis and Conjugated Equine Estrogen in Women Without a Uterus. Arch Int Med. 2006;166:772-780.
- Cushman M, et al. Estrogen Plus Progestin and Risk of Venous Thrombosis. JAMA. 2004;292:1573-1580.
- Stefanick ML, et al. Effects of Conjugated Equine Estrogens on Breast Cancer and Mammography Screening in Postmenopausal Women With Hysterectomy. JAMA. 2006;295:1647-1657.
- Chlebowski RT, et al. Influence of Estrogen Plus Progestin on Breast Cancer and Mammography in Healthy Postmenopausal Women. JAMA. 2003;289:3234-3253.
- Anderson GL, et al. Effects of Estrogen Plus Progestin on Gynecologic Cancers and Associated Diagnostic Procedures. JAMA. 2003;290:1739-1748.
- Shumaker SA, et al. Conjugated Equine Estrogens and Incidence of Probable Dementia and Mild Cognitive Impairment in Postmenopausal Women. JAMA. 2004;291:2947-2958.
- Jackson RD, et al. Effects of Conjugated Equine Estrogen on Risk of Fracture and BMD in Postmenopausal Women With Hysterectomy: Results From the Women’s Health Initiative Randomized Trial. J Bone Miner Res. 2006;21:817-828.
- Hendrix, SL, et al. Effects of Conjugated Equine Estrogen on Stroke in the Women’s Health Initiative. Circulation. 2006;113:2425-2434.
17. Patient Counseling Information
Advise the patient to read FDA-approved patient labeling (Patient Information and Instructions for Use).
Vaginal Bleeding
Inform women to report any vaginal bleeding to their healthcare provider as soon as possible [see Warnings and Precautions (5.2)].
Possible Serious Adverse Reactions with Estrogen-Alone Therapy
Inform postmenopausal women of possible serious adverse reactions of estrogen-alone therapy including cardiovascular disorders, malignant neoplasms, and possible dementia [see Warning and Precautions (5.1, 5.2, 5.3)].
Possible Less Serious but Common Adverse Reactions with Estrogen-Alone Therapy
Inform postmenopausal women of possible less serious but common adverse reactions of estrogen-alone therapy such as headaches, breast pain and tenderness, nausea and vomiting.
For all medical inquiries contact:
ACTAVIS
Medical Communications
Parsippany, NJ 07054
1-800-272-5525
Distributed By:
Actavis Pharma, Inc.
Parsippany, NJ 07054 USA
| ALORA
estradiol patch |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| ALORA
estradiol patch |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| ALORA
estradiol patch |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| ALORA
estradiol patch |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| Labeler - Actavis Pharma, Inc. (119723554) |




![Figure 3
Mean % Change from Baseline at 1 and 2 Years in the Bone Marrow Density of Non-Osteoporotic Women, Following Therapy with Alora, 0.025, 0.05, and 0.075 mg/day and Placebo [Completer and Intent-to-Treat Populations with Last Observation Carried Forward (LOCF)].](https://cdn.themeditary.com/images/2023/09/07/alora-06.webp)