Drug Class: Selective immunosuppressants
Highlights of Prescribing Information
ATGAM® (lymphocyte immune globulin, anti-thymocyte globulin [equine]), sterile solution, for intravenous use only
Initial U.S. Approval: 1981
WARNING: ANAPHYLAXIS
See full prescribing information for complete boxed warning.
Anaphylaxis has been reported with the use of ATGAM. ATGAM can cause potentially life‑threatening anaphylaxis when injected intravenously. Monitor patients for signs and symptoms of anaphylaxis during infusion and for at least 24 hours after infusion [see Warnings and Precautions (5.1) and Adverse Reactions (6.1)].
Recent Major Changes
|
Boxed Warning |
5/2023 |
|
Dosage and Administration (2) |
5/2023 |
|
Contraindications (4) |
5/2023 |
|
Warnings and Precautions (5) |
5/2023 |
Indications and Usage for Atgam
ATGAM is an immunoglobulin G indicated for:
- •
- Renal allograft rejection. (1.1)
- •
- Aplastic anemia (moderate to severe) in patients unsuitable for bone marrow transplantation. (1.2)
- •
-
Limitations of Use:
The usefulness of ATGAM has not been demonstrated in patients with aplastic anemia who are suitable candidates for bone marrow transplantation or in patients with aplastic anemia secondary to neoplastic disease, storage disease, myelofibrosis, Fanconi's syndrome, or in patients known to have been exposed to myelotoxic agents or radiation. (1.2)
Atgam Dosage and Administration
Intravenous use only.
|
Indication |
Dosage |
|
Renal allograft rejection |
10 to 15 mg/kg daily intravenously for 14 days; additional alternate-day therapy up to a total of 21 doses may be given. (2.1) |
|
Aplastic anemia |
10 to 20 mg/kg daily intravenously for 8 to 14 days; additional alternate-day therapy up to a total of 21 doses may be given. (2.1) |
Dosage Forms and Strengths
ATGAM 50 mg/mL concentrate for solution for infusion. (3)
Contraindications
Anaphylactic reaction during prior administration of ATGAM or any other equine gamma globulin preparation. (4)
Warnings and Precautions
- •
- Anaphylaxis, which can be life-threatening, has been reported. To identify those at greatest risk, skin testing before treatment is strongly recommended. Discontinue ATGAM if anaphylaxis occurs. (5.1)
- •
- Monitor patients for signs and symptoms of cytokine release syndrome. (5.2)
- •
- Monitor patients for signs and symptoms of infusion-associated reactions. (5.3)
- •
- Monitor patients for signs and symptoms of serum sickness. (5.4)
- •
- Monitor and report any infection suspected to have been transmitted. (5.5)
- •
- Monitor patients for concurrent infection, including cytomegalovirus, Epstein-Barr virus, and herpes simplex virus infection. (5.6)
- •
- Do not administer live vaccines to patients about to receive, receiving, or after treatment with ATGAM due to a potential of uncontrolled viral replication in the immunosuppressed patient. (5.7)
- •
- Consider discontinuing therapy if severe and unremitting thrombocytopenia or neutropenia occurs. (5.8)
- •
- Monitor liver and renal function as clinically indicated and manage according to relevant clinical guidelines. (5.9)
Adverse Reactions/Side Effects
The most common (incidence >10%) adverse reactions are pyrexia, chills, rash, thrombocytopenia, leukopenia, and arthralgia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Pfizer Inc. at 1-800-438-1985 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
Previously masked reactions to ATGAM may appear following reduced doses of immunosuppressants. (7)
Use In Specific Populations
- •
- Pregnancy: Use only if the potential benefit justifies the risk. (8.1)
- •
- Lactation: Discontinue breast-feeding during treatment with ATGAM or discontinue ATGAM treatment. (8.2)
- •
- Contraception: Advise females of reproductive potential to use effective contraception during treatment with ATGAM and for up to 10 weeks after cessation of therapy. Advise males with a female partner of reproductive potential to use effective contraception during treatment with ATGAM and for at least 10 weeks after cessation of therapy. (8.3)
- •
- Geriatric: Start dosing at the low end of the dosage range. (8.5)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 5/2023
Related/similar drugs
furosemide, Lasix, azathioprine, Imuran, Promacta, eltrombopag, ThymoglobulinFull Prescribing Information
WARNING: ANAPHYLAXIS
Anaphylaxis has been reported with the use of ATGAM. ATGAM can cause potentially life‑threatening anaphylaxis when injected intravenously. Monitor patients for signs and symptoms of anaphylaxis during infusion and for at least 24 hours after infusion [see Warnings and Precautions (5.1) and Adverse Reactions (6.1)].
1. Indications and Usage for Atgam
1.2 Aplastic Anemia
ATGAM is indicated for the treatment of moderate to severe aplastic anemia in patients unsuitable for bone marrow transplantation [see Clinical Studies (14.2)].
The usefulness of ATGAM has not been demonstrated in patients with aplastic anemia who are suitable candidates for bone marrow transplantation or in patients with aplastic anemia secondary to neoplastic disease, storage disease, myelofibrosis, Fanconi's syndrome, or in patients known to have been exposed to myelotoxic agents or radiation.
2. Atgam Dosage and Administration
Administer ATGAM intravenously and use with concomitant immunosuppressants.
2.1 Dosing Information
2.2 Preparation and Administration Instructions
Preparation of Solution
- •
- Visually inspect parenteral drug products for particulate matter and discoloration prior to administration, whenever solution and container permit. However, because ATGAM is a gamma globulin product, it can be transparent to slightly opalescent, colorless to faintly pink or faintly brown, and may develop a slight granular or flaky deposit. Do not shake ATGAM (diluted or undiluted) because excessive foaming and/or denaturation of the protein may occur.
- •
- Dilute ATGAM for intravenous infusion in an inverted bottle/bag of sterile vehicle so the undiluted ATGAM does not contact the air inside. Add the total daily dose of ATGAM to the sterile vehicle (see Compatibility and Stability). Do not exceed a concentration of 4 mg of ATGAM per mL. Gently rotate or swirl the diluted solution to effect thorough mixing.
Administration
Diluted ATGAM should be at room temperature before infusion. ATGAM is appropriately administered into a vascular shunt, arterial venous fistula, or a high-flow central vein using an in-line filter (not supplied) with a pore size of 0.2 to 1.0 micron. Use the in-line filter (not supplied) with all infusions of ATGAM to prevent the administration of any insoluble material that may develop in the product. Use high-flow veins to minimize the occurrence of phlebitis and thrombosis. Infuse ATGAM over a period of at least 4 hours. Monitor patients for signs and symptoms of anaphylaxis during infusion and for at least 24 hours after infusion [see Warnings and Precautions (5.1) and Adverse Reactions (6)].
- •
- Once diluted, ATGAM has been shown to be physically and chemically stable for up to 24 hours at concentrations of up to 4 mg per mL in the following diluents: 0.9% Sodium Chloride Injection, 5% Dextrose and 0.225% Sodium Chloride Injection, and 5% Dextrose and 0.45% Sodium Chloride Injection.
- •
- Do not dilute ATGAM in Dextrose Injection, USP, as low salt concentrations may cause precipitation. Do not use highly acidic infusion solutions since these solutions may contribute to physical instability over time.
- •
- Store diluted ATGAM at room temperature. The diluted solution must be infused within 24 hours (including infusion time).
4. Contraindications
Do not administer ATGAM to a patient who has had an anaphylactic reaction during prior administration of ATGAM or any other equine gamma globulin preparation [see Warnings and Precautions (5.1)].
5. Warnings and Precautions
5.1 Anaphylaxis
Anaphylaxis has been reported with the use of ATGAM. Anaphylaxis is potentially life-threatening. Discontinue ATGAM if anaphylaxis occurs. Generalized rash, tachycardia, dyspnea, and hypotension can be signs of an anaphylactic reaction.
Skin Testing
To identify those at greatest risk of systemic anaphylaxis, skin testing potential recipients is strongly recommended before commencing treatment. Consult an allergist for epicutaneous (prick) and intradermal testing and interpretation. Positive skin testing to ATGAM suggests clinical hypersensitivity and increased risk of a systemic allergic reaction (including anaphylaxis) should the drug be dosed intravenously. In the event of a positive skin test, seriously consider alternative forms of therapy. The predictive value of this test has not been proven clinically, and allergic reactions such as anaphylaxis have occurred in patients whose skin tests were negative. It is important to note that skin testing does not inform risk of delayed hypersensitivity reactions such as serum sickness.
Monitoring and Management of Anaphylaxis
Administer ATGAM in a healthcare facility where a physician familiar with the treatment of potentially life-threatening allergic reactions is in attendance. Monitor patients for signs and symptoms of anaphylaxis during infusion and for at least 24 hours after infusion of ATGAM. Have epinephrine and emergency equipment available for treatment of acute allergic symptoms, should they occur.
5.2 Cytokine Release Syndrome
Cytokine release syndrome has been reported with the use of ATGAM. Cytokine release syndrome can be fatal. Clinical signs may include fever, chills, headache, chest pain, hypotension, dyspnea, tachypnea, and edema. Monitor patients for signs and symptoms of cytokine release syndrome and manage according to relevant clinical guidelines.
5.3 Infusion-Associated Reactions
Serious infusion-associated reactions have been reported with the use of ATGAM. Clinical signs associated with infusion-associated reactions include generalized rash, tachycardia, dyspnea, and hypotension. Monitor patients for signs and symptoms of infusion-associated reactions and manage according to relevant clinical guidelines.
5.4 Serum Sickness
Serum sickness is a delayed hypersensitivity/immune reaction. Symptoms of serum sickness including rash, arthralgia, pyrexia, chills, and pain have been reported. Monitor patients for signs and symptoms of serum sickness and manage according to relevant clinical guidelines.
5.5 Transmissible Infectious Agents
Because ATGAM is made from equine and human blood components, it may carry a risk of transmitting infectious agents, e.g., viruses and the Creutzfeldt-Jakob disease (CJD) agent. This also applies to unknown or emerging viruses and other pathogens.
Report any infection suspected to have been transmitted by this product to Pfizer Inc. at 1-800-438-1985.
5.6 Infections
Due to the immunosuppressive effects of ATGAM, opportunistic infections (viral, bacterial and fungal) have been reported. Sepsis has also been reported. There is an increased risk of viral reactivation (e.g., cytomegalovirus [CMV], Epstein–Barr virus [EBV] infection, herpes simplex virus [HSV]). Monitor patients carefully for concurrent infection.
5.7 Immunizations
Do not administer live vaccines to patients about to receive, receiving, or after treatment with ATGAM. Concomitant administration of ATGAM with live virus vaccines carries a potential of uncontrolled viral replication in the immunosuppressed patient. There is insufficient information to fully define the extent of the risk, or the period of time during which the risk exists. If administered, live viruses may interfere with ATGAM treatment.
5.8 Thrombocytopenia and Neutropenia
Thrombocytopenia and neutropenia have been reported with the use of ATGAM. If thrombocytopenia occurs, consider platelet transfusions to maintain platelets at clinically acceptable levels. Consider discontinuing ATGAM if severe and unremitting thrombocytopenia or neutropenia occurs.
5.9 Hepatic and Renal Function Tests
In patients with aplastic anemia and other hematologic abnormalities who have received ATGAM, abnormal test results of liver function (SGOT, SGPT, alkaline phosphatase) and renal function (serum creatinine) have been observed. Monitor liver and renal functions as clinically indicated and manage according to relevant clinical guidelines.
6. Adverse Reactions/Side Effects
The most clinically significant adverse reactions are anaphylaxis, infection, thrombocytopenia, leukopenia, arthralgia, edema, bradycardia, and abnormal renal and liver function tests.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The safety of ATGAM has been evaluated in 367 patients with renal allograft rejection and 109 patients with aplastic anemia.
The renal allograft rejection and aplastic anemia patients received a similar dosing regimen, and these data were pooled to obtain the frequencies listed in Tables 1 and 2 below.
The most commonly reported adverse reactions (occurring in greater than 10% of patients) are pyrexia, chills, rash, thrombocytopenia, leukopenia, and arthralgia.
|
|
|
Adverse Reaction*,† |
ATGAM |
|
Frequency (%) |
|
|
(N = 476) |
|
|
Pyrexia |
39.5 |
|
Chills |
26.5 |
|
Rash |
25.6 |
|
Thrombocytopenia |
21.6 |
|
Leukopenia |
17.9 |
|
Arthralgia |
17.2 |
|
Urticaria |
9.2 |
|
Headache |
5.3 |
|
Pruritus |
4.6 |
|
Nausea |
4.2 |
|
Infection |
3.4 |
|
Vomiting |
3.4 |
|
Thrombophlebitis |
3.2 |
|
Hypertension |
2.9 |
|
Hypotension |
2.9 |
|
Diarrhea |
2.9 |
|
Abdominal pain upper |
2.7 |
|
Chest pain |
2.7 |
|
Infusion site pain |
2.1 |
|
Edema |
2.1 |
|
Bradycardia |
1.5 |
|
Back pain |
1.5 |
|
Lymphadenopathy |
1.3 |
|
Arteriovenous fistula thrombosis |
1.3 |
|
Dizziness |
1.1 |
|
Dyspnea |
1.1 |
|
Tachycardia |
1.1 |
|
Liver function test abnormal |
1.0 |
|
|
|
Adverse Reaction*,† |
ATGAM |
|
Frequency (%) |
|
|
(N = 476) |
|
|
Convulsion |
0.8 |
|
Pleural effusion |
0.8 |
|
Night sweats |
0.8 |
|
Serum sickness |
0.6 |
|
Hyperglycemia |
0.6 |
|
Stomatitis |
0.6 |
|
Renal function test abnormal |
0.6 |
|
Herpes simplex |
0.4 |
|
Agitation |
0.4 |
|
Hiccups |
0.4 |
|
Proteinuria |
0.4 |
|
Asthenia |
0.4 |
|
Malaise |
0.4 |
|
Wound dehiscence |
0.4 |
|
Anaphylactic reaction |
0.2 |
|
Encephalitis |
0.2 |
|
Paresthesia |
0.2 |
|
Renal artery thrombosis |
0.2 |
|
Iliac vein occlusion |
0.2 |
|
Laryngospasm |
0.2 |
|
Pulmonary edema |
0.2 |
|
Dermatitis allergic |
0.2 |
|
Periorbital edema |
0.2 |
|
Toxic epidermal necrolysis |
0.2 |
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of ATGAM. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Infections and infestations: Sepsis, Hepatitis viral, Localized infection, Systemic infection (bacterial, viral, fungal).
Blood and lymphatic system disorders: Anemia, Eosinophilia, Granulocytopenia, Hemolysis, Hemolytic anemia, Neutropenia, Pancytopenia
Psychiatric disorders: Confusional state, Disorientation
Nervous system disorders: Dyskinesia, Syncope, Tremor
Cardiac disorders: Cardiac failure congestive
Vascular disorders: Deep vein thrombosis, Vasculitis
Respiratory, thoracic and mediastinal disorders: Apnea, Cough, Epistaxis, Oropharyngeal pain
Gastrointestinal disorders: Abdominal pain, Gastrointestinal hemorrhage, Gastrointestinal perforation, Oral pain
Skin and subcutaneous tissue disorders: Hyperhidrosis
Musculoskeletal and connective tissue disorders: Flank pain, Muscle rigidity, Myalgia, Pain in extremity
Renal and urinary disorders: Kidney enlargement, Kidney rupture, Renal failure acute
Congenital, familial and genetic disorders: Aplasia
General disorders and administration site conditions: Infusion site erythema, Infusion site swelling, Pain
7. Drug Interactions
A potential pharmacodynamic interaction concerns the concomitant administration of ATGAM with corticosteroids and other immunosuppressants, which are associated with an increased susceptibility to bacterial, viral and fungal infections, as they inhibit the immune system. The severity of the infections such as septicemia may be masked and their clinical presentations may be atypical.
Monitor patients receiving ATGAM and immunosuppressive agents such as corticosteroids when the dose of corticosteroids and other immunosuppressants is being reduced, since this adjustment of dose may result in reduced immunosuppression and lead to development of previously masked reactions to ATGAM.
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
There are no adequate and well-controlled studies in pregnant women. There is a limited amount of data from the use of ATGAM in pregnant women. It is also not known whether ATGAM can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. The outcome of pregnancies cannot be determined. Use ATGAM during pregnancy only if the potential benefit to the mother justifies the potential risk to the fetus.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcome. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
In embryo-fetal toxicity studies, ATGAM was administered to rats and cynomolgus monkeys for 11 and 16 days, respectively during organogenesis. In rats, hypoplastic cervical vertebrae, a finding consistent with delayed skeletal development, were observed in fetuses whose dams received ATGAM at doses of 100 mg/kg/day during organogenesis. In monkey reproduction studies, maternal toxicity (vaginal bleeding, decreased body weight and loss of appetite) was observed with ATGAM doses ≥20 mg/kg/day after 16 days of dosing. Fetal deaths occurred in dams treated with 20 mg/kg/day ATGAM earlier in organogenesis (days 20‑35), but not when treatment was given at a later part of organogenesis (days 35-50). The maternal and fetal deaths were attributed to maternal anemia due to red blood cell antigen that humans do not share. Therefore, this toxicity is not considered relevant to human fetal development.
8.2 Lactation
Risk Summary
It is not known if ATGAM is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in breast-feeding neonates and infants from ATGAM, a decision should be made whether to discontinue breast-feeding or to discontinue the drug taking into account the importance of the drug to the mother.
Data
In animal studies, a single dose of ATGAM up to 40 mg/kg was not detected at the limit of quantification in the milk of lactating cynomolgus monkeys.
8.3 Females and Males of Reproductive Potential
Contraception
Females
It is not known if ATGAM can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)]. Advise females of reproductive potential to use effective contraception during treatment with ATGAM and for at least 10 weeks after cessation of therapy.
Males
Advise males with a female partner of reproductive potential to use effective contraception during treatment with ATGAM and for at least 10 weeks after cessation of therapy.
Infertility
In fertility studies, ATGAM at doses 10, 20 and 40 mg/kg/day was administered to cynomolgus monkeys (Macaca fascicularis) for 14 days either before (male monkeys) or before and after (female monkeys) cohabitation with untreated mates. ATGAM treatment was not associated with male or female hormonal or copulation behavior changes. A decrease in fertility index in female monkeys receiving ATGAM was seen. Female toxicity, including death, was observed with ATGAM doses of ≥20 mg/kg/day. While the etiology of this toxicity is uncertain, it may be attributed to hemolytic anemia due to cross-reactivity of ATGAM to a monkey red blood antigen.
8.4 Pediatric Use
Experience with children has been limited. ATGAM has been administered safely to a small number of pediatric renal allograft recipients and pediatric aplastic anemia patients at dosage levels comparable to those in adults.
8.5 Geriatric Use
Clinical experience in a limited number of elderly patients (≥65 years of age) has not identified differences in responses between the elderly and younger patients. Select the dose for an elderly patient with caution, starting at the low end of the dosage range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of comorbidities or other drug therapy in this age group.
10. Overdosage
The maximum tolerated dose of ATGAM Sterile Solution is expected to vary from patient to patient due to the biological nature of the product. The largest single daily dose known to be administered to one patient (renal allograft recipient) was 7,000 mg administered at a concentration of approximately 10 mg/mL Sodium Chloride Injection, USP, seven times the recommended total dose and infusion concentration. In this patient, the administration of ATGAM was not associated with any signs of acute intoxication or late sequelae.
A maximum therapeutic dose has not been established therefore the definition of overdose for ATGAM has not been clearly defined. Some renal allograft patients have received up to 50 doses in 4 months, and others have received 28-day courses of 21 doses followed by as many as 3 more courses for the treatment of acute rejection. The incidence of toxicologic manifestations did not increase with any of these regimens; however, close monitoring of the patient is recommended.
11. Atgam Description
ATGAM Sterile Solution contains lymphocyte immune globulin, anti-thymocyte globulin [equine]. It is the purified, concentrated, and sterile gamma globulin, primarily monomeric IgG, from hyperimmune serum of horses immunized with human thymus lymphocytes. ATGAM is a transparent to slightly opalescent aqueous protein solution. It may appear colorless to faintly pink or faintly brown and is nearly odorless. It may develop a slight granular or flaky deposit [see Dosage and Administration (2.2)].
Precise methods of determining the potency of ATGAM have not been established, thus activity may potentially vary from lot to lot. Before release for clinical use, each lot of ATGAM is tested to assure its ability to inhibit rosette formation between human peripheral lymphocytes and sheep red blood cells in vitro. In each lot, antibody activity against human red blood cells and platelets is also measured and determined to be within acceptable limits. Only lots that meet the acceptance criteria for pyrogens and test negative for antihuman serum protein antibody and antiglomerular basement membrane antibody are released.
Each milliliter of ATGAM contains 50 mg of horse gamma globulin stabilized in 0.3 molar glycine to a pH of approximately 6.8.
12. Atgam - Clinical Pharmacology
12.1 Mechanism of Action
ATGAM is composed of antibodies that bind a wide variety of proteins on the surface of lymphocytes. In addition, ATGAM binds to granulocytes, platelets, bone marrow cells, and other cell types. The mechanism of ATGAM-induced immunosuppression has not been determined. Published data indicate that the primary mechanism is the depletion of circulating lymphocytes, with greatest effect on T lymphocytes. Lymphocyte depletion may be caused by complement dependent lysis and/or activation-induced apoptosis. In addition, immunosuppression may be mediated by the binding of antibodies to lymphocytes which results in partial activation and induction of T lymphocyte anergy.
The mechanism of ATGAM therapy for aplastic anemia is attributed to its immunosuppressive actions. In addition, ATGAM directly stimulates the growth of hematopoietic stem cells and release of hematopoietic growth factors such as interleukin-3 and granulocyte/macrophage colony stimulating factor.
14. Clinical Studies
14.1 Renal Allograft Rejection
US Studies
The effectiveness of ATGAM for treatment of acute allograft rejection was evaluated in three different treatment applications: as a substitute for standard therapy, in conjunction with standard therapy at the time of diagnosis of the first rejection episode, and in conjunction with standard therapy in steroid resistant rejection episodes.
A randomized controlled trial of the use of ATGAM as a substitute for standard therapy for treatment of the first acute rejection episode was conducted at one transplant center in recipients of living related renal allografts. A total of 22 patients were studied; 11 in each of the two treatment groups [ATGAM versus standard therapy (bolus doses of Solu-Medrol®)]. Patients randomized to the ATGAM group received 14–21 doses of ATGAM therapy, starting on the day the rejection was diagnosed. ATGAM was administered daily according to a dose-by-rosette regimen which resulted in a mean daily dose of approximately 15 mg/kg. Patients randomized to the control group received Solu-Medrol® at a dosage of 15 mg/kg starting on the day the rejection was diagnosed, administered either daily or on alternate days for 3 to 7 doses to complete a maximum total dose of 5,000 mg for the course of the rejection episode. In this study, ATGAM was at least effective as standard therapy for treatment of acute allograft rejection. All 11 ATGAM‑treated patients achieved resolution of first rejection compared with 10/11 control patients. At one year, the functional graft survival rate was 91% in the ATGAM group (10/11) and 64% in the control group (7/11). Patient survival was similar in the two treatment groups (11/11 ATGAM patients versus 10/11 control patients).
The effect of ATGAM when administered in conjunction with standard therapy at the time of diagnosis of the first rejection episode was studied under two different protocols with cadaveric and living related renal allograft rejection patients. The results from these studies demonstrate the efficacy associated with the addition of ATGAM to standard therapy for treatment of the first rejection episode in renal allograft recipients. In Study 1, a randomized controlled, two center trial of ATGAM use for treatment of acute rejection in cadaveric renal allograft rejection patients, the addition of ATGAM to standard rejection therapy (methylprednisolone sodium succinate) resulted in an increased frequency of resolution of the first acute rejection episode which was statistically significant (p <0.01). ATGAM-treated patients achieved a rejection resolution rate of 80% (36/45) compared with 54% (25/46) in the control group. There was a statistically significant improvement in functional graft survival favoring the ATGAM group (p <0.01), and a statistically significant steroid sparing effect during the first rejection episode among patients in the ATGAM group. There was no difference in the patient survival rate between the two treatment groups. Study 2 was a randomized controlled trial conducted at five different transplant centers. In this study, the addition of ATGAM to standard rejection therapy (bolus doses of Solu-Medrol®) for treatment of acute rejection in recipients of living related renal transplants resulted in an increased frequency of rejection resolution and improvement in functional graft survival. Due to the small sample size, the difference between the ATGAM group and the control group in functional graft survival rate did not achieve statistical significance. Marginal statistical significance was demonstrated in rejection reversal rate and intravenous steroid sparing among ATGAM patients (p=0.10 and p=0.07). Patient survival rates were similar in the two treatment groups.
Results from randomized controlled trials in patients with first acute renal allograft rejection episodes refractory to conventional steroid therapy have demonstrated that ATGAM, when administered in conjunction with standard therapy, yields efficacy results superior to those of standard therapy alone. One study investigated two different regimens of ATGAM; immediate and delayed therapy. Patients were enrolled at the time of first rejection episode and randomized among three treatment groups: control (no ATGAM), immediate ATGAM, and delayed ATGAM. Patients in all three treatment groups received standard rejection therapy in the form of bolus doses of Solu-Medrol® 15 mg/kg/day IV, while patients in the two ATGAM groups received ATGAM therapy in addition to Solu-Medrol®. In the immediate ATGAM group, ATGAM administration started at the time of diagnosis of rejection (concurrent with standard therapy). In the delayed ATGAM group, ATGAM administration started on rejection day 4 (following the first three doses of Solu-Medrol®). Patients in both of the treated groups received from 10 to 21 doses of ATGAM. Results favored the two ATGAM groups (and particularly the immediate ATGAM group) in both outcome of first rejection and functional graft survival. The improvement in functional graft survival was statistically significant (p=0.05). There was also a statistically significant difference in patient survival rate favoring the ATGAM-treated groups (p=0.02).
The effectiveness of ATGAM for reversal of acute renal allograft rejection was also demonstrated in other controlled studies performed in various medical centers. In these studies, ATGAM was administered at time of diagnosis of the first rejection episode at a range of 10 to 15 mg/kg per day for 14 to 15 days, followed by alternate‑day therapy for a total of 21 doses in 28 days.
14.2 Aplastic Anemia
The use of ATGAM for the treatment of moderate to severe aplastic anemia in patients unsuitable for bone marrow transplantation is based on data from three controlled studies.
The effectiveness of the ATGAM therapy in the studies described below was evaluated by the hematological response and survival rates (Table 3).
10 to 20 mg/kg daily for 8 to 14 days
Study 1
A total of 41 patients with moderate or severe aplastic anemia ages 6 to 69 years, who were not candidates for bone marrow transplantation were enrolled in a randomized controlled study. The objective of this study was to determine the efficacy of ATGAM as a single agent, in restoring hematopoiesis in patients with moderate to severe aplastic anemia. Twenty-one (n = 21) patients in the ATGAM treatment group received 20 mg/kg/day for 8 days, while control patients (n = 20) were observed for 3 months. All patients were given oral prednisone (40 mg/m2/day) starting on day 8 then tapered over 1 to 2 weeks.
At 3 months post-study enrollment, 11 patients in the supportive care group who showed no improvement became eligible and were crossed over to receive ATGAM therapy. Efficacy was evaluated as sustained improvement in peripheral blood counts within 3 months of entry into the study. A statistically significant (p<0.01) difference was observed between the two treatment groups in hematological improvement based on the investigator's evaluation; 11 of 21 (52%) patients in the ATGAM group responded, compared with no patients (0 of 20) in the control group. Six of the 11 crossover patients from the control group showed improvement after 3 months of therapy. Overall, of 32 patients in both the ATGAM group and the control group who crossed over to receive ATGAM, 17 patients (53%) had a hematological improvement. Estimated 1-year survival rate was 62% for all 32 patients treated with ATGAM. The 2-year survival rate was 100% among the ATGAM responders [17 of the 32 patients (53%) compared to 14% for the nonresponders].
Fever, chills, and erythematous or urticarial rash were seen in all ATGAM treated patients. Platelet counts decreased during ATGAM infusion and daily platelet transfusions were necessary. Serum sickness occurred in all patients within 6 to 18 days of ATGAM initiation and was well-controlled with standard therapy. Three patients experienced transient hypotension.
Study 2
A randomized double-blind, placebo prospective, controlled study was conducted to compare the safety and efficacy of ATGAM and androgen (oxymetholone; OXY) immunosuppressive therapy with the combination of ATGAM, androgen (OXY) and an infusion of human leukocyte antigen (HLA) mismatched bone marrow in patients with severe aplastic anemia who were not candidates for bone marrow transplantation. Allocation to treatment group was based on the availability of mismatched bone marrow donors. A total of 42 patients, ages 1 to 69 years were treated. Eighteen patients received ATGAM at a dose of 16 mg/kg/day for 10 doses with concomitant androgens (OXY) at a dose of 3 mg/kg/day for a minimum of 3 months, and 24 patients received an infusion of bone marrow from an HLA mismatched donor 48 hours after the completion of ATGAM treatment.
At 3 months after entry into the study, 51% of patients with disease of idiopathic etiology (21 of the 41 evaluable patients from both groups) showed improvement based on investigator's evaluation of transfusion requirements and peripheral blood counts. Hematological response rate (complete/moderate based on sponsor's evaluation) at 3 months for the ATGAM and androgen group was 44% compared with 43% for the group receiving ATGAM, androgen and bone marrow infusion. The group of patients who received mismatched bone marrow infusion had better estimated 1-year survival rate, although the difference between these estimates was not statistically significant (p=0.14); 83% at 12 months for the group receiving bone marrow infusion versus 59% for the ATGAM and androgen alone group. Estimated 1-year survival rate for both groups combined was 73%.
The most commonly reported adverse events were rash, fever, arthralgias, chills, headache, myalgia and pruritus.
A pooled analysis of data from Studies 1 and 2 revealed an overall estimated 1-year survival rate of 69% in ATGAM-treated patients.
Study 3
A total of 53 patients (3 to 76 years of age) participated in this randomized, placebo-controlled, double-blind study to determine if androgens add to the efficacy of ATGAM in providing favorable hematologic response rates in patients with moderate to severe aplastic anemia. All patients were treated with ATGAM 20 mg/kg/day IV for 8 days, and were randomized to receive the oral androgen (oxymetholone 4 mg/kg/day or fluoxymesterone 25 mg/m2/day) (n = 26), or a matched placebo (n = 27). Both groups received oral prednisone (40 mg/m2/day) beginning on day 8 which was tapered and discontinued in 1 to 2 weeks. A group of historical controls from previous studies (n = 68; 1 to 72 years of age) who received ATGAM (20 mg/kg/day IV for 8 days) without androgens were included for treatment results comparison. The proportions of subjects who presented complete or partial response at 6 months were 42% in the ATGAM plus androgen group, 44% in the ATGAM plus placebo group, and 51% in the historical controls. The difference in response rates was not significant (p>0.9). Survival at 2 years was also comparable in the two groups for patients with severe aplastic anemia; 55% in the ATGAM plus androgen group compared with 50% in the ATGAM plus placebo group (p=0.65), and 56% for the historical controls. In patients with moderate aplastic anemia, two-year survival for the ATGAM plus androgen group was 63% compared with 100% in those receiving ATGAM plus placebo and 72% in the historical controls who received ATGAM alone.
Adverse reactions in both groups were comparable and included rash, chills, gastrointestinal disturbances, and joint pain during ATGAM infusion, as well as symptoms of serum sickness in all patients. Five patients had asymptomatic sinus bradycardia; six patients required antihypertensive therapy. Alanine transaminase or alkaline phosphatase levels increased to >2 times the upper limits of normal in 7 patients receiving ATGAM plus androgen, and in nine patients receiving ATGAM plus placebo.
|
||||||
|
Study |
ATGAM + comparator or other therapy |
No. of subjects |
Response rate %
|
P Value |
Survival rate %
|
P Value (or 95% CI) |
|
10 to 20 mg/kg/day for 8 to 14 days |
||||||
|
Study 1 |
ATGAM |
21 |
47†/ 52‡ (3 mo) |
<0.01†/<0.01‡ |
62§ (12 mo) |
NA |
|
Control |
20 |
6†/ 0‡ (3 mo) |
||||
|
Study 2 |
ATGAM + Bone marrow infusion |
24 |
43 (3 mo) |
Not reported |
83 (12 mo) |
=0.14 |
|
ATGAM |
18 |
44 (3 mo) |
59 (12 mo) |
|||
|
Study 3 |
ATGAM + Androgen |
26 |
42 (6 mo) |
>0.9 |
55¶ (24 mo) |
=0.65 |
|
ATGAM + Placebo |
27 |
44 (6 mo) |
50¶ (24 mo) |
|||
|
ATGAM historical controls |
68 |
51 (6 mo) |
NA |
56 (24 mo) | ||
15. References
- 1.
- Hardy MA, Nowygrod R, Elberg A, Appel G. Use of ATG in treatment of steroid-resistant rejection. Transplantation 1980; 29(2):162–4.
- 2.
- Nowygrod R, Appel G, Hardy MA. Use of ATG for reversal of acute allograft rejection. Transplant Proc 1981; 13(1):469–72.
- 3.
- Filo RS, Smith EJ, Leapman SB. Reversal of acute renal allograft rejection with adjunctive ATG therapy. Transplant Proc 1981; 13(1):482–90.
- 4.
- Shield CF III, Cosimi AB, Tolkoff Rubin N, et al. Use of antithymocyte globulin for reversal of acute allograft rejection. Transplantation 1979; 28(6):461–4.
- 5.
- Rubin RH, Cosimi AB, Hirsch MS, Herrin JT. Effects of antithymocyte globulin on cytomegalovirus infection in renal transplant recipients. Transplantation 1981; 31(2):143–5.
- 6.
- Cosimi AB, Wortis HH, Delmonico FL, Russell PS. Randomized clinical trial of antithymocyte globulin in cadaver renal allograft recipients: importance of T cell monitoring. Surgery 1976; 80(2):155–63.
- 7.
- Wechter WJ, Brodie JA, Morrell RM, et al. Antithymocyte globulin (ATGAM) in renal allograft recipients: multicenter trials using a 14-dose regimen. Transplantation 1979; 28(4):294–302.
- 8.
- Butt KMH, Zielinski CM, Parsa I, et al. Trends in immunosuppression for kidney transplantation. Kidney Int 1978; 13(Suppl 8): S95–S8.
- 9.
- Ettenger RB, Rosenthal JT, Marik JL, et al. Improved cadaveric renal transplant outcome in children. Pediatric Nephrol 1991; 5:137–42.
16. How is Atgam supplied
ATGAM Sterile Solution, containing 50 mg/mL lymphocyte immune globulin, anti-thymocyte globulin [equine], is supplied as follows:
5 – 5 mL ampoules: NDC 0009-7224-02
17. Patient Counseling Information
Advise patients receiving ATGAM that they will be monitored in a facility equipped and staffed with adequate laboratory and supportive medical resources.
Anaphylaxis
Advise the patient that ATGAM may be discontinued and immediate medical attention will be provided if any signs/symptoms of anaphylaxis occur [see Warnings and Precautions (5.1)].
Cytokine Release Syndrome
Advise the patient on the risk of cytokine release syndrome [see Warnings and Precautions (5.2)].
Infusion-Associated Reactions
Advise the patient on the clinical signs associated with infusion-associated reactions [see Warnings and Precautions (5.3)].
Serum Sickness
Advise the patient on the clinical signs associated with serum sickness [see Warnings and Precautions (5.4)].
Transmissible Infectious Agents
Despite screening and testing, products manufactured using components of human blood such as ATGAM may carry a risk of transmitting infectious agents (e.g., viruses). Discuss the risks and benefits of therapy with patients before initiating treatment [see Warnings and Precautions (5.5)].
Infections
Advise the patient to report any signs and symptoms of infection (e.g., fever, sweating, chills, muscle aches, cough, shortness of breath, diarrhea, or stomach pain) [see Warnings and Precautions (5.6)].
Thrombocytopenia and Neutropenia
Advise the patient to report any signs and symptoms of thrombocytopenia and/or neutropenia (e.g., unusual bleeding, bruising, rash of dark red spots under the skin, fever, sweating, chills, muscle aches, cough, shortness of breath, diarrhea, or stomach pain) [see Warnings and Precautions (5.8)].
Hepatic and Renal Function Tests
Advise the patient that monitoring of liver and renal function will occur. Advise the patient of abnormal liver and renal function test results [see Warnings and Precautions (5.9)].
Healthcare providers should refer to labels.fda.gov or DailyMed for the most updated version of the labeling.
This product's labeling may have been updated. For the most current prescribing information, please visit www.pfizer.com. For medical information about ATGAM, please visit www.pfizermedinfo.com or call 1-800-438-1985.
U.S. Govt. License No. 1216
LAB-0019-11.0
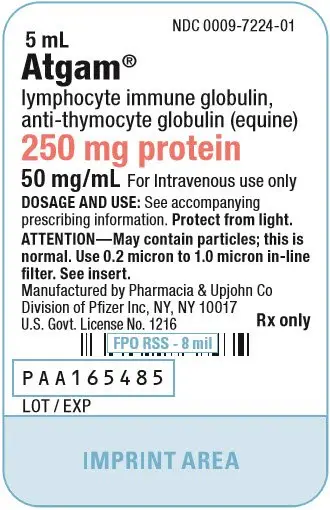
PRINCIPAL DISPLAY PANEL - 5 mL Ampule Label
NDC 0009-7224-01
5 mL
Atgam®
lymphocyte immune globulin,
anti-thymocyte globulin (equine)
250 mg protein
50 mg/mL For Intravenous use only
DOSAGE AND USE: See accompanying
prescribing information. Protect from light.
ATTENTION—May contain particles; this is
normal. Use 0.2 micron to 1.0 micron in-line
filter. See insert.
Manufactured by Pharmacia & Upjohn Co
Division of Pfizer Inc, NY, NY 10017
U.S. Govt. License No. 1216
Rx only
PAA165485
LOT / EXP
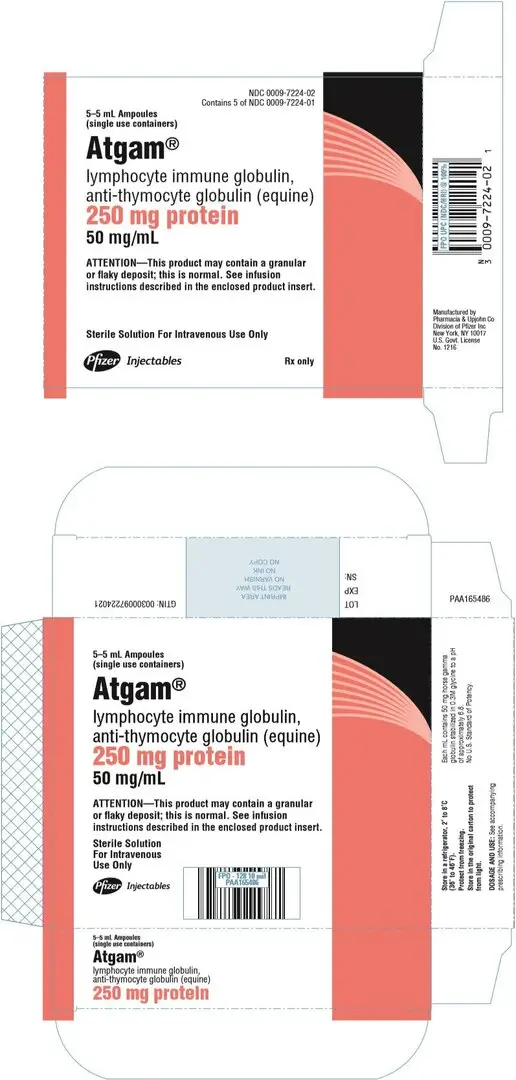
PRINCIPAL DISPLAY PANEL - 5 mL Ampule Carton
NDC 0009-7224-02
Contains 5 of NDC 0009-7224-01
5–5 mL Ampoules
(single use containers)
Atgam®
lymphocyte immune globulin,
anti-thymocyte globulin (equine)
250 mg protein
50 mg/mL
ATTENTION—This product may contain a granular
or flaky deposit; this is normal. See infusion
instructions described in the enclosed product insert.
Sterile Solution For Intravenous Use Only
Pfizer Injectables
Rx only
| ATGAM
equine thymocyte immune globulin injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Pharmacia & Upjohn Company LLC (618054084) |
| Registrant - Pfizer Inc (113480771) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pharmacia & Upjohn Company LLC | 618054084 | ANALYSIS(0009-7224) , MANUFACTURE(0009-7224) , API MANUFACTURE(0009-7224) , PACK(0009-7224) , LABEL(0009-7224) | |