Drug Detail:Celestone soluspan (injection) (Betamethasone (injection) [ bay-ta-meth-a-sone ])
Drug Class: Glucocorticoids
Celestone Soluspan Description
CELESTONE® SOLUSPAN® Injectable Suspension is a sterile aqueous suspension containing 3 mg per milliliter betamethasone (equivalent to 3.95 mg betamethasone sodium phosphate USP) and 3 mg per milliliter betamethasone acetate. Inactive ingredients per mL: 8.9 mg dibasic sodium phosphate dihydrate; 3.8 mg monobasic sodium phosphate dihydrate; 0.1 mg edetate disodium; and 0.2 mg benzalkonium chloride as preservative. The pH is between 6.8 and 7.2.
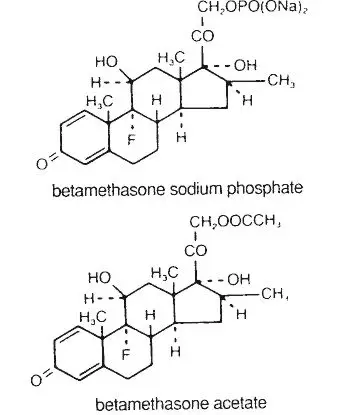
The formula for betamethasone sodium phosphate is C22H28FNa208P and it has a molecular weight of 516.40. Chemically, it is 9-Fluoro-11β,17,21-trihydroxy-16β-methylpregna-1,4-diene-3,20-dione 21-(disodium phosphate).
The formula for betamethasone acetate is C24H31FO6 and it has a molecular weight of 434.50. Chemically, it is 9-Fluoro-11β,17,21-trihydroxy-16β-methylpregna-1,4-diene-3,20-dione 21-acetate.
The chemical structures for betamethasone sodium phosphate and betamethasone acetate are as follows:
 |
Betamethasone sodium phosphate is a white to practically white, odorless powder, and is hygroscopic. It is freely soluble in water and in methanol, but is practically insoluble in acetone and in chloroform.
Betamethasone acetate is a white to creamy white, odorless powder that sinters and resolidifies at about 165°C, and remelts at about 200°C-220°C with decomposition. It is practically insoluble in water, but freely soluble in acetone, and is soluble in alcohol and in chloroform.
Warnings
CELESTONE® SOLUSPAN® Injectable Suspension should not be administered intravenously.
Infections
Vaccination
Administration of live or live, attenuated vaccines is contraindicated in patients receiving immunosuppressive doses of corticosteroids. Killed or inactivated vaccines may be administered. However, the response to such vaccines cannot be predicted. Immunization procedures may be undertaken in patients who are receiving corticosteroids as replacement therapy, eg, for Addison's disease.
Neurologic
Reports of severe medical events have been associated with the intrathecal route of administration (see ADVERSE REACTIONS, Gastrointestinal and Neurologic/Psychiatric sections).
Results from one multicenter, randomized, placebo-controlled study with methylprednisolone hemisuccinate, an IV corticosteroid, showed an increase in early mortality (at 2 weeks) and late mortality (at 6 months) in patients with cranial trauma who were determined not to have other clear indications for corticosteroid treatment. High doses of corticosteroids, including CELESTONE SOLUSPAN, should not be used for the treatment of traumatic brain injury.
Precautions
Neuro-psychiatric
Although controlled clinical trials have shown corticosteroids to be effective in speeding the resolution of acute exacerbations of multiple sclerosis, they do not show that they affect the ultimate outcome or natural history of the disease. The studies do show that relatively high doses of corticosteroids are necessary to demonstrate a significant effect (see DOSAGE AND ADMINISTRATION).
An acute myopathy has been observed with the use of high doses of corticosteroids, most often occurring in patients with disorders of neuromuscular transmission (eg, myasthenia gravis), or in patients receiving concomitant therapy with neuromuscular blocking drugs (eg, pancuronium). This acute myopathy is generalized, may involve ocular and respiratory muscles, and may result in quadriparesis. Elevation of creatinine kinase may occur. Clinical improvement or recovery after stopping corticosteroids may require weeks to years.
Psychic derangements may appear when corticosteroids are used, ranging from euphoria, insomnia, mood swings, personality changes, and severe depression to frank psychotic manifestations. Also, existing emotional instability or psychotic tendencies may be aggravated by corticosteroids.
Drug Interactions
Amphotericin B Injection and Potassium-Depleting Agents
When corticosteroids are administered concomitantly with potassium-depleting agents (ie, amphotericin B, diuretics), patients should be observed closely for development of hypokalemia. There have been cases reported in which concomitant use of amphotericin B and hydrocortisone was followed by cardiac enlargement and congestive heart failure.
Adverse Reactions/Side Effects
Gastrointestinal
Abdominal distention, bowel/bladder dysfunction (after intrathecal administration), elevation in serum liver enzyme levels (usually reversible upon discontinuation), hepatomegaly, increased appetite, nausea, pancreatitis, peptic ulcer with possible perforation and hemorrhage, perforation of the small and large intestine (particularly in patients with inflammatory bowel disease), ulcerative esophagitis.
Musculoskeletal
Aseptic necrosis of femoral and humeral heads, calcinosis (following intra-articular or intralesional use), Charcot-like arthropathy, loss of muscle mass, muscle weakness, osteoporosis, pathologic fracture of long bones, postinjection flare (following intra-articular use), steroid myopathy, tendon rupture, vertebral compression fractures.
Neurologic/Psychiatric
Convulsions, depression, emotional instability, euphoria, headache, increased intracranial pressure with papilledema (pseudotumor cerebri) usually following discontinuation of treatment, insomnia, mood swings, neuritis, neuropathy, paresthesia, personality changes, psychic disorders, vertigo. Arachnoiditis, meningitis, paraparesis/paraplegia, and sensory disturbances have occurred after intrathecal administration (see WARNINGS, Neurologic section).
Celestone Soluspan Dosage and Administration
Benzyl alcohol as a preservative has been associated with a fatal "Gasping Syndrome" in premature infants and infants of low birth weight. Solutions used for further dilution of this product should be preservative-free when used in the neonate, especially the premature infant. The initial dosage of parenterally administered CELESTONE® SOLUSPAN® Injectable Suspension may vary from 0.25 to 9.0 mg per day depending on the specific disease entity being treated. However, in certain overwhelming, acute, life-threatening situations, administrations in dosages exceeding the usual dosages may be justified and may be in multiples of the oral dosages.
It Should Be Emphasized That Dosage Requirements Are Variable and Must Be Individualized on the Basis of the Disease Under Treatment and the Response of the Patient. After a favorable response is noted, the proper maintenance dosage should be determined by decreasing the initial drug dosage in small decrements at appropriate time intervals until the lowest dosage which will maintain an adequate clinical response is reached. Situations which may make dosage adjustments necessary are changes in clinical status secondary to remissions or exacerbations in the disease process, the patient's individual drug responsiveness, and the effect of patient exposure to stressful situations not directly related to the disease entity under treatment. In this latter situation it may be necessary to increase the dosage of the corticosteroid for a period of time consistent with the patient's condition. If after long-term therapy the drug is to be stopped, it is recommended that it be withdrawn gradually rather than abruptly.
In the treatment of acute exacerbations of multiple sclerosis, daily doses of 30 mg of betamethasone for a week followed by 12 mg every other day for 1 month are recommended (see PRECAUTIONS, Neuro-psychiatric section).
In pediatric patients, the initial dose of betamethasone may vary depending on the specific disease entity being treated. The range of initial doses is 0.02 to 0.3 mg/kg/day in three or four divided doses (0.6 to 9 mg/m2bsa/day).
For the purpose of comparison, the following is the equivalent milligram dosage of the various glucocorticoids:
| Cortisone, 25 | Triamcinolone, 4 |
| Hydrocortisone, 20 | Paramethasone, 2 |
| Prednisolone, 5 | Betamethasone, 0.75 |
| Prednisone, 5 | Dexamethasone, 0.75 |
| Methylprednisolone, 4 |
These dose relationships apply only to oral or intravenous administration of these compounds. When these substances or their derivatives are injected intramuscularly or into joint spaces, their relative properties may be greatly altered.
If coadministration of a local anesthetic is desired, CELESTONE SOLUSPAN Injectable Suspension may be mixed with 1% or 2% lidocaine hydrochloride, using the formulations which do not contain parabens. Similar local anesthetics may also be used. Diluents containing methylparaben, propylparaben, phenol, etc., should be avoided, since these compounds may cause flocculation of the steroid. The required dose of CELESTONE SOLUSPAN Injectable Suspension is first withdrawn from the vial into the syringe. The local anesthetic is then drawn in, and the syringe shaken briefly. Do not inject local anesthetics into the vial of CELESTONE SOLUSPAN Injectable Suspension.
| CELESTONE SOLUSPAN
betamethasone acetate and betamethasone sodium phosphate injection, suspension |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Organon LLC (117494753) |