Drug Detail:Anthrax immune globulin iv (human) (monograph) (Anthrasil)
Drug Class:
Highlights of Prescribing Information
ANTHRASIL [Anthrax Immune Globulin Intravenous (Human)], sterile solution for infusion
Initial U.S. Approval: 2015
WARNING: INTERACTIONS WITH GLUCOSE MONITORING SYSTEMS AND THROMBOSIS
See full prescribing information for complete boxed warning.
• Maltose in immune globulin products, including ANTHRASIL, may give falsely high blood glucose levels with some blood point-of-care glucose testing systems (for example those based on the GDH-PQQ or glucose-dye-oxidoreductase methods) resulting in inappropriate administration of insulin and life-threatening hypoglycemia. To avoid interference by maltose contained in ANTHRASIL, perform blood glucose measurements in patients receiving ANTHRASIL with a glucose-specific method (monitor and test strips).
• Thrombosis may occur with immune globulin products, including ANTHRASIL. Risk factors may include advanced age, prolonged immobilization, hypercoagulable conditions, history of venous or arterial thrombosis, use of estrogens, indwelling vascular catheters, hyperviscosity and cardiovascular risk factors. Thrombosis may occur in the absence of known risk factors.
• For patients at risk of thrombosis, administer ANTHRASIL at the minimum infusion rate practicable. Ensure adequate hydration in patients before administration. Monitor for signs and symptoms of thrombosis and assess blood viscosity in patients at risk of hyperviscosity.
Indications and Usage for Anthrasil
ANTHRASIL is an Anthrax Immune Globulin Intravenous (Human) indicated for the treatment of inhalational anthrax in adult and pediatric patients in combination with appropriate antibacterial drugs (1).
The effectiveness of ANTHRASIL is based solely on efficacy studies conducted in animal models of inhalational anthrax.
Anthrasil Dosage and Administration
For intravenous use only.
Dosing of ANTHRASIL
|
Patient Group |
Dosea |
Starting Infusion Rate (first 30 min) |
Incremental Infusion Rate if Tolerated (every 30 min) |
Max Infusion Rate |
|
Adults (≥17 years) |
7 vials (420 units) |
0.5 mL/min |
1 mL/min |
2 mL/min |
|
Pediatric <1 year to ≤16 years |
1–7 vials (60–420 units) based on patient weight |
0.01 mL/kg/min (do not exceed the adult rate) |
0.02 mL/kg/min |
0.04 mL/kg/min (do not exceed the adult rate) |
|
a Select initial dose based on clinical severity; severe cases may warrant use of 14 vials (840 units) in adults and 2 to 14 vials (based on weight) in pediatric patients weighing >5 kg. |
||||
Adjust dose and consider redosing based on clinical severity and response to treatment (2.1)
Weight-based Pediatric Dose
| Body Weight (kg) | Vials per Dosea | Body Weight (kg) | Vials per Dose |
|---|---|---|---|
|
<5 |
1 |
25 to <35 |
4 |
|
<10 |
1 |
35 to <50 |
5 |
|
10 to <18 |
2 |
50 to <60 |
6 |
|
18 to <25 |
3 |
≥60 |
7 |
|
a Select initial dose based on clinical severity. Dose may be doubled for severe cases in patients >5 kg. |
|||
Administer ANTHRASIL by slow intravenous infusion using an infusion pump (maximum 2 mL per minute).
Dosage Forms and Strengths
Each single-use vial contains a minimum potency of ≥60 units by Toxin Neutralization Assay (TNA) (3).
Contraindications
- • History of anaphylactic or severe systemic reaction to human immune globulins ( 4 )
- • IgA deficiency with antibodies against IgA and a history of IgA hypersensitivity ( 4 )
Warnings and Precautions
- •Hypersensitivity reactions including anaphylaxis (5.1)
- •Interference with blood and urine glucose testing (5.2, 5.9)
- • Thrombosis may occur. Monitor patients at risk (5.3 )
- • Monitor renal function and urine output in patients at risk of acute renal dysfunction/failure (5.4 )
- • Infuse ANTHRASIL at the minimum rate practicable in patients at risk of thrombosis or renal failure (5.5 )
- • Monitor for clinical signs and symptoms of hemolysis and hemolytic anemia (5.6 )
- • Aseptic meningitis syndrome (AMS) (5.7 )
- • Transfusion-related Acute Lung Injury (TRALI)] (5.10)
- • Transmission of infectious agents from human plasma (5.11 )
Adverse Reactions/Side Effects
The most common adverse reactions to ANTHRASIL observed in >5% of healthy volunteers in clinical trials were headache, infusion site pain and swelling, nausea, and back pain (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Emergent BioSolutions Canada Inc. at 1-800-769-2304 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
[Enter highlight text here] (7)
Use In Specific Populations
- • Pregnancy: No human or animal data are available ( 8.1 )
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 5/2018
Full Prescribing Information
WARNING: INTERACTIONS WITH GLUCOSE MONITORING SYSTEMS AND THROMBOSIS
• Maltose in immune globulin products, including ANTHRASIL, may give falsely high blood glucose levels with some blood point-of-care glucose testing systems (for example those based on the GDH-PQQ or glucose-dye-oxidoreductase methods) resulting in inappropriate administration of insulin and life-threatening hypoglycemia. To avoid interference by maltose contained in ANTHRASIL, perform blood glucose measurements in patients receiving ANTHRASIL with a glucose-specific method (monitor and test strips).
• Thrombosis may occur with immune globulin products, including ANTHRASIL. Risk factors may include advanced age, prolonged immobilization, hypercoagulable conditions, history of venous or arterial thrombosis, use of estrogens, indwelling vascular catheters, hyperviscosity and cardiovascular risk factors. Thrombosis may occur in the absence of known risk factors.
• For patients at risk of thrombosis, administer ANTHRASIL at the minimum infusion rate practicable. Ensure adequate hydration in patients before administration. Monitor for signs and symptoms of thrombosis and assess blood viscosity in patients at risk of hyperviscosity.
1. Indications and Usage for Anthrasil
ANTHRASIL is an Anthrax Immune Globulin Intravenous (Human) indicated for the treatment of inhalational anthrax in adult and pediatric patients in combination with appropriate antibacterial drugs.
The effectiveness of ANTHRASIL is based solely on efficacy studies conducted in animal models of inhalational anthrax [See 13.2 Animal Toxicology and/or Pharmacology].
Limitations:
- •
- ANTHRASIL does not have direct antibacterial activity.
- •
- ANTHRASIL does not cross the blood-brain barrier and does not prevent or treat meningitis.
- •
- There have been no studies of ANTHRASIL in the pediatric, geriatric, or obese populations.
2. Anthrasil Dosage and Administration
For intravenous use only.
2.1 Dose
| Patient Group | Dosea | Starting Infusion Rate (first 30 minutes) | Incremental Infusion Rate if Tolerated (every 30 minutes) | Maximum Infusion Rate |
|---|---|---|---|---|
|
Adults ≥17 years |
7 vials (420 units) |
0.5 mL/min |
1 mL/min |
2 mL/min |
|
Pediatric <1 year to ≤16 years |
1–7 vials (60–420 units) based on patient weight |
0.01 mL/kg/min (do not exceed the adult rate) |
0.02 mL/kg/min |
0.04 mL/kg/min (do not exceed the adult rate) |
|
a Select initial dose based on clinical severity; severe cases may warrant use of 14 vials (840 units) in adults and 2 to 14 vials (based on weight) in pediatric patients weighing >5 kg. |
||||
| Body Weight (kg) | Number of ANTHRASIL Vials per Doseb |
|---|---|
|
<5 |
1 |
|
<10 |
1 |
|
10 to <18 |
2 |
|
18 to <25 |
3 |
|
25 to <35 |
4 |
|
35 to <50 |
5 |
|
50 to <60 |
6 |
|
≥60 |
7 |
|
a The pediatric dosing is derived from allometric scaling based on observed adult exposure to ANTHRASIL at 420 units by Toxin Neutralization Assay (TNA) dose. |
|
|
b Select initial dose based on clinical severity. Dose may be doubled for severe cases in patients >5 kg. |
|
The initial dose of ANTHRASIL for the treatment of inhalational anthrax in adults in combination with appropriate antimicrobial therapy is 420 units (seven vials). Data in animal models suggest that administration of higher doses may result in improved survival [See 13.2 Animal Toxicology and/or Pharmacology]. An initial dose of 840 units (14 vials) may be considered, depending on the clinical status of the patient.
Depending on the severity of symptoms and the response to treatment, consider an initial dose of 840 units (14 vials) and repeat dosing especially in patients experiencing substantial hemorrhage as reflected in large transfusion requirements, patients with significant compartmental fluid losses such as from large volume and/or repeated therapeutic thoracentesis and/or abdominal paracentesis, and in patients whose own immune response may be impaired/delayed. Take the magnitude of ongoing blood and fluid losses and the clinical status of the patient into account in determining the time interval between doses when repeat doses are administered. Repeated dosing and single doses greater than 840 units in humans have not been studied. Without substantially delaying therapy, give consideration to performing therapeutic thoracentesis and/or abdominal paracentesis as indicated prior to or concurrently with administration of ANTHRASIL.
2.2 Preparation and Administration
- Each vial of ANTHRASIL has a minimum potency of ≥60 units per vial [See 3 DOSAGE FORMS AND STRENGTHS].
- 1.
- Bring ANTHRASIL vials to room temperature.
- •
- Thaw frozen vials rapidly for immediate use by placing at room temperature for one hour followed by a water bath at 37°C (98.6°F) until thawed.
- •
- Alternatively, thaw vials by placing the required number of vials in a refrigerator at 2 to 8°C (36 to 46°F) until the vials are thawed (approximately 14 hours).
- •
- Do not thaw in a microwave oven. Do not refreeze vials.
- •
- Bring thawed vials to room temperature by letting sit on a bench for a few minutes prior to infusion.
- 2.
- Inspect vials to ensure the product is fully thawed and free from discoloration and particulate matter. The solution should be clear or slightly opalescent. Do not use solutions that are cloudy, turbid or have particulates.
- 3.
- Inspect vials to ensure there is no damage to the seal or vial. If damaged, do not use and contact the manufacturer.
- 4.
- Gently swirl upright vials by hand to ensure uniformity. Do not shake the vial during preparation to avoid foaming.
- 5.
- Follow the steps below to prepare the ANTHRASIL infusion bag:
- •
- Remove the protective caps from the product vials.
- •
- Wipe the exposed central portion of the rubber stopper with an isopropyl alcohol swab.
- •
- Withdraw the vial contents of ANTHRASIL into a syringe, aseptically transfer into an appropriately sized intravenous bag and label with the volume to be infused.
- •
- No further dilution is required.
- •
- Once punctured, use the vial contents to prepare the infusion bag and administer as soon as possible. ANTHRASIL contains no preservative.
- 6.
- Administer in an intravenous line with constant infusion pump. Use of an in-line filter is optional.
- 7.
- If adverse reactions occur, such as flushing, headache, nausea, changes in pulse rate or blood pressure, slow the rate of infusion or temporarily stop the infusion.
- ANTHRASIL vials are for single use only. Discard any unused portion.
3. Dosage Forms and Strengths
Each vial of ANTHRASIL contains a minimum potency of ≥60 units per vial.
4. Contraindications
- •
- ANTHRASIL is contraindicated in individuals with a history of anaphylaxis or prior severe systemic reaction associated with the parenteral administration of this or other human immune globulin preparations.
- •
- ANTHRASIL is contraindicated in IgA-deficient patients with antibodies against IgA and a history of IgA hypersensitivity, as it contains trace amounts of IgA (less than or equal to 40 mcg per mL) [see 5.1 Hypersensitivity Reactions].
5. Warnings and Precautions
5.1 Hypersensitivity Reactions
Hypersensitivity reactions may occur with ANTHRASIL.
Administer ANTHRASIL in a setting where appropriate equipment, medication (including epinephrine) and personnel trained in the management of hypersensitivity, anaphylaxis and shock are available.
Monitor all patients for signs and symptoms of acute allergic reactions (e.g. urticaria, pruritus, erythema, angioedema, bronchospasm with wheezing or cough, stridor, laryngeal edema, hypotension, tachycardia) during and following the ANTHRASIL infusion. In case of severe hypersensitivity reactions, discontinue the administration of ANTHRASIL immediately and administer appropriate emergency care.
ANTHRASIL contains trace amounts of IgA (less than or equal to 40 mcg per mL). Patients with known antibodies to IgA may have greater risk of developing severe hypersensitivity and anaphylactic reactions. ANTHRASIL is contraindicated in patients with antibodies against IgA and a history of hypersensitivity reaction [See 4 CONTRAINDICATIONS].
5.2 Interference with Blood Glucose Testing
ANTHRASIL contains maltose. Maltose has been shown to give falsely high blood glucose levels in certain types of blood glucose testing systems (for example, by systems based on glucose dehydrogenase pyrroloquinolinequinone (GDH‑PQQ) or glucose‑dye-oxidoreductase methods). Due to the potential for falsely elevated glucose readings (or falsely normal glucose readings when hypoglycemia is present), only use testing systems that are glucose‑specific to test or monitor blood glucose levels in patients receiving ANTHRASIL.
Review the product information of the blood glucose testing system, including that of the test strips, to determine if the system is appropriate for use with maltose-containing parenteral products. If any uncertainty exists, contact the manufacturer of the testing system to determine if the system is appropriate for use with maltose-containing parenteral products.
5.3 Thrombosis
Thrombosis may occur following treatment with immune globulin products, including ANTHRASIL [See BOXED WARNING]. Risk factors include cardiovascular risk factors, advanced age, impaired cardiac output, hypercoagulable disorders, prolonged periods of immobilization, history of arterial or venous thrombosis, estrogen use, indwelling central vascular catheters, and/or known or suspected hyperviscosity. Thrombosis may occur in the absence of known risk factors. Weigh the potential risks and benefits of ANTHRASIL against those of alternative therapies for all patients for whom ANTHRASIL administration is being considered.
Because of the potentially increased risk of thrombosis, consider baseline assessment of blood viscosity in patients at risk for hyperviscosity, including those with cryoglobulins, fasting chylomicronemia/markedly high triacylglycerols (triglycerides), or monoclonal gammopathies.
In patients with risk factors where the benefits of ANTHRASIL administration out-weigh the potential risks of thrombosis, administer ANTHRASIL at the minimum rate of infusion practicable. Ensure adequate hydration in patients before administration. Monitor for signs and symptoms of thrombosis.
5.4 Acute Renal Dysfunction/Failure
Acute renal dysfunction, acute renal failure, osmotic nephropathy, acute tubular necrosis, proximal tubular nephropathy, and death may occur upon use of immune globulin intravenous products, including ANTHRASIL. Use ANTHRASIL with caution in patients with any degree of pre-existing renal insufficiency and in patients at risk of developing renal insufficiency (including, but not limited to those with diabetes mellitus, age greater than 65 years, volume depletion, paraproteinemia, sepsis, and patients receiving known nephrotoxic drugs), administering at the minimum rate of infusion practicable. Ensure that patients are not volume depleted before ANTHRASIL infusion. Do not exceed the recommended infusion rate, and follow the infusion schedule closely. Periodic monitoring of renal function and urine output is important in patients judged to be at increased risk of developing acute renal failure. Assess renal function, including measurement of blood urea nitrogen (BUN) and serum creatinine, before the initial infusion of ANTHRASIL and at appropriate intervals thereafter. If renal function deteriorates, consider discontinuing ANTHRASIL.
Most cases of renal insufficiency following administration of immune globulin products have occurred in patients receiving total doses containing 400 mg per kg of sucrose or greater. ANTHRASIL does not contain sucrose.
5.5 Infusion Rate Precautions
Adverse reactions (such as chills, fever, headache, nausea and vomiting) may be related to the rate of infusion. Follow closely the recommended infusion rate given under 2.1 Dose. Closely monitor and carefully observe patients and their vital signs for any symptoms throughout the infusion period and immediately following an infusion.
5.6 Hemolysis
Hemolytic anemia and hemolysis may develop subsequent to ANTHRASIL administration. ANTHRASIL may contain blood group antibodies that may act as hemolysins and induce in vivo coating of red blood cells with immune globulin, causing a positive direct antiglobulin reaction and hemolysis. Acute hemolysis, including intravascular hemolysis, has been reported following immune globulin administration and delayed hemolytic anemia can develop due to enhanced red blood cell sequestration. Severe hemolysis may lead to renal dysfunction/failure.
The following risk factors may be associated with the development of hemolysis: high doses (e.g., >2 g per kg), given either as a single administration or divided over several days, and non-O blood group (1). Other individual patient factors, such as an underlying inflammatory state (as may be reflected by, for example, elevated C-reactive protein or erythrocyte sedimentation rate), have been hypothesized to increase the risk of hemolysis (2), but their role is uncertain.
Monitor ANTHRASIL recipients for clinical signs and symptoms of hemolysis. Consider appropriate laboratory testing in higher risk patients, including measurement of hemoglobin or hematocrit prior to infusion and within approximately 36 to 96 hours and again approximately seven to 10 days post infusion. If signs and/or symptoms of hemolysis or a significant drop in hemoglobin or hematocrit have been observed after infusion, perform additional confirmatory laboratory testing.
5.7 Aseptic Meningitis Symptom (AMS)
AMS may occur in association with administration of immune globulin products, including ANTHRASIL. AMS usually is associated with high total doses (>2 g per kg) and begins within several hours to two days following treatment. Discontinuation of treatment has resulted in remission of AMS within several days without sequelae.
AMS is characterized by the following symptoms and signs: severe headache, nuchal rigidity, drowsiness, fever, photophobia, painful eye movements, and nausea and vomiting. Cerebrospinal fluid (CSF) studies are frequently positive with pleocytosis up to several thousand cells per cubic millimeter, predominately from the granulocytic series, and with elevated protein levels up to several hundred mg per dL, but negative culture results. Conduct a detailed neurological examination in patients exhibiting such symptoms and signs, including CSF studies, to rule out other causes of meningitis (particularly anthrax meningitis).
5.8 Monitoring: Laboratory Tests
- •
- Consider periodic monitoring of renal function and urine output in patients judged to be at increased risk of developing acute renal failure. Assess renal function, including measurement of BUN and serum creatinine, before the initial infusion of ANTHRASIL and at appropriate intervals thereafter.
- •
- Because of the potentially increased risk of thrombosis, consider baseline assessment of blood viscosity in patients at risk for hyperviscosity, including those with cryoglobulins, fasting chylomicronemia/markedly high triacylglycerols (triglycerides), or monoclonal gammopathies.
- •
- If signs and/or symptoms of hemolysis are present after an infusion of ANTHRASIL, perform appropriate laboratory testing for confirmation.
If TRALI is suspected, perform appropriate tests for the presence of anti-HLA and anti-neutrophil antibodies in the product. TRALI may be managed using oxygen therapy with adequate ventilator support.
5.9 Interference with Laboratory Tests
ANTHRASIL contains maltose, which can be misinterpreted as glucose by certain types of blood glucose testing systems (for example, those based on the GDH-PQQ or glucose-dye-oxidoreductase methods). Due to the potential for falsely elevated glucose readings, use only testing systems that are glucose-specific to test or monitor blood glucose levels in patients receiving ANTHRASIL [See BOXED WARNING and 5.2 Interference with Blood Glucose Testing].
Antibodies present in ANTHRASIL may interfere with some serological tests. After administration of immune globulins like ANTHRASIL, a transitory increase of passively transferred antibodies in the patient’s blood may result in positive results in serological testing (e.g. Coombs’ test) [See 5.6 Hemolysis].
Urinalysis after ANTHRASIL administration may result in elevated glucose [See 6.1 Clinical Trials Experience]. As this is a known transient effect, testing should be repeated to determine if further action is warranted.
5.10 Transfusion-related Acute Lung Injury (TRALI)
Noncardiogenic pulmonary edema may occur in patients receiving immune globulin products, including ANTHRASIL. TRALI is characterized by severe respiratory distress, pulmonary edema, hypoxemia, normal left ventricular function, and fever and typically occurs within one to six hours after transfusion.
Monitor recipients for pulmonary adverse reactions. If TRALI is suspected, perform tests for the presence of anti-HLA and anti-neutrophil antibodies in the product.
5.11 Transmission of Infectious Agents from Human Plasma
Because ANTHRASIL is made from human plasma, it may carry a risk of transmitting blood-borne infectious agents, e.g., viruses, the variant Creutzfeld-Jakob disease (vCJD) agent, and, theoretically, the Creutzfeld-Jakob disease (CJD) agent. No cases of transmission of viral diseases, vCJD or CJD have been associated with the use of ANTHRASIL.
All infections thought to have been possibly transmitted by this product should be reported by the physician or other health care provider to Emergent BioSolutions Canada Inc. at 1-800-768-2304.
6. Adverse Reactions/Side Effects
The most common adverse reactions to ANTHRASIL observed in >5% of subjects in the healthy volunteer clinical trial were headache, infusion site pain, nausea, infusion site swelling, and back pain. The safety profile of the product may be different in patients with severe inhalational/systemic anthrax from that seen in the healthy volunteer trial. The incidence and/or severity of some adverse reactions to ANTHRASIL and other intravenous immune globulin products may be related to the total protein/polyclonal antibody load administered.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In a double blind, randomized, placebo-controlled study designed to assess the safety and pharmacokinetics of three doses of ANTHRASIL after a single intravenous infusion in healthy volunteers, 72 healthy adult subjects were randomized to receive a dose of 210, 420 or 840 units of ANTHRASIL by Toxin Neutralization Assay (TNA) (N=18/dosing group) or an equal volume of saline placebo (N=6/dosing group). A total of 54 healthy volunteers received one of the three ANTHRASIL doses while 18 healthy volunteers received a saline placebo.
A second stage of the study, designed only for additional safety assessment, was a randomized, open-label study in 20 healthy adult volunteers. Subjects were randomized to receive a dose of 840 units by TNA from one of two additional product lots (10 subjects per lot). There was no placebo group.
|
System Organ Class |
Preferred Term |
AIGIV Blinded Randomized Group (N=54) |
Placebo |
||||
|
No. of |
No. of |
% of |
No. of |
No. of |
% of |
||
|
Gastrointestinal disorders |
Nausea |
5 |
5 |
9.3 |
2 |
1 |
5.6 |
|
General disorders and administration site conditions |
Infusion site pain |
7 |
5 |
9.3 |
0 |
0 |
0.0 |
|
Infusion site swelling |
5 |
4 |
7.4 |
0 |
0 |
0.0 |
|
|
Musculoskeletal and connective tissue disorders |
Back pain |
2 |
2 |
3.7 |
1 |
1 |
5.6 |
|
Nervous system disorders |
Headache |
15 |
11 |
20.4 |
3 |
1 |
5.6 |
There were no serious adverse reactions reported in any of the AIGIV or saline placebo control groups in these studies. Non-serious adverse events and adverse reactions were more frequent in the active AIGIV dosage groups that in the subjects administered placebo.
Headache and back pain rates occurred in a dose-dependent fashion. Back pain was observed with 840 unit doses in five out of 74 subjects (6.8%).
Dose-related elevations in urine glucose were also noted transiently following infusion [See 5.9 Interference with Laboratory Testing].
Infusion of ANTHRASIL was stopped for four subjects due to adverse reactions. One subject was withdrawn due to chest discomfort, flushing, tachycardia and throat tightness.
Patient Experience
Nineteen adult patients with severe systemic anthrax have been dosed with single 420 unit doses of ANTHRASIL and antimicrobial therapy through expanded access use with the Centers for Disease Control and Prevention (CDC): three patients with inhalational anthrax, 15 patients with anthrax due to injection of anthrax-contaminated heroin and one patient with gastrointestinal anthrax.
A total of 16 serious adverse reactions that began within 72 hours of infusion were reported for eight out of 19 patients (42%) as follows: acute respiratory distress syndrome (n=2), pulmonary edema, pleural effusion, acute renal insufficiency/failure (n=4), coagulopathy, cardiac arrest/death (not otherwise specified, n=2), hypotension, ascites, metabolic acidosis, hyperkalemia, and edema/perhipheral edema.
Six deaths were reported including one patient with inhalational anthrax. The cause of death in three of these six expired patients, including the patient who expired with inhalational anthrax, was consistent with progression of anthrax disease or co-morbidities and the cause of death in the remaining three patients was not determined or available.
7. Drug Interactions
7.1 Ciprofloxacin and Levofloxacin
Based on animal studies, ANTHRASIL did not interfere with antibiotic therapy. Concomitant administration of ANTHRASIL with levofloxacin or ciprofloxacin in exposed rabbits and cynomolgus macaques, respectively, did not affect the efficacy of antibacterial therapy.
7.2 Live, Attenuated Vaccines
Immune globulin administration may impair the efficacy of live attenuated vaccines such as measles, rubella, mumps and varicella. Defer vaccination with live virus vaccines until approximately three months after administration of ANTHRASIL. Revaccinate people who received ANTHRASIL shortly after live virus vaccination three months after the administration of ANTHRASIL.
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
There are no human data to establish the presence or absence of ANTHRASIL associated risk.
8.2 Lactation
Risk Summary
There are no data to assess the presence or absence of ANTHRASIL in human milk, the effects on the breastfed child or the effects on milk production/excretion.
8.4 Pediatric Use
Safety and effectiveness of ANTHRASIL in the pediatric population (≤16 yrs of age) have not been studied. Allometric scaling was used to derive dosing regimens to provide pediatric patients with exposure comparable to the observed exposure in adults receiving 420 units and 840 units. The dose for pediatric patients is based on body weight.
8.5 Geriatric Use
Safety and effectiveness of ANTHRASIL in the geriatric population (>65 yrs of age) have not been studied.
8.6 Renal Insufficiency
Use ANTHRASIL with caution in patients with any degree of pre-existing renal insufficiency and in patients at risk of developing renal insufficiency (including, but not limited to those with diabetes mellitus, age greater than 65 years, volume depletion, paraproteinemia, sepsis, and patients receiving known nephrotoxic drugs), administering at the minimum rate of infusion practicable. Ensure that patients are not volume depleted before ANTHRASIL infusion. Do not exceed the recommended infusion rate, and follow the infusion schedule closely.
11. Anthrasil Description
ANTHRASIL, Anthrax Immune Globulin Intravenous (Human), is a sterile solution of purified human immune globulin G (IgG) containing polyclonal antibodies that bind the protective antigen (PA) component of Bacillus anthracis lethal and edema toxins. It is stabilized with 10% maltose and 0.03% polysorbate 80 (pH is between 5.0 and 6.5) and contains no preservative. The product is a clear or slightly opalescent colorless liquid, free of foreign particles, supplied in a 50 mL vial with variable fill volume. The total protein concentration ranges from 40 to 70 mg per mL. An adult dosage of 420 units (seven vials) of ANTHRASIL contains up to 0.368 g protein per kg body weight, and an adult dosage of 840 units (14 vials) contains up to 0.736 g protein per kg body weight. The protein load exposure to pediatric patients due to ANTHRASIL administration may range from 0.32 to 1.26 g per kg of body weight, depending on the weight-based pediatric dose.
ANTHRASIL is prepared using plasma collected from healthy, screened donors who were immunized with BioThrax® (Anthrax Vaccine Adsorbed) to achieve high titers of anti-anthrax antibody (meeting minimum potency specifications) and purified by an anion-exchange column chromatography method. The source plasma is tested by FDA licensed nucleic acid testing (NAT) for human immunodeficiency virus-1 (HIV-1), hepatitis B virus (HBV) and hepatitis C virus (HCV). Plasma also was tested by in-process NAT for hepatitis A virus (HAV) and parvovirus B19 (B19) via minipool testing; the limit for B19 in the manufacturing pool is set not to exceed 104 International Units of B19 DNA per mL.
The manufacturing process contains two steps implemented specifically for virus clearance. The solvent and detergent step (using tri-n-butyl phosphate and Triton X-100) is effective in the inactivation of enveloped viruses such as HBV, HCV and HIV. Virus filtration, using a Planova 20N virus filter, is effective for the removal of viruses based on their size, including some non-enveloped viruses. These two viral clearance steps are designed to increase product safety by reducing the risk of transmission of enveloped and non-enveloped viruses. In addition to these two specific steps, the process step of anion-exchange chromatography was identified as contributing to the overall viral clearance capacity for small non-lipid enveloped viruses.
The inactivation and reduction of known enveloped and non-enveloped model viruses were validated in laboratory studies as summarized in Table 2. The viruses employed for spiking studies were selected to represent those viruses that are potential contaminants in the product, and to represent a wide range of physiochemical properties in order to challenge the manufacturing process’s ability for viral clearance in general.
|
Enveloped |
Enveloped |
Non-Enveloped |
|||||
|
Genome |
RNA |
DNA |
RNA |
DNA |
|||
|
Virus |
HIV-1 |
BVDV |
PRV |
HAV |
EMC |
MMV |
PPV |
|
Family |
Retrovirus |
Flavivirus |
Herpes virus |
Picornavirus |
Parvovirus |
||
|
Size (nm) |
80–100 |
50–70 |
120–200 |
25–30 |
30 |
20–25 |
18–24 |
|
Anion Exchange Chromatography (partitioning) |
Not evaluated |
2.3 |
n.e. |
3.4 |
n.e. |
||
|
20N Filtration (size exclusion) |
≥4.7 |
≥3.5 |
≥5.6 |
n.e. |
4.8 |
n.e. |
4.1 |
|
Solvent/Detergent (inactivation) |
≥4.7 |
≥7.3 |
≥5.5 |
Not evaluated |
|||
|
Total Reduction (log10) |
≥9.4 |
≥10.8 |
≥11.1 |
2.3 |
4.8 |
3.4 |
4.1 |
|
Abbreviations: |
|||||||
|
BVDV = Bovine viral diarrhea virus; model virus for hepatitis C virus (HCV) and West Nile virus (WNV) |
|||||||
|
DNA = Deoxyribonucleic Acid |
|||||||
|
EMC = Encephalomyocarditis virus; model for HAV and for small non-enveloped viruses in general |
|||||||
|
HIV-1 = Human immunodeficiency virus-1; relevant virus for HIV-1 and model for HIV-2 |
|||||||
|
HAV = Human hepatitis A virus; relevant virus for HAV and model for small non-enveloped viruses in general |
|||||||
|
MMV = Murine minute virus; model for human B19 parvovirus and for small non-enveloped viruses in general |
|||||||
|
n.e. = Not evaluated |
|||||||
|
PPV = Porcine parvovirus; model for human B19 parvovirus and for small non-enveloped viruses in general |
|||||||
|
PRV = Pseudorabies virus; model for large enveloped DNA viruses, including herpes |
|||||||
|
RNA = Ribonucleic Acid |
|||||||
The product potency, as determined by an in vitro toxin neutralization assay (TNA), is expressed in arbitrary units by comparison to a standard calibrated against the Centers for Disease Control and Prevention (CDC) Reference Serum standard. Each vial contains approximately 40 to 70 mg per mL total protein and ≥60 units of toxin neutralizing activity. The product contains ≤40 mcg per mL of immune globulin A (IgA) as well as residual amounts of solvent and detergent, which are used to inactivate lipid-enveloped viruses.
12. Anthrasil - Clinical Pharmacology
12.1 Mechanism of Action
The polyclonal immune globulin G in ANTHRASIL is a passive immunizing agent that neutralizes anthrax toxin. ANTHRASIL binds to protective antigen (PA) to prevent PA mediated cellular entry of anthrax edema factor and lethal factor. ANTHRASIL is administered in combination with appropriate antibiotic therapy as the product itself is not known to have direct antibacterial activity against anthrax bacteria, which otherwise may continue to grow and product anthrax toxins.
12.3 Pharmacokinetics
The mean TNA activities for three doses of ANTHRASIL (210, 420 and 840 units TNA) in the clinical trial in healthy volunteers [See 14 CLINICAL STUDIES] are plotted on a semi-log scale in Figure 1. The pharmacokinetics of ANTHRASIL after intravenous infusion of the three dose levels were characterized; the peak levels of ANTHRASIL were reached immediately after infusion and then declined over the duration of study (84 days). The mean TNA activity remained above the lower limit of quantitation (5 milliunits per mL) over the entire 84-day post-dose period for the three doses studied.
Figure 1 Mean TNA Activities for Three Doses of ANTHRASIL
A summary of the mean pharmacokinetic results for the TNA data collected in the healthy volunteer study is presented in Table 3.
| PK Parameters | Dose Levels | |||||
|---|---|---|---|---|---|---|
| 210 U TNA | N | 420 U TNA | N | 840 U TNA | N | |
|
Arithmetic Mean (CV%) |
||||||
|
AUC0-t (mU·d/mL) |
1031.8 (23.3) |
15 |
2176.7 (18.9) |
17 |
4271.0 (22.3) |
16 |
|
AUC0-∞ (mU·d/mL) |
1277.5 (27.7) |
7 |
2536.7 (14.7) |
16 |
4788.8 (26.5) |
15 |
|
Cmax (mU/mL) |
83.0 (13.4) |
15 |
156.4 (21.7) |
17 |
316.7 (18.3) |
16 |
|
t½ (d) |
24.3 (33.3) |
7 |
28.3 (19.9) |
16 |
28.0 (25.2) |
15 |
|
CL (mL/d) |
174.2 (24.1) |
7 |
169.7 (17.9) |
16 |
188.6 (29.5) |
15 |
|
Vd (mL) |
5714.8 (11.4) |
7 |
6837.2 (20.4) |
16 |
7238.2 (19.4) |
15 |
|
Median (Min-Max) |
||||||
|
Tmax (d) |
0.116 |
15 |
0.120 |
17 |
0.169 |
16 |
|
(0.109–1.068) |
(0.120–0.412) |
(0.165–0.459) | ||||
In comparison to healthy subjects, patients with inhalational anthrax are expected to initially have greater clearance of anti-PA antibodies and lower AUC from ANTHRASIL administration due to the presence of PA antigen.
Mean PK results (TNA data) were evaluated by sex and revealed no sex-related differences over the dose range studied. Systemic exposure of ANTHRASIL increased in a dose-proportional manner over the dose range studied. ANTHRASIL has a serum elimination half-life of 24 to 28 days in healthy humans.
Inhalational anthrax patients, concomitantly treated with antibiotics and a single 420 unit TNA dose of ANTHRASIL, exhibited increases in serum and pleural anti-PA levels; these levels remained at >50% of the peak anti-PA levels over the next five days. The peak serum anti-PA levels in these patients following ANTHRASIL administration (132 to 160 mcg/mL, mean 145 mcg/mL) overlapped with those obtained with the 420 unit dose in healthy volunteers (135 to 250 mcg/mL, mean 190 mcg/mL, median 192 mcg/mL), although mean levels were approximately 25% lower in the inhalational anthrax patients. In the three inhalational anthrax patients, serum and pleural levels of lethal factor declined after initiation of antibiotics and further decreased over the period of five days following ANTHRASIL administration; however, due at least in part to ANTHRASIL targeting the PA component of lethal toxin, plasma and pleural fluid lethal factor levels remained detectable when measured two to five days following ANTHRASIL administration.
Because the effectiveness of ANTHRASIL cannot ethically be tested in placebo-controlled trials in humans, a comparison of ANTHRASIL exposures achieved in healthy human subjects to those observed in animal models of inhalational anthrax in therapeutic efficacy studies was necessary to support the dosage regimen. A dose of 420 units has a similar exposure to the efficacious dose of 15 U/kg administered to New Zealand white rabbits and cynomolgus macaques. In cynomolgus macaques treated with ANTHRASIL monotherapy, a higher dose of 30 U/kg, with a similar exposure to a human dose of 840 units, may result in improved survival [See 13.2 Animal Toxicology and/or Pharmacology]. As a result, the initial dosing regimen is given as a range of 420 to 840 units, and the recommended regimen includes the potential for repeat dosing.
13. Nonclinical Toxicology
Immune globulins are normal constituents of the human body. Toxicology studies have not been performed with ANTHRASIL or its components.
The evaluation of new treatment options for anthrax using placebo-controlled human trials is unethical and infeasible. Therefore, the effectiveness of ANTHRASIL for treatment of inhalational anthrax is based on well controlled efficacy studies conducted in rabbits and cynomolgus macaques.
13.2 Animal Toxicology and/or Pharmacology
Anthrax infected New Zealand white rabbits and cynomolgus macaques administered an intravenous injection of ANTHRASIL (15 units TNA per kg) that did not survive their infection showed an increase in the severity and/or incidence of central nervous system lesions (bacteria, hemorrhage and necrosis) as compared to immune globulin (“placebo”) treated animals who also did not survive the infection. The mean time to death between non-surviving ANTHRASIL and placebo treated animals was comparable. Surviving rabbits had no evidence of central nervous system lesions at the end of the study. No surviving cynomolgus macaques in monotherapeutic studies were tested for central nervous system lesions.
Monotherapeutic Studies in Animal Models
In a monotherapeutic efficacy study, rabbits were exposed to a target dose of 200 x LD50 aerosolized anthrax spores and then administered 15 units per kg of ANTHRASIL at the onset of toxemia, as determined by the presence of PA in serum samples. Detection of PA was used as the trigger for initiation of treatment, while bacteremia status provided a retrospective confirmation of disease. Ninety-eight (98) percent of the treated animals were bacteremic prior to treatment. Of the animals that were toxemic and bacteremic prior to treatment, ANTHRASIL treatment resulted in a 26% survival in comparison to a 2% survival with IGIV placebo treatment (Table 4) over the 36 day duration of the study. ANTHRASIL treatment resulted in a significant decrease in the proportion of rabbits that were toxemic or bacteremic. The time to resolution of toxemia (p=0.0006) or bacteremia (p=0.0074) was also significantly reduced in rabbits that received ANTHRASIL.
Efficacy of ANTHRASIL was also assessed in cynomolgus macaques exposed to a target dose of 200 x LD50 aerosolized anthrax spores. Treatment with placebo or one of three dose levels of ANTHRASIL was initiated after animals became toxemic (positive for PA detection in serum samples), and bacteremia status provided a retrospective confirmation of disease. Survival was assessed over a period of 88 days in toxemic animals that were confirmed to be bacteremic at the time of treatment. Survival was 0% in placebo treated animals. Animals treated with 7.5 units per kg exhibited 36% survival, those treated with 15 units per kg exhibited 43% survival, and those treated with 30 units per kg exhibited 70% survival (Table 4). Compared to placebo, these survival rates were statistically significant at p=0.0451, 0.0339, and 0.0031, respectively. The differences in survival between the 7.5, 15, and 30 unit per kg doses of ANTHRASIL were not statistically significant. ANTHRASIL treated animals showed a statistically significant reduction in anthrax toxin when compared to placebo treated animals.
|
NZW Rabbits at 36 Days PI |
Cynomolgus Macaques at 28 Days PI |
|||
|
No. Survivors (%)a |
p-Valueb |
No. Survivors (%)a |
p-Valuec |
|
|
Placebo |
1/48 (2) |
– |
0/11 (0) |
– |
|
ANTHRASIL 7.5 U/kgd |
– |
– |
4/11 (36) |
0.0451 |
|
ANTHRASIL 15 U/kg |
13/50 (26) |
0.0009 |
6/14 (43) |
0.0339 |
|
ANTHRASIL 30 U/kgd |
– |
– |
7/10 (70) |
0.0031 |
|
a Survival among animals that were bacteremic and toxemic prior to treatment |
||||
|
b Two-sided Fisher’s exact test |
||||
|
c Bonferroni-Holm adjusted one-sided Fisher’s exact test |
||||
|
d Dose not evaluated in rabbits in this study |
||||
|
PI = Post-infection |
||||
ANTHRASIL Efficacy in Combination with Antibiotics
The efficacy of ANTHRASIL administered with levofloxacin was determined in New Zealand white rabbits with systemic disease. No significant difference between the control (normal immune globulin [IGIV] plus levofloxacin) and treatment groups (ANTHRASIL plus levofloxacin) was seen when combination treatment was delayed up to 60 hours post-challenge. There was no observed antagonism between levofloxacin and ANTHRASIL in this study. This study also supported that ANTHRASIL effectively cleared toxemia when administered with antibiotics. In ANTHRASIL treated groups, all animals cleared PA toxemia post-ANTHRASIL administration and only 4/31 (13%) of ANTHRASIL treated animals exhibited a single transient positive PA result for toxemia at the 12 or 18 hour time point post-dosing. Placebo control animals exhibited more persistent toxemia, with 26/32 (81%) having positive PA results for 18 to 90 hours post-treatment.
In a second study, treatment was delayed beyond 60 hours to simulate a clinical scenario. When combination treatment was initiated at 60, 72, 84 or 96 hours post anthrax exposure, differences in survival were seen, but no statistically significant added survival benefit was observed between groups that received placebo (IGIV plus levofloxacin) or ANTHRASIL (15 units per kg plus levofloxacin). An increase in survival was observed with ANTHRASIL when treatment was delayed to 96 hours post exposure, but was not statistically significant. When treatment was delayed to 96 hours, survival was 25% (2/8) in the antibiotic plus IGIV control group and 71% (5/7) in the ANTHRASIL plus levofloxacin group. A marginal improvement of 10 to 15% was observed at other time points, suggesting a trend in added benefit with ANTHRASIL. This study also demonstrated a significant effect of ANTHRASIL on toxemia. The majority of ANTHRASIL treated animals became negative for PA (toxemia) within one hour post-infusion of ANTHRASIL and remained negative, even with the delayed treatment from 60 to 96 hours post-anthrax challenge and high levels of toxemia pretreatment. In contrast, placebo treated animals remained toxemic up to three days after initiating antibiotic treatment.
The efficacy of ANTHRASIL co-administered with levofloxacin was evaluated in New Zealand white rabbits when treatment was delayed to 96 hours after anthrax spore inhalation. The dose of levofloxacin was chosen to yield a comparable exposure to that achieved by the recommended dose in humans. Of the animals that survived to be treated (19% of those challenged), antibacterial drug plus ANTHRASIL (15 units per kg) resulted in 58% (18/31) survival compared to 39% (13/33) survival in rabbits treated with antibacterial drug and IGIV placebo (p=0.14, Z-test).
When animals were stratified by pre-treatment toxemia (PA) in a post hoc analysis, added benefit was observed in animals treated with ANTHRASIL and levofloxacin when they had pre-treatment PA levels between 200 and 800 ng/mL (p=0.02, Fisher’s exact test). When pre-treatment toxemia was low (PA <200 ng/mL), survival was greater than 90% in all animals, regardless of treatment (Table 5). Animals with very high levels of toxemia (>800 ng/mL) did not survive irrespective of the treatment administered.
|
Pre-treatment PA (ng/mL) |
IGIV Placebo + Levofloxacin (%) |
ANTHRASIL + Levofloxacin (%) |
|
<200 |
11/12 (91.7) |
8/9 (88.9) |
|
200–800 |
2/11 (18.2) |
10/14 (71.4) |
|
>800 |
0/10 (0) |
0/8 (0) |
|
All pre-treatment PA levels |
13/33 (39.4) |
18/31 (58.1) |
ANTHRASIL and antibiotic combination treatment was also studied in the cynomolgus macaque model of inhalational anthrax. In this study, delay of initiation of treatment to 64 hours post anthrax exposure resulted in 75% (9/12) survival in the placebo plus ciprofloxacin treatment group versus 83% (10/12) survival in the ANTHRASIL (15 units per kg) plus ciprofloxacin group (p=1).
No antagonism of ANTHRASIL when administered with antibiotic as a concomitant therapy was observed.
ANTHRASIL in Post-exposure Prophylaxis
A post exposure prophylactic study assessed the survival following aerosol exposure to a lethal dose of anthrax spores (200 x LD50) in New Zealand white rabbits administered ANTHRASIL (7.5, 15 or 30 units TNA per kg) at 30 hours post-anthrax challenge compared to placebo controls. All three doses of ANTHRASIL improved survival when given 30 hours post-anthrax challenge. When animals that were both bacteremic and toxemic were treated at 30 hours following challenge, there was a 22% (2/9) survival with a dose of 15 units TNA per kg and a 33% (4/12) survival with a dose of 30 units TNA per kg. All rabbits in the placebo arm died.
14. Clinical Studies
Because it is not ethical or feasible to conduct placebo-controlled clinical trials in humans with inhalational anthrax, the effectiveness of ANTHRASIL is based on efficacy studies demonstrating a survival benefit in animal models of inhalational anthrax infection [See 13.2 Animal Toxicology and/or Pharmacology]. The safety has been assessed in healthy adults and in a limited number of patients with anthrax who were treated with ANTHRASIL under expanded access use.
Safety and Pharmacokinetics of ANTHRASIL in Healthy Volunteers
In a double blind, randomized, placebo-controlled study designed to assess the safety and pharmacokinetics of three doses of ANTHRASIL after a single intravenous infusion in healthy volunteers, a total of 72 healthy adult subjects were randomized to receive a dose of 210, 420 or 840 units of ANTHRASIL by TNA (N=18/dosing group) or an equal volume of saline placebo (N=6/dosing group).
A second stage of this study, designed only for additional safety assessment, was a randomized, open-label study in 20 healthy adult volunteers. Subjects were randomized to receive a dose of 840 units by TNA from one of two additional product lots (10 subjects per lot). There was no placebo group [See 6 ADVERSE REACTIONS and 12.3 Pharmacokinetics].
Patient Experience
Nineteen adult patients have been treated with ANTHRASIL under expanded access use, including three patients with inhalational anthrax, one patient with gastrointestinal anthrax and 15 patients with injectional anthrax due to injection of anthrax-contaminated heroin. Patients were receiving antimicrobial therapy before, during and after ANTHRASIL administration.
In patients with inhalational anthrax, two out of three patients treated with ANTHRASIL plus antimicrobial therapy survived and one died from progression of anthrax disease, systemic candidiasis and multiorgan failure. Among the 15 patients with injectional anthrax treated with ANTHRASIL plus antibiotics, 10 survived and five died (two from progression of anthrax disease; the cause of death was not determined or available for three patients). The single patient with gastrointestinal anthrax treated with ANTHRASIL survived. Therapy for these systemic anthrax cases included aggressive supportive measures including mechanical ventilation and pulmonary/abdominal fluid drainage.
In the three inhalational patients, the ANTHRASIL dose of 420 units by TNA resulted in increased anti-PA levels (correlating with increased TNA activity); these levels remained stable up to seven to 20 days post-administration, probably reflecting the rising antibody production by the patient at the same time that the exogenously-administered antibody was being cleared.
In some injectional anthrax cases, complicated by hemorrhage and pleural and/or peritoneal fluid losses from thoracentesis and/or paracentesis, serum anti-PA antibody levels fell as much as approximately 90% from their post-ANTHRASIL peak levels by 24 hours following ANTHRASIL administration. In the gastrointestinal anthrax patient, serum anti-PA levels were observed prior to ANTHRASIL infusion with further increases in anti-PA levels post-administration and maintenance of anti-PA above pre-administration levels for 11 days was observed.
15. References
- 1.
- Kahwaji J, Barker E, Pepkowitz S, Klapper E, Villicana R, Peng A, et al. Acute hemolysis after high-dose intravenous immunoglobulin therapy in highly HLA sensitized patients. Clin J Am Soc Nephrol. 2009 December;4;1993–97.
- 2.
- Daw Z, Padmore R, Neurath D, Cober N, Tokessy M, Desjardins D, et al. Hemolytic transfusion reactions after administration of intravenous immune (gamma) globulin: a case series analysis. Transfusion. 2008;48(8):1598-601.
16. How is Anthrasil supplied
16.1 How Supplied
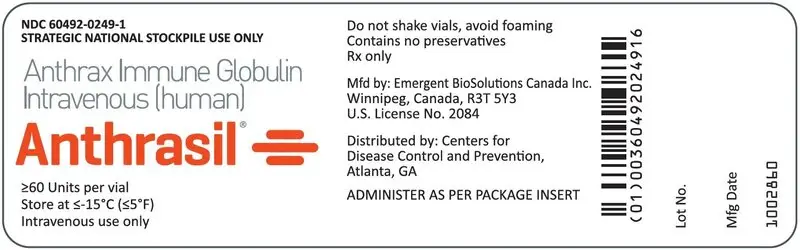
NDC 60492-0249-1 for single vial
NDC 60492-0249-2 for shelf carton containing seven vials
ANTHRASIL is supplied as a 50 mL single dose vial seated with a butyl rubber stopper and an aluminum seal with a plastic flip-top cap. Each vial, regardless of fill volume, contains ≥60 units. It is packaged in a shelf carton with seven vials and a package insert.
ANTHRASIL does not contain natural rubber latex.
16.2 Storage and Handling
Store frozen at or below ≤-15°C (≤5°F) until required for use. Do not use after expiration date.
Once punctured, use the vial contents to prepare the infusion bag and infuse as soon as possible. ANTHRASIL contains no preservative.
Do not refreeze, reuse or save ANTHRASIL for future use.
Discard any partially used vials.
17. Patient Counseling Information
See FDA-approved patient labeling (Patient Information).
Discuss the risks and benefits of this product with the patient or their legally authorized representative before administering it to the patient.
- •
- Inform patients of the potential for hypersensitivity reactions, especially in individuals with previous reactions to human immune globulin and in individuals deficient in IgA. Advise patients to be aware of the following symptoms associated with allergic reactions: hives, rash, chest tightness, wheezing, shortness of breath, or feeling light headed or dizzy when they stand. Patients should be cautioned to seek medical attention immediately should they experience any one or more of the above mentioned symptoms, as well as other side effects including injection site pain, chills, fever, headache, nausea, vomiting, and joint pain.
- •
- Advise patients that the maltose contained in ANTHRASIL can interfere with some types of blood glucose monitoring systems. Advise patients to use only testing systems that are glucose‑specific for monitoring blood glucose levels as the interference of maltose could result in falsely elevated glucose readings that could lead to untreated hypoglycemia or to inappropriate insulin administration, resulting in life-threatening hypoglycemia.
- •
- Inform patients that ANTHRASIL is an immune globulin product; therefore, there is the potential risk of developing other reactions observed with the immunoglobulin product class such as thrombosis, hemolysis, aseptic meningitis syndrome (AMS), transfusion-related acute lung injury (TRALI), acute respiratory distress syndrome (ARDS) and acute renal dysfunction or failure.
- •
- Advise patients that ANTHRASIL may impair the effectiveness of certain live virus vaccines such as measles, rubella (i.e. German measles), mumps, and varicella (i.e. chickenpox).
- •
- Inform patients that ANTHRASIL is prepared from human plasma. Products made from human plasma may contain infectious agents such as viruses that can cause disease.
- •
- Inform patients that the efficacy of ANTHRASIL is based solely on efficacy studies demonstrating a survival benefit in animals and that the effectiveness of ANTHRASIL has not been tested in humans with anthrax. The safety of ANTHRASIL has been tested in healthy adults.
Patient Information
ANTHRASIL [Anthrax Immune Globulin Intravenous (Human)]
What is anthrax?
Anthrax is a serious disease caused by a germ called Bacillus anthracis. This germ makes a poison called a toxin. People who are exposed to anthrax germs are at risk of serious illness, including death. You/your child cannot get anthrax from another person. Symptoms of anthrax disease usually start within seven days of breathing in anthrax germs, but can take up to six or seven weeks to appear.
- •
- Early symptoms can be any of the following: fever, chills, tiredness, cough, muscle aches or headache.
- •
- Later symptoms can be any of the following: shortness of breath, chest discomfort, confusion or nausea.
What is ANTHRASIL?
Medicines like antibiotics can kill anthrax germs. However, the anthrax poison (toxin) may continue to cause severe sickness even after the germs are gone. When someone gets the anthrax vaccine, their body’s immune system makes antibodies against anthrax. Antibodies help to fight off disease and can also help to fight off the anthrax poison.
ANTHRASIL [Anthrax Immune Globulin Intravenous (Human)] is made by taking anthrax antibodies from well people who have been vaccinated. It does not contain the anthrax germ or poison. The antibodies in ANTHRASIL can then be given to someone with anthrax. This may make the sick person’s disease less severe, decrease the duration of illness and increase their chance of surviving.
The effectiveness of ANTHRASIL has been studied only in animals.
The safety of ANTHRASIL was studied in healthy adults. There have been no studies of ANTHRASIL in persons less than 17 years of age.
Who should use ANTHRASIL?
Your doctor may give you ANTHRASIL if they suspect that you/your child have been exposed to anthrax and may have anthrax in your lungs.
You should get the treatment as quickly as possible to stop the progression of the illness.
Before you receive ANTHRASIL, tell your healthcare provider about all of your medical conditions, including if you are:
- •
- Allergic to any of the ingredients in ANTHRASIL
- •
- Deficient for immune globulin A (IgA)
- •
- Pregnant or planning to become pregnant. It is not known if ANTHRASIL will harm your unborn baby.
- •
- Breastfeeding or plan to breastfeed. It is not known if ANTHRASIL passes into your breast milk. You and your healthcare provider should decide if you will receive ANTHRASIL or breastfeed.
- •
- Diabetic. ANTHRASIL contains maltose, which can give false readings on some glucose testing meters. If you are diabetic, ask your doctor what types of glucose testing meters can be used safely while you are getting ANTHRASIL.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins and herbal supplements.
How will you receive ANTHRASIL?
ANTHRASIL is given as an infusion into your vein. Your doctor will determine the dose of ANTHRASIL. The treatment may take several hours to administer. Your doctor will decide if you need more than one infusion.
What are the possible side effects of ANTHRASIL?
The most common side effects of ANTHRASIL are:
- •
- Headache
- •
- Pain at site of needle entry
- •
- Nausea
- •
- Swelling at site of needle entry
- •
- Back pain
ANTHRASIL can cause allergic reactions. Tell your doctor right away if you have trouble breathing, swelling of your tongue or lips, a very fast heart rate, or feel very weak because these symptoms can be signs of a serious allergic reaction.
Talk to your doctor about any side effects that concern you. You can ask your doctor for additional prescribing information that is available to healthcare professionals.
What other information do you need to know about ANTHRASIL?
ANTHRASIL is made from human plasma. The plasma donors are carefully screened and the plasma is carefully cleaned, but there is a small risk that it may give you a virus. Talk to your doctor if you have any symptoms that concern you.
Tell your doctor if you have recently received a vaccine of any sort, or plan to be vaccinated. Use of ANTHRASIL may cause vaccines such as measles, rubella, mumps and varicella to not work as well. Vaccination with some vaccines may need to be delayed until approximately three months after use of ANTHRASIL. If you received ANTHRASIL shortly after a vaccination you may need to be re-vaccinated three months after the administration of ANTHRASIL. Talk to your doctor.
You may report side effects directly to Emergent BioSolutions Canada Inc. at 1-800-768-2304 or to the FDA’s MedWatch reporting system at 1-800-FDA-1088.
Manufactured by:
Emergent BioSolutions Canada Inc.
155 Innovation Drive
Winnipeg, MB Canada
R3T 5Y3
US License No. 2084
| ANTHRASIL
anthrax immune globulin (human) liquid |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Emergent BioSolutions Canada Inc. (203508049) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Emergent BioSolutions Canada Inc. | 203508049 | MANUFACTURE(60492-0249) | |