Drug Detail:Aspruzyo sprinkle (Ranolazine [ ra-noe-la-zeen ])
Drug Class: Antianginal agents
Highlights of Prescribing Information
ASPRUZYO SPRINKLETM (ranolazine) extended-release granules, for oral use
Initial U.S. Approval: 2006
Indications and Usage for Aspruzyo Sprinkle
ASPRUZYO Sprinkle is an antianginal indicated for the treatment of chronic angina. (1) (1)
Aspruzyo Sprinkle Dosage and Administration
500 mg orally twice daily and increase to 1000 mg orally twice daily, based on clinical symptoms (2.1) (2)
Dosage Forms and Strengths
Extended-release granules: 500 and 1000 mg (3) (3)
Contraindications
- •
- Strong CYP3A inhibitors (e.g., ketoconazole, clarithromycin, nelfinavir) (4, 7.1)
- •
- CYP3A inducers (e.g., rifampin, phenobarbital, St. John's wort) (4, 7.1)
- •
- Liver cirrhosis (4, 8.6)
Warnings and Precautions
- •
- QT interval prolongation: Can occur with ranolazine. Little information available on high doses, long exposure, use with QT interval‑ prolonging drugs, potassium channel variants causing prolonged QT interval, in patients with a family history of (or congenital) long QT syndrome, or in patients with known acquired QT interval prolongation. (5.1)
- •
- Renal failure: Monitor renal function after initiation and periodically in patients with moderate to severe renal impairment (CrCL <60 mL/min). If acute renal failure develops, discontinue ASPRUZYO Sprinkle. (5.2)
Adverse Reactions/Side Effects
Most common adverse reactions (> 4% and more common than with placebo) are dizziness, headache, constipation, nausea. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Sun Pharmaceutical Industries, Inc. at 1-800-818-4555 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- •
- Moderate CYP3A inhibitors (e.g., diltiazem, verapamil, erythromycin): Limit ASPRUZYO Sprinkle to 500 mg twice daily. (7.1)
- •
- P-gp inhibitors (e.g., cyclosporine): Ranolazine exposure increased. Titrate ASPRUZYO Sprinkle based on clinical response. (7.1)
- •
- CYP3A substrates: Limit simvastatin to 20 mg when used with ASPRUZYO Sprinkle. Doses of other sensitive CYP3A substrates (e.g., lovastatin) and CYP3A substrates with narrow therapeutic range (e.g., cyclosporine, tacrolimus, sirolimus) may need to be reduced with ASPRUZYO Sprinkle. (7.2)
- •
- OCT2 substrates: Limit the dose of metformin to 1700 mg daily when used with ASPRUZYO Sprinkle 1000 mg twice daily. Doses of other OCT2 substrates may require adjusted doses. (7.2)
- •
- Drugs transported by P-gp (e.g., digoxin), or drugs metabolized by CYP2D6 (e.g., tricyclic antidepressants) may need reduced doses when used with ASPRUZYO Sprinkle. (7.2)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 3/2022
Related/similar drugs
amlodipine, metoprolol, aspirin, carvedilol, propranolol, atenololFull Prescribing Information
1. Indications and Usage for Aspruzyo Sprinkle
ASPRUZYO Sprinkle is indicated for the treatment of chronic angina.
ASPRUZYO Sprinkle may be used with beta-blockers, nitrates, calcium channel blockers, anti‑platelet therapy, lipid-lowering therapy, ACE inhibitors, and angiotensin receptor blockers.
2. Aspruzyo Sprinkle Dosage and Administration
2.1 Dosing Information
Initiate ASPRUZYO Sprinkle dosing at 500 mg orally twice daily and increase to 1000 mg orally twice daily, as needed, based on clinical symptoms.
The maximum recommended daily dose of ASPRUZYO Sprinkle is 1000 mg twice daily.
If a dose of ASPRUZYO Sprinkle is missed, take the prescribed dose at the next scheduled time; do not double the next dose.
Directions for use with soft food (e.g., applesauce and yogurt)
- •
- Sprinkle granules on one tablespoonful of soft food and consume immediately.
- •
- Do not crush or chew the granules.
Direction for nasogastric and gastric tube administration
Nasogastric (NG) tube: Add the content of a sachet to a plastic catheter tip syringe and add 50 mL of water. Gently shake the syringe for approximately 15 seconds. Promptly deliver through a 12 French or larger NG tube. Ensure no granules are left in the syringe. Rinse with additional water (about 15 mL) if needed.
Gastrostomy/Gastric (G) tube: Add the content of a sachet to a plastic catheter tip syringe and add 30 mL of water. Gently shake the syringe for approximately 15 seconds. Promptly deliver through a 12 French or larger G-tube. Rinse with 20 mL of water in the syringe. Ensure no granules are left in the syringe. Rinse with additional water (about 15 mL) if needed.
2.2 Dose Modification
Dose adjustments may be needed when ASPRUZYO Sprinkle is taken in combination with other drugs [see Drug Interactions (7.1)]. Limit the maximum dose of ASPRUZYO Sprinkle to 500 mg twice daily in patients on moderate CYP3A inhibitors such as diltiazem, verapamil, and erythromycin. Use of ASPRUZYO Sprinkle with strong CYP3A inhibitors and CYP3A inducers is contraindicated [see Contraindications (4), Drug Interactions (7.1)].
3. Dosage Forms and Strengths
ASPRUZYO Sprinkle (ranolazine) is supplied as unit-dose sachets containing 500 or 1000 mg of white to off-white, coated, extended-release granules.
4. Contraindications
ASPRUZYO Sprinkle is contraindicated in patients:
- •
- Taking strong inhibitors of CYP3A [see Drug Interactions (7.1)]
- •
- Taking inducers of CYP3A [see Drug Interactions (7.1)]
- •
- With liver cirrhosis [see Use in Specific Populations (8.6)]
5. Warnings and Precautions
5.1 QT Interval Prolongation
Ranolazine blocks IKr and prolongs the QTc interval in a dose-related manner. Clinical experience in an acute coronary syndrome population did not show an increased risk of proarrhythmia or sudden death [see Clinical Studies (14.2)]. However, there is little experience with high doses (> 1000 mg twice daily) or exposure, other QT‑prolonging drugs, potassium channel variants resulting in a long QT interval, in patients with a family history of (or congenital) long QT syndrome, or in patients with known acquired QT interval prolongation.
5.2 Renal Failure
Acute renal failure has been observed in patients with severe renal impairment (creatinine clearance [CrCL] < 30 mL/min) while taking ranolazine. If acute renal failure develops (e.g., marked increase in serum creatinine associated with an increase in blood urea nitrogen [BUN]), discontinue ASPRUZYO Sprinkle and treat appropriately [see Use in Specific Populations (8.7)].
Monitor renal function after initiation and periodically in patients with moderate to severe renal impairment (CrCL < 60 mL/min) for increases in serum creatinine accompanied by an increase in BUN.
6. Adverse Reactions/Side Effects
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
A total of 2018 patients with chronic angina were treated with ranolazine in controlled clinical trials. Of the patients treated with ranolazine, 1026 were enrolled in three double‑blind, placebo-controlled, randomized studies (CARISA, ERICA, MARISA) of up to 12 weeks' duration. In addition, upon study completion, 1251 patients received treatment with ranolazine in open-label, long-term studies; 1227 patients were exposed to ranolazine for more than 1 year, 613 patients for more than 2 years, 531 patients for more than 3 years, and 326 patients for more than 4 years.
At recommended doses, about 6% of patients discontinued treatment with ranolazine because of an adverse event in controlled studies in angina patients compared to about 3% on placebo. The most common adverse events that led to discontinuation more frequently on ranolazine than placebo were dizziness (1.3% versus 0.1%), nausea (1% versus 0%), asthenia, constipation, and headache (each about 0.5% versus 0%). Doses above 1000 mg twice daily are poorly tolerated.
In controlled clinical trials of angina patients, the most frequently reported treatment‑emergent adverse reactions (> 4% and more common on ranolazine than on placebo) were dizziness (6.2%), headache (5.5%), constipation (4.5%), and nausea (4.4%). Dizziness may be dose-related. In open-label, long-term treatment studies, a similar adverse reaction profile was observed.
The following additional adverse reactions occurred at an incidence of 0.5 to 4.0% in patients treated with ranolazine and were more frequent than the incidence observed in placebo-treated patients:
Cardiac Disorders- bradycardia, palpitations
Ear and Labyrinth Disorders- tinnitus, vertigo
Eye Disorders- blurred vision
Gastrointestinal Disorders- abdominal pain, dry mouth, vomiting, dyspepsia
General Disorders and Administrative Site Adverse Events- asthenia, peripheral edema
Metabolism and Nutrition Disorders- anorexia
Nervous System Disorders- syncope (vasovagal)
Psychiatric Disorders- confusional state
Renal and Urinary Disorders- hematuria
Respiratory, Thoracic, and Mediastinal Disorders- dyspnea
Skin and Subcutaneous Tissue Disorders- hyperhidrosis
Vascular Disorders- hypotension, orthostatic hypotension
Other (< 0.5%) but potentially medically important adverse reactions observed more frequently with ranolazine than placebo treatment in all controlled studies included: angioedema, renal failure, eosinophilia, chromaturia, blood urea increased, hypoesthesia, paresthesia, tremor, pulmonary fibrosis, thrombocytopenia, leukopenia, and pancytopenia.
A large clinical trial in acute coronary syndrome patients was unsuccessful in demonstrating a benefit for ranolazine, but there was no apparent proarrhythmic effect in these high-risk patients [see Clinical Studies (14.2)].
Laboratory Abnormalities:
Ranolazine produces elevations of serum creatinine by 0.1 mg/dL, regardless of previous renal function, likely because of inhibition of creatinine's tubular secretion. In general, the elevation has a rapid onset, shows no signs of progression during long-term therapy, is reversible after discontinuation of ranolazine, and is not accompanied by changes in BUN. In healthy volunteers, ranolazine 1000 mg twice daily had no effect upon the glomerular filtration rate. More marked and progressive increases in serum creatinine, associated with increases in BUN or potassium, indicating acute renal failure, have been reported after initiation of ranolazine in patients with severe renal impairment [see Warnings and Precautions (5.2), Use in Specific Populations (8.7)].
6.2 Post-marketing Experience
The following adverse reactions have been identified during post-approval use of ranolazine. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure:
Nervous System Disorders- Abnormal coordination, myoclonus, paresthesia, tremor, and other serious neurologic adverse events have been reported to occur, sometimes concurrently, in patients taking ranolazine. The onset of events was often associated with an increase in ranolazine dose or exposure. Many patients reported symptom resolution following drug discontinuation or dose decrease.
Metabolism and Nutrition Disorders- Cases of hypoglycemia have been reported in diabetic patients on antidiabetic medication.
Psychiatric Disorders- hallucination
Renal and Urinary Disorders- dysuria, urinary retention
Skin and Subcutaneous Tissue Disorders- angioedema, pruritus, rash
7. Drug Interactions
7.1 Effects of Other Drugs on Ranolazine
Strong CYP3A Inhibitors
Concomitant use of ASPRUZYO Sprinkle with strong CYP3A inhibitors, including ketoconazole, itraconazole, clarithromycin, nefazodone, nelfinavir, ritonavir, indinavir, and saquinavir is contraindicated [see Contraindications (4), Clinical Pharmacology (12.3)].
Moderate CYP3A Inhibitors
Limit the dose of ASPRUZYO Sprinkle to 500 mg twice daily in patients on moderate CYP3A inhibitors, including diltiazem, verapamil, erythromycin, fluconazole, and grapefruit juice or grapefruit-containing products [see Dosage and Administration (2.2), Clinical Pharmacology (12.3)].
P-gp Inhibitors
Concomitant use of ASPRUZYO Sprinkle and P-gp inhibitors, such as cyclosporine, may result in increases in ranolazine concentrations. Titrate ASPRUZYO Sprinkle based on clinical response in patients concomitantly treated with predominant P-gp inhibitors such as cyclosporine [see Dosage and Administration (2.2)].
CYP3A Inducers
Concomitant use of ASPRUZYO Sprinkle with CYP3A inducers such as rifampin, rifabutin, rifapentine, phenobarbital, phenytoin, carbamazepine, and St. John's wort is contraindicated [see Contraindications (4), Clinical Pharmacology (12.3)].
Alcohol
An in-vitro dissolution study was conducted to evaluate the impact of alcohol on extended-release characteristics of ASPRUZYO Sprinkle. The in-vitro study showed that alcohol causes a rapid release of ranolazine from ASPRUZYO Sprinkle that may increase the risk of adverse events associated with ASPRUZYO Sprinkle. Patients should not consume alcohol when taking ASPRUZYO Sprinkle [see Clinical Pharmacology (12.3)].
7.2 Effects of Ranolazine on Other Drugs
Drugs Metabolized by CYP3A
Limit the dose of simvastatin in patients on any dose of ASPRUZYO Sprinkle to 20 mg once daily, when ASPRUZYO Sprinkle is co-administered. Dose adjustment of other sensitive CYP3A substrates (e.g., lovastatin) and CYP3A substrates with a narrow therapeutic range (e.g., cyclosporine, tacrolimus, sirolimus) may be required as ASPRUZYO Sprinkle may increase plasma concentrations of these drugs [see Clinical Pharmacology (12.3)].
Drugs Transported by P-gp
Concomitant use of ASPRUZYO Sprinkle and digoxin results in increased exposure to digoxin. The dose of digoxin may have to be adjusted [see Clinical Pharmacology (12.3)].
Drugs Metabolized by CYP2D6
The exposure to CYP2D6 substrates, such as tricyclic antidepressants and antipsychotics, may be increased during co-administration with ASPRUZYO Sprinkle, and lower doses of these drugs may be required.
Drugs Transported by OCT2
In subjects with type 2 diabetes mellitus, concomitant use of ASPRUZYO Sprinkle 1000 mg twice daily and metformin results in increased plasma levels of metformin. When ASPRUZYO Sprinkle 1000 mg twice daily is co-administered with metformin, metformin dose should not exceed 1700 mg/day. Monitor blood glucose levels and risks associated with high exposures of metformin.
Metformin exposure was not significantly increased when given with ranolazine 500 mg twice daily [see Clinical Pharmacology (12.3)].
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
There are no available data on ranolazine use in pregnant women to inform any drug‑associated risks. Studies in rats and rabbits showed no evidence of fetal harm at exposures 4 times the maximum recommended human dose (MRHD) (see Data).
In the U.S. general population, the estimated background risk of major birth defects and of miscarriage of clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Animal Data
Embryofetal toxicity studies were conducted in rats and rabbits orally administered ranolazine during organogenesis. In rats, decreased fetal weight and reduced ossification were observed at doses (corresponding to 4-fold the AUC for the MRHD) that caused maternal weight loss. No adverse fetal effects were observed in either species exposed (AUC) to ranolazine at exposures (AUC) equal to the MRHD.
8.2 Lactation
Risk Summary
There are no data on the presence of ranolazine in human milk, the effects on the breastfed infant, or the effects on milk production. However, ranolazine is present in rat milk [see Use in Specific Populations (8.1)]. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for ranolazine and any potential adverse effects on the breastfed infant from ranolazine or from the underlying maternal condition.
Adult female rats were administered ranolazine orally from gestation day 6 through postnatal day 20. No adverse effects on pup development, behavior, or reproduction parameters were observed at a maternal dosage level of 60 mg/kg/day (equal to the MHRD based on AUC). At maternally toxic doses, male and female pups exhibited increased mortality and decreased body weight, and female pups showed increased motor activity. The pups were potentially exposed to low amounts of ranolazine via the maternal milk.
8.5 Geriatric Use
Of the chronic angina patients treated with ranolazine in controlled studies, 496 (48%) were ≥ 65 years of age, and 114 (11%) were ≥ 75 years of age. No overall differences in efficacy were observed between older and younger patients. There were no differences in safety for patients ≥ 65 years compared to younger patients, but patients ≥ 75 years of age on ranolazine, compared to placebo, had a higher incidence of adverse events, serious adverse events, and drug discontinuations due to adverse events. In general, dose selection for an elderly patient should usually start at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease, or other drug therapy.
8.6 Use in Patients with Hepatic Impairment
ASPRUZYO Sprinkle is contraindicated in patients with liver cirrhosis. In a study of cirrhotic patients, the Cmax of ranolazine was increased 30% in cirrhotic patients with mild (Child‑ Pugh Class A) hepatic impairment but increased 80% in cirrhotic patients with moderate (Child-Pugh Class B) hepatic impairment compared to patients without hepatic impairment. This increase was not enough to account for the 200% increase in QT prolongation seen in cirrhotic patients with mild to moderate hepatic impairment [see Clinical Pharmacology (12.2)].
8.7 Use in Patients with Renal Impairment
A pharmacokinetic study of ranolazine in subjects with severe renal impairment (CrCL< 30 mL/min) was stopped when 2 of 4 subjects developed acute renal failure after receiving ranolazine 500 mg twice daily for 5 days (lead-in phase) followed by 1000 mg twice a day (1 dose in one subject and 11 doses in the other). Increases in creatinine, BUN, and potassium were observed in 3 subjects during the 500 mg lead-in phase. One subject required hemodialysis, while the other 2 subjects improved upon drug discontinuation [see Warnings and Precautions (5.2)]. Monitor renal function periodically in patients with moderate to severe renal impairment. Discontinue ASPRUZYO Sprinkle if acute renal failure develops.
In a separate study, Cmax was increased between 40% and 50% in patients with mild, moderate, or severe renal impairment compared to patients with no renal impairment, suggesting a similar increase in exposure in patients with renal failure independent of the degree of impairment. The pharmacokinetics of ranolazine has not been assessed in patients on dialysis.
10. Overdosage
Hypotension, QT prolongation, bradycardia, myoclonic activity, severe tremor, unsteady gait/incoordination, dizziness, nausea, vomiting, dysphasia, and hallucinations have been seen in cases of oral overdose of ranolazine. In cases of extreme overdose of ranolazine fatal outcomes have been reported. In clinical studies, high intravenous exposure resulted in diplopia, paresthesia, confusion, and syncope.
In addition to general supportive measures, continuous ECG monitoring may be warranted in the event of overdose.
Since ranolazine is about 62% bound to plasma proteins, hemodialysis is unlikely to be effective in clearing ranolazine.
11. Aspruzyo Sprinkle Description
ASPRUZYO Sprinkle contains ranolazine, an antianginal available as white to off-white coated extended-release granules filled in a sachet for oral administration.
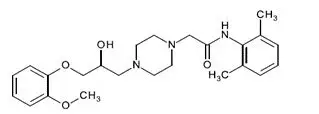
Ranolazine is a racemic mixture, chemically described as 1-piperazineacetamide, N‑(2,6-dimethylphenyl)-4-[2-hydroxy-3-(2-methoxyphenoxy)propyl]-(±)-. It has a molecular formula of C24H33N3O4, a molecular weight of 427.54 g/mole, and the following structural formula:
Ranolazine is off-white to white powder. Ranolazine is soluble in dichloromethane and methanol.
ASPRUZYO Sprinkle contains 500 mg or 1000 mg of ranolazine and the following inactive ingredients: amino methacrylate copolymer, dibutyl sebacate, ethyl cellulose, hypromellose, magnesium stearate, methacrylic acid and ethyl acrylate copolymer, microcrystalline cellulose, and talc.
12. Aspruzyo Sprinkle - Clinical Pharmacology
12.1 Mechanism of Action
The mechanism of action of ranolazine's antianginal effects has not been determined. Ranolazine has anti-ischemic and antianginal effects that do not depend upon reductions in heart rate or blood pressure. It does not affect the rate-pressure product, a measure of myocardial work, at maximal exercise. Ranolazine at therapeutic levels can inhibit the cardiac late sodium current (INa). However, the relationship of this inhibition to angina symptoms is uncertain.
The QT prolongation effect of ranolazine on the surface electrocardiogram is the result of inhibition of IKr which prolongs the ventricular action potential.
12.2 Pharmacodynamics
Hemodynamic Effects
Patients with chronic angina treated with ranolazine in controlled clinical studies had minimal changes in mean heart rate (< 2 bpm) and systolic blood pressure (< 3 mm Hg). Similar results were observed in subgroups of patients with CHF NYHA Class I or II, diabetes, or reactive airway disease, and in elderly patients.
Electrocardiographic Effects
Dose and plasma concentration-related increases in the QTc interval [see Warnings and Precautions (5.1)], reductions in T wave amplitude, and, in some cases, notched T waves, have been observed in patients treated with ranolazine. These effects are believed to be caused by ranolazine and not by its metabolites. The relationship between the change in QTc and ranolazine plasma concentrations is linear, with a slope of about 2.6 msec/1000 ng/mL, through exposures corresponding to doses several-fold higher than the maximum recommended dose of 1000 mg twice daily. The variable blood levels attained after a given dose of ranolazine give a wide range of effects on QTc. At Tmax following repeat dosing at 1000 mg twice daily, the mean change in QTc is about 6 msec, but in the 5% of the population with the highest plasma concentrations, the prolongation of QTc is at least 15 msec. In cirrhotic subjects with mild or moderate hepatic impairment, the relationship between plasma level of ranolazine and QTc is much steeper [see Contraindications (4)].
Age, weight, gender, race, heart rate, congestive heart failure, diabetes, and renal impairment did not alter the slope of the QTc-concentration relationship of ranolazine.
No proarrhythmic effects were observed on 7-day Holter recordings in 3,162 acute coronary syndrome patients treated with ranolazine. There was a significantly lower incidence of arrhythmias (ventricular tachycardia, bradycardia, supraventricular tachycardia, and new atrial fibrillation) in patients treated with ranolazine (80%) versus placebo (87%), including ventricular tachycardia ≥ 3 beats (52% versus 61%). However, this difference in arrhythmias did not lead to a reduction in mortality, a reduction in arrhythmia hospitalization, or a reduction in arrhythmia symptoms.
12.3 Pharmacokinetics
The pharmacokinetic parameter of ranolazine after single dose administration of 1000 mg ASPRUZYO Sprinkle under fasting conditions are summarized in table 1.
Table 1: Pharmacokinetic parameters of ranolazine after single dose administration of 1000 mg ASPRUZYO Sprinkle under fasting conditions.
|
Parameter |
ASPRUZYO Sprinkle |
|
|
Mean |
CV (%) |
|
|
Cmax (mcg/mL) |
1.95 |
30 |
|
Tmax (hr)* |
10 (2 to 16) | |
|
AUC0-t (mcg.hr/mL) |
31.4 |
36 |
|
AUC0-∞ (mcg.hr/mL) |
31.7 |
36 |
|
T1/2 (hr) |
5.3 |
27 |
|
Kel (hr-1) |
0.15 |
29 |
*Median range (min-max) is provided
Ranolazine is extensively metabolized in the gut and liver and its absorption is highly variable. The pharmacokinetics of the (+) R-and (-) S-enantiomers of ranolazine are similar in healthy volunteers. Steady state is generally achieved within 3 days of twice-daily dosing with ranolazine. At steady state over the dose range of 500 to 1000 mg twice daily, Cmax and AUC0-T increase slightly more than proportionally to dose, 120% and 140%, respectively. With twice-daily dosing, the trough:peak ratio of the ranolazine plasma concentration is 0.3 to 0.6. The pharmacokinetics of ranolazine is unaffected by age and sex.
Absorption and Distribution
After oral administration of ranolazine 1000 mg, median Tmax was 10 hours under fasting conditions and 4.5 to 6 hours under fed. After oral administration of 14C-ranolazine as a solution, 73% of the dose is systemically available as ranolazine or metabolites. The bioavailability of ranolazine from ranolazine granules relative to that from a solution of ranolazine is 76%. Because ranolazine is a substrate of P-gp, inhibitors of P-gp may increase the absorption of ranolazine. Over the concentration range of 0.25 to 10 mcg/mL, ranolazine is approximately 62% bound to human plasma proteins.
Food Effect
Compared to the fasted state, the systemic exposure (AUC) increased by 10% and peak drug concentration (Cmax) increased by 27% when the dose was given 30 minutes after a high fat meal. After administration with a low fat low calorie meal AUC increased by 6% and Cmax increased by 48%.
Metabolism and Excretion
Ranolazine is metabolized mainly by CYP3A and, to a lesser extent, by CYP2D6. Following a single oral dose of ranolazine solution, approximately 75% of the dose is excreted in urine and 25% in feces. Ranolazine is metabolized rapidly and extensively in the liver and intestine; less than 5% is excreted unchanged in urine and feces. The pharmacologic activity of the metabolites has not been well characterized. The mean elimination half-lives of ranolazine is approximately 5 hours post single dose ranging from 2 to 11 hours. After dosing to steady state with 500 mg to 1500 mg twice daily, the four most abundant metabolites in plasma have AUC values ranging from about 5 to 33% that of ranolazine and display apparent half-lives ranging from 6 to 22 hours.
Drug Interactions
Effect of Other Drugs on Ranolazine
In vitro data indicate that ranolazine is a substrate of CYP3A and, to a lesser degree, of CYP2D6. Ranolazine is also a substrate of P-glycoprotein.
Strong CYP3A Inhibitors
Plasma levels of ranolazine with ranolazine 1000 mg twice daily are increased by 220% when co-administered with ketoconazole 200 mg twice daily [see Contraindications (4)].
Moderate CYP3A Inhibitors
Plasma levels of ranolazine with ranolazine 1000 mg twice daily are increased by 50 to 130% by diltiazem 180 to 360 mg, respectively. Plasma levels of ranolazine with ranolazine 750 mg twice daily are increased by 100% by verapamil 120 mg three times daily [see Drug Interactions (7.1)].
Weak CYP3A Inhibitors
The weak CYP3A inhibitors simvastatin (20 mg once daily) and cimetidine (400 mg three times daily) do not increase the exposure to ranolazine in healthy volunteers.
CYP3A Inducers
Rifampin 600 mg once daily decreases the plasma concentrations of ranolazine (1000 mg twice daily) by approximately 95% [see Contraindications (4)].
CYP2D6 Inhibitors
Paroxetine 20 mg once daily increased ranolazine concentrations by 20% in healthy volunteers receiving ranolazine 1000 mg twice daily. No dose adjustment of ranolazine is required in patients treated with CYP2D6 inhibitors.
Digoxin
Plasma concentrations of ranolazine are not significantly altered by concomitant digoxin at 0.125 mg once daily.
Effect of Ranolazine on Other Drugs
In vitro ranolazine and its O-demethylated metabolite are weak inhibitors of CYP3A and moderate inhibitors of CYP2D6 and P-gp. In vitro ranolazine is an inhibitor of OCT2.
CYP3A Substrates
The plasma levels of simvastatin, a CYP3A substrate, and its active metabolite are increased by 100% in healthy volunteers receiving 80 mg once daily and ranolazine 1000 mg twice daily [see Drug Interactions (7.2)]. Mean exposure to atorvastatin (80 mg daily) is increased by 40% following co-administration with ranolazine (1000 mg twice daily) in healthy volunteers. However, in one subject the exposure to atorvastatin and metabolites was increased by ~400% in the presence of ranolazine.
Diltiazem
The pharmacokinetics of diltiazem is not affected by ranolazine in healthy volunteers receiving diltiazem 60 mg three times daily and ranolazine 1000 mg twice daily.
P-gp Substrates
Ranolazine increases digoxin concentrations by 50% in healthy volunteers receiving ranolazine 1000 mg twice daily and digoxin 0.125 mg once daily [see Drug Interactions (7.2)].
CYP2D6 Substrates
Ranolazine 750 mg twice daily increases the plasma concentrations of a single dose of immediate release metoprolol (100 mg), a CYP2D6 substrate, by 80% in extensive CYP2D6 metabolizers with no need for dose adjustment of metoprolol. In extensive metabolizers of dextromethorphan, a substrate of CYP2D6, ranolazine inhibits partially the formation of the main metabolite dextrorphan.
OCT2 Substrates
In subjects with type 2 diabetes mellitus, the exposure to metformin is increased by 40% and 80% following administration of ranolazine 500 and 1000 mg twice daily, respectively. If co-administered with ranolazine 1000 mg twice daily, do not exceed metformin doses of 1700 mg/day [see Drug Interactions (7.2)].
Alcohol
An in-vitro dissolution study was conducted to evaluate the impact of alcohol on extended-release characteristics of ASPRUZYO Sprinkle. The in-vitro study showed that alcohol causes a rapid release of ranolazine from ASPRUZYO Sprinkle that may increase the risk of adverse events associated with ASPRUZYO Sprinkle. Patients should not consume alcohol when taking ASPRUZYO Sprinkle.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Ranolazine tested negative for genotoxic potential in the following assays: Ames bacterial mutation assay, Saccharomyces assay for mitotic gene conversion, chromosomal aberrations assay in Chinese hamster ovary (CHO) cells, mammalian CHO/HGPRT gene mutation assay, and mouse and rat bone marrow micronucleus assays.
There was no evidence of carcinogenic potential in mice or rats. The highest oral doses used in the carcinogenicity studies were 150 mg/kg/day for 21 months in rats (900 mg/m2/day) and 50 mg/kg/day for 24 months in mice (150 mg/m2/day). These maximally tolerated doses are 0.8 and 0.1 times, respectively, the daily maximum recommended human dose (MRHD) of 2,000 mg on a surface area basis. A published study reported that ranolazine promoted tumor formation and progression to malignancy when given to transgenic APC (min/+) mice at a dose of 30 mg/kg twice daily. The clinical significance of this finding is unclear.
In male and female rats, oral administration of ranolazine that produced exposures (AUC) approximately 3-fold or 5-fold higher, respectively, than the MRHD had no effect on fertility.
14. Clinical Studies
14.1 Chronic Stable Angina
CARISA (Combination Assessment of Ranolazine In Stable Angina) was a study in 823 chronic angina patients randomized to receive 12 weeks of treatment with twice-daily ranolazine 750 mg, 1000 mg, or placebo, who also continued on daily doses of atenolol 50 mg, amlodipine 5 mg, or diltiazem CD 180 mg. Sublingual nitrates were used in this study as needed.
In this trial, statistically significant (p < 0.05) increases in modified Bruce treadmill exercise duration and time to angina were observed for each ranolazine dose versus placebo, at both trough (12 hours after dosing) and peak (4 hours after dosing) plasma levels, with minimal effects on blood pressure and heart rate. The changes versus placebo in exercise parameters are presented in Table 2. Exercise treadmill results showed no increase in effect on exercise at the 1000 mg dose compared to the 750-mg dose.
Table 2 Exercise Treadmill Results (CARISA)
|
Mean Difference from Placebo (sec) |
||
|
CARISA (N = 791) |
|
|
750 mg |
1000 mg |
|
24a 34b |
24 a 26 a |
|
30 a 38 b |
26 a 38 b |
|
20 41 b |
21 35b |
- a p-value ≤ 0.05 b p-value ≤ 0.005
The effects of ranolazine on angina frequency and nitroglycerin use are shown in Table 3.
Table 3 Angina Frequency and Nitroglycerin Use (CARISA)
|
Placebo |
Ranolazine 750 mga |
Ranolazine 1000 mga |
||
|
|
258 |
272 |
261 |
|
3.3 |
2.5 |
2.1 |
|
|
- |
0.006 |
<0.001 |
|
|
|
252 |
262 |
244 |
|
3.1 |
2.1 |
1.8 |
|
|
- |
0.016 |
<0.001 |
|
- a Twice daily
Tolerance to ranolazine did not develop after 12 weeks of therapy. Rebound increases in angina, as measured by exercise duration, have not been observed following abrupt discontinuation of ranolazine.
Ranolazine has been evaluated in patients with chronic angina who remained symptomatic despite treatment with the maximum dose of an antianginal agent. In the ERICA (Efficacy of Ranolazine In Chronic Angina) trial, 565 patients were randomized to receive an initial dose of ranolazine 500 mg twice daily or placebo for 1 week, followed by 6 weeks of treatment with ranolazine 1000 mg twice daily or placebo, in addition to concomitant treatment with amlodipine 10 mg once daily. In addition, 45% of the study population also received long-acting nitrates. Sublingual nitrates were used as needed to treat angina episodes. Results are shown in Table 4. Statistically significant decreases in angina attack frequency (p = 0.028) and nitroglycerin use (p = 0.014) were observed with ranolazine compared to placebo. These treatment effects appeared consistent across age and use of long-acting nitrates.
Table 4 Angina Frequency and Nitroglycerin Use (ERICA)
|
Placebo |
Ranolazinea |
||
|
Angina Frequency (attacks/week) |
|
281 |
277 |
|
4.3 |
3.3 |
|
|
2.4 |
2.2 |
|
|
Nitroglycerin Use (doses/week) |
|
281 |
277 |
|
3.6 |
2.7 |
|
|
1.7 |
1.3 |
|
- a 1000 mg twice daily
Gender
Effects on angina frequency and exercise tolerance were considerably smaller in women than in men. In CARISA, the improvement in Exercise Tolerance Test (ETT) in females was about 33% of that in males at the 1000 mg twice-daily dose level. In ERICA, where the primary endpoint was angina attack frequency, the mean reduction in weekly angina attacks was 0.3 for females and 1.3 for males.
Race
There were insufficient numbers of non-Caucasian patients to allow for analyses of efficacy or safety by racial subgroup.
14.2 Lack of Benefit in Acute Coronary Syndrome
In a large (n = 6560) placebo-controlled trial (MERLIN-TIMI 36) in patients with acute coronary syndrome, there was no benefit shown on outcome measures. However, the study is somewhat reassuring regarding proarrhythmic risks, as ventricular arrhythmias were less common on ranolazine [see Clinical Pharmacology (12.2)], and there was no difference between ranolazine and placebo in the risk of all-cause mortality (relative risk ranolazine: placebo 0.99 with an upper 95% confidence limit of 1.22).
16. How is Aspruzyo Sprinkle supplied
ASPRUZYO Sprinkle is supplied as white to off-white coated, extended-release granules in sachets of 500 or 1000 mg. Packages are
|
Strength |
NDC |
|
|
Unit-dose Sachet (Child-resistant) |
500 mg |
NDC 47335-624-11 |
|
Unit-dose Sachet (Child-resistant) |
1000 mg |
NDC 47335-625-11 |
|
30 Unit-dose Sachets (Child-resistant) |
500 mg |
NDC 47335-624-30 |
|
30 Unit-dose Sachets (Child-resistant) |
1000 mg |
NDC 47335-625-30 |
|
60 Unit-dose Sachets (Child-resistant) |
500 mg |
NDC 47335-624-60 |
|
60 Unit-dose Sachets (Child-resistant) |
1000 mg |
NDC 47335-625-60 |
Store ASPRUZYO Sprinkle at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C to 30°C (59°F to 86°F). [See USP Controlled Room Temperature].
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Inform patients that ASPRUZYO Sprinkle will not abate an acute angina episode.
Drug Interactions
-
-
- •
- Advise patients to discuss with their healthcare provider any prescription or over-the-counter medications and supplements prior to concomitant use [see Drug Interactions (7)].
- •
- Advise patients to limit grapefruit juice or grapefruit products when taking ASPRUZYO Sprinkle [see Drug Interactions (7)].
QT Interval Prolongation
-
-
- •
- Advise patients to inform their physician of any personal or family history of QTc prolongation, congenital long QT syndrome, or if they are receiving drugs that prolong the QTc interval such as [see Warnings and Precautions (5.1)].
Dizziness, Fainting
-
-
- •
- Inform patients that ASPRUZYO Sprinkle may cause dizziness and lightheadedness. Patients should know how they react to ASPRUZYO Sprinkle before they operate an automobile or machinery, or engage in activities requiring mental alertness or coordination [see Adverse Reactions (6.1)].
- •
- Advise patients to contact their physician if they experience fainting spells while taking ASPRUZYO Sprinkle.
Administration
-
-
- •
- Instruct patients to take ASPRUZYO Sprinkle as directed.
- •
- Advise patients not to crush or chew the granules.
All trademarks are the property of their respective owners.
Manufactured by:
Sun Pharmaceutical Industries Ltd.
Mohali, INDIA
Distributed by:
Sun Pharmaceutical Industries, Inc.
Cranbury, NJ 08512
FDA-04
Patient Medication Information
Patient Information
ASPRUZYO Sprinkle (as-PROO-zee-oh spring-KUHL)
(ranolazine) extended-release granules
What is ASPRUZYO Sprinkle?
ASPRUZYO Sprinkle is a prescription medicine used to treat angina that keeps coming back (chronic angina).
ASPRUZYO Sprinkle may be used with other medicines that are used for heart problems and blood pressure control.
It is not known if ASPRUZYO Sprinkle is safe and effective in children.
Do not take ASPRUZYO Sprinkle if:
- •
- you take any of the following medicines:
- •
- for fungus infection: ketoconazole, itraconazole
- •
- for infection: clarithromycin
- •
- for depression: nefazodone
- •
- for HIV: nelfinavir, ritonavir, indinavir saquinavir
- •
- for tuberculosis (TB): rifampin, rifabutin, rifapentine
- •
- for seizures: phenobarbital, phenytoin, and carbamazepine
- •
- St. John's wort
- •
- you have scarring of your liver (liver cirrhosis)
Before taking ASPRUZYO Sprinkle, tell your healthcare provider about all of your medical conditions, including if you:
- •
- have or have a family history of a heart problem, called 'QT prolongation' or 'long QT syndrome'
- •
- have liver problems
- •
- have kidney problems
- •
- are pregnant or plan to become pregnant. It is not known if ASPRUZYO Sprinkle will harm your unborn baby.
- •
- are breastfeeding or plan to breastfeed. It is not known if ranolazine passes into your breast milk. Talk to your healthcare provider about the best way to feed your baby.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. ASPRUZYO Sprinkle may affect the way other medicines work and other medicines may affect how ASPRUZYO Sprinkle works.
Know the medicines you take. Keep a list of them to show your healthcare provider or pharmacist when you get a new medicine.
How should I take ASPRUZYO Sprinkle?
- •
- Take ASPRUZYO Sprinkle exactly as your healthcare provider tells you.
- •
- Your healthcare provider will tell you how much ASPRUZYO Sprinkle to take and when to take it. Do not change your dose unless your healthcare provider tells you to.
- •
- Tell your healthcare provider if you still have symptoms of angina after starting ASPRUZYO Sprinkle.
- •
- Take ASPRUZYO Sprinkle 2 times a day.
- •
- ASPRUZYO Sprinkle may be taken or given as follows:
To open the sachet fold back on dotted line and tear at notch or use scissors.
Directions for use with soft food (e.g., applesauce and yogurt):
- •
- Sprinkle granules on one tablespoonful of soft food and consume immediately.
- •
- Do not crush or chew the granules.
Giving ASPRUZYO Sprinkle with water through a 12 French or larger nasogastric (NG) tube:
- •
- Add the granules from the sachet to a plastic catheter tip syringe and add 50 mL of water.
- •
- Gently shake the syringe for about 15 seconds.
- •
- Connect the catheter tip syringe to the NG tube and give the mixture right away.
- •
- Make sure that no granules are left in the syringe. Rinse the syringe with about 15 mL of additional water if needed and give through NG tube.
Giving ASPRUZYO Sprinkle with water through a 12 French or larger gastric (G) tube:
- •
- Add the granules from the sachet to a plastic catheter tip syringe and add 30 mL of water.
- •
- Gently shake the syringe for about 15 seconds.
- •
- Connect the catheter tip syringe to the G-tube and give the mixture right away.
- •
- Rinse the syringe with 20 mL of additional water and give through G-tube.
- •
- Make sure that no granules are left in the syringe. Rinse the syringe with about 15 mL of additional water if needed and give through G-tube.
- •
- If you miss a dose of ASPRUZYO Sprinkle, take the next dose of ASPRUZYO Sprinkle at your regular time. Do not make up for the missed dose. Do not take 2 doses at the same time.
- •
- If you take too much ASPRUZYO Sprinkle, call your healthcare provider, or go to the nearest emergency room right away.
What should I avoid while taking ASPRUZYO Sprinkle?
- •
- You should limit grapefruit, grapefruit juice, and products that contain grapefruit during treatment with ASPRUZYO Sprinkle. Grapefruit products can increase the amount of ASPRUZYO Sprinkle in your body.
- •
- ASPRUZYO Sprinkle can cause dizziness, lightheadedness, and fainting. If you have these symptoms, do not drive a car, use machinery, or do anything that needs you to be alert.
- •
- You should not drink alcohol during treatment with ASPRUZYO Sprinkle.
What are the possible side effects of ASPRUZYO Sprinkle?
ASPRUZYO Sprinkle may cause serious side effects, including:
- •
- Changes in the electrical activity of your heart called QT prolongation. Your healthcare provider may check the electrical activity of your heart with an electrocardiogram (ECG). Tell your healthcare provider right away if you feel faint, lightheaded, or feel your heart beating irregularly or fast during treatment with ASPRUZYO Sprinkle. These may be symptoms related to QT prolongation.
- •
- Kidney failure in people who already have severe kidney problems. Your healthcare provider may do blood tests to check your kidneys during treatment with ASPRUZYO Sprinkle.
The most common side effects of ASPRUZYO Sprinkle include:
- •
- dizziness
- •
- headache
- •
- constipation
- •
- nausea
These are not all of the possible side effects of ASPRUZYO Sprinkle.
Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store ASPRUZYO Sprinkle?
- •
- Store ASPRUZYO Sprinkle at room temperature between 68°F to 77°F (20°C to 25°C).
- •
- Keep ASPRUZYO Sprinkle and all medicines out of the reach of children.
General information about the safe and effective use of ASPRUZYO Sprinkle.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use ASPRUZYO Sprinkle for a condition for which it was not prescribed. Do not give ASPRUZYO Sprinkle to other people, even if they have the same condition you have. It may harm them. You can ask your pharmacist or healthcare provider for information about ASPRUZYO Sprinkle that is written for health professionals.
What are the ingredients in ASPRUZYO Sprinkle?
Active ingredient: ranolazine
Inactive ingredients: amino methacrylate copolymer, dibutyl sebacate, ethyl cellulose, hypromellose, magnesium stearate, methacrylic acid and ethyl acrylate copolymer, microcrystalline cellulose, and talc.
Manufactured by: Sun Pharmaceutical Industries Ltd., Mohali, INDIA
Distributed by: Sun Pharmaceutical Industries, Inc., Cranbury, NJ 08512
For more information, call 1-800-818-4555.
- This Patient Information has been approved by the U.S. Food and Drug Administration. Issued: February/2022
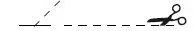
Package/Label Display Panel
NDC 47335-624-30
ASPRUZYO Sprinkle™ (ranolazine) extended-release granules
500 mg per sachet
- Rx only SUN PHARMA
Contains 30 sachets
| ASPRUZYO SPRINKLE
ranolazine granule |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| ASPRUZYO SPRINKLE
ranolazine granule |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| Labeler - SUN PHARMACEUTICAL INDUSTRIES, INC. (146974886) |
| Registrant - SUN PHARMACEUTICAL INDUSTRIES, INC. (146974886) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Sun Pharmaceutical Industries Limited | 650456002 | MANUFACTURE(47335-624, 47335-625) | |