Drug Detail:Chantix (Varenicline [ ver-en-e-kleen ])
Drug Class: Smoking cessation agents
Highlights of Prescribing Information
CHANTIX® (varenicline) tablets, for oral use
Initial U.S. Approval: 2006
Recent Major Changes
| Warnings and Precautions, Cardiovascular Events (5.5) | 6/2018 |
Indications and Usage for Chantix
CHANTIX is a nicotinic receptor partial agonist indicated for use as an aid to smoking cessation treatment. (1 and 2.1)
Chantix Dosage and Administration
- Begin CHANTIX dosing one week before the date set by the patient to stop smoking. Alternatively, the patient can begin CHANTIX dosing and then quit smoking between days 8 and 35 of treatment. (2.1)
- Starting Week: 0.5 mg once daily on days 1–3 and 0.5 mg twice daily on days 4–7. (2.1)
- Continuing Weeks: 1 mg twice daily for a total of 12 weeks. (2.1)
- An additional 12 weeks of treatment is recommended for successful quitters to increase likelihood of long-term abstinence. (2.1)
- Consider a gradual approach to quitting smoking with CHANTIX for patients who are sure that they are not able or willing to quit abruptly. Patients should begin CHANTIX dosing and reduce smoking by 50% from baseline within the first four weeks, by an additional 50% in the next four weeks, and continue reducing with the goal of reaching complete abstinence by 12 weeks. Continue treatment for an additional 12 weeks, for a total of 24 weeks. (2.1)
- Severe Renal Impairment (estimated creatinine clearance less than 30 mL/min): Begin with 0.5 mg once daily and titrate to 0.5 mg twice daily. For patients with end-stage renal disease undergoing hemodialysis, a maximum of 0.5 mg daily may be given if tolerated. (2.2)
- Consider dose reduction for patients who cannot tolerate adverse effects. (2.1)
- Another attempt at treatment is recommended for those who fail to stop smoking or relapse when factors contributing to the failed attempt have been addressed. (2.1)
- Provide patients with appropriate educational materials and counseling to support the quit attempt. (2.1)
Dosage Forms and Strengths
Tablets: 0.5 mg and 1 mg (3)
Contraindications
History of serious hypersensitivity or skin reactions to CHANTIX. (4)
Warnings and Precautions
- Neuropsychiatric Adverse Events: Postmarketing reports of serious or clinically significant neuropsychiatric adverse events have included changes in mood (including depression and mania), psychosis, hallucinations, paranoia, delusions, homicidal ideation, aggression, hostility, agitation, anxiety, and panic, as well as suicidal ideation, suicide attempt, and completed suicide. Observe patients attempting to quit smoking with CHANTIX for the occurrence of such symptoms and instruct them to discontinue CHANTIX and contact a healthcare provider if they experience such adverse events. (5.1)
- Seizures: New or worsening seizures have been observed in patients taking CHANTIX. CHANTIX should be used cautiously in patients with a history of seizures or other factors that can lower the seizure threshold. (5.2)
- Interaction with Alcohol: Increased effects of alcohol have been reported. Instruct patients to reduce the amount of alcohol they consume until they know whether CHANTIX affects them. (5.3)
- Accidental Injury: Accidental injuries (e.g., traffic accidents) have been reported. Instruct patients to use caution driving or operating machinery until they know how CHANTIX may affect them. (5.4)
- Cardiovascular Events: Patients with underlying cardiovascular (CV) disease may be at increased risk of CV events; however, these concerns must be balanced with the health benefits of smoking cessation. Instruct patients to notify their healthcare providers of new or worsening CV symptoms and to seek immediate medical attention if they experience signs and symptoms of myocardial infarction (MI) or stroke. (5.5 and 6.1)
- Somnambulism: Cases of somnambulism have been reported in patients taking CHANTIX. Some cases described harmful behavior to self, others, or property. Instruct patients to discontinue CHANTIX and notify their healthcare provider if they experience somnambulism. (5.6 and 6.2)
- Angioedema and Hypersensitivity Reactions: Such reactions, including angioedema, infrequently life-threatening, have been reported. Instruct patients to discontinue CHANTIX and immediately seek medical care if symptoms occur. (5.7 and 6.2)
- Serious Skin Reactions: Rare, potentially life-threatening skin reactions have been reported. Instruct patients to discontinue CHANTIX and contact a healthcare provider immediately at first appearance of skin rash with mucosal lesions. (5.8 and 6.2)
- Nausea: Nausea is the most common adverse reaction (up to 30% incidence rate). Dose reduction may be helpful. (5.9)
Adverse Reactions/Side Effects
Most common adverse reactions (>5% and twice the rate seen in placebo-treated patients) were nausea, abnormal (e.g., vivid, unusual, or strange) dreams, constipation, flatulence, and vomiting. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Pfizer Inc. at 1-800-438-1985 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Other Smoking Cessation Therapies: Safety and efficacy in combination with other smoking cessation therapies has not been established. Coadministration of varenicline and transdermal nicotine resulted in a high rate of discontinuation due to adverse events. (7.1)
- Effect of Smoking Cessation on Other Drugs: Pharmacokinetics or pharmacodynamics of certain drugs (e.g., theophylline, warfarin, insulin) may be altered, necessitating dose adjustment. (7.2)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 2/2019
Full Prescribing Information
1. Indications and Usage for Chantix
CHANTIX is indicated for use as an aid to smoking cessation treatment.
2. Chantix Dosage and Administration
2.1 Usual Dosage for Adults
Smoking cessation therapies are more likely to succeed for patients who are motivated to stop smoking and who are provided additional advice and support. Provide patients with appropriate educational materials and counseling to support the quit attempt.
The patient should set a date to stop smoking. Begin CHANTIX dosing one week before this date. Alternatively, the patient can begin CHANTIX dosing and then quit smoking between days 8 and 35 of treatment.
CHANTIX should be taken orally after eating and with a full glass of water.
The recommended dose of CHANTIX is 1 mg twice daily following a 1-week titration as follows:
| Days 1 – 3: | 0.5 mg once daily |
| Days 4 – 7: | 0.5 mg twice daily |
| Day 8 – end of treatment: | 1 mg twice daily |
Patients should be treated with CHANTIX for 12 weeks. For patients who have successfully stopped smoking at the end of 12 weeks, an additional course of 12 weeks treatment with CHANTIX is recommended to further increase the likelihood of long-term abstinence.
For patients who are sure that they are not able or willing to quit abruptly, consider a gradual approach to quitting smoking with CHANTIX. Patients should begin CHANTIX dosing and reduce smoking by 50% from baseline within the first four weeks, by an additional 50% in the next four weeks, and continue reducing with the goal of reaching complete abstinence by 12 weeks. Continue CHANTIX treatment for an additional 12 weeks, for a total of 24 weeks of treatment. Encourage patients to attempt quitting sooner if they feel ready [see Clinical Studies (14.5)].
Patients who are motivated to quit, and who did not succeed in stopping smoking during prior CHANTIX therapy for reasons other than intolerability due to adverse events or who relapsed after treatment, should be encouraged to make another attempt with CHANTIX once factors contributing to the failed attempt have been identified and addressed.
Consider a temporary or permanent dose reduction in patients who cannot tolerate the adverse effects of CHANTIX.
3. Dosage Forms and Strengths
Capsular, biconvex tablets: 0.5 mg (white to off-white, debossed with "Pfizer" on one side and "CHX 0.5" on the other side) and 1 mg (light blue, debossed with "Pfizer" on one side and "CHX 1.0" on the other side).
4. Contraindications
CHANTIX is contraindicated in patients with a known history of serious hypersensitivity reactions or skin reactions to CHANTIX.
5. Warnings and Precautions
5.1 Neuropsychiatric Adverse Events including Suicidality
Serious neuropsychiatric adverse events have been reported in patients being treated with CHANTIX [see Adverse Reactions (6.2)]. These postmarketing reports have included changes in mood (including depression and mania), psychosis, hallucinations, paranoia, delusions, homicidal ideation, aggression, hostility, agitation, anxiety, and panic, as well as suicidal ideation, suicide attempt, and completed suicide. Some patients who stopped smoking may have been experiencing symptoms of nicotine withdrawal, including depressed mood. Depression, rarely including suicidal ideation, has been reported in smokers undergoing a smoking cessation attempt without medication. However, some of these adverse events occurred in patients taking CHANTIX who continued to smoke.
Neuropsychiatric adverse events occurred in patients without and with pre-existing psychiatric disease; some patients experienced worsening of their psychiatric illnesses. Some neuropsychiatric adverse events, including unusual and sometimes aggressive behavior directed to oneself or others, may have been worsened by concomitant use of alcohol [see Warnings and Precautions (5.3), Adverse Reactions (6.2)]. Observe patients for the occurrence of neuropsychiatric adverse events. Advise patients and caregivers that the patient should stop taking CHANTIX and contact a healthcare provider immediately if agitation, depressed mood, or changes in behavior or thinking that are not typical for the patient are observed, or if the patient develops suicidal ideation or suicidal behavior. The healthcare provider should evaluate the severity of the symptoms and the extent to which the patient is benefiting from treatment, and consider options including dose reduction, continued treatment under closer monitoring, or discontinuing treatment. In many postmarketing cases, resolution of symptoms after discontinuation of CHANTIX was reported. However, the symptoms persisted in some cases; therefore, ongoing monitoring and supportive care should be provided until symptoms resolve.
The neuropsychiatric safety of CHANTIX was evaluated in a randomized, double-blind, active and placebo-controlled study that included patients without a history of psychiatric disorder (non-psychiatric cohort, N=3912) and patients with a history of psychiatric disorder (psychiatric cohort, N=4003). In the non-psychiatric cohort, CHANTIX was not associated with an increased incidence of clinically significant neuropsychiatric adverse events in a composite endpoint comprising anxiety, depression, feeling abnormal, hostility, agitation, aggression, delusions, hallucinations, homicidal ideation, mania, panic, and irritability. In the psychiatric cohort, there were more events reported in each treatment group compared to the non-psychiatric cohort, and the incidence of events in the composite endpoint was higher for each of the active treatments compared to placebo: Risk Differences (RDs) (95%CI) vs. placebo were 2.7% (-0.05, 5.4) for CHANTIX, 2.2% (-0.5, 4.9) for bupropion, and 0.4% (-2.2, 3.0) for transdermal nicotine. In the non-psychiatric cohort, neuropsychiatric adverse events of a serious nature were reported in 0.1% of CHANTIX-treated patients and 0.4% of placebo-treated patients. In the psychiatric cohort, neuropsychiatric events of a serious nature were reported in 0.6% of CHANTIX-treated patients, with 0.5% involving psychiatric hospitalization. In placebo-treated patients, serious neuropsychiatric events occurred in 0.6%, with 0.2% requiring psychiatric hospitalization [see Clinical Studies (14.10)].
5.2 Seizures
During clinical trials and the postmarketing experience, there have been reports of seizures in patients treated with CHANTIX. Some patients had no history of seizures, whereas others had a history of seizure disorder that was remote or well-controlled. In most cases, the seizure occurred within the first month of therapy. Weigh this potential risk against the potential benefits before prescribing CHANTIX in patients with a history of seizures or other factors that can lower the seizure threshold. Advise patients to discontinue CHANTIX and contact a healthcare provider immediately if they experience a seizure while on treatment [see Adverse Reactions (6.2)].
5.3 Interaction with Alcohol
There have been postmarketing reports of patients experiencing increased intoxicating effects of alcohol while taking CHANTIX. Some cases described unusual and sometimes aggressive behavior, and were often accompanied by amnesia for the events. Advise patients to reduce the amount of alcohol they consume while taking CHANTIX until they know whether CHANTIX affects their tolerance for alcohol [see Adverse Reactions (6.2)].
5.4 Accidental Injury
There have been postmarketing reports of traffic accidents, near-miss incidents in traffic, or other accidental injuries in patients taking CHANTIX. In some cases, the patients reported somnolence, dizziness, loss of consciousness or difficulty concentrating that resulted in impairment, or concern about potential impairment, in driving or operating machinery. Advise patients to use caution driving or operating machinery or engaging in other potentially hazardous activities until they know how CHANTIX may affect them.
5.5 Cardiovascular Events
A comprehensive evaluation of cardiovascular (CV) risk with CHANTIX suggests that patients with underlying CV disease may be at increased risk; however, these concerns must be balanced with the health benefits of smoking cessation. CV risk has been assessed for CHANTIX in randomized controlled trials (RCT) and meta-analyses of RCTs. In a smoking cessation trial in patients with stable CV disease, CV events were infrequent overall; however, nonfatal myocardial infarction (MI) and nonfatal stroke occurred more frequently in patients treated with CHANTIX compared to placebo. All-cause and CV mortality was lower in patients treated with CHANTIX [see Clinical Studies (14.8)]. This study was included in a meta-analysis of 15 CHANTIX efficacy trials in various clinical populations that showed an increased hazard ratio for Major Adverse Cardiovascular Events (MACE) of 1.95; however, the finding was not statistically significant (95% CI: 0.79, 4.82). In the large postmarketing neuropsychiatric safety outcome trial, an analysis of adjudicated MACE events was conducted for patients while in the trial and during a 28-week non-treatment extension period. Few MACE events occurred during the trial; therefore, the findings did not contribute substantively to the understanding of CV risk with CHANTIX. Instruct patients to notify their healthcare providers of new or worsening CV symptoms and to seek immediate medical attention if they experience signs and symptoms of MI or stroke [see Clinical Studies (14.10)].
5.6 Somnambulism
Cases of somnambulism have been reported in patients taking CHANTIX. Some cases described harmful behavior to self, others, or property. Instruct patients to discontinue CHANTIX and notify their healthcare provider if they experience somnambulism [see Adverse Reactions (6.2)].
5.7 Angioedema and Hypersensitivity Reactions
There have been postmarketing reports of hypersensitivity reactions including angioedema in patients treated with CHANTIX [see Adverse Reactions (6.2), Patient Counseling Information (17)]. Clinical signs included swelling of the face, mouth (tongue, lips, and gums), extremities, and neck (throat and larynx). There were infrequent reports of life-threatening angioedema requiring emergent medical attention due to respiratory compromise. Instruct patients to discontinue CHANTIX and immediately seek medical care if they experience these symptoms.
5.8 Serious Skin Reactions
There have been postmarketing reports of rare but serious skin reactions, including Stevens-Johnson Syndrome and erythema multiforme, in patients using CHANTIX [see Adverse Reactions (6.2)]. As these skin reactions can be life-threatening, instruct patients to stop taking CHANTIX and contact a healthcare provider immediately at the first appearance of a skin rash with mucosal lesions or any other signs of hypersensitivity.
5.9 Nausea
Nausea was the most common adverse reaction reported with CHANTIX treatment. Nausea was generally described as mild or moderate and often transient; however, for some patients, it was persistent over several months. The incidence of nausea was dose-dependent. Initial dose-titration was beneficial in reducing the occurrence of nausea. For patients treated to the maximum recommended dose of 1 mg twice daily following initial dosage titration, the incidence of nausea was 30% compared with 10% in patients taking a comparable placebo regimen. In patients taking CHANTIX 0.5 mg twice daily following initial titration, the incidence was 16% compared with 11% for placebo. Approximately 3% of patients treated with CHANTIX 1 mg twice daily in studies involving 12 weeks of treatment discontinued treatment prematurely because of nausea. For patients with intolerable nausea, a dose reduction should be considered.
6. Adverse Reactions/Side Effects
The following serious adverse reactions were reported in postmarketing experience and are discussed in greater detail in other sections of the labeling:
- Neuropsychiatric Adverse Events including Suicidality [see Warnings and Precautions (5.1)]
- Seizures [see Warnings and Precautions (5.2)]
- Interaction with Alcohol [see Warnings and Precautions (5.3)]
- Accidental Injury [see Warnings and Precautions (5.4)]
- Cardiovascular Events [see Warnings and Precautions (5.5)]
- Somnambulism [see Warnings and Precautions (5.6)]
- Angioedema and Hypersensitivity Reactions [see Warnings and Precautions (5.7)]
- Serious Skin Reactions [see Warnings and Precautions (5.8)]
In the placebo-controlled premarketing studies, the most common adverse events associated with CHANTIX (>5% and twice the rate seen in placebo-treated patients) were nausea, abnormal (vivid, unusual, or strange) dreams, constipation, flatulence, and vomiting.
The treatment discontinuation rate due to adverse events in patients dosed with 1 mg twice daily was 12% for CHANTIX, compared to 10% for placebo in studies of three months' treatment. In this group, the discontinuation rates that are higher than placebo for the most common adverse events in CHANTIX-treated patients were as follows: nausea (3% vs. 0.5% for placebo), insomnia (1.2% vs. 1.1% for placebo), and abnormal dreams (0.3% vs. 0.2% for placebo).
Smoking cessation, with or without treatment, is associated with nicotine withdrawal symptoms and has also been associated with the exacerbation of underlying psychiatric illness.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, the adverse reactions rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
During the premarketing development of CHANTIX, over 4500 subjects were exposed to CHANTIX, with over 450 treated for at least 24 weeks and approximately 100 for a year. Most study participants were treated for 12 weeks or less.
The most common adverse event associated with CHANTIX treatment is nausea, occurring in 30% of patients treated at the recommended dose, compared with 10% in patients taking a comparable placebo regimen [see Warnings and Precautions (5.9)].
Table 1 shows the adverse events for CHANTIX and placebo in the 12- week fixed dose premarketing studies with titration in the first week [Studies 2 (titrated arm only), 4, and 5]. Adverse events were categorized using the Medical Dictionary for Regulatory Activities (MedDRA, Version 7.1).
MedDRA High Level Group Terms (HLGT) reported in ≥5% of patients in the CHANTIX 1 mg twice daily dose group, and more commonly than in the placebo group, are listed, along with subordinate Preferred Terms (PT) reported in ≥1% of CHANTIX patients (and at least 0.5% more frequent than placebo). Closely related Preferred Terms such as 'Insomnia', 'Initial insomnia', 'Middle insomnia', 'Early morning awakening' were grouped, but individual patients reporting two or more grouped events are only counted once.
| SYSTEM ORGAN CLASS High Level Group Term | CHANTIX 0.5 mg BID | CHANTIX 1 mg BID | Placebo |
|---|---|---|---|
| Preferred Term | N=129 | N=821 | N=805 |
|
|||
| GASTROINTESTINAL (GI) | |||
| GI Signs and Symptoms | |||
| Nausea | 16 | 30 | 10 |
| Abdominal Pain * | 5 | 7 | 5 |
| Flatulence | 9 | 6 | 3 |
| Dyspepsia | 5 | 5 | 3 |
| Vomiting | 1 | 5 | 2 |
| GI Motility/Defecation Conditions | |||
| Constipation | 5 | 8 | 3 |
| Gastroesophageal reflux disease | 1 | 1 | 0 |
| Salivary Gland Conditions | |||
| Dry mouth | 4 | 6 | 4 |
| PSYCHIATRIC DISORDERS | |||
| Sleep Disorder/Disturbances | |||
| Insomnia † | 19 | 18 | 13 |
| Abnormal dreams | 9 | 13 | 5 |
| Sleep disorder | 2 | 5 | 3 |
| Nightmare | 2 | 1 | 0 |
| NERVOUS SYSTEM | |||
| Headaches | |||
| Headache | 19 | 15 | 13 |
| Neurological Disorders NEC | |||
| Dysgeusia | 8 | 5 | 4 |
| Somnolence | 3 | 3 | 2 |
| Lethargy | 2 | 1 | 0 |
| GENERAL DISORDERS | |||
| General Disorders NEC | |||
| Fatigue/Malaise/Asthenia | 4 | 7 | 6 |
| RESPIR/THORACIC/MEDIAST | |||
| Respiratory Disorders NEC | |||
| Rhinorrhea | 0 | 1 | 0 |
| Dyspnea | 2 | 1 | 1 |
| Upper Respiratory Tract Disorder | 7 | 5 | 4 |
| SKIN/SUBCUTANEOUS TISSUE | |||
| Epidermal and Dermal Conditions | |||
| Rash | 1 | 3 | 2 |
| Pruritis | 0 | 1 | 1 |
| METABOLISM and NUTRITION | |||
| Appetite/General Nutrition Disorders | |||
| Increased appetite | 4 | 3 | 2 |
| Decreased appetite/Anorexia | 1 | 2 | 1 |
The overall pattern and frequency of adverse events during the longer-term premarketing trials was similar to those described in Table 1, though several of the most common events were reported by a greater proportion of patients with long-term use (e.g., nausea was reported in 40% of patients treated with CHANTIX 1 mg twice daily in a one year study, compared to 8% of placebo-treated patients).
Following is a list of treatment-emergent adverse events reported by patients treated with CHANTIX during all premarketing clinical trials and updated based on pooled data from 18 placebo-controlled pre- and postmarketing studies, including approximately 5,000 patients treated with varenicline. Adverse events were categorized using MedDRA, Version 16.0. The listing does not include those events already listed in the previous tables or elsewhere in labeling, those events for which a drug cause was remote, those events which were so general as to be uninformative, and those events reported only once which did not have a substantial probability of being acutely life-threatening.
Blood and Lymphatic System Disorders. Infrequent: anemia, lymphadenopathy. Rare: leukocytosis, splenomegaly, thrombocytopenia.
Cardiac Disorders. Infrequent: angina pectoris, myocardial infarction, palpitations, tachycardia. Rare: acute coronary syndrome, arrhythmia, atrial fibrillation, bradycardia, cardiac flutter, cor pulmonale, coronary artery disease, ventricular extrasystoles.
Ear and Labyrinth Disorders. Infrequent: tinnitus, vertigo. Rare: deafness, Meniere's disease.
Endocrine Disorders. Infrequent: thyroid gland disorders.
Eye Disorders. Infrequent: conjunctivitis, eye irritation, eye pain, vision blurred, visual impairment. Rare: blindness transient, cataract subcapsular, dry eye, night blindness, ocular vascular disorder, photophobia, vitreous floaters.
Gastrointestinal Disorders. Frequent: diarrhea, toothache. Infrequent: dysphagia, eructation, gastritis, gastrointestinal hemorrhage, mouth ulceration. Rare: enterocolitis, esophagitis, gastric ulcer, intestinal obstruction, pancreatitis acute.
General Disorders and Administration Site Conditions. Frequent: chest pain. Infrequent: chest discomfort, chills, edema, influenza-like illness, pyrexia.
Hepatobiliary Disorders. Rare: gall bladder disorder.
Investigations. Frequent: liver function test abnormal, weight increased. Infrequent: electrocardiogram abnormal. Rare: muscle enzyme increased, urine analysis abnormal.
Metabolism and Nutrition Disorders. Infrequent: diabetes mellitus, hypoglycemia. Rare: hyperlipidemia, hypokalemia.
Musculoskeletal and Connective Tissue Disorders. Frequent: arthralgia, back pain, myalgia. Infrequent: arthritis, muscle cramp, musculoskeletal pain. Rare: myositis, osteoporosis.
Nervous System Disorders. Frequent: disturbance in attention, dizziness. Infrequent: amnesia, convulsion, migraine, parosmia, syncope, tremor. Rare: balance disorder, cerebrovascular accident, dysarthria, mental impairment, multiple sclerosis, VIIth nerve paralysis, nystagmus, psychomotor hyperactivity, psychomotor skills impaired, restless legs syndrome, sensory disturbance, transient ischemic attack, visual field defect.
Psychiatric Disorders. Infrequent: dissociation, libido decreased, mood swings, thinking abnormal. Rare: bradyphrenia, disorientation, euphoric mood.
Renal and Urinary Disorders. Infrequent: nocturia, pollakiuria, urine abnormality. Rare: nephrolithiasis, polyuria, renal failure acute, urethral syndrome, urinary retention.
Reproductive System and Breast Disorders. Frequent: menstrual disorder. Infrequent: erectile dysfunction. Rare: sexual dysfunction.
Respiratory, Thoracic and Mediastinal Disorders. Frequent: respiratory disorders. Infrequent: asthma, epistaxis, rhinitis allergic, upper respiratory tract inflammation. Rare: pleurisy, pulmonary embolism.
Skin and Subcutaneous Tissue Disorders. Infrequent: acne, dry skin, eczema, erythema, hyperhidrosis, urticaria. Rare: photosensitivity reaction, psoriasis.
Vascular Disorders. Infrequent: hot flush. Rare: thrombosis.
CHANTIX has also been studied in postmarketing trials including (1) a trial conducted in patients with chronic obstructive pulmonary disease (COPD), (2) a trial conducted in generally healthy patients (similar to those in the premarketing studies) in which they were allowed to select a quit date between days 8 and 35 of treatment ("alternative quit date instruction trial"), (3) a trial conducted in patients who did not succeed in stopping smoking during prior CHANTIX therapy, or who relapsed after treatment ("re-treatment trial"), (4) a trial conducted in patients with stable cardiovascular disease, (5) a trial conducted in patients with stable schizophrenia or schizoaffective disorder, (6) a trial conducted in patients with major depressive disorder, (7) a postmarketing neuropsychiatric safety outcome trial in patients without or with a history of psychiatric disorder, (8) a non-treatment extension of the postmarketing neuropsychiatric safety outcome trial that assessed CV safety, (9) a trial in patients who were not able or willing to quit abruptly and who were instructed to quit gradually ("gradual approach to quitting smoking trial").
Adverse events in the trial of patients with COPD (1), in the alternative quit date instruction trial (2), and in the gradual approach to quitting smoking trial (9) were similar to those observed in premarketing studies. In the re-treatment trial (3), the profile of common adverse events was similar to that previously reported, but, in addition, varenicline-treated patients also commonly reported diarrhea (6% vs. 4% in placebo-treated patients), depressed mood disorders and disturbances (6% vs. 1%), and other mood disorders and disturbances (5% vs. 2%).
In the trial of patients with stable cardiovascular disease (4), more types and a greater number of cardiovascular events were reported compared to premarketing studies, as shown in Table 1 and in Table 2 below.
| CHANTIX 1 mg BID | Placebo | |
|---|---|---|
| N=353 | N=350 | |
|
||
| Adverse Events ≥1% in either treatment group | ||
| Up to 30 days after treatment | ||
| Angina pectoris | 3.7 | 2.0 |
| Chest pain | 2.5 | 2.3 |
| Peripheral edema | 2.0 | 1.1 |
| Hypertension | 1.4 | 2.6 |
| Palpitations | 0.6 | 1.1 |
| Adjudicated Cardiovascular Mortality (up to 52 weeks) | 0.3 | 0.6 |
| Adjudicated Nonfatal Serious Cardiovascular Events ≥1% in either treatment group | ||
| Up to 30 days after treatment | ||
| Nonfatal MI | 1.1 | 0.3 |
| Hospitalization for angina pectoris | 0.6 | 1.1 |
| Beyond 30 days after treatment and up to 52 weeks | ||
| Need for coronary revascularization* | 2.0 | 0.6 |
| Hospitalization for angina pectoris | 1.7 | 1.1 |
| New diagnosis of peripheral vascular disease (PVD) or admission for a PVD procedure | 1.4 | 0.6 |
In the trial of patients with stable schizophrenia or schizoaffective disorder (5), 128 smokers on antipsychotic medication were randomized 2:1 to varenicline (1 mg twice daily) or placebo for 12 weeks with 12-week non-drug follow-up. The most common treatment emergent adverse events reported in this trial are shown in Table 3 below.
| CHANTIX 1 mg BID | Placebo | |
|---|---|---|
| N=84 | N=43 | |
| Adverse Events ≥10% in the varenicline group | ||
| Nausea | 24 | 14 |
| Headache | 11 | 19 |
| Vomiting | 11 | 9 |
| Psychiatric Adverse Events ≥5% and at a higher rate than in the placebo group | ||
| Insomnia | 10 | 5 |
For the trial of patients with major depressive disorder (6), the most common treatment emergent adverse events reported are shown in Table 4 below. Additionally, in this trial, patients treated with varenicline were more likely than patients treated with placebo to report one of events related to hostility and aggression (3% vs. 1%).
| CHANTIX 1 mg BID | Placebo | |
|---|---|---|
| N=256 | N=269 | |
| Adverse Events ≥10% in either treatment group | ||
| Nausea | 27 | 10 |
| Headache | 17 | 11 |
| Abnormal dreams | 11 | 8 |
| Insomnia | 11 | 5 |
| Irritability | 11 | 8 |
| Psychiatric Adverse Events ≥2% in any treatment group and not included above | ||
| Depressed mood disorders and disturbances | 11 | 9 |
| Anxiety | 7 | 9 |
| Agitation | 7 | 4 |
| Tension | 4 | 3 |
| Hostility | 2 | 0.4 |
| Restlessness | 2 | 2 |
In the trial of patients without or with a history of psychiatric disorder (7), the most common adverse events in subjects treated with varenicline were similar to those observed in premarketing studies. Most common treatment-emergent adverse events reported in this trial are shown in Table 5 below.
| CHANTIX 1 mg BID | Placebo | |
|---|---|---|
| Adverse Events ≥10% in the varenicline group | ||
| Entire study population, N | 1982 | 1979 |
| Nausea | 25 | 7 |
| Headache | 12 | 10 |
| Psychiatric Adverse Events ≥2% in any treatment group | ||
| Non-psychiatric cohort, N | 975 | 982 |
| Abnormal dreams | 8 | 4 |
| Agitation | 3 | 3 |
| Anxiety | 5 | 6 |
| Depressed mood | 3 | 3 |
| Insomnia | 10 | 7 |
| Irritability | 3 | 4 |
| Sleep disorder | 3 | 2 |
| Psychiatric cohort, N | 1007 | 997 |
| Abnormal dreams | 12 | 5 |
| Agitation | 5 | 4 |
| Anxiety | 8 | 6 |
| Depressed mood | 5 | 5 |
| Depression | 5 | 5 |
| Insomnia | 9 | 7 |
| Irritability | 5 | 7 |
| Nervousness | 2 | 3 |
| Sleep disorder | 3 | 2 |
In the non-treatment extension of the postmarketing neuropsychiatric safety outcomes trial that assessed CV safety (8), the most common adverse events in subjects treated with varenicline and occurring up to 30 days after last dose of treatment were similar to those observed in premarketing studies.
6.2 Postmarketing Experience
The following adverse events have been reported during post-approval use of CHANTIX. Because these events are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
There have been reports of depression, mania, psychosis, hallucinations, paranoia, delusions, homicidal ideation, aggression, hostility, anxiety, and panic, as well as suicidal ideation, suicide attempt, and completed suicide in patients attempting to quit smoking while taking CHANTIX [see Warnings and Precautions (5.1)].
There have been postmarketing reports of new or worsening seizures in patients treated with CHANTIX [see Warnings and Precautions (5.2)].
There have been postmarketing reports of patients experiencing increased intoxicating effects of alcohol while taking CHANTIX. Some reported neuropsychiatric events, including unusual and sometimes aggressive behavior [see Warnings and Precautions (5.1) and (5.3)].
There have been reports of hypersensitivity reactions, including angioedema [see Warnings and Precautions (5.7)].
There have also been reports of serious skin reactions, including Stevens-Johnson Syndrome and erythema multiforme, in patients taking CHANTIX [see Warnings and Precautions (5.8)].
There have been reports of myocardial infarction (MI) and cerebrovascular accident (CVA) including ischemic and hemorrhagic events in patients taking CHANTIX. In the majority of the reported cases, patients had pre-existing cardiovascular disease and/or other risk factors. Although smoking is a risk factor for MI and CVA, based on temporal relationship between medication use and events, a contributory role of varenicline cannot be ruled out [see Warnings and Precautions (5.5)].
There have been reports of hyperglycemia in patients following initiation of CHANTIX.
There have been reports of somnambulism, some resulting in harmful behavior to self, others, or property in patients treated with CHANTIX [see Warnings and Precautions (5.6)].
7. Drug Interactions
Based on varenicline characteristics and clinical experience to date, CHANTIX has no clinically meaningful pharmacokinetic drug interactions [see Clinical Pharmacology (12.3)].
8. Use In Specific Populations
8.4 Pediatric Use
CHANTIX is not recommended for use in pediatric patients 16 years of age or younger because its efficacy in this population was not demonstrated.
Single and multiple-dose pharmacokinetics of varenicline have been investigated in pediatric patients aged 12 to 17 years old (inclusive) and were approximately dose-proportional over the 0.5 mg to 2 mg daily dose range studied. Steady-state systemic exposure in adolescent patients of bodyweight >55 kg, as assessed by AUC (0-24), was comparable to that noted for the same doses in the adult population. When 0.5 mg BID was given, steady-state daily exposure of varenicline was, on average, higher (by approximately 40%) in adolescent patients with bodyweight ≤55 kg compared to that noted in the adult population.
The efficacy and safety of varenicline was evaluated in a randomized, double-blind, placebo-controlled study of 312 patients aged 12 to 19 years, who smoked an average of at least 5 cigarettes per day during the 30 days prior to recruitment, had a score of at least 4 on the Fagerstrom Test for Nicotine Dependence scale, and at least one previous failed quit attempt. Patients were stratified by age (12 to 16 years of age, n=216 and 17 to 19 years of age, n=96) and by body weight (≤55 kg and >55 kg). Patients were randomized to one of two doses of varenicline, adjusted by weight to provide plasma levels in the efficacious range (based on adult studies) and placebo. Patients received treatment for 12 weeks, followed by a non-treatment period of 40 weeks, along with age-appropriate counseling throughout the study. Results from this study showed that varenicline, at either dose studied, did not improve continuous abstinence rates at weeks 9 through 12 of treatment compared with placebo in subjects 12 to 19 years of age. The varenicline safety profile in this study was consistent with that observed in adult studies.
8.5 Geriatric Use
A combined single- and multiple-dose pharmacokinetic study demonstrated that the pharmacokinetics of 1 mg varenicline given once daily or twice daily to 16 healthy elderly male and female smokers (aged 65–75 years) for 7 consecutive days was similar to that of younger subjects. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Varenicline is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function [see Dosage and Administration (2.2)].
No dosage adjustment is recommended for elderly patients.
8.6 Renal Impairment
Varenicline is substantially eliminated by renal glomerular filtration along with active tubular secretion. Dose reduction is not required in patients with mild to moderate renal impairment. For patients with severe renal impairment (estimated creatinine clearance <30 mL/min), and for patients with end-stage renal disease undergoing hemodialysis, dosage adjustment is needed [see Dosage and Administration (2.2), Clinical Pharmacology (12.3)].
10. Overdosage
In case of overdose, standard supportive measures should be instituted as required.
Varenicline has been shown to be dialyzed in patients with end-stage renal disease [see Clinical Pharmacology (12.3)], however, there is no experience in dialysis following overdose.
11. Chantix Description
CHANTIX tablets contain varenicline (as the tartrate salt), which is a partial nicotinic agonist selective for α4β2 nicotinic acetylcholine receptor subtypes.
Varenicline, as the tartrate salt, is a powder which is a white to off-white to slightly yellow solid with the following chemical name: 7,8,9,10-tetrahydro-6,10-methano-6H-pyrazino[2,3- h][3]benzazepine, (2R,3R)-2,3-dihydroxybutanedioate (1:1). It is highly soluble in water. Varenicline tartrate has a molecular weight of 361.35 Daltons, and a molecular formula of C13H13N3 ∙ C4H6O6. The chemical structure is:
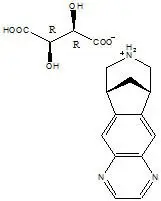
CHANTIX is supplied for oral administration in two strengths: a 0.5 mg capsular biconvex, white to off-white, film-coated tablet debossed with "Pfizer" on one side and "CHX 0.5" on the other side and a 1 mg capsular biconvex, light blue film-coated tablet debossed with "Pfizer" on one side and "CHX 1.0" on the other side. Each 0.5 mg CHANTIX tablet contains 0.85 mg of varenicline tartrate equivalent to 0.5 mg of varenicline free base; each 1 mg CHANTIX tablet contains 1.71 mg of varenicline tartrate equivalent to 1 mg of varenicline free base. The following inactive ingredients are included in the tablets: microcrystalline cellulose, anhydrous dibasic calcium phosphate, croscarmellose sodium, colloidal silicon dioxide, magnesium stearate, Opadry® White (for 0.5 mg), Opadry® Blue (for 1 mg), and Opadry® Clear.
12. Chantix - Clinical Pharmacology
12.1 Mechanism of Action
Varenicline binds with high affinity and selectivity at α4β2 neuronal nicotinic acetylcholine receptors. The efficacy of CHANTIX in smoking cessation is believed to be the result of varenicline's activity at α4β2 sub-type of the nicotinic receptor where its binding produces agonist activity, while simultaneously preventing nicotine binding to these receptors.
Electrophysiology studies in vitro and neurochemical studies in vivo have shown that varenicline binds to α4β2 neuronal nicotinic acetylcholine receptors and stimulates receptor-mediated activity, but at a significantly lower level than nicotine. Varenicline blocks the ability of nicotine to activate α4β2 receptors and thus to stimulate the central nervous mesolimbic dopamine system, believed to be the neuronal mechanism underlying reinforcement and reward experienced upon smoking. Varenicline is highly selective and binds more potently to α4β2 receptors than to other common nicotinic receptors (>500-fold α3β4, >3,500-fold α7, >20,000-fold α1βγδ), or to non-nicotinic receptors and transporters (>2,000-fold). Varenicline also binds with moderate affinity (Ki = 350 nM) to the 5-HT3 receptor.
12.3 Pharmacokinetics
Drug-Drug Interactions
In vitro studies demonstrated that varenicline does not inhibit the following cytochrome P450 enzymes (IC50 >6400 ng/mL): 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, and 3A4/5. Also, in human hepatocytes in vitro, varenicline does not induce the cytochrome P450 enzymes 1A2 and 3A4.
In vitro studies demonstrated that varenicline does not inhibit human renal transport proteins at therapeutic concentrations. Therefore, drugs that are cleared by renal secretion (e.g., metformin [see below]) are unlikely to be affected by varenicline.
In vitro studies demonstrated the active renal secretion of varenicline is mediated by the human organic cation transporter OCT2. Co-administration with inhibitors of OCT2 (e.g., cimeditine [see below]) may not necessitate a dose adjustment of CHANTIX as the increase in systemic exposure to CHANTIX is not expected to be clinically meaningful. Furthermore, since metabolism of varenicline represents less than 10% of its clearance, drugs known to affect the cytochrome P450 system are unlikely to alter the pharmacokinetics of CHANTIX [see Clinical Pharmacology (12.3)]; therefore, a dose adjustment of CHANTIX would not be required.
Drug interaction studies were performed with varenicline and digoxin, warfarin, transdermal nicotine, bupropion, cimetidine, and metformin. No clinically meaningful pharmacokinetic drug-drug interactions have been identified.
Metformin
When co-administered to 30 smokers, varenicline (1 mg twice daily) did not alter the steady-state pharmacokinetics of metformin (500 mg twice daily), which is a substrate of OCT2. Metformin had no effect on varenicline steady-state pharmacokinetics.
Cimetidine
Co-administration of an OCT2 inhibitor, cimetidine (300 mg four times daily), with varenicline (2 mg single dose) to 12 smokers increased the systemic exposure of varenicline by 29% (90% CI: 21.5%, 36.9%) due to a reduction in varenicline renal clearance.
14. Clinical Studies
The efficacy of CHANTIX in smoking cessation was demonstrated in six clinical trials in which a total of 3659 chronic cigarette smokers (≥10 cigarettes per day) were treated with CHANTIX. In all clinical studies, abstinence from smoking was determined by patient self-report and verified by measurement of exhaled carbon monoxide (CO≤10 ppm) at weekly visits. Among the CHANTIX-treated patients enrolled in these studies, the completion rate was 65%. Except for the dose-ranging study (Study 1) and the maintenance of abstinence study (Study 6), patients were treated for 12 weeks and then were followed for 40 weeks post-treatment. Most patients enrolled in these trials were white (79–96%). All studies enrolled almost equal numbers of men and women. The average age of patients in these studies was 43 years. Patients on average had smoked about 21 cigarettes per day for an average of approximately 25 years. Patients set a date to stop smoking (target quit date) with dosing starting 1 week before this date.
Seven additional studies evaluated the efficacy of CHANTIX in patients with cardiovascular disease, in patients with chronic obstructive pulmonary disease [see Clinical Studies (14.7)], in patients instructed to select their quit date within days 8 and 35 of treatment [see Clinical Studies (14.4)], patients with major depressive disorder [see Clinical Studies (14.9)], patients who had made a previous attempt to quit smoking with CHANTIX, and either did not succeed in quitting or relapsed after treatment [see Clinical Studies (14.6)], in patients without or with a history of psychiatric disorder enrolled in a postmarketing neuropsychiatric safety outcome trial [see Warnings and Precautions (5.1), Clinical Studies (14.10)], and in patients who were not able or willing to quit abruptly and were instructed to quit gradually [see Clinical studies (14.5)].
In all studies, patients were provided with an educational booklet on smoking cessation and received up to 10 minutes of smoking cessation counseling at each weekly treatment visit according to Agency for Healthcare Research and Quality guidelines.
14.2 Urge to Smoke
Based on responses to the Brief Questionnaire of Smoking Urges and the Minnesota Nicotine Withdrawal scale "urge to smoke" item, CHANTIX reduced urge to smoke compared to placebo.
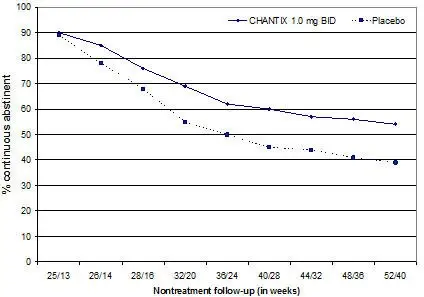
14.3 Long-Term Abstinence
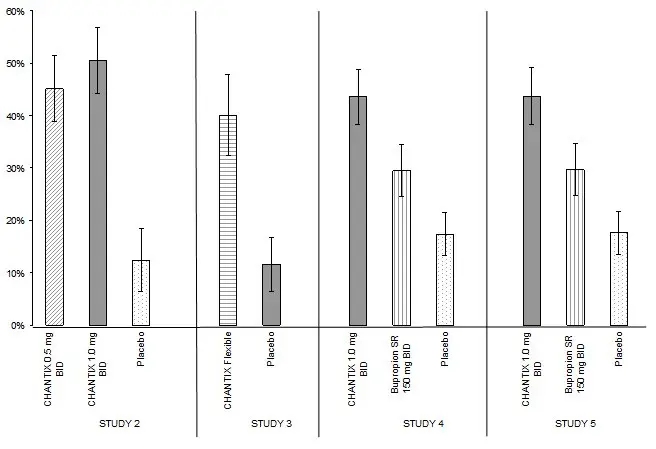
Studies 1 through 5 included 40 weeks of post-treatment follow-up. In each study, CHANTIX-treated patients were more likely to maintain abstinence throughout the follow-up period than were patients treated with placebo (Figure 2, Table 8).
| Figure 2: Continuous Abstinence, Weeks 9 through 52 |
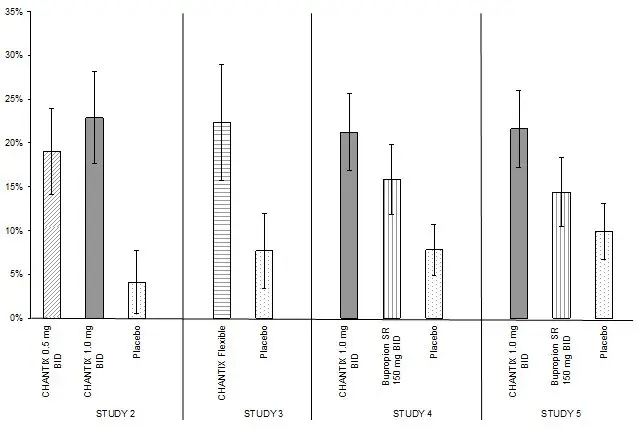 |
| CHANTIX 0.5 mg BID | CHANTIX 1 mg BID | CHANTIX Flexible | Bupropion SR | Placebo | |
|---|---|---|---|---|---|
| BID = twice daily | |||||
| Study 2 | 19% (14%, 24%) | 23% (18%, 28%) | 4% (1%, 8%) |
||
| Study 3 | 22% (16%, 29%) | 8% (3%, 12%) |
|||
| Study 4 | 21% (17%, 26%) | 16% (12%, 20%) | 8% (5%, 11%) |
||
| Study 5 | 22% (17%, 26%) | 14% (11%, 18%) | 10% (7%, 13%) |
||
14.4 Alternative Instructions for Setting a Quit Date
CHANTIX was evaluated in a double-blind, placebo-controlled trial where patients were instructed to select a target quit date between Day 8 and Day 35 of treatment. Subjects were randomized 3:1 to CHANTIX 1 mg twice daily (N=486) or placebo (N=165) for 12 weeks of treatment and followed for another 12 weeks post-treatment. Patients treated with CHANTIX had a superior rate of CO-confirmed abstinence during weeks 9 through 12 (54%) compared to patients treated with placebo (19%) and from weeks 9 through 24 (35%) compared to subjects treated with placebo (13%).
14.5 Gradual Approach to Quitting Smoking
CHANTIX was evaluated in a 52-week double-blind placebo-controlled study of 1,510 subjects who were not able or willing to quit smoking within four weeks, but were willing to gradually reduce their smoking over a 12 week period before quitting. Subjects were randomized to either CHANTIX 1 mg twice daily (N=760) or placebo (N=750) for 24 weeks and followed up post-treatment through week 52. Subjects were instructed to reduce the number of cigarettes smoked by at least 50 percent by the end of the first four weeks of treatment, followed by a further 50 percent reduction from week four to week eight of treatment, with the goal of reaching complete abstinence by 12 weeks. After the initial 12-week reduction phase, subjects continued treatment for another 12 weeks. Subjects treated with CHANTIX had a significantly higher Continuous Abstinence Rate compared with placebo at weeks 15 through 24 (32% vs. 7%) and weeks 15 through 52 (24% vs. 6%).
14.6 Re-Treatment Study
CHANTIX was evaluated in a double-blind, placebo-controlled trial of patients who had made a previous attempt to quit smoking with CHANTIX, and either did not succeed in quitting or relapsed after treatment. Subjects were randomized 1:1 to CHANTIX 1 mg twice daily (N=249) or placebo (N=245) for 12 weeks of treatment and followed for 40 weeks post-treatment. Patients included in this study had taken CHANTIX for a smoking-cessation attempt in the past (for a total treatment duration of a minimum of two weeks), at least three months prior to study entry, and had been smoking for at least four weeks.
Patients treated with CHANTIX had a superior rate of CO-confirmed abstinence during weeks 9 through 12 (45%) compared to patients treated with placebo (12%) and from weeks 9 through 52 (20%) compared to subjects treated with placebo (3%).
| Weeks 9 through 12 | Weeks 9 through 52 | |||
|---|---|---|---|---|
| CHANTIX 1 mg BID | Placebo | CHANTIX 1 mg BID | Placebo | |
| BID = twice daily | ||||
| Retreatment Study | 45% (39%, 51%) | 12% (8%, 16%) | 20% (15%, 25%) | 3% (1%, 5%) |
14.7 Subjects with Chronic Obstructive Pulmonary Disease
CHANTIX was evaluated in a randomized, double-blind, placebo-controlled study of subjects aged ≥ 35 years with mild-to-moderate COPD with post-bronchodilator FEV1/FVC <70% and FEV1 ≥ 50% of predicted normal value. Subjects were randomized to CHANTIX 1 mg twice daily (N=223) or placebo (N=237) for a treatment of 12 weeks and then were followed for 40 weeks post-treatment. Subjects treated with CHANTIX had a superior rate of CO-confirmed abstinence during weeks 9 through 12 (41%) compared to subjects treated with placebo (9%) and from week 9 through 52 (19%) compared to subjects treated with placebo (6%).
| Weeks 9 through 12 | Weeks 9 through 52 | |||
|---|---|---|---|---|
| CHANTIX 1 mg BID | Placebo | CHANTIX 1 mg BID | Placebo | |
| BID = twice daily | ||||
| COPD Study | 41% (34%, 47%) | 9% (6%, 13%) | 19% (14%, 24%) | 6% (3%, 9%) |
14.8 Subjects with Cardiovascular Disease and Other Cardiovascular Analyses
CHANTIX was evaluated in a randomized, double-blind, placebo-controlled study of subjects aged 35 to 75 years with stable, documented cardiovascular disease (diagnoses other than, or in addition to, hypertension) that had been diagnosed for more than 2 months. Subjects were randomized to CHANTIX 1 mg twice daily (N=353) or placebo (N=350) for a treatment period of 12 weeks and then were followed for 40 weeks post-treatment. Subjects treated with CHANTIX had a superior rate of CO-confirmed abstinence during weeks 9 through 12 (47%) compared to subjects treated with placebo (14%) and from week 9 through 52 (20%) compared to subjects treated with placebo (7%).
| Weeks 9 through 12 | Weeks 9 through 52 | |||
|---|---|---|---|---|
| CHANTIX 1 mg BID | Placebo | CHANTIX 1 mg BID | Placebo | |
| BID = twice daily | ||||
| CVD Study | 47% (42%, 53%) | 14% (11%, 18%) | 20% (16%, 24%) | 7% (5%, 10%) |
In this study, all-cause and CV mortality was lower in patients treated with CHANTIX, but certain nonfatal CV events occurred more frequently in patients treated with CHANTIX than in patients treated with placebo [see Warnings and Precautions (5.5), Adverse Reactions (6.1)]. Table 12 below shows mortality and the incidence of selected nonfatal serious CV events occurring more frequently in the CHANTIX arm compared to the placebo arm. These events were adjudicated by an independent blinded committee. Nonfatal serious CV events not listed occurred at the same incidence or more commonly in the placebo arm. Patients with more than one CV event of the same type are counted only once per row. Some of the patients requiring coronary revascularization underwent the procedure as part of management of nonfatal MI and hospitalization for angina.
| Mortality and Cardiovascular Events | CHANTIX (N=353) n (%) | Placebo (N=350) n (%) |
|---|---|---|
| Mortality (Cardiovascular and All-cause up to 52 weeks) | ||
| Cardiovascular | 1 (0.3) | 2 (0.6) |
| All-cause | 2 (0.6) | 5 (1.4) |
| Nonfatal Cardiovascular Events (rate on CHANTIX > Placebo) | ||
| Up to 30 days after treatment | ||
| Nonfatal myocardial infarction | 4 (1.1) | 1 (0.3) |
| Nonfatal Stroke | 2 (0.6) | 0 (0) |
| Beyond 30 days after treatment and up to 52 weeks | ||
| Nonfatal myocardial infarction | 3 (0.8) | 2 (0.6) |
| Need for coronary revascularization | 7 (2.0) | 2 (0.6) |
| Hospitalization for angina pectoris | 6 (1.7) | 4 (1.1) |
| Transient ischemia attack | 1 (0.3) | 0 (0) |
| New diagnosis of peripheral vascular disease (PVD) or admission for a PVD procedure | 5 (1.4) | 2 (0.6) |
Following the CVD study, a meta-analysis of 15 clinical trials of ≥12 weeks treatment duration, including 7002 patients (4190 CHANTIX, 2812 placebo), was conducted to systematically assess the CV safety of CHANTIX. The study in patients with stable CV disease described above was included in the meta-analysis. There were lower rates of all-cause mortality (CHANTIX 6 [0.14%]; placebo 7 [0.25%]) and CV mortality (CHANTIX 2 [0.05%]; placebo 2 [0.07%]) in the CHANTIX arms compared with the placebo arms in the meta-analysis.
The key CV safety analysis included occurrence and timing of a composite endpoint of Major Adverse Cardiovascular Events (MACE), defined as CV death, nonfatal MI, and nonfatal stroke. These events included in the endpoint were adjudicated by a blinded, independent committee. Overall, a small number of MACE occurred in the trials included in the meta-analysis, as described in Table 13. These events occurred primarily in patients with known CV disease.
| CHANTIX N=4190 | Placebo N=2812 |
|
|---|---|---|
|
||
| MACE cases, n (%) | 13 (0.31%) | 6 (0.21%) |
| Patient-years of exposure | 1316 | 839 |
| Hazard Ratio (95% CI) | ||
| 1.95 (0.79, 4.82) | ||
| Rate Difference per 1,000 patient-years (95% CI) | ||
| 6.30 (-2.40, 15.10) | ||
The meta-analysis showed that exposure to CHANTIX resulted in a hazard ratio for MACE of 1.95 (95% confidence interval from 0.79 to 4.82) for patients up to 30 days after treatment; this is equivalent to an estimated increase of 6.3 MACE events per 1,000 patient-years of exposure. The meta-analysis showed higher rates of CV endpoints in patients on CHANTIX relative to placebo across different time frames and pre-specified sensitivity analyses, including various study groupings and CV outcomes. Although these findings were not statistically significant they were consistent. Because the number of events was small overall, the power for finding a statistically significant difference in a signal of this magnitude is low.
Additionally, a cardiovascular endpoint analysis was added to the postmarketing neuropsychiatric safety outcome study along with a non-treatment extension, [see Warnings and Precautions (5.5), Adverse Reactions (6.1), Clinical Studies (14.10)].
14.9 Subjects with Major Depressive Disorder
CHANTIX was evaluated in a randomized, double-blind, placebo-controlled study of subjects aged 18 to 75 years with major depressive disorder without psychotic features (DSM-IV TR). If on medication, subjects were to be on a stable antidepressant regimen for at least two months. If not on medication, subjects were to have experienced a major depressive episode in the past 2 years, which was successfully treated. Subjects were randomized to CHANTIX 1 mg twice daily (N=256) or placebo (N=269) for a treatment of 12 weeks and then followed for 40 weeks post-treatment. Subjects treated with CHANTIX had a superior rate of CO-confirmed abstinence during weeks 9 through 12 (36%) compared to subjects treated with placebo (16%) and from week 9 through 52 (20%) compared to subjects treated with placebo (10%).
| Weeks 9 through 12 | Weeks 9 through 52 | |||
|---|---|---|---|---|
| CHANTIX 1 mg BID | Placebo | CHANTIX 1 mg BID | Placebo | |
| BID = twice daily | ||||
| MDD Study | 36% (30%, 42%) | 16% (11%, 20%) | 20% (15%, 25%) | 10% (7%, 14%) |
14.10 Postmarketing Neuropsychiatric Safety Outcome Trial
CHANTIX was evaluated in a randomized, double-blind, active and placebo-controlled trial that included subjects without a history of psychiatric disorder (non-psychiatric cohort, N=3912) and with a history of psychiatric disorder (psychiatric cohort, N=4003). Subjects aged 18–75 years, smoking 10 or more cigarettes per day were randomized 1:1:1:1 to CHANTIX 1 mg BID, bupropion SR 150 mg BID, NRT patch 21 mg/day with taper or placebo for a treatment period of 12 weeks; they were then followed for another 12 weeks post-treatment. [See Warnings and Precautions (5.1)]
A composite safety endpoint intended to capture clinically significant neuropsychiatric (NPS) adverse events included the following NPS adverse events: anxiety, depression, feeling abnormal, hostility, agitation, aggression, delusions, hallucinations, homicidal ideation, mania, panic, paranoia, psychosis, irritability, suicidal ideation, suicidal behavior or completed suicide.
As shown in Table 15, the use of CHANTIX, bupropion, and NRT in the non-psychiatric cohort was not associated with an increased risk of clinically significant NPS adverse events compared with placebo. Similarly, in the non-psychiatric cohort, the use of CHANTIX was not associated with an increased risk of clinically significant NPS adverse events in the composite safety endpoint compared with bupropion or NRT.
| CHANTIX (N=975) n (%) | Bupropion (N=968) n (%) | NRT (N=987) n (%) | Placebo (N=982) n (%) |
|
|---|---|---|---|---|
| Clinically Significant NPS | 30 (3.1) | 34 (3.5) | 33 (3.3) | 40 (4.1) |
| Serious NPS | 1 (0.1) | 5 (0.5) | 1 (0.1) | 4 (0.4) |
| Psychiatric Hospitalizations | 1 (0.1) | 2 (0.2) | 0 (0.0) | 1 (0.1) |
As shown in Table 16, there were more clinically significant NPS adverse events reported in patients in the psychiatric cohort in each treatment group compared with the non-psychiatric cohort. The incidence of events in the composite endpoint was higher for each of the active treatments compared to placebo: Risk Differences (RDs) (95%CI) vs placebo were 2.7% (-0.05, 5.4) for CHANTIX, 2.2% (-0.5, 4.9) for bupropion, and 0.4% (-2.2, 3.0) for NRT transdermal nicotine.
| CHANTIX (N=1007) n (%) | Bupropion (N=1004) n (%) | NRT (N=995) n (%) | Placebo (N=997) n (%) |
|
|---|---|---|---|---|
| Clinically Significant NPS | 123 (12.2) | 118 (11.8) | 98 (9.8) | 95 (9.5) |
| Serious NPS | 6 (0.6) | 8 (0.8) | 4 (0.4) | 6 (0.6) |
| Psychiatric hospitalizations | 5 (0.5) | 8 (0.8) | 4 (0.4) | 2 (0.2) |
There was one completed suicide, which occurred during treatment in a patient treated with placebo in the non-psychiatric cohort. There were no completed suicides reported in the psychiatric cohort.
In both cohorts, subjects treated with CHANTIX had a superior rate of CO-confirmed abstinence during weeks 9 through 12 and 9 through 24 compared to subjects treated with bupropion, nicotine patch and placebo.
| CHANTIX 1 mg BID | Bupropion SR 150 mg BID | NRT 21 mg/day with taper | Placebo | |
|---|---|---|---|---|
| BID = twice daily | ||||
| Weeks 9 through 12 | ||||
| Non-Psychiatric Cohort | 38% (35%, 41%) | 26% (23%, 29%) | 26% (24%, 29%) | 14% (12%, 16%) |
| Psychiatric Cohort | 29% (26%, 32%) | 19% (17%, 22%) | 20% (18%, 23%) | 11% (10%, 14%) |
| Weeks 9 through 24 | ||||
| Non-Psychiatric Cohort | 25% (23%, 28%) | 19% (16%, 21%) | 18% (16%, 21%) | 11% (9%, 13%) |
| Psychiatric Cohort | 18% (16%, 21%) | 14% (12%, 16%) | 13% (11%, 15%) | 8% (7%, 10%) |
16. How is Chantix supplied
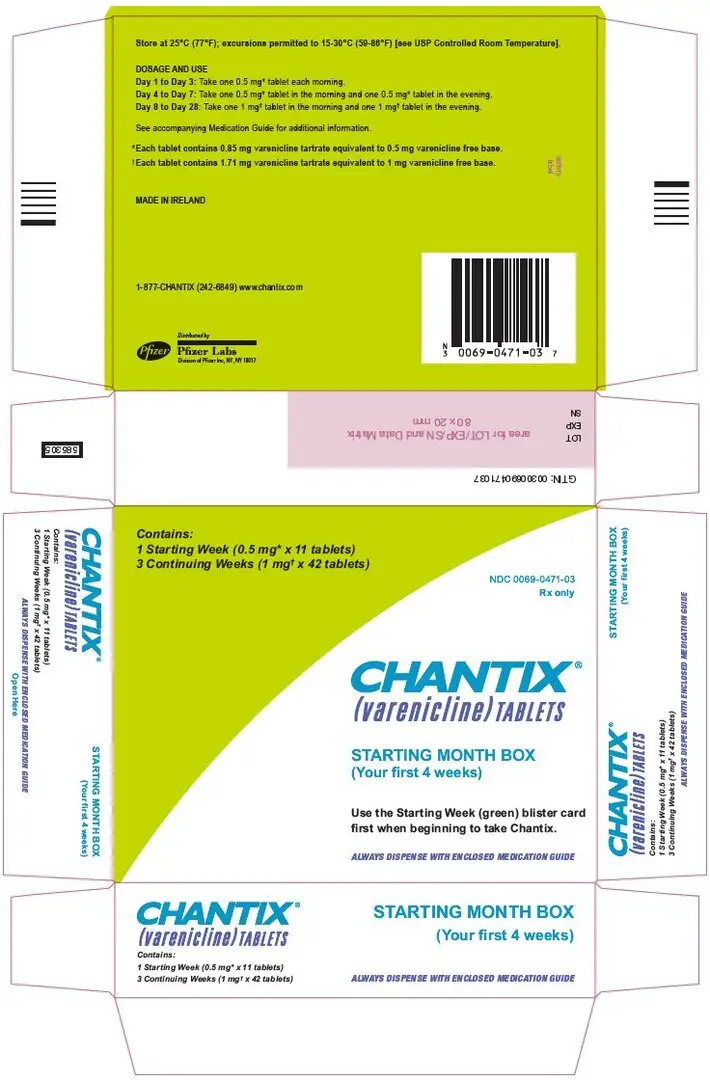
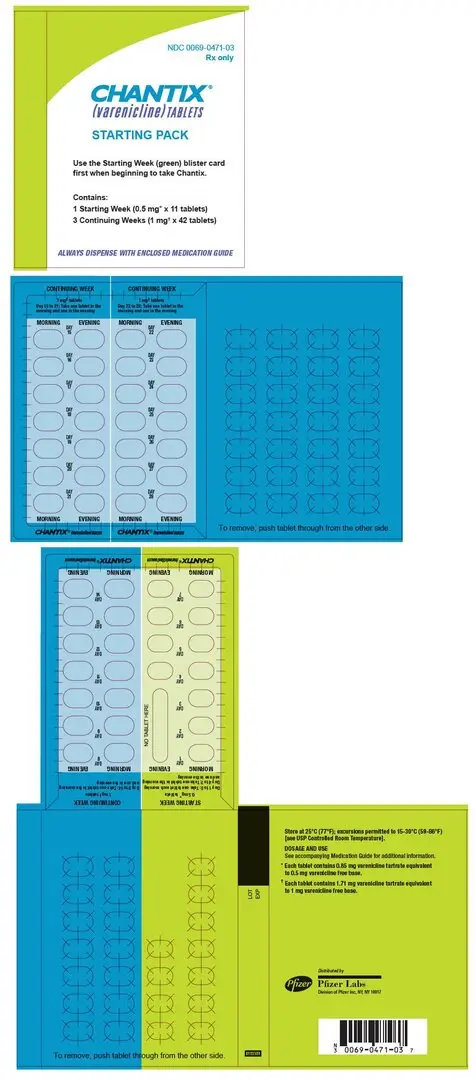
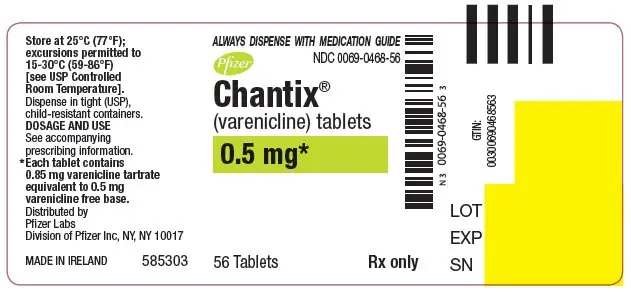
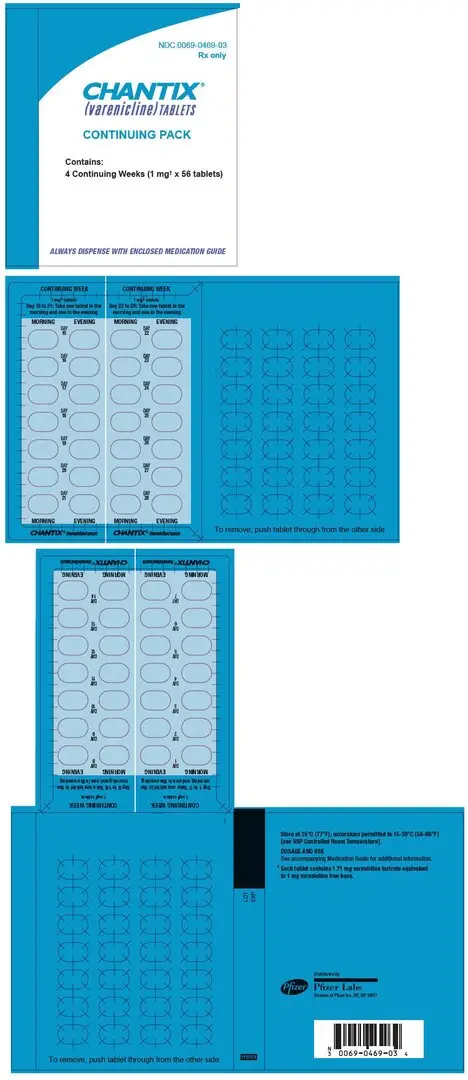
CHANTIX is supplied for oral administration in two strengths: a 0.5 mg capsular biconvex, white to off-white, film-coated tablet debossed with "Pfizer" on one side and "CHX 0.5" on the other side and a 1 mg capsular biconvex, light blue film-coated tablet debossed with "Pfizer" on one side and "CHX 1.0" on the other side. CHANTIX is supplied in the following package configurations:
| Description | NDC | |
|---|---|---|
| Packs | Starting 4-week card: 0.5 mg × 11 tablets and 1 mg × 42 tablets | NDC 0069-0471-03 |
| Continuing 4-week card: 1 mg × 56 tablets | NDC 0069-0469-03 | |
| Starting Month Box: 0.5 mg × 11 tablets and 1 mg × 42 tablets | NDC 0069-0471-03 | |
| Continuing Month Box: 1 mg × 56 tablets | NDC 0069-0469-03 | |
| Bottles | 0.5 mg - bottle of 56 | NDC 0069-0468-56 |
| 1 mg - bottle of 56 | NDC 0069-0469-56 |
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised Feb 2019 | |||||
|
MEDICATION GUIDE |
||||||
|
What is the most important information I should know about CHANTIX? When you try to quit smoking, with or without CHANTIX, you may have symptoms that may be due to nicotine withdrawal, including: |
||||||
|
|
|
||||
|
Some people have even experienced suicidal thoughts when trying to quit smoking without medication. Sometimes quitting smoking can lead to worsening of mental health problems that you already have, such as depression. Some people have had serious side effects while taking CHANTIX to help them quit smoking, including: New or worse mental health problems, such as changes in behavior or thinking, aggression, hostility, agitation, depressed mood, or suicidal thoughts or actions. Some people had these symptoms when they began taking CHANTIX, and others developed them after several weeks of treatment, or after stopping CHANTIX. These symptoms happened more often in people who had a history of mental health problems before taking CHANTIX, than in people without a history of mental health problems. Stop taking CHANTIX and call your healthcare provider right away if you, your family, or caregiver notice any of these symptoms. Work with your healthcare provider to decide whether you should continue to take CHANTIX. In many people, these symptoms went away after stopping CHANTIX, but in some people symptoms continued after stopping CHANTIX. It is important for you to follow-up with your healthcare provider until your symptoms go away. Before taking CHANTIX, tell your healthcare provider if you have ever had depression or other mental health problems. You should also tell your healthcare provider about any symptoms you had during other times you tried to quit smoking, with or without CHANTIX. |
||||||
|
What is CHANTIX? CHANTIX is a prescription medicine to help people stop smoking. Quitting smoking can lower your chances of having lung disease, heart disease or getting certain types of cancer that are related to smoking. CHANTIX has not been shown to be effective in children 16 years of age and under. CHANTIX should not be used in children 16 years of age and under. It is not known if CHANTIX is safe and effective when used with other stop smoking medicines. |
||||||
|
Who should not take CHANTIX? Do not take CHANTIX if you have had a serious allergic or skin reaction to CHANTIX. Symptoms may include:
|
||||||
|
|
|
||||
|
What should I tell my healthcare provider before taking CHANTIX? See "What is the most important information I should know about CHANTIX?" Before you take CHANTIX, tell your healthcare provider if you:
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins and herbal supplements. Your healthcare provider may need to change the dose of some of your medicines when you stop smoking. You should not use CHANTIX while using other medicines to quit smoking. Tell your healthcare provider if you use other treatments to quit smoking. Know the medicines you take. Keep a list of them with you to show your healthcare provider and pharmacist when you get a new medicine. |
||||||
|
How should I take CHANTIX?
|
||||||
|
Weeks 1 through 4 |
Reduce your smoking to reach one-half of your starting daily number of cigarettes. Example: If you usually smoke 20 cigarettes each day, reduce your smoking to 10 cigarettes each day during weeks 1 through 4. | |||||
|
Weeks 5 through 8 |
Reduce your smoking to reach one-quarter of your starting daily number of cigarettes. Example: If you usually smoked 20 cigarettes each day, reduce your smoking to 5 cigarettes each day during weeks 5 through 8. | |||||
|
Weeks 9 through 12 |
Keep reducing your smoking until you are no longer smoking (you reach zero cigarettes each day). | |||||
|
||||||
|
||||||
|
Day 1 to Day 3 |
| |||||
|
Day 4 to Day 7 |
| |||||
|
Day 8 to end of treatment |
| |||||
|
||||||
|
What should I avoid while taking CHANTIX?
|
||||||
|
|
|||||
|
What are the possible side effects of CHANTIX? Serious side effects of CHANTIX may include:
Stop taking CHANTIX and get medical help right away if you have any of the following symptoms:
The most common side effects of CHANTIX include:
Tell your healthcare provider about side effects that bother you or that do not go away. These are not all the side effects of CHANTIX. Ask your healthcare provider or pharmacist for more information. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||||||
|
How should I store CHANTIX?
|
||||||
|
General information about the safe and effective use of CHANTIX Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use CHANTIX for a condition for which it was not prescribed. Do not give your CHANTIX to other people, even if they have the same symptoms that you have. It may harm them. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about CHANTIX that is written for healthcare professionals. For more information about CHANTIX and tips on how to quit smoking, go to www.CHANTIX.com or call 1-877-242-6849. If you are motivated to quit smoking and did not succeed during prior CHANTIX treatment for reasons other than side effects, or if you returned to smoking after treatment, speak with your healthcare provider about whether another course of CHANTIX therapy may be right for you. |
||||||
|
What are the ingredients in CHANTIX? Active ingredient: varenicline tartrate Inactive ingredients: microcrystalline cellulose, anhydrous dibasic calcium phosphate, croscarmellose sodium, colloidal silicon dioxide, magnesium stearate, Opadry® White (for 0.5 mg), Opadry® Blue (for 1 mg), and Opadry® Clear.
LAB-0328-17.0 |
||||||
| CHANTIX
varenicline tartrate tablet, film coated |
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| CHANTIX
varenicline tartrate tablet, film coated |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| CHANTIX
varenicline tartrate kit |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Labeler - Pfizer Labs, Division of Pfizer Inc. (134489525) |
| Registrant - Pfizer Inc (113480771) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pfizer Ireland Pharmaceuticals | 985052076 | ANALYSIS(0069-0468, 0069-0469, 0069-0471) , API MANUFACTURE(0069-0468, 0069-0469, 0069-0471) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pfizer Pharmaceuticals LLC | 829084545 | API MANUFACTURE(0069-0468, 0069-0469, 0069-0471) , MANUFACTURE(0069-0468, 0069-0469, 0069-0471) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pfizer Italia S.r.l. | 458521908 | ANALYSIS(0069-0468, 0069-0469, 0069-0471) , MANUFACTURE(0069-0468, 0069-0469, 0069-0471) , PACK(0069-0468, 0069-0469, 0069-0471) , LABEL(0069-0468, 0069-0469, 0069-0471) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pfizer Manufacturing Deutschland GmbH | 341970073 | PACK(0069-0468, 0069-0469, 0069-0471) , LABEL(0069-0468, 0069-0469, 0069-0471) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Upjohn Manufacturing Ireland Unlimited Company | 986030667 | ANALYSIS(0069-0468, 0069-0469, 0069-0471) , API MANUFACTURE(0069-0468, 0069-0469, 0069-0471) | |