Drug Detail:Arava (Leflunomide [ le-floo-noe-mide ])
Drug Class: Antirheumatics Selective immunosuppressants
Highlights of Prescribing Information
ARAVA (leflunomide), tablets, for oral use
Initial U.S. Approval: 1998
WARNING: EMBRYO-FETAL TOXICITY and HEPATOTOXICITY
See full prescribing information for complete boxed warning.
Embryo-Fetal Toxicity
- Teratogenicity and embryo-lethality occurred in animals administered leflunomide. ( 5.1, 8.1)
- Exclude pregnancy prior to initiating ARAVA therapy. ( 5.1, 8.3)
- Advise use of effective contraception in females of reproductive potential during treatment and during a drug elimination procedure. ( 5.1, 5.3, 8.3)
- Stop ARAVA and use an accelerated drug elimination procedure if the patient becomes pregnant. ( 5.1, 5.3, 8.1)
Hepatotoxicity
- Severe liver injury and fatal liver failure have been reported. ( 5.2)
- Avoid ARAVA use in patients with pre-existing liver disease, or those with serum alanine aminotransferase (ALT) >2 × ULN. ( 5.2, 8.6)
- Use caution when ARAVA is given with other potentially hepatotoxic drugs. ( 5.2)
- Monitor ALT levels. Interrupt ARAVA treatment if ALT elevation >3-fold ULN. If likely leflunomide-induced, start accelerated drug elimination procedure and monitor liver tests weekly until normalized. ( 5.2, 5.3)
Indications and Usage for Arava
ARAVA is a pyrimidine synthesis inhibitor indicated for the treatment of adults with active rheumatoid arthritis. ( 1)
Arava Dosage and Administration
- Loading dosage for patients at low risk for ARAVA-associated hepatotoxicity and ARAVA-associated myelosuppression: 100 mg daily for 3 days. ( 2.1)
- Maintenance dosage: 20 mg daily. (
2.1)
- Maximum recommended daily dosage: 20 mg once daily. ( 2.1)
- If 20 mg once daily is not tolerated, may decrease dosage to 10 mg once daily. ( 2.1)
- Screen patients for active and latent tuberculosis, pregnancy test (females), blood pressure, and laboratory tests before starting ARAVA. ( 2.2)
Dosage Forms and Strengths
Tablets: 10 mg, 20 mg, 100 mg. ( 3)
Contraindications
- Pregnancy. ( 4, 5.1, 8.1)
- Severe hepatic impairment. ( 4, 5.2)
- Hypersensitivity to ARAVA or any of its inactive components. ( 4)
- Current teriflunomide treatment. ( 4)
Warnings and Precautions
- After stopping ARAVA, it is recommended that an accelerated drug elimination procedure be used to reduce the plasma concentrations of the active metabolite, teriflunomide. ( 5.3)
- Severe infections (including sepsis), pancytopenia, agranulocytosis, and thrombocytopenia: Stop ARAVA and use accelerated elimination procedure. Do not start ARAVA in patients with active infection. Monitor CBCs during treatment with ARAVA. ( 5.4)
- Stevens-Johnson syndrome and toxic epidermal necrolysis, Drug reaction with eosinophilia and systemic symptoms (DRESS): Stop ARAVA and use accelerated elimination procedure. ( 5.5)
- Peripheral neuropathy: If patient develops symptoms consistent with peripheral neuropathy, evaluate patient and consider discontinuing ARAVA. ( 5.7)
- Interstitial lung disease: May be fatal. New onset or worsening symptoms may necessitate discontinuation of ARAVA and initiation of accelerated elimination procedure. ( 5.8)
- Increased blood pressure: Monitor and treat. ( 5.10)
Adverse Reactions/Side Effects
- The most commonly reported adverse reactions (≥10%) regardless of relation to ARAVA treatment were diarrhea, respiratory infection, nausea, headache, rash, abnormal liver enzymes, and dyspepsia. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact sanofi-aventis U.S. LLC at 1-800-633-1610 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Drugs metabolized by CYP2C8 and OAT3 transporters: Monitor patients because teriflunomide may increase exposure of these drugs. ( 7)
- Teriflunomide may increase exposure of ethinylestradiol and levonorgestrel. Choose an appropriate oral contraceptive. ( 7)
- Drugs metabolized by CYP1A2: Monitor patients because teriflunomide may decrease exposure of these drugs. ( 7)
- Warfarin: Monitor INR as teriflunomide may decrease INR. ( 7)
- Drugs metabolized by BCRP and OATP1B1/B3 transporters: Monitor patients because teriflunomide may increase exposure of these drugs. ( 7)
- Rosuvastatin: The dose of rosuvastatin should not exceed 10 mg once daily in patients taking ARAVA. ( 7)
Use In Specific Populations
- Lactation: Discontinue breastfeeding. ( 8.2)
- Safety and effectiveness in pediatric patients <12 years of age have not been established. ( 8.4)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 12/2021
Full Prescribing Information
1. Indications and Usage for Arava
ARAVA is indicated for the treatment of adults with active rheumatoid arthritis (RA).
2. Arava Dosage and Administration
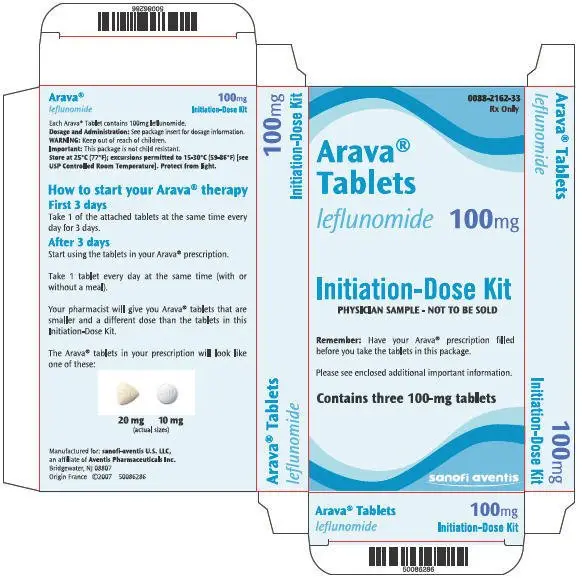
2.1 Recommended Dosage
The recommended dosage of ARAVA is 20 mg once daily. Treatment may be initiated with or without a loading dose, depending upon the patient's risk of ARAVA-associated hepatotoxicity and ARAVA-associated myelosuppression. The loading dose provides steady-state concentrations more rapidly.
- For patients who are at low risk for ARAVA-associated hepatotoxicity and ARAVA-associated myelosuppression, the recommended ARAVA loading dose is 100 mg once daily for 3 days. Subsequently administer 20 mg once daily.
- For patients at high risk for ARAVA-associated hepatotoxicity (e.g., those taking concomitant methotrexate) or ARAVA-associated myelosuppression (e.g., patients taking concomitant immunosuppressants), the recommended ARAVA dosage is 20 mg once daily without a loading dose [see Warnings and Precautions (5.2, 5.4)] .
The maximum recommended daily dose is 20 mg once per day. Consider dosage reduction to 10 mg once daily for patients who are not able to tolerate 20 mg daily (i.e., for patients who experience any adverse events listed in Table 1).
Monitor patients carefully after dosage reduction and after stopping therapy with ARAVA, since the active metabolite of leflunomide, teriflunomide, is slowly eliminated from the plasma [see Clinical Pharmacology (12.3)] . After stopping ARAVA treatment, an accelerated drug elimination procedure is recommended to reduce the plasma concentrations of the active metabolite, teriflunomide [see Warnings and Precautions (5.3)] . Without use of an accelerated drug elimination procedure, it may take up to 2 years to reach undetectable plasma teriflunomide concentrations after stopping ARAVA [see Clinical Pharmacology (12.3)] .
2.2 Evaluation and Testing Prior to Starting ARAVA
Prior to starting ARAVA treatment, the following evaluations and tests are recommended:
- Evaluate patients for active tuberculosis and screen patients for latent tuberculosis infection [see Warnings and Precautions (5.4)]
- Laboratory tests including serum alanine aminotransferase (ALT); and white blood cell, hemoglobin or hematocrit, and platelet counts [see Warnings and Precautions (5.2, 5.4)]
- For females of reproductive potential, pregnancy testing [see Warnings and Precautions (5.1)]
- Check blood pressure [see Warnings and Precautions (5.10)]
3. Dosage Forms and Strengths
ARAVA Tablets are available in three strengths:
- Tablets: 10 mg, supplied as white, round film-coated tablet embossed with "ZBN" on one side
- Tablets: 20 mg, supplied as light-yellow, triangular film-coated tablet embossed with "ZBO" on one side
- Tablets: 100 mg, supplied as white, round film-coated tablet embossed with "ZBP" on one side
4. Contraindications
ARAVA is contraindicated in:
- Pregnant women. ARAVA may cause fetal harm. If a woman becomes pregnant while taking this drug, stop ARAVA, apprise the patient of the potential hazard to the fetus, and begin a drug elimination procedure [see Warnings and Precautions (5.1, 5.3) and Use in Specific Populations (8.1)] .
- Patients with severe hepatic impairment [see Warnings and Precautions (5.2)] .
- Patients with known hypersensitivity to leflunomide or any of the other components of ARAVA. Known reactions include anaphylaxis [see Adverse Reactions (6.1)] .
- Patients being treated with teriflunomide [see Drug Interactions (7)] .
5. Warnings and Precautions
5.1 Embryo-Fetal Toxicity
ARAVA may cause fetal harm when administered to a pregnant woman. Teratogenicity and embryo-lethality occurred in animal reproduction studies with leflunomide at doses lower than the human exposure level [see Use in Specific Populations (8.1)] .
ARAVA is contraindicated for use in pregnant women [see Contraindications (4)] . Exclude pregnancy before starting treatment with ARAVA in females of reproductive potential [see Dosage and Administration (2.2)] . Advise females of reproductive potential to use effective contraception during ARAVA treatment and during an accelerated drug elimination procedure after ARAVA treatment [see Use in Specific Populations (8.3)] . If a woman becomes pregnant while taking ARAVA, stop treatment with ARAVA, apprise the patient of the potential risk to a fetus, and perform an accelerated drug elimination procedure to achieve nondetectable plasma concentrations of teriflunomide, the active metabolite of leflunomide [see Warnings and Precautions (5.3)] .
Upon discontinuing ARAVA, it is recommended that all females of reproductive potential undergo an accelerated drug elimination procedure. Women receiving ARAVA treatment who wish to become pregnant must discontinue ARAVA and undergo an accelerated drug elimination procedure, which includes verification that plasma concentrations of the active metabolite of leflunomide, teriflunomide, are less than 0.02 mg/L (0.02 mcg/mL). Based on animal data, human plasma concentrations of teriflunomide of less than 0.02 mg/L (0.02 mcg/mL) are expected to have minimal embryo-fetal risk [see Contraindications (4), Warnings and Precautions (5.3), and Use in Specific Populations (8.1)] .
5.2 Hepatotoxicity
Severe liver injury, including fatal liver failure, has been reported in some patients treated with ARAVA. Patients with pre-existing acute or chronic liver disease, or those with serum alanine aminotransferase (ALT) of greater than twice the upper limits of normal (>2 × ULN) before initiating treatment, should not be treated with ARAVA. Use caution when ARAVA is given with other potentially hepatotoxic drugs. Monitoring of ALT levels is recommended at least monthly for six months after starting ARAVA, and thereafter every 6 to 8 weeks. If ALT elevation >3-fold ULN occurs, interrupt ARAVA therapy and investigate the cause. If likely ARAVA-induced, perform the accelerated drug elimination procedure and monitor liver tests weekly until normalized [see Warnings and Precautions (5.3)] . If ARAVA-induced liver injury is unlikely because some other cause has been found, resumption of ARAVA therapy may be considered.
If ARAVA and methotrexate are given concomitantly, follow the American College of Rheumatology (ACR) guidelines for monitoring methotrexate liver toxicity with ALT, AST, and serum albumin testing.
5.3 Procedure for Accelerated Elimination of ARAVA and its Active Metabolite
The active metabolite of leflunomide, teriflunomide, is eliminated slowly from the plasma [see Clinical Pharmacology (12.3)] .
Use of an accelerated drug elimination procedure will rapidly reduce plasma concentrations of leflunomide and its active metabolite, teriflunomide. Therefore, an accelerated elimination procedure should be considered at any time after discontinuation of ARAVA, and in particular, when a patient has experienced a severe adverse reaction (e.g., hepatotoxicity, serious infection, bone marrow suppression, Stevens-Johnson Syndrome, toxic epidermal necrolysis, peripheral neuropathy, interstitial lung disease), suspected hypersensitivity, or has become pregnant. It is recommended that all women of childbearing potential undergo an accelerated elimination procedure after stopping ARAVA treatment.
Without use of an accelerated drug elimination procedure, it may take up to 2 years to reach plasma teriflunomide concentrations of less than 0.02 mg/L, the plasma concentration not associated with embryo-fetal toxicity in animals.
Elimination can be accelerated by the following procedures:
- Administer cholestyramine 8 grams orally 3 times daily for 11 days.
- Alternatively, administer 50 grams of activated charcoal powder (made into a suspension) orally every 12 hours for 11 days.
Verify plasma teriflunomide concentrations of less than 0.02 mg/L (0.02 µg/mL) by two separate tests at least 14 days apart. If plasma teriflunomide concentrations are higher than 0.02 mg/L, repeat cholestyramine and/or activated charcoal treatment.
The duration of accelerated drug elimination treatment may be modified based on the clinical status and tolerability of the elimination procedure. The procedure may be repeated as needed, based on teriflunomide concentrations and clinical status.
Use of the accelerated drug elimination procedure may potentially result in return of disease activity if the patient had been responding to ARAVA treatment.
5.4 Immunosuppression, Bone Marrow Suppression, and Risk of Serious Infections
ARAVA is not recommended for patients with severe immunodeficiency, bone marrow dysplasia, or severe, uncontrolled infections. If a serious infection occurs, consider interrupting ARAVA therapy and initiating the accelerated drug elimination procedure [see Warnings and Precautions (5.3)] . Medications like ARAVA that have immunosuppression potential may cause patients to be more susceptible to infections, including opportunistic infections, especially Pneumocystis jirovecii pneumonia, tuberculosis (including extra-pulmonary tuberculosis), and aspergillosis. Severe infections including sepsis, which may be fatal, have been reported in patients receiving ARAVA, especially Pneumocystis jirovecii pneumonia and aspergillosis. Most of the reports were confounded by concomitant immunosuppressant therapy and/or comorbid illness which, in addition to rheumatoid arthritis, may predispose patients to infection.
Cases of tuberculosis were observed in clinical studies with teriflunomide, the metabolite of ARAVA. Prior to initiating ARAVA, all patients should be screened for active and inactive ("latent") tuberculosis infection as per commonly used diagnostic tests. ARAVA has not been studied in patients with a positive tuberculosis screen, and the safety of ARAVA in individuals with latent tuberculosis infection is unknown. Patients testing positive in tuberculosis screening should be treated by standard medical practice prior to therapy with ARAVA and monitored carefully during ARAVA treatment for possible reactivation of the infection.
Pancytopenia, agranulocytosis, and thrombocytopenia have been reported in patients receiving ARAVA alone. These events have been reported most frequently in patients who received concomitant treatment with methotrexate or other immunosuppressive agents, or who had recently discontinued these therapies; in some cases, patients had a prior history of a significant hematologic abnormality.
Patients taking ARAVA should have platelet, white blood cell count and hemoglobin or hematocrit monitored at baseline and monthly for six months following initiation of therapy and every 6 to 8 weeks thereafter. If used with concomitant methotrexate and/or other potential immunosuppressive agents, chronic monitoring should be monthly. If evidence of bone marrow suppression occurs in a patient taking ARAVA, stop treatment with ARAVA and perform an accelerated drug elimination procedure to reduce the plasma concentration of the ARAVA active metabolite, teriflunomide [see Warnings and Precautions (5.3)] .
In any situation in which the decision is made to switch from ARAVA to another antirheumatic agent with a known potential for hematologic suppression, it would be prudent to monitor for hematologic toxicity, because there will be overlap of systemic exposure to both compounds.
5.5 Stevens-Johnson Syndrome, Toxic Epidermal Necrolysis, and Drug Reactions with Eosinophilia and Systemic Symptoms
Rare cases of Stevens-Johnson syndrome and toxic epidermal necrolysis, and drug reaction with eosinophilia and systemic symptoms (DRESS) have been reported in patients receiving ARAVA. If a patient taking ARAVA develops any of these conditions, stop ARAVA treatment and perform an accelerated drug elimination procedure [see Warnings and Precautions (5.3)] .
5.6 Malignancy and Lymphoproliferative Disorders
The risk of malignancy, particularly lymphoproliferative disorders, is increased with the use of some immunosuppression medications. There is a potential for immunosuppression with ARAVA. No apparent increase in the incidence of malignancies and lymphoproliferative disorders was reported in the clinical trials of ARAVA, but larger dosages and longer-term studies would be needed to determine whether there is an increased risk of malignancy or lymphoproliferative disorders with ARAVA.
5.7 Peripheral Neuropathy
Cases of peripheral neuropathy have been reported in patients receiving ARAVA and in clinical studies with teriflunomide, the active metabolite of leflunomide. Most patients recovered after discontinuation of treatment, but some patients had persistent symptoms. Age older than 60 years, concomitant neurotoxic medications, and diabetes may increase the risk for peripheral neuropathy. If a patient taking ARAVA develops a peripheral neuropathy, consider discontinuing ARAVA therapy and performing an accelerated drug elimination procedure [see Warnings and Precautions (5.3)] .
5.8 Interstitial Lung Disease
Interstitial lung disease and worsening of pre-existing interstitial lung disease have been reported during treatment with ARAVA and has been associated with fatal outcomes [see Adverse Reactions (6.2)] . The risk of ARAVA-associated interstitial lung disease is increased in patients with a history of interstitial lung disease. Interstitial lung disease is a potentially fatal disorder that may occur acutely at any time during therapy and has a variable clinical presentation. New onset or worsening pulmonary symptoms, such as cough and dyspnea, with or without associated fever, may be a reason for discontinuation of ARAVA therapy and for further investigation as appropriate. If discontinuation of ARAVA is necessary, consider performing an accelerated drug elimination procedure [see Warnings and Precautions (5.3)] .
5.9 Vaccinations
No clinical data are available on the efficacy and safety of vaccinations during ARAVA treatment. Vaccination with live vaccines is, however, not recommended. The long half-life of the active metabolite of ARAVA should be considered when contemplating administration of a live vaccine after stopping ARAVA.
5.10 Blood Pressure Monitoring
In placebo-controlled studies with the active metabolite of ARAVA, teriflunomide, elevations in blood pressure were observed in some subjects. Blood pressure should be checked before starting treatment with ARAVA and monitored periodically thereafter [ see Adverse Reactions (6.1)] .
6. Adverse Reactions/Side Effects
The following serious adverse reactions are described elsewhere in the labeling:
- Hepatotoxicity [see Warnings and Precautions (5.2)]
- Immunosuppression [see Warnings and Precautions (5.4)]
- Bone marrow suppression [see Warnings and Precautions (5.4)]
- Stevens-Johnson syndrome and toxic epidermal necrolysis [see Warnings and Precautions (5.5)]
- Peripheral neuropathy [see Warnings and Precautions (5.7)]
- Interstitial lung disease [see Warnings and Precautions (5.8)]
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
In clinical studies (Trials 1, 2, and 3), 1,865 patients were treated with ARAVA administered as either monotherapy or in combination with methotrexate or sulfasalazine. Patients ranged in age from 19 to 85 years, with an overall median age of 58 years. The mean duration of RA was 6 years ranging from 0 to 45 years.
Elevation of Liver Enzymes
Treatment with ARAVA was associated with elevations of liver enzymes, primarily ALT and AST, in a significant number of patients; these effects were generally reversible. Most transaminase elevations were mild (≤2-fold ULN) and usually resolved while continuing treatment. Marked elevations (>3-fold ULN) occurred infrequently and reversed with dose reduction or discontinuation of treatment. Table 1 shows liver enzyme elevations seen with monthly monitoring in clinical trials Trial 1 and Trial 2. It was notable that the absence of folate use in Trial 3 was associated with a considerably greater incidence of liver enzyme elevation on methotrexate.
| Trial 1 | Trial 2 | Trial 3 * | ||||||
|---|---|---|---|---|---|---|---|---|
| ARAVA | PL | MTX | ARAVA | PL | SSZ | ARAVA | MTX | |
| 20 mg/day
(n= 182) | (n=118) | 7.5–15 mg/wk
(n=182) | 20 mg/day
(n=133) | (n=92) | 2 g/day
(n=133) | 20 mg/day
(n=501) | 7.5–15 mg/wk
(n=498) |
|
| MTX = methotrexate, PL = placebo, SSZ = sulfasalazine, ULN = Upper limit of normal | ||||||||
|
||||||||
| ALT (SGPT) | ||||||||
| >3-fold ULN (n %) | 8(4.4) | 3(2.5) | 5(2.7) | 2(1.5) | 1(1.1) | 2(1.5) | 13(2.6) | 83 (16.7) |
| Reversed to ≤2-fold ULN: | 8 | 3 | 5 | 2 | 1 | 2 | 12 | 82 |
| Timing of Elevation | ||||||||
| 0–3 Months | 6 | 1 | 1 | 2 | 1 | 2 | 7 | 27 |
| 4–6 Months | 1 | 1 | 3 | - | - | - | 1 | 34 |
| 7–9 Months | 1 | 1 | 1 | - | - | - | - | 16 |
| 10–12 Months | - | - | - | - | - | - | 5 | 6 |
In a 6 month study of 263 patients with persistent active rheumatoid arthritis despite methotrexate therapy, and with normal LFTs, ARAVA was administered to a group of 130 patients starting at 10 mg per day and increased to 20 mg as needed. An increase in ALT greater than or equal to three times the ULN was observed in 3.8% of patients compared to 0.8% in 133 patients continued on methotrexate with placebo.
Most Common Adverse Reactions
The most common adverse reactions in ARAVA-treated patients with RA include diarrhea, elevated liver enzymes (ALT and AST), alopecia, and rash. Table 2 displays the most common adverse reactions in the controlled studies in patients with RA at one year (≥5% in any ARAVA treatment group).
| Placebo-Controlled Trials | Active-Controlled Trials | All RA Studies | |||||
|---|---|---|---|---|---|---|---|
| Trial 1 and 2 | Trial 3 * | ||||||
| ARAVA
20 mg/day (n=315) | PL
(n=210) | SSZ
2 g/day (n=133) | MTX
7.5–15 mg/wk (n=182) | ARAVA
20 mg/day (n=501) | MTX
7.5–15 mg/wk (n=498) | ARAVA
(n=1339) † |
|
| MTX = methotrexate, PL = placebo, SSZ = sulfasalazine | |||||||
|
|||||||
| Diarrhea | 27% | 12% | 10% | 20% | 22% | 10% | 17% |
| Headache | 13% | 11% | 12% | 21% | 10% | 8% | 7% |
| Nausea | 13% | 11% | 19% | 18% | 13% | 18% | 9% |
| Rash | 12% | 7% | 11% | 9% | 11% | 10% | 10% |
| Abnormal Liver Enzymes | 10% | 2% | 4% | 10% | 6% | 17% | 5% |
| Alopecia | 9% | 1% | 6% | 6% | 17% | 10% | 10% |
| Hypertension ‡ | 9% | 4% | 4% | 3% | 10% | 4% | 10% |
| Asthenia | 6% | 4% | 5% | 6% | 3% | 3% | 3% |
| Back Pain | 6% | 3% | 4% | 9% | 8% | 7% | 5% |
| GI/Abdominal Pain | 6% | 4% | 7% | 8% | 8% | 8% | 5% |
| Abdominal Pain | 5% | 4% | 4% | 8% | 6% | 4% | 6% |
| Allergic Reaction | 5% | 2% | 0% | 6% | 1% | 2% | 2% |
| Bronchitis | 5% | 2% | 4% | 7% | 8% | 7% | 7% |
| Dizziness | 5% | 3% | 6% | 5% | 7% | 6% | 4% |
| Mouth Ulcer | 5% | 4% | 3% | 10% | 3% | 6% | 3% |
| Pruritus | 5% | 2% | 3% | 2% | 6% | 2% | 4% |
| Rhinitis | 5% | 2% | 4% | 3% | 2% | 2% | 2% |
| Vomiting | 5% | 4% | 4% | 3% | 3% | 3% | 3% |
| Tenosynovitis | 2% | 0% | 1% | 2% | 5% | 1% | 3% |
Adverse events during a second year of treatment with ARAVA in clinical trials were consistent with those observed during the first year of treatment and occurred at a similar or lower incidence.
6.2 Postmarketing Experience
The following additional adverse reactions have been identified during postapproval use of ARAVA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and Lymphatic System: agranulocytosis, leukopenia, neutropenia, pancytopenia
Infection: opportunistic infections, severe infections including sepsis
Gastrointestinal: acute hepatic necrosis, colitis, including microscopic colitis, hepatitis, jaundice/cholestasis, pancreatitis, severe liver injury such as hepatic failure
Immune System: angioedema
Nervous system: peripheral neuropathy
Respiratory: interstitial lung disease, including interstitial pneumonitis and pulmonary fibrosis, which may be fatal, pulmonary hypertension
Skin and Appendages: erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, vasculitis including cutaneous necrotizing vasculitis, cutaneous lupus erythematosus, pustular psoriasis, or worsening psoriasis, skin ulcer
7. Drug Interactions
Following oral administration, leflunomide is metabolized to an active metabolite, teriflunomide, which is responsible for essentially all of leflunomide's in vivo activity. Drug interaction studies have been conducted with both ARAVA (leflunomide) and with its active metabolite, teriflunomide, where the metabolite was directly administered to the test subjects.
8. Use In Specific Populations
8.3 Females and Males of Reproductive Potential
ARAVA may cause fetal harm when administered during pregnancy. Advise females of the potential risk to the fetus. Advise females to notify their healthcare provider immediately if pregnancy occurs or is suspected during treatment [see Use in Specific Populations (8.1)] .
Women receiving ARAVA treatment who wish to become pregnant should discontinue ARAVA and undergo an accelerated drug elimination procedure to achieve plasma teriflunomide concentrations of less than 0.02 mg/L (0.02 mcg/mL) [see Warnings and Precautions (5.3)] .
8.4 Pediatric Use
The safety and effectiveness of ARAVA in pediatric patients have not been established.
The safety and effectiveness of ARAVA in the treatment of polyarticular course juvenile idiopathic arthritis (JIA) was evaluated in a single multicenter, double-blind, active-controlled trial in 94 pediatric patients (1:1 randomization) with polyarticular course juvenile idiopathic arthritis (JIA) as defined by the American College of Rheumatology (ACR). In this population, ARAVA treatment was found not to be effective.
The safety of ARAVA was studied in 74 patients with polyarticular course JIA ranging in age from 3–17 years (47 patients from the active-controlled study and 27 from an open-label safety and pharmacokinetic study). The most common adverse events included abdominal pain, diarrhea, nausea, vomiting, oral ulcers, upper respiratory tract infections, alopecia, rash, headache, and dizziness. Less common adverse events included anemia, hypertension, and weight loss. Fourteen pediatric patients experienced ALT and/or AST elevations, nine between 1.2 and 3-fold the upper limit of normal, and five between 3 and 8-fold the upper limit of normal.
8.5 Geriatric Use
Of the total number of subjects in controlled clinical trials (Trials 1, 2, and 3) of ARAVA, 234 subjects were 65 years and over [see Clinical Studies (14)] . No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. No dosage adjustment is needed in patients over 65.
8.6 Hepatic Impairment
Dedicated studies of the effect of hepatic impairment on leflunomide pharmacokinetics have not been conducted. Given the need to metabolize leflunomide into the active species, the role of the liver in drug elimination/recycling, and the possible risk of increased hepatic toxicity, the use of ARAVA in patients with hepatic impairment is not recommended.
10. Overdosage
There have been reports of chronic overdose in patients taking ARAVA at daily dose up to five times the recommended daily dose and reports of acute overdose in adults and children. Adverse events were consistent with the safety profile for ARAVA [see Adverse Reactions (6)] . The most frequent adverse events observed were diarrhea, abdominal pain, leukopenia, anemia, and elevated liver function tests.
In the event of a significant overdose or toxicity, perform an accelerated drug elimination procedure to accelerate elimination [see Warnings and Precautions (5.3)] .
Studies with both hemodialysis and CAPD (chronic ambulatory peritoneal dialysis) indicate that teriflunomide, the primary metabolite of leflunomide, is not dialyzable [see Clinical Pharmacology (12.3)] .
11. Arava Description
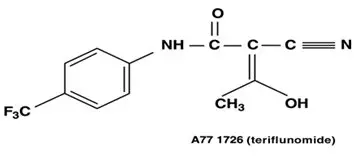
ARAVA (leflunomide) is a pyrimidine synthesis inhibitor. The chemical name for leflunomide is N-(4´-trifluoromethylphenyl)-5-methylisoxazole-4-carboxamide. It has an empirical formula C 12H 9F 3N 2O 2, a molecular weight of 270.2 and the following structural formula:
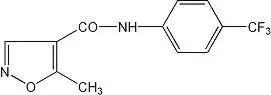
ARAVA is available for oral administration as tablets containing 10, 20, or 100 mg of active drug. Combined with leflunomide are the following inactive ingredients: colloidal silicon dioxide, crospovidone, hypromellose, lactose monohydrate, magnesium stearate, polyethylene glycol, povidone, starch, talc, titanium dioxide, and yellow ferric oxide (20 mg tablet only).
12. Arava - Clinical Pharmacology
12.1 Mechanism of Action
Leflunomide is an isoxazole immunomodulatory agent that inhibits dihydroorotate dehydrogenase (a mitochondrial enzyme involved in de novo pyrimidine synthesis) and has antiproliferative activity. Several in vivo and in vitro experimental models have demonstrated an anti-inflammatory effect.
12.3 Pharmacokinetics
Following oral administration, leflunomide is metabolized to an active metabolite, teriflunomide, which is responsible for essentially all of leflunomide's in vivo activity. Plasma concentrations of the parent drug, leflunomide, have been occasionally seen at very low concentrations. Studies of the pharmacokinetics of leflunomide have primarily examined the plasma concentrations of the active metabolite, teriflunomide.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No evidence of carcinogenicity was observed in a 2-year bioassay in rats at oral doses of leflunomide up to the maximally tolerated dose of 6 mg/kg (approximately 1/40 the maximum human teriflunomide systemic exposure based on AUC). However, male mice in a 2-year bioassay exhibited an increased incidence in lymphoma at an oral dose of 15 mg/kg, the highest dose studied (1.7 times the human teriflunomide exposure based on AUC). Female mice, in the same study, exhibited a dose-related increased incidence of bronchoalveolar adenomas and carcinomas combined beginning at 1.5 mg/kg (approximately 1/10 the human teriflunomide exposure based on AUC). The significance of the findings in mice relative to the clinical use of ARAVA is not known.
Leflunomide was not mutagenic in the Ames assay, the unscheduled DNA synthesis assay, or in the HGPRT gene mutation assay. In addition, leflunomide was not clastogenic in the in vivo mouse micronucleus assay or in the in vivo Chinese hamster bone marrow cell cytogenic test. However, 4-trifluoromethylaniline (TFMA), a minor metabolite of leflunomide, was mutagenic in the Ames assay and in the HGPRT gene mutation assay, and was clastogenic in the in vitro Chinese hamster cell chromosomal aberration assay. TFMA was not clastogenic in the in vivo mouse micronucleus assay or in the in vivo Chinese hamster bone marrow cell cytogenic test.
Leflunomide had no effect on fertility or reproductive performance in either male or female rats at oral doses up to 4.0 mg/kg (approximately 1/30 the human teriflunomide exposure based on AUC) [see Use in Specific Populations (8.1, 8.6)] .
14. Clinical Studies
The efficacy of ARAVA in the treatment of rheumatoid arthritis (RA) was demonstrated in three controlled trials showing reduction in signs and symptoms, and inhibition of structural damage. In two placebo controlled trials, efficacy was demonstrated for improvement in physical function. In these trials, efficacy was evaluated by:
- 1. Reduction of signs and symptoms
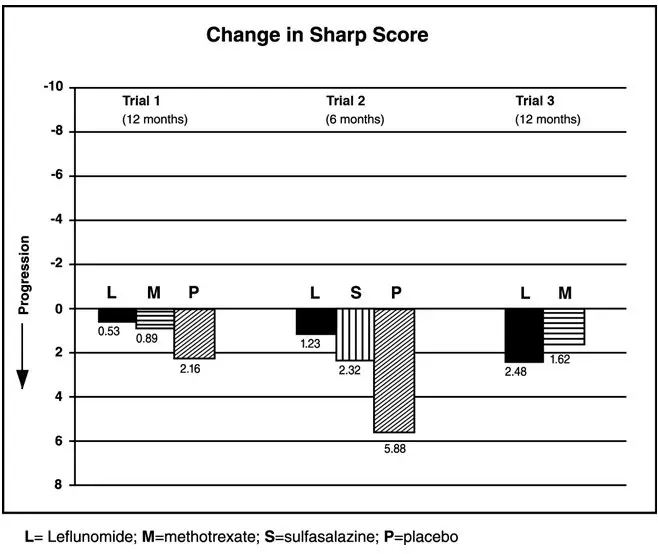
Relief of signs and symptoms was assessed using the American College of Rheumatology (ACR) 20 Responder Index, a composite of clinical, laboratory, and functional measures in rheumatoid arthritis. An "ACR20 Responder" is a patient who had ≥20% improvement in both tender and swollen joint counts and in 3 of the following 5 criteria: physician global assessment, patient global assessment, functional ability measure (Modified Health Assessment Questionnaire [MHAQ]), visual analog pain scale, and erythrocyte sedimentation rate or C-reactive protein. An "ACR20 Responder at Endpoint" is a patient who completed the study and was an ACR20 Responder at the completion of the study. - 2. Inhibition of structural damage
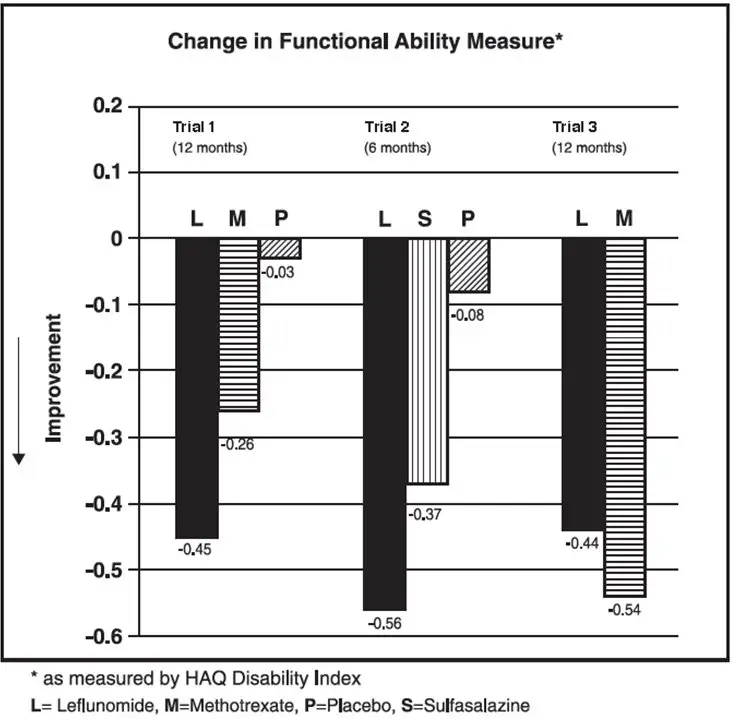
Inhibition of structural damage compared to control was assessed using the Sharp score, a composite score of x-ray erosions and joint space narrowing in hands/wrists and forefeet. - 3. Improvement in physical function
Improvement in physical function was assessed using the Health Assessment Questionnaire (HAQ) and the Medical Outcomes Survey Short Form (SF-36).
In all ARAVA trials, participants of at least 18 years of age and in ARA functional class of I, II, or III received an initial loading dose of 100 mg leflunomide per day for three days, followed by 20 mg per day thereafter.
Exclusion criteria included patients with a history of hypersensitivity to the study medication; women who were pregnant or breastfeeding and men or women of child bearing age and potential who had not received contraceptives for at least 4 weeks before entering the study and to be maintained throughout the study and for at least 6 months after discontinuing treatment; patients with a history of inflammatory disease, impaired renal function or liver impairment, cardiac failure, congenital or acquired immunodeficiency, impaired coagulation, or a history of recent major traumatic injury; and patients taking intra-articular or systemic concomitant medications which could affect the safety and/or efficacy of the study medication.
Clinical Trial Results
Clinical response
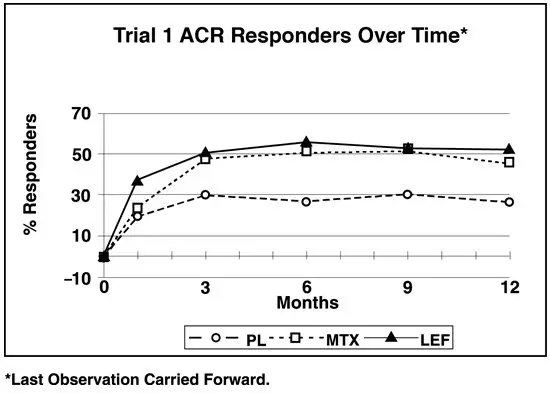
The ACR20 Responder at Endpoint rates are shown in Figure 1. ARAVA was statistically significantly superior to placebo in reducing the signs and symptoms of RA by the primary efficacy analysis, ACR20 Responder at Endpoint, in study Trial 1 (at the primary 12 months endpoint) and Trial 2 (at 6 month endpoint). ACR20 Responder at Endpoint rates with ARAVA treatment were consistent across the 6 and 12 month studies (41%–49%). No consistent differences were demonstrated between leflunomide and methotrexate or between leflunomide and sulfasalazine. ARAVA treatment effect was evident by 1 month, stabilized by 3 to 6 months, and continued throughout the course of treatment as shown in Figure 1.
Figure 1: Percentage of ACR20 Responders at Endpoint in Patients with Active RA in Trials 1, 2, and 3
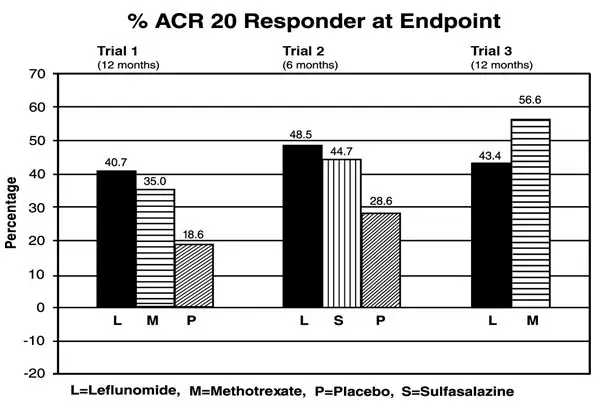
| Comparisons | 95% Confidence Interval | p Value | |
|---|---|---|---|
| Trial 1 | ARAVA vs Placebo | (12, 32) | <0.0001 |
| Methotrexate vs Placebo | (8, 30) | <0.0001 | |
| ARAVA vs Methotrexate | (-4, 16) | NS | |
| Trial 2 | ARAVA vs Placebo | (7, 33) | 0.0026 |
| Sulfasalazine vs Placebo | (4, 29) | 0.0121 | |
| ARAVA vs Sulfasalazine | (-8, 16) | NS | |
| Trial 3 | ARAVA vs Methotrexate | (-19, -7) | <0.0001 |
Figure 2: ACR20 Responders over Time in Patients with Active RA in Trial 1*
ACR50 and ACR70 Responders are defined in an analogous manner to the ACR 20 Responder, but use improvements of 50% or 70%, respectively (Table 3). Mean change for the individual components of the ACR Responder Index are shown in Table 4.
| Study and Treatment Group | ACR20 | ACR50 | ACR70 |
|---|---|---|---|
|
|||
| Placebo-Controlled Studies | |||
| Trial 1 (12 months) | |||
| ARAVA (n=178) † | 52 ‡ | 34 ‡ | 20 ‡ |
| Placebo (n=118) † | 26 | 8 | 4 |
| Methotrexate (n=180) † | 46 | 23 | 9 |
| Trial 2 (6 months) | |||
| ARAVA (n=130) † | 55 ‡ | 33 ‡ | 10 § |
| Placebo (n=91) † | 29 | 14 | 2 |
| Sulfasalazine (n=132) † | 57 | 30 | 8 |
| Non-Placebo Active-Controlled Studies | |||
| Trial 3 (12 months) | |||
| ARAVA (n=495) † | 51 | 31 | 10 |
| Methotrexate (n=489) † | 65 | 44 | 16 |
Table 4 shows the results of the components of the ACR response criteria for Trial 1, Trial 2, and Trial 3. ARAVA was significantly superior to placebo in all components of the ACR Response criteria in study Trial 1 and Trial 2. In addition, ARAVA was significantly superior to placebo in improving morning stiffness, a measure of RA disease activity, not included in the ACR Response criteria. No consistent differences were demonstrated between ARAVA and the active comparators.
| Components | Placebo-Controlled Studies | Non–Placebo-Controlled Study | ||||||
|---|---|---|---|---|---|---|---|---|
| Trial 1 (12 months) | Trial 2 Non-US
(6 months) | Trial 3 Non-US
(12 months) |
||||||
| Leflunomide | Methotrexate | Placebo | Leflunomide | Sulfasalazine | Placebo | Leflunomide | Methotrexate | |
|
||||||||
| Tender joint count † | -7.7 | -6.6 | -3.0 | -9.7 | -8.1 | -4.3 | -8.3 | -9.7 |
| Swollen joint count † | -5.7 | -5.4 | -2.9 | -7.2 | -6.2 | -3.4 | -6.8 | -9.0 |
| Patient global assessment ‡ | -2.1 | -1.5 | 0.1 | -2.8 | -2.6 | -0.9 | -2.3 | -3.0 |
| Physician global assessment ‡ | -2.8 | -2.4 | -1.0 | -2.7 | -2.5 | -0.8 | -2.3 | -3.1 |
| Physical function/disability
(MHAQ/HAQ) | -0.29 | -0.15 | 0.07 | -0.50 | -0.29 | -0.04 | -0.37 | -0.44 |
| Pain intensity ‡ | -2.2 | -1.7 | -0.5 | -2.7 | -2.0 | -0.9 | -2.1 | -2.9 |
| Erythrocyte Sedimentation rate | -6.26 | -6.48 | 2.56 | -7.48 | -16.56 | 3.44 | -10.12 | -22.18 |
| C-reactive protein | -0.62 | -0.50 | 0.47 | -2.26 | -1.19 | 0.16 | -1.86 | -2.45 |
| Not included in the ACR Responder Index | ||||||||
| Morning Stiffness (min) | -101.4 | -88.7 | 14.7 | -93.0 | -42.4 | -6.8 | -63.7 | -86.6 |
16. How is Arava supplied
How Supplied
ARAVA (leflunomide) Tablets
| Strength | Quantity | NDC Number | Description |
|---|---|---|---|
| 10 mg | 30 count bottle | 0088-2160-30 | White, round film-coated tablet embossed with "ZBN" on one side. |
| 20 mg | 30 count bottle | 0088-2161-30 | Light yellow, triangular film-coated tablet embossed with "ZBO" on one side. |
| 100 mg | 3 count blister pack | 0088-2162-33 | White, round film-coated tablet embossed with "ZBP" on one side. |
| ARAVA
leflunomide tablet, film coated |
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| ARAVA
leflunomide tablet, film coated |
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
| ARAVA
leflunomide tablet, film coated |
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| Labeler - sanofi-aventis U.S. LLC (783243835) |
| Registrant - Sanofi (739980787) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| OPELLA HEALTHCARE INTERNATIONAL SAS | 275857012 | analysis(0088-2160, 0088-2161, 0088-2162) , manufacture(0088-2160, 0088-2161, 0088-2162) , pack(0088-2160, 0088-2161, 0088-2162) , label(0088-2160, 0088-2161, 0088-2162) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| EUROAPI Germany GmbH | 343459891 | api manufacture(0088-2160, 0088-2161, 0088-2162) | |