Drug Detail:Codar ar (Chlorpheniramine and codeine [ klor-fen-ir-a-meed-and-koe-deen ])
Drug Class: Upper respiratory combinations
Highlights of Prescribing Information
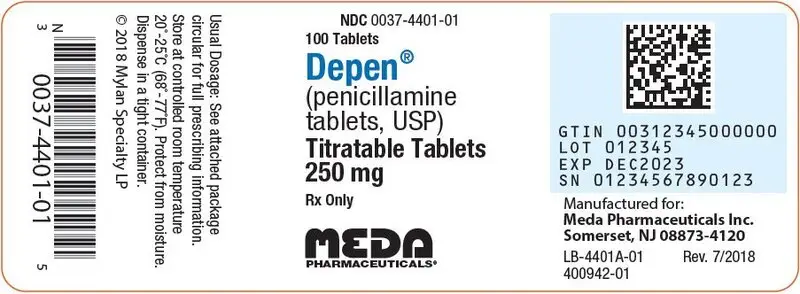
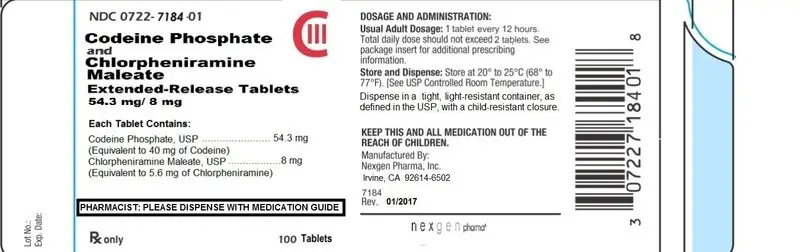
CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE (codeine phosphate and chlorpheniramine maleate) extended release tablets, CIII
Initial U.S. Approval: 1985
WARNING
DEATH RELATED TO ULTRA-RAPID METABOLISM OF CODEINE TO MORPHINE and
RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
Ultra-Rapid Metabolism
Respiratory depression and death have occurred in children who received codeine following tonsillectomy and/or adenoidectomy and had evidence of being ultra-rapid metabolizers of codeine due to a CYP2D6 polymorphism. (5.1)
Concomitant Use with Benzodiazepines, CNS Depressants
Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death [see Warning and Precautions (5.2) Drug Interactions (7.1). Avoid use of opioid cough medications in patients taking benzodiazepines, other CNS depressants, or alcohol.
Recent Major Changes
- Boxed Warning 1/2017
- Warnings and Precautions (5.2) 1/2017
Indications and Usage for Codeine and Chlorpheniramine ER Tablets
CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE is a combination of codeine phosphate, an opiate agonist antitussive, and chlorpheniramine maleate, a histamine-1 (H1) receptor antagonist indicated for the relief of cough and symptoms associated with upper respiratory allergies or a common cold. (1) Important Limitations of Use Not indicated for pediatric patients under 18 years of age (8.4))
Codeine and Chlorpheniramine ER Tablets Dosage and Administration
- Adults and children 18 years of age and older: 1 tablet every 12 hours, not to exceed 2 doses in 24 hours. (2.1)
Dosage Forms and Strengths
Extended release (ER) tablet: contains 54.3 mg of codeine phosphate (equivalent to 40 mg of codeine) and 8 mg of chlorpheniramine maleate (equivalent to 5.6 mg of chlorpheniramine). (3)
Contraindications
- •
- Post-operative pain management in children undergoing tonsillectomy and/or adenoidectomy. (4)
- •
- Patients with known hypersensitivity to codeine, chlorpheniramine, or any of the product components of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE. (4)
Warnings and Precautions
- •
- Risk of death in ultra-rapid metabolizers: Conversion of codeine into its active metabolite, morphine, may occur more rapidly and completely resulting in higher than expected morphine levels and respiratory depression or death. (5.1)
- •
- Risks using with Benzodiazepines or other CNS Depressants. (5.2)
- •
- Dose-related respiratory depression. Use with caution. (5.3)
- •
- Drug dependence: Prescribe with caution that is appropriate to the use of other opioids. (5.4)
- •
- Head injury, intra-cranial lesions, or increased intracranial pressure: Avoid in patients with head injury, intra-cranial lesions, or increased intracranial pressure. (5.5)
- •
- Activities requiring mental alertness: Avoid engaging in hazardous tasks requiring complete mental alertness such as driving or operating machinery. Avoid concurrent use of alcohol or other central nervous system depressants.. (5.6)
- •
- Prolonged use may cause Obstructive Bowel Disease (5.7)
- •
- Acute abdominal conditions: Use caution in patients with acute abdominal conditions. (5.8)
- •
- Special risk patients: Caution in elderly patients and those with asthma, persistent or chronic cough, hypothyroidism, Addison’s disease, prostatic hypertrophy or urethral stricture. (5.9)
Adverse Reactions/Side Effects
Common adverse reactions of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE include: Nausea and vomiting, constipation, abdominal distension, abdominal pain, blurred vision, diplopia, visual disturbances, confusion, dizziness, depression, drowsiness, sedation, headache, euphoria, facial dyskinesia, feeling faint, light-headedness, general feeling of discomfort or illness, excitability, nervousness, agitation, restlessness, somnolence, insomnia, dyskinesia, irritability, tremor. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Nexgen Pharma, Inc. at 888-710-0006 or go to www.nexgenpharma.com or FDA at 1-800-FDA-1088
Drug Interactions
- •
- Opioids, antihistamines, antipsychotics, anti-anxiety agents, or other CNS depressants: may cause additive CNS depression. (7.1)
- •
- MAOIs or tricyclic antidepressants: may increase the effect of either the antidepressant or codeine. (7.2)
- •
- Anticholinergic drugs: Use with caution. Additive adverse effects resulting from cholinergic blockage (e.g., xerostomia, blurred vision, or constipation) may occur. (7.3)
- •
- Inhibitors or inducers of metabolic enzymes: Concomitant use of cytochrome P450 2D6 and 3A4 enzyme inhibitors or inducers may result in an altered response to codeine, monitor antitussive activity. Chlorpheniramine may inhibit the hepatic metabolism of phenytoin, monitor phenytoin toxicity. (7.4)
Use In Specific Populations
- •
- Pregnancy: Based on animal data, may cause fetal harm. (8.1)
- •
- Labor: Use of codeine during labor can produce respiratory depression in the neonate. (8.2)
- •
- Nursing mothers: The risk of infant exposure to codeine and morphine through breast milk should be weighed against the benefits of breastfeeding for both the mother and the baby. (8.3)
- •
- Pediatric patients: Safety and effectiveness of this drug product has not been established for patients under 18. (8.4)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 1/2017
Full Prescribing Information
WARNINGDEATH RELATED TO ULTRA-RAPID METABOLISM OF CODEINE TO MORPHINE andRISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
Ultra-Rapid Metabolism
Respiratory depression and death have occurred in children who received codeine following tonsillectomy and/or adenoidectomy and had evidence of being ultra-rapid metabolizers of codeine due to a CYP2D6 polymorphism. (5.1)
Concomitant Use with Benzodiazepines, CNS Depressants
Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death [see Warning and Precautions (5.2) Drug Interactions (7.1). Avoid use of opioid cough medications in patients taking benzodiazepines, other CNS depressants, or alcohol.
1. Indications and Usage for Codeine and Chlorpheniramine ER Tablets
CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE is indicated for the relief of cough and symptoms associated with upper respiratory allergies or a common cold in adults 18 years of age and older.
Important Limitations of Use
Not indicated for pediatric patients under 18 years of age [see Use in Special Population (8.4)]
3. Dosage Forms and Strengths
Extended release tablets: Each tablet contains 54.3 mg of codeine phosphate (equivalent to 40 mg of codeine) and 8 mg of chlorpheniramine maleate (equivalent to 5.6 mg of chlorpheniramine). Each tablet is white to off-white, uncoated, round, debossed with NXG on one side and CC on the other side.
4. Contraindications
- CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE is contraindicated in:
- Postoperative pain management in children who have undergone tonsillectomy and/or adenoidectomy [see Warnings and Precautions (5.1)].
Patients with known hypersensitivity to codeine, chlorpheniramine or any of the inactive ingredients of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE. Persons known to be hypersensitive to certain other opioids may exhibit cross-sensitivity to codeine.
5. Warnings and Precautions
5.1 Death Related to Ultra-Rapid Metabolism of Codeine to Morphine
Respiratory depression and death have occurred in children who received codeine in the post-operative period following tonsillectomy and/or adenoidectomy and had evidence of being ultra-rapid metabolizers of codeine (i.e., multiple copies of the gene for cytochrome P450 isoenzyme 2D6 or high morphine concentrations). Deaths have also occurred in nursing infants who were exposed to high levels of morphine in breast milk because their mothers were ultra-rapid metabolizers of codeine. [see Use in Specific Populations (8.3)]
Some individuals may be ultra-rapid metabolizers because of a specific CYP2D6 genotype (gene duplications denoted as *1/*1xN or *1/*2xN). The prevalence of this CYP2D6 phenotype varies widely and has been estimated at 0.5 to 1% in Chinese and Japanese, 0.5 to 1% in Hispanics, 1 to 10% in Caucasians, 3% in African Americans, and 16 to 28% in North Africans, Ethiopians, and Arabs. Data are not available for other ethnic groups. These individuals convert codeine into its active metabolite, morphine, more rapidly and completely than other people. This rapid conversion results in higher than expected serum morphine levels. Even at labeled dosage regimens, individuals who are ultra-rapid metabolizers may have life-threatening or fatal respiratory depression or experience signs of overdose (such as extreme sleepiness, confusion, or shallow breathing). [see Overdosage (10)]
Children with obstructive sleep apnea who are treated with codeine for post-tonsillectomy and/or adenoidectomy pain may be particularly sensitive to the respiratory depressant effects of codeine that has been rapidly metabolized to morphine. CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE is contraindicated for post-operative pain management in all pediatric patients undergoing tonsillectomy and/or adenoidectomy [see Contraindications (4)].
When prescribing codeine-containing drugs, healthcare professionals should choose the lowest effective dose for the shortest period of time and inform patients and caregivers about these risks and the signs of morphine overdose. [see Use in Specific Populations (8),Overdosage (10)]
5.2 Risks from Concomitant Use with Benzodiazepines or other CNS Depressants
Concomitant use of opioids, including CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE, with benzodiazepines, or other CNS depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Because of these risks, avoid use of opioid cough medications in patients taking Benzodiazepines, other CNS depressants, or alcohol [see Drug Interactions (7.1)].
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioids alone. Because of similar pharmacologic properties, it is reasonable to expect similar risk with concomitant use of opioid cough medications and benzodiazepines, other CNS depressants, or alcohol.
Advise both patients and caregivers about the risks of respiratory depression and sedation if CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE is used with benzodiazepines, alcohol, or other CNS depressants. [see Patient Counseling Information (17)]
5.3 Respiratory Depression
Codeine, one of the active ingredients in CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE, produces dose-related respiratory depression by directly acting on brain stem respiratory centers.
Overdose of codeine in adults has been associated with fatal respiratory depression, and the use of codeine in children has been associated with fatal respiratory depression. Exercise caution when administering CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE because of the potential for respiratory depression. If respiratory depression occurs, discontinue CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE and use naloxone hydrochloride when indicated to antagonize the effect and other supportive measures as necessary. [see Overdosage (10)].
5.4 Drug Dependence
Codeine can produce drug dependence of the morphine type and, therefore, has the potential for being abused. Psychological dependence, physical dependence, and tolerance may develop upon repeated administration of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE. Prescribe and administer CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE with the same degree of caution appropriate to the use of other opioid drugs. [see Drug Abuse and Dependence (9.2, 9.3)]
5.5 Head Injury and Increased Intracranial Pressure
The respiratory depression effects of opioids and their capacity to elevate cerebrospinal fluid pressure may be markedly exaggerated in the presence of head injury, other intracranial lesions, or a pre-existing increase in intracranial pressure. Furthermore, opioids produce adverse reactions that may obscure the clinical course of patients with head injuries. The use of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE should be avoided in these patients.
5.6 Activities Requiring Mental Alertness
Codeine and chlorpheniramine, the active ingredients in CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE, may produce marked drowsiness and impair the mental and/or physical abilities required for the performance of potentially hazardous tasks such as driving a car or operating machinery. Advise patients to avoid engaging in hazardous tasks requiring mental alertness and motor coordination after ingestion of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE. Concurrent use of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE with alcohol or other central nervous system depressants should be avoided because additional impairment of central nervous system performance may occur.
5.7 Obstructive Bowel Disease
Chronic use of opioids, including codeine, may result in obstructive bowel disease especially in patients with underlying intestinal motility disorders. Codeine may cause or aggravate constipation. Use with caution in patients with underlying intestinal motility disorders.
5.8 Acute Abdominal Conditions
CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE should be used with caution in patients with acute abdominal conditions since the administration of codeine may obscure the diagnosis or clinical course of patients with acute abdominal conditions. The concurrent use of other anticholinergics with codeine may produce paralytic ileus. [see Drug Interactions (7.3)]
5.9 Special Risk Patients
As with other opioids, CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE should be used with caution in elderly or debilitated patients and those with asthma, persistent or chronic cough, hypothyroidism, Addison's disease, prostatic hypertrophy or urethral stricture. The usual precautions should be observed and the possibility of respiratory depression should be kept in mind.
6. Adverse Reactions/Side Effects
Use of codeine, an opioid, may result in the following:
- •
- Respiratory depression [see Warnings and Precautions (5.3) and Overdosage (10)]
- •
- Drug dependence [see Warnings and Precautions (5.4)]
- •
- Increased intracranial pressure [see Warnings and Precautions (5.5)]
- •
- Decreased mental alertness with impaired mental and/or physical abilities [see Warnings and Precautions (5.6)]
- •
- Paralytic ileus [see Warnings and Precautions (5.7)]
Use of chlorpheniramine, an antihistamine, may result in:
- •
- Decreased mental alertness with impaired mental and/or physical abilities [see Warnings and Precautions (5.6)]
Adverse reactions listed below have been reported in the literature for codeine and chlorpheniramine and may be expected to occur with CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE. Also included are events that occurred during clinical pharmacokinetic studies (in a total of 66 healthy adult volunteers with either single or multiple dose exposure) with CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE and judged by the investigator to be related to study treatment. Because these reactions may be reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Allergic: Allergic laryngospasm, nasal stuffiness, bronchospastic allergic reaction, hives, itching, swelling of face.
Body as a whole: Asthenia, feeling of relaxation, redness or flushing of the face, unusual tiredness, weakness. Cardiovascular: Fast, or slow heartbeat, hypertension, hypotension, orthostatic hypotension, palpitations, shock-like state, syncope.
Dermatological System: Skin rash, pruritus, erythema, urticaria, excessive perspiration, dermatitis.
Endocrine System: Changes in glucose utilization, decreased lactation, early menses, glycosuria, gynecomastia, hypoglycemia, increased appetite, increased libido, pheochromocytoma stimulation.
Gastrointestinal System: Nausea and vomiting,, constipation, abdominal distension, abdominal pain, acute pancreatitis, dry mouth, dyspepsia, epigastric distress, loss of appetite, diarrhea, gastro-esophageal reflux, gastrointestinal hypomotility.
Genitourinary System: Ureteral spasm, urinary retention, dysuria, urinary frequency, urinary hesitancy, irritative bladder symptom.
Nervous System: Blurred vision, diplopia, visual disturbances, confusion, dizziness, depression, drowsiness, sedation, headache, euphoria, facial dyskinesia, false sense of well-being, feeling faint, lightheadedness, general feeling of discomfort or illness, excitability nervousness, agitation, restlessness, somnolence, insomnia, dyskinesia, irritability, tremor.
Respiratory: Dryness of the pharynx and respiratory passages, laryngismus, atelectasis, wheezing, troubled breathing, respiratory depression, hiccups.
Special Senses: labyrinthitis, tinnitus, vertigo, hypermetropia, lacrimation increased, mydriasis, photophobia.
7. Drug Interactions
7.1 Benzodiazepines, Opioids, Antihistamines, Antipsychotics, Anti-anxiety Agents, or Other CNS Depressants (Including Alcohol)
The use of benzodiazepines, opioids, antihistamines, antipsychotics, anti-anxiety agents, or other CNS depressants (including alcohol) concomitantly with CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE may cause an additive CNS depressant effect, profound sedation, respiratory depression, coma, and death and should be avoided. [see Warnings and Precautions (5.2)].
7.2 Monoamine Oxidase Inhibitors and Tricyclic Antidepressants
Do not prescribe CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE if the patient is taking a monoamine oxidase inhibitor (MAOI) (i.e., certain drugs used for depression, psychiatric or emotional conditions, or Parkinson’s disease), or for 2 weeks after stopping a MAOI drug. The use of MAOIs or tricyclic antidepressants with codeine preparations may increase the effect of either the antidepressant or codeine.
7.3 Anticholinergic Drugs
Codeine and chlorpheniramine should be administered cautiously to persons receiving other anticholinergic drugs in order to avoid paralytic ileus and excessive anticholinergic effects.
Additive adverse effects resulting from cholinergic blockade (e.g., xerostomia, blurred vision, or constipation) may occur when anticholinergic drugs are administered with chlorpheniramine.
7.4 Inhibitors or Inducers of Metabolic Enzymes
Codeine is metabolized by the CYP2D6 and CYP3A4 isoenzymes [see Pharmacokinetics (12.3)]. The concurrent use of drugs that preferentially induce codeine N-demethylation (via CYP3A4) may increase the plasma concentrations of codeine’s inactive metabolite norcodeine. Drugs that inhibit codeine O-demethylation (via CYP2D6), may decrease the plasma concentration of codeine’s active metabolites, morphine and morphine-6-glucuronide. The contribution of these active metabolites to the overall antitussive effect of codeine is not known, but should be considered.
Adverse event reports in the literature suggest a possible drug interaction involving increased serum phenytoin levels and phenytoin toxicity when chlorpheniramine and phenytoin are co-administered. The exact mechanism for this interaction is not known, however it is believed that chlorpheniramine may inhibit the hepatic metabolism of phenytoin. Patients should be monitored for evidence of phenytoin toxicity such as ataxia, hyperreflexia, nystagmus and tremor when these two drugs are co-administered.
8. Use In Specific Populations
8.1 Pregnancy
Teratogenic Effects
Pregnancy Category C
There are no adequate and well-controlled studies of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE in pregnant women.
Reproductive toxicity studies have not been conducted with CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE; however, studies are available with individual active ingredients or related active ingredients. Because animal reproduction studies are not always predictive of human response, CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE should be used during pregnancy only if the benefit justifies the potential risk to the fetus.
Codeine:
Codeine has embryolethal and fetotoxic effects in rats. In a study in which pregnant rats were dosed throughout organogenesis, a dose approximately 15 times the maximum recommended human daily dose (MRHDD; on a mg/m2 basis at an oral maternal dose of 120 mg/kg/day) increased resorptions and decreased fetal weight; however, these effects occurred in the presence of maternal toxicity.
In studies in which rabbits and mice were dosed throughout organogenesis, codeine at doses approximately 7 and 35 times the MRHDD (on a mg/m2 basis at 30 and 600 mg/kg/day, respectively) produced no adverse developmental effects.
Chlorpheniramine:
A retrospective study found a small, but statistically significant, association between maternal use of chlorpheniramine and inguinal hernia and eye or ear anomalies in children. Other retrospective studies have found that the frequency of congenital anomalies, in general, was not increased among offspring of women who took chlorpheniramine during pregnancy. The significance of these findings to the therapeutic use of chlorpheniramine in human pregnancy is not known.
In studies with chlorpheniramine in which pregnant rats and rabbits were dosed throughout organogenesis, oral doses up to approximately 25 and 30times the MRHDD on a mg/m2 basis, respectively, produced no adverse developmental effects. However, when mice were dosed throughout pregnancy, a dose approximately 9times the MRHDD (on a mg/m2 basis at an oral maternal dose of 20 mg/kg/day) was embryolethal, and postnatal survival was decreased when dosing was continued after parturition. Embryolethality was also observed when male and female rats were dosed with approximately 9times the MRHDD (on a mg/m2 basis at an oral parental dose of 10 mg/kg/day) prior to mating.
Nonteratogenic Effects
Codeine:
Babies born to mothers who have been taking opioids regularly prior to delivery will be physically dependent. The withdrawal signs include irritability and excessive crying, tremors, hyperactive reflexes, increased respiratory rate, increased stools, sneezing, yawning, vomiting, and fever. The intensity of the syndrome does not always correlate with the duration of maternal opioid use or dose.
8.2 Lactation
As with all opioids, administration of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE to the mother shortly before delivery may result in some degree of respiratory depression in the newborn, especially if higher doses are used.
8.3 Females and Males of Reproductive Potential
Caution should be exercised when CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE is administered to nursing mothers. Codeine is secreted into human milk. In women with normal codeine metabolism (normal CYP2D6 activity), the amount of codeine secreted into human milk is low and dose-dependent. However, some women are ultra-rapid metabolizers of codeine. These women achieve higher-than-expected serum levels of codeine's active metabolite, morphine, leading to higher-than-expected levels of morphine in breast milk and potentially dangerously high serum morphine levels in their breastfed infants. Therefore, maternal use of codeine can potentially lead to serious adverse reactions, including death, in nursing infants.
The risk of infant exposure to codeine and morphine through breast milk should be weighed against the benefits of breastfeeding for both the mother and the baby. Caution should be exercised when codeine is administered to a nursing woman. If a codeine containing product is selected, the lowest dose should be prescribed for the shortest period of time to achieve the desired clinical effect. Mothers using codeine should be informed about when to seek immediate medical care and how to identify the signs and symptoms of neonatal toxicity, such as drowsiness or sedation, difficulty breastfeeding, breathing difficulties, and decreased tone, in their baby. Nursing mothers who are ultra-rapid metabolizers may also experience overdose symptoms such as extreme sleepiness, confusion, or shallow breathing. Prescribers should closely monitor mother-infant pairs and notify treating pediatricians about the use of codeine during breast-feeding [see Warnings and Precautions (5.1)].
Chlorpheniramine is excreted in human milk. The clinical significance is unknown; however, the anticholinergic action of chlorpheniramine may suppress lactation if taken prior to nursing.
8.4 Pediatric Use
Safety and effectiveness of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE in patients under 18 years of age have not been established. The use of codeine in children has been associated with fatal respiratory depression. [see Warnings and Precautions (5.1)].
8.5 Geriatric Use
Clinical efficacy and safety studies have not been conducted with CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE. Other reported clinical experience with the individual active ingredients of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. In general, dose selection for an elderly patient should be made with caution, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Renal Impairment
Pharmacokinetics of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE has not been characterized in renal impairment subjects.
Both codeine phosphate and chlorpheniramine maleate are cleared substantially by the kidney. As such, impaired renal function could potentially lead to the risk of decreased clearance and thereby increased retention or systemic levels of both these drugs. CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE should be used with caution in patients with severe renal impairment.
8.7 Hepatic Impairment
Pharmacokinetics of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE has not been characterized in hepatic impairment subjects. Both codeine and chlorpheniramine maleate are extensively metabolized by liver before elimination from the body. As such, impaired hepatic function could potentially lead to the risk of decreased metabolism and thereby increased systemic levels of both these drugs. CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE should be used with caution in patients with severe hepatic impairment.
9. Drug Abuse and Dependence
9.1 Controlled Substance
CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE is a Schedule III controlled prescription product containing codeine and should be prescribed and administered with caution.
9.2 Abuse
Codeine can produce drug dependence of the morphine type and therefore, has the potential for being abused. Psychological dependence, physical dependence, and tolerance may develop upon repeated administration of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE, and it should be prescribed and administered with the same degree of caution appropriate to the use of other opioid drugs.
9.3 Dependence
Psychological dependence, physical dependence, and tolerance may develop upon repeated administration of opioids; therefore, CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE should be prescribed and administered with caution.
Physical dependence, the condition in which continued administration of the drug is required to prevent the appearance of a withdrawal syndrome, assumes clinically significant proportions only after several weeks of continued oral opioid use, although some mild degree of physical dependence may develop after a few days of opioid therapy.
10. Overdosage
No human overdosage data are available for CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE.
Codeine
Overdosage with codeine is characterized by respiratory depression (a decrease in respiratory rate and/or tidal volume, Cheyne-Stokes respiration, cyanosis), extreme somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, and sometimes bradycardia and hypotension. In severe overdosage, apnea, circulatory collapse, cardiac arrest, and death may occur.
Codeine may cause miosis, even in total darkness. Pinpoint pupils are a sign of opioid overdose but are not pathognomonic (e.g., pontine lesions of hemorrhagic or ischemic origin may produce similar findings). Marked mydriasis rather than miosis may be seen with hypoxia in overdose situations.
Chlorpheniramine
Manifestations of chlorpheniramine overdosage may vary from central nervous system depression to stimulation. Central toxic effects are characterized by agitation, anxiety, delirium, disorientation, hallucinations, hyperactivity, sedation, and seizures. Severe overdosage may produce coma, medullary paralysis, and death. Peripheral toxicity includes hypertension, tachycardia, dysrhythmias, vasodilation, hyperpyrexia, mydriasis, urinary retention, and diminished gastrointestinal motility. Dry mouth, pharynx, bronchi, and nasal passages may be observed.
Impaired secretion from sweat glands following toxic doses of drugs with anticholinergic side effects may predispose to hyperthermia.
An adult ingested 400 mg chlorpheniramine with no reported serious adverse effects. Toxic psychosis, a possible class effect from overdose of sedating antihistamines, has been reported with accidental overdose of chlorpheniramine.
Treatment of overdosage consists of discontinuation of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE together with institution of appropriate therapy.
Give primary attention to re-establishment of adequate respiratory exchange through provision of a patent airway and the institution of assisted or controlled ventilation. The opioid antagonist naloxone hydrochloride is a specific antidote for respiratory depression that may result from overdosage or unusual sensitivity to opioids including codeine. Therefore, an appropriate dose of naloxone hydrochloride should be administered, preferably by the intravenous route, simultaneously with efforts at respiratory resuscitation. For further information, see full prescribing information for naloxone hydrochloride. An antagonist should not be administered in the absence of clinically significant respiratory or circulatory depression. Oxygen, intravenous fluids, vasopressors, and other supportive measures should be employed as indicated. Gastric emptying may be useful in removing unabsorbed drug.
Hemodialysis is not routinely used to enhance the elimination of codeine or chlorpheniramine from the body. Urinary excretion of chlorpheniramine is increased when the pH of the urine is acidic; however, acid diuresis is NOT recommended to enhance elimination in overdose, as the risks of acidemia and acute tubular necrosis in patients with rhabdomyolysis far outweigh any potential benefits.
11. Codeine and Chlorpheniramine ER Tablets Description
CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE are extended release tablets that contain 54.3 mg of codeine phosphate (equivalent to 40 mg of codeine) and 8 mg of chlorpheniramine maleate (equivalent to 5.6 mg of chlorpheniramine)..
Codeine phosphate [morphine3methyl ether phosphate (1:1) (salt)] hemihydrate, is a narcotic analgesic and antitussive. It has the following structural formula:
Chlorpheniramine maleate is 2-pyridinepropanamine, γ-(4-chlorophenyl)-N,N-dimethyl-, (Z)-2-butenedioate (1:1) and has the following chemical structure:
CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE are white to off-white, uncoated, standard round extended release matrix tablets.
Other ingredients: hypromellose, lactose monohydrate, cellulose microcrystalline, polysorbate 80, magnesium stearate, and colloidal silicon dioxide.
12. Codeine and Chlorpheniramine ER Tablets - Clinical Pharmacology
12.1 Mechanism of Action
Codeine: Codeine is a semisynthetic narcotic antitussive and analgesic with multiple actions qualitatively similar to those of morphine. The precise mechanism of action of codeine and other opiates is not known; however, codeine is believed to act centrally on the cough center. In excessive doses, codeine will depress respiration. Codeine can produce miosis, euphoria, and physical and physiological dependence.
Chlorpheniramine: Chlorpheniramine is a propylamine derivative antihistamine (H1-receptor antagonist) of the alkylamine class that also possesses anticholinergic and sedative activity. It prevents released histamine from dilating capillaries and causing edema of the respiratory mucosa.
12.3 Pharmacokinetics
Absorption
Pharmacokinetic (PK) parameters (Mean ± SD) for CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE in fasting, healthy volunteers are shown in the table below.
|
PK Parameter |
Single-dose |
Multiple-dose (BID for 6.5 days) |
||
|
Codeine Mean (± SD) |
Chlorpheniramine Maleate Mean (± SD) |
Codeine Mean (± SD) |
Chlorpheniramine Maleate Mean (± SD) |
|
|
Tmax (h) (Range) |
3 (2-12) |
6 (4-12) |
3 (2-5) |
5 (3-7) |
|
Cmax (ng/mL) |
46 (11) |
9 (3) | ||
|
AUCinf (ng.h/mL) for single-dose OR AUC12 (ng.h/mL) for multiple-dose |
383 (99) |
312 (137) | ||
|
Half life (h) |
4 (1) |
21 (7) |
Not determined |
Not determined |
Food Effect
The presence of a high-fat, high-calorie meal did not significantly impact the PK parameters of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE.
Distribution
Codeine has been reported to have an apparent volume of distribution of approximately 3-6 L/kg, indicating extensive distribution of the drug into tissues. About 7-25% of codeine, reportedly, is bound to plasma proteins. Codeine passes the blood brain barrier and the placental barrier. Small amounts of codeine and its metabolite, morphine, are transferred to human breast milk.
Chlorpheniramine is widely distributed throughout the tissues of the body, including the central nervous system. It reportedly has an apparent steady-state volume of distribution of approximately 3.2 L/kg in adults and children and is about 70% bound to plasma proteins. Chlorpheniramine and its metabolites likely cross the placental barrier and are excreted into human breast milk.
Metabolism
About 70-80% of the administered dose of codeine is metabolized by conjugation with glucuronic acid to codeine-6‑ glucuronide (C6G) and via O-demethylation to morphine (about 5-10%) and N-demethylation to norcodeine (about 10%) respectively. UDP-glucuronosyltransferase (UGT) 2B7 and 2B4 are the major enzymes mediating glucurodination of codeine to C6G. Cytochrome P-450 (CYP) 2D6 and CYP3A4 are the major enzymes mediating O-demethylation and N-demethylation of codeine respectively. Morphine and norcodeine are further metabolized by conjugation with glucuronic acid. Morphine and its M6 glucuronide conjugate are pharmacologically active. Whether C6G has pharmacological activity is unknown. Norcodeine and M3 glucuronide conjugate of morphine are generally not considered to be pharmacologically active.
Chlorpheniramine is rapidly and extensively metabolized via demethylation in the liver, forming mono- and didesmethyl derivatives. Oxidative metabolism of chlorpheniramine is catalyzed by cytochrome P-450 2D6.
Elimination
Approximately 90% of the total dose of codeine is excreted through the kidneys, of which approximately 10% is unchanged codeine. Plasma half-life of codeine was observed to be about 4 hours with CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE.
Chlorpheniramine and its metabolites are primarily excreted through the kidneys, with large individual variation. Urinary excretion depends on urine pH and flow rate. Plasma half-life of chlorpheniramine was observed to be about 21 hours with CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity, mutagenicity, and reproductive studies have not been conducted with CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE however, published information is available for the active ingredients
Codeine: In 2-year studies in F344/N rats and B6C3F1 mice, codeine showed no evidence of tumorigenicity at dietary doses up to 70 and 400 mg/kg/day, respectively (approximately 9 and 25 times, respectively, the MRHDD dose for adults and children on a mg/m2 basis).
Codeine was not mutagenic in the in vitro bacterial reverse mutation assay or clastogenic in the in vitro Chinese hamster ovary (CHO) cell chromosomal aberration assay.
Fertility studies with codeine have not been conducted.
Chlorpheniramine: In 2-year studies in F344/N rats and B6C3F1 mice, chlorpheniramine maleate showed no evidence of tumorigenicity when administered 5 days/week at oral doses up to 30 and 50 mg/kg/day, respectively (approximately 25 and 20 times, respectively, the MRHDD on a mg/m2 basis).
Chlorpheniramine maleate was not mutagenic in the in vitro bacterial reverse mutation assay or the in vitro mouse lymphoma forward mutation assay. Chlorpheniramine maleate was clastogenic in the in vitro CHO cell chromosomal aberration assay.
Chlorphenirimaleate had no effects on fertility in rats and rabbits at oral doses approximately 25 and 30 times, respectively, the MRHDD on a mg/m2 basis.
14. Clinical Studies
The efficacy of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE is based on previously established findings of effectiveness of codeine and chlorpheniramine at the proposed doses.
16. How is Codeine and Chlorpheniramine ER Tablets supplied
CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE is supplied as white to off-white, uncoated, standard round tablet, debossed with NXG on one side and CC on the other side. Supplied in bottles of 100 tablets: NDC 0722-7184-01.
Store at 20 to 25°C (68 to 77°F) [see USP Controlled Room Temperature]. Dispense in a tight, light-resistant container, as defined in the USP, with a child-resistant closure.
Keep this and all medicine out of reach of children.
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Overdosage: Advise patients not to increase the dose or dosing frequency of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE because serious adverse events such as respiratory depression may occur with overdosage. [see Warnings and Precautions (5.2); Overdosage (10)]
Interactions with Benzodiazepines and Other Central Nervous System Depressants: Inform patients and caregivers that potentially fatal additive effects may occur if CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE is used with benzodiazepines or other CNS depressants, including alcohol. Because of this risk, patients should avoid concomitant use of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE with benzodiazepines or other CNS depressants, including alcohol [see Warnings and Precautions (5.3), Drug Interactions (7.1)].
Activities Requiring Mental Alertness: Caution patients that CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE may produce marked drowsiness and impair the mental and/or physical abilities required for the performance of potentially hazardous tasks such as driving a car or operating machinery. [see Warnings and Precautions (5.6)]
Controlled Substance Status/Potential for Abuse and Dependence: Caution patients that CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE contains codeine and can produce drug dependence. [see Abuse and Dependence (9.2, 9.3)].
Manufactured by:
Nexgen Pharma, Inc.
Irvine, CA 92614
(Rev. 1/2017)
Patient Package Insert
|
MEDICATION GUIDE CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE extended release tablets, CIII |
|
What is the most important information I should know about CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE?
|
|
What is CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE? CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE is a prescription medicine used to treat cough and upper respiratory symptoms that you can have with allergies or a common cold. CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE is for adults 18 years and older. CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE contains 2 medicines, codeine and chlorpheniramine. Codeine is a narcotic cough suppressant. Chlorpheniramine is an antihistamine. CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE is a federal controlled substance (CIII) because it contains codeine that can be abused or lead to dependence. Keep CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE in a safe place to prevent misuse and abuse. Selling or giving away CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE may harm others and is against the law. CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE is not for children under 18 years of age. It is not known if CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE is safe and effective in children. |
|
Who should not take CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE? Do not give CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE to a child to treat pain after tonsillectomy or adenoidectomy surgery. Do not take CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE if you are allergic to any of the ingredients in CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE. See the end of this Medication Guide for a complete list of ingredients in CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE. You may have an increased risk of having an allergic reaction to CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE if you are allergic to certain other opioid medicines. |
|
Before taking CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE, tell your healthcare provider about all of your medical conditions, including if you:
|
|
Tell your healthcare provider about all of the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Using CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE with certain other medicines may affect each other. Using CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE with other medicines can cause serious side effects. Especially tell your healthcare provider if you:
Ask your healthcare provider if you are not sure if you take one of these medicines. |
|
How should I take CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE?
|
|
What should I avoid while taking CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE?
|
|
What are the possible side effects of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE? CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE may cause serious side effects, including:
The most common side effects of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE include:
These are not all the possible side effects of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
|
How should I store CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE?
|
|
General information about the safe and effective use of CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE. Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE for a condition for which it was not prescribed. Do not give CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE that is written for health professionals. What are the ingredients in CODEINE PHOSPHATE AND CHLORPHENIRAMINE MALEATE? Active ingredients: codeine and chlorpheniramine Inactive ingredients: Hypromellose, lactose monohydrate, cellulose microcrystalline, polysorbate 80, magnesium stearate, and colloidal silicon dioxide. Manufactured By: Nexgen Pharma, Inc. For more information go to www.nexgenpharma.com or call 888-710-0006 |
This Medication Guide has been approved by the U.S. Food and Drug Administration Issued: January 2017
| CODEINE AND CHLORPHENIRAMINE MALEATE ER
codeine and chlorpheniramine maleate er tablet, extended release |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Labeler - Nexgen Pharma, Inc. (048488621) |
| Registrant - Spiraso LLC (079226327) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Nexgen Pharma, Inc. | 160356114 | MANUFACTURE(0722-7184) , PACK(0722-7184) , ANALYSIS(0722-7184) , LABEL(0722-7184) | |