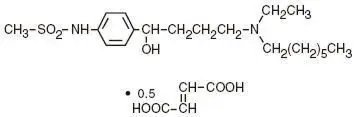
Drug Detail:Corvert (Ibutilide [ eye-bue-til-ide ])
Drug Class: Group III antiarrhythmics
Corvert - Clinical Pharmacology
Clinical Studies
Treatment with intravenous ibutilide fumarate for acute termination of recent onset atrial flutter/fibrillation was evaluated in 466 patients participating in two randomized, double-blind, placebo-controlled clinical trials. Patients had had their arrhythmias for 3 hours to 90 days, were anticoagulated for at least 2 weeks if atrial fibrillation was present more than 3 days, had serum potassium of at least 4.0 mEq/L and QTc below 440 msec, and were monitored by telemetry for at least 24 hours. Patients could not be on class I or other class III antiarrhythmics (these had to be discontinued at least 5 half-lives prior to infusion) but could be on calcium channel blockers, beta blockers, or digoxin. In one trial, single 10-minute infusions of 0.005 to 0.025 mg/kg were tested in parallel groups (0.3 to 1.5 mg in a 60 kg person). In the second trial, up to two infusions of ibutilide fumarate were evaluated—the first 1.0 mg, the second given 10 minutes after completion of the first infusion, either 0.5 or 1.0 mg. In a third double-blind study, 319 patients with atrial fibrillation or atrial flutter of 3 hours to 45 days duration were randomized to receive single, 10-minute intravenous infusions of either sotalol (1.5 mg/kg) or CORVERT (1 mg or 2 mg). Among patients with atrial flutter, 53% receiving 1 mg ibutilide fumarate and 70% receiving 2 mg ibutilide fumarate converted, compared to 18% of those receiving sotalol. In patients with atrial fibrillation, 22% receiving 1 mg ibutilide fumarate and 43% receiving 2 mg ibutilide fumarate converted compared to 10% of patients receiving sotalol.
Patients in registration trials were hemodynamically stable. Patients with specific cardiovascular conditions such as symptomatic heart failure, recent acute myocardial infarction, and angina were excluded. About two thirds had cardiovascular symptoms, and the majority of patients had left atrial enlargement, decreased left ventricular ejection fraction, a history of valvular disease, or previous history of atrial fibrillation or flutter. Electrical cardioversion was allowed 90 minutes after the infusion was complete. Patients could be given other antiarrhythmic drugs 4 hours postinfusion.
Results of the first two studies are shown in the tables below. Conversion of atrial flutter/ fibrillation usually (70% of those who converted) occurred within 30 minutes of the start of infusion and was dose related. The latest conversion seen was at 90 minutes after the start of the infusion. Most converted patients remained in normal sinus rhythm for 24 hours. Overall responses in these patients, defined as termination of arrhythmias for any length of time during or within 1 hour following completed infusion of randomized dose, were in the range of 43% to 48% at doses above 0.0125 mg/kg (vs 2% for placebo). Twenty-four hour responses were similar. For these atrial arrhythmias, ibutilide was more effective in patients with flutter than fibrillation ( ≥ 48% vs ≤ 40%).
| PERCENT OF PATIENTS WHO CONVERTED (First Trial) | ||||||
|---|---|---|---|---|---|---|
| Ibutilide | ||||||
| Placebo | 0.005 mg/kg | 0.01 mg/kg | 0.015 mg/kg | 0.025 mg/kg | ||
| n | 41 | 41 | 40 | 38 | 40 | |
|
||||||
| Both | Initially* | 2 | 12 | 33 | 45 | 48 |
| At 24 hours† | 2 | 12 | 28 | 42 | 43 | |
| Atrial flutter | Initially* | 0 | 14 | 30 | 58 | 55 |
| At 24 hours† | 0 | 14 | 30 | 58 | 50 | |
| Atrial fibrillation | Initially* | 5 | 10 | 35 | 32 | 40 |
| At 24 hours† | 5 | 10 | 25 | 26 | 35 | |
| PERCENT OF PATIENTS WHO CONVERTED (Second Trial) | ||||
|---|---|---|---|---|
| Ibutilide | ||||
| Placebo | 1.0 mg/0.5 mg | 1.0 mg/1.0 mg | ||
| n | 86 | 86 | 94 | |
|
||||
| Both | Initially* | 2 | 43 | 44 |
| At 24 hours† | 2 | 34 | 37 | |
| Atrial flutter | Initially* | 2 | 48 | 63 |
| At 24 hours† | 2 | 45 | 59 | |
| Atrial fibrillation | Initially* | 2 | 38 | 25 |
| At 24 hours† | 2 | 21 | 17 | |
The numbers of patients who remained in the converted rhythm at the end of 24 hours were slightly less than those patients who converted initially, but the difference between conversion rates for ibutilide compared to placebo was still statistically significant. In long-term follow-up, approximately 40% of all patients remained recurrence free, usually with chronic prophylactic treatment, 400 to 500 days after acute treatment, regardless of the method of conversion.
Patients with more recent onset of arrhythmia had a higher rate of conversion. Response rates were 42% and 50% for patients with onset of atrial fibrillation/flutter for less than 30 days in the two efficacy studies compared to 16% and 31% in those with more chronic arrhythmias.
Ibutilide was equally effective in patients below and above 65 years of age and in men and women. Female patients constituted about 20% of patients in controlled studies.
Warnings
Proarrhythmia
Like other antiarrhythmic agents, CORVERT Injection can induce or worsen ventricular arrhythmias in some patients. This may have potentially fatal consequences. Torsades de pointes, a polymorphic ventricular tachycardia that develops in the setting of a prolonged QT interval, may occur because of the effect CORVERT has on cardiac repolarization, but CORVERT can also cause polymorphic VT in the absence of excessive prolongation of the QT interval. In general, with drugs that prolong the QT interval, the risk of torsades de pointes is thought to increase progressively as the QT interval is prolonged and may be worsened with bradycardia, a varying heart rate, and hypokalemia. In clinical trials conducted in patients with atrial fibrillation and atrial flutter, those with QTc intervals >440 msec were not usually allowed to participate, and serum potassium had to be above 4.0 mEq/L. Although change in QTc was dose dependent for ibutilide, there was no clear relationship between risk of serious proarrhythmia and dose in clinical studies, possibly due to the small number of events. In clinical trials of intravenous ibutilide, patients with a history of congestive heart failure (CHF) or low left ventricular ejection fraction appeared to have a higher incidence of sustained polymorphic ventricular tachycardia (VT), than those without such underlying conditions; for sustained polymorphic VT the rate was 5.4% in patients with a history of CHF and 0.8% without it. There was also a suggestion that women had a higher risk of proarrhythmia, but the sex difference was not observed in all studies and was most prominent for nonsustained ventricular tachycardia. The incidence of sustained ventricular arrhythmias was similar in male (1.8%) and female (1.5%) patients, possibly due to the small number of events. CORVERT is not recommended in patients who have previously demonstrated polymorphic ventricular tachycardia (eg, torsades de pointes).
During registration trials, 1.7% of patients with atrial flutter or atrial fibrillation treated with CORVERT developed sustained polymorphic ventricular tachycardia requiring cardioversion. In these clinical trials, many initial episodes of polymorphic ventricular tachycardia occurred after the infusion of CORVERT was stopped but generally not more than 40 minutes after the start of the first infusion. There were, however, instances of recurrent polymorphic VT that occurred about 3 hours after the initial infusion. In two cases, the VT degenerated into ventricular fibrillation, requiring immediate defibrillation. Other cases were managed with cardiac pacing and magnesium sulfate infusions. Nonsustained polymorphic ventricular tachycardia occurred in 2.7% of patients and nonsustained monomorphic ventricular tachycardias occurred in 4.9% of the patients (see ADVERSE REACTIONS).
Proarrhythmic events must be anticipated. Skilled personnel and proper equipment, including cardiac monitoring equipment, intracardiac pacing facilities, a cardioverter/defibrillator, and medication for treatment of sustained ventricular tachycardia, including polymorphic ventricular tachycardia, must be available during and after administration of CORVERT. Before treatment with CORVERT, hypokalemia and hypomagnesemia should be corrected to reduce the potential for proarrhythmia. Patients should be observed with continuous ECG monitoring for at least 4 hours following infusion or until QTc has returned to baseline. Longer monitoring is required if any arrhythmic activity is noted. Management of polymorphic ventricular tachycardia includes discontinuation of ibutilide, correction of electrolyte abnormalities, especially potassium and magnesium, and overdrive cardiac pacing, electrical cardioversion, or defibrillation. Pharmacologic therapies include magnesium sulfate infusions. Treatment with antiarrhythmics should generally be avoided.
Precautions
Adverse Reactions/Side Effects
CORVERT Injection was generally well tolerated in clinical trials. Of the 586 patients with atrial fibrillation or atrial flutter who received CORVERT in phase II/III studies, 149 (25%) reported medical events related to the cardiovascular system, including sustained polymorphic ventricular tachycardia (1.7%) and nonsustained polymorphic ventricular tachycardia (2.7%).
Other clinically important adverse events with an uncertain relationship to CORVERT include the following (0.2% represents one patient): sustained monomorphic ventricular tachycardia (0.2%), nonsustained monomorphic ventricular tachycardia (4.9%), AV block (1.5%), bundle branch block (1.9%), ventricular extrasystoles (5.1%), supraventricular extrasystoles (0.9%), hypotension/postural hypotension (2.0%), bradycardia/sinus bradycardia (1.2%), nodal arrhythmia (0.7%), congestive heart failure (0.5%), tachycardia/sinus tachycardia/supraventricular tachycardia (2.7%), idioventricular rhythm (0.2%), syncope (0.3%), and renal failure (0.3%). The incidence of these events, except for syncope, was greater in the group treated with CORVERT than in the placebo group.
Another adverse reaction that may be associated with the administration of CORVERT was nausea, which occurred with a frequency greater than 1% more in ibutilide-treated patients than those treated with placebo.
The medical events reported for more than 1% of the placebo- and ibutilide-treated patients are shown in the following Table.
| Event | Placebo N=127 | All Ibutilide N=586 |
||
|---|---|---|---|---|
| Patients | Patients | |||
| n | % | n | % | |
| CARDIOVASCULAR | ||||
| Ventricular extrasystoles | 1 | 0.8 | 30 | 5.1 |
| Nonsustained monomorphic VT | 1 | 0.8 | 29 | 4.9 |
| Nonsustained polymorphic VT | — | — | 16 | 2.7 |
| Hypotension | 2 | 1.6 | 12 | 2.0 |
| Bundle branch block | — | — | 11 | 1.9 |
| Sustained polymorphic VT | — | — | 10 | 1.7 |
| AV block | 1 | 0.8 | 9 | 1.5 |
| Hypertension | — | — | 7 | 1.2 |
| QT segment prolonged | — | — | 7 | 1.2 |
| Bradycardia | 1 | 0.8 | 7 | 1.2 |
| Palpitation | 1 | 0.8 | 6 | 1.0 |
| Tachycardia | 1 | 0.8 | 16 | 2.7 |
| GASTROINTESTINAL | ||||
| Nausea | 1 | 0.8 | 11 | 1.9 |
| CENTRAL NERVOUS SYSTEM | ||||
| Headache | 4 | 3.1 | 21 | 3.6 |
In the post-cardiac surgery study (see CLINICAL STUDIES), similar types of medical events were reported. In the 1 mg ibutilide fumarate treatment group (N=70), 2 patients (2.9%) developed sustained polymorphic ventricular tachycardia and 2 other patients (2.9%) developed nonsustained polymorphic ventricular tachycardia. Polymorphic ventricular tachycardia was not reported in the 73 patients in the 0.5 mg dose group or in the 75 patients in the 0.25 mg dose group.
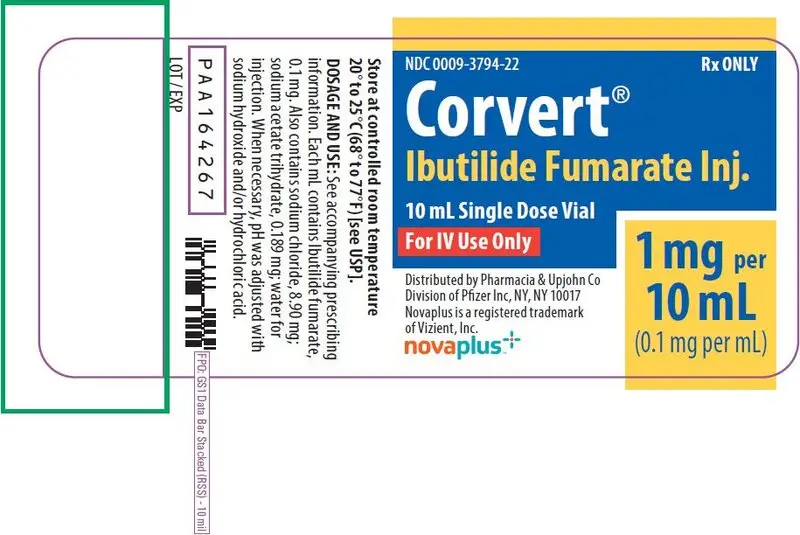
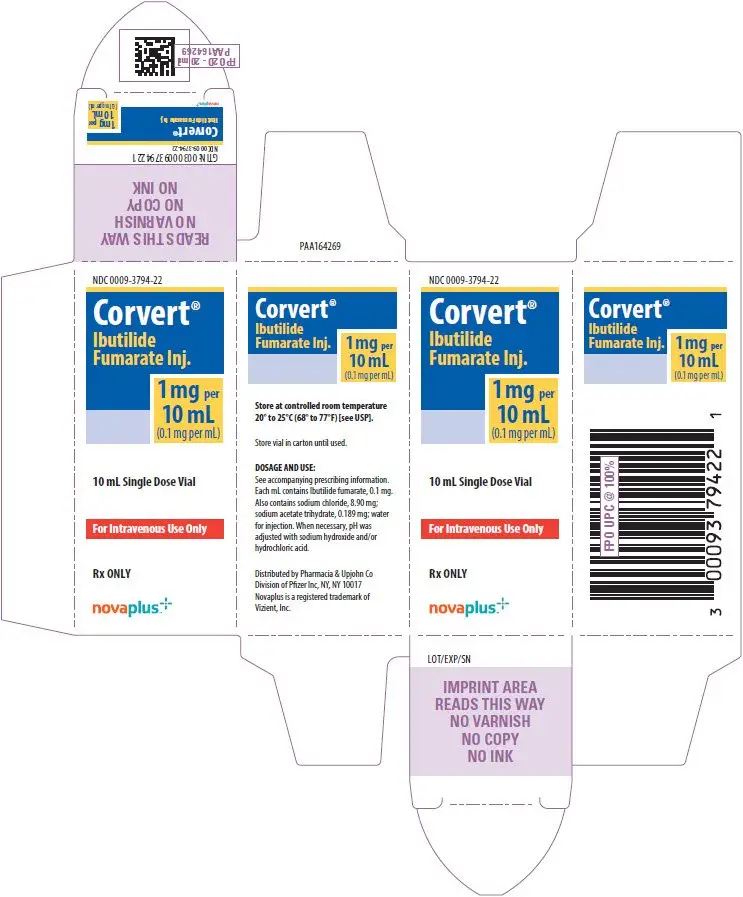
| CORVERT
ibutilide fumarate injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Pharmacia & Upjohn Company LLC (618054084) |
| Registrant - Pfizer Inc (113480771) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pharmacia & Upjohn Company LLC | 618054084 | ANALYSIS(0009-3794) , MANUFACTURE(0009-3794) , API MANUFACTURE(0009-3794) , PACK(0009-3794) , LABEL(0009-3794) | |