Drug Detail:Darzalex (Daratumumab [ dar-a-toom-ue-mab ])
Drug Class: CD38 monoclonal antibodies
Highlights of Prescribing Information
DARZALEX ® (daratumumab) injection, for intravenous use
Initial U.S. Approval: 2015
Indications and Usage for Darzalex
DARZALEX is a CD38-directed cytolytic antibody indicated for the treatment of adult patients with multiple myeloma:
- in combination with lenalidomide and dexamethasone in newly diagnosed patients who are ineligible for autologous stem cell transplant and in patients with relapsed or refractory multiple myeloma who have received at least one prior therapy
- in combination with bortezomib, melphalan and prednisone in newly diagnosed patients who are ineligible for autologous stem cell transplant
- in combination with bortezomib, thalidomide, and dexamethasone in newly diagnosed patients who are eligible for autologous stem cell transplant
- in combination with bortezomib and dexamethasone in patients who have received at least one prior therapy
- in combination with carfilzomib and dexamethasone in patients with relapsed or refractory multiple myeloma who have received one to three prior lines of therapy
- in combination with pomalidomide and dexamethasone in patients who have received at least two prior therapies including lenalidomide and a proteasome inhibitor
- as monotherapy, in patients who have received at least three prior lines of therapy including a proteasome inhibitor (PI) and an immunomodulatory agent or who are double-refractory to a PI and an immunomodulatory agent. ( 1)
Darzalex Dosage and Administration
- Pre-medicate with corticosteroids, antipyretics and antihistamines. ( 2.3)
- Dilute and administer as an intravenous infusion. ( 2.5)
- Recommended dose is 16 mg/kg actual body weight. See full prescribing information for drugs used in combination and schedule ( 2.2)
- Administer post-infusion medications. ( 2.3)
Dosage Forms and Strengths
Injection:
- 100 mg/5 mL solution in a single-dose vial ( 3)
- 400 mg/20 mL solution in a single-dose vial ( 3)
Contraindications
Patients with a history of severe hypersensitivity to daratumumab or any of the components of the formulation. ( 4)
Warnings and Precautions
- Infusion-related reactions: Interrupt DARZALEX infusion for infusion-related reactions of any severity. Permanently discontinue the infusion in case of anaphylactic reactions or life-threatening infusion-related reactions and institute appropriate emergency care. ( 2.4, 5.1)
- Interference with cross-matching and red blood cell antibody screening: Type and screen patients prior to starting treatment. Inform blood banks that a patient has received DARZALEX. ( 5.2, 7.1)
- Neutropenia: Monitor complete blood cell counts periodically during treatment. Monitor patients with neutropenia for signs of infection. Dose delay may be required to allow recovery of neutrophils. ( 5.3)
- Thrombocytopenia: Monitor complete blood cell counts periodically during treatment. Dose delay may be required to allow recovery of platelets. ( 5.4)
- Embryo-Fetal Toxicity: Can cause fetal harm. Advise pregnant women of the potential risk to a fetus and advise females of reproductive potential to use effective contraception ( 5.6, 8.1, 8.3).
Adverse Reactions/Side Effects
The most frequently reported adverse reactions (incidence ≥20%) are: upper respiratory infection, neutropenia, infusion-related reactions, thrombocytopenia, diarrhea, constipation, anemia, peripheral sensory neuropathy, fatigue, peripheral edema, nausea, cough, pyrexia, dyspnea, and asthenia. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Janssen Biotech, Inc. at 1-800-526-7736 (1-800-JANSSEN) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 1/2023
Full Prescribing Information
1. Indications and Usage for Darzalex
DARZALEX is indicated for the treatment of adult patients with multiple myeloma:
- in combination with lenalidomide and dexamethasone in newly diagnosed patients who are ineligible for autologous stem cell transplant and in patients with relapsed or refractory multiple myeloma who have received at least one prior therapy.
- in combination with bortezomib, melphalan and prednisone in newly diagnosed patients who are ineligible for autologous stem cell transplant.
- in combination with bortezomib, thalidomide, and dexamethasone in newly diagnosed patients who are eligible for autologous stem cell transplant.
- in combination with bortezomib and dexamethasone in patients who have received at least one prior therapy.
- in combination with carfilzomib and dexamethasone in patients with relapsed or refractory multiple myeloma who have received one to three prior lines of therapy.
- in combination with pomalidomide and dexamethasone in patients who have received at least two prior therapies including lenalidomide and a proteasome inhibitor.
- as monotherapy, in patients who have received at least three prior lines of therapy including a proteasome inhibitor (PI) and an immunomodulatory agent or who are double-refractory to a PI and an immunomodulatory agent.
2. Darzalex Dosage and Administration
2.1 Important Dosing Information
- Administer pre-infusion and post-infusion medications [see Dosage and Administration (2.3)] .
- Administer only as an intravenous infusion after dilution in 0.9% Sodium Chloride Injection, USP [see Dosage and Administration (2.5)].
- DARZALEX should be administered by a healthcare provider, with immediate access to emergency equipment and appropriate medical support to manage infusion-related reactions if they occur [see Warnings and Precautions (5.1)].
- Type and screen patients prior to starting DARZALEX [see Warnings and Precautions (5.2)] .
2.2 Recommended Dosage
Monotherapy and In Combination with Lenalidomide (D-Rd) or Pomalidomide (D-Pd) and Dexamethasone
The DARZALEX dosing schedule in Table 1 is for combination therapy (4-week cycle regimens) and monotherapy as follows:
- combination therapy with lenalidomide and low-dose dexamethasone for newly diagnosed patients ineligible for autologous stem cell transplant (ASCT) and in patients with relapsed/refractory multiple myeloma
- combination therapy with pomalidomide and low-dose dexamethasone for patients with relapsed/refractory multiple myeloma
- monotherapy for patients with relapsed/refractory multiple myeloma.
The recommended dose of DARZALEX is 16 mg/kg actual body weight administered as an intravenous infusion according to the following dosing schedule:
| Weeks | Schedule |
|---|---|
|
|
| Weeks 1 to 8 | weekly (total of 8 doses) |
| Weeks 9 to 24 * | every two weeks (total of 8 doses) |
| Week 25 onwards until disease progression † | every four weeks |
For dosing instructions of combination agents administered with DARZALEX, see Clinical Studies (14) and manufacturer's prescribing information.
In Combination with Bortezomib, Melphalan and Prednisone (D-VMP)
The DARZALEX dosing schedule in Table 2 is for combination therapy with bortezomib, melphalan and prednisone (6-week cycle regimen) for patients with newly diagnosed multiple myeloma ineligible for ASCT.
The recommended dose of DARZALEX is 16 mg/kg actual body weight administered as an intravenous infusion according to the following dosing schedule:
| Weeks | Schedule |
|---|---|
|
|
| Weeks 1 to 6 | weekly (total of 6 doses) |
| Weeks 7 to 54 * | every three weeks (total of 16 doses) |
| Week 55 onwards until disease progression † | every four weeks |
For dosing instructions of combination agents administered with DARZALEX see Clinical Studies (14.1).
In Combination with Bortezomib, Thalidomide and Dexamethasone (D-VTd)
The DARZALEX dosing schedule in Table 3 is for combination therapy with bortezomib, thalidomide, and dexamethasone (4-week cycle regimen) for patients with newly diagnosed multiple myeloma eligible for ASCT.
The recommended dose of DARZALEX is 16 mg/kg actual body weight administered as an intravenous infusion according to the following dosing schedule:
| Treatment phase | Weeks | Schedule |
|---|---|---|
|
||
| Induction | Weeks 1 to 8 | weekly (total of 8 doses) |
| Weeks 9 to 16 * | every two weeks (total of 4 doses) | |
| Stop for high dose chemotherapy and ASCT | ||
| Consolidation | Weeks 1 to 8 † | every two weeks (total of 4 doses) |
For dosing instructions of combination agents administered with DARZALEX, see Clinical Studies (14.1) and the manufacturer's prescribing information.
In Combination with Bortezomib and Dexamethasone (D-Vd)
The DARZALEX dosing schedule in Table 4 is for combination therapy with bortezomib and dexamethasone (3-week cycle) for patients with relapsed/refractory multiple myeloma.
The recommended dose of DARZALEX is 16 mg/kg actual body weight administered as an intravenous infusion according to the following dosing schedule:
| Weeks | Schedule |
|---|---|
|
|
| Weeks 1 to 9 | weekly (total of 9 doses) |
| Weeks 10 to 24 * | every three weeks (total of 5 doses) |
| Week 25 onwards until disease progression † | every four weeks |
For dosing instructions of combination agents administered with DARZALEX see Clinical Studies (14.2) and manufacturer's prescribing information .
In Combination with Carfilzomib and Dexamethasone (DKd)
The recommended dosage for DARZALEX when administered in combination with carfilzomib and dexamethasone (4-week cycle) for patients with relapsed/refractory multiple myeloma is provided in Table 5.
| Weeks | DARZALEX Dose * | Schedule |
|---|---|---|
|
||
| Week 1 | 8 mg/kg | days 1 and 2 (total 2 doses) |
| Weeks 2 to 8 | 16 mg/kg | weekly (total of 7 doses) |
| Weeks 9 to 24 † | 16 mg/kg | every two weeks (total of 8 doses) |
| Week 25 onwards until disease progression ‡ | 16 mg/kg | every four weeks |
For dosing instructions of combination agents administered with DARZALEX see Clinical Studies (14.1) and manufacturer's prescribing information .
Infusion Rates
Administer DARZALEX intravenously at the infusion rate described below in Table 6. Consider incremental escalation of the infusion rate only in the absence of infusion-related reactions.
The recommended dose of 16 mg/kg to be administered on Day 1 when DARZALEX is administered as monotherapy or in combination may be split over two consecutive days, such that an 8 mg/kg dose is administered on Day 1 and Day 2, respectively.
| Dilution volume | Initial rate (first hour) | Rate increment * | Maximum rate | |
|---|---|---|---|---|
|
||||
| Week 1 Infusion | ||||
| Option 1 (Single dose infusion) | ||||
| Week 1 Day 1 (16 mg/kg) | 1,000 mL | 50 mL/hour | 50 mL/hour every hour | 200 mL/hour |
| Option 2 (Split dose infusion) | ||||
| Week 1 Day 1 (8 mg/kg) | 500 mL | 50 mL/hour | 50 mL/hour every hour | 200 mL/hour |
| Week 1 Day 2 (8 mg/kg) | 500 mL | 50 mL/hour | 50 mL/hour every hour | 200 mL/hour |
| Week 2 (16 mg/kg)† | 500 mL | 50 mL/hour | 50 mL/hour every hour | 200 mL/hour |
| Week 3 onwards (16 mg/kg)‡ | 500 mL | 100 mL/hour | 50 mL/hour every hour | 200 mL/hour |
2.4 Dosage Modifications for Adverse Reactions
No dose reductions of DARZALEX are recommended. Consider withholding DARZALEX to allow recovery of blood cell counts in the event of myelosuppression [see Warnings and Precautions (5.3, 5.4)] .
For information concerning drugs given in combination with DARZALEX, see manufacturer's prescribing information.
3. Dosage Forms and Strengths
DARZALEX is a colorless to pale yellow, preservative-free solution available as:
Injection:
- 100 mg/5 mL (20 mg/mL) in a single-dose vial.
- 400 mg/20 mL (20 mg/mL) in a single-dose vial.
4. Contraindications
DARZALEX is contraindicated in patients with a history of severe hypersensitivity (e.g. anaphylactic reactions) to daratumumab or any of the components of the formulation [see Warnings and Precautions (5.1)] .
5. Warnings and Precautions
5.1 Infusion-Related Reactions
DARZALEX can cause severe and/or serious infusion-related reactions including anaphylactic reactions. These reactions can be life-threatening and fatal outcomes have been reported [see Adverse Reactions (6.3)] .
In clinical trials (monotherapy and combination: N=2,066), infusion-related reactions occurred in 37% of patients with the Week 1 (16 mg/kg) infusion, 2% with the Week 2 infusion, and cumulatively 6% with subsequent infusions. Less than 1% of patients had a Grade 3/4 infusion-related reaction at Week 2 or subsequent infusions. The median time to onset was 1.5 hours (range: 0 to 73 hours). The incidence of infusion modification due to reactions was 36%. Median durations of 16 mg/kg infusions for the Week 1, Week 2, and subsequent infusions were approximately 7, 4, and 3 hours respectively. Nearly all reactions occurred during infusion or within 4 hours of completing DARZALEX. Prior to the introduction of post-infusion medication in clinical trials, infusion-related reactions occurred up to 48 hours after infusion.
Severe reactions have occurred, including bronchospasm, hypoxia, dyspnea, hypertension, tachycardia, headache, laryngeal edema, pulmonary edema, and ocular adverse reactions, including choroidal effusion, acute myopia, and acute angle closure glaucoma. Signs and symptoms may include respiratory symptoms, such as nasal congestion, cough, throat irritation, as well as chills, vomiting and nausea. Less common signs and symptoms were wheezing, allergic rhinitis, pyrexia, chest discomfort, pruritus, hypotension, and blurred vision [see Adverse Reactions (6.1)] .
When DARZALEX dosing was interrupted in the setting of ASCT (CASSIOPEIA) for a median of 3.75 months (range: 2.4 to 6.9 months), upon re-initiation of DARZALEX, the incidence of infusion-related reactions was 11% for the first infusion following ASCT. Infusion rate/dilution volume used upon re-initiation was that used for the last DARZALEX infusion prior to interruption for ASCT. Infusion-related reactions occurring at re-initiation of DARZALEX following ASCT were consistent in terms of symptoms and severity (Grade 3 or 4: <1%) with those reported in previous studies at Week 2 or subsequent infusions.
In EQUULEUS, patients receiving combination treatment (n=97) were administered the first 16 mg/kg dose at Week 1 split over two days i.e. 8 mg/kg on Day 1 and Day 2, respectively. The incidence of any grade infusion-related reactions was 42%, with 36% of patients experiencing infusion-related reactions on Day 1 of Week 1, 4% on Day 2 of Week 1, and 8% with subsequent infusions. The median time to onset of a reaction was 1.8 hours (range: 0.1 to 5.4 hours). The incidence of infusion interruptions due to reactions was 30%. Median durations of infusions were 4.2 hours for Week 1-Day 1, 4.2 hours for Week 1-Day 2, and 3.4 hours for the subsequent infusions.
Pre-medicate patients with antihistamines, antipyretics and corticosteroids. Frequently monitor patients during the entire infusion [see Dosage and Administration (2.3)] . Interrupt DARZALEX infusion for reactions of any severity and institute medical management as needed. Permanently discontinue DARZALEX therapy if an anaphylactic reaction or life-threatening (Grade 4) reaction occurs and institute appropriate emergency care. For patients with Grade 1, 2, or 3 reactions, reduce the infusion rate when re-starting the infusion [see Dosage and Administration (2.4)] .
To reduce the risk of delayed infusion-related reactions, administer oral corticosteroids to all patients following DARZALEX infusions [see Dosage and Administration (2.3)] . Patients with a history of chronic obstructive pulmonary disease may require additional post-infusion medications to manage respiratory complications. Consider prescribing short- and long-acting bronchodilators and inhaled corticosteroids for patients with chronic obstructive pulmonary disease [see Dosage and Administration (2.3)] .
Ocular adverse reactions, including acute myopia and narrowing of the anterior chamber angle due to ciliochoroidal effusions with potential for increased intraocular pressure or glaucoma, have occurred with DARZALEX infusion. If ocular symptoms occur, interrupt DARZALEX infusion and seek immediate ophthalmologic evaluation prior to restarting DARZALEX.
5.2 Interference with Serological Testing
Daratumumab binds to CD38 on red blood cells (RBCs) and results in a positive Indirect Antiglobulin Test (Indirect Coombs test). Daratumumab-mediated positive indirect antiglobulin test may persist for up to 6 months after the last daratumumab infusion. Daratumumab bound to RBCs masks detection of antibodies to minor antigens in the patient's serum [see References (15)] . The determination of a patient's ABO and Rh blood type are not impacted [see Drug Interactions (7.1)] .
Notify blood transfusion centers of this interference with serological testing and inform blood banks that a patient has received DARZALEX. Type and screen patients prior to starting DARZALEX [see Dosage and Administration (2.1)] .
5.3 Neutropenia
DARZALEX may increase neutropenia induced by background therapy [see Adverse Reactions (6.1)].
Monitor complete blood cell counts periodically during treatment according to manufacturer's prescribing information for background therapies. Monitor patients with neutropenia for signs of infection. Consider withholding DARZALEX until recovery of neutrophils.
5.4 Thrombocytopenia
DARZALEX may increase thrombocytopenia induced by background therapy [see Adverse Reactions (6.1)].
Monitor complete blood cell counts periodically during treatment according to manufacturer's prescribing information for background therapies. Consider withholding DARZALEX until recovery of platelets.
5.5 Interference with Determination of Complete Response
Daratumumab is a human IgG kappa monoclonal antibody that can be detected on both, the serum protein electrophoresis (SPE) and immunofixation (IFE) assays used for the clinical monitoring of endogenous M-protein [see Drug Interactions (7.1)] . This interference can impact the determination of complete response and of disease progression in some patients with IgG kappa myeloma protein.
5.6 Embryo-Fetal Toxicity
Based on the mechanism of action, DARZALEX can cause fetal harm when administered to a pregnant woman. DARZALEX may cause depletion of fetal immune cells and decreased bone density. Advise pregnant women of the potential risk to a fetus. Advise females with reproductive potential to use effective contraception during treatment with DARZALEX and for 3 months after the last dose [see Use in Specific Populations (8.1, 8.3)] .
The combination of DARZALEX with lenalidomide, pomalidomide, or thalidomide is contraindicated in pregnant women, because lenalidomide, pomalidomide, and thalidomide may cause birth defects and death of the unborn child. Refer to the lenalidomide, pomalidomide, or thalidomide prescribing information on use during pregnancy.
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Infusion-related reactions [see Warning and Precautions (5.1)] .
- Neutropenia [see Warning and Precautions (5.3)] .
- Thrombocytopenia [see Warning and Precautions (5.4)] .
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety data described below reflects exposure to DARZALEX (16 mg/kg) in 2,459 patients with multiple myeloma including 2,303 patients who received DARZALEX in combination with background regimens and 156 patients who received DARZALEX as monotherapy. In this pooled safety population, the most common adverse reactions (≥20%) were upper respiratory infection, neutropenia, infusion-related reactions, thrombocytopenia, diarrhea, constipation, anemia, peripheral sensory neuropathy, fatigue, peripheral edema, nausea, cough, pyrexia, dyspnea, and asthenia.
Newly Diagnosed Multiple Myeloma Ineligible for Autologous Stem Cell Transplant
Combination Treatment with Lenalidomide and Dexamethasone (DRd)
The safety of DARZALEX in combination with lenalidomide and dexamethasone was evaluated in MAIA [see Clinical Studies (14.1)]. Adverse reactions described in Table 7 reflect exposure to DARZALEX for a median treatment duration of 25.3 months (range: 0.1 to 40.44 months) for daratumumab-lenalidomide-dexamethasone (DRd) and of 21.3 months (range: 0.03 to 40.64 months) for lenalidomide-dexamethasone (Rd).
Serious adverse reactions with a 2% greater incidence in the DRd arm compared to the Rd arm were pneumonia (DRd 15% vs Rd 8%), bronchitis (DRd 4% vs Rd 2%) and dehydration (DRd 2% vs Rd <1%).
| Body System
Adverse Reaction | DRd (N=364) | Rd (N=365) | ||||
|---|---|---|---|---|---|---|
| All Grades (%) | Grade 3 (%) | Grade 4 (%) | All Grades (%) | Grade 3 (%) | Grade 4 (%) | |
| Key: D=daratumumab, Rd=lenalidomide-dexamethasone. | ||||||
|
||||||
| Gastrointestinal disorders | ||||||
| Diarrhea | 57 | 7 | 0 | 46 | 4 | 0 |
| Constipation | 41 | 1 | <1 | 36 | <1 | 0 |
| Nausea | 32 | 1 | 0 | 23 | 1 | 0 |
| Vomiting | 17 | 1 | 0 | 12 | <1 | 0 |
| Infections | ||||||
| Upper respiratory tract infection * | 52 | 2 | <1 | 36 | 2 | <1 |
| Bronchitis † | 29 | 3 | 0 | 21 | 1 | 0 |
| Pneumonia ‡ | 26 | 14 | 1 | 14 | 7 | 1 |
| Urinary tract infection | 18 | 2 | 0 | 10 | 2 | 0 |
| General disorders and administration site conditions | ||||||
| Infusion-related reactions § | 41 | 2 | <1 | 0 | 0 | 0 |
| Peripheral edema ¶ | 41 | 2 | 0 | 33 | 1 | 0 |
| Fatigue | 40 | 8 | 0 | 28 | 4 | 0 |
| Asthenia | 32 | 4 | 0 | 25 | 3 | <1 |
| Pyrexia | 23 | 2 | 0 | 18 | 2 | 0 |
| Chills | 13 | 0 | 0 | 2 | 0 | 0 |
| Musculoskeletal and connective tissue disorders | ||||||
| Back pain | 34 | 3 | <1 | 26 | 3 | <1 |
| Muscle spasms | 29 | 1 | 0 | 22 | 1 | 0 |
| Respiratory, thoracic and mediastinal disorders | ||||||
| Dyspnea # | 32 | 3 | <1 | 20 | 1 | 0 |
| Cough Þ | 30 | <1 | 0 | 18 | 0 | 0 |
| Nervous system disorders | ||||||
| Peripheral sensory neuropathy | 24 | 1 | 0 | 15 | 0 | 0 |
| Headache | 19 | 1 | 0 | 11 | 0 | 0 |
| Paresthesia | 16 | 0 | 0 | 8 | 0 | 0 |
| Metabolism and nutrition disorders | ||||||
| Decreased appetite | 22 | 1 | 0 | 15 | <1 | <1 |
| Hyperglycemia | 14 | 6 | 1 | 8 | 3 | 1 |
| Hypocalcemia | 14 | 1 | <1 | 9 | 1 | 1 |
| Vascular disorders | ||||||
| Hypertension ß | 13 | 6 | <1 | 7 | 4 | 0 |
Laboratory abnormalities worsening during treatment from baseline listed in Table 8.
| DRd (N=364) | Rd (N=365) | |||||
|---|---|---|---|---|---|---|
| All Grades
(%) | Grade 3
(%) | Grade 4
(%) | All Grades
(%) | Grade 3
(%) | Grade 4
(%) |
|
| Key: D=daratumumab, Rd=lenalidomide-dexamethasone. | ||||||
| Leukopenia | 90 | 30 | 5 | 82 | 20 | 4 |
| Neutropenia | 91 | 39 | 17 | 77 | 28 | 11 |
| Lymphopenia | 84 | 41 | 11 | 75 | 36 | 6 |
| Thrombocytopenia | 67 | 6 | 3 | 58 | 7 | 4 |
| Anemia | 47 | 13 | 0 | 57 | 24 | 0 |
Combination Treatment with Bortezomib, Melphalan and Prednisone
The safety of DARZALEX in combination with bortezomib, melphalan and prednisone was evaluated in ALCYONE [see Clinical Studies (14.1)]. Adverse reactions described in Table 9 reflect exposure to DARZALEX for a median treatment duration of 14.7 months (range: 0 to 25.8 months) for daratumumab, bortezomib, melphalan and prednisone (D-VMP) and of 12 months (range: 0.1 to 14.9 months) for VMP.
Serious adverse reactions with at least a 2% greater incidence in the D-VMP arm compared to the VMP arm were pneumonia (D-VMP 11% vs VMP 4%), upper respiratory tract infection (D-VMP 5% vs VMP 1%), and pulmonary edema (D-VMP 2% vs VMP 0%).
| Body System
Adverse Reaction | D-VMP (N=346) | VMP (N=354) | ||||
|---|---|---|---|---|---|---|
| All Grades (%) | Grade 3 (%) | Grade 4 (%) | All Grades (%) | Grade 3 (%) | Grade 4 (%) | |
| Key: D=daratumumab, VMP=bortezomib-melphalan-prednisone | ||||||
|
||||||
| Infections | ||||||
| Upper respiratory tract infection * | 48 | 5 | 0 | 28 | 3 | 0 |
| Pneumonia † | 16 | 12 | < 1 | 6 | 5 | < 1 |
| General disorders and administration site conditions | ||||||
| Infusion-related reactions ‡ | 28 | 4 | 1 | 0 | 0 | 0 |
| Peripheral edema § | 21 | 1 | < 1 | 14 | 1 | 0 |
| Respiratory, thoracic and mediastinal disorders | ||||||
| Cough ¶ | 16 | < 1 | 0 | 8 | < 1 | 0 |
| Dyspnea # | 13 | 2 | 1 | 5 | 1 | 0 |
| Vascular disorders | ||||||
| Hypertension Þ | 10 | 4 | < 1 | 3 | 2 | 0 |
Laboratory abnormalities worsening during treatment from baseline listed in Table 10.
| D-VMP (N=346) | VMP (N=354) | |||||
|---|---|---|---|---|---|---|
| All Grades
(%) | Grade 3
(%) | Grade 4
(%) | All Grades
(%) | Grade 3
(%) | Grade 4
(%) |
|
| Key: D=daratumumab, VMP=bortezomib-melphalan-prednisone | ||||||
| Thrombocytopenia | 88 | 27 | 11 | 88 | 26 | 16 |
| Neutropenia | 86 | 34 | 10 | 87 | 32 | 11 |
| Lymphopenia | 85 | 46 | 12 | 83 | 44 | 9 |
| Anemia | 47 | 18 | 0 | 50 | 21 | 0 |
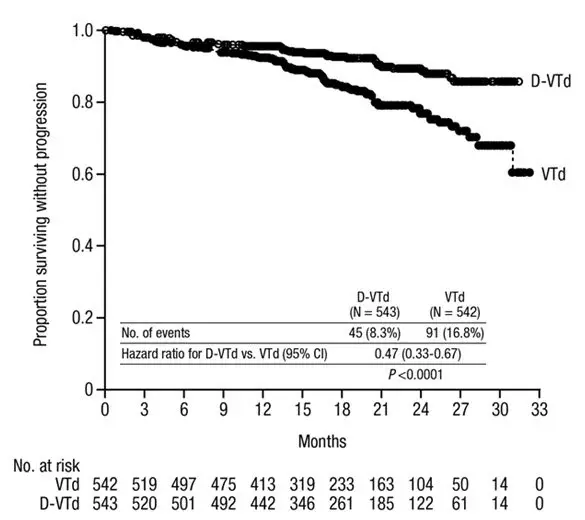
Newly Diagnosed Multiple Myeloma Eligible for Autologous Stem Cell Transplant
Combination Treatment with Bortezomib, Thalidomide and Dexamethasone (DVTd)
The safety of DARZALEX in combination with bortezomib, thalidomide and dexamethasone was evaluated in CASSIOPEIA [see Clinical Studies (14.1)]. Adverse reactions described in Table 11 reflect exposure to DARZALEX up to day 100 post-transplant. The median duration of induction/ASCT/consolidation treatment was 8.9 months (range: 7.0 to 12.0 months) for DVTd and 8.7 months (range: 6.4 to 11.5 months) for VTd.
Serious adverse reactions with a 2% greater incidence in the DVTd arm compared to the VTd arm were bronchitis (DVTd 2% vs VTd <1%) and pneumonia (DVTd 6% vs VTd 4%).
| Body System
Adverse Reaction | DVTd (N=536) | VTd (N=538) | ||||
|---|---|---|---|---|---|---|
| All Grades (%) | Grade 3 (%) | Grade 4 (%) | All Grades (%) | Grade 3 (%) | Grade 4 (%) | |
| Key: D=daratumumab, VTd=bortezomib-thalidomide -dexamethasone.
Note: Hematology laboratory related toxicities were excluded and reported separately in the table below |
||||||
|
||||||
| General disorders and administration site conditions | ||||||
| Infusion-related reactions * | 35 | 3 | <1 | 0 | 0 | 0 |
| Pyrexia | 26 | 2 | <1 | 21 | 2 | 0 |
| Gastrointestinal disorders | ||||||
| Nausea | 30 | 4 | 0 | 24 | 2 | <1 |
| Vomiting | 16 | 2 | 0 | 10 | 2 | 0 |
| Infections | ||||||
| Upper respiratory tract infection † | 27 | 1 | 0 | 17 | 1 | 0 |
| Bronchitis ‡ | 20 | 1 | 0 | 13 | 1 | 0 |
| Respiratory, thoracic and mediastinal disorders | ||||||
| Cough § | 17 | 0 | 0 | 9 | 0 | 0 |
| Vascular disorders | ||||||
| Hypertension | 10 | 4 | 0 | 5 | 2 | 0 |
| DVTd (N=536) | VTd (N=538) | |||||
|---|---|---|---|---|---|---|
| All Grades
(%) | Grade 3
(%) | Grade 4
(%) | All Grades
(%) | Grade 3
(%) | Grade 4
(%) |
|
| Key: D=daratumumab, VTd=bortezomib-thalidomide -dexamethasone. | ||||||
| Lymphopenia | 95 | 44 | 15 | 91 | 37 | 10 |
| Leukopenia | 82 | 14 | 10 | 57 | 6 | 9 |
| Thrombocytopenia | 81 | 9 | 5 | 58 | 8 | 3 |
| Neutropenia | 63 | 19 | 14 | 41 | 10 | 9 |
| Anemia | 36 | 4 | 0 | 35 | 5 | 0 |
Relapsed/Refractory Multiple Myeloma
Combination Treatment with Lenalidomide and Dexamethasone
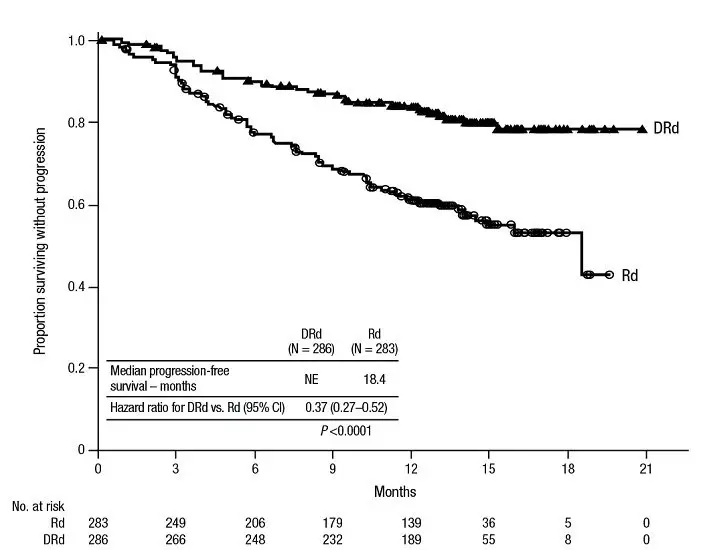
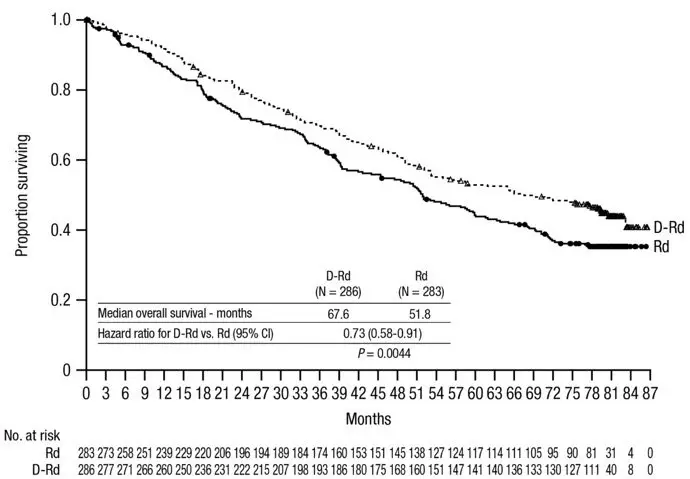
The safety of DARZALEX in combination with lenalidomide and dexamethasone was evaluated in POLLUX [see Clinical Studies (14.2)]. Adverse reactions described in Table 13 reflect exposure to DARZALEX for a median treatment duration of 13.1 months (range: 0 to 20.7 months) for daratumumab-lenalidomide-dexamethasone (DRd) and of 12.3 months (range: 0.2 to 20.1 months) for lenalidomide-dexamethasone (Rd).
Serious adverse reactions occurred in 49% of patients in the DRd arm compared with 42% in the Rd arm. Serious adverse reactions with at least a 2% greater incidence in the DRd arm compared to the Rd arm were pneumonia (DRd 12% vs Rd 10%), upper respiratory tract infection (DRd 7% vs Rd 4%), influenza and pyrexia (DRd 3% vs Rd 1% for each).
Adverse reactions resulted in discontinuations for 7% (n=19) of patients in the DRd arm versus 8% (n=22) in the Rd arm.
| Adverse Reaction | DRd (N=283) | Rd (N=281) | ||||
|---|---|---|---|---|---|---|
| All Grades
(%) | Grade 3
(%) | Grade 4
(%) | All Grades
(%) | Grade 3
(%) | Grade 4
(%) |
|
| Key: D=daratumumab, Rd=lenalidomide-dexamethasone. | ||||||
|
||||||
| Infections | ||||||
| Upper respiratory tract infection * | 65 | 6 | < 1 | 51 | 4 | 0 |
| General disorders and administration site conditions | ||||||
| Infusion-related reactions † | 48 | 5 | 0 | 0 | 0 | 0 |
| Fatigue | 35 | 6 | < 1 | 28 | 2 | 0 |
| Pyrexia | 20 | 2 | 0 | 11 | 1 | 0 |
| Gastrointestinal disorders | ||||||
| Diarrhea | 43 | 5 | 0 | 25 | 3 | 0 |
| Nausea | 24 | 1 | 0 | 14 | 0 | 0 |
| Vomiting | 17 | 1 | 0 | 5 | 1 | 0 |
| Respiratory, thoracic and mediastinal disorders | ||||||
| Cough ‡ | 30 | 0 | 0 | 15 | 0 | 0 |
| Dyspnea § | 21 | 3 | < 1 | 12 | 1 | 0 |
| Musculoskeletal and connective tissue disorders | ||||||
| Muscle spasms | 26 | 1 | 0 | 19 | 2 | 0 |
| Nervous system disorders | ||||||
| Headache | 13 | 0 | 0 | 7 | 0 | 0 |
Laboratory abnormalities worsening during treatment from baseline listed in Table 14.
| DRd (N=283) | Rd (N=281) | |||||
|---|---|---|---|---|---|---|
| All Grades
(%) | Grade 3
(%) | Grade 4
(%) | All Grades
(%) | Grade 3
(%) | Grade 4
(%) |
|
| Key: D=daratumumab, Rd=lenalidomide-dexamethasone. | ||||||
| Lymphopenia | 95 | 42 | 10 | 87 | 32 | 6 |
| Neutropenia | 92 | 36 | 17 | 87 | 32 | 8 |
| Thrombocytopenia | 73 | 7 | 6 | 67 | 10 | 5 |
| Anemia | 52 | 13 | 0 | 57 | 19 | 0 |
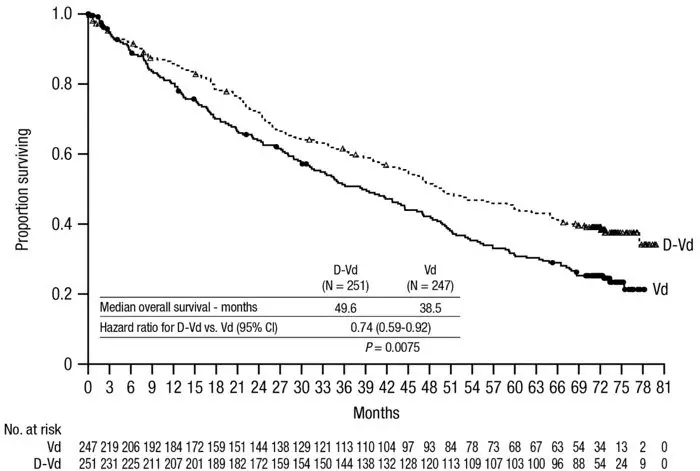
Combination Treatment with Bortezomib and Dexamethasone
The safety of DARZALEX in combination with bortezomib and dexamethasone was evaluated in CASTOR [see Clinical Studies (14.2)]. Adverse reactions described in Table 15 reflect exposure to DARZALEX for a median treatment duration of 6.5 months (range: 0 to 14.8 months) for daratumumab-bortezomib-dexamethasone (DVd) and of 5.2 months (range: 0.2 to 8.0 months) for bortezomib-dexamethasone (Vd) arm.
Serious adverse reactions occurred in 42% of patients in the DVd arm compared with 34% in the Vd arm. Serious adverse reactions with at least a 2% greater incidence in the DVd arm compared to the Vd arm were upper respiratory tract infection (DVd 5% vs Vd 2%), diarrhea and atrial fibrillation (DVd 2% vs Vd 0% for each).
Adverse reactions resulted in discontinuations for 7% (n=18) of patients in the DVd arm versus 9% (n=22) in the Vd arm.
| Adverse Reaction | DVd (N=243) | Vd (N=237) | ||||
|---|---|---|---|---|---|---|
| All Grades
(%) | Grade 3
(%) | Grade 4
(%) | All Grades
(%) | Grade 3
(%) | Grade 4
(%) |
|
| Key: D=daratumumab, Vd=bortezomib-dexamethasone. | ||||||
|
||||||
| Nervous system disorders | ||||||
| Peripheral sensory neuropathy | 47 | 5 | 0 | 38 | 6 | < 1 |
| General disorders and administration site conditions | ||||||
| Infusion-related reactions * | 45 | 9 | 0 | 0 | 0 | 0 |
| Peripheral edema † | 22 | 1 | 0 | 13 | 0 | 0 |
| Pyrexia | 16 | 1 | 0 | 11 | 1 | 0 |
| Infections | ||||||
| Upper respiratory tract infection ‡ | 44 | 6 | 0 | 30 | 3 | < 1 |
| Gastrointestinal disorders | ||||||
| Diarrhea | 32 | 3 | < 1 | 22 | 1 | 0 |
| Vomiting | 11 | 0 | 0 | 4 | 0 | 0 |
| Respiratory, thoracic and mediastinal disorders | ||||||
| Cough § | 27 | 0 | 0 | 14 | 0 | 0 |
| Dyspnea ¶ | 21 | 4 | 0 | 11 | 1 | 0 |
Laboratory abnormalities worsening during treatment are listed in Table 16.
| DVd (N=243) | Vd (N=237) | |||||
|---|---|---|---|---|---|---|
| All Grades
(%) | Grade 3
(%) | Grade 4
(%) | All Grades
(%) | Grade 3
(%) | Grade 4
(%) |
|
| Key: D=daratumumab, Vd=bortezomib-dexamethasone. | ||||||
| Thrombocytopenia | 90 | 28 | 19 | 85 | 22 | 13 |
| Lymphopenia | 89 | 41 | 7 | 81 | 24 | 3 |
| Neutropenia | 58 | 12 | 3 | 40 | 5 | < 1 |
| Anemia | 48 | 13 | 0 | 56 | 14 | 0 |
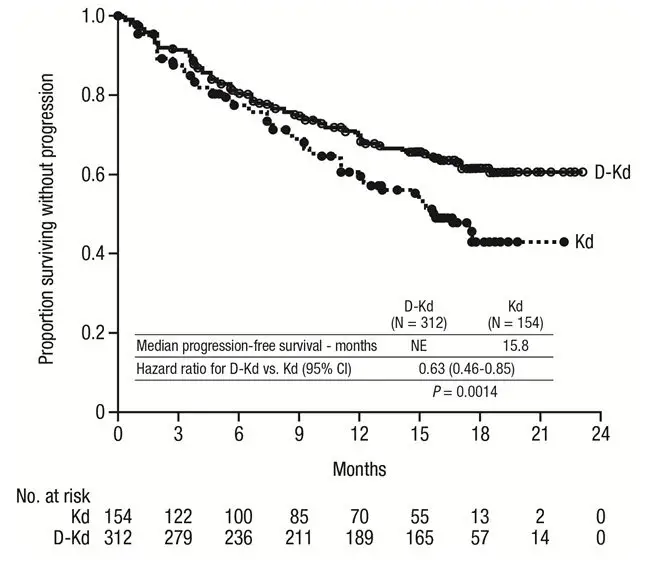
Combination Treatment with Twice-Weekly (20/56 mg/m 2) Carfilzomib and Dexamethasone
The safety of DARZALEX in combination with twice weekly carfilzomib and dexamethasone was evaluated in CANDOR [see Clinical Studies (14.2)] . Adverse reactions described in Table 17 reflect exposure to DARZALEX for a median treatment duration of 16.1 months (range: 0.1 to 23.7 months) for the daratumumab-carfilzomib-dexamethasone (DKd) group and median treatment duration of 9.3 months (range: 0.1 to 22.4 months) for the carfilzomib-dexamethasone group (Kd).
Serious adverse reactions occurred in 56% of patients who received DARZALEX in combination with Kd and 46% of patients who received Kd. The most frequent serious adverse reactions reported in the DKd arm as compared with the Kd arm were pneumonia (DKd 14% vs Kd 9%), pyrexia (DKd 4.2% vs Kd 2.0%), influenza (DKd 3.9% vs Kd 1.3%), sepsis (DKd 3.9% vs Kd 1.3%), anemia (DKd 2.3% vs Kd 0.7%), bronchitis (DKd 1.9% vs Kd 0%), and diarrhea (DKd 1.6% vs Kd 0%). Fatal adverse reactions within 30 days of the last dose of any study treatment occurred in 10% of 308 patients who received DARZALEX in combination with Kd versus 5% of 153 patients who received Kd. The most frequent fatal adverse reaction was infection (4.5% vs 2.6%).
Permanent discontinuation of DARZALEX due to an adverse reaction occurred in 9% of patients. Adverse reactions (>1%) which resulted in permanent discontinuation of DARZALEX included pneumonia.
Infusion-related reactions that occurred on the day of administration of any DARZALEX dose or on the next day occurred in 18% of patients and that occurred on the day of administration of the first DARZALEX dose or the next day occurred in 12%.
| Adverse Reaction | DKd (N=308) | Kd (N=153) | ||
|---|---|---|---|---|
| All Grades | Grades 3 or 4 | All Grades | Grades 3 or 4 | |
| (%) | (%) | (%) | (%) | |
| Key: D=daratumumab; Kd=carfilzomib-dexamethasone | ||||
|
||||
| General Disorders and Administration Site Conditions | ||||
| Infusion-related reactions * | 41 | 12 | 28 | 5 |
| Fatigue † | 32 | 11 | 28 | 8 |
| Pyrexia | 20 | 1.9 | 15 | 0.7 |
| Infections | ||||
| Respiratory tract infection ‡ | 40 § | 7 | 29 | 3.3 |
| Pneumonia | 18 § | 13 | 12 | 9 |
| Bronchitis | 17 | 2.6 | 12 | 1.3 |
| Blood and lymphatic system disorders | ||||
| Thrombocytopenia ¶ | 37 | 25 | 30 | 16 |
| Anemia # | 33 | 17 | 31 | 14 |
| Gastrointestinal disorders | ||||
| Diarrhea | 32 | 3.9 | 14 | 0.7 |
| Nausea | 18 | 0 | 13 | 0.7 |
| Vascular Disorders | ||||
| Hypertension | 31 | 18 | 28 | 13 |
| Respiratory, Thoracic and Mediastinal Disorders | ||||
| Cough Þ | 21 | 0 | 21 | 0 |
| Dyspnea | 20 | 3.9 | 22 | 2.6 |
| Psychiatric disorders | ||||
| Insomnia | 18 | 3.9 | 11 | 2 |
| Musculoskeletal and connective tissue disorders | ||||
| Back pain | 16 | 1.9 | 10 | 1.3 |
Combination Treatment with Once-Weekly (20/70 mg/m 2) Carfilzomib and Dexamethasone
The safety of DARZALEX in combination with once-weekly carfilzomib and dexamethasone was evaluated in EQUULEUS [see Clinical Studies (14.2)] . Adverse reactions described in Table 18 reflect exposure to DARZALEX for a median treatment duration of 19.8 months (range: 0.3 to 34.5 months).
Serious adverse reactions were reported in 48% of patients. The most frequent serious adverse reactions reported were pneumonia (4.7%), upper respiratory tract infection (4.7%), basal cell carcinoma (4.7%), influenza (3.5%), general physical health deterioration (3.5%), and hypercalcemia (3.5%). Fatal adverse reactions within 30 days of the last dose of any study treatment occurred in 3.5% of patients who died of general physical health deterioration, multi-organ failure secondary to pulmonary aspergillosis, and disease progression.
Permanent discontinuation of DARZALEX due to an adverse reaction occurred in 8% of patients. No adverse reactions which resulted in permanent discontinuation of DARZALEX occurred in more than one patient.
Infusion-related reactions that occurred on the day of administration of any DARZALEX dose or on the next day occurred in 44% of patients. For patients who received the split first dose of DARZALEX, infusion-related reactions that occurred in 36% and 4% on the first and second day of administration of DARZALEX, respectively.
| Adverse Reaction | DKd (N=85) | |
|---|---|---|
| All Grades (%) | Grades 3 or 4 (%) | |
| Key: D=daratumumab; Kd=carfilzomib-dexamethasone | ||
|
||
| Blood and lymphatic system disorders | ||
| Thrombocytopenia * | 68 | 32 |
| Anemia † | 52 | 21 |
| Neutropenia ‡ | 31 | 21 |
| Lymphopenia § | 29 | 25 |
| General disorder and administration site conditions | ||
| Fatigue ¶ | 54 | 18 |
| Infusion-related reactions # | 53 | 12 |
| Pyrexia | 37 | 1.2 |
| Infections | ||
| Respiratory tract infection Þ | 53 | 3.5 |
| Bronchitis | 19 | 0 |
| Nasopharyngitis | 18 | 0 |
| Influenza | 17 | 3.5 |
| Gastrointestinal disorders | ||
| Nausea | 42 | 1.2 |
| Vomiting | 40 | 1.2 |
| Diarrhea | 38 | 2.4 |
| Constipation | 17 | 0 |
| Respiratory, thoracic and mediastinal disorders | ||
| Dyspnea | 35 | 3.5 |
| Cough ß | 33 | 0 |
| Vascular disorders | ||
| Hypertension | 33 | 20 |
| Psychiatric disorders | ||
| Insomnia | 33 | 4.7 |
| Nervous system disorders | ||
| Headache | 27 | 1.2 |
| Musculoskeletal and connective tissue disorders | ||
| Back pain | 25 | 0 |
| Pain in extremity | 15 | 0 |
Monotherapy
The safety of DARZALEX was evaluated in 156 adult patients with relapsed and refractory multiple myeloma in three open-label, clinical trials. Patients received DARZALEX 16 mg/kg. The median duration of exposure was 3.3 months (range: 0.03 to 20.04 months).
Serious adverse reactions were reported in 51 (33%) patients. The most frequent serious adverse reactions were pneumonia (6%), general physical health deterioration (3%), and pyrexia (3%).
Adverse reactions resulted in treatment delay for 24 (15%) patients, most frequently for infections. Adverse reactions resulted in discontinuations for 6 (4%) patients.
Adverse reactions occurring in at least 10% of patients are presented in Table 21. Table 22 describes Grade 3–4 laboratory abnormalities reported at a rate of ≥10%.
| Adverse Reaction | DARZALEX
(N=156) |
||
|---|---|---|---|
| All Grades
(%) | Grade 3
(%) | Grade 4
(%) |
|
|
|||
| General disorders and administration site conditions | |||
| Infusion-related reaction * | 48 | 3 | 0 |
| Fatigue | 39 | 2 | 0 |
| Pyrexia | 21 | 1 | 0 |
| Chills | 10 | 0 | 0 |
| Gastrointestinal disorders | |||
| Nausea | 27 | 0 | 0 |
| Diarrhea | 16 | 1 | 0 |
| Constipation | 15 | 0 | 0 |
| Vomiting | 14 | 0 | 0 |
| Musculoskeletal and connective tissue disorders | |||
| Back pain | 23 | 2 | 0 |
| Arthralgia | 17 | 0 | 0 |
| Pain in extremity | 15 | 1 | 0 |
| Musculoskeletal chest pain | 12 | 1 | 0 |
| Respiratory, thoracic and mediastinal disorders | |||
| Cough | 21 | 0 | 0 |
| Nasal congestion | 17 | 0 | 0 |
| Dyspnea | 15 | 1 | 0 |
| Infections | |||
| Upper respiratory tract infection | 20 | 1 | 0 |
| Nasopharyngitis | 15 | 0 | 0 |
| Pneumonia † | 11 | 6 | 0 |
| Metabolism and nutrition disorders | |||
| Decreased appetite | 15 | 1 | 0 |
| Nervous system disorders | |||
| Headache | 12 | 1 | 0 |
| Vascular disorders | |||
| Hypertension | 10 | 5 | 0 |
| Daratumumab 16 mg/kg (N=156) | |||
|---|---|---|---|
| All Grades
(%) | Grade 3
(%) | Grade 4
(%) |
|
| Lymphopenia | 72 | 30 | 10 |
| Neutropenia | 60 | 17 | 3 |
| Thrombocytopenia | 48 | 10 | 8 |
| Anemia | 45 | 19 | 0 |
6.2 Immunogenicity
As with all therapeutic proteins, there is the potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies in the studies described below with the incidence of antibodies in other studies or to other daratumumab products may be misleading.
In clinical trials of patients with multiple myeloma treated with DARZALEX as monotherapy or as combination therapies, 0.35% (6/1,713) of patients developed treatment-emergent anti-daratumumab antibodies. Of those, 4 patients tested positive for neutralizing antibodies.
6.3 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of daratumumab. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Immune System disorders: Anaphylactic reaction, IRR (including deaths)
Gastrointestinal disorders: Pancreatitis
Infections: Cytomegalovirus, Listeriosis
8. Use In Specific Populations
8.3 Females and Males of Reproductive Potential
DARZALEX can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)] .
8.4 Pediatric Use
Safety and effectiveness of DARZALEX in pediatric patients have not been established.
8.5 Geriatric Use
Of the 2,459 patients who received DARZALEX at the recommended dose, 38% were 65 to 74 years of age, and 15% were 75 years of age or older. No overall differences in effectiveness were observed between these patients and younger patients. The incidence of serious adverse reactions was higher in older than in younger patients [see Adverse Reactions (6.1)] . Among patients with relapsed and refractory multiple myeloma (n=1,213), the serious adverse reactions that occurred more frequently in patients 65 years and older were pneumonia and sepsis. Within the DKd group in CANDOR, fatal adverse reactions occurred in 14% of patients 65 years and older compared to 6% of patients less than 65 years. Among patients with newly diagnosed multiple myeloma who are ineligible for autologous stem cell transplant (n=710), the serious adverse reaction that occurred more frequently in patients 75 years and older was pneumonia.
11. Darzalex Description
Daratumumab is an immunoglobulin G1 kappa (IgG1κ) human monoclonal antibody that binds to CD38 antigen. It is produced in Chinese Hamster Ovary (CHO) cells using recombinant DNA technology. The molecular weight of daratumumab is approximately 148 kDa.
DARZALEX ® (daratumumab) injection is supplied as a colorless to pale yellow preservative-free solution for intravenous use in a single-dose vial. The pH is 5.5.
Each DARZALEX 20 mL single-dose vial contains (NDC 57894-502-20) 400 mg daratumumab, glacial acetic acid (3.7 mg), mannitol (510 mg), polysorbate 20 (8 mg), sodium acetate trihydrate (59.3 mg), sodium chloride (70.1 mg), and Water for Injection, USP.
Each DARZALEX 5 mL single-dose vial contains (NDC 57894-502-05) 100 mg daratumumab, glacial acetic acid (0.9 mg), mannitol (127.5 mg), polysorbate 20 (2 mg), sodium acetate trihydrate (14.8 mg), sodium chloride (17.5 mg), and Water for Injection, USP.
Each DARZALEX 20 mL single-dose vial contains (NDC 57894-505-20) 400 mg daratumumab, L-histidine (7 mg), L-histidine hydrochloride monohydrate (32.6 mg), L-methionine (20 mg), polysorbate 20 (8 mg), sorbitol (1093 mg), and Water for Injection, USP.
Each DARZALEX 5 mL single-dose vial contains (NDC 57894-505-05) 100 mg daratumumab, L-histidine (1.8 mg), L-histidine hydrochloride monohydrate (8.2 mg), L-methionine (5 mg), polysorbate 20 (2 mg), sorbitol (273.3 mg), and Water for Injection, USP.
12. Darzalex - Clinical Pharmacology
12.1 Mechanism of Action
CD38 is a transmembrane glycoprotein (48 kDa) expressed on the surface of hematopoietic cells, including multiple myeloma and other cell types and tissues and has multiple functions, such as receptor mediated adhesion, signaling, and modulation of cyclase and hydrolase activity. Daratumumab is an IgG1κ human monoclonal antibody (mAb) that binds to CD38 and inhibits the growth of CD38 expressing tumor cells by inducing apoptosis directly through Fc mediated cross linking as well as by immune-mediated tumor cell lysis through complement dependent cytotoxicity (CDC), antibody dependent cell mediated cytotoxicity (ADCC) and antibody dependent cellular phagocytosis (ADCP). A subset of myeloid derived suppressor cells (CD38+MDSCs), regulatory T cells (CD38+T regs) and B cells (CD38+B regs) are decreased by daratumumab.
12.2 Pharmacodynamics
NK cells express CD38 and are susceptible to daratumumab mediated cell lysis. Decreases in absolute counts and percentages of total NK cells (CD16+CD56+) and activated (CD16+CD56 dim) NK cells in peripheral whole blood and bone marrow were observed with DARZALEX treatment.
12.3 Pharmacokinetics
Daratumumab area under the concentration-time curve (AUC) increases more than proportionally over a dosage range from 1 to 24 mg/kg (0.06 to 1.5 times the approved recommended dosage) as monotherapy or 1 to 16 mg/kg (0.06 to 1 time the approved recommended dosage) as combination therapy.
Following administration of the approved recommended dosage of DARZALEX as monotherapy or in combination therapy, the mean serum maximal concentration (C max) was approximately 2.7 to 3-fold higher at the end of weekly dosing compared to the first dose. The mean ± standard deviation (SD) trough serum concentration (C min) at the end of weekly dosing was 573 ± 332 µg/mL when DARZALEX was administered as monotherapy and 502 ± 196 to 607 ± 231 µg/mL when DARZALEX was administered as combination therapy. Split dosing of the first dose resulted in a different PK profile in the first day compared to single dosing; however, similar C max and C min concentrations were both predicted and observed following the administration of the second split dose on Week 1 Day 2.
When DARZALEX was administered as monotherapy, daratumumab steady state was achieved approximately 5 months into the every 4-week dosing period (by the 21 st infusion). At steady state, daratumumab mean ± SD accumulation ratio for C max was 1.6 ± 0.5.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenicity or genotoxicity studies have been conducted with daratumumab. No animal studies have been performed to evaluate the potential effects of daratumumab on reproduction or development, or to determine potential effects on fertility in males or females.
14. Clinical Studies
14.1 Newly Diagnosed Multiple Myeloma
Combination Treatment with Bortezomib, Melphalan and Prednisone (VMP) in Patients Ineligible for Autologous Stem Cell Transplant
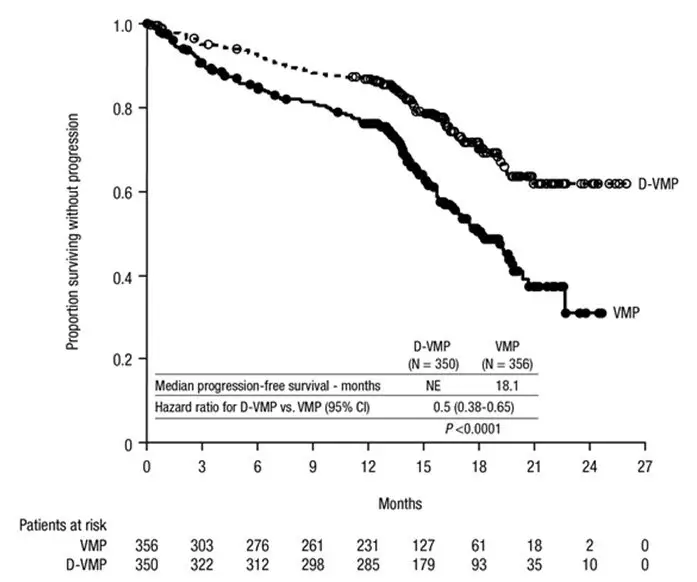
ALCYONE (NCT02195479), an open-label, randomized, active-controlled trial, compared treatment with DARZALEX 16 mg/kg in combination with bortezomib, melphalan and prednisone (D-VMP), to treatment with VMP in patients with newly diagnosed multiple myeloma ineligible for autologous stem cell transplant. Bortezomib was administered by subcutaneous (SC) injection at a dose of 1.3 mg/m 2 body surface area twice weekly at Weeks 1, 2, 4 and 5 for the first 6-week cycle (Cycle 1; 8 doses), followed by once weekly administrations at Weeks 1, 2, 4 and 5 for eight more 6-week cycles (Cycles 2–9; 4 doses per cycle). Melphalan at 9 mg/m 2, and prednisone at 60 mg/m 2 were orally administered on Days 1 to 4 of the nine 6-week cycles (Cycles 1–9). DARZALEX was continued until disease progression or unacceptable toxicity.
A total of 706 patients were randomized: 350 to the D-VMP arm and 356 to the VMP arm. The baseline demographic and disease characteristics were similar between the two treatment groups. The median age was 71 (range: 40–93) years, with 30% of the patients ≥75 years of age. The majority were white (85%), female (54%), 25% had an ECOG performance score of 0, 50% had an ECOG performance score of 1 and 25% had an ECOG performance score of 2. Nineteen percent of patients had ISS Stage I, 42% had ISS Stage II and 38% had ISS Stage III disease. Efficacy was evaluated by PFS based on IMWG criteria and overall survival (OS).
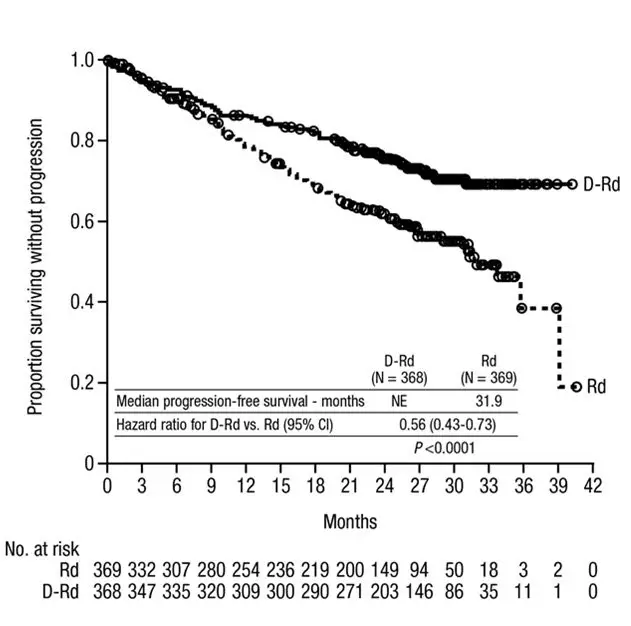
ALCYONE demonstrated an improvement in PFS in the D-VMP arm as compared to the VMP arm (HR=0.50; 95% CI: 0.38, 0.65; p<0.0001), representing a 50% reduction in the risk of disease progression or death in patients treated with D-VMP. After a median follow-up of 40 months, the median PFS was 36.4 months (95% CI: 32.1, 45.9) in the D-VMP arm and 19.3 months (95% CI: 18.0, 20.4) in the VMP arm.
|
| Figure 3: Kaplan-Meier Curve of PFS in ALCYONE* |
|
|
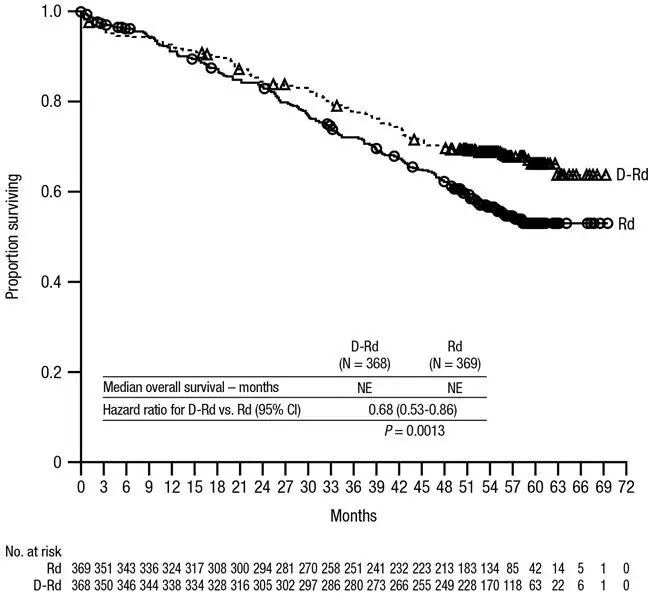
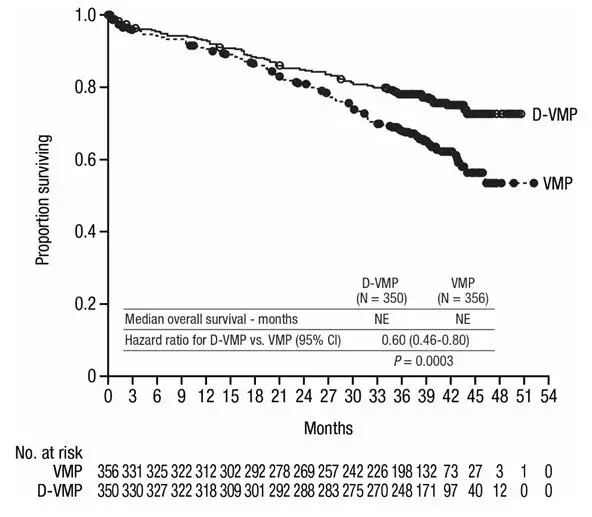
After a median follow-up of 40 months, ALCYONE demonstrated an improvement in overall survival (OS) in the D-VMP arm as compared to the VMP arm (HR=0.60; 95% CI: 0.46, 0.80; p=0.0003), representing a 40% reduction in the risk of death in patients treated in the D-VMP arm. Median OS was not reached for either arm.
Figure 4: Kaplan-Meier Curve of OS in ALCYONE
Additional efficacy results from ALCYONE are presented in Table 24.
| D-VMP (N=350) | VMP (N=356) | |
|---|---|---|
| D-VMP = daratumumab-bortezomib-melphalan-prednisone; VMP = bortezomib-melphalan-prednisone; MRD = minimal residual disease; CI = confidence interval | ||
|
||
| Overall response (sCR+CR+VGPR+PR) n(%) * | 318 (90.9%) | 263 (73.9%) |
| p-value † | <0.0001 | |
| Stringent complete response (sCR) | 63 (18.0%) | 25 (7.0%) |
| Complete response (CR) | 86 (24.6%) | 62 (17.4%) |
| Very good partial response (VGPR) | 100 (28.6%) | 90 (25.3%) |
| Partial response (PR) | 69 (19.7%) | 86 (24.2%) |
| MRD negativity rate *, ‡ n(%) | 78 (22.3%) | 22 (6.2%) |
| 95% CI (%) | (18.0, 27.0) | (3.9, 9.2) |
| p-value § | <0.0001 | |
| MRD negativity rate in patients with CR or better ‡ | ||
| Number of patients with CR or better | N=149 | N=87 |
| MRD negativity rate n(%) | 74 (49.7%) | 22 (25.3%) |
| 95% CI (%) | (41.4, 58.0) | (16.6, 35.7) |
In responders, the median time to response was 0.79 months (range: 0.4 to 15.5 months) in the D-VMP group and 0.82 months (range: 0.7 to 12.6 months) in the VMP group. The median duration of response had not been reached in the D-VMP group and was 21.3 months (range: 0.5+, 23.7+) in the VMP group.
14.2 Relapsed/Refractory Multiple Myeloma
Combination Treatment with Pomalidomide and Dexamethasone
EQUULEUS (NCT01998971) was an open-label trial in which 103 patients with multiple myeloma who had received a prior PI and an immunomodulatory agent, received 16 mg/kg DARZALEX in combination with pomalidomide and low-dose dexamethasone until disease progression. Pomalidomide (4 mg once daily orally on Days 1–21 of repeated 28-day [4-week] cycles) was given with low dose oral or intravenous dexamethasone 40 mg/week (reduced dose of 20 mg/week for patients >75 years or BMI <18.5). On DARZALEX infusion days, 20 mg of the dexamethasone dose was given as a pre-infusion medication and the remainder given the day after the infusion. For patients on a reduced dexamethasone dose, the entire 20 mg dose was given as a DARZALEX pre-infusion medication.
The median patient age was 64 years (range: 35 to 86 years) with 8% of patients ≥75 years of age. Patients in the study had received a median of 4 prior lines of therapy. Seventy-four percent (74%) of patients had received prior ASCT. Ninety-eight percent (98%) of patients received prior bortezomib treatment, and 33% of patients received prior carfilzomib. All patients received prior lenalidomide treatment, with 98% of patients previously treated with the combination of bortezomib and lenalidomide. Eighty nine percent (89%) of patients were refractory to lenalidomide and 71% refractory to bortezomib; 64% of patients were refractory to bortezomib and lenalidomide.
Efficacy results were based on overall response rate as determined by Independent Review Committee using IMWG criteria (see Table 30).
| N=103 | |
|---|---|
| ORR = sCR+CR+VGPR+PR
CI = Confidence Interval |
|
| Overall response rate (ORR) | 61 (59.2%) |
| 95% CI (%) | (49.1, 68.8) |
| Stringent complete response (sCR) | 8 (7.8%) |
| Complete response (CR) | 6 (5.8%) |
| Very good partial response (VGPR) | 29 (28.2%) |
| Partial response (PR) | 18 (17.5%) |
The median time to response was 1 month (range: 0.9 to 2.8 months). The median duration of response was 13.6 months (range: 0.9+ to 14.6+ months).
Monotherapy
SIRIUS (NCT01985126), was an open-label trial evaluating DARZALEX monotherapy in patients with relapsed or refractory multiple myeloma who had received at least 3 prior lines of therapy including a proteasome inhibitor and an immunomodulatory agent or who were double-refractory to a proteasome inhibitor and an immunomodulatory agent. In 106 patients, DARZALEX 16 mg/kg was administered with pre- and post-infusion medication. Treatment continued until unacceptable toxicity or disease progression.
The median patient age was 63.5 years (range: 31 to 84 years), 49% were male and 79% were White. Patients had received a median of 5 prior lines of therapy. Eighty percent of patients had received prior autologous stem cell transplantation (ASCT). Prior therapies included bortezomib (99%), lenalidomide (99%), pomalidomide (63%) and carfilzomib (50%). At baseline, 97% of patients were refractory to the last line of treatment, 95% were refractory to both, a proteasome inhibitor (PI) and immunomodulatory agent, and 77% were refractory to alkylating agents.
Efficacy results were based on overall response rate as determined by the Independent Review Committee assessment using IMWG criteria (see Table 31).
| N=106 | |
|---|---|
| ORR = sCR+CR+VGPR+PR
CI = confidence interval |
|
| Overall response rate (ORR) | 31 (29.2%) |
| 95% CI (%) | (20.8, 38.9) |
| Stringent complete response (sCR) | 3 (2.8%) |
| Complete response (CR) | 0 |
| Very good partial response (VGPR) | 10 (9.4%) |
| Partial response (PR) | 18 (17.0%) |
The median time to response was 1 month (range: 0.9 to 5.6 months). The median duration of response was 7.4 months (range: 1.2 to 13.1+ months).
Study GEN501 (NCT00574288) was an open-label dose escalation trial evaluating DARZALEX monotherapy in patients with relapsed or refractory multiple myeloma who had received at least 2 different cytoreductive therapies. In 42 patients, DARZALEX 16 mg/kg was administered with pre- and post-infusion medication. Treatment continued until unacceptable toxicity or disease progression.
The median patient age was 64 years (range: 44 to 76 years), 64% were male and 76% were White. Patients in the study had received a median of 4 prior lines of therapy. Seventy-four percent of patients had received prior ASCT. Prior therapies included bortezomib (100%), lenalidomide (95%), pomalidomide (36%) and carfilzomib (19%). At baseline, 76% of patients were refractory to the last line of treatment, 64% of patients were refractory to both, a PI and an immunomodulatory agent, and 60% of patients were refractory to alkylating agents.
Overall response rate was 36% (95% CI: 21.6, 52.0%) with 1 CR and 3 VGPR. The median time to response was 1 month (range: 0.5 to 3.2 months). The median duration of response was not estimable (range: 2.2 to 13.1+ months).
15. References
- Chapuy, CI, RT Nicholson, MD Aguad, et al., 2015, Resolving the daratumumab interference with blood compatibility testing, Transfusion, 55:1545–1554 (accessible at http://onlinelibrary.wiley.com/doi/10.1111/trf.13069/epdf).
| DARZALEX
daratumumab injection, solution, concentrate |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| DARZALEX IV
daratumumab injection, solution, concentrate |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - Janssen Biotech, Inc. (099091753) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Cilag AG | 483237103 | manufacture(57894-502, 57894-505) , pack(57894-502, 57894-505) , label(57894-502, 57894-505) , analysis(57894-502, 57894-505) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Vetter Pharma Fertigung GmbH & Co. KG | 312670654 | manufacture(57894-502) , analysis(57894-502) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Janssen Biologics B.V. | 409612918 | analysis(57894-502, 57894-505) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Janssen Biotech, Inc. | 038978363 | analysis(57894-502, 57894-505) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Vetter Pharma Fertigung GmbH & Co. KG | 344217323 | analysis(57894-502) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Vetter Pharma Fertigung GmbH & Co. KG | 316126754 | analysis(57894-502) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Vetter Pharma Fertigung GmbH & Co. KG | 341629292 | analysis(57894-502) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Janssen Sciences Ireland Unlimited Company | 986030167 | analysis(57894-502, 57894-505) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| PPD Development Ireland Ltd. | 985036175 | analysis(57894-502) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| AndersonBrecon, Inc. | 053217022 | pack(57894-502) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Biogen, MA Inc. | 841087823 | api manufacture(57894-502) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Samsung Biologics Co, LTD | 557810567 | api manufacture(57894-502) , analysis(57894-502) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Baxter Pharmaceutical Solutions, LLC | 604719430 | manufacture(57894-502) , label(57894-502) , pack(57894-502) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| FUJIFILM Diosynth Biotechnologies Denmark ApS | 307258082 | api manufacture(57894-505) | |