Drug Detail:Androderm (Testosterone topical [ tes-tos-ter-one-top-i-kal ])
Drug Class: Androgens and anabolic steroids
Highlights of Prescribing Information
ANDRODERM® (testosterone transdermal system), for topical use CIII
Initial U.S. Approval: 1953
Recent Major Changes
Contraindications (4) 05/2020
Indications and Usage for Androderm
ANDRODERM is an androgen indicated for replacement therapy in males for conditions associated with a deficiency or absence of endogenous testosterone (1):
- Primary hypogonadism (congenital or acquired)
- Hypogonadotropic hypogonadism (congenital or acquired)
Limitations of use
- Safety and efficacy of ANDRODERM in men with “age-related hypogonadism” have not been established. (1)
- Safety and efficacy of ANDRODERM in males less than 18 years old have not been established. (1, 8.4)
Androderm Dosage and Administration
- Prior to initiating ANDRODERM confirm the diagnosis of hypogonadism by ensuring that serum testosterone has been measured in the morning on at least two separate days and that these concentrations are below the normal range (2.1).
- The recommended starting dose is one ANDRODERM 4 mg/day system (not two 2 mg/day systems) applied nightly for 24 hours, delivering approximately 4 mg of testosterone per day. (2.1)
- To ensure proper dosing, approximately 2 weeks after starting therapy, the early morning serum testosterone concentration should be measured following system application in the previous evening. (2.1, 12.3)
- Serum testosterone concentrations measured in the early morning outside the range of 400 - 930 ng/dL require increasing the daily dose to 6 mg (i.e., one 4 mg/day and one 2 mg/day system) or decreasing the daily dose to 2 mg (i.e., one 2 mg/day system), maintaining nightly application. (2.1)
- Patients currently maintained on ANDRODERM 2.5 mg/day systems applied once daily may be switched to ANDRODERM 2 mg/day systems applied once daily in the evening at the next scheduled dose. (2.1)
- Patients currently maintained on ANDRODERM 5 mg/day systems applied once daily may be switched to ANDRODERM 4 mg/day systems applied once daily in the evening at the next scheduled dose. (2.1)
- Patients currently maintained on ANDRODERM 7.5 mg (2.5 mg/day and 5 mg/day systems) applied once daily may be switched to ANDRODERM 6 mg (2 mg/day and 4 mg/day systems) applied once daily in the evening at the next scheduled dose. (2.1)
- To ensure proper dosing, approximately 2 weeks after switching therapy an early morning serum testosterone concentration should be measured following system application the previous evening. (2.1, 12.3)
Dosage Forms and Strengths
Transdermal system: 2 mg/day and 4 mg/day. (3)
Contraindications
- Men with carcinoma of the breast or known or suspected carcinoma of the prostate. (4, 5.1)
- Women who are pregnant. Testosterone may cause fetal harm. (4, 5.6, 8.1)
Warnings and Precautions
- Monitor patients with benign prostatic hyperplasia (BPH) for worsening of signs and symptoms of BPH. (5.1)
- Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE) have been reported in patients using testosterone products. Evaluate patients with signs or symptoms consistent with DVT or PE. (5.3)
- Some postmarketing studies have shown an increased risk of myocardial infarction and stroke associated with the use of testosterone replacement therapy. (5.4)
- Avoid exposure of women to ANDRODERM. (5.6)
- Exogenous administration of testosterone may lead to azoospermia. (5.6)
- Edema with or without congestive heart failure, may be a complication in patients with pre-existing cardiac, renal, or hepatic disease. (5.9)
- Sleep apnea may occur in those with risk factors. (5.11)
- Monitor serum testosterone, prostate specific antigen (PSA), liver function, lipid concentrations, hematocrit and hemoglobin periodically. (5.1, 5.2, 5.7, 5.12)
- Skin burns have been reported at the application site in patients wearing an aluminized transdermal system during a magnetic resonance imaging scan (MRI). Because ANDRODERM contains aluminum, it is recommended to remove the system before undergoing an MRI. (5.15)
Adverse Reactions/Side Effects
The most common adverse reactions (incidence > 3%) are application site reactions, and back pain. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Allergan at 1-800-678-1605 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Androgens may decrease blood glucose and insulin requirement in diabetic patients. (7.1)
- Changes in anticoagulant activity may be seen with androgens. More frequent monitoring of International Normalized Ratio (INR) and prothrombin time is recommended. (7.2)
- Use of testosterone with adrenocorticotropic hormone (ACTH) or corticosteroids may result in increased fluid retention. Use with caution, particularly in patients with cardiac, renal, or hepatic disease. (7.3)
Use In Specific Populations
There are insufficient long-term safety data in geriatric patients using ANDRODERM to assess the potential risks of cardiovascular disease and prostate cancer. (8.5)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 5/2020
Related/similar drugs
testosterone, AndroGel, Depo-Testosterone, Xyosted, HCG, PregnylFull Prescribing Information
1. Indications and Usage for Androderm
ANDRODERM is indicated for replacement therapy in adult males for conditions associated with a deficiency or absence of endogenous testosterone.
-
Primary hypogonadism (congenital or acquired): testicular failure due to conditions such as cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchiectomy, Klinefelter Syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. These men usually have low serum testosterone concentrations and gonadotropins (FSH, LH) above the normal range.
- Hypogonadotropic hypogonadism (congenital or acquired): gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. These men have low testosterone serum concentrations but have gonadotropins in the normal or low range.
Limitations of use
- Safety and efficacy of ANDRODERM in men with “age-related hypogonadism” (also referred to as “late-onset hypogonadism”) have not been established.
- Safety and efficacy of ANDRODERM in males less than 18 years old have not been established [see Use in Specific Populations (8.4)].
2. Androderm Dosage and Administration
2.1 Dosing Information
Prior to initiating ANDRODERM, confirm the diagnosis of hypogonadism by ensuring that serum testosterone concentrations have been measured in the morning on at least two separate days and that these serum testosterone concentrations are below the normal range.
The recommended starting dose is one ANDRODERM 4 mg/day system (not two 2 mg/day systems) applied nightly for 24 hours, delivering approximately 4 mg of testosterone per day. To ensure proper dosing, approximately 2 weeks after starting therapy, the early morning serum testosterone concentration should be measured following system application the previous evening. Serum concentrations outside the range of 400 - 930 ng/dL require increasing the daily dose to 6 mg (i.e., one 4 mg/day and one 2 mg/day system) or decreasing the daily dose to 2 mg (i.e., one 2 mg/day system), maintaining nightly application.
Patients currently maintained on ANDRODERM 2.5 mg/day, 5 mg/day, and 7.5 mg/day may be switched to the 2 mg/day, 4 mg/day, and 6 mg/day dosage using the following schema:
- Patients using 2.5 mg daily may be switched to 2 mg/day systems at the next scheduled dose.
- Patients using 5 mg daily may be switched to 4 mg/day systems at the next scheduled dose.
- Patients using 7.5 mg daily may be switched to 6 mg (2 mg/day and 4 mg/day systems) at the next scheduled dose.
To ensure proper dosing, approximately 2 weeks after switching therapy, the early morning serum testosterone concentration should be measured following system application the previous evening.
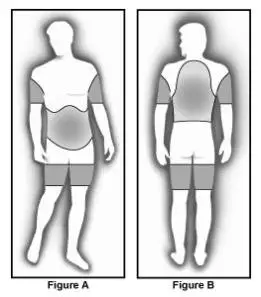
The adhesive side of the ANDRODERM system should be applied to a clean, dry area of the skin on the back, abdomen, upper arms, or thighs. Avoid application over bony prominences or on a part of the body that may be subject to prolonged pressure during sleep or sitting (e.g., the deltoid region of the upper arm, the greater trochanter of the femur, and the ischial tuberosity). DO NOT APPLY TO THE SCROTUM. The sites of application should be rotated, with an interval of 7 days between applications to the same site. The area selected should not be oily, damaged, or irritated.
The system should be applied immediately after opening the pouch and removing the protective release liner. The system should be pressed firmly in place, making sure there is good contact with the skin, especially around the edges.
The patient should avoid swimming, showering, or washing the administration site for a minimum of 3 hours after application [see Clinical Pharmacology (12.3)].
Mild skin irritation may be ameliorated by treatment of the affected skin with over-the-counter topical hydrocortisone cream applied after system removal. Applying a small amount of 0.1% triamcinolone acetonide cream to the skin under the central drug reservoir of the ANDRODERM system has been shown to reduce the incidence and severity of skin irritation.
4. Contraindications
- ANDRODERM is contraindicated in men with carcinoma of the breast or known or suspected carcinoma of the prostate [see Warnings and Precautions (5.1)].
- ANDRODERM is contraindicated in women who are pregnant. Testosterone can cause virilization of the female fetus when administered to a pregnant woman. If a pregnant woman is exposed to ANDRODERM, she should be apprised of the potential hazard to the fetus [see Use in Specific Populations (8.1)].
5. Warnings and Precautions
5.1 Worsening of Benign Prostatic Hyperplasia and Potential Risk of Prostate Cancer
- Monitor patients with benign prostatic hyperplasia (BPH) for worsening of signs and symptoms of BPH.
- Patients treated with androgens may be at increased risk for prostate cancer. Evaluate patients for prostate cancer prior to initiating treatment. It is appropriate to re-evaluate patients 3 to 6 months after initiation of treatment, and then in accordance with prostate cancer screening practices [see Contraindications (4)].
5.2 Polycythemia
Increases in hematocrit, reflective of increases in red blood cell mass, may require lowering or discontinuation of testosterone. Check hematocrit prior to initiating testosterone treatment. It is appropriate to re-evaluate the hematocrit 3 to 6 months after starting testosterone treatment, and then monitor annually. Discontinue testosterone therapy if the hematocrit becomes elevated. Testosterone therapy may be restarted when the hematocrit decreases to an acceptable level. An increase in red blood cell mass may increase the risk of thromboembolic events.
5.3 Venous Thromboembolism
There have been postmarketing reports of venous thromboembolic events, including deep vein thrombosis (DVT) and pulmonary embolism (PE), in patients using testosterone products such as ANDRODERM. Evaluate patients who report symptoms of pain, edema, warmth and erythema in the lower extremity for DVT and those who present with acute shortness of breath for PE. If a venous thromboembolic event is suspected, discontinue treatment with ANDRODERM and initiate appropriate workup and management [see Adverse Reactions (6.2)].
5.4 Cardiovascular Risk
Long term clinical safety trials have not been conducted to assess the cardiovascular outcomes of testosterone replacement therapy in men. To date, epidemiologic studies and randomized controlled trials have been inconclusive for determining the risk of major adverse cardiovascular events (MACE) such as non-fatal myocardial infarction, non-fatal stroke, and cardiovascular death, with the use of testosterone compared to non-use. Some studies, but not all, have reported an increased risk of MACE in association with use of testosterone replacement therapy in men. Patients should be informed of this possible risk when deciding whether to use or to continue to use ANDRODERM.
5.6 Use in Women
Due to lack of controlled studies in women and potential virilizing effects, ANDRODERM is not indicated for use in women [see Contraindications (4) and Use in Specific Populations (8.1, 8.3)].
5.7 Potential for Adverse Effects on Spermatogenesis
At large doses of exogenous androgens, including ANDRODERM, spermatogenesis may be suppressed through feedback inhibition of pituitary follicle-stimulating hormone (FSH) that could lead to adverse effects on semen parameters including reduction of sperm count.
5.9 Edema
Androgens, including ANDRODERM, may promote retention of sodium and water. Edema, with or without congestive heart failure, may be a serious complication in patients with pre-existing cardiac, renal, or hepatic disease [see Adverse Reactions (6)].
5.11 Sleep Apnea
The treatment of hypogonadal men with testosterone may potentiate sleep apnea in some patients, especially those with risk factors such as obesity and chronic lung disease.
6. Adverse Reactions/Side Effects
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Table 1 shows the adverse reactions that were reported by > 3% of 36 hypogonadal men who were treated with ANDRODERM 2 mg/day, 4 mg/day, or 6 mg/day for 28 days. Of note, all hypogonadal men studied had been stable users of topical testosterone replacement products prior to the study and there was no washout period between therapies. Furthermore, there was only one subject titrated to 6 mg/day and he withdrew from the study prematurely.
| Adverse Reaction | Overall
N = 36 % |
| Application site pruritus | 17 |
| Application site vesicles | 6 |
| Back pain | 6 |
Other less common adverse reactions reported by < 3% of patients included: application site erythema, application site exfoliation, chills, diarrhea, fatigue, gastroesophageal reflux disease, hemarthrosis, hematuria, headache, polyuria, and prostatitis. The overall incidence of application site reactions of any kind was 28% (10 subjects with 13 adverse reactions).
No serious adverse reactions to ANDRODERM 2 mg/day and 4 mg/day were reported during the clinical trial.
Table 2 shows the adverse reactions that were reported in > 3% of 122 patients in clinical studies with ANDRODERM dosage strengths of 2.5 mg/day, 5 mg/day, and 7.5 mg/day. The most common adverse reactions reported were application site reactions. Transient mild to moderate erythema was observed at the site of application in the majority of patients at some time during treatment. The overall incidence of application site reactions of any kind was 48% (59 subjects with 107 adverse reactions).
| Adverse Reaction | Overall
N = 122 % |
| Application site pruritus | 37 |
| Application site blistering | 12 |
| Application site erythema | 7 |
| Application site vesicles | 6 |
| Prostate abnormalities | 5 |
| Headache | 4 |
| Contact dermatitis to system | 4 |
| Application site burning | 3 |
| Application site induration | 3 |
| Depression | 3 |
The following reactions occurred in less than 3% of patients: rash, gastrointestinal bleeding, fatigue, body pain, pelvic pain, hypertension, peripheral vascular disease, increased appetite, accelerated growth, anxiety, confusion, decreased libido, paresthesia, thinking abnormalities, vertigo, acne, bullae at application site, mechanical irritation at application site, rash at application site, contamination of application site, prostate carcinoma, dysuria, hematuria, impotence, urinary incontinence, urinary tract infection, and testicular abnormalities.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of ANDRODERM. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Cardiovascular Disorders:
Myocardial infarction, stroke [see Warnings and Precautions (5.4)]
Vascular Disorders:
Venous thromboembolism [see Warnings and Precautions (5.3)]
7. Drug Interactions
7.1 Insulin
Changes in insulin sensitivity or glycemic control may occur in patients treated with androgens. In diabetic patients, the metabolic effects of androgens may decrease blood glucose and, therefore, insulin requirement.
7.2 Oral Anticoagulants
Changes in anticoagulant activity may be seen with androgens. More frequent monitoring of INR and prothrombin time is recommended in patients taking anticoagulants, especially at the initiation and termination of androgen therapy.
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
ANDRODERM is contraindicated in pregnant women. Testosterone is teratogenic and may cause fetal harm when administered to a pregnant woman based on data from animal studies and its mechanism of action [see Contraindications (4) and Clinical Pharmacology (12.1)]. Exposure of a female fetus to androgens may result in varying degrees of virilization. In animal developmental studies, exposure to testosterone in utero resulted in hormonal and behavioral changes in offspring and structural impairments of reproductive tissues in female and male offspring. These studies did not meet current standards for nonclinical development toxicity studies. Data
Animal Data
In developmental studies conducted in rats, rabbits, pigs, sheep and rhesus monkeys, pregnant animals received intramuscular injection of testosterone during the period of organogenesis. Testosterone treatment at doses that were comparable to those used for testosterone replacement therapy resulted in structural impairments in both female and male offspring. Structural impairments observed in females included increased ano-genital distance, phallus development, empty scrotum, no external vagina, intrauterine growth retardation, reduced ovarian reserve, and increased ovarian follicular recruitment. Structural impairments seen in male offspring included increased testicular weight, larger seminal tubular lumen diameter, and higher frequency of occluded tubule lumen. Increased pituitary weight was seen in both sexes.
Testosterone exposure in utero also resulted in hormonal and behavioral changes in offspring. Hypertension was observed in pregnant female rats and their offspring exposed to doses approximately twice those used for testosterone replacement therapy.
8.3 Females and Males of Reproductive Potential
Infertility
Testicular abnormalities have been identified during use of ANDRODERM [see Adverse Reactions (6.1].
During treatment with large doses of exogenous androgens, including ANDRODERM, spermatogenesis may be suppressed through feedback inhibition of the hypothalamic-pituitary-testicular axis [see Warnings and Precautions (5.7)]. Reduced fertility is observed in some men taking testosterone replacement therapy. Testicular atrophy, subfertility, and infertility have also been reported in men who abuse anabolic androgenic steroids [see Drug Abuse and Dependence (9.2)]. With either type of use, the impact on fertility may be irreversible.
8.4 Pediatric Use
Safety and efficacy of ANDRODERM have not been established in males <18 years of age. Improper use may result in acceleration of bone age and premature closure of epiphyses.
8.5 Geriatric Use
There have not been sufficient numbers of geriatric patients involved in controlled clinical studies utilizing ANDRODERM to determine whether efficacy in those over 65 years of age differs from younger patients. Additionally, there are insufficient long-term safety data in geriatric patients utilizing ANDRODERM to assess a potential incremental risk of cardiovascular disease and prostate cancer.
9. Drug Abuse and Dependence
9.2 Abuse
Drug abuse is intentional non-therapeutic use of a drug, even once, for its rewarding psychological and physiological effects. Abuse and misuse of testosterone are seen in male and female adults and adolescents. Testosterone, often in combination with other anabolic androgenic steroids (AAS), and not obtained by prescription through a pharmacy, may be abused by athletes and bodybuilders. There have been reports of misuse by men taking higher doses of legally obtained testosterone than prescribed and continuing testosterone despite adverse events or against medical advice.
Abuse-Related Adverse Reactions
Serious adverse reactions have been reported in individuals who abuse anabolic androgenic steroids and include cardiac arrest, myocardial infarction, hypertrophic cardiomyopathy, congestive heart failure, cerebrovascular accident, hepatotoxicity, and serious psychiatric manifestations, including major depression, mania, paranoia, psychosis, delusions, hallucinations, hostility and aggression.
The following adverse reactions have also been reported in men: transient ischemic attacks, convulsions, hypomania, irritability, dyslipidemias, testicular atrophy, subfertility, and infertility.
The following additional adverse reactions have been reported in male and female adolescents: premature closure of bony epiphyses with termination of growth, and precocious puberty.
Because these reactions are reported voluntarily from a population of uncertain size and may include abuse of other agents, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
11. Androderm Description
ANDRODERM (testosterone transdermal system) is designed to deliver testosterone continuously for 24 hours following application to intact, non-scrotal skin (e.g., back, abdomen, thighs, upper arms).
Two strengths of ANDRODERM are available that deliver approximately 2 mg or 4 mg of testosterone per day.
ANDRODERM has a central drug delivery reservoir surrounded by a peripheral adhesive area. The ANDRODERM 2 mg/day system has a total contact surface area of 32 cm2 with a 6.0 cm2 central drug delivery reservoir containing 9.7 mg testosterone USP, dissolved in an alcohol-based gel. The ANDRODERM 4 mg/day system has a total contact surface area of 39 cm2 with a 12.0 cm2 central drug delivery reservoir containing 19.5 mg testosterone USP, dissolved in an alcohol-based gel. Testosterone USP is a white, or creamy white crystalline powder or crystals chemically described as 17ß-hydroxyandrost-4-en-3-one.
The ANDRODERM systems have six components as shown in Figure 1. Proceeding from the top toward the surface attached to the skin, the system is composed of (1) metallized polyester/Surlyn® (ethylene-methacrylic acid copolymer)/ethylene vinyl acetate backing film with alcohol resistant ink, (2) a drug reservoir of testosterone USP, alcohol USP, glycerin USP, glycerol monooleate, methyl laurate, sodium hydroxide NF, to adjust pH, and purified water USP, gelled with carbomer copolymer Type B NF, (3) a permeable polyethylene microporous membrane, and (4) a peripheral layer of acrylic adhesive surrounding the central, active drug delivery area of the system. Prior to opening of the system and application to the skin, the central delivery surface of the system is sealed with a peelable laminate disc (5) composed of a five-layer laminate containing polyester/polyesterurethane adhesive/aluminum foil/polyester-urethane adhesive/polyethylene. The disc is attached to and removed with the release liner (6), a silicone-coated polyester film, which is removed before the system can be used.
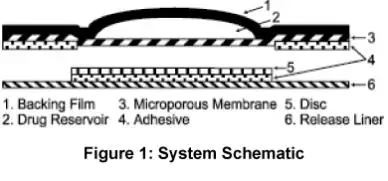
The active ingredient in the system is testosterone. The remaining components of the system are pharmacologically inactive.
12. Androderm - Clinical Pharmacology
12.1 Mechanism of Action
Endogenous androgens, including testosterone and dihydrotestosterone (DHT), are responsible for the normal growth and development of the male sex organs and for maintenance of secondary sex characteristics. These effects include the growth and maturation of prostate, seminal vesicles, penis and scrotum; the development of male hair distribution, such as facial, pubic, chest and axillary hair; laryngeal enlargement; vocal cord thickening; and alterations in body musculature and fat distribution. Testosterone and DHT are necessary for the normal development of secondary sex characteristics.
Male hypogonadism, a clinical syndrome resulting from insufficient secretion of testosterone, has two main etiologies. Primary hypogonadism is caused by defects of the gonads, such as Klinefelter Syndrome or Leydig cell aplasia, whereas secondary hypogonadism is the failure of the hypothalamus (or pituitary) to produce sufficient gonadotropins (FSH, LH).
12.3 Pharmacokinetics
Absorption
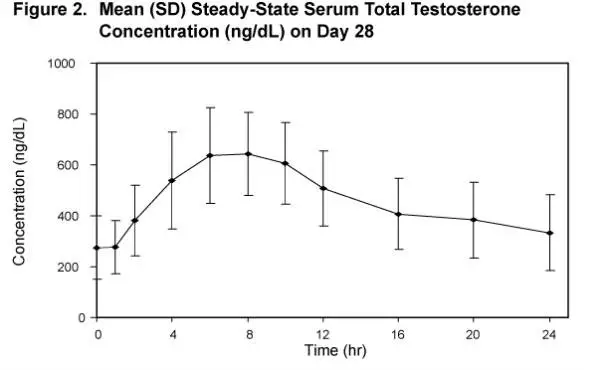
ANDRODERM delivers physiologic amounts of testosterone, producing circulating testosterone concentrations that approximate the normal concentration range (300 - 1030 ng/dL) seen in healthy men. ANDRODERM provides a continuous daily dose of testosterone in a self-contained transdermal system. Following ANDRODERM application, testosterone is continuously absorbed during the 24-hour dosing period with a median (range) Tmax of 8 (4-12) hours.
Distribution
Circulating testosterone is primarily bound in the serum to sex hormone-binding globulin (SHBG) and albumin. Approximately 40% of testosterone in plasma is bound to SHBG, 2% remains unbound (free) and the rest is bound to albumin and other proteins.
Metabolism
Testosterone is metabolized to various 17-keto steroids through two different pathways. The major active metabolites of testosterone are estradiol and dihydrotestosterone (DHT).
During steady-state pharmacokinetic studies in hypogonadal men treated with ANDRODERM, the average DHT:T and E2:T ratios were approximately 1:10 and 1:200, respectively.
Excretion
There is considerable variation in the half-life of testosterone as reported in the literature, ranging from 10 to 100 minutes. About 90% of a dose of testosterone given intramuscularly is excreted in the urine as glucuronic and sulfuric acid conjugates of testosterone and its metabolites; about 6% of a dose is excreted in the feces, mostly in the unconjugated form. Inactivation of testosterone occurs primarily in the liver.
Upon removal of the ANDRODERM systems, serum testosterone concentrations decrease with an apparent half-life of approximately 70 minutes. Hypogonadal concentrations are reached within 24 hours following system removal. There is no accumulation of testosterone during continuous treatment.
Effect of Showering
In a two-way crossover study, the effects of showering on the pharmacokinetics of total testosterone following a single application of ANDRODERM 4 mg/day were assessed in 16 hypogonadal males. Showering 3 hours after application of ANDRODERM increased Cavg by 0.5% and decreased Cmax by 0.4% respectively, as compared to not showering. The systemic exposure to ANDRODERM was similar following applications with or without showering 3 hours after application.
PATIENT INFORMATION
ANDRODERM® (an-dro-derm) CIII
(testosterone transdermal system)
for topical use
Read this Patient Information before you start taking ANDRODERM and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or your treatment.
What is ANDRODERM?
ANDRODERM is a prescription medicine that contains testosterone. ANDRODERM is used to treat adult males who have low or no testosterone due to certain medical conditions.
Your healthcare provider will test your blood for testosterone before you start and while you are taking ANDRODERM.
It is not known if ANDRODERM is safe or effective to treat men who have low testosterone due to aging.
It is not known if ANDRODERM is safe and effective in children younger than 18 years old. Improper use of ANDRODERM may affect bone growth in children.
ANDRODERM is a controlled substance (CIII) because it contains testosterone that can be a target for people who abuse prescription medicines. Keep your ANDRODERM in a safe place to protect it. Never give your ANDRODERM to anyone else, even if they have the same symptoms you have. Selling or giving away this medicine may harm others and it is against the law.
ANDRODERM is not meant for use by women.
Who should not use ANDRODERM?
Do not use ANDRODERM if you:
- are a man who has breast cancer
- have or might have prostate cancer
- are pregnant ANDRODERM may harm your unborn baby.
Talk to your healthcare provider before taking this medicine if you have any of the above conditions.
What should I tell my healthcare provider before using ANDRODERM?
Before you use ANDRODERM, tell your healthcare provider if you:
- have breast cancer
- have or might have prostate cancer
- have urinary problems due to an enlarged prostate
- have heart problems
- have kidney or liver problems
- have problems breathing while you sleep (sleep apnea)
- have diabetes
- have any other medical conditions
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements.
Using ANDRODERM with other medicines can affect each other. Especially, tell your healthcare provider if you take:
- insulin
- medicines that decrease blood clotting
- corticosteroids
Know the medicines you take. Ask your healthcare provider or pharmacist for a list of all your medicines if you are not sure. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine.
How should I use ANDRODERM?
- It is important that you apply ANDRODERM exactly as your healthcare provider tells you to.
- ANDRODERM patches come in 2 different doses and different patch sizes.
- Your healthcare provider will tell you how many ANDRODERM patches to apply and when to apply them.
- Your healthcare provider may change your ANDRODERM dose. Do not change your ANDRODERM dose without talking with your healthcare provider.
- Apply ANDRODERM at about the same time each night.
- Wait 3 hours before showering, bathing, or swimming. This will ensure that the greatest amount of ANDRODERM is absorbed into your system.
- ANDRODERM does not need to be removed during sex or while you take a shower or bath.
- Strenuous exercise or excessive perspiration may loosen your ANDRODERM patch or cause it to fall off.
- If your ANDRODERM patch becomes loose, smooth it down again by rubbing your finger firmly around the edges. Do not tape ANDRODERM patches to your skin.
○ If your ANDRODERM patch falls off before noon, put on a new ANDRODERM patch and wear it until you put on a new ANDRODERM patch at your regular time.
○ If your ANDRODERM patch falls off after noon, do not put on a new one. Wait and apply your ANDRODERM patch at your regular time.
- You should change your ANDRODERM patch every 24 hours. You should remove the old patch before applying the new one.
- You should change (rotate) your ANDRODERM application site every day. Do not use a site that you have used before for at least 7 days.
- Skin redness may happen on the skin where your ANDRODERM patch was removed. If your skin redness does not go away, talk to your healthcare provider. Your healthcare provider may tell you to use an over-the-counter hydrocortisone cream on your red skin.
- Patches that have aluminum in them can cause skin burns at the patch site during a magnetic resonance imaging scan (MRI). Because ANDRODERM contains aluminum, you should take off your ANDRODERM patch before you have an MRI.
- Do not use an ANDRODERM patch if the pouch seal is broken or the patch is cut, damaged, or changed in any way. Throw it away and get a new one.
Applying ANDRODERM:
- Before applying ANDRODERM, make sure that the application area is clean, dry, and there is no broken skin.
- Avoid areas of skin that are oily, perspire heavily, or are covered with hair, since ANDRODERM may not stick well to these areas.
- ANDRODERM is to be applied to your back, stomach area (abdomen), upper arms, or thighs only (See Figure A and Figure B). Do not apply ANDRODERM to any other parts of your body such as your scrotum, buttocks or over a bony area.
 |
|
| 1. Open the foil pouch. Tear along the edge and remove the patch from the pouch (See Figure C). Do not cut the ANDRODERM protective pouch. |  |
| 2. Remove the protective plastic liner and silver disc from the patch. Hold on to the tabs on the patch and the protective plastic liner and gently pull the two apart to remove the plastic liner and silver disc from the patch (See Figure D).
This will expose the adhesive and central reservoir area on the patch (See Figure E).
|  |
| 3. Check the protective plastic liner. You should not see any glue (adhesive) sticking to the liner. Do not use the ANDRODERM patch if you see any adhesive sticking to the liner. Throw away the ANDRODERM patch and get a new one. Throw away the clear plastic liner and silver disc. | |
| 4. Apply the patch. Apply the patch right away after you remove the patch from the protective pouch and remove the plastic liner. Place the patch flat on the skin with the sticky side down and firmly press around the edges. Make sure that the patch sticks well to the skin. | |
What are the possible side effects of ANDRODERM?
ANDRODERM can cause serious side effects including:
-
If you already have an enlargement of your prostate gland your signs and symptoms may get worse while using ANDRODERM. This can include:
○ increased urination at night
○ trouble starting your urine stream
○ having to pass urine many times during the day
○ having an urge that you have to go to the bathroom right away
○ having a urine accident
○ being unable to pass urine or weak urine flow
-
Possible increased risk of prostate cancer. Your healthcare provider should check you for prostate cancer or any other prostate problems before you start and while you use ANDRODERM.
-
Blood clots in the legs or lungs. Signs and symptoms of a blood clot in your leg can include leg pain, swelling or redness. Signs and symptoms of a blood clot in your lungs can include difficulty breathing or chest pain. This can include pain, swelling or redness of your legs.
- Possible increased risk of heart attack or stroke.
-
In large doses ANDRODERM may lower your sperm count.
-
Swelling of your ankles, feet, or body, with or without heart failure.
-
Enlarged or painful breasts.
- Problems breathing while you sleep (sleep apnea).
Call your healthcare provider right away if you have any of the serious side effects listed above.
The most common side effects of ANDRODERM include:
- skin redness, irritation, burning, or blisters where ANDRODERM is applied
- back pain
- depression
- headache
- prostate abnormalities
Other side effects include more erections than are normal for you or erections that last a long time.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of ANDRODERM. For more information, ask your healthcare provider or pharmacist.
Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store ANDRODERM?
- Keep ANDRODERM at room temperature between 68°F to 77°F (20°C to 25°C).
- Keep ANDRODERM in its sealed protective foil pouch until you are ready to use it. Do not remove an ANDRODERM patch from the pouch until you are ready to use it.
- Safely throw away your used ANDRODERM patch. Fold your used ANDRODERM patch in half so that the sticky sides stick together. Throw away your used ANDRODERM patch in the household trash.
- Be careful to prevent accidental exposure of ANDRODERM to children or pets.
General information about the safe and effective use of ANDRODERM
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use ANDRODERM for a condition for which it was not prescribed. Do not give ANDRODERM to other people, even if they have the same symptoms you have. It may harm them.
This Patient Information leaflet summarizes the most important information about ANDRODERM. If you would like more information, talk to your healthcare provider. You can ask your pharmacist or healthcare provider for information about ANDRODERM that is written for health professionals.
For more information, go to www.androderm.com or call 1-800-678-1605. If you have questions or concerns about your ANDRODERM treatment, ask your healthcare provider or pharmacist.
What are the ingredients in ANDRODERM?
Active ingredient: testosterone
Inactive ingredients:
-
Backing Film: Metallized polyester/Surlyn® (ethylene-methacrylic acid copolymer)/ethylene vinyl acetate backing film with alcohol resistant ink
-
Drug Reservoir: Testosterone USP, alcohol USP, glycerin USP, glycerol monooleate, methyl laurate, sodium hydroxide NF, purified water USP, gelled with carbomer copolymer Type B NF
-
Microporous Membrane: a permeable polyethylene microporous membrane
-
Adhesive: a peripheral layer of acrylic adhesive surrounding the central, active drug delivery area of the system
-
Disc: a five-layer laminate containing polyester/polyesturethane adhesive/aluminum foil/polyester-urethane adhesive/polyethylene
- Release Liner: a silicone-coated polyester film, which is removed before the system can be used
For all medical inquiries contact:
Allergan
Medical Communications
1-800-678-1605
Distributed by: Allergan USA, Inc. Madison, NJ 07940
This Patient Information has been approved by the U.S. Food and Drug Administration
ANDRODERM® is a registered trademark of Allergan Sales, LLC.
© 2020 Allergan.
All rights reserved.
Allergan® and its design are trademarks of Allergan, Inc.
All trademarks are the property of their respective owners.
Content Updated: 05/2020
v1.0PPI5990
| ANDRODERM
testosterone patch |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| ANDRODERM
testosterone patch |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| Labeler - Allergan, Inc. (144796497) |