Drug Detail:Azor (Amlodipine and olmesartan [ am-loe-de-peen-ol-me-sar-tan ])
Drug Class: Angiotensin II inhibitors with calcium channel blockers
Highlights of Prescribing Information
AZOR (amlodipine and olmesartan medoxomil) tablets, for oral use
Initial U.S. Approval: 2007
WARNING: FETAL TOXICITY
See full prescribing information for complete boxed warning.
-
When pregnancy is detected, discontinue Azor as soon as possible (5.1, 8.1).
- Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus (5.1, 8.1).
Indications and Usage for Azor
- Azor is a combination of amlodipine besylate, a dihydropyridine calcium channel blocker, and olmesartan medoxomil, an angiotensin II receptor blocker, indicated for the treatment of hypertension, alone or with other antihypertensive agents, to lower blood pressure. Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular events, primarily strokes and myocardial infarctions (1).
- Azor may also be used as initial therapy in patients likely to need multiple antihypertensive agents to achieve their blood pressure goals (1).
Azor Dosage and Administration
- Recommended starting dose: 5/20 mg once daily (2).
- Titrate as needed in two-week intervals up to a maximum of 10/40 mg once daily (2).
Dosage Forms and Strengths
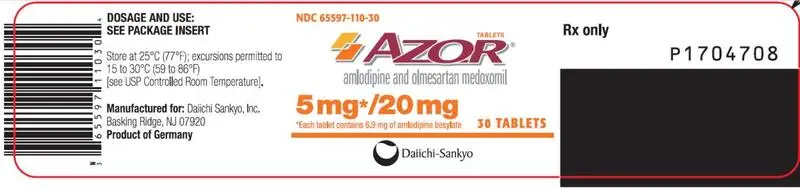
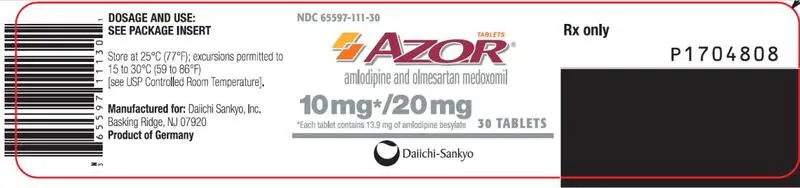
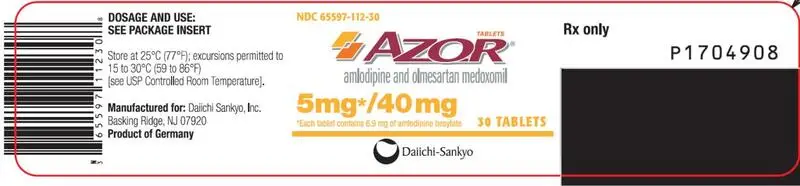
Tablets: (amlodipine/olmesartan medoxomil content) 5/20 mg, 10/20 mg, 5/40 mg, and 10/40 mg (3).
Contraindications
- Do not co-administer aliskiren with Azor in patients with diabetes (4).
Warnings and Precautions
- Anticipate hypotension in volume- or salt-depleted patients with treatment initiation. Start treatment under close supervision (5.2).
- Increased angina or myocardial infarction may occur upon dosage initiation or increase (5.3).
- Impaired renal function: changes in renal function may occur (5.4).
- Sprue-like enteropathy has been reported. Consider discontinuation of Azor in cases where no other etiology is found (5.6).
Adverse Reactions/Side Effects
Most common adverse reaction (incidence ≥3%) is edema (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Daiichi Sankyo, Inc. at 1-877-437-7763 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
Amlodipine (7.1):
- If simvastatin is co-administered with amlodipine, do not exceed 20 mg daily of simvastatin.
- Increased exposure of cyclosporine and tacrolimus.
- Increased exposure of amlodipine when coadministered with CYP3A inhibitors.
Olmesartan medoxomil (7.2):
- Nonsteroidal anti-inflammatory drugs (NSAIDS) may lead to increased risk of renal impairment and loss of antihypertensive effect.
- Dual inhibition of the renin-angiotensin system: Increased risk of renal impairment, hypotension, and hyperkalemia.
- Colesevelam hydrochloride: Consider administering olmesartan at least 4 hours before colesevelam hydrochloride dose.
- Lithium: Increases in serum lithium concentrations and lithium toxicity.
Use In Specific Populations
- Lactation: Breastfeeding is not recommended (8.2).
- Geriatric: Not recommended for initial therapy in patients ≥75 years old (8.5)
- Hepatic Impairment: Not recommended for initial therapy (8.6).
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 10/2020
Related/similar drugs
amlodipine, lisinopril, metoprolol, losartan, furosemide, hydrochlorothiazideFull Prescribing Information
1. Indications and Usage for Azor
Azor is indicated for the treatment of hypertension, alone or with other antihypertensive agents, to lower blood pressure. Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular (CV) events, primarily strokes and myocardial infarctions. These benefits have been seen in controlled trials of antihypertensive drugs from a wide variety of pharmacologic classes including the class to which this drug principally belongs. There are no controlled trials demonstrating risk reduction with Azor.
Control of high blood pressure should be part of comprehensive cardiovascular risk management, including, as appropriate, lipid control, diabetes management, antithrombotic therapy, smoking cessation, exercise, and limited sodium intake. Many patients will require more than one drug to achieve blood pressure goals. For specific advice on goals and management, see published guidelines, such as those of the National High Blood Pressure Education Program’s Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC).
Numerous antihypertensive drugs, from a variety of pharmacologic classes and with different mechanisms of action, have been shown in randomized controlled trials to reduce cardiovascular morbidity and mortality, and it can be concluded that it is blood pressure reduction, and not some other pharmacologic property of the drugs, that is largely responsible for those benefits. The largest and most consistent cardiovascular outcome benefit has been a reduction in the risk of stroke, but reductions in myocardial infarction and cardiovascular mortality also have been seen regularly.
Elevated systolic or diastolic pressure causes increased cardiovascular risk, and the absolute risk increase per mmHg is greater at higher blood pressures, so that even modest reductions of severe hypertension can provide substantial benefit. Relative risk reduction from blood pressure reduction is similar across populations with varying absolute risk, so the absolute benefit is greater in patients who are at higher risk independent of their hypertension (for example, patients with diabetes or hyperlipidemia), and such patients would be expected to benefit from more aggressive treatment to a lower blood pressure goal.
Some antihypertensive drugs have smaller blood pressure effects (as monotherapy) in black patients, and many antihypertensive drugs have additional approved indications and effects (e.g., on angina, heart failure, or diabetic kidney disease). These considerations may guide selection of therapy.
Azor may also be used as initial therapy in patients who are likely to need multiple antihypertensive agents to achieve their blood pressure goals.
Patients with moderate or severe hypertension are at relatively high risk for cardiovascular events (such as strokes, heart attacks, and heart failure), kidney failure, and vision problems, so prompt treatment is clinically relevant. The decision to use a combination as initial therapy should be individualized and should be shaped by considerations such as baseline blood pressure, the target goal, and the incremental likelihood of achieving goal with a combination compared to monotherapy. Individual blood pressure goals may vary based upon the patient’s risk.
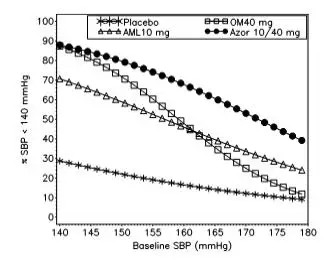
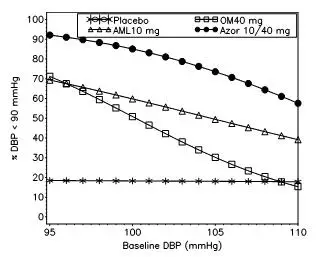
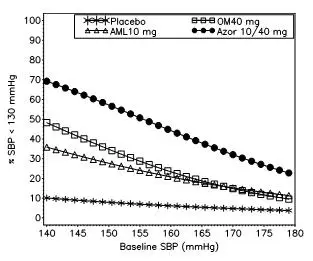
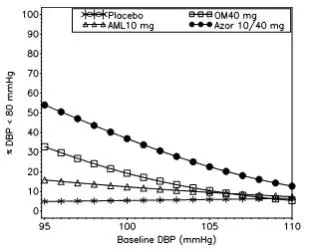
Data from an 8-week, placebo-controlled, parallel-group factorial study [see Clinical Studies (14.1)] provide estimates of the probability of reaching a blood pressure goal with Azor compared to amlodipine or olmesartan medoxomil monotherapy. The figures below provide estimates of the likelihood of achieving the targeted systolic or diastolic blood pressure goals with Azor 10/40 mg compared with amlodipine or olmesartan medoxomil monotherapy, based upon baseline systolic or diastolic blood pressure. The curve of each treatment group was estimated by logistic regression modeling from all available data of that treatment group. The right tail of each curve is less reliable because of small numbers of subjects with high baseline blood pressures.
|
|
|
| Figure 1: Probability of Achieving Systolic Blood Pressure (SBP) < 140 mmHg at Week 8 With LOCF | Figure 2: Probability of Achieving Diastolic Blood Pressure (DBP) < 90 mmHg at Week 8 With LOCF |
|
|
|
| Figure 3: Probability of Achieving Systolic Blood Pressure (SBP) < 130 mmHg at Week 8 With LOCF | Figure 4: Probability of Achieving Diastolic Blood Pressure (DBP) < 80 mmHg at Week 8 With LOCF |
The figures above provide an approximation of the likelihood of reaching a targeted blood pressure goal (e.g., Week 8 SBP <140 mmHg or <130 mmHg or a DBP <90 mmHg or <80 mmHg) for the high-dose treatment groups evaluated in the study. Azor 5/20 mg, the lowest dose combination treatment group, increases the probability of reaching blood pressure goal compared with the highest dose monotherapies, amlodipine 10 mg and olmesartan medoxomil 40 mg.
For example, a patient with a baseline blood pressure of 160/100 mmHg has about a 48% likelihood of achieving a goal of <140 mmHg (systolic) and a 51% likelihood of achieving a goal of <90 mmHg (diastolic) on monotherapy with olmesartan medoxomil 40 mg, and about a 46% likelihood of achieving a goal of <140 mmHg (systolic) and a 60% likelihood of achieving a goal of <90 mmHg (diastolic) on monotherapy with amlodipine 10 mg. The likelihood of achieving these same goals increases to 63% (systolic) and 71% (diastolic) on Azor 5/20 mg, and to 68% (systolic) and 85% (diastolic) on Azor 10/40 mg.
2. Azor Dosage and Administration
The usual starting dose of Azor is 5/20 mg once daily. The dosage can be increased after 1 to 2 weeks of therapy to a maximum dose of one 10/40 mg tablet once daily as needed to control blood pressure [see Clinical Studies (14.1)].
3. Dosage Forms and Strengths
Azor tablets are formulated for oral administration in the following strength combinations:
| 5/20 | 5/40 | 10/20 | 10/40 | |
| Amlodipine equivalent (mg) | 5 | 5 | 10 | 10 |
| Olmesartan medoxomil (mg) | 20 | 40 | 20 | 40 |
4. Contraindications
Do not co-administer aliskiren with Azor in patients with diabetes [see Drug Interactions (7.2)].
5. Warnings and Precautions
5.1 Fetal Toxicity
Azor can cause fetal harm when administered to a pregnant woman. Use of drugs that act on the renin-angiotensin system during the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and death. Resulting oligohydramnios can be associated with fetal lung hypoplasia and skeletal deformations. Potential neonatal adverse effects include skull hypoplasia, anuria, hypotension, renal failure, and death. When pregnancy is detected, discontinue Azor as soon as possible [see Use in Specific Populations (8.1)].
5.2 Hypotension in Volume- or Salt-Depleted Patients
Olmesartan medoxomil. In patients with an activated renin-angiotensin system, such as volume- and/or salt-depleted patients (e.g., those being treated with high doses of diuretics) symptomatic hypotension may be anticipated after initiation of treatment with olmesartan medoxomil. Initiate treatment with Azor under close medical supervision. If hypotension does occur, place the patient in the supine position and, if necessary, give an intravenous infusion of normal saline. A transient hypotensive response is not a contraindication to further treatment, which usually can be continued without difficulty once the blood pressure has stabilized.
Amlodipine. Symptomatic hypotension is possible, particularly in patients with severe aortic stenosis. Because of the gradual onset of action, acute hypotension is unlikely.
5.3 Increased Angina or Myocardial Infarction
Patients, particularly those with severe obstructive coronary artery disease, may develop increased frequency, duration, or severity of angina or acute myocardial infarction on starting calcium channel blocker therapy or at the time of dosage increase. The mechanism of this effect has not been elucidated.
5.4 Impaired Renal Function
Changes in renal function may be anticipated in susceptible individuals treated with olmesartan medoxomil as a consequence of inhibiting the renin-angiotensin-aldosterone system. In patients whose renal function may depend upon the activity of the renin-angiotensin-aldosterone system (e.g., patients with severe congestive heart failure), treatment with angiotensin converting enzyme inhibitors and angiotensin receptor antagonists has been associated with oliguria or progressive azotemia and (rarely) with acute renal failure and/or death. Similar effects may occur in patients treated with Azor because of the olmesartan medoxomil component [see Drug Interactions (7) and Clinical Pharmacology (12.3)].
In studies of ACE inhibitors in patients with unilateral or bilateral renal artery stenosis, increases in serum creatinine or blood urea nitrogen (BUN) have been reported. There has been no long-term use of olmesartan medoxomil in patients with unilateral or bilateral renal artery stenosis, but similar effects would be expected with olmesartan medoxomil and Azor.
5.5 Patients with Hepatic Impairment
Patients with hepatic impairment have decreased clearance of amlodipine. Starting amlodipine or adding amlodipine at 2.5 mg in hepatically impaired patients is recommended. The lowest dose of Azor is 5/20 mg; therefore, initial therapy with Azor is not recommended in hepatically impaired patients [see Use in Specific Populations (8.6)].
Since amlodipine is extensively metabolized by the liver and the plasma elimination half-life (t½) is 56 hours in patients with severely impaired hepatic function, titrate slowly when administering to patients with severe hepatic impairment.
5.6 Sprue-like Enteropathy
Severe, chronic diarrhea with substantial weight loss has been reported in patients taking olmesartan months to years after drug initiation. Intestinal biopsies of patients often demonstrated villous atrophy. If a patient develops these symptoms during treatment with olmesartan, exclude other etiologies. Consider discontinuation of Azor in cases where no other etiology is identified.
6. Adverse Reactions/Side Effects
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
Azor
The data described below reflect exposure to Azor in more than 1600 patients including more than 1000 exposed for at least 6 months and more than 700 exposed for 1 year. Azor was studied in one placebo-controlled factorial trial [see Clinical Trials (14.1)]. The population had a mean age of 54 years and included approximately 55% males. Seventy-one percent were Caucasian and 25% were Black. Patients received doses ranging from 5/20 mg to 10/40 mg orally once daily.
The overall incidence of adverse reactions on therapy with Azor was similar to that seen with corresponding doses of the individual components of Azor, and to placebo. The reported adverse reactions were generally mild and seldom led to discontinuation of treatment (2.6% for Azor and 6.8% for placebo).
Edema
Edema is a known, dose-dependent adverse effect of amlodipine but not of olmesartan medoxomil.
The placebo-subtracted incidence of edema during the 8-week, randomized, double-blind treatment period was highest with amlodipine 10 mg monotherapy. The incidence was significantly reduced when 20 mg or 40 mg of olmesartan medoxomil was added to the 10 mg amlodipine dose.
Placebo-Subtracted Incidence of Edema During the Double-Blind Treatment Period
| Olmesartan Medoxomil | ||||
| Placebo | 20 mg | 40 mg | ||
| Amlodipine | Placebo | -* | -2.4% | 6.2% |
| 5 mg | 0.7% | 5.7% | 6.2% | |
| 10 mg | 24.5% | 13.3% | 11.2% | |
| *12.3% = actual placebo incidence | ||||
Across all treatment groups, the frequency of edema was generally higher in women than men, as has been observed in previous studies of amlodipine.
There was a greater decrease in hemoglobin and hematocrit in patients treated with Azor as compared to patients receiving either component.
Adverse reactions seen at lower rates during the double-blind period also occurred in the patients treated with Azor at about the same or greater incidence as in patients receiving placebo. These included hypotension, orthostatic hypotension, rash, pruritus, palpitation, urinary frequency, and nocturia.
The adverse event profile obtained from 44 weeks of open-label combination therapy with amlodipine plus olmesartan medoxomil was similar to that observed during the 8-week, double-blind, placebo-controlled period.
Initial Therapy
Analyzing the data described above specifically for initial therapy, it was observed that higher doses of Azor caused slightly more hypotension and orthostatic symptoms, but not at the recommended starting dose of Azor 5/20 mg. No increase in the incidence of syncope or near syncope was observed. The incidences of discontinuation because of any treatment emergent adverse events in the double-blind phase are summarized in the table below.
Discontinuation for any Treatment Emergent Adverse Event1
| Olmesartan Medoxomil | |||||
| Placebo | 10 mg | 20 mg | 40 mg | ||
| Amlodipine | Placebo | 4.9% | 4.3% | 5.6% | 3.1% |
| 5 mg | 3.7% | 0.0% | 1.2% | 3.7% | |
| 10 mg | 5.5% | 6.8% | 2.5% | 5.6% | |
| 1 Hypertension is counted as treatment failure and not as treatment emergent adverse event. N=160-163 subjects per treatment group. |
|||||
Amlodipine.
Amlodipine has been evaluated for safety in more than 11,000 patients in U.S. and foreign clinical trials. Most adverse reactions reported during therapy with amlodipine were of mild or moderate severity. In controlled clinical trials directly comparing amlodipine (N=1730) in doses up to 10 mg to placebo (N=1250), discontinuation of amlodipine due to adverse reactions was required in only about 1.5% of amlodipine-treated patients and about 1% of placebo-treated patients. The most common side effects were headache and edema. The incidence (%) of dose-related side effects was as follows:
| Adverse Event | Placebo N=520 | 2.5 mg N=275 | 5.0 mg N=296 | 10.0 mg N=268 |
| Edema | 0.6 | 1.8 | 3.0 | 10.8 |
| Dizziness | 1.5 | 1.1 | 3.4 | 3.4 |
| Flushing | 0.0 | 0.7 | 1.4 | 2.6 |
| Palpitation | 0.6 | 0.7 | 1.4 | 4.5 |
For several adverse experiences that appear to be drug- and dose-related, there was a greater incidence in women than men associated with amlodipine treatment as shown in the following table:
| Adverse Event | Placebo | Amlodipine | ||
| Male=% (N=914) | Female=% (N=336) | Male=% (N=1218) | Female=% (N=512) |
|
| Edema | 1.4 | 5.1 | 5.6 | 14.6 |
| Flushing | 0.3 | 0.9 | 1.5 | 4.5 |
| Palpitation | 0.9 | 0.9 | 1.4 | 3.3 |
| Somnolence | 0.8 | 0.3 | 1.3 | 1.6 |
Olmesartan medoxomil.
Olmesartan medoxomil has been evaluated for safety in more than 3825 patients/subjects, including more than 3275 patients treated for hypertension in controlled trials. This experience included about 900 patients treated for at least 6 months and more than 525 treated for at least 1 year. Treatment with olmesartan medoxomil was well tolerated, with an incidence of adverse events similar to that seen with placebo. Events were generally mild, transient, and without relationship to the dose of olmesartan medoxomil.
The overall frequency of adverse events was not dose related. Analysis of gender, age, and race groups demonstrated no differences between olmesartan medoxomil- and placebo-treated patients. The rate of withdrawals due to adverse events in all trials of hypertensive patients was 2.4% (i.e., 79/3278) of patients treated with olmesartan medoxomil and 2.7% (i.e., 32/1179) of control patients. In placebo-controlled trials, the only adverse event that occurred in more than 1% of patients treated with olmesartan medoxomil and at a higher incidence in olmesartan medoxomil treated patients vs. placebo was dizziness (3% vs 1%).
7. Drug Interactions
7.1 Drug Interactions with Amlodipine
Simvastatin: Co-administration of simvastatin with amlodipine increases the systemic exposure of simvastatin. Limit the dose of simvastatin in patients on amlodipine to 20 mg daily [see Clinical Pharmacology (12.3)].
Immunosuppressants: Amlodipine may increase the systemic exposure of cyclosporine or tacrolimus when co-administered. Frequent monitoring of trough blood levels of cyclosporine and tacrolimus is recommended and adjust the dose when appropriate [see Clinical Pharmacology (12.3)].
CYP3A Inhibitors: Co-administration of amlodipine with CYP3A inhibitors (moderate and strong) results in increased systemic exposure to amlodipine and may require dose reduction. Monitor for symptoms of hypotension and edema when amlodipine is co-administered with CYP3A inhibitors to determine the need for dose adjustment.
CYP3A Inducers: No information is available on the quantitative effects of CYP3A inducers on amlodipine. Blood pressure should be closely monitored when amlodipine is co-administered with CYP3A inducers.
7.2 Drug Interactions with Olmesartan Medoxomil
Non-Steroidal Anti-Inflammatory Agents including Selective Cyclooxygenase-2 Inhibitors (COX-2 Inhibitors):
In patients who are elderly, volume-depleted (including those on diuretic therapy), or with compromised renal function, co-administration of NSAIDs, including selective COX-2 inhibitors, with angiotensin II receptor antagonists, including olmesartan medoxomil, may result in deterioration of renal function, including possible acute renal failure. These effects are usually reversible. Monitor renal function periodically in patients receiving olmesartan medoxomil and NSAID therapy.
The antihypertensive effect of angiotensin II receptor antagonists, including olmesartan medoxomil may be attenuated by NSAIDs including selective COX-2 inhibitors.
Dual Blockade of the Renin-Angiotensin System (RAS):
Dual blockade of the RAS with angiotensin receptor blockers, ACE inhibitors, or aliskiren is associated with increased risks of hypotension, hyperkalemia, and changes in renal function (including acute renal failure) compared to monotherapy. Most patients receiving the combination of two RAS inhibitors do not obtain any additional benefit compared to monotherapy. In general, avoid combined use of RAS inhibitors. Closely monitor blood pressure, renal function and electrolytes in patients on Azor and other agents that affect the RAS.
Do not co-administer aliskiren with Azor in patients with diabetes [see Contraindications (4)]. Avoid use of aliskiren with Azor in patients with renal impairment (GFR <60 ml/min).
Use with Colesevelam Hydrochloride:
Concurrent administration of bile acid sequestering agent colesevelam hydrochloride reduces the systemic exposure and peak plasma concentration of olmesartan. Administration of olmesartan at least 4 hours prior to colesevelam hydrochloride decreased the drug interaction effect. Consider administering olmesartan at least 4 hours before the colesevelam hydrochloride dose [see Clinical Pharmacology (12.3)].
Lithium:
Increases in serum lithium concentrations and lithium toxicity have been reported during concomitant administration of lithium with angiotensin II receptor antagonists, including AZOR. Monitor serum lithium levels during concomitant use.
8. Use In Specific Populations
8.1 Pregnancy
8.4 Pediatric Use
The safety and effectiveness of Azor in pediatric patients have not been established.
8.5 Geriatric Use
Of the total number of subjects in the double-blind clinical study of Azor, 20% (384/1940) were 65 years of age or older and 3% (62/1940) were 75 years or older. No overall differences in safety or effectiveness were observed between subjects 65 years of age or older and younger subjects.
Elderly patients have decreased clearance of amlodipine. Starting amlodipine or adding amlodipine at 2.5 mg in patients ≥75 years old is recommended. The lowest dose of Azor is 5/20 mg; therefore, initial therapy with Azor is not recommended in patients ≥75 years old.
Amlodipine. Reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. Elderly patients have decreased clearance of amlodipine with a resulting increase of AUC of approximately 40% to 60%, and a lower initial dose may be required.
Olmesartan medoxomil. Of the total number of hypertensive patients receiving olmesartan medoxomil in clinical studies, more than 20% were 65 years of age and over, while more than 5% were 75 years of age and older. No overall differences in effectiveness or safety were observed between elderly patients and younger patients. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Hepatic Impairment
There are no studies of Azor in patients with hepatic insufficiency, but both amlodipine and olmesartan medoxomil show moderate increases in exposure in patients with hepatic impairment.
The recommended initial dose of amlodipine in patients with severe hepatic impairment is 2.5 mg, a dose not available with Azor.
Amlodipine. Amlodipine is extensively metabolized by the liver and the plasma elimination half-life (t½) is 56 hours in patients with severely impaired hepatic function [see Warnings and Precautions (5.5)].
Olmesartan medoxomil. Increases in AUC0-∞ and peak plasma concentration (Cmax) for olmesartan were observed with moderate hepatic impairment compared to those in matched controls with an increase in AUC of about 60%.
12. Azor - Clinical Pharmacology
12.3 Pharmacokinetics
The pharmacokinetics of amlodipine and olmesartan medoxomil from Azor are equivalent to the pharmacokinetics of amlodipine and olmesartan medoxomil when administered separately. The bioavailability of both components is well below 100%, but neither component is affected by food. The effective half-lives of amlodipine (45±11 hours) and olmesartan (7±1 hours) result in a 2- to 3- fold accumulation for amlodipine and negligible accumulation for olmesartan with once-daily dosing.
Amlodipine. After oral administration of therapeutic doses of amlodipine, absorption produces peak plasma concentrations between 6 and 12 hours. Absolute bioavailability is estimated as between 64% and 90%.
Olmesartan medoxomil. Olmesartan medoxomil is rapidly and completely bioactivated by ester hydrolysis to olmesartan during absorption from the gastrointestinal tract. The absolute bioavailability of olmesartan medoxomil is approximately 26%. After oral administration, the peak plasma concentration (Cmax) of olmesartan is reached after 1 to 2 hours. Food does not affect the bioavailability of olmesartan medoxomil.
Distribution
Amlodipine. Ex vivo studies have shown that approximately 93% of the circulating drug is bound to plasma proteins in hypertensive patients. Steady-state plasma levels of amlodipine are reached after 7 to 8 days of consecutive daily dosing.
Olmesartan medoxomil. The volume of distribution of olmesartan is approximately 17 L. Olmesartan is highly bound to plasma proteins (99%) and does not penetrate red blood cells. The protein binding is constant at plasma olmesartan concentrations well above the range achieved with recommended doses.
In rats, olmesartan crossed the blood-brain barrier poorly, if at all. Olmesartan passed across the placental barrier in rats and was distributed to the fetus. Olmesartan was distributed to milk at low levels in rats.
Metabolism and Excretion
Amlodipine. Amlodipine is extensively (about 90%) converted to inactive metabolites via hepatic metabolism. Elimination from the plasma is biphasic with a terminal elimination half-life of about 30 to 50 hours. Ten percent of the parent compound and 60% of the metabolites are excreted in the urine.
Olmesartan medoxomil. Following the rapid and complete conversion of olmesartan medoxomil to olmesartan during absorption, there is virtually no further metabolism of olmesartan. Total plasma clearance of olmesartan is 1.3 L/h, with a renal clearance of 0.6 L/h. Approximately 35% to 50% of the absorbed dose is recovered in urine while the remainder is eliminated in feces via the bile.
Olmesartan appears to be eliminated in a biphasic manner with a terminal elimination half-life of approximately 13 hours. Olmesartan shows linear pharmacokinetics following single oral doses of up to 320 mg and multiple oral doses of up to 80 mg. Steady-state levels of olmesartan are achieved within 3 to 5 days and no accumulation in plasma occurs with once-daily dosing.
Specific Populations
Geriatric Patients
The pharmacokinetic properties of Azor in the elderly are similar to those of the individual components.
Amlodipine. Elderly patients have decreased clearance of amlodipine with a resulting increase in AUC of approximately 40% to 60%, and a lower initial dose may be required.
Olmesartan medoxomil. The pharmacokinetics of olmesartan medoxomil were studied in the elderly (≥65 years). Overall, maximum plasma concentrations of olmesartan were similar in young adults and the elderly. Modest accumulation of olmesartan was observed in the elderly with repeated dosing; AUCѕѕ, τ was 33% higher in elderly patients, corresponding to an approximate 30% reduction in CLR.
Pediatric Patients
Amlodipine. Sixty-two hypertensive patients aged 6 to 17 years received doses of amlodipine between 1.25 mg and 20 mg. Weight-adjusted clearance and volume of distribution were similar to values in adults.
Olmesartan medoxomil. The pharmacokinetics of olmesartan medoxomil have not been investigated in patients <18 years of age.
Male and Female Patients
Population pharmacokinetic analysis indicated that female patients had approximately 15% smaller clearances of olmesartan than male patients. Gender had no effect on the clearance of amlodipine.
Olmesartan medoxomil. Minor differences were observed in the pharmacokinetics of olmesartan medoxomil in women compared to men. AUC and Cmax were 10% to 15% higher in women than in men.
14. Clinical Studies
14.1 Azor
An 8-week multicenter, randomized, double-blind, placebo controlled, parallel group factorial study in patients with mild to severe hypertension was conducted to determine if treatment with Azor was associated with clinically significant reduction in blood pressure compared to the respective monotherapies. The study randomized 1940 patients equally to one of the following 12 treatment arms: placebo, monotherapy treatment with amlodipine 5 mg or 10 mg, monotherapy treatment with olmesartan medoxomil 10 mg, 20 mg, or 40 mg, or combination therapy with amlodipine/ olmesartan medoxomil at doses of 5/10 mg, 5/20 mg, 5/40 mg, 10/10 mg, 10/20 mg, and 10/40 mg. Patients discontinued their prior antihypertensive treatment. The mean baseline blood pressure of the study population was 164/102 mmHg. Of the total cohort, 970 patients were treated with the combination as initial therapy.
Treatment with Azor resulted in statistically significant greater reductions in diastolic and systolic blood pressure compared to the respective monotherapy components. Maximum antihypertensive effects were attained within 2 weeks after a change in dose.
The following table presents the results for mean reduction in seated systolic and diastolic blood pressure following 8 weeks of treatment with Azor. Placebo-adjusted reductions from baseline in blood pressure were progressively greater with increases in dose of both amlodipine and olmesartan medoxomil components of Azor.
Reduction in Seated Systolic/Diastolic Blood Pressure (mmHg): Combination Therapy vs. Monotherapy Components (Double-Blind Treatment Period)
| Olmesartan medoxomil | |||||||
| (mmHg) | Placebo | 10 mg | 20 mg | 40 mg | |||
| Amlodipine | Placebo | Mean Change | -5/-3 | -12/-8 | -14/-9 | -16/-10 | |
| Placebo-Adjusted Mean Change | -- | -8/-5 | -10/-6 | -13/-7 | |||
| 5 mg | Mean Change | -15/-9 | -24/-14 | -24/-14 | -25/-16 | ||
| Placebo-Adjusted Mean Change | -12/-7 | -20/-11 | -20/-11 | -22/-13 | |||
| 10 mg | Mean Change | -20/-13 | -25/-16 | -29/-17 | -30/-19 | ||
| Placebo-Adjusted Mean Change | -16/-10 | -22/-13 | -25/-14 | -26/-16 | |||
The antihypertensive effect of Azor was similar in patients with and without prior antihypertensive medication use, in patients with and without diabetes, in patients ≥65 years of age and <65 years of age, and in women and men. Limited data exist in patients ≥75 years of age.
Azor was effective in treating black patients (usually a low-renin population), and the magnitude of blood pressure reduction in black patients approached that observed for non-Black patients. This effect in black patients has been seen with ACE inhibitors, angiotensin receptor blockers, and beta-blockers.
The blood pressure lowering effect was maintained throughout the 24-hour period with Azor once daily, with trough-to-peak ratios for systolic and diastolic response between 71% and 82%.
Upon completing the 8-week, double-blind, placebo-controlled study, 1684 patients entered a 44-week open-label extension and received combination therapy with amlodipine 5 mg plus olmesartan medoxomil 40 mg. During the open-label extension, patients whose blood pressure was not adequately controlled (i.e., did not achieve a blood pressure goal of <140/90 mmHg, or <130/80 mmHg for those patients with diabetes) on amlodipine/olmesartan medoxomil 5/40 mg were titrated to amlodipine /olmesartan medoxomil 10/40 mg. Patients whose blood pressure was still not adequately controlled were offered additional hydrochlorothiazide 12.5 mg and subsequently 25 mg as required to achieve adequate blood pressure goal.
There are no trials of Azor demonstrating reductions in cardiovascular risk in patients with hypertension, but at least one pharmacologically similar drug has demonstrated such benefits.
| AZOR
amlodipine besylate and olmesartan medoxomil tablet, film coated |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| AZOR
amlodipine besylate and olmesartan medoxomil tablet, film coated |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| AZOR
amlodipine besylate and olmesartan medoxomil tablet, film coated |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| AZOR
amlodipine besylate and olmesartan medoxomil tablet, film coated |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| Labeler - Daiichi Sankyo Inc. (068605067) |




![The structural formula for amlodipine besylate is chemically described as 3-ethyl-5-methyl (±)-2-[(2-aminoethoxy)methyl]-4-(2-chlorophenyl)-1,4-dihydro-6-methyl-3,5-pyridinedicarboxylate, monobenzenesulphonate. Its empirical formula is C20H25ClN2O5•C6H6O3S.](https://cdn.themeditary.com/images/2023/09/02/azor-05.webp)
![The structural formula for olmesartan medoxomil is chemically described as 2,3-dihydroxy-2-butenyl 4-(1-hydroxy-1-methylethyl)-2-propyl-1-[p-(o-1H-tetrazol-5-ylphenyl)benzyl]imidazole-5-carboxylate, cyclic 2,3-carbonate. Its empirical formula is C29H30N6O6.](https://cdn.themeditary.com/images/2023/09/02/azor-06.webp)