Drug Detail:Besremi (Ropeginterferon alfa-2b-njft)
Drug Class: Antineoplastic interferons
Highlights of Prescribing Information
WARNING: RISK OF SERIOUS DISORDERS
See full prescribing information for complete boxed warning.
Risk of Serious Disorders: Interferon alfa products may cause or aggravate fatal or life-threatening neuropsychiatric, autoimmune, ischemic, and infectious disorders. Monitor closely and withdraw therapy with persistently severe or worsening signs or symptoms of the above disorders.
Indications and Usage for Besremi
BESREMi is an interferon alfa-2b indicated for the treatment of adults with polycythemia vera ( 1)
Besremi Dosage and Administration
- Recommended starting dose: 100 mcg by subcutaneous injection every 2 weeks (50 mcg if receiving hydroxyurea).
- Increase the dose by 50 mcg every 2 weeks (up to a maximum of 500 mcg) until hematological parameters are stabilized ( 2.1)
- Interrupt or discontinue dosing if certain adverse reactions occur ( 2.3, 5)
Dosage Forms and Strengths
- Injection: 500 mcg/mL solution in a single-dose prefilled syringe ( 3)
Contraindications
- Existence of, or history of severe psychiatric disorders, particularly severe depression, suicidal ideation or suicide attempt ( 4)
- Hypersensitivity to interferon or to any component of BESREMi ( 4)
- Hepatic impairment (Child-Pugh B or C) ( 4)
- History or presence of active serious or untreated autoimmune disease ( 4)
- Immunosuppressed transplant recipients ( 4)
Warnings and Precautions
Patients exhibiting the following events should be closely monitored and may require dose reduction or discontinuation of therapy:
- Depression and Suicide: Monitor closely for symptoms and need for treatment. ( 5.1)
- Endocrine Toxicity: Discontinue if endocrine disorders occur that cannot be medically managed. ( 5.2)
- Cardiovascular Toxicity: Avoid use in patients with severe, acute or unstable cardiovascular disease. Monitor patients with history of cardiovascular disorders more frequently. ( 5.3)
- Decreased Peripheral Blood Counts: Perform blood counts at baseline, every 2 weeks during titration, and at least every 3-6 months during maintenance treatment. ( 5.4)
- Hypersensitivity Reactions: Stop treatment and immediately manage reaction. ( 5.5)
- Pancreatitis: Consider discontinuation if confirmed pancreatitis ( 5.6)
- Colitis: Discontinue if signs or symptoms of colitis ( 5.7)
- Pulmonary Toxicity: Discontinue if pulmonary infiltrates or pulmonary function impairment ( 5.8)
- Ophthalmologic Toxicity: Advise patients to have eye examinations before and during treatment. Evaluate eye symptoms promptly and discontinue if new or worsening eye disorders. ( 5.9)
- Hyperlipidemia: Monitor serum triglycerides before BESREMi treatment and intermittently during therapy and manage when elevated. ( 5.10)
- Hepatotoxicity: Monitor liver enzymes and hepatic function at baseline and during treatment. Reduce dose or discontinue depending on severity. ( 5.11)
- Renal Toxicity: Monitor serum creatinine at baseline and during therapy. Discontinue if severe renal impairment develops. ( 5.12)
- Dental and Periodontal Toxicity: Advise patients on good oral hygiene and to have regular dental examinations. ( 5.13)
- Dermatologic Toxicity: Consider discontinuing if clinically significant dermatologic toxicity. ( 5.14)
- Driving and Operating Machinery: Advise patients to avoid driving or using machinery if they experience dizziness, somnolence, or hallucination. ( 5.15)
Adverse Reactions/Side Effects
The most common adverse reactions reported in > 40% of patients were influenza-like illness, arthralgia, fatigue, pruritus, nasopharyngitis, and musculoskeletal pain ( 6).
To report SUSPECTED ADVERSE REACTIONS, contact PharmaEssentia at 1-800-999-2449 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Monitor patients taking CYP450 substrates with a narrow therapeutic index for adverse reactions to inform the need for dose adjustment of the concomitant drug ( 7.1)
- Avoid use with myelosuppressive agents and monitor patients receiving the combination for effects of excessive myelosuppression ( 7.2)
- Avoid use with narcotics, hypnotics or sedatives. Monitor patients receiving the combination for excessive central nervous system toxicity ( 7.3)
Use In Specific Populations
- Pregnancy: Can cause fetal harm. Advise females of reproductive potential of the potential risk to a fetus and to use effective contraception. ( 8.1, 8.3)
- Lactation: Advise women not to breastfeed during treatment and for 8 weeks after the final dose. ( 8.2)
- Avoid use in patients with eGFR <30 mL/min. ( 8.6)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 11/2021
Related/similar drugs
Jakafi, ruxolitinib, ropeginterferon alfa-2bFull Prescribing Information
These highlights do not include all the information needed to use BESREMi safely and effectively. See full prescribing information for BESREMi. BESREMi (ropeginterferon alfa-2b-njft) injection, for subcutaneous use Initial U.S. Approval: 2021
WARNING: RISK OF SERIOUS DISORDERS
Risk of Serious Disorders: Interferon alfa products may cause or aggravate fatal or life-threatening neuropsychiatric, autoimmune, ischemic, and infectious disorders. Patients should be monitored closely with periodic clinical and laboratory evaluations. Therapy should be withdrawn in patients with persistently severe or worsening signs or symptoms of these conditions. In many, but not all cases, these disorders resolve after stopping therapy [ see Warnings and Precautions (5.1, 5,2, 5.3, 5.4) and Adverse Reactions (6.1)].
1. Indications and Usage for Besremi
BESREMi is indicated for the treatment of adults with polycythemia vera.
2. Besremi Dosage and Administration
2.1 Pre-Treatment Testing
Pregnancy testing is recommended prior to BESREMi treatment in females of reproductive potential [see Use in Specific Populations (8.3)] .
2.3 Dose Modifications
Monitor CBC every 2 weeks during the titration phase and dose modification phase. Phlebotomy as rescue treatment to normalize blood hyperviscosity may be necessary [see Clinical Pharmacology (12.2)] .
If dose interruption occurs, resume dosing at previously attained levels. If drug-related toxicities arise, reduce the dose to the next lower level or interrupt in accordance with the table below (Table 1). If there is insufficient efficacy at the decreased dose following dose modification, a dose increase attempt to the next higher dose level should be considered after recovery to grade 1 toxicity.
| Adverse Reaction * | Severity | Dosage Modification |
|---|---|---|
|
||
| Liver enzyme elevation with concomitant bilirubin elevation, or other evidence of hepatic decompensation | Any increase above baseline | Interrupt treatment until recovery, restart at dose 50 mcg lower than the interrupted dose. If the interrupted dose is 50 mcg, refrain from treatment until recovery. Consider permanent discontinuation if toxicity persists after four dose-modifications. |
| Liver enzyme elevation | >5 × the upper limit of normal (ULN) but ≤20 × ULN | Decrease dose by 50 mcg; if toxicity does not improve, continue decreasing at biweekly intervals until alanine aminotransferase (ALT) and aspartate aminotransferase (AST) recover < 3 × ULN if baseline was normal; 3 × baseline if baseline was abnormal, and gamma-glutamyltransferase (GGT) recovers to < 2.5 × ULN if baseline was normal; 2.5 × baseline if baseline was abnormal. |
| If the interrupted dose is 50 mcg, refrain from treatment until recovery. | ||
| >20 × ULN | Interrupt treatment until ALT and AST recover to < 3 × ULN if baseline was normal; 1.5 × baseline if baseline was abnormal, and gamma-glutamyltransferase (GGT) recovers to < 2.5 × ULN if baseline was normal; 2 × baseline if baseline was abnormal. Consider permanent discontinuation if toxicity persists after four dose-modifications. | |
| Cytopenia | Anemia: Hemoglobin (Hgb) < 8 g/dL | Decrease dose by 50 mcg; if toxicity does not improve, continue decreasing at biweekly intervals until recovery of Hgb >10.0 g/dL, platelets >75,000/mm 3, and WBC >3,000/mm 3 |
| Thrombocytopenia: platelet count < 50,000/mm 3 but ≥25,000/mm 3 | ||
| Leukopenia: white blood cell count (WBC) <2000/mm 3 but ≥1,000/mm 3 | ||
| If the interrupted dose is 50 mcg, refrain from treatment until recovery. | ||
| Anemia: Hemoglobin levels are life threatening, or urgent intervention needed | Interrupt treatment until recovery of Hgb >10.0 g/dL, platelets >75,000/mm 3, and WBC >3,000/mm 3. | |
| Thrombocytopenia: platelet count <25,000/mm 3 | Consider permanent discontinuation if toxicity persists after four dose-modifications. | |
| Leukopenia: WBC <1000/mm 3 | ||
| Depression | Mild, without suicidal ideation | Consider psychiatric consultation if persistent (>8 weeks). |
| Moderate, without suicidal ideation | Consider dose reduction and psychiatric consultation. | |
| Severe, or any severity with suicidal ideation | Discontinue therapy, recommend psychiatric consultation. | |
2.4 Preparation and Administration
Read the INSTRUCTIONS FOR USE before administering the single-dose BESREMi prefilled syringe. BESREMi is for subcutaneous injection only and may be administered by either a healthcare professional, a patient or a caregiver. Before a decision is made to allow BESREMi to be administered by a patient or caregiver, ensure that the patient is an appropriate candidate for self-administration or administration by a caregiver. Proper training on storage, preparation and administration technique should be provided. If a patient or caregiver is not an appropriate candidate for any reason, then BESREMi should be administered by a healthcare professional.
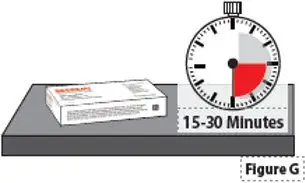
Before each injection, remove the carton that contains the BESREMi prefilled syringe from the refrigerator. Keep the prefilled syringe in the carton and lay it flat on a clean work surface for 15-30 minutes to allow the prefilled syringe to reach room temperature [59 ˚F to 77 ˚F (15 ˚C to 25 ˚C)].
Before injection, visually inspect BESREMi in the prefilled syringe for particulate matter and discoloration before administration (do not use if the solution in the syringe is cloudy, discolored, contains particulate matter or if the syringe shows any sign of damage).
3. Dosage Forms and Strengths
Injection: 500 mcg/mL clear and colorless to slightly yellowish solution in a single-dose prefilled syringe.
4. Contraindications
BESREMi is contraindicated in patients with:
- Existence of, or history of severe psychiatric disorders, particularly severe depression, suicidal ideation, or suicide attempt
- Hypersensitivity to interferons including interferon alfa-2b or any of the inactive ingredients of BESREMi
- Moderate (Child-Pugh B) or severe (Child-Pugh C) hepatic impairment
- History or presence of active serious or untreated autoimmune disease
- Immunosuppressed transplant recipients
5. Warnings and Precautions
5.1 Depression and Suicide
Life-threatening or fatal neuropsychiatric reactions have occurred in patients receiving interferon alfa products, including BESREMi. These reactions may occur in patients with and without previous psychiatric illness. Serious neuropsychiatric reactions have been observed in 3% of patients treated with BESREMi during the clinical development program. Among the 178 patients in the clinical development program of BESREMi, 17 cases of depression, depressive symptoms, depressed mood, and listlessness occurred. Of these seventeen cases, 3.4% of the patients recovered with temporary drug interruption and 2.8% stopped BESREMi treatment.
Other central nervous system effects, including suicidal ideation, attempted suicide, aggression, bipolar disorder, mania and confusion have been observed with other interferon alfa products. BESREMi is contraindicated in patients with a history of severe psychiatric disorders, particularly severe depression, suicidal ideation, or suicide attempt [see Contraindications (4)] .
Closely monitor patients for any symptoms of psychiatric disorders and consider psychiatric consultation and treatment if such symptoms emerge. If psychiatric symptoms worsen, it is recommended to discontinue BESREMi therapy.
5.2 Endocrine Toxicity
Endocrine toxicity has occurred in patients receiving interferon alfa products, including BESREMi. These toxicities may include worsening hypothyroidism and hyperthyroidism. Autoimmune thyroiditis and hyperglycemia, including new onset type 1 diabetes, have been reported in patients receiving interferon alfa-2b products. Eight cases of hyperthyroidism (4.5%), seven cases of hypothyroidism (3.9%) and five cases (2.8%) of autoimmune thyroiditis/thyroiditis occurred in the development program of BESREMi.
Do not use BESREMi in patients with active serious or untreated endocrine disorders associated with autoimmune disease [Contraindications (4)]. Evaluate thyroid function in patients who develop symptoms suggestive of thyroid disease during BESREMi therapy. Discontinue BESREMi in patients who develop endocrine disorders that cannot be adequately managed during treatment with BESREMi.
5.3 Cardiovascular Toxicity
Cardiovascular toxicity has occurred in patients receiving interferon alfa products, including BESREMi. Toxicities may include cardiomyopathy, myocardial infarction, atrial fibrillation and coronary artery ischemia [see Adverse Reactions (6.1)] . Patients with a history of cardiovascular disorders should be closely monitored for cardiovascular toxicity during BESREMi therapy. Avoid use of BESREMi in patients with severe or unstable cardiovascular disease, (e.g., uncontrolled hypertension, congestive heart failure (≥ NYHA class 2), serious cardiac arrhythmia, significant coronary artery stenosis, unstable angina) or recent stroke or myocardial infarction.
5.4 Decreased Peripheral Blood Counts
Decreased peripheral blood counts have occurred in patients receiving interferon alfa products, including BESREMi. These toxicities may include thrombocytopenia (increasing the risk of bleeding), anemia, and leukopenia (increasing the risk of infection). Thrombocytopenia of grade 3 (platelet counts <50,000 – 25,000/mm 3) or greater occurred in 2% of BESREMi-treated patients. Anemia of grade 3 (Hgb < 8 g/dL) or greater occurred in 1% of BESREMi-treated patients. Leukopenia of grade 3 (WBC counts <2,000 – 1,000/mm 3) or greater occurred in 2% of BESREMi-treated patients. Infection occurred in 48% of BESREMi treated patients, while serious infections occurred in 8% of BESREMi treated patients. Monitor complete blood counts at baseline, during titration and every 3-6 months during the maintenance phase. Monitor patients for signs and symptoms of infection or bleeding.
5.5 Hypersensitivity Reactions
Hypersensitivity reactions have occurred in patients receiving interferon alfa products, including BESREMi. BESREMi is contraindicated in patients with hypersensitivity reactions to interferon products or any of the inactive ingredients in BESREMi [see Contraindications (4)] . Toxicities may include serious, acute hypersensitivity reactions (e.g., urticaria, angioedema, bronchoconstriction, anaphylaxis). If such reactions occur, discontinue BESREMi and institute appropriate medical therapy immediately. Transient rashes may not necessitate interruption of treatment.
5.6 Pancreatitis
Pancreatitis has occurred in patients receiving interferon alfa products, including BESREMi. Pancreatitis was reported in 2.2% of patients receiving BESREMi. Symptoms may include nausea, vomiting, upper abdominal pain, bloating, and fever. Patients may experience elevated lipase, amylase, white blood cell count, or altered renal/hepatic function. Interrupt BESREMi treatment in patients with possible pancreatitis and evaluate promptly. Consider discontinuation of BESREMi in patients with confirmed pancreatitis.
5.7 Colitis
Fatal and serious ulcerative or hemorrhagic/ischemic colitis have occurred in patients receiving interferon alfa products, some cases occurring as early as 12 weeks after start of treatment. Symptoms may include abdominal pain, bloody diarrhea, and fever. Discontinue BESREMi in patients who develop these signs or symptoms. Colitis may resolve within 1 to 3 weeks of stopping treatment.
5.8 Pulmonary Toxicity
Pulmonary toxicity has occurred in patients receiving interferon alfa products, including BESREMi. Pulmonary toxicity may manifest as dyspnea, pulmonary infiltrates, pneumonia, bronchiolitis obliterans, interstitial pneumonitis, pulmonary hypertension, and sarcoidosis. Some events have resulted in respiratory failure or death. Discontinue BESREMi in patients who develop pulmonary infiltrates or pulmonary function impairment.
5.9 Ophthalmologic Toxicity
Ophthalmologic toxicity has occurred in patients receiving interferon alfa products, including BESREMi. These toxicities may include severe eye disorders such as retinopathy, retinal hemorrhage, retinal exudates, retinal detachment and retinal artery or vein occlusion which may result in blindness. During BESREMi therapy, 23% of patients were identified with an eye disorder. Eyes disorders ≥5% included cataract (6%) and dry eye (5%). Advise patients to have eye examinations before and during BESREMi therapy, specifically in those patients with a retinopathy-associated disease such as diabetes mellitus or hypertension. Evaluate eye symptoms promptly. Discontinue BESREMi in patients who develop new or worsening eye disorders.
5.10 Hyperlipidemia
Hyperlipidemia has occurred in patients treated with interferon alfa products, including BESREMi. Hyperlipidemia, hypertriglyceridemia, or dyslipidemia occurred in 3% of patients receiving BESREMi. Elevated triglycerides may result in pancreatitis [see Warnings and Precautions (5.6)] . Monitor serum triglycerides before BESREMi treatment and intermittently during therapy and manage when elevated. Consider discontinuation of BESREMi in patients with persistently, markedly elevated triglycerides.
5.11 Hepatotoxicity
Hepatotoxicity has occurred in patients receiving interferon alfa products, including BESREMi. These toxicities may include increases in serum ALT, AST, GGT and bilirubin. BESREMi is contraindicated in patients with moderate (Child-Pugh B) or severe (Child-Pugh C) hepatic impairment [see Contraindications (4)] .
Increases in serum ALT ≥3 times the upper limit of normal (ULN), AST ≥3 times the ULN, GGT ≥3 times the ULN, and bilirubin >2 times the ULN have been observed in patients treated with BESREMi.
In the clinical development program of BESREMi, 36 patients (20%) experienced liver enzyme elevations, 33 of whom had elevations of 1.25-5× ULN. Patients were able to resume BESREMi upon resolution of liver enzyme elevations. Liver enzyme elevations have also been reported in patients after long-term BESREMi therapy.
Monitor liver enzymes and hepatic function at baseline and during BESREMi treatment. Reduce BESREMi dosage by 50 mcg for increased AST/ALT/GGT then monitor AST/ALT/GGT weekly until the values return to baseline or grade 1 (ALT and AST < 3 × ULN if baseline was normal; 1.5 - 3 × baseline if baseline was abnormal, and GGT < 2.5 × ULN if baseline was normal; 2 - 2.5 × baseline if baseline was abnormal) [see Dosage and Administration (2.3)]. If toxicity does not improve, continue decreasing the BESREMi dose at biweekly intervals until recovery to grade 1. Hold if AST/ALT/GGT > 20 × ULN and consider permanent discontinuation if increased liver enzyme levels persist after four dose-reductions. Discontinue BESREMi in patients who develop evidence of hepatic decompensation (characterized by jaundice, ascites, hepatic encephalopathy, hepatorenal syndrome or variceal hemorrhage) during treatment [see Use in Specific Populations (8.7)] .
5.12 Renal Toxicity
Renal toxicity has occurred in patients receiving interferon alfa products, including BESREMi. During BESREMi therapy, <1% of patients were reported to develop renal impairment and <1% of patients were reported to have toxic nephropathy. Monitor serum creatinine at baseline and during therapy. Avoid use of BESREMi in patients with eGFR <30 mL/min. Discontinue BESREMi if severe renal impairment develops during treatment [see Use in Specific Populations (8.6)] .
5.13 Dental and Periodontal Toxicity
Dental and periodontal toxicities may occur in patients receiving interferon alfa products, including BESREMi. These toxicities may include dental and periodontal disorders, which may lead to loss of teeth. In addition, dry mouth could have a damaging effect on teeth and oral mucous membranes during long-term treatment with BESREMi. Patients should have good oral hygiene and regular dental examinations.
5.14 Dermatologic Toxicity
Dermatologic toxicity has occurred in patients receiving interferon alfa products, including BESREMi. These toxicities have included skin rash, pruritus, alopecia, erythema, psoriasis, xeroderma, dermatitis acneiform, hyperkeratosis, and hyperhidrosis. Consider discontinuation of BESREMi if clinically significant dermatologic toxicity occurs.
5.15 Driving and Operating Machinery
BESREMi may impact the ability to drive and use machinery. Patients should not drive or use heavy machinery until they know how BESREMi affects their abilities. Patients who experience dizziness, somnolence or hallucination during BESREMi therapy should avoid driving or using machinery.
5.16 Embryo-Fetal Toxicity
Based on the mechanism of action, BESREMi can cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (12.1) and Use in Specific Populations (8.1)] . Pregnancy testing is recommended in females of reproductive potential prior to treatment with BESREMi. Advise females of reproductive potential to use an effective method of contraception during treatment with BESREMi and for at least 8 weeks after the final dose [see Dosage and Administration (2.1) and Use in Specific Populations (8.1, 8.3)] .
6. Adverse Reactions/Side Effects
6.1 Clinical Trials Experience
The following clinically significant adverse reactions are described elsewhere in the labeling.
- Depression and Suicide [see Warnings and Precautions (5.1)]
- Endocrine Toxicity [see Warnings and Precautions (5.2)]
- Cardiovascular Toxicity [see Warnings and Precautions (5.3)]
- Decreased Peripheral Blood Counts [see Warnings and Precautions (5.4)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.5)]
- Pancreatitis [see Warnings and Precautions (5.6)]
- Colitis [see Warnings and Precautions (5.7)]
- Pulmonary Toxicity [see Warnings and Precautions (5.8)]
- Ophthalmologic Toxicity [see Warnings and Precautions (5.9)]
- Hyperlipidemia [see Warnings and Precautions (5.10)]
- Hepatotoxicity [see Warnings and Precautions (5.11)]
- Renal Toxicity [see Warnings and Precautions (5.12)]
- Dental and Periodontal Toxicity [see Warnings and Precautions (5.13)]
- Dermatologic Toxicity [see Warnings and Precautions (5.14)]
- Driving and Operating Machinery [see Warnings and Precautions (5.15)]
- Embryo-Fetal Toxicity [see Warnings and Precautions (5.16)]
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The pooled safety population described in the Warnings and Precautions section reflects exposure to BESREMi as monotherapy for the treatment of polycythemia vera dosed every two to four weeks in 178 patients in two open-label trials [ PEGINVERA, PROUD/CONTINUATION PV]. The mean age at baseline was 58.6 years (range 30-85 years), 88 (49.4%) women, 90 (50.6%) men, 177 (99%) Caucasian and 1 (1%) Asian. Among 178 patients who received BESREMi, 80% were exposed for 12 months or longer. The mean dose of BESREMi was 334 mcg SD ± 121 during the treatment period. In this pooled safety population, the most common adverse reactions greater than 10%, were liver enzyme elevations (20%), leukopenia (20%), thrombocytopenia (19%), arthralgia (13%), fatigue (12%), myalgia (11%), and influenza-like illness (11%).
The safety findings described below reflect exposure to BESREMi as monotherapy for the treatment of polycythemia vera in 51 patients in the PEGINVERA study [see Clinical Studies (14)] . Among the 51 patients receiving BESREMi, 71% were exposed for 12 months or longer, 63% were exposed for three years or longer, and 53% were exposed for greater than five years.
Serious adverse reactions were reported in 16% of patients in the PEGINVERA study. The most common serious adverse reactions observed during the study (≥ 4%) included urinary tract infection (8%), transient ischemic attack (6%) and depression (4%).
Adverse reactions requiring permanent discontinuation in >2% of patients who received BESREMi included depression (8%), arthralgia (4%), fatigue (4%), and general physical health deterioration (4%) In the PEGINVERA study, patients were not pre-screened for depression or anxiety disorders.
The most common adverse reactions reported in ≥10% of patients in the PEGINVERA study are listed in Table 2.
| Adverse Reactions * | BESREMi
N=51 % |
|---|---|
| Grouped Term Definitions | |
|
|
| Influenza-like illness † | 59 |
| Arthralgia | 47 |
| Fatigue ‡ | 47 |
| Pruritis | 45 |
| Nasopharyngitis § | 43 |
| Musculoskeletal pain ¶ | 41 |
| Headache # | 39 |
| Diarrhea | 33 |
| Hyperhidrosis Þ | 29 |
| Nausea | 28 |
| Upper respiratory tract infection ß | 27 |
| Local administration site reactions | 26 |
| Dizziness | 22 |
| Abdominal pain à | 20 |
| Depression | 20 |
| Sleep disorder è | 20 |
| Leukopenia | 18 |
| Decreased appetite | 18 |
| Alopecia | 16 |
| Edema ð | 16 |
| Hypertension ø | 16 |
| Muscle spasms | 16 |
| Neutropenia | 16 |
| Rash ý | 16 |
| Transaminase elevations £ | 16 |
| Urinary tract infection | 16 |
| Thrombocytopenia | 12 |
| Vertigo | 12 |
Clinically relevant adverse reactions in < 10% of patients include:
Cardiovascular System: Atrial fibrillation
6.2 Immunogenicity
As with all therapeutic proteins, there is potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors, including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies in the studies described below with the incidence of antibodies in other studies or to other interferon alfa-2b products may be misleading.
The incidence of binding antibodies to ropeginterferon alfa-2b-njft was 1.4% (2/146) and they were observed as early as 8 weeks post-dosing. Among the patients who tested positive for binding antibodies, none developed neutralizing antibodies.
7. Drug Interactions
7.1 Drugs Metabolized by Cytochrome P450
Certain proinflammatory cytokines, including interferons, can suppress CYP450 enzymes resulting in increased exposures of some CYP substrates [see Clinical Pharmacology (12.3)] . Therefore, patients on BESREMi who are receiving concomitant drugs that are CYP450 substrates with a narrow therapeutic index should be monitored to inform the need for dosage modification for these concomitant drugs.
8. Use In Specific Populations
8.2 Lactation
There are no data on the presence of BESREMi in human or animal milk, the effects on the breastfed child, or the effects on milk production. Because of the potential for serious adverse reactions in breastfed children from BESREMi, advise women not to breastfeed during treatment and for 8 weeks after the final dose.
8.3 Females and Males of Reproductive Potential
BESREMi may cause embryo-fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)] .
8.5 Geriatric Use
Clinical studies of BESREMi did not include sufficient numbers of subjects aged 65 years and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other therapy.
8.6 Renal Impairment
No dose adjustment is necessary in patients with estimated glomerular filtration rate (eGFR) ≥30 mL/min [see Clinical Pharmacology (12.3)]. Avoid use of BESREMi in patients with eGFR <30 mL/min [see Warnings and Precautions (5.12)].
8.7 Hepatic Impairment
BESREMi is contraindicated in patients with hepatic impairment (Child-Pugh B or C) [see Contraindications (4)] .
Increased liver enzyme levels have been observed in patients treated with BESREMi. When the increase in liver enzyme levels is progressive and persistent, reduce the dose of BESREMi. If the increase in liver enzymes is progressive and clinically significant despite dose-reduction, or if there is evidence of hepatic impairment (Child-Pugh B or C), discontinue BESREMi [see Dosage and Administration (2.2) and Warnings and Precautions (5.11)] .
10. Overdosage
Overdosage of BESREMi may result in influenza-like symptoms or other adverse reactions. There is no antidote to BESREMi overdosage. In case of an overdose, frequently monitor signs and symptoms for adverse reactions.
11. Besremi Description
Ropeginterferon alfa-2b-njft, an interferon alfa-2b, is an N-terminal monopegylated covalent conjugate of proline interferon alfa-2b, produced in Escherichia coli cells by recombinant DNA technology, with a methoxy polyethylene glycol (mPEG) moiety. Ropeginterferon alfa-2b-njft has an approximate molecular weight of 60 kDa and the approximate molecular weight of the PEG portion of the molecule is 40 kDa.
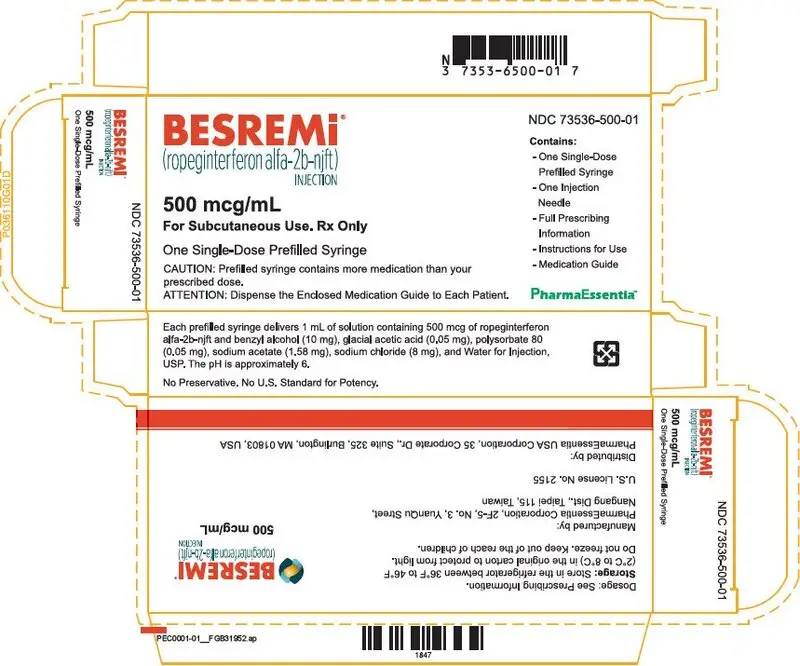
BESREMi (ropeginterferon alfa-2b-njft) injection is a sterile, preservative-free, clear and colorless to slightly yellowish solution for subcutaneous use supplied in a single dose prefilled syringe.
Each prefilled syringe delivers 1 mL of solution containing 500 mcg of ropeginterferon alfa-2b-njft and benzyl alcohol (10 mg), glacial acetic acid (0.05 mg), polysorbate 80 (0.05 mg), sodium acetate (1.58 mg), sodium chloride (8 mg), and Water for Injection, USP. The pH is approximately 6.
12. Besremi - Clinical Pharmacology
12.1 Mechanism of Action
Interferon alfa belongs to the class of type I interferons, which exhibit their cellular effects in polycythemia vera in the bone marrow by binding to a transmembrane receptor termed interferon alfa receptor (IFNAR). Binding to IFNAR initiates a downstream signaling cascade through the activation of kinases, in particular Janus kinase 1 (JAK1) and tyrosine kinase 2 (TYK2) and activator of transcription (STAT) proteins. Nuclear translocation of STAT proteins controls distinct gene-expression programs and exhibits various cellular effects. The actions involved in the therapeutic effects of interferon alfa in polycythemia vera are not fully elucidated.
12.2 Pharmacodynamics
The efficacy of ropeginterferon alfa-2b-njft is dependent on the stabilization of hematological parameters (hematocrit <45%, platelets <400 × 10 9/L and leukocytes <10 × 10 9/L). Pharmacokinetic-pharmacodynamic analyses have demonstrated that the reduction in the individual hematological parameters is dependent on ropeginterferon alfa-2b-njft concentrations. Complete hematological response (CHR, defined as a patient achieving hematocrit <45% without phlebotomy [at least 2 months since last phlebotomy], platelets ≤400 × 10 9/L and leukocytes ≤10 × 10 9/L) increased with increasing ropeginterferon alfa-2b-njft concentration over time. Based on the exposure-response (E-R) analyses using data from the PEGINVERA study, the predicted probability of CHR (95% Prediction Intervals) was 22% (11% – 34%) before treatment, 50% (38% – 62%) at week 20 (end of titration), 64% (47% – 78%) at week 52, and 70% (55% – 88%) at week 104. The E-R analyses show that the maximum probability of CHR is reached after 2 years of continuous treatment.
12.3 Pharmacokinetics
In patients with polycythemia vera, the estimated steady state C max, C min and area under the curve (AUC) after a two-week dosing interval of BESREMi over a dose range of 100 mcg to 500 mcg ranged from 4.4 – 31 ng/mL, 1.4 – 12 ng/mL, and 1011 – 7809 ng×h/mL, respectively. The estimated steady state C max occurs between 2 to 5 days.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Ropeginterferon alfa-2b-njft has not been tested for its carcinogenic potential. Neither ropeginterferon alfa-2b-njft nor its components, interferon or methoxypolyethylene glycol, caused damage to DNA when tested in the standard battery of mutagenesis assays. Ropeginterferon alfa-2b-njft effects on fertility have not been assessed [see Use in Specific Populations (8.1, 8.2, 8.3)] .
14. Clinical Studies
The efficacy and safety of BESREMi were evaluated in the PEGINVERA study, a prospective, multicenter, single-arm trial of 7.5 years duration. The study included 51 adults with polycythemia vera. The mean age at baseline was 56 years (range 35-82 years) with 20 (39%) women and 31 (61%) men. All patients had the JAK2V617F mutation with 16% of subjects being newly diagnosed; 84% had known disease with a median duration of 2.2 years. One-third (33%) of patients were undergoing treatment with hydroxyurea (HU) upon study entry. At baseline, the mean ± SD hematocrit, platelets, and leukocytes were 45% ± 4.0%, 457 ×10 9/L ± 187 ×10 9/L and 11.8 × 10 9/L ± 5.2 × 10 9/L, respectively. Median spleen size was 13.2 cm with 16 (31%) having splenomegaly (defined as a longitudinal diameter of >12 cm for women and >13 cm for men). Eleven patients (22%) had a prior history of a major cardiovascular event including pulmonary embolism (6), stroke (2), myocardial infarction (2) and portal vein thrombosis (1).
In stage I, the maximum tolerated dose, defined as the highest administered dose without dose-limiting toxicities was determined to be 540 mcg. In stage II, an intra-patient dose escalation began at 150 mcg, or 100 mcg if titrating from hydroxyurea, or at the highest dose achieved in those patients enrolled during stage I. Titration with BESREMi occurred every two-weeks at doses of 225 mcg, 300 mcg, 400 mcg and 450 mcg with dose escalation stopping when hematological parameters were stabilized. For patients transitioning from hydroxyurea, the hydroxyurea dose was tapered off over the first 12 weeks of treatment to avoid toxicity. After at least one year on therapy and at a median time of 21.5 months, 28 eligible patients in the PEGINVERA study increased the dosing interval to once every 4 weeks. Because of formulation changes, the recommended starting dose, titration amounts, and maximum dose of BESREMi differ slightly from those used in the trial [see Dosage and Administration (2)] .
The median duration of treatment exposure was 61 months and 53% of patients completed at least 60 months of treatment. Thirty-six patients completed one year of treatment with eleven patients discontinuing after one year of treatment mainly due to treatment emergent adverse events. The mean dose of BESREMi was 237 mcg (± 110) during the treatment period.
The efficacy of BESREMi was evaluated in the PEGINVERA study by assessing complete hematological response (CHR) defined as hematocrit <45% and no phlebotomy in the preceding 2 months, platelets ≤400 × 10 9/L and leukocytes ≤10 × 10 9/L, normal spleen size (longitudinal diameter ≤ 12 cm for females and ≤ 13 cm for males) assessed by ultrasound and absence of thromboembolic events.
The CHR in the treated population during the treatment period was 61% (31/51) (95% CI: 46, 74). The median duration of response was 14.3 months (95% CI: 5.5, 30.1).
Among the patients in the treated population who achieved a CHR, the median time to response was 7.8 months of treatment with BESREMi. It required 1.2 years of treatment with BESREMi for 50% of patients (hydroxyurea-naïve) to achieve a CHR and 1.4 years for 50% of patients with prior hydroxyurea use to achieve a CHR.
A hematological response based only on hematocrit, platelets, and leukocytes was achieved among 80% of patients treated with BESREMi (41/51) (95% CI: 67, 90). The median duration of this response was 20.8 months (95% CI: 13.0, 43.8).
16. How is Besremi supplied
16.1 How Supplied
BESREMi (ropeginterferon alfa-2b-njft) injection is a sterile, preservative-free, clear and colorless to slightly yellowish solution for subcutaneous administration in a single-dose prefilled syringe. Each carton contains one 500 mcg/mL prefilled syringe with a 30 gauge, ½ inch safety hypodermic needle (NDC 73536-500-01).
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide and Instructions for Use).
| INSTRUCTIONS FOR USE
BESREMi [bez-reh-me] (ropeginterferon alfa-2b-njft) injection, for subcutaneous use Single-dose prefilled syringe |
|||
|---|---|---|---|
| This "Instructions for Use" has been approved by the U.S. Food and Drug Administration. | Issued: November 2021 | ||
| This "Instructions for Use" contains information on how to prepare and inject BESREMi under your skin (subcutaneous injection) using the single-dose prefilled syringe. | |||
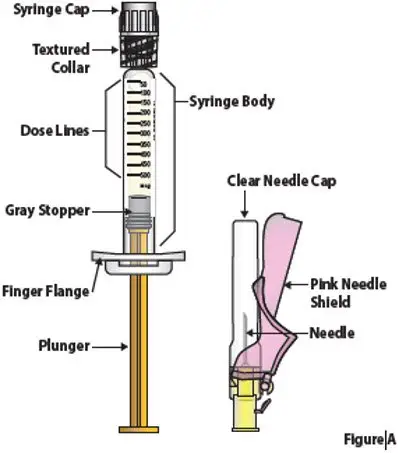
| Guide to Prefilled syringe and Needle Parts (Figure A) | |||
|
|
|||
| Storing BESREMi | |||
Store the BESREMi carton in the refrigerator between 36°F to 46°F (2°C to 8°C) (Figure B).
|
|||
| Important information you need to know before injecting BESREMi | |||
Read this Instructions for Use before using your single-dose BESREMi prefilled syringe for the first time and each time you get a new prescription. There may be new information. This leaflet does not take the place of talking with your healthcare provider about your medical condition or your treatment. Ask your healthcare provider about the right way to prepare and give your BESREMi injection.
|
|||
|
|
|||
| Gather and check supplies | |||
| 1. | Prepare BESREMi Prefilled Syringe | ||
| 1.1. | Take the BESREMi carton out of the refrigerator (Figure E).
|
||
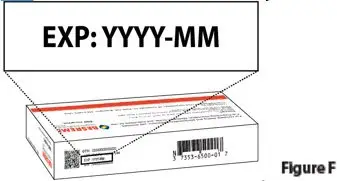
| 1.2. | Check the expiration date ("EXP") on the top panel of the carton to make sure it has not passed (Figure F).
Do not use the prefilled syringe if the expiration date has passed.
|
||
| 1.3. | Let carton containing the BESREMi prefilled syringe sit on a clean work surface for
15 to 30 minutes to allow it to come to room temperature (Figure G).
Do not warm the prefilled syringe any other way. |
||
|
|
|||
| 2. | Gather supplies for injection | ||
| 2.1. | After allowing the prefilled syringe to come to room temperature for 15 to 30 minutes inside the carton, gather the following additional supplies.
Alcohol Swab (Figure H).
|
||
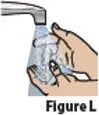
| 3. | Wash hands and remove syringe from tray | ||
| 3.1. | Wash your hands with soap and water, then dry your hands (Figure L).
|
||
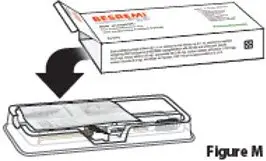
| 3.2. | Open the carton and remove the clear plastic tray that holds the BESREMi prefilled syringe and needle package (Figure M).
|
||
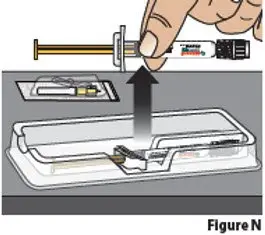
| 3.3. | Remove the needle package and BESREMi prefilled syringe from the plastic tray. Hold the prefilled syringe by the middle of the syringe body during removal (Figure N).
|
||
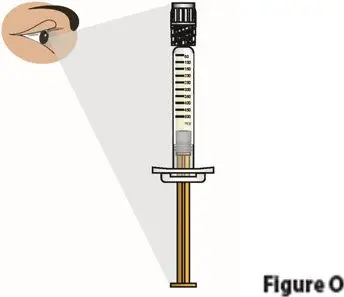
| 4. | Check the liquid medicine in the BESREMi prefilled syringe | ||
| 4.1. | Check the liquid medicine in the prefilled syringe (Figure O). The liquid should be clear and colorless to slightly yellow, and should not have particles.
Do not use the prefilled syringe if the liquid is cloudy, discolored, or contains particles. Contact your healthcare provider or pharmacist. |
||
| 4.2. | Check the syringe to see if it is damaged or broken (Figure O).
Do not use if it shows any signs of damage or breakage. Contact your healthcare provider or pharmacist.
|
||
| Prepare syringe for injection | |||
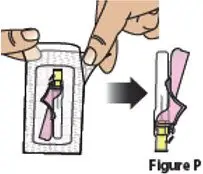
| 5. | Attach the needle to the BESREMi prefilled syringe | ||
| 5.1. | Carefully open the needle package, remove the needle, and set it aside (Figure P).
Throw away the packaging into household trash.
|
||
| 5.2. | Hold the prefilled syringe as shown. Remove the prefilled syringe cap by unscrewing it counter-clockwise (Figure Q).
Throw away the syringe cap into household trash. Do not allow the tip of the prefilled syringe to touch anything.
|
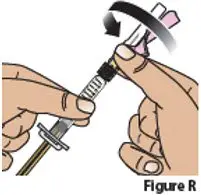
||
| 5.3. | Attach the needle to the prefilled syringe by firmly pushing it into the collar of the syringe and then screwing (turn clock-wise) it on until it feels securely attached (Figure R).
|
||
| 6. | Choose and clean injection site | ||
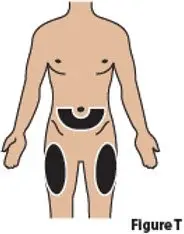
| 6.1. | Choose one of the following injection sites (Figure T):
|
||
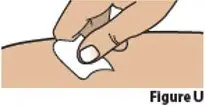
| 6.2. | Clean the chosen injection site with an alcohol swab and let it air dry (Figure U).
Do not blow on or touch the injection site after it has been cleaned.
|
||
| 7. | Uncap needle and move air bubbles to top | ||
| 7.1. | Pull the pink needle shield back (Figure V).
Note: The pink needle shield will be used after the injection to cover the needle and protect you from needle-stick injuries.
|
||
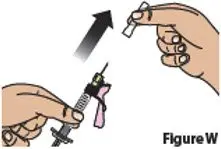
| 7.2. | Hold the syringe from the syringe body.
Remove the clear needle cap by pulling it straight off (Figure W). Throw away the needle cap into household trash. Do not recap needle.
|
||
| 7.3. | Hold the prefilled syringe with the needle pointing up.
Tap on the body of the prefilled syringe to move any air bubbles to the top (Figure X).
|
||
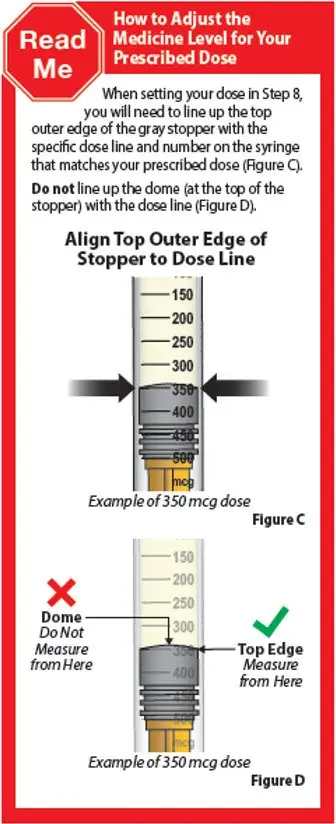
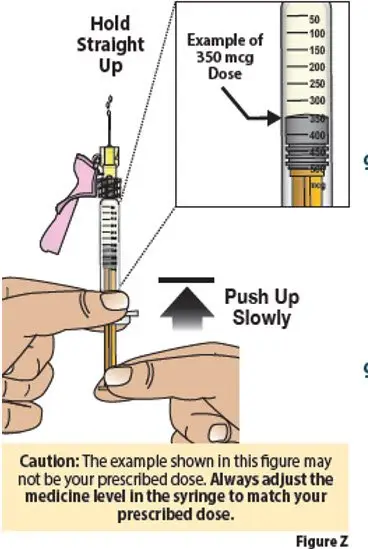
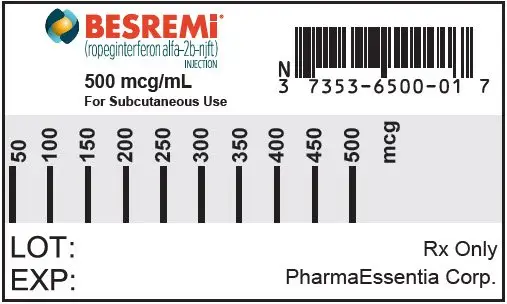
| 8. | Set your dose | ||
| 8.1. | Check your prescription to identify your prescribed dose (Figure Y). Depending on your prescribed dose, you may have to adjust the dose in the syringe by getting rid of (discarding) some medicine from the prefilled syringe before you inject the medicine.
|
||
| 8.2. | To set your dose follow the 4 steps below:
|
||
| Inject BESREMi | |||
| 9. | Give Injection | ||
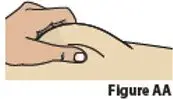
| 9.1. | Pinch the chosen injection site (Figure AA).
|
||
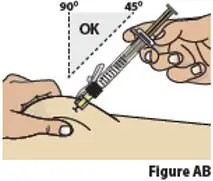
| 9.2. | While pinching the skin, insert the needle at a 45 to 90 degree angle into the pinched skin (Figure AB).
Then release the pinched skin.
|
||
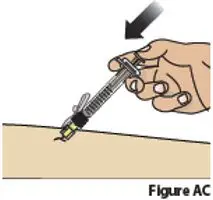
| 9.3. | Inject the medicine by slowly pressing down on the plunger all the way until it stops (Figure AC).
|
||
| 9.4. | After all the liquid medicine is injected, remove the needle from the skin (Figure AD).
|
||
| 9.5 | Cover needle
Carefully push the pink needle shield over the needle until it snaps into place and covers the needle (Figure AE). This helps prevent needle-stick injuries. Do not recap the needle using the needle cap. Only use the pink needle shield to cover the needle. |
||
|
|
|||
| Do not reuse the prefilled syringe and needle. | |||
| Disposing of used prefilled syringes and needles | |||
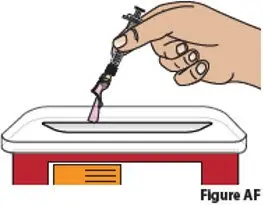
| 10. | Dispose of used prefilled syringes and needles.
|
||
| 11 | Check injection site. | ||
| 11.1 | If there is a small amount of blood or liquid at the injection site, press a gauze or cotton ball over the injection site until the bleeding stops (Figure AG). | ||
| 11.2 | Do not rub the injection site. If needed, you may apply a small adhesive bandage. | ||
|
|
|||
| Additional information. | |||
| For additional information about BESREMi and a video demonstration on how to use BESREMi, go to:
www.BESREMi.com |
|||
| Manufactured by:
PharmaEssentia Corporation 2F-5 No. 3 YuanQu Street Nangang Dist. Taipei, Taiwan U.S. License number: 2155 |
|||
| Distributed by:
PharmaEssentia Corporation 35 Corporate Drive, Suite 325, Burlington, MA 01803, USA |
|||
| BESREMi is a trademark/registered trademark of PharmaEssentia
Copyright 2021 PharmaEssentia |
|||
| BESREMI
ropeginterferon alfa-2b injection |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - PharmaEssentia USA (080514277) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| PharmaEssentia Corporation, Taichung Plant | 658873411 | api manufacture(73536-500) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| PYRAMID Laboratories, Inc. | 783409162 | analysis(73536-500) , manufacture(73536-500) | |