Drug Detail:Cotellic (Cobimetinib [ koe-bi-me-ti-nib ])
Drug Class: Multikinase inhibitors
Highlights of Prescribing Information
COTELLIC® (cobimetinib) tablets, for oral use
Initial U.S. Approval: 2015
Recent Major Changes
| Indications and Usage, Histiocytic Neoplasms (1.2) | 10/2022 |
| Dosage and Administration (2.1, 2.2) | 10/2022 |
| Warning and Precautions (5.2, 5.3, 5.4, 5.5, 5.6, 5.7) | 10/2022 |
Indications and Usage for Cotellic
COTELLIC® is a kinase inhibitor indicated:
- For the treatment of adult patients with unresectable or metastatic melanoma with a BRAF V600E or V600K mutation, in combination with vemurafenib. (1.1, 14.1)
- As a single agent for the treatment of adult patients with histiocytic neoplasms. (1.2, 14.2)
Cotellic Dosage and Administration
- Confirm the presence of BRAF V600E or V600K mutation in tumor specimens prior to initiation of COTELLIC with vemurafenib for patients with melanoma. (2.1)
- The recommended dose is 60 mg orally once daily for the first 21 days of each 28-day cycle until disease progression or unacceptable toxicity. Take COTELLIC with or without food. (2.2)
Dosage Forms and Strengths
Tablets: 20 mg (3)
Contraindications
None. (4)
Warnings and Precautions
- New primary malignancies, cutaneous and non-cutaneous: Monitor patients for new malignancies prior to initiation of therapy, while on therapy, and for up to 6 months following the last dose of COTELLIC. (5.1)
- Hemorrhage: Major hemorrhagic events can occur with COTELLIC. Monitor for signs and symptoms of bleeding. (5.2, 2.3)
- Cardiomyopathy: The risk of cardiomyopathy is increased in patients receiving COTELLIC with vemurafenib compared with vemurafenib as a single agent. The safety of COTELLIC has not been established in patients with decreased left ventricular ejection fraction (LVEF). Evaluate LVEF before treatment, after one month of treatment, then every 3 months thereafter during treatment with COTELLIC. (5.3, 2.3)
- Severe Dermatologic Reactions: Monitor for severe skin rashes. Interrupt, reduce, or discontinue COTELLIC. (5.4, 2.3)
- Serous Retinopathy and Retinal Vein Occlusion: Perform an ophthalmological evaluation at regular intervals and for any visual disturbances. Permanently discontinue COTELLIC for retinal vein occlusion (RVO). (5.5, 2.3)
- Hepatotoxicity: Monitor liver laboratory tests during treatment and as clinically indicated. (5.6, 2.3)
- Rhabdomyolysis: Monitor creatine phosphokinase periodically and as clinically indicated for signs and symptoms of rhabdomyolysis. (5.7, 2.3)
- Severe Photosensitivity: Advise patients to avoid sun exposure. (5.8, 2.3)
- Embryo-Fetal Toxicity: Can cause fetal harm. Advise females of reproductive potential of the potential risk to a fetus and to use effective contraception. (5.9, 8.1, 8.3)
Adverse Reactions/Side Effects
Unresectable or Metastatic Melanoma: Most common adverse reactions for COTELLIC (≥20%) are diarrhea, photosensitivity reaction, nausea, pyrexia, and vomiting. The most common (≥5%) Grade 3-4 laboratory abnormalities are increased GGT, increased CPK, hypophosphatemia, increased ALT, lymphopenia, increased AST, increased alkaline phosphatase, hyponatremia. (6.1)
Histiocytic neoplasms: Most common adverse reactions (≥20%) are acneiform dermatitis, diarrhea, infection, fatigue, nausea, edema, dry skin, maculopapular rash, pruritus, dyspepsia, vomiting, dyspnea and urinary tract infections. The most common (≥5%) grade 3-4 lab abnormalities include: Hyponatremia, increased blood creatine phosphokinase, hypokalemia, increased blood creatinine, increased AST, hypocalcemia, lymphopenia, leukopenia, anemia (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Genentech at 1-888-835-2555 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
Avoid concomitant administration of COTELLIC with strong or moderate CYP3A inducers or inhibitors. (2.3, 7.1, 7.2)
Use In Specific Populations
Lactation: Do not breastfeed while taking COTELLIC. (8.2)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 5/2023
Full Prescribing Information
1. Indications and Usage for Cotellic
2. Cotellic Dosage and Administration
2.1 Patient Selection for Treatment of Melanoma
Confirm the presence of BRAF V600E or V600K mutation in tumor specimens prior to initiation of treatment with COTELLIC with vemurafenib. Information on FDA-approved tests for the detection of BRAF V600 mutations in melanoma is available at: http://www.fda.gov/CompanionDiagnostics.
2.2 Recommended Dosage
The recommended dosage regimen of COTELLIC is 60 mg (three 20 mg tablets) orally taken once daily for the first 21 days of each 28-day cycle until disease progression or unacceptable toxicity [see Clinical Studies (14)].
Take COTELLIC with or without food [see Clinical Pharmacology (12.3)].
If a dose of COTELLIC is missed or if vomiting occurs when the dose is taken, resume dosing with the next scheduled dose.
2.3 Dose Modifications
Adverse Reactions
Review the Full Prescribing Information for vemurafenib for recommended dose modifications.
| First Dose Reduction | 40 mg orally once daily |
| Second Dose Reduction | 20 mg orally once daily |
| Subsequent Modification | Permanently discontinue COTELLIC if unable to tolerate 20 mg orally once daily |
| Severity of Adverse Reaction* | Dose Modification for COTELLIC |
|---|---|
|
|
| New Primary Malignancies (cutaneous and non-cutaneous) | No dose modification is required. |
| Hemorrhage | |
| Grade 3 | Withhold COTELLIC for up to 4 weeks.
|
| Grade 4 | Permanently discontinue. |
| Cardiomyopathy | |
| Asymptomatic, absolute decrease in LVEF from baseline of greater than 10% and less than institutional lower limit of normal (LLN) | Withhold COTELLIC for 2 weeks; repeat LVEF. Resume at next lower dose if all of the following are present:
Permanently discontinue if any of the following are present:
|
| Symptomatic LVEF decrease from baseline | Withhold COTELLIC for up to 4 weeks, repeat LVEF. Resume at next lower dose if all of the following are present:
Permanently discontinue if any of the following are present:
|
| Dermatologic Reactions | |
| Grade 2 (intolerable), Grade 3 or 4 | Withhold or reduce dose. |
| Serous Retinopathy or Retinal Vein Occlusion | |
| Serous retinopathy | Withhold COTELLIC for up to 4 weeks.
|
| Retinal vein occlusion | Permanently discontinue COTELLIC. |
| Liver Laboratory Abnormalities and Hepatotoxicity | |
| First occurrence Grade 4 | Withhold COTELLIC for up to 4 weeks.
|
| Recurrent Grade 4 | Permanently discontinue COTELLIC. |
| Rhabdomyolysis and Creatine Phosphokinase (CPK) elevations | |
| Withhold COTELLIC for up to 4 weeks.
|
| Photosensitivity | |
| Grade 2 (intolerable), Grade 3 or Grade 4 | Withhold COTELLIC for up to 4 weeks.
|
| Other | |
| Withhold COTELLIC for up to 4 weeks.
|
| First occurrence of any Grade 4 adverse reaction |
|
| Recurrent Grade 4 adverse reaction | Permanently discontinue COTELLIC. |
3. Dosage Forms and Strengths
Tablets: 20 mg, white, round, film-coated, debossed on one side with "COB".
5. Warnings and Precautions
Review the Full Prescribing Information for vemurafenib for information on the serious risks of vemurafenib.
5.1 New Primary Malignancies
New primary malignancies, cutaneous and non-cutaneous, can occur with COTELLIC.
5.2 Hemorrhage
Hemorrhage, including major hemorrhages defined as symptomatic bleeding in a critical area or organ, can occur with COTELLIC.
In Trial 1, the incidence of Grade 3–4 hemorrhages was 1.2% in patients receiving COTELLIC with vemurafenib and 0.8% in patients receiving vemurafenib. Hemorrhage (all grades) was 13% in patients receiving COTELLIC with vemurafenib and 7% in patients receiving vemurafenib. Cerebral hemorrhage occurred in 0.8% of patients receiving COTELLIC with vemurafenib and in none of the patients receiving vemurafenib. Gastrointestinal tract hemorrhage (3.6% vs 1.2%), reproductive system hemorrhage (2.0% vs 0.4%), and hematuria (2.4% vs 0.8%) also occurred at a higher incidence in patients receiving COTELLIC with vemurafenib compared with patients receiving vemurafenib.
In Trial 2, in patients with histiocytic neoplasms, 19% of patients experienced hemorrhage events (all were of grade 1 severity).
Withhold COTELLIC for Grade 3 hemorrhagic events. If improved to Grade 0 or 1 within 4 weeks, resume COTELLIC at a lower dose level. Discontinue COTELLIC for Grade 4 hemorrhagic events and any Grade 3 hemorrhagic events that do not improve [see Dosage and Administration (2.3)].
5.3 Cardiomyopathy
Cardiomyopathy, defined as symptomatic and asymptomatic decline in left ventricular ejection fraction (LVEF), can occur with COTELLIC. The safety of COTELLIC has not been established in patients with a baseline LVEF that is either below institutional lower limit of normal (LLN) or below 50%.
In Trial 1, patients were assessed for decreases in LVEF by echocardiograms or MUGA at baseline, Week 5, Week 17, Week 29, Week 43, and then every 4 to 6 months thereafter while receiving treatment. Grade 2 or 3 decrease in LVEF occurred in 26% of patients receiving COTELLIC with vemurafenib and 19% of patients receiving vemurafenib. The median time to first onset of LVEF decrease was 4 months (range 23 days to 13 months). Of the patients with decreased LVEF, 22% had dose interruption and/or reduction and 14% required permanent discontinuation. Decreased LVEF resolved to above the LLN or within 10% of baseline in 62% of patients receiving COTELLIC with a median time to resolution of 3 months (range: 4 days to 12 months).
In Trial 2, in patients with histiocytic neoplasms, 8% of patients experienced grade 2 ejection fraction decreased and 12% experienced grade 3-4 events. The median time to first onset of LVEF decrease was 29 days (range 22 days to 114 days). Of the patients with decreased LVEF, all had dose interruption and/or reduction and none required permanent discontinuation. Decreased LVEF resolved to above the LLN or within 10% of baseline in 60% of patients receiving COTELLIC with a median time to resolution of 31 days (range: 13 days to 126 days).
Evaluate LVEF prior to initiation, 1 month after initiation, and every 3 months thereafter until discontinuation of COTELLIC. Manage events of left ventricular dysfunction through treatment interruption, reduction, or discontinuation [see Dosage and Administration (2.3)]. In patients restarting COTELLIC after a dose reduction or interruption, evaluate LVEF at approximately 2 weeks, 4 weeks, 10 weeks, and 16 weeks, and then as clinically indicated.
5.4 Severe Dermatologic Reactions
Severe rash and other skin reactions can occur with COTELLIC.
In Trial 1, Grade 3 to 4 rash, occurred in 16% of patients receiving COTELLIC with vemurafenib and in 17% of patients receiving vemurafenib, including Grade 4 rash in 1.6% of patients receiving COTELLIC with vemurafenib and 0.8% of the patients receiving vemurafenib. The incidence of rash resulting in hospitalization was 3.2% in patients receiving COTELLIC with vemurafenib and 2.0% in patients receiving vemurafenib. In patients receiving COTELLIC, the median time to onset of Grade 3 or 4 rash events was 11 days (range: 3 days to 2.8 months). Among patients with Grade 3 or 4 rash events, 95% experienced complete resolution with the median time to resolution of 21 days (range 4 days to 17 months).
In Trial 2, in patients with histiocytic neoplasms, 81% of patients experienced rash events (all were of grade 1-2 severity).
Interrupt, reduce the dose, or discontinue COTELLIC [see Dosage and Administration (2.3)].
5.5 Serous Retinopathy and Retinal Vein Occlusion
Ocular toxicities can occur with COTELLIC, including serous retinopathy (fluid accumulation under layers of the retina).
In Trial 1, ophthalmologic examinations including retinal evaluation were performed pretreatment and at regular intervals during treatment. Symptomatic and asymptomatic serous retinopathy was identified in 26% of patients receiving COTELLIC with vemurafenib. The majority of these events were reported as chorioretinopathy (13%) or retinal detachment (12%). The time to first onset of serous retinopathy events ranged between 2 days to 9 months. The reported duration of serous retinopathy ranged between 1 day to 15 months. One patient in each arm developed retinal vein occlusion.
In Trial 2, in patients with histiocytic neoplasms, 4% experienced grade 2 retinopathy and 4% experienced grade 3 retinal vascular disorder.
Perform an ophthalmological evaluation at regular intervals and any time a patient reports new or worsening visual disturbances. If serous retinopathy is diagnosed, interrupt COTELLIC until visual symptoms improve. Manage serous retinopathy with treatment interruption, dose reduction, or with treatment discontinuation [see Dosage and Administration (2.3)].
5.6 Hepatotoxicity
Hepatotoxicity can occur with COTELLIC.
The incidences of Grade 3 or 4 liver laboratory abnormalities in Trial 1 among patients receiving COTELLIC with vemurafenib compared to patients receiving vemurafenib were: 11% vs. 5% for alanine aminotransferase, 8% vs. 2.1% for aspartate aminotransferase, 1.6% vs. 1.2% for total bilirubin, and 7% vs. 3.3% for alkaline phosphatase [see Adverse Drug Reactions (6.1)]. Concurrent elevation in ALT >3 times the upper limit of normal (ULN) and bilirubin >2 × ULN in the absence of significant alkaline phosphatase >2 × ULN occurred in one patient (0.4%) receiving COTELLIC with vemurafenib and no patients receiving single-agent vemurafenib.
In Trial 2, in patients with histiocytic neoplasms, 9% of the patients receiving COTELLIC experienced grade 3 or 4 aspartate aminotransferase increased and 5% of the patients experienced grade 3 or 4 alanine aminotransferase increased.
Monitor liver laboratory tests before initiation of COTELLIC and monthly during treatment, or more frequently as clinically indicated. Manage Grade 3 and 4 liver laboratory abnormalities with dose interruption, reduction, or discontinuation of COTELLIC [see Dosage and Administration (2.3)].
5.7 Rhabdomyolysis
Rhabdomyolysis can occur with COTELLIC.
In Trial 1, Grade 3 or 4 CPK elevations, including asymptomatic elevations over baseline, occurred in 14% of patients receiving COTELLIC with vemurafenib and 0.5% of patients receiving vemurafenib. The median time to first occurrence of Grade 3 or 4 CPK elevations was 16 days (range: 12 days to 11 months) in patients receiving COTELLIC with vemurafenib; the median time to complete resolution was 15 days (range: 9 days to 11 months). Elevation of serum CPK increase of more than 10 times the baseline value with a concurrent increase in serum creatinine of 1.5 times or greater compared to baseline occurred in 3.6% of patients receiving COTELLIC with vemurafenib and in 0.4% of patients receiving vemurafenib.
Obtain baseline serum CPK and creatinine levels prior to initiating COTELLIC, periodically during treatment, and as clinically indicated. If CPK is elevated, evaluate for signs and symptoms of rhabdomyolysis or other causes. Depending on the severity of symptoms or CPK elevation, dose interruption or discontinuation of COTELLIC may be required [see Dosage and Administration (2.3)].
In Trial 2, in patients with histiocytic neoplasms, 27% of patients experienced grade 2 CPK elevation and 27% of patients experienced grade 3-4 CPK elevation.
5.8 Severe Photosensitivity
Photosensitivity, including severe cases, can occur with COTELLIC.
In Trial 1, photosensitivity was reported in 47% of patients receiving COTELLIC with vemurafenib: 43% of patients with Grades 1 or 2 photosensitivity and the remaining 4% with Grade 3 photosensitivity. Median time to first onset of photosensitivity of any grade was 2 months (range: 1 day to 14 months) in patients receiving COTELLIC with vemurafenib, and the median duration of photosensitivity was 3 months (range: 2 days to 14 months). Among the 47% of patients with photosensitivity reactions on COTELLIC with vemurafenib, 63% experienced resolution of photosensitivity reactions.
Advise patients to avoid sun exposure, wear protective clothing and use a broad-spectrum UVA/UVB sunscreen and lip balm (SPF ≥30) when outdoors. Manage intolerable Grade 2 or greater photosensitivity with dose modifications [see Dosage and Administration (2.3)].
5.9 Embryo-Fetal Toxicity
Based on its mechanism of action and findings from animal reproduction studies, COTELLIC can cause fetal harm when administered to a pregnant woman. In animal reproduction studies, oral administration of cobimetinib in pregnant rats during the period of organogenesis was teratogenic and embryotoxic at doses resulting in exposures [area under the curves (AUCs)] that were 0.9 to 1.4-times those observed in humans at the recommended human dose of 60 mg. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with COTELLIC, and for 2 weeks following the final dose of COTELLIC [see Use in Specific Populations (8.1, 8.3), Clinical Pharmacology (12.1)].
6. Adverse Reactions/Side Effects
The following adverse reactions are discussed in greater detail in other sections of the label:
- New Primary Cutaneous Malignancies [see Warnings and Precautions (5.1)]
- Hemorrhage [see Warnings and Precautions (5.2)]
- Cardiomyopathy [see Warnings and Precautions (5.3)]
- Serious Dermatologic Reactions [see Warnings and Precautions (5.4)]
- Serous Retinopathy and Retinal Vein Occlusion [see Warnings and Precautions (5.5)]
- Hepatotoxicity [see Warnings and Precautions (5.6)]
- Rhabdomyolysis [see Warnings and Precautions (5.7)]
- Severe Photosensitivity [see Warnings and Precautions (5.8)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Unresectable or Metastatic Melanoma
The safety of COTELLIC was evaluated in Trial 1, a randomized (1:1), double-blind, active-controlled trial in previously untreated patients with BRAF V600 mutation-positive, unresectable or metastatic melanoma [see Clinical Studies (14)]. All patients received vemurafenib 960 mg twice daily on Days 1–28 and received either COTELLIC 60 mg once daily (n=247) or placebo (n=246) on Days 1–21 of each 28-day treatment cycle until disease progression or unacceptable toxicity. In the COTELLIC plus vemurafenib arm, 66% percent of patients were exposed for greater than 6 months and 24% of patients were exposed for greater than 1 year. Patients with abnormal liver function tests, history of acute coronary syndrome within 6 months, evidence of Class II or greater congestive heart failure (New York Heart Association), active central nervous system lesions, or evidence of retinal pathology were excluded from Trial 1. The demographics and baseline tumor characteristics of patients enrolled in Trial 1 are summarized in Clinical Studies [see Clinical Studies (14)].
In Trial 1, 15% of patients receiving COTELLIC experienced an adverse reaction that resulted in permanent discontinuation of COTELLIC. The most common adverse reactions resulting in permanent discontinuation were liver laboratory abnormalities defined as increased aspartate aminotransferase (AST) (2.4%), increased gamma glutamyltransferase (GGT) (1.6%) and increased alanine aminotransferase (ALT) (1.6%); rash (1.6%); pyrexia (1.2%); and retinal detachment (2%). Among the 247 patients receiving COTELLIC, adverse reactions led to dose interruption or reductions in 55%. The most common reasons for dose interruptions or reductions of COTELLIC were rash (11%), diarrhea (9%), chorioretinopathy (7%), pyrexia (6%), vomiting (6%), nausea (5%), and increased creatine phosphokinase (CPK) (4.9%). The most common (≥20%) adverse reactions with COTELLIC were diarrhea, photosensitivity reaction, nausea, pyrexia, and vomiting.
| Adverse reactions | COTELLIC + Vemurafenib (n=247) | Placebo + Vemurafenib (n=246) |
||
|---|---|---|---|---|
| All Grades†
(%) | Grades 3–4 (%) | All Grades (%) | Grades 3–4 (%) |
|
|
||||
| GASTROINTESTINAL DISORDERS | ||||
| Diarrhea | 60 | 6 | 31 | 1 |
| Nausea | 41 | 1 | 25 | 1 |
| Vomiting | 24 | 1 | 13 | 1 |
| Stomatitis‡ | 14 | 1 | 8 | 0 |
| SKIN AND SUBCUTANEOUS TISSUE DISORDERS | ||||
| Photosensitivity reaction§ | 46 | 4 | 35 | 0 |
| Acneiform dermatitis | 16 | 2 | 11 | 1 |
| GENERAL DISORDERS AND ADMINISTRATION SITE CONDITIONS | ||||
| Pyrexia | 28 | 2 | 23 | 0 |
| Chills | 10 | 0 | 5 | 0 |
| VASCULAR DISORDERS | ||||
| Hypertension | 15 | 4 | 8 | 2 |
| Hemorrhage¶ | 13 | 1 | 7 | <1 |
| EYE DISORDERS | ||||
| Vision impaired# | 15 | <1 | 4 | 0 |
| Chorioretinopathy | 13 | <1 | <1 | 0 |
| Retinal detachmentÞ | 12 | 2 | <1 | 0 |
The following clinically relevant adverse reactions (all grades) of COTELLIC were reported with <10% incidence in Trial 1:
Respiratory, thoracic and mediastinal disorders: Pneumonitis
| Laboratory | COTELLIC + Vemurafenib | Placebo + Vemurafenib | ||
|---|---|---|---|---|
| All Grades† | Grades 3–4† | All Grades† | Grades 3–4† | |
| % | % | % | % | |
| AST - aspartate aminotransferase, ALT - alanine aminotransferase, GGT - gamma-glutamyltransferase | ||||
|
||||
| Chemistry | ||||
| Increased creatinine | 100 | 3.3 | 100 | 0.4 |
| Increased AST | 73 | 8 | 44 | 2.1 |
| Increased ALT | 68 | 11 | 55 | 5 |
| Increased alkaline phosphatase | 71 | 7 | 56 | 3.3 |
| Increased creatine phosphokinase‡ | 79 | 14 | 16 | 0.5 |
| Hypophosphatemia | 68 | 12 | 38 | 6 |
| Increased GGT | 65 | 21 | 61 | 17 |
| Hyponatremia | 38 | 6 | 33 | 2.1 |
| Hypoalbuminemia | 42 | 0.8 | 20 | 0.4 |
| Hypokalemia | 25 | 4.5 | 17 | 3.3 |
| Hyperkalemia | 26 | 2.9 | 15 | 0.4 |
| Hypocalcemia | 24 | 0.4 | 10 | 1.7 |
| Hematology | ||||
| Anemia | 69 | 2.5 | 57 | 3.3 |
| Lymphopenia§ | 73 | 10 | 55 | 8 |
| Thrombocytopenia | 18 | 0 | 10 | 0 |
Histiocytic Neoplasms
The safety of COTELLIC was evaluated in Trial 2, a single-center single-arm trial in patients with histiocytic neoplasms [see Clinical Studies (14)]. In Trial 2, 26 patients with histiocytic neoplasms received COTELLIC 60 mg once daily for 21 days on, then 7 days off, in a 28-day treatment cycle. The median treatment duration was 10.7 months. Table 5 presents adverse reactions in at least 15% of patients reported with histiocytic neoplasms treated with COTELLIC. Table 6 presents laboratory abnormalities of grades ≥3 reported in patients with histiocytic neoplasms treated COTELLIC.
In Trial 2, 4 patients (15%) receiving COTELLIC experienced an adverse reaction that resulted in permanent discontinuation of COTELLIC. One patient discontinued due to worsening of underlying dyspnea and hypoxia; one patient discontinued due to retinal vascular disorder; one patient discontinued due to hyponatremia; and the other patient discontinued due to pneumonia.
| Body Systems Adverse reactions | All Grades* (%) (n=26) | Grades ≥3* (%) (n=26) |
|---|---|---|
|
||
| GASTROINTESTINAL DISORDERS | ||
| Diarrhea | 62 | 8 |
| Nausea | 46 | 0 |
| Dyspepsia† | 27 | 0 |
| Vomiting | 27 | 0 |
| Dry Mouth | 15 | 0 |
| Oral pain‡ | 15 | 0 |
| GENERAL DISORDERS AND ADMINISTRATION SITE CONDITIONS | ||
| Fatigue§ | 42 | 0 |
| Edema¶ | 42 | 4 |
| Pain | 15 | 0 |
| INFECTIONS AND INFESTATIONS | ||
| Infections# | 62 | 23 |
| Urinary tract infection | 23 | 8 |
| Pulmonary infectionsÞ | 19 | 12 |
| INJURY, POISONING AND PROCEDURAL COMPLICATIONS | ||
| Fall | 15 | 4 |
| INVESTIGATIONS | ||
| Decreased Ejection Fraction | 19 | 12 |
| RENAL AND URINARY | ||
| Acute kidney injury | 15 | 12 |
| RESPIRATORY, THORACIC AND MEDIASTINAL DISORDERS | ||
| Dyspnea | 27 | 15 |
| Cough | 15 | 0 |
| SKIN AND SUBCUTANEOUS TISSUE DISORDERS | ||
| Acneiform dermatitis | 65 | 0 |
| Dry skin | 31 | 0 |
| Maculo-papular rash | 31 | 0 |
| Pruritus | 31 | 4 |
| VASCULAR DISORDERS | ||
| Hemorrhageß | 19 | 0 |
| Hypertension | 15 | 4 |
The following clinically relevant adverse reactions (all grades) of COTELLIC were reported with <15% incidence in Trial 2:
Eye disorders: Vision blurred (12%), retinal vascular disorder (4%) and retinopathy (4%).
Gastrointestinal disorders: Stomatitis (12%)
Nervous system disorders: Headache (12%)
Respiratory, thoracic, and mediastinal disorders: Hypoxia (12%), pulmonary edema (4%), and respiratory failure (8%).
| Grades 3–4†
% |
|
|---|---|
| AST - aspartate aminotransferase, ALT - alanine aminotransferase | |
|
|
| Chemistry | |
| Increased blood creatine phosphokinase | 27 |
| Hyponatremia | 18 |
| Hypokalemia | 12 |
| Increased blood creatinine | 9 |
| Increased AST | 9 |
| Hypocalcemia | 9 |
| Increased ALT | 5 |
| Hematology | |
| Lymphopenia | 27 |
| Leukopenia | 9 |
| Anemia | 8 |
| Neutropenia | 5 |
7. Drug Interactions
7.1 Effect of Strong or Moderate CYP3A Inhibitors on COTELLIC
Coadministration of COTELLIC with itraconazole (a strong CYP3A4 inhibitor) increased cobimetinib systemic exposure by 6.7-fold. Avoid concurrent use of COTELLIC and strong or moderate CYP3A inhibitors. If concurrent short term (14 days or less) use of moderate CYP3A inhibitors including certain antibiotics (e.g., erythromycin, ciprofloxacin) is unavoidable for patients who are taking COTELLIC 60 mg, reduce COTELLIC dose to 20 mg. After discontinuation of a moderate CYP3A inhibitor, resume COTELLIC at the previous dose [see Dosage and Administration (2.3) and Clinical Pharmacology (12.3)]. Use an alternative to a strong or moderate CYP3A inhibitor in patients who are taking a reduced dose of COTELLIC (40 or 20 mg daily) [see Dosage and Administration (2.3) and Clinical Pharmacology (12.3)].
7.2 Effect of Strong or Moderate CYP3A Inducers on COTELLIC
Coadministration of COTELLIC with a strong CYP3A inducer may decrease cobimetinib systemic exposure by more than 80% and reduce its efficacy. Avoid concurrent use of COTELLIC and strong or moderate CYP3A inducers including but not limited to carbamazepine, efavirenz, phenytoin, rifampin, and St. John's Wort [see Clinical Pharmacology (12.3)].
8. Use In Specific Populations
8.4 Pediatric Use
The safety and effectiveness of COTELLIC have not been established in pediatric patients.
The safety and effectiveness of COTELLIC were assessed, but not established, in a multi-center, open-label, dose-escalation study in 55 pediatric patients aged 2 to 17 years with solid tumors [NCT02639546]. No new safety events were observed in pediatric patients in this trial.
Exposure in pediatric patients who received COTELLIC at the maximum tolerated dosage were lower than those previously observed in adults who received the approved recommended dosage.
8.5 Geriatric Use
Clinical studies of COTELLIC did not include sufficient numbers of patients aged 65 years and older to determine whether they respond differently from younger patients.
8.6 Hepatic Impairment
Adjustment in the starting dose of COTELLIC is not required in patients with mild (Child-Pugh score A), moderate (Child-Pugh B) or severe (Child-Pugh C) hepatic impairment [see Clinical Pharmacology (12.3)].
8.7 Renal Impairment
No dedicated pharmacokinetic trial in patients with renal impairment has been conducted. Dose adjustment is not recommended for mild to moderate renal impairment (CLcr 30 to 89 mL/min) based on the results of the population pharmacokinetic analysis. A recommended dose has not been established for patients with severe renal impairment [see Clinical Pharmacology (12.3)].
11. Cotellic Description
Cobimetinib fumarate is a kinase inhibitor. The chemical name is (S)-[3,4-difluoro-2-(2-fluoro-4-iodophenylamino)phenyl] [3-hydroxy-3-(piperidin-2-yl)azetidin-1-yl]methanone hemifumarate. It has a molecular formula C46H46F6I2N6O8 (2 C21H21F3IN3O2 ∙ C4H4O4) with a molecular mass of 1178.71 as a fumarate salt. Cobimetinib fumarate has the following chemical structure:
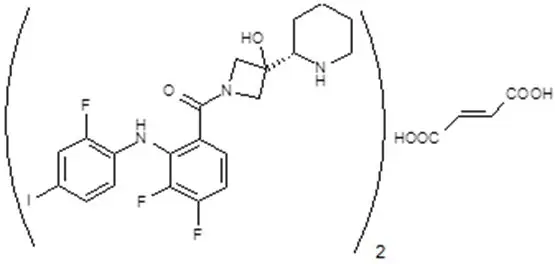
Cobimetinib is a fumarate salt appearing as white to off-white solid and exhibits a pH dependent solubility.
COTELLIC (cobimetinib) tablets are supplied as white, round, film-coated 20 mg tablets for oral administration, debossed on one side with "COB". Each 20 mg tablet contains 22 mg of cobimetinib fumarate, which corresponds to 20 mg of the cobimetinib free base.
The inactive ingredients of COTELLIC are: Tablet Core: microcrystalline cellulose, lactose monohydrate, croscarmellose sodium, magnesium stearate. Coating: polyvinyl alcohol, titanium dioxide, polyethylene glycol 3350, talc.
12. Cotellic - Clinical Pharmacology
12.1 Mechanism of Action
Cobimetinib is a reversible inhibitor of mitogen-activated protein kinase (MAPK)/extracellular signal regulated kinase 1 (MEK1) and MEK2. MEK proteins are upstream regulators of the extracellular signal-related kinase (ERK) pathway, which promotes cellular proliferation. BRAF V600E and K mutations result in constitutive activation of the BRAF pathway which includes MEK1 and MEK2. In mice implanted with tumor cell lines expressing BRAF V600E, cobimetinib inhibited tumor cell growth.
Cobimetinib and vemurafenib target two different kinases in the RAS/RAF/MEK/ERK pathway. Compared to either drug alone, coadministration of cobimetinib and vemurafenib resulted in increased apoptosis in vitro and reduced tumor growth in mouse implantation models of tumor cell lines harboring BRAF V600E mutations. Cobimetinib also prevented vemurafenib-mediated growth enhancement of a wild-type BRAF tumor cell line in an in vivo mouse implantation model.
12.3 Pharmacokinetics
The pharmacokinetics of cobimetinib was studied in healthy subjects and cancer patients. Cobimetinib exhibits linear pharmacokinetics in the dose range of 3.5 to 100 mg (i.e., 0.06 to 1.7 times the recommended dosage). Following oral administration of COTELLIC 60 mg once daily, steady-state was reached by 9 days with a mean accumulation ratio of 2.4-fold (44% CV).
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies with cobimetinib have not been conducted. Cobimetinib was not genotoxic in studies evaluating reverse mutations in bacteria, chromosomal aberrations in mammalian cells, and micronuclei in bone marrow of rats.
No dedicated fertility studies have been performed with cobimetinib in animals; however, effects on reproductive tissues observed in general toxicology studies conducted in animals suggest that there is potential for cobimetinib to impair fertility. In female rats, degenerative changes included increased apoptosis/necrosis of corpora lutea and vaginal epithelial cells at cobimetinib doses approximately twice those in humans at the clinically recommended dose of 60 mg based on body surface area. In male dogs, testicular degeneration occurred at exposures as low as approximately 0.1 times the exposure in humans at the clinically recommended dose of 60 mg.
14. Clinical Studies
14.1 Unresectable or Metastatic Melanoma
The safety and efficacy of COTELLIC was established in a multicenter, randomized (1:1), double-blinded, placebo-controlled trial conducted in 495 patients with previously untreated, BRAF V600 mutation-positive, unresectable or metastatic, melanoma. The presence of BRAF V600 mutation was detected using the cobas® 4800 BRAF V600 mutation test. All patients received vemurafenib 960 mg orally twice daily on days 1–28 and were randomized to receive COTELLIC 60 mg or matching placebo orally once daily on days 1–21 of an every 28-day cycle. Randomization was stratified by geographic region (North America vs. Europe vs. Australia/New Zealand/others) and disease stage (unresectable Stage IIIc, M1a, or M1b vs. Stage M1c). Treatment continued until disease progression or unacceptable toxicity. Patients randomized to receive placebo were not offered COTELLIC at the time of disease progression.
The major efficacy outcome was investigator-assessed progression-free survival (PFS) per RECIST v1.1. Additional efficacy outcomes were investigator-assessed confirmed objective response rate, overall survival, PFS as assessed by blinded independent central review, and duration of response.
The median age of the study population was 55 years (range 23 to 88 years), 58% of patients were male, 93% were White and 5% had no race reported, 60% had stage M1c disease, 72% had a baseline ECOG performance status of 0, 45% had an elevated baseline serum lactate dehydrogenase (LDH), 10% had received prior adjuvant therapy, and <1% had previously treated brain metastases. Patients with available tumor samples were retrospectively tested using next generation sequencing to further classify mutations as V600E or V600K; test results were obtained on 81% of randomized patients. Of these, 86% were identified as having a V600E mutation and 14% as having a V600K mutation.
Efficacy results are summarized in Table 7 and Figure 1.
| COTELLIC + Vemurafenib (n=247) | Placebo + Vemurafenib (n=248) |
|
|---|---|---|
| CI - Confidence Intervals; NE - not estimable | ||
|
||
| Progression-Free Survival (Investigator-Assessed) | ||
| Number of Events (%) | 143 (58%) | 180 (73%) |
| Progression | 131 | 169 |
| Death | 12 | 11 |
| Median PFS, months (95% CI) | 12.3 (9.5, 13.4) | 7.2 (5.6, 7.5) |
| Hazard Ratio (95% CI) | 0.56 (0.45, 0.70) | |
| p-value (stratified log-rank test) | <0.001 | |
| Overall Survival * | ||
| Number of Deaths (%) | 114 (46.2%) | 141 (56.9%) |
| Median OS, months (95% CI) | 22.3 (20.3, NE) | 17.4 (15.0, 19.8) |
| Hazard Ratio (95% CI) | 0.69 (0.54,0.88) | |
| p -value (stratified log-rank test) | 0.0032 | |
| Objective Response Rate | ||
| Objective Response Rate | 70% | 50% |
| (95% CI) | (64%, 75%) | (44%, 56%) |
| Complete Response | 16% | 10% |
| Partial Response | 54% | 40% |
| p-value | <0.001 | |
| Median Duration of Response, months (95% CI) | 13.0 (11.1, 16.6) | 9.2 (7.5, 12.8) |
Figure 1 Kaplan-Meier Curves of Overall Survival
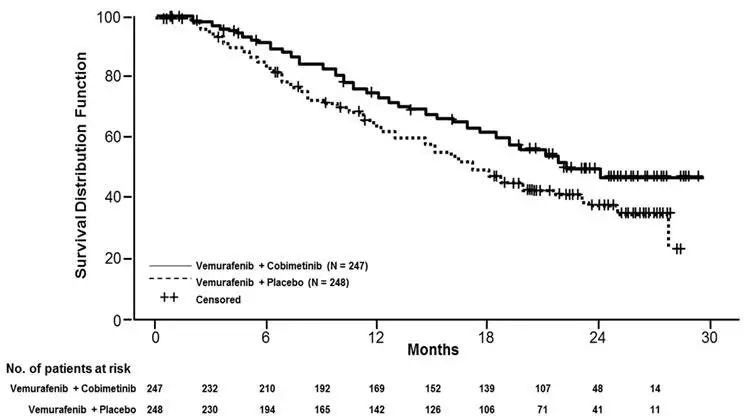
The effect on PFS was also supported by analysis of PFS based on the assessment by blinded independent review. A trend favoring the COTELLIC with vemurafenib arm was observed in exploratory subgroup analyses of PFS, OS, and ORR in both BRAF V600 mutation subtypes (V600E or V600K) in the 81% of patients in this trial where BRAF V600 mutation type was determined.
14.2 Histiocytic Neoplasms
A single-center, single-arm trial (Trial 2) was conducted to evaluate the efficacy, safety, and tolerability of COTELLIC as a single agent in adult patients with histologically confirmed histiocytic neoplasms of any mutational status. Patients with documented BRAF V600E mutations were enrolled if they were unable to access a BRAF inhibitor or discontinued a BRAF inhibitor due to toxicity. Enrolled patients had multi-system disease, recurrent or refractory disease, or single-system disease that is unlikely to benefit from conventional therapies, based on best available evidence.
The trial included 26 patients with histiocytic neoplasms including Langerhans Cell Histiocytosis (n=4), Rosai-Dorfman Disease (n=4), Erdheim-Chester Disease (n=13), Xanthogranuloma (n=2) and Mixed Histiocytosis (n=3). Patients with BRAF V600 mutant positive (n=6) and BRAF V600 Wild type (n=20) received COTELLIC. Twenty-one patients (81%) had received prior systemic therapies. The median age was 50.5 years (range, 18 to 79 years). Sixty-five percent of patients were men (n=17) and 35% were women (n=9). The majority of patients were White (85%), 8% were Black or African American and 4% were Asian; 96% were neither Hispanic nor Latino.
Patients were treated with COTELLIC 60 mg once daily for 21 days on, then 7 days off, in a 28-day treatment cycle (n=26). Eighteen patients required a dose reduction to 40 mg, and five patients required an additional dose reduction to 20 mg. The median duration of treatment following a dose reduction to 40 mg and 20 mg was 6.6 months and 3.9 months respectively.
The major efficacy outcome was best overall response rate (BORR), maintained on two occasions at least four weeks apart, as assessed by the investigator using the PET Response Criteria (PRC). Other clinical outcomes included PRC-based duration of response (DOR), and BORR maintained on two occasions at least four weeks apart, as assessed by investigator using RECIST v1.1.
The median duration of follow-up was 11.4 months (range, 0.2 to 36.8 months). The median time to PRC-based response was 2.0 (range, 0.2 to 17.3 months). The median PRC-based DOR was 31 months (range, 2 to 31 months). See Table 8 below for efficacy results.
| Response | PET Response, *,† Enrolled Patients (n=26)‡ | RECIST Response, Enrolled Patients (n=26)§ |
|---|---|---|
|
||
| Overall response rate, n (%) | 20 (76.9%) | 12 (46.2%) |
| (95% Clopper-Pearson CI) | (56.4, 91) | (26.6, 66.6) |
| Best Response, n (%) | ||
| Complete Response | 16 (61.5%) | 3 (11.5%) |
| Partial Response | 4 (15.4%) | 9 (34.6%) |
16. How is Cotellic supplied
COTELLIC (cobimetinib) is supplied as 20 mg film-coated tablets debossed on one side with "COB". COTELLIC tablets are available in bottles of 63 tablets.
NDC 50242-717-01
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Inform patients of the following:
| PATIENT INFORMATION COTELLIC® (co-TELL-ic) (cobimetinib) tablet |
|||
| Important: If your healthcare provider prescribes vemurafenib, also read the Medication Guide that comes with vemurafenib. | |||
| What is COTELLIC? | |||
COTELLIC is a prescription medicine that is used:
|
|||
| Your healthcare provider will perform a test to make sure that COTELLIC is right for you. | |||
| It is not known if COTELLIC is safe and effective in children under 18 years of age. | |||
Before you take COTELLIC, tell your healthcare provider about all of your medical conditions, including if you:
|
|||
| Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Certain medicines may affect the blood levels of COTELLIC. | |||
| Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine. | |||
How should I take COTELLIC?
|
|||
| What should I avoid during treatment with COTELLIC? | |||
Avoid sunlight during treatment with COTELLIC. COTELLIC can make your skin sensitive to sunlight. You may burn more easily and get severe sunburns. To help protect against sunburn:
|
|||
| What are the possible side effects of COTELLIC? COTELLIC may cause serious side effects, including:
|
|||
Check your skin regularly and tell your healthcare provider right away if you have any skin changes including:
|
|||
|
|
||
|
|||
|
|
||
|
|||
|
|
||
| Your healthcare provider should check your eyes if you notice any of the symptoms above. | |||
|
|||
|
|
||
|
|||
|
|
||
|
|||
|
|
||
| See "What should I avoid during treatment with COTELLIC?" for information on protecting your skin during treatment with COTELLIC. | |||
| The most common side effects of COTELLIC in adults with unresectable or metastatic melanoma include: | |||
|
|
||
| The most common side effects of COTELLIC in adults with histiocytic neoplasms include: | |||
|
|
||
Your healthcare provider will do blood tests during treatment with COTELLIC. The most common changes to blood tests include:
|
|||
| COTELLIC may cause fertility problems in males and females, which may affect your ability to have a child. Talk to your healthcare provider if this is a concern for you. These are not all of the possible side effects of COTELLIC. |
|||
| Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. | |||
| You may also report side effects to Genentech at 1-888-835-2555. | |||
How should I store COTELLIC?
|
|||
| Keep COTELLIC and all medicine out of the reach of children. | |||
| General information about the safe and effective use of COTELLIC | |||
| Medicines are sometimes prescribed for purposes other than those listed in a Patient Information Leaflet. Do not use COTELLIC for a condition for which it was not prescribed. Do not give COTELLIC to other people, even if they have the same symptoms that you have. It may harm them. You can ask your healthcare provider or pharmacist for information about COTELLIC that is written for health professionals. | |||
| What are the ingredients in COTELLIC? | |||
| Active ingredient: cobimetinib fumarate | |||
| Inactive ingredients: | |||
| Tablet Core: microcrystalline cellulose, lactose monohydrate, croscarmellose sodium, magnesium stearate | |||
| Coating: polyvinyl alcohol, titanium dioxide, polyethylene glycol 3350, talc | |||
| Distributed by: Genentech USA, Inc., A Member of the Roche Group, 1 DNA Way, South San Francisco, CA 94080-4990. | |||
| COTELLIC® is a registered trademark of Genentech, Inc. | |||
| ©2022 Genentech, Inc. All rights reserved. For more information go to www.COTELLIC.com or call 1-877-436-3683. | |||
| This Patient Information has been approved by the U.S. Food and Drug Administration. | Revised: 10/2022 | ||
| COTELLIC
cobimetinib tablet, film coated |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Genentech, Inc. (080129000) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Genentech, Inc. | 080129000 | ANALYSIS(50242-717) , API MANUFACTURE(50242-717) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| F. Hoffmann-La Roche AG | 482242971 | API MANUFACTURE(50242-717) , ANALYSIS(50242-717) , MANUFACTURE(50242-717) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| F. Hoffmann-La Roche Ltd. | 485244961 | ANALYSIS(50242-717) | |