Drug Detail:Doral (Quazepam [ kway-ze-pam ])
Drug Class: Benzodiazepines
Highlights of Prescribing Information
DORAL ® (quazepam) for oral use C-IV
Initial U.S. Approval: 1985
WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS; ABUSE, MISUSE, AND ADDICTION; and DEPENDENCE AND WITHDRAWAL REACTIONS
See full prescribing information for complete boxed warning.
- Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required.
- Follow patients for signs and symptoms of respiratory depression and sedation ( 5.1, 7).
- The use of benzodiazepines, including DORAL, exposes users to risks of abuse, misuse, and addiction, which can lead to overdose or death. Before prescribing DORAL and throughout treatment, assess each patient’s risk for abuse, misuse, and addiction ( 5.2).
- Abrupt discontinuation or rapid dosage reduction of DORAL after continued use may precipitate acute withdrawal reactions, which can be life-threatening. To reduce the risk of withdrawal reactions, use a gradual taper to discontinue DORAL or reduce the dosage ( 2.3, 5.3).
Recent Major Changes
| Warnings and Precautions ( 5.9) | 01/2023 |
Indications and Usage for Doral Tablets
DORAL, a gamma-aminobutyric (GABAA) agonist, is indicated for the treatment of insomnia characterized by difficulty falling asleep, frequent nocturnal awakenings, and/or early morning awakenings. ( 1)
Doral Tablets Dosage and Administration
Use the lowest dose effective for the patient:
- Recommended initial dose is 7.5 mg ( 2)
- Split the 15 mg tablet along the score line to achieve 7.5 mg dose ( 2)
- The elderly and debilitated may be more sensitive to benzodiazepines ( 2)
Dosage Forms and Strengths
15 mg functionally scored tablet, oral ( 3)
Contraindications
- Hypersensitivity to DORAL or other benzodiazepines ( 4)
- Established or suspected sleep apnea, or chronic pulmonary insufficiency ( 4)
Warnings and Precautions
- CNS depressant effects: Impaired alertness and motor coordination, including risk of daytime impairment. Caution patients against driving and other activities requiring complete mental alertness ( 5.4)
- The failure of insomnia to remit after 7 to 10 days of treatment may indicate the presence of a primary psychiatric and/or medical illness that should be evaluated. ( 5.5)
- Severe anaphylactic/anaphylactoid reactions: Angioedema and anaphylaxis have been reported. Do not rechallenge if such reactions occur. ( 5.6)
- Sleep driving and other complex behaviors while not fully awake. Risk increases with dose and concomitant CNS depressants and alcohol. Immediately evaluate any new onset behavioral changes ( 5.7)
- Worsening of depression or suicidal thinking may occur: Prescribe the least number of tablets feasible to avoid intentional overdose ( 5.8)
Adverse Reactions/Side Effects
Most common adverse reactions (>1%): drowsiness, headache, fatigue, dizziness, dry mouth, dyspepsia ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Galt Pharmaceuticals at 1-844-416-4284 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. ( 6)
Drug Interactions
- CNS Depressants: downward dose adjustment may be necessary due to additive effects ( 7)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 1/2023
Related/similar drugs
lorazepam, melatonin, zolpidem, diphenhydramine, Ativan, AmbienFull Prescribing Information
1. Indications and Usage for Doral Tablets
DORAL is indicated for the treatment of insomnia characterized by difficulty in falling asleep, frequent nocturnal awakenings, and/or early morning awakenings. The effectiveness of DORAL has been established in placebo-controlled clinical studies of 5 nights duration in acute and chronic insomnia. The sustained effectiveness of DORAL has been established in chronic insomnia in a sleep lab (polysomnographic) study of 28 nights duration. Because insomnia is often transient and intermittent, the prolonged administration of DORAL Tablets is generally not necessary or recommended. Since insomnia may be a symptom of several other disorders, the possibility that the complaint may be related to a condition for which there is a more specific treatment should be considered.
2. Doral Tablets Dosage and Administration
2.1 Dosage Recommendations
Use the lowest dose effective for the patient, as important adverse effects of DORAL are dose related. The recommended initial dose is 7.5 mg. The 7.5 mg dose can be increased to 15 mg if necessary for efficacy. The 7.5 mg dose can be achieved by splitting the 15 mg tablet along the score line.
2.3 Discontinuation or Dosage Reduction of DORAL
To reduce the risk of withdrawal reactions, use a gradual taper to discontinue DORAL or reduce the dosage. If a patient develops withdrawal reactions, consider pausing the taper or increasing the dosage to the previous tapered dosage level. Subsequently decrease the dosage more slowly [see Warnings and Precautions ( 5.3) and Drug Abuse and Dependence ( 9.3)] .
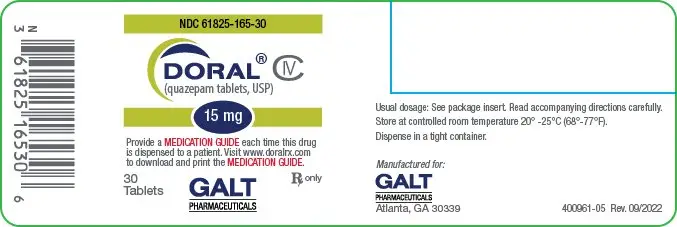
3. Dosage Forms and Strengths
Tablets, 15 mg, functionally scored, capsule-shaped, light orange, slightly white speckled tablets, impressed with the product identification number 15 on one side of the tablet, and the product name (DORAL) on the other.
4. Contraindications
DORAL is contraindicated in patients with known hypersensitivity to DORAL or other benzodiazepines. Rare cases of angioedema involving the tongue, glottis or larynx have been reported in patients after taking the first or subsequent doses of DORAL. Some patients have had additional symptoms such as dyspnea, throat closing, or nausea and vomiting that suggest anaphylaxis. Patients who develop such reactions should not be rechallenged with DORAL.
Contraindicated in patients with established or suspected sleep apnea, or with pulmonary insufficiency.
5. Warnings and Precautions
5.1 Risks from Concomitant Use with Opioids
Concomitant use of benzodiazepines, including DORAL, and opioids may result in profound sedation, respiratory depression, coma, and death. Because of these risks, reserve concomitant prescribing of these drugs in patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioids alone. If a decision is made to prescribe DORAL concomitantly with opioids, prescribe the lowest effective dosages and minimum durations of concomitant use, and follow patients closely for signs and symptoms of respiratory depression and sedation. In patients already receiving an opioid analgesic, prescribe a lower initial dose of DORAL than indicated in the absence of an opioid and titrate based on clinical response. If an opioid is initiated in a patient already taking DORAL, prescribe a lower initial dose of the opioid and titrate based upon clinical response.
Advise both patients and caregivers about the risks of respiratory depression and sedation when DORAL is used with opioids. Advise patients not to drive or operate heavy machinery until the effects of concomitant use with the opioid have been determined. [see Drug Interactions ( 7)] .
5.2 Abuse, Misuse, and Addiction
The use of benzodiazepines, including DORAL, exposes users to the risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of benzodiazepines often (but not always) involve the use of doses greater than the maximum recommended dosage and commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or death [see Drug Abuse and Dependence ( 9.2)] .
Before prescribing DORAL and throughout treatment, assess each patient’s risk for abuse, misuse, and addiction (e.g., using a standardized screening tool). Use of DORAL, particularly in patients at elevated risk, necessitates counseling about the risks and proper use of DORAL along with monitoring for signs and symptoms of abuse, misuse, and addiction. Prescribe the lowest effective dosage; avoid or minimize concomitant use of CNS depressants and other substances associated with abuse, misuse, and addiction (e.g., opioid analgesics, stimulants); and advise patients on the proper disposal of unused drug. If a substance use disorder is suspected, evaluate the patient and institute (or refer them for) early treatment, as appropriate.
5.3 Dependence and Withdrawal Reactions
To reduce the risk of withdrawal reactions, use a gradual taper to discontinue DORAL or reduce the dosage (a patient-specific plan should be used to taper the dose) [see Dosage and Administration ( 2.3)] .
Patients at an increased risk of withdrawal adverse reactions after benzodiazepine discontinuation or rapid dosage reduction include those who take higher dosages, and those who have had longer durations of use.
Acute Withdrawal Reactions
The continued use of benzodiazepines, including DORAL, may lead to clinically significant physical dependence. Abrupt discontinuation or rapid dosage reduction of DORAL after continued use, or administration of flumazenil (a benzodiazepine antagonist) may precipitate acute withdrawal reactions, which can be life-threatening (e.g., seizures)
[see Drug Abuse and Dependence (
9.3)]
.
Protracted Withdrawal Syndrome
In some cases, benzodiazepine users have developed a protracted withdrawal syndrome with withdrawal symptoms lasting weeks to more than 12 months
[see Drug Abuse and Dependence (
9.3)]
.
5.4 CNS-Depressant Effects and Daytime Impairment
DORAL is a central nervous system (CNS) depressant and can impair daytime function in some patients even when used as prescribed. Prescribers should monitor for excess depressant effects, but impairment can occur in the absence of subjective symptoms, and may not be reliably detected by ordinary clinical exam (i.e. less than formal psychomotor testing). While pharmacodynamics tolerance or adaptation to some adverse depressant effects of DORAL may develop, patients using DORAL should be cautioned against driving or engaging in other hazardous activities or activities requiring complete mental alertness.
Additive effects occur with concomitant use of other CNS depressants (e.g., other benzodiazepines, opioids, tricyclic antidepressants, alcohol), including daytime use. Downward dose adjustment of DORAL and concomitant CNS depressants should be considered. The potential for adverse drug interactions continues for several days following discontinuation of DORAL, until serum levels of both active parent drug and psychoactive metabolites decline.
Use of DORAL with other sedative-hypnotics is not recommended. Alcohol generally should not be used during treatment with DORAL. The risk of next-day psychomotor impairment is increased if DORAL is taken with less than a full night of sleep remaining (7 to 8 hours); if higher than the recommended dose is taken; if co-administered with other CNS depressants [see Dosage and Administration ( 2.1)] .
Because DORAL can cause drowsiness and a decreased level of consciousness, patients particularly the elderly, are at higher risk of falls.
5.5 Need to Evaluate for Co-morbid Diagnoses
Because sleep disturbances may be the presenting manifestation of a physical and/or psychiatric disorder, symptomatic treatment of insomnia should be initiated only after a careful evaluation of the patient. The failure of insomnia to remit after 7 to 10 days of treatment may indicate the presence of a primary psychiatric and/or medical illness that should be evaluated. Worsening of insomnia or the emergence of new thinking or behavior abnormalities may be the consequence of an unrecognized psychiatric or physical disorder. Such findings have emerged during the course of treatment with sedative-hypnotic drugs.
5.6 Severe Anaphylactic and Anaphylactoid Reactions
Rare cases of angioedema involving the tongue, glottis or larynx have been reported in patients after taking the first or subsequent doses of sedative-hypnotics, including DORAL. Some patients have had additional symptoms such as dyspnea, throat closing, or nausea and vomiting that suggest anaphylaxis.
Some patients have required medical therapy in the emergency department. If angioedema involves the tongue, glottis or larynx, airway obstruction may occur and be fatal. Patients who develop angioedema after treatment with DORAL should not be rechallenged with the drug.
5.7 Abnormal Thinking and Behavior Changes
Abnormal thinking and behavior changes have been reported in patients treated with sedative-hypnotics including DORAL. Some of these changes include decreased inhibition (e.g., aggressiveness and extroversion that seemed out of character), bizarre behavior, and depersonalization. Visual and auditory hallucinations have also been reported. Amnesia, and other neuro-psychiatric symptoms may occur.
Paradoxical reactions such as stimulation, agitation, increased muscle spasticity, and sleep disturbances may occur unpredictably.
Complex behaviors such as "sleep-driving" (i.e., driving while not fully awake, with amnesia for the event) have been reported with use of sedative-hypnotics. These behaviors can occur with initial treatment or in patients previously tolerant of DORAL or other sedative-hypnotics. Although these behaviors can occur with use at therapeutic doses, risk is increased by higher doses or concomitant use of alcohol or other CNS depressants. Due to risk to the patient and community, DORAL should be discontinued if "sleep-driving" occurs.
Other complex behaviors (e.g., preparing and eating food, making phone calls, or having sex) have been reported in patients who are not fully awake after taking a sedative-hypnotic. As with sleep-driving, patients usually do not remember these events.
5.8 Worsening of Depression
Benzodiazepines may worsen depression. Consequently, appropriate precautions (e.g., limiting the total prescription size and increased monitoring for suicidal ideation) should be considered.
5.9 Neonatal Sedation and Withdrawal Syndrome
Use of DORAL late in pregnancy can result in sedation (respiratory depression, lethargy, hypotonia) and/or withdrawal symptoms (hyperreflexia, irritability, restlessness, tremors, inconsolable crying, and feeding difficulties) in the neonate [see Use in Specific Populations ( 8.1)] . Monitor neonates exposed to DORAL during pregnancy or labor for signs of sedation and monitor neonates exposed to DORAL during pregnancy for signs of withdrawal; manage these infants accordingly.
6. Adverse Reactions/Side Effects
The following serious adverse reactions are discussed in greater detail in other sections of the label:
- Risks from Concomitant Use with Opioids [see Warnings and Precautions ( 5.1)]
- Abuse, Misuse, and Addiction [see Warnings and Precautions ( 5.2)]
- Dependence and Withdrawal Reactions [see Warnings and Precautions ( 5.3)]
- CNS-depressant effects and next-day impairment [see Warnings and Precautions ( 5.4)]
- Abnormal thinking and behavior changes, and complex behaviors [see Warnings and Precautions ( 5.7)]
- Worsening of depression [see Warnings and Precautions ( 5.8)]
- Neonatal Sedation and Withdrawal Syndrome [see Warnings and Precautions ( 5.9)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The table shows adverse reactions occurring at an incidence of 1% or greater in relatively short-duration, placebo-controlled clinical trials of DORAL.
| DORAL 15 mg | PLACEBO | |
| NUMBER OF PATIENTS | 267 | 268 |
| % OF PATIENTS REPORTING | ||
| Central Nervous System | ||
| Daytime Drowsiness | 12 | 3 |
| Headache | 5 | 2 |
| Fatigue | 2 | 0 |
| Dizziness | 2 | <1 |
| Autonomic Nervous System | ||
| Dry Mouth | 2 | <1 |
| Gastrointestinal System | ||
| Dyspepsia | 1 | <1 |
A double-blind, controlled sleep laboratory study (N=30) in elderly patients compared the effects of DORAL 7.5 mg and 15 mg to that of placebo over a period of 7 days. Both the 7.5 mg and 15 mg doses appeared to be well tolerated. Caution must be used in interpreting this data due to the small size of the study.
7. Drug Interactions
The concomitant use of benzodiazepines and opioids increases the risk of respiratory depression because of actions at different receptor sites in the CNS that control respiration. Benzodiazepines interact at GABAA sites and opioids interact primarily at mu receptors. When benzodiazepines and opioids are combined, the potential for benzodiazepines to significantly worsen opioid-related respiratory depression exists. Limit dosage and duration of concomitant use of benzodiazepines and opioids, and monitor patients closely for respiratory depression and sedation.
Benzodiazepines, including DORAL, produce additive CNS depressant effects when co-administered with ethanol or other CNS depressants (e.g. psychotropic medications, anticonvulsants, antihistamines). Downward dose adjustment of DORAL and/or concomitant CNS depressants may be necessary because of additive effects.
8. Use In Specific Populations
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy registry that monitors pregnancy outcomes in women exposed to psychiatric medications, including Doral, during pregnancy. Healthcare providers are encouraged to register patients by calling the National Pregnancy Registry for Psychiatric Medications at 1-866-961-2388 or visiting on line at https://womensmentalhealth.org/pregnancyregistry/.
Risk Summary
Infants born to mothers using benzodiazepines late in pregnancy have been reported to experience symptoms of sedation and/or neonatal withdrawal
[see Warnings and Precautions (
5.9) and
Clinical Considerations]
. Available data from published observational studies of pregnant women exposed to benzodiazepines do not report a clear association with benzodiazepines and major birth defects
(see Data).
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated risk of major birth defects and of miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Benzodiazepines cross the placenta and may produce respiratory depression, hypotonia, and sedation in neonates. Monitor neonates exposed to Doral during pregnancy or labor for signs of sedation, respiratory depression, hypotonia, and feeding problems. Monitor neonates exposed to Doral during pregnancy for signs of withdrawal. Manage these neonates accordingly
[see Warnings and Precautions (
5.9)]
.
Data
Human Data
Published data from observational studies on the use of benzodiazepines during pregnancy do not report a clear association with benzodiazepines and major birth defects. Although early studies reported an increased risk of congenital malformations with diazepam and chlordiazepoxide, there was no consistent pattern noted. In addition, the majority of more recent case-control and cohort studies of benzodiazepine use during pregnancy, which were adjusted for confounding exposures to alcohol, tobacco and other medications, have not confirmed these findings.
Animal Data
Developmental toxicity studies of DORAL in mice at doses up to 400 times the human dose (15 mg) revealed no major drug-related malformations. Minor fetal skeletal variations that occurred were delayed ossification of the sternum, vertebrae, distal phalanges and supraoccipital bones, at doses approximately 70 and 400 times the human dose. A developmental toxicity study of DORAL in New Zealand rabbits at doses up to approximately 130 times the human dose demonstrated no effect on fetal morphology or development of offspring.
8.3 Nursing Mothers
Risk Summary
Quazepam and its metabolites are present in breast milk. There are reports of sedation, poor feeding and poor weight gain in infants exposed to benzodiazepines through breast milk. The effects of quazepam on milk production are unknown. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for DORAL and any potential adverse effects on the breastfed infant from DORAL or from the underlying maternal condition.
Clinical Considerations
Infants exposed to DORAL through breast milk should be monitored for sedation, poor feeding and poor weight gain.
8.5 Geriatric Use
DORAL may cause confusion and over-sedation in the elderly. Elderly patients generally should be started on a low dose of DORAL and observed closely. Elderly and debilitated patients may be more sensitive to benzodiazepines, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. A double-blind controlled sleep laboratory study (N=30) compared the effects of DORAL 7.5 mg and 15 mg to that of placebo over a period of 7 days. Both the 7.5 mg and 15 mg doses appeared to be well tolerated. Caution must be used in interpreting this data due to the small size of the study.
9. Drug Abuse and Dependence
9.2 Abuse
DORAL is a benzodiazepine and a CNS depressant with a potential for abuse and addiction. Abuse is the intentional, nontherapeutic use of a drug, even once, for its desirable psychological or physiological effects. Misuse is the intentional use, for therapeutic purposes, of a drug by an individual in a way other than prescribed by a health care provider or for whom it was not prescribed. Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that may include a strong desire to take the drug, difficulties in controlling drug use (e.g., continuing drug use despite harmful consequences, giving a higher priority to drug use than other activities and obligations), and possible tolerance or physical dependence. Even taking benzodiazepines as prescribed may put patients at risk for abuse and misuse of their medication. Abuse and misuse of benzodiazepines may lead to addiction.
Abuse and misuse of benzodiazepines often (but not always) involve the use of doses greater than the maximum recommended dosage and commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or death. Benzodiazepines are often sought by individuals who abuse drugs and other substances, and by individuals with addictive disorders [see Warnings and Precautions ( 5.2)] .
The following adverse reactions have occurred with benzodiazepine abuse and/or misuse: abdominal pain, amnesia, anorexia, anxiety, aggression, ataxia, blurred vision, confusion, depression, disinhibition, disorientation, dizziness, euphoria, impaired concentration and memory, indigestion, irritability, muscle pain, slurred speech, tremors, and vertigo.
The following severe adverse reactions have occurred with benzodiazepine abuse and/or misuse: delirium, paranoia, suicidal ideation and behavior, seizures, coma, breathing difficulty, and death. Death is more often associated with polysubstance use (especially benzodiazepines with other CNS depressants such as opioids and alcohol).
9.3 Dependence
Physical Dependence
DORAL may produce physical dependence from continued therapy. Physical dependence is a state that develops as a result of physiological adaptation in response to repeated drug use, manifested by withdrawal signs and symptoms after abrupt discontinuation or a significant dose reduction of a drug. Abrupt discontinuation or rapid dosage reduction of benzodiazepines or administration of flumazenil, a benzodiazepine antagonist, may precipitate acute withdrawal reactions, including seizures, which can be life-threatening. Patients at an increased risk of withdrawal adverse reactions after benzodiazepine discontinuation or rapid dosage reduction include those who take higher dosages (i.e., higher and/or more frequent doses) and those who have had longer durations of use
[see Warnings and Precautions (
5.3)]
.
To reduce the risk of withdrawal reactions, use a gradual taper to discontinue DORAL or reduce the dosage [see Dosage and Administration ( 2.3) and Warnings and Precautions ( 5.3)] .
Acute Withdrawal Signs and Symptoms
Acute withdrawal signs and symptoms have included abnormal involuntary movements, anxiety, blurred vision, depersonalization, depression, derealization, dizziness, fatigue, gastrointestinal adverse reactions (e.g., nausea, vomiting, diarrhea, weight loss, decreased appetite), headache, hyperacusis, hypertension, irritability, insomnia, memory impairment, muscle pain and stiffness, panic attacks, photophobia, restlessness, tachycardia, and tremor. More severe acute withdrawal signs and symptoms, including life-threatening reactions, have included catatonia, convulsions, delirium tremens, depression, hallucinations, mania, psychosis, and suicidality.
Protracted Withdrawal Syndrome
Protracted withdrawal syndrome associated with benzodiazepines is characterized by anxiety, cognitive impairment, depression, insomnia, formication, motor symptoms (e.g., weakness, tremor, muscle twitches), paresthesia, and tinnitus that persists beyond 4 to 6 weeks after initial benzodiazepine withdrawal. Protracted withdrawal symptoms may last weeks to more than 12 months. As a result, there may be difficulty in differentiating withdrawal symptoms from potential re-emergence or continuation of symptoms for which the benzodiazepine was being used.
Tolerance
Tolerance to DORAL may develop from continued therapy. Tolerance is a physiological state characterized by a reduced response to a drug after repeated administration (i.e., a higher dose of a drug is required to produce the same effect that was once obtained at a lower dose). Tolerance may develop within days or weeks of the therapeutic effects of DORAL; however, little tolerance develops to the amnestic reactions and other cognitive impairments caused by benzodiazepines.
10. Overdosage
Overdosage of benzodiazepines is characterized by central nervous system depression ranging from drowsiness to coma. In mild to moderate cases, symptoms can include drowsiness, confusion, dysarthia, lethargy, hypnotic state, diminished reflexes, ataxia, and hypotonia. Rarely, paradoxical or disinhibitory reactions (including agitation, irritability, impulsivity, violent behavior, confusion, restlessness, excitement, and talkativeness) may occur. In severe overdosage cases, patients may develop respiratory depression and coma. Overdosage of benzodiazepines in combination with other CNS depressants (including alcohol and opioids) may be fatal [see Warnings and Precautions ( 5.2)] . Markedly abnormal (lowered or elevated) blood pressure, heart rate, or respiratory rate raise the concern that additional drugs and/or alcohol are involved in the overdosage.
In managing benzodiazepine overdosage, employ general supportive measures, including intravenous fluids and airway management. Flumazenil, a specific benzodiazepine receptor antagonist indicated for the complete or partial reversal of the sedative effects of benzodiazepines in the management of benzodiazepine overdosage, can lead to withdrawal and adverse reactions, including seizures, particularly in the context of mixed overdosage with drugs that increase seizure risk (e.g., tricyclic and tetracyclic antidepressants) and in patients with long-term benzodiazepine use and physical dependency. The risk of withdrawal seizures with flumazenil use may be increased in patients with epilepsy. Flumazenil is contraindicated in patients who have received a benzodiazepine for control of a potentially life-threatening condition (e.g., status epilepticus). If the decision is made to use flumazenil, it should be used as an adjunct to, not as a substitute for, supportive management of benzodiazepine overdosage. See the flumazenil injection Prescribing Information.
Consider contacting a poison center (1-800-222-1222) or medical toxicologist for additional overdosage management recommendations.
11. Doral Tablets Description
DORAL contains quazepam, a trifluoroethyl benzodiazepine hypnotic agent, having the chemical name 7-chloro-5- (o-fluoro-phenyl)-1,3-dihydro-1-(2,2,2- trifluoroethyl)-2H-1,4-benzodiazepine-2-thione and the following structural
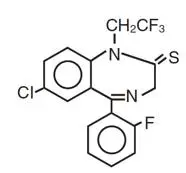
Quazepam has the empirical formula C 17H 11ClF 4N 2S, and a molecular weight of 386.8. It is a white crystalline compound, soluble in ethanol and insoluble in water.
Each DORAL Tablet contains 15 mg of quazepam. The inactive ingredients for DORAL Tablets include cellulose, corn starch, FD&C Yellow No. 6, lactose, magnesium stearate, silicon dioxide, and sodium lauryl sulfate.
12. Doral Tablets - Clinical Pharmacology
12.1 Mechanism of Action
DORAL, like other central nervous system agents of the 14-benzodiazepine class, presumably exerts its effects by binding to stereo-specific receptors at several sites within the central nervous system (CNS). The exact mechanism of action is unknown.
12.3 Pharmacokinetics
Absorption
DORAL is rapidly (absorption half-life of about 30 minutes) and well absorbed from the gastrointestinal tract. The peak plasma concentration of quazepam is approximately 20 ng/mL after a 15 mg dose and occurs at about 2 hours.
Metabolism
Quazepam, the active parent compound, is extensively metabolized in the liver; two of the plasma metabolites are 2-oxoquazepam and N-desalkyl-2-oxoquazepam. All three compounds show CNS depressant activity.
Distribution
The degree of plasma protein binding for quazepam and its two major metabolites is greater than 95%.
Elimination
Following administration of 14C-quazepam, 31% of the dose appeared in the urine and 23% in the feces over five days; only trace amounts of unchanged drug were present in the urine.
The mean elimination half-life of quazepam and 2-oxoquazepam is 39 hours and that of N-desalkyl-2-oxoquazepam is 73 hours. Steady-state levels of quazepam and 2-oxoquazepam are attained by the seventh daily dose and that of N-desalkyl-2-oxoquazepam by the thirteenth daily dose.
Special Populations
Geriatrics: The pharmacokinetics of quazepam and 2-oxoquazepam in geriatric subjects are comparable to those seen in young adults; as with desalkyl metabolites of other benzodiazepines, the elimination half-life of N-desalkyl-2-oxoquazepam in geriatric patients is about twice that of young adults.
Drug Interactions
Bupropion (a CYP2B6 substrate): Co-administration of a single dose of 150 mg Bupropion Hydrochloride XL with steady state quazepam did not significantly affect the AUC and Cmax of bupropion or its primary metabolite, hydroxybupropion.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
DORAL showed no evidence of carcinogenicity in oral carcinogenicity studies in mice and hamsters.
Mutagenesis
DORAL was negative in the bacterial reverse mutation (Ames) assay and equivocal in the mouse lymphoma tk assay.
Impairment of Fertility
Reproduction studies in mice conducted with DORAL at doses equal to 60 and
180 times the human dose of 15 mg produced slight reductions in fertility rate. Similar reductions in fertility rate have been reported in mice dosed with other benzodiazepines, and is believed to be related to the sedative effects of these drugs at high doses
14. Clinical Studies
The effectiveness of DORAL was established in placebo-controlled clinical studies of 5 nights duration in acute and chronic insomnia. The sustained effectiveness of DORAL was established in chronic insomnia in a sleep laboratory (polysomnographic) study of 28 nights duration. In the sleep laboratory study, DORAL significantly decreased sleep latency and total wake time, and significantly increased total sleep time and percent sleep time, for one or more nights.
DORAL 15 mg was effective on the first night of administration. Sleep latency, total wake time and wake time after sleep onset were still decreased and percent sleep time was still increased for several nights after the drug was discontinued. Percent slow wave sleep was decreased, and REM sleep was essentially unchanged. No transient sleep disturbance, such as “rebound insomnia,” was observed after withdrawal of the drug in sleep laboratory studies in 12 patients using 15 mg doses.
A double-blind, controlled sleep laboratory study (N=30) in elderly patients compared the effects of DORAL 7.5 mg and 15 mg to that of placebo over a period of 7 days. Both the 7.5 mg and 15 mg doses appeared to be effective. Caution must be used in interpreting this data due to the small size of the study.
16. How is Doral Tablets supplied
DORAL ® Tablets, 15 mg, functionally scored, capsule-shaped, light orange, slightly white speckled tablets, impressed with the product identification number 15 on one side of the tablet, and the product name (DORAL) on the other.
| 15 mg | Bottles of 30 | NDC 61825-165-30 |
Store DORAL Tablets at controlled room temperature 20°-25°C (68°-77°F).
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling ( Medication Guide).
Risks from Concomitant Use with Opioids
Inform patients and caregivers that potentially fatal additive effects may occur if DORAL is used with opioids and not to use such drugs concomitantly unless supervised by a healthcare provider
[see Warnings and Precautions (
5.1), Drug Interactions (
7)]
Abuse, Misuse, and Addiction
Inform patients that the use of DORAL even at recommended dosages, exposes users to risks of abuse, misuse, and addiction, which can lead to overdose and death, especially when used in combination with other medications (e.g., opioid analgesics), alcohol, and/or illicit substances. Inform patients about the signs and symptoms of benzodiazepine abuse, misuse, and addiction; to seek medical help if they develop these signs and/or symptoms; and on the proper disposal of unused drug
[see Warnings and Precautions (
5.2) and Drug Abuse and Dependence (
9.2)]
.
Withdrawal Reactions
Inform patients that the continued use of DORAL may lead to clinically significant physical dependence and that abrupt discontinuation or rapid dosage reduction of DORAL may precipitate acute withdrawal reactions, which can be life-threatening. Inform patients that in some cases, patients have developed a protracted withdrawal syndrome with withdrawal symptoms lasting weeks to more than 12 months. Instruct patients that discontinuation or dosage reduction of DORAL may require a slow taper
[see Warnings and Precautions (
5.3) and Drug Abuse and Dependence (
9.3)]
.
CNS Depressant Effects and Next-Day Impairment
Tell patients that DORAL can cause next-day impairment, even in the absence of symptoms. Caution patients against driving or engaging in other hazardous activities or activities requiring complete mental alertness when using DORAL. Tell patients that daytime impairment may persist for several days following discontinuation of DORAL. Advise patients that increased drowsiness and decreased consciousness may increase the risk of falls in some patients
[see Warnings and Precautions (
5.4)]
Severe Allergic Reactions
Inform patients that severe allergic reactions can occur from DORAL. Describe the signs/symptoms of these reactions and advise patients to seek medical attention immediately if these occur
[see Warnings and Precautions (
5.6)]
.
Abnormal Thinking and Behavior Change
Instruct patients that sedative hypnotics can cause abnormal thinking and behavior change, including “sleep-driving” and other complex behaviors while not being fully awake (preparing and eating food, making phone calls, or having sex). Tell patients to call you immediately if they develop any of these symptoms
[see Warnings and Precautions (
5.7)]
.
Suicide
Tell patients that DORAL can worsen depression, and to immediately report any suicidal thoughts
[see Warnings and Precautions (
5.8)]
.
Alcohol and Other Drugs
Ask patients about alcohol consumption, medicines they are taking now, and drugs they may be taking without a prescription. Advise patients that alcohol generally should not be used during treatment with DORAL.
Pregnancy
Advise pregnant females that use of DORAL late in pregnancy can result in sedation (respiratory depression, lethargy, hypotonia) and/or withdrawal symptoms (hyperreflexia, irritability, restlessness, tremors, inconsolable crying, and feeding difficulties) in newborns
[see Warnings and Precautions (
5.9), Use in Specific Populations (
8.1)]
. Instruct patients to inform their healthcare provider if they are pregnant.
Advise patients that there is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to DORAL during pregnancy [see Use in Specific Populations ( 8.1)] .
Nursing
Instruct patients to notify their healthcare provider if they are breastfeeding or intend to breastfeed. Instruct breastfeeding patients using DORAL to monitor infants for excessive sedation, poor feeding and poor weight gain, and to seek medical attention if they notice these signs
[see Use in Specific Populations (
8.3)]
.
Galt Pharmaceuticals, LLC.
Atlanta, GA 30339
Printed in USA. 500494-12 Rev. 01/2023
Medication Guide
|
Medication Guide
|
|
|
What is the most important information I should know about DORAL?
Do not drive or operate heavy machinery until you know how taking DORAL with opioids affects you.
Call your healthcare provider right away if you find out that you have done any of the above activities after taking DORAL. |
|
|
What is DORAL?
|
|
|
Do not take DORAL if you:
|
|
|
Before you take DORAL, tell your healthcare provider about all of your medical conditions, including if you:
Tell your healthcare provider about all of the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Taking DORAL with certain other medicines can cause side effects or affect how well DORAL or the other medicines work. Do not start or stop other medicines without talking to your healthcare provider. Do not take DORAL with other medicines that can make you sleepy unless your healthcare provider tells you to. |
|
|
How should I take DORAL?
|
|
|
What are the possible side effects of DORAL? DORAL may cause serious side effects, including:
Call your healthcare provider right away if you have any of the above side effects while taking DORAL. The most common side effects of DORAL include:
After you stop taking a sleep medicine, you may have symptoms for the next 1 to 2 days such as:
These are not all the possible side effects of DORAL. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
|
|
How should I store DORAL?
|
|
|
General information about the safe and effective use of Doral. Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use DORAL for a condition for which it was not prescribed. Do not give DORAL to other people, even if they have the same symptoms that you have. It may harm them. You can ask your healthcare provider or pharmacist for information about DORAL that is written for healthcare professionals. |
|
|
What are the ingredients in DORAL? Active Ingredient: quazepam Inactive Ingredients: cellulose, corn starch, FD&C Yellow No.6, lactose, magnesium stearate, silicon dioxide, and sodium lauryl sulfate Distributed by Galt Pharmaceuticals, Atlanta, GA 30339 USA. If you would like more information, call Galt Pharmaceuticals at 1-855-965-2783 or visit www.doralrx.com. |
|
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised: 01/2023 |
| DORAL
quazepam tablet |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Galt Pharmaceuticals, LLC (079214973) |