Drug Detail:Dysport (Abobotulinumtoxina [ a-boe-bot-ue-lye-num-tox-in-a ])
Drug Class: Skeletal muscle relaxants
Highlights of Prescribing Information
DYSPORT® (abobotulinumtoxinA) for injection, for intramuscular use
Initial U.S. Approval: 2009
WARNING: DISTANT SPREAD OF TOXIN EFFECT
See full prescribing information for complete boxed warning
The effects of DYSPORT and all botulinum toxin products may spread from the area of injection to produce symptoms consistent with botulinum toxin effects. These symptoms have been reported hours to weeks after injection. Swallowing and breathing difficulties can be life-threatening and there have been reports of death. The risk of symptoms is probably greatest in children treated for spasticity but symptoms can occur in adults, particularly in those patients who have underlying conditions that would predispose them to these symptoms (5.1).
Recent Major Changes
| Dosage and Administration (2.2, 2.3, 2.5, 2.6) | 1/2023 |
Indications and Usage for Dysport
DYSPORT is an acetylcholine release inhibitor and a neuromuscular blocking agent indicated for:
- The treatment of cervical dystonia in adults (1.1)
- The temporary improvement in the appearance of moderate to severe glabellar lines associated with procerus and corrugator muscle activity in adults < 65 years of age (1.2)
- The treatment of spasticity in patients 2 years of age and older (1.3)
Dysport Dosage and Administration
Preparation of DYSPORT Solution for Administration (2.2)
- Once reconstituted, store in original container in a refrigerator at 2°C to 8°C (36°F to 46°F) and use within 24 hours
- Do not freeze after reconstitution
- Reconstitution instructions are specific for the 300 Unit and 500 Unit vials
- Reconstituted DYSPORT is intended for intramuscular injection only. After reconstitution, DYSPORT should be used for only one injection session and for only one patient
Cervical Dystonia (2.3)
- Initial dose is 500 Units given intramuscularly as a divided dose among the affected muscles
- Re-treatment every 12 to 16 weeks or longer, as necessary, based on return of clinical symptoms with doses administered between 250 Units and 1000 Units to optimize clinical benefit
- Re-treatment should not occur in intervals of less than 12 weeks
- Titrate in 250 Unit steps according to patient's response
Glabellar Lines (2.4)
- Administer a total dose of 50 Units, divided in five equal aliquots of 10 Units each, intramuscularly to affected muscles to achieve clinical effect
- Re-treatment should be administered no more frequently than every 3 months
Spasticity in Adults (2.5)
- Select dose based on muscles affected, severity of spasticity, and treatment and adverse reaction history with botulinum toxins
- Dosing for upper limb spasticity: between 500 Units and 1000 Units
- Dosing for lower limb spasticity: up to 1500 Units
- The maximum recommended total dose per treatment session (upper and lower limb combined) in adults is 1500 Units
- Re-treatment, based on return of clinical symptoms, should not occur in intervals of less than 12 weeks
Spasticity in Pediatric Patients (2.6)
- Select dose based on the affected muscle, severity of spasticity, and treatment and adverse reaction history with all botulinum toxins.
- Recommended dosing for upper limb spasticity: 8 Units/kg to 16 Units/kg per limb. The maximum recommended total dose administered per treatment session must not exceed 16 Units/kg or 640 Units, whichever is lower.
- Recommended dosing for lower limb spasticity: 10 Units/kg to 15 Units/kg per limb. Total dose per treatment session must not exceed 15 Units/kg for unilateral lower limb injections, 30 Units/kg for bilateral injections, or 1000 Units, whichever is lower.
- The maximum recommended total dose per treatment session is 30 Units/kg or 1000 Units, whichever is lower. Re-treatment, based on return of clinical symptoms, should not occur in intervals of less than 3 months.
Dosage Forms and Strengths
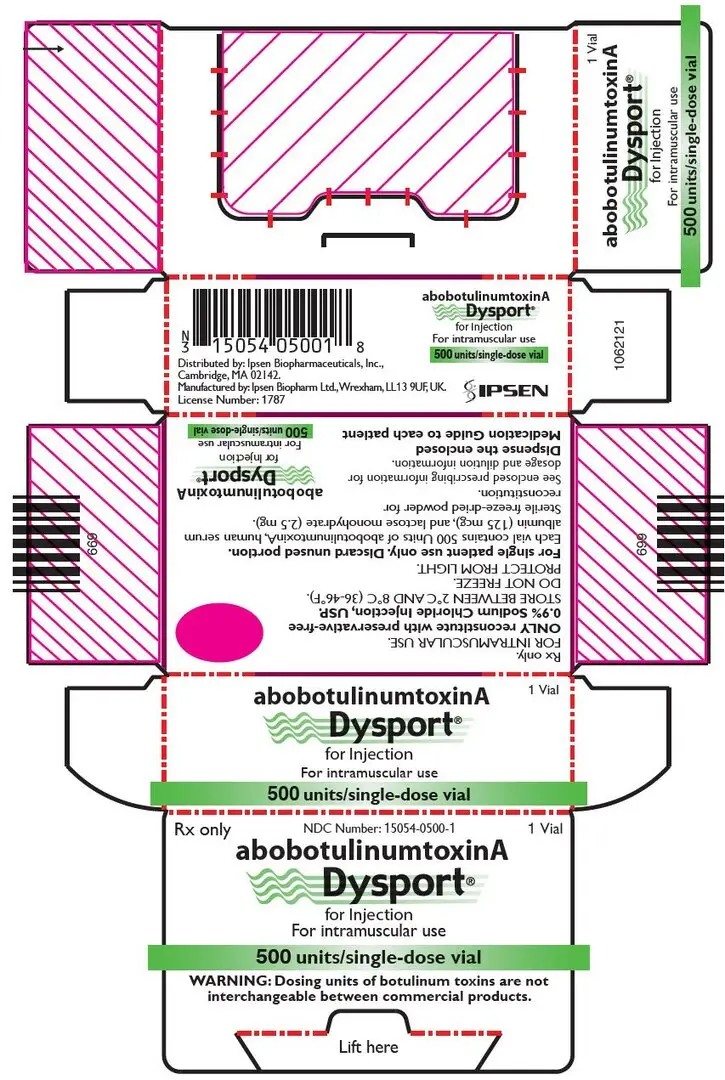
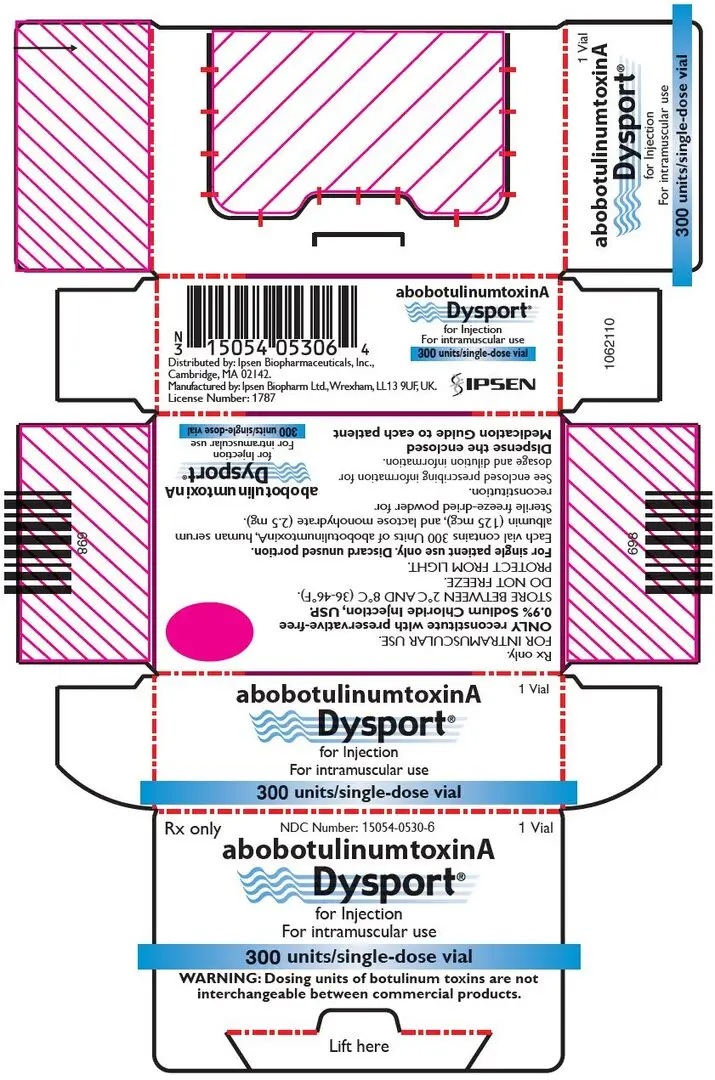
- For Injection: 300 Units or 500 Units lyophilized powder in a single-dose vial (3)
Contraindications
- Hypersensitivity to:
- any botulinum toxin product or excipients (4, 5.3)
- cow's milk protein (4, 5.3)
- Infection at the proposed injection site(s) (4)
Warnings and Precautions
- The potency units of DYSPORT are not interchangeable with other preparations of botulinum toxin products (5.2)
- Immediate medical attention may be required in cases of respiratory, speech or swallowing difficulties (5.4)
- Recommended dose and frequency of administration should not be exceeded (5.5)
- Dry eye may occur with glabellar line treatment; if symptoms persist, consider referring patient to an ophthalmologist (5.6)
- Concomitant neuromuscular disorder may exacerbate clinical effects of treatment (5.7)
Adverse Reactions/Side Effects
Most commonly observed adverse reactions are (6.1):
Cervical Dystonia
(≥5%): muscular weakness, dysphagia, dry mouth, injection site discomfort, fatigue, headache, musculoskeletal pain, dysphonia, injection site pain and eye disorders
Glabellar Lines
(≥2%): nasopharyngitis, headache, injection site pain, injection site reaction, upper respiratory tract infection, eyelid edema, eyelid ptosis, sinusitis, nausea, and blood present in urine
Spasticity in Adults
- Upper limb spasticity (≥4%): muscular weakness
- Lower limb spasticity (≥5%): falls, muscular weakness, and pain in extremity
Spasticity in Pediatric Patients
- Upper limb spasticity (≥10%): upper respiratory tract infection and pharyngitis
- Lower limb spasticity (≥10%): nasopharyngitis, cough, and pyrexia
To report SUSPECTED ADVERSE REACTIONS, contact Ipsen Biopharmaceuticals, Inc. at 855-463-5127 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
Drug Interactions
- Concomitant use of DYSPORT and aminoglycosides or other agents interfering with neuromuscular transmission or muscle relaxants, should be observed closely because effect of DYSPORT may be potentiated (7.1, 7.4)
- Anticholinergic drugs may potentiate systemic anticholinergic effects (7.2)
- The effect of administering different botulinum neurotoxins during the course of treatment with DYSPORT is unknown (7.3)
Use In Specific Populations
- Administer DYSPORT with care in elderly patients, reflecting the greater frequency of concomitant disease and other drug therapy (8.5)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 1/2023
Full Prescribing Information
WARNING: DISTANT SPREAD OF TOXIN EFFECT
Postmarketing reports indicate that the effects of DYSPORT and all botulinum toxin products may spread from the area of injection to produce symptoms consistent with botulinum toxin effects. These may include asthenia, generalized muscle weakness, diplopia, blurred vision, ptosis, dysphagia, dysphonia, dysarthria, urinary incontinence and breathing difficulties. These symptoms have been reported hours to weeks after injection. Swallowing and breathing difficulties can be life threatening and there have been reports of death. The risk of symptoms is probably greatest in children treated for spasticity but symptoms can also occur in adults treated for spasticity and other conditions, particularly in those patients who have underlying conditions that would predispose them to these symptoms. In unapproved uses and in approved indications, cases of spread of effect have been reported at doses comparable to or lower than the maximum recommended total dose [see Warnings and Precautions (5.1)].
1. Indications and Usage for Dysport
2. Dysport Dosage and Administration
2.1 Instructions for Safe Use
The potency units of DYSPORT are not interchangeable with other preparations of botulinum toxin products and, therefore, units of biological activity of DYSPORT cannot be compared to or converted into units of any other botulinum toxin products assessed with any other specific assay method [see Warnings and Precautions (5.2) and Description (11)]. Reconstituted DYSPORT is intended for intramuscular injection only.
2.2 Preparation of DYSPORT Solution for Administration
DYSPORT is supplied as a dry powder, in single-dose 300 Unit and 500 Unit vials, which must be reconstituted with preservative-free 0.9% Sodium Chloride Injection, USP using aseptic technique prior to intramuscular injection. Table 1 provides dilution instructions for the 300 Unit and 500 Unit vials, depending on the desired final concentration. The desired final concentration after dilution varies depending on the indication (see Table 2 for the recommended solution concentration after dilution).
| Diluent* per 500 Unit Vial | Resulting Dose Units per 0.1 mL | Diluent* per 300 Unit Vial | Resulting Dose Units per 0.1 mL |
|---|---|---|---|
| Note: These dilutions are calculated for an injection volume of 0.1 mL. A decrease or increase in the DYSPORT dose is also possible by administering a smaller or larger injection volume (i.e., 0.05 mL (50% decrease in dose), 0.08 mL (20% decrease in dose) or 0.15 mL (50% increase in dose)). | |||
|
|||
| 1 mL | 50 Units | 0.6 mL | 50 Units |
| 2 mL 2.5 mL | 25 Units 20 Units | -- 1.5 mL | -- 20 Units |
| -- | -- | 2.5 mL | 12 Units |
| 5 mL† | 10 Units | 3 mL | 10 Units |
Using an appropriately sized sterile syringe, needle and aseptic technique, draw up the required amount of sterile, preservative-free 0.9% Sodium Chloride Injection, USP (see Table 1). Insert the needle into the DYSPORT vial. The partial vacuum will begin to pull the saline into the vial. Any remaining required saline should be expressed into the vial manually. Do not use the vial if no partial vacuum is observed. Swirl gently to dissolve. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration.
Reconstituted DYSPORT should be a clear, colorless solution, free of particulate matter, otherwise it should not be injected. Expel any air bubbles in the syringe barrel. Remove the needle used to reconstitute the product and attach an appropriately sized new sterile needle for injection.
After reconstitution, DYSPORT should be used for only one injection session and for only one patient. Discard any unused portion. Once reconstituted, unused DYSPORT may be stored in the original container, in a refrigerator at 2°C to 8°C (36°F to 46°F), protected from light for up to 24 hours until time of use. It must be discarded if not used within 24 hours. Do not freeze reconstituted DYSPORT. Discard the vial and needle in accordance with local regulations.
| Indication | Recommended Concentration | Recommended DYSPORT Dose |
|---|---|---|
|
||
| Cervical Dystonia, Adults | 50 Units/0.1 mL or 25 Units/0.1 mL | 500 Units to 1000 Units |
| Glabellar Lines, Adults | 12 Units/0.1 mL or 20 Units/0.1 mL | 50 Units, divided in five equal aliquots of 10 Units (0.08 mL) each or 50 Units, divided in five equal aliquots of 10 Units (0.05 mL) each |
| Spasticity, Adults* | 10 Units/0.1 mL or 20 Units/0.1 mL | Upper Limb: 500 Units to 1000 Units Lower Limb: 1000 Units to 1500 Units Maximum total dose per treatment session = 1500 Units |
| Spasticity, Pediatric Patients† | 20 Units/0.1 mL or 50 Units/0.1 mL‡ | Upper Limb: 8 Units/kg to 16 Units/kg per limb
|
2.3 Dosing in Cervical Dystonia
The recommended initial dose of DYSPORT for the treatment of cervical dystonia in adults is 500 Units given intramuscularly as a divided dose among affected muscles in patients with or without a history of prior treatment with botulinum toxin. (A description of the average DYSPORT dose and percentage of total dose injected into specific muscles in the pivotal clinical trials can be found in Table 15 of Section 14.1, Clinical Studies – Cervical Dystonia.) Limiting the dose injected into the sternocleidomastoid muscle may reduce the occurrence of dysphagia. Clinical studies with DYSPORT in cervical dystonia suggest that the peak effect occurs between two and four weeks after injection. Simultaneous guided injection of DYSPORT with EMG and/or ultrasound may be helpful in locating active muscles.
2.4 Dosing in Glabellar Lines
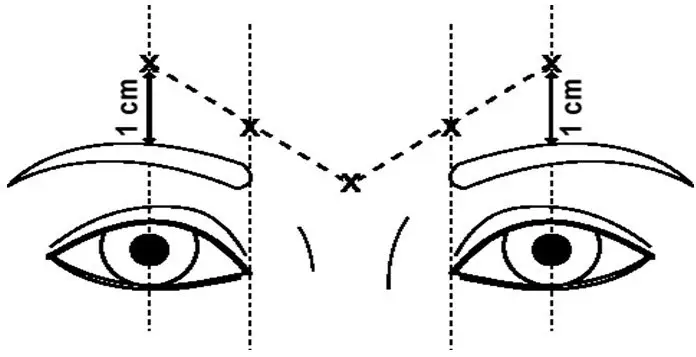
The dose of DYSPORT for the treatment of glabellar lines in adults is a total of 50 Units given intramuscularly in five equal aliquots of 10 Units each to achieve clinical effect (see Figure 1).
The clinical effect of DYSPORT may last up to four months. Repeat dosing in clinical studies demonstrated continued efficacy with up to four repeated administrations. It should be administered no more frequently than every three months. When used for re-treatment, DYSPORT should be reconstituted and injected using the same techniques as the initial treatment.
2.5 Dosing in Spasticity in Adults
Dosing in initial and subsequent treatment sessions should be tailored to the individual based on the size, number and location of muscles involved, severity of spasticity, the presence of local muscle weakness, the patient's response to previous treatment, and/or adverse reaction history with botulinum toxins.
No more than 1 mL should generally be administered at any single injection site. The maximum recommended total dose (upper and lower limb combined) of DYSPORT for the treatment of spasticity in adults is 1500 Units.
Although actual location of the injection sites can be determined by palpation, the use of injection guiding technique (e.g., electromyography, electrical stimulation, or ultrasound) is recommended to target the injection sites.
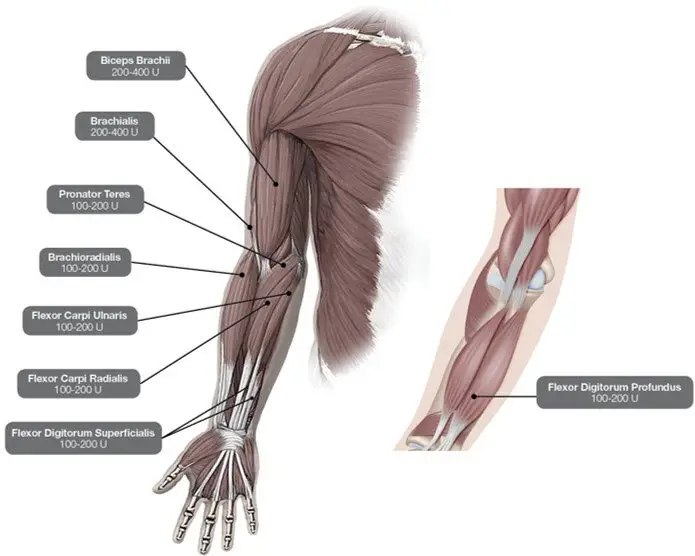
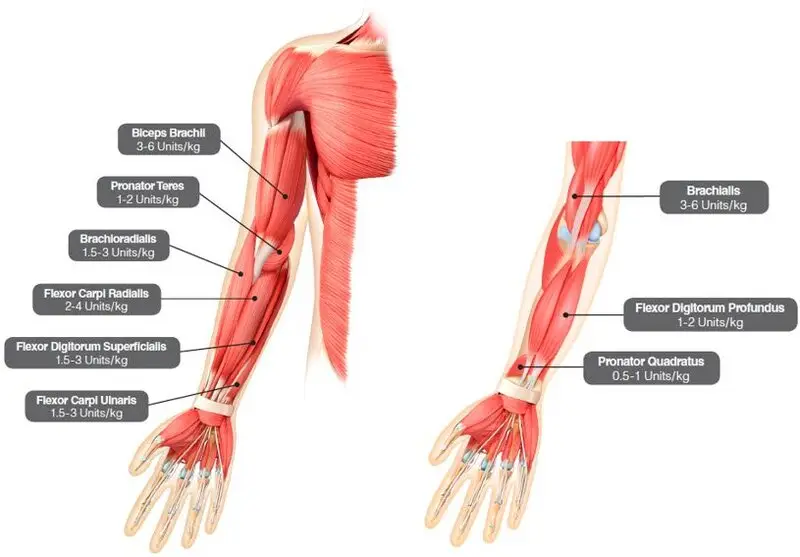
Upper Limb Spasticity
In the clinical trial that assessed the efficacy and safety of DYSPORT for treatment of upper limb spasticity in adults [see Clinical Studies (14.3)], doses of 500 Units and 1000 Units were divided among selected muscles at a given treatment session (see Table 3 and Figure 2).
| Muscles Injected | Recommended Dose DYSPORT | Recommended Number of Injection(s) per Muscle |
|---|---|---|
| Flexor carpi radialis (FCR) | 100 Units to 200 Units | 1 to 2 |
| Flexor carpi ulnaris (FCU) | 100 Units to 200 Units | 1 to 2 |
| Flexor digitorum profundus (FDP) | 100 Units to 200 Units | 1 to 2 |
| Flexor digitorum superficialis (FDS) | 100 Units to 200 Units | 1 to 2 |
| Brachialis | 200 Units to 400 Units | 1 to 2 |
| Brachioradialis | 100 Units to 200 Units | 1 to 2 |
| Biceps Brachii (BB) | 200 Units to 400 Units | 1 to 2 |
| Pronator Teres | 100 Units to 200 Units | 1 |
Figure 2: Muscles for Injection for Upper Limb Spasticity in Adults
Repeat DYSPORT treatment should be administered when the effect of a previous injection has diminished, but no sooner than 12 weeks after the previous injection. A majority of patients in clinical studies were retreated between 12-16 weeks; however some patients had a longer duration of response (i.e., 20 weeks). The degree and pattern of muscle spasticity at the time of re-injection may necessitate alterations in the dose of DYSPORT and muscles to be injected. Clinical improvement may be expected one week after administration of DYSPORT.
Lower Limb Spasticity
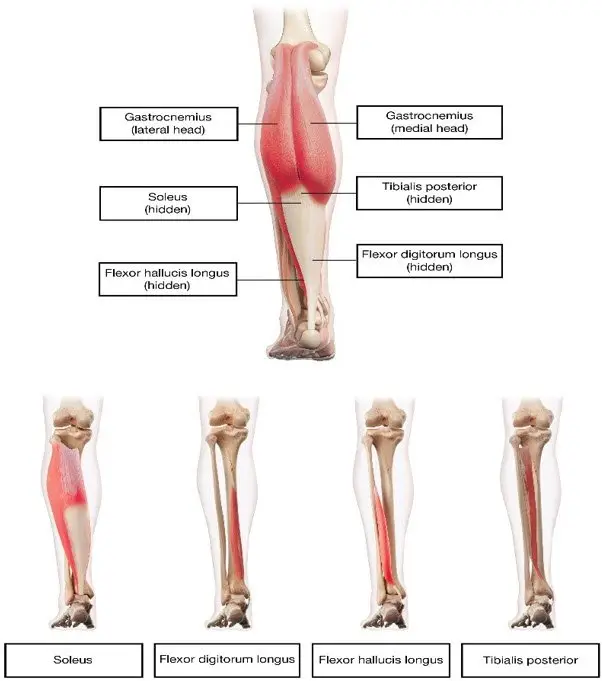
In the clinical trial that assessed the efficacy and safety of DYSPORT for treatment of lower limb spasticity in adults [see Clinical Studies (14.3)], doses of 1000 Units and 1500 Units were divided among selected muscles at a given treatment session (see Table 4 and Figure 3).
| Muscles Injected | Recommended DYSPORT Dose | Recommended Number of Injection Sites per Muscle |
|---|---|---|
| Distal Muscles | ||
| Gastrocnemius | ||
| Medial head | 100 Units to 150 Units | 1 |
| Lateral head | 100 Units to 150 Units | 1 |
| Soleus | 330 Units to 500 Units | 3 |
| Tibialis posterior | 200 Units to 300 Units | 2 |
| Flexor digitorum longus | 130 Units to 200 Units | 1 to 2 |
| Flexor hallucis longus | 70 Units to 200 Units | 1 |
Figure 3: Muscles for Injection for Lower Limb Spasticity in Adults
Repeat DYSPORT treatment should be administered when the effect of a previous injection has diminished, but no sooner than 12 weeks after the previous injection. A majority of patients in clinical studies were retreated between 12-16 weeks. The degree and pattern of muscle spasticity at the time of re-injection may necessitate alterations in the dose of DYSPORT and muscles to be injected.
2.6 Dosing in Spasticity in Pediatric Patients
DYSPORT dosing for spasticity in pediatric patients is based on Units per kilogram of body weight. To calculate the total units of DYSPORT required for treatment of one limb, select the dose of DYSPORT in Units/kg and the body weight (kg) of the patient (see Tables 5 and 6). Dosing in initial and sequential treatment sessions should be tailored to the individual patient based on the size, number and location of muscles involved, severity of spasticity, the presence of local muscle weakness, the patient's response to previous treatment, and/or adverse reaction history with botulinum toxins.
No more than 0.5 mL should generally be administered at any single injection site. The maximum recommended total dose of DYSPORT in a single treatment session for spasticity in pediatric patients 2 years and older is 30 Units/kg or 1000 Units in a 3-month interval.
Although actual location of the injection sites can be determined by palpation, the use of injection guiding technique (e.g., electromyography or electrical stimulation, or ultrasound) is recommended to target the injection sites.
Upper Limb Spasticity in Pediatric Patients 2 Years of Age and Older
In the clinical trial that assessed the efficacy and safety of DYSPORT for treatment of upper limb spasticity in pediatric patients 2 years of age or older with a weight of at least 10 kg [see Clinical Studies (14.4)], doses of 8 Units/kg or 16 Units/kg were divided among selected muscles of the target upper limb at a given treatment session (see Table 5 and Figure 4).
Table 5 describes the recommended Units/kg dose of DYSPORT per muscle. The maximum recommended total dose of DYSPORT administered for treatment of upper limb spasticity must not exceed 16 Units/kg or 640 Units, whichever is lower.
| Muscle | Recommended Dose Range per muscle per upper limb (Units/kg Body Weight) | Number of injection sites per muscle |
|---|---|---|
| Brachialis | 3 Units/kg to 6 Units/kg | Up to 2 |
| Brachioradialis | 1.5 Units/kg to 3 Units/kg | 1 |
| Biceps brachii | 3 Units/kg to 6 Units/kg | Up to 2 |
| Pronator teres | 1 Units/kg to 2 Units/kg | 1 |
| Pronator quadratus | 0.5 Units/kg to 1 Units/kg | 1 |
| Flexor carpi radialis (FCR) | 2 Units/kg to 4 Units/kg | Up to 2 |
| Flexor carpi ulnaris (FCU) | 1.5 Units/kg to 3 Units/kg | 1 |
| Flexor digitorum profundus (FDP) | 1 Units/kg to 2 Units/kg | 1 |
| Flexor digitorum superficialis (FDS) | 1.5 Units/kg to 3 Units/kg | Up to 4 |
| Total dose | 8 Units/kg to 16 Units/kg in upper limbs (and not exceeding 640 Units) | |
Figure 4: Muscles for Injection for Upper Limb Spasticity in Pediatric Patients
Repeat DYSPORT treatment should be administered when the effect of a previous injection has diminished but no sooner than 16 weeks after the previous injection. A majority of patients in the clinical study were retreated between 16-28 weeks; however, some patients had a longer duration of response (i.e., 34 weeks or more). The degree and pattern of muscle spasticity at the time of re-injection may necessitate alterations in the dose of DYSPORT and muscles to be injected.
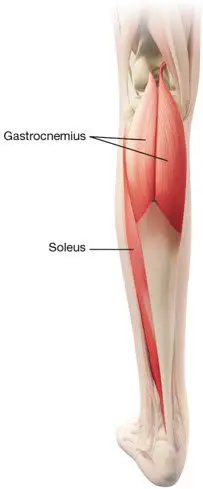
Lower Limb Spasticity in Pediatric Patients 2 Years of Age and Older In the clinical trial that assessed the efficacy and safety of DYSPORT for treatment of lower limb spasticity in pediatric patients 2 years of age or older [see Clinical Studies (14.4)], doses of 10 Units/kg to 15 Units/kg were divided among selected muscles of the target lower limb at a given treatment session (see Table 6 and Figure 5).
Table 6 describes the recommended Units/kg dose of DYSPORT per muscle of the Gastrocnemius-Soleus Complex (GSC). The recommended total DYSPORT dose per treatment session is 10 Units/kg to 15 Units/kg for unilateral lower limb injections or 20 Units/kg to 30 Units/kg for bilateral lower limb injections. However, the total dose of DYSPORT administered in a 3-month interval must not exceed 15 Units/kg for unilateral lower limb injections, 30 Units/kg for bilateral lower limb injections, or 1000 units, whichever is lower. The total dose administered should be divided between the affected spastic muscles of the lower limb(s). When possible, the dose should be distributed across more than 1 injection site in any single muscle (see Table 6).
| Muscle Injected | Recommended DYSPORT Dose Range per muscle per leg (Units/kg Body Weight) | Recommended number of injections per muscle |
|---|---|---|
|
||
| Gastrocnemius | 6 Units/kg to 9 Units/kg* | Up to 4 |
| Soleus | 4 Units/kg to 6 Units/kg* | Up to 2 |
| Total | 10 Units/kg to 15 Units/kg divided across both muscles | Up to 6 |
Figure 5: Muscles for Injection for Lower Limb Spasticity in Pediatric Patients
Although actual location of the injection sites can be determined by palpation, the use of injection guiding technique (e.g., electromyography or electrical stimulation, or ultrasound) is recommended to target the injection sites.
Repeat DYSPORT treatment should be administered when the effect of a previous injection has diminished but no sooner than 12 weeks after the previous injection. A majority of patients in the clinical studies were retreated between 16-22 weeks, however; some had a longer duration of response. The degree and pattern of muscle spasticity and overall clinical benefit at the time of re-injection may necessitate alterations in the dose of DYSPORT and muscles to be injected.
The safety and effectiveness of DYSPORT injected into proximal muscles of the lower limb for the treatment of spasticity in pediatric patients has not been established.
3. Dosage Forms and Strengths
For injection: 300 Units or 500 Units of lyophilized powder in a single-dose vial for reconstitution with preservative-free 0.9% Sodium Chloride Injection, USP.
4. Contraindications
DYSPORT is contraindicated in patients with:
- Known hypersensitivity to any botulinum toxin products, cow's milk protein, or to any of the components in the formulation [see Warnings and Precautions (5.3)]. This product may contain trace amounts of cow's milk protein [see Description (11)].
- Infection at the proposed injection site(s).
5. Warnings and Precautions
5.1 Spread of Toxin Effect
Postmarketing safety data from DYSPORT and other approved botulinum toxins suggest that botulinum toxin effects may, in some cases, be observed beyond the site of local injection. The symptoms are consistent with the mechanism of action of botulinum toxin and may include asthenia, generalized muscle weakness, diplopia, blurred vision, ptosis, dysphagia, dysphonia, dysarthria, urinary incontinence and breathing difficulties. These symptoms have been reported hours to weeks after injection. Swallowing and breathing difficulties can be life-threatening and there have been reports of death related to spread of toxin effects. The risk of symptoms is probably greatest in children treated for spasticity but symptoms can also occur in adults treated for spasticity and other conditions, particularly in those patients who have underlying conditions that would predispose them to these symptoms. In unapproved uses and approved indications, symptoms consistent with spread of toxin effect have been reported at doses comparable to or lower than the maximum recommended total dose .
5.2 Lack of Interchangeability between Botulinum Toxin Products
The potency Units of DYSPORT are specific to the preparation and assay method utilized. They are not interchangeable with other preparations of botulinum toxin products and, therefore, units of biological activity of DYSPORT cannot be compared to or converted into units of any other botulinum toxin products assessed with any other specific assay method [see Description (11)].
5.3 Hypersensitivity Reactions
Serious hypersensitivity reactions have been reported with DYSPORT. Hypersensitivity reactions include anaphylaxis, serum sickness, urticaria, soft tissue edema, and dyspnea. If such a serious hypersensitivity reaction occurs, discontinue further injection of DYSPORT and institute appropriate medical therapy immediately.
5.4 Dysphagia and Breathing Difficulties
Treatment with DYSPORT and other botulinum toxin products can result in swallowing or breathing difficulties. Patients with pre-existing swallowing or breathing difficulties may be more susceptible to these complications. In most cases, this is a consequence of weakening of muscles in the area of injection that are involved in breathing or swallowing. When distant effects occur, additional respiratory muscles may be involved [see Boxed Warning and Warnings and Precautions (5.2)].
Deaths as a complication of severe dysphagia have been reported after treatment with botulinum toxin. Dysphagia may persist for several weeks and require use of a feeding tube to maintain adequate nutrition and hydration. Aspiration may result from severe dysphagia and is a particular risk when treating patients in whom swallowing or respiratory function is already compromised.
Treatment of cervical dystonia with botulinum toxins may weaken neck muscles that serve as accessory muscles of ventilation. This may result in a critical loss of breathing capacity in patients with respiratory disorders who may have become dependent upon these accessory muscles. There have been post-marketing reports of serious breathing difficulties, including respiratory failure.
Patients treated with botulinum toxin may require immediate medical attention should they develop problems with swallowing, speech or respiratory disorders. These reactions can occur within hours to weeks after injection with botulinum toxin [see Boxed Warning, Warnings and Precautions (5.2), Adverse Reactions (6.1), Clinical Pharmacology (12.2)].
5.5 Facial Anatomy in the Treatment of Glabellar Lines
Caution should be exercised when administering DYSPORT to patients with surgical alterations to the facial anatomy, excessive weakness or atrophy in the target muscle(s), marked facial asymmetry, inflammation at the injection site(s), ptosis, excessive dermatochalasis, deep dermal scarring, thick sebaceous skin [see Dosage and Administration (2.4)] or the inability to substantially lessen glabellar lines by physically spreading them apart [see Clinical Studies (14.2)].
Do not exceed the recommended dosage and frequency of administration of DYSPORT. In clinical trials, subjects who received a higher dose of DYSPORT had an increased incidence of eyelid ptosis.
5.6 Dry Eye with the Treatment of Glabellar Lines
Dry eye has been reported with the use of DYSPORT in the treatment of glabellar lines [see Adverse Reactions (6.3)]. Reduced tear production, reduced blinking, and corneal disorders, may occur with use of botulinum toxins, including DYSPORT. If symptoms of dry eye (e.g., eye irritation, photophobia, or visual changes) persist, consider referring patient to an ophthalmologist [see Boxed Warning and Warnings and Precautions 5.2].
5.7 Pre-existing Neuromuscular Disorders
Individuals with peripheral motor neuropathic diseases, amyotrophic lateral sclerosis or neuromuscular junction disorders (e.g., myasthenia gravis or Lambert-Eaton syndrome) should be monitored particularly closely when given botulinum toxin. Patients with neuromuscular disorders may be at increased risk of clinically significant effects including severe dysphagia and respiratory compromise from typical doses of DYSPORT [see Adverse Reactions (6.1)].
5.8 Human Albumin and Transmission of Viral Diseases
This product contains albumin, a derivative of human blood. Based on effective donor screening and product manufacturing processes, it carries an extremely remote risk for transmission of viral diseases and variant Creutzfeldt-Jakob disease (vCJD). There is a theoretical risk for transmission of Creutzfeldt-Jakob disease (CJD), but if that risk actually exists, the risk of transmission would also be considered extremely remote. No cases of transmission of viral diseases, CJD, or vCJD have ever been identified for licensed albumin or albumin contained in other licensed products.
6. Adverse Reactions/Side Effects
The following serious adverse reactions are discussed below and elsewhere in labeling:
- Distant Spread of Toxin Effect [see Warnings and Precautions (5.1)]
- Lack of Interchangeability between Botulinum Toxin Products [see Warnings and Precautions (5.2)]
- Spread of Toxin Effect [see Warnings and Precautions (5.2)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.3)]
- Dysphagia and Breathing Difficulties [see Warnings and Precautions (5.4)]
- Facial Anatomy in the Treatment of Glabellar Lines [see Warnings and Precautions (5.5)]
- Dry Eye with the Treatment of Glabellar Lines [see Warnings and Precautions (5.6)]
- Pre-existing Neuromuscular Disorders [see Warnings and Precautions (5.7)]
- Human Albumin and Transmission of Viral Diseases [see Warnings and Precautions (5.8)]
- Intradermal Immune Reaction [see Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Cervical Dystonia
The data described below reflect exposure to DYSPORT in 446 cervical dystonia patients in 7 studies. Of these, two studies were randomized, double-blind, single treatment, placebo-controlled studies with subsequent optional open-label treatment in which dose optimization (250 to 1000 Units per treatment) over the course of 5 treatment cycles was allowed [see Clinical Studies (14.1)].
The population was almost entirely Caucasian (99%) with a median age of 51 years (range 18–82 years). Most patients (87%) were less than 65 years of age; 58.4% were women.
Common Adverse Reactions
The most commonly reported adverse reactions (occurring in 5% or more of patients who received 500 Units of DYSPORT in the placebo-controlled clinical trials) in cervical dystonia patients were: muscular weakness, dysphagia, dry mouth, injection site discomfort, fatigue, headache, musculoskeletal pain, dysphonia, injection site pain and eye disorders (consisting of blurred vision, diplopia, and reduced visual acuity and accommodation). Other than injection site reactions, most adverse reactions became noticeable about one week after treatment and lasted several weeks.
The rates of adverse reactions were higher in the combined controlled and open-label experience than in the placebo-controlled trials.
During the clinical studies, two patients (<1%) experienced adverse reactions leading to withdrawal. One patient experienced disturbance in attention, eyelid disorder, feeling abnormal and headache, and one patient experienced dysphagia.
Table 7 compares the incidence of the most frequent adverse reactions from a single treatment cycle of 500 Units of DYSPORT compared to placebo [see Clinical Studies (14.1)].
| Adverse Reactions | DYSPORT 500 Units (N=173) % | Placebo (N=182) % |
|---|---|---|
| Any Adverse Reaction | 61 | 51 |
|
||
| General disorders and administration site conditions | ||
| Injection site discomfort | 13 | 8 |
| Fatigue | 12 | 10 |
| Injection site pain | 5 | 4 |
| Musculoskeletal and connective tissue disorders | ||
| Muscular weakness | 16 | 4 |
| Musculoskeletal pain | 7 | 3 |
| Gastrointestinal disorders | ||
| Dysphagia | 15 | 4 |
| Dry mouth | 13 | 7 |
| Nervous system disorders | ||
| Headache | 11 | 9 |
| Respiratory, thoracic and mediastinal disorders | ||
| Dysphonia | 6 | 2 |
| Eye Disorders* | 7 | 2 |
Dose-response relationships for common adverse reactions in a randomized multiple fixed-dose study in which the total dose was divided between two muscles (the sternocleidomastoid and splenius capitis) are shown in Table 8.
|
Adverse Reactions | DYSPORT Dose | |||
|---|---|---|---|---|
| 250 Units % | 500 Units % | 1000 Units % | Placebo % |
|
|
||||
| Any Adverse Reaction | 37 | 65 | 83 | 30 |
| Dysphagia | 21 | 29 | 39 | 5 |
| Dry Mouth | 21 | 18 | 39 | 10 |
| Muscular Weakness | 11 | 12 | 56 | 0 |
| Injection Site Discomfort | 5 | 18 | 22 | 10 |
| Dysphonia | 0 | 18 | 28 | 0 |
| Facial Paresis | 5 | 0 | 11 | 0 |
| Eye Disorders* | 0 | 6 | 17 | 0 |
Glabellar Lines
In placebo-controlled clinical trials of DYSPORT, the most common adverse reactions (≥2%) following injection of DYSPORT were nasopharyngitis, headache, injection site pain, injection site reaction, upper respiratory tract infection, eyelid edema, eyelid ptosis, sinusitis, nausea, and blood present in urine.
Table 9 reflects exposure to DYSPORT in 398 patients 19 to 75 years of age who were evaluated in the randomized, placebo-controlled clinical studies that assessed the use of DYSPORT for the temporary improvement in the appearance of glabellar lines [see Clinical Studies (14.2)]. Adverse reactions of any cause occurred in 48% of the DYSPORT-treated patients and 33% of the placebo-treated patients.
| Adverse Reactions by Body System | DYSPORT (N=398) %* | Placebo (N=496) %* |
|---|---|---|
|
||
| Any Adverse Reaction | 48 | 33 |
| Eye Disorders | ||
| Eyelid Edema | 2 | 0 |
| Eyelid Ptosis | 2 | <1 |
| Gastrointestinal Disorders | ||
| Nausea | 2 | 1 |
| General Disorders and Administration Site Conditions | ||
| Injection Site Pain | 3 | 2 |
| Injection Site Reaction | 3 | <1 |
| Infections and Infestations | ||
| Nasopharyngitis | 10 | 4 |
| Upper Respiratory Tract Infection | 3 | 2 |
| Sinusitis | 2 | 1 |
| Investigations | ||
| Blood Present in Urine | 2 | <1 |
| Nervous System Disorders | ||
| Headache | 9 | 5 |
In the clinical trials safety database, where some patients received up to twelve treatments with DYSPORT, adverse reactions were reported for 57% (1425/2491) of patients. The most frequently reported of these adverse reactions were headache, nasopharyngitis, injection site pain, sinusitis, URI, injection site bruising, and injection site reaction (numbness, discomfort, erythema, tenderness, tingling, itching, stinging, warmth, irritation, tightness, swelling).
Adverse reactions that occurred after repeated injections in 2–3% of the population included bronchitis, influenza, pharyngolaryngeal pain, cough, contact dermatitis, injection site swelling, and injection site discomfort.
The incidence of eyelid ptosis did not increase in the long-term safety studies with multiple re-treatments at intervals ≥ three months. The majority of the reports of eyelid ptosis were mild to moderate in severity and resolved over several weeks [see Dosage and Administration (2.4)].
Spasticity in Adults
Upper Limb Spasticity in Adults
Table 10 lists the adverse reactions that occurred in ≥2% of patients in any DYSPORT dose group and more frequent than placebo in double-blind studies evaluating the treatment of upper limb spasticity in adults. The most common adverse reactions (≥4%) in any DYSPORT dose group was muscular weakness.
| DYSPORT | Placebo | ||
|---|---|---|---|
| Adverse Reactions | 500 Units (N=197) % | 1000 Units (N=194) % |
(N=279) % |
| Infections and infestations | |||
| Influenza | 1 | 2 | 1 |
| Infection | 1 | 2 | 1 |
| Musculoskeletal and connective tissue disorders | |||
| Muscular weakness | 2 | 4 | 1 |
| Pain in extremity | 0 | 2 | 1 |
| Back pain | 1 | 2 | 1 |
| Nervous system disorders | |||
| Headache | 1 | 2 | 1 |
| Convulsion | 2 | 2 | 1 |
| Syncope | 1 | 2 | 0 |
| Hypoesthesia | 0 | 2 | <1 |
| Partial seizures | 0 | 2 | 0 |
| General disorders and administration site conditions | |||
| Fatigue | 2 | 2 | 0 |
| Asthenia | 2 | 1 | <1 |
| Injury, poisoning and procedural complications | |||
| Fall | 2 | 3 | 2 |
| Injury | 2 | 2 | 1 |
| Contusion | 1 | 2 | <1 |
| Gastrointestinal disorders | |||
| Diarrhea | 1 | 2 | <1 |
| Constipation | 0 | 2 | 1 |
| Investigation | |||
| Blood triglycerides increased | 2 | 1 | 0 |
| Respiratory, thoracic and mediastinal disorders | |||
| Cough | 1 | 2 | 1 |
| Vascular disorders | |||
| Hypertension | 1 | 2 | <1 |
| Psychiatric disorders | |||
| Depression | 2 | 3 | 1 |
6.2 Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity.
The incidence of antibody formation is highly dependent on the sensitivity and specificity of the assay. In addition, the observed incidence of antibody positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies across products in this class may be misleading.
6.3 Postmarketing Experience
Because adverse reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following adverse reactions have been identified during post-approval use of DYSPORT: vertigo, photophobia, influenza-like illness, amyotrophy, burning sensation, facial paresis, hypoesthesia, erythema, dry eye, and excessive granulation tissue. Hypersensitivity reactions including anaphylaxis have been reported.
7. Drug Interactions
7.1 Aminoglycosides and Other Agents Interfering with Neuromuscular Transmission
Co-administration of DYSPORT and aminoglycosides or other agents interfering with neuromuscular transmission (e.g., curare-like agents) should only be performed with caution because the effect of the botulinum toxin may be potentiated. If co-administered, observe the patient closely.
7.2 Anticholinergic Drugs
Use of anticholinergic drugs after administration of DYSPORT may potentiate systemic anticholinergic effects such as blurred vision.
7.3 Other Botulinum Neurotoxin Products
The effect of administering botulinum neurotoxin products including DYSPORT, at the same time or within several months of each other is unknown. Excessive weakness may be exacerbated by another administration of botulinum toxin prior to the resolution of the effects of a previously administered botulinum toxin.
8. Use In Specific Populations
8.4 Pediatric Use
10. Overdosage
Excessive doses of DYSPORT may be expected to produce neuromuscular weakness with a variety of symptoms. Respiratory support may be required where excessive doses cause paralysis of respiratory muscles. In the event of overdose, the patient should be medically monitored for symptoms of excessive muscle weakness or muscle paralysis [see Boxed Warning and Warnings and Precautions (5.2)]. Symptomatic treatment may be necessary.
Symptoms of overdose are likely not to be present immediately following injection. Should accidental injection or oral ingestion occur, the person should be medically supervised for several weeks for signs and symptoms of excessive muscle weakness or paralysis.
There is no significant information regarding overdose from clinical studies.
In the event of overdose, antitoxin raised against botulinum toxin is available from the Centers for Disease Control and Prevention (CDC) in Atlanta, GA. However, the antitoxin will not reverse any botulinum toxin-induced effects already apparent by the time of antitoxin administration. In the event of suspected or actual cases of botulinum toxin poisoning, please contact your local or state Health Department to process a request for antitoxin through the CDC. If you do not receive a response within 30 minutes, please contact the CDC directly at 770-488-7100. More information can be obtained at https://www.cdc.gov/laboratory/drugservice/index.html.
11. Dysport Description
Botulinum toxin type A, the active ingredient in DYSPORT, is a purified neurotoxin type A complex produced by fermentation of the bacterium Clostridium botulinum type A, Hall Strain. It is purified from the culture supernatant by a series of precipitation, dialysis, and chromatography steps. The neurotoxin complex is composed of the neurotoxin, hemagglutinin proteins and non-toxin non-hemagglutinin protein.
DYSPORT® (abobotulinumtoxinA) for injection is a sterile, lyophilized powder supplied in a single-dose vial for reconstitution intended for intramuscular injection. Each vial contains 300 Units or 500 Units of lyophilized abobotulinumtoxinA, human serum albumin (125 mcg) and lactose (2.5 mg). DYSPORT may contain trace amounts of cow's milk proteins [see Contraindications (4) and Warnings and Precautions (5.3)].
The primary release procedure for DYSPORT uses a cell-based potency assay to determine the potency relative to a reference standard. The assay and reference material are specific to DYSPORT. One unit of DYSPORT corresponds to the calculated median lethal intraperitoneal dose (LD50) in mice. Due to specific details of the assay system, such as vehicle, dilution scheme and laboratory protocols, Units of biological activity of DYSPORT cannot be converted into Units of any other botulinum toxin or any toxin assessed with any other specific assay method.
12. Dysport - Clinical Pharmacology
12.1 Mechanism of Action
DYSPORT inhibits release of the neurotransmitter, acetylcholine, from peripheral cholinergic nerve endings. Toxin activity occurs in the following sequence: Toxin heavy chain mediated binding to specific surface receptors on nerve endings, internalization of the toxin by receptor mediated endocytosis, pH-induced translocation of the toxin light chain to the cell cytosol and cleavage of SNAP25 leading to intracellular blockage of neurotransmitter exocytosis into the neuromuscular junction. This accounts for the therapeutic utility of the toxin in diseases characterized by excessive efferent activity in motor nerves.
Recovery of transmission occurs gradually as the neuromuscular junction recovers from SNAP25 cleavage and as new nerve endings are formed.
14. Clinical Studies
14.1 Cervical Dystonia
The efficacy of DYSPORT was evaluated in two randomized, double-blind, placebo-controlled, single-dose, parallel-group studies in treatment-naive cervical dystonia patients. The principal analyses from these trials provide the primary demonstration of efficacy involving 252 patients (121 on DYSPORT, 131 on placebo) with 36% male and 64% female. Ninety-nine percent of the patients were Caucasian.
In both placebo-controlled studies (Study 1 and Study 2), a dose of 500 Units of DYSPORT was given by intramuscular injection divided among two to four affected muscles. These studies were followed by long-term open-label extensions that allowed titration in 250 Unit steps to doses in a range of 250 to 1000 Units, after the initial dose of 500 Units. In the extension studies, re-treatment was determined by clinical need after a minimum of 12 weeks. The median time to re-treatment was 14 weeks and 18 weeks for the 75th percentile.
The primary assessment of efficacy was based on the total Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS) change from baseline at Week 4 for both studies. The scale evaluates the severity of dystonia, patient-perceived disability from dystonia, and pain. The adjusted mean change from baseline in the TWSTRS total score was statistically significantly greater for the DYSPORT group than the placebo group at Week 4 in both studies (see Table 14).
| Study 1 | Study 2 | |||
|---|---|---|---|---|
| DYSPORT 500 Units N=55 | Placebo N=61 | DYSPORT 500 Units N=37 | Placebo N=43 |
|
|
||||
| Baseline (Week 0) | ||||
| Mean (SD) | 43.8 (8.0) | 45.8 (8.9) | 45.1 (8.7) | 46.2 (9.4) |
| Week 4 | ||||
| Mean (SD) | 30.0 (12.7) | 40.2 (11.8) | 35.2 (13.8) | 42.4 (12.2) |
| Change from Baseline* | -15.6 (2.0) | -6.7 (2.0) | -9.6 (2.0) | -3.7 (1.8) |
| Treatment difference | -8.9† | -5.9† | ||
| 95% confidence interval | [-12.9 to -4.7] | [-10.6 to -1.3] | ||
| Week 8 |
|
|||
| Mean (SD) | 29.3 (11.0) | 39.6 (13.5) | ||
| Change from Baseline* | -14.7 (2.0) | -5.9 (2.0) | ||
| Treatment difference | -8.8† | |||
| 95% confidence interval | [-12.9 to -4.7] | |||
Analyses by gender, weight, geographic region, underlying pain, cervical dystonia severity at baseline and history of treatment with botulinum toxin did not show any meaningful differences between groups.
Table 15 indicates the average DYSPORT dose, and percentage of total dose, injected into specific muscles in the pivotal clinical trials.
| Number of patients injected per muscle* | DYSPORT Dose Injected | Percentage of the total DYSPORT Dose Injected | |||
|---|---|---|---|---|---|
| Median [DYSPORT Units] (min, max) | 75th percentile [DYSPORT Units] | Median [%] (min, max) | 75th percentile [%] |
||
|
|||||
| Sternocleidomastoid | 90 | 125 Units (50, 350) | 150 Units | 26.5 % (10, 70) | 30.0 % |
| Splenius capitis | 85 | 200 Units (75, 450) | 250 Units | 40.0 % (15, 90) | 50.0 % |
| Trapezius | 50 | 102.6 Units (50, 300) | 150 Units | 20.6 % (10, 60) | 30.0 % |
| Levator scapulae | 35 | 105.3 Units (50, 200) | 125 Units | 21.1 % (10, 40) | 25.0 % |
| Scalenus (medius and anterior) | 26 | 115.5 Units (50, 300) | 150 Units | 23.1 % (10, 60) | 30.0 % |
| Semispinalis capitis | 21 | 131.6 Units (50, 250) | 175 Units | 29.4 % (10, 50) | 35.0 % |
| Longissimus | 3 | 150 Units (100, 200) | 200 Units | 30.0 % (20, 40) | 40.0 % |
14.2 Glabellar Lines
Three double-blind, randomized, placebo-controlled, clinical studies evaluated the efficacy of DYSPORT for use in the temporary improvement of the appearance of moderate to severe glabellar lines. These three studies enrolled healthy adults (ages 19-75) with glabellar lines of at least moderate severity at maximum frown. Subjects were excluded if they had marked ptosis, deep dermal scarring, or a substantial inability to lessen glabellar lines, even by physically spreading them apart. The subjects in these studies received either DYSPORT or placebo. The total dose was delivered in equally divided aliquots to specified injection sites (see Figure 1).
Investigators and subjects assessed efficacy at maximum frown by using a 4-point scale (none, mild, moderate, severe).
Overall treatment success was defined as post-treatment glabellar line severity of none or mild with at least 2 grade improvement from baseline for the combined investigator and subject assessments (composite assessment) on Day 30 (see Table 16). Additional endpoints for each of the studies were post-treatment glabellar line severity of none or mild with at least a 1 grade improvement from baseline for the separate investigator and subject assessments on Day 30.
After completion of the randomized studies, subjects were offered participation in a two-year, open-label re-treatment study to assess the safety of multiple treatments.
| 2 Grade Improvement | ||
|---|---|---|
| Study | DYSPORT n/N (%) | Placebo n/N (%) |
| GL-1 | 58/105 (55%) | 0/53 (0%) |
| GL-2 | 37/71 (52%) | 0/71 (0%) |
| GL-3 | 120/200 (60%) | 0/100 (0%) |
Treatment with DYSPORT reduced the severity of glabellar lines for up to four months.
Study GL-1
Study GL-1 was a single-dose, double-blind, multicenter, randomized, placebo-controlled study in which 158 previously untreated subjects received either placebo or 50 Units of DYSPORT, administered in five aliquots of 10 Units (see Figure 1). Subjects were followed for 180 days. The mean age was 43 years; most of the subjects were women (85%), and predominantly Caucasian (49%) or Hispanic (47%). At Day 30, 55% of DYSPORT-treated subjects achieved treatment success: a composite 2 grade improvement of glabellar line severity at maximum frown (see Table 16).
In study GL-1, the reduction of glabellar line severity at maximum frown was greater at Day 30 in the DYSPORT group compared to the placebo group as assessed by both Investigators and subjects (see Table 17).
| Investigators' Assessment | Subjects' Assessment | |||
|---|---|---|---|---|
| Day | DYSPORT N=105 | Placebo N=53 | DYSPORT N=105 | Placebo N=53 |
| 14 | 90% 95 | 17% 9 | 77% 81 | 9% 5 |
| 30 | 88% 92 | 4% 2 | 74% 78 | 9% 5 |
| 60 | 64% 67 | 2% 1 | 60% 63 | 6% 3 |
| 90 | 43% 45 | 6% 3 | 36% 38 | 6% 3 |
| 120 | 23% 24 | 4% 2 | 19% 20 | 6% 3 |
| 150 | 9% 9 | 2% 1 | 8% 8 | 4% 2 |
| 180 | 6% 6 | 0% 0 | 7% 7 | 8% 4 |
Study GL-2
Study GL-2 was a repeat-dose, double-blind, multicenter, placebo-controlled, randomized study. The study was initiated with two or three open-label treatment cycles of 50 Units of DYSPORT administered in five aliquots of 10 Units DYSPORT (see Figure 1). After the open-label treatments, subjects were randomized to receive either placebo or 50 Units of DYSPORT. Subjects could have received up to four treatments through the course of the study. Efficacy was assessed in the final randomized treatment cycle. The study enrolled 311 subjects into the first treatment cycle and 142 subjects were randomized into the final treatment cycle. Overall, the mean age was 47 years; most of the subjects were women (86%) and predominantly Caucasian (80%).
At Day 30, 52% of DYSPORT-treated subjects achieved treatment success: a composite 2 grade improvement of glabellar line severity at maximum frown (see Table 16).
The proportion of responders in the final treatment cycle was comparable to the proportion of responders in all prior treatment cycles.
After the final repeat treatment with DYSPORT, the reduction of glabellar line severity at maximum frown was greater at Day 30 in the DYSPORT group compared to the placebo group as assessed by both Investigators and subjects (see Table 18).
| Investigators' Assessment | Subjects' Assessment | |||
|---|---|---|---|---|
| Day | DYSPORT N=71 | Placebo N=71 | DYSPORT N=71 | Placebo N=71 |
| 30 | 85% 60 | 4% 3 | 79% 56 | 1% 1 |
Study GL-3
Study GL-3 was a single-dose, double-blind, multicenter, randomized, placebo-controlled study in which 300 previously untreated subjects received either placebo or 50 Units of DYSPORT, administered in five aliquots of 10 Units (see Figure 1). Subjects were followed for 150 days. The mean age was 44 years; most of the subjects were women (87%), and predominantly Caucasian (75%) or Hispanic (18%).
At Day 30, 60% of DYSPORT-treated subjects achieved treatment success: a composite 2 grade improvement of glabellar line severity at maximum frown (see Table 16).
In study GL-3, the reduction of glabellar line severity at maximum frown was greater at Day 30 in the DYSPORT group compared to the placebo group as assessed by both Investigators and subjects (see Table 19).
| Investigators' Assessment | Subjects' Assessment | |||
|---|---|---|---|---|
| Day | DYSPORT N=200 | Placebo N=100 | DYSPORT N=200 | Placebo N=100 |
| 14 | 83% 166 | 5% 5 | 83% 165 | 2% 2 |
| 30 | 86% 171 | 0% 0 | 82% 163 | 2% 2 |
| 60 | 75% 150 | 1% 1 | 65% 130 | 4% 4 |
| 90 | 51% 102 | 1% 1 | 46% 91 | 2% 2 |
| 120 | 29% 58 | 1% 1 | 31% 61 | 3% 3 |
| 150 | 16% 32 | 1% 1 | 16% 31 | 3% 3 |
14.3 Spasticity in Adults
Upper Limb Spasticity
The efficacy and safety of DYSPORT for the treatment of upper limb spasticity in adults was evaluated in a randomized, multicenter, double-blind, placebo-controlled study that included 238 patients (159 DYSPORT and 79 placebo) with upper limb spasticity (Modified Ashworth Scale (MAS) score ≥2 in the primary targeted muscle group for toxin-naive patients or MAS score ≥3 in the primary targeted muscle group for toxin non-naive patients at least 4 months after the last botulinum toxin injection, of any serotype) who were at least 6 months post-stroke or post-traumatic brain injury. The median age of the patients in this study was 55 years (range 18 to 78 years), 64% were male, and 86% were Caucasian.
DYSPORT 500 Units (N=80), DYSPORT 1000 Units (N=79), or placebo (N=79) was injected intramuscularly into the affected upper limb muscles. After injection of the primary targeted muscle groups (PTMG), the remainder of the dose was injected into at least two additional upper limb muscles determined by the patient's individual presentation. Table 20 provides the mean and range of DYSPORT doses injected and the number of injections into specific muscles of the upper limb.
| Muscle | DYSPORT Treatment Group | Number of Patients | Mean DYSPORT Units Injected (Min, Max) | Number of Injection Sites Median, [Q1 ; Q3] |
|---|---|---|---|---|
|
||||
| Flexor digitorum profundus (FDP)* | 500 U | 54 | 93.5 Units (50 to 100) | 1, [1 ; 2] |
| 1000 U | 65 | 195.5 Units (100 to 300) | 2, [1 ; 2] | |
| Flexor digitorum superficialis (FDS)* | 500 U | 63 | 95.4 Units (50 to 100) | 2, [1 ; 2] |
| 1000 U | 73 | 196.8 Units (100 to 300) | 2, [1 ; 2] | |
| Flexor carpi radialis (FCR)* | 500 U | 57 | 92.2 Units (25 to 100) | 1, [1 ; 2] |
| 1000 U | 57 | 178.1 Units (80 to 300) | 1, [1 ; 2] | |
| Flexor carpi ulnaris (FCU)* | 500 U | 47 | 89.9 Units (25 to 180) | 1, [1 ; 2] |
| 1000 U | 49 | 171.2 Units (80 to 200) | 1, [1 ; 2] | |
| Brachialis* | 500 U | 60 | 148.5 Units (50 to 200) | 2, [1 ; 2] |
| 1000 U | 43 | 321.4 Units (100 to 400) | 2, [2 ; 2] | |
| Brachioradialis* | 500 U | 42 | 88.3 Units (50 to 200) | 1, [1 ; 2] |
| 1000 U | 28 | 172.1 Units (50 to 200) | 1, [1 ; 2] | |
| Biceps Brachii (BB) | 500 U | 28 | 106.4 Units (50 to 200) | 2, [1 ; 2] |
| 1000 U | 19 | 207.4 Units (100 to 400) | 2, [1 ; 2] | |
| Pronator Teres | 500 U | 14 | 81.8 Units (45 to 200) | 1, [1 ; 1] |
| 1000 U | 30 | 157.3 Units (80 to 200) | 1, [1 ; 1] | |
The co-primary efficacy variables were muscle tone assessed by the MAS at the primary targeted muscle group at Week 4 and the Physician Global Assessment (PGA; ranges from –4 = markedly worse to +4= markedly improved) at Week 4 (see Table 21).
| Placebo (N=79) | DYSPORT | ||
|---|---|---|---|
| (500 Units) (N=80) | (1000 Units) (N=79) |
||
| LS= Least Square; | |||
|
|||
| LS Mean Change from Baseline in PTMG Muscle Tone on the MAS | -0.3 | -1.2* | -1.4* |
| LS Mean PGA of Response to Treatment | 0.7 | 1.4* | 1.8* |
| LS Mean Change from Baseline in Wrist Flexor Muscle Tone on the MAS | -0.3 (n=54) | -1.4 (n=57) | -1.6 (n=58) |
| LS Mean Change from Baseline in Finger Flexor Muscle Tone on the MAS | -0.3 (n=70) | -0.9 (n=66) | -1.2 (n=73) |
| LS Mean Change from Baseline in Elbow Flexor Muscle Tone on the MAS | -0.3 (n=56) | -1.0 (n=61) | -1.2 (n=48) |
Lower Limb Spasticity
The efficacy of DYSPORT for the treatment of lower limb spasticity was evaluated in a randomized, multicenter, double-blind, placebo-controlled study that included 381 patients (253 DYSPORT and 128 placebo). Patients had lower limb spasticity (Modified Ashworth Scale (MAS) score ≥2 in the affected ankle joint for toxin-naive patients, or MAS score ≥3 in the affected ankle joint for toxin non-naive patients) and were at least 6 months post-stroke or post-traumatic brain injury.
Table 22 provides the median DYSPORT doses injected and the number of injections into specific muscles of the lower limb as reported in the double-blind study. In the study, the gastrocnemius and soleus muscles, and at least one additional lower limb muscle were injected, according to the clinical presentation.
| Injected Muscle | DYSPORT Units Injected | Number of Injection Sites |
|---|---|---|
| Gastrocnemius Lateral | 100 Units to 150 Units | 1 |
| Medial | 100 Units to 150 Units | 1 |
| Soleus | 333 Units to 500 Units | 3 |
| Tibialis posterior | 200 Units to 300 Units | 2 |
| Flexor digitorum longus | 133 Units to 200 Units | 1 to 2 |
| Flexor hallucis longus | 67 Units to 200 Units | 1 |
The primary efficacy variable was muscle tone assessed by the MAS at the ankle joint at Week 4. The first secondary endpoint was the Physician Global Assessment at Week 4 (see Table 23).
| LS Mean Change from Baseline on the Modified Ashworth Scale | DYSPORT 1000 Units (N=125) | DYSPORT 1500 Units (N=128) | Placebo (N=128) |
|---|---|---|---|
|
|||
| Week 4 | -0.6 | -0.8* | -0.5 |
| LS Mean Physician Global Assessment Score Investigator | |||
| Week 4 | 0.9 | 0.9 | 0.7 |
14.4 Spasticity in Pediatric Patients
Upper Limb Spasticity in Pediatric Patients
The efficacy of DYSPORT for the treatment of upper limb spasticity in pediatric patients 2 to 17 years of age was evaluated in a double-blind, low-dose controlled, multicenter study (NCT02106351). A total of 208 patients with spasticity because of cerebral palsy who were toxin naive or non-naive (66% had prior treatment with a botulinum toxin), weighed at least 10 kgs, and had a baseline Modified Ashworth Score (MAS) of grade 2 or greater (99% patients) at the primary targeted muscle groups (PTMG) were enrolled in the modified Intention to Treat population (mITT). Patients received DYSPORT 16 Units/kg (n=70), DYSPORT 8 Units/kg (n=69), or DYSPORT 2 Units/kg (n=69) injected into the upper limb. The elbow flexors and wrist flexors respectively were the PTMG in 57% and in 43% of patients. The median age of the patients in this study was 9 years (range 2 to 17 years; 57% were between 2 and 9 years of age); 60% of patients were male, and 75% were White.
The primary efficacy endpoint was the mean change from baseline in MAS in the PTMG at Week 6 (see Table 24). The secondary efficacy endpoint was the mean Physician Global Assessment (PGA) score assessed at Week 6 (Table 25). Although PGA scores numerically favored DYSPORT treatment over the low-dose control, the difference was not statistically significant.
| Control Group | Treatment Groups | ||
|---|---|---|---|
| DYSPORT 2 U/kg (N=69) | DYSPORT 8 U/kg (N=69) | DYSPORT 16 U/kg (N=70) |
|
|
|||
| Baseline | |||
| Mean (SD) | 3.1 (0.3) | 3.1 (0.3) | 3.1 (0.5) |
| Week 6 | |||
| LS* mean change from baseline in PTMG† on MAS | -1.6 | -2.0 | -2.3 |
| Difference from control in LS* means | -0.4 | -0.7 | |
| p-value ‡ | 0.0118§ | <0.0001 | |
| Week 16 | |||
| LS mean change from baseline in PTMG† on MAS | -0.9 | -1.2 | -1.5 |
| Difference from control in LS* means | -0.3§ | -0.6§ | |
| Control Group | Treatment Groups | ||
|---|---|---|---|
| Dysport 2 U/kg (N=68) | Dysport 8 U/kg (N=69) | Dysport 16 U/kg (N=70) |
|
|
|||
| Week 6 | |||
| Mean score (SD) | 1.7 (0.9) | 2.0 (0.9) | 2.0 (0.9) |
| LS* mean in PGA | 1.8 | 2.0 | 2.0 |
| Difference from control in LS* means | 0.2 | 0.2 | |
| p-value † | 0.2043 | 0.1880 | |
| Week 16 | |||
| Mean score (SD) | 1.7 (1.0) | 1.6 (1.1) | 1.9 (1.2) |
| LS* mean in PGA | 1.8 | 1.7 | 1.9 |
| Difference from control in LS* means | -0.1 | 0.1 | |
| p-value † | 0.7001 | 0.4041 | |
Lower Limb Spasticity in Pediatric Patients
The efficacy of DYSPORT for the treatment of lower limb spasticity in patients 2 to 17 years of age was evaluated in a double-blind, placebo-controlled, multicenter study . A total of 235 patients with cerebral palsy causing dynamic equinus foot deformity who were toxin-naive or non-naive and had a Modified Ashworth Score (MAS) of grade 2 or greater at the ankle plantar flexors were enrolled. Patients received DYSPORT 10 Units/kg/leg (n=79), DYSPORT 15 Units/kg/leg (n=79) or placebo (n=77) injected into the gastrocnemius and soleus muscles (see Table 27). Forty-one percent of patients (n=66) were treated bilaterally and received a total lower limb DYSPORT dose of either 20 Units/kg (n=37) or 30 Units/kg (n=29). The median age of the patients in this study was 5 years (range 2 to 17 years); 60% of patients were male, and 73% were Caucasian.
The primary efficacy endpoint was the mean change from baseline in MAS in ankle plantar flexor at Week 4; a co-primary endpoint was the mean Physician's Global Assessment (PGA) score at Week 4 (see Table 26).
| Placebo (N=77) | DYSPORT 10 Units/kg/leg (N=79) | DYSPORT 15 Units/kg/leg (N=79) |
||
|---|---|---|---|---|
| LS=Least Square | ||||
|
||||
| LS Mean Change from Baseline in Ankle plantar flexor Muscle Tone on the MAS | Week 4 | -0.5 | -0.9* | -1.0* |
| Week 12 | -0.5 | -0.8* | -1.0* | |
| LS Mean PGA of Response to Treatment | Week 4 | 0.7 | 1.5* | 1.5* |
| Week 12 | 0.4 | 0.8* | 1.0* | |
16. How is Dysport supplied
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised 7/2020 | |||
|
MEDICATION GUIDE |
||||
|
What is the most important information I should know about DYSPORT? DYSPORT may cause serious side effects that can be life threatening including:
These problems can happen within hours, or days to weeks after an injection of DYSPORT. Call your doctor or get medical help right away if you have any of these problems after treatment with DYSPORT: 1. Problems swallowing, speaking, or breathing. These problems can happen within hours, or days to weeks after an injection of DYSPORT usually because the muscles that you use to breathe and swallow can become weak after the injection. Death can happen as a complication if you have severe problems with swallowing or breathing after treatment with DYSPORT.
2. Spread of toxin effects. In some cases, the effect of botulinum toxin may affect areas of the body away from the injection site and cause symptoms of a serious condition called botulism. The symptoms of botulism include: |
||||
|
|
|||
|
These symptoms can happen within hours, or days to weeks after you receive an injection of DYSPORT. These problems could make it unsafe for you to drive a car or do other dangerous activities. See "What should I avoid while receiving DYSPORT?" |
||||
|
What is DYSPORT? DYSPORT is a prescription medicine that is injected into muscles and used:
It is not known whether DYSPORT is safe or effective in people younger than:
It is not known whether DYSPORT is safe or effective for the treatment of other wrinkles. |
||||
|
Who should not take DYSPORT? Do not take DYSPORT if you:
|
||||
|
What should I tell my doctor before taking DYSPORT? Tell your doctor about all your medical conditions, including if you:
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins and herbal products. Using DYSPORT with certain other medicines may cause serious side effects. Do not start any new medicines until you have told your doctor that you have received DYSPORT in the past. Especially tell your doctor if you:
Ask your doctor if you are not sure if your medicine is one that is listed above. Know the medicines you take. Keep a list of your medicines with you to show your doctor and pharmacist each time you get a new medicine. |
||||
|
How will I receive DYSPORT?
|
||||
|
What should I avoid while receiving DYSPORT? DYSPORT may cause loss of strength or general muscle weakness, blurred vision, or drooping eyelids within hours to weeks of taking DYSPORT. If this happens, do not drive a car, operate machinery, or do other dangerous activities. See "What is the most important information I should know about DYSPORT?" |
||||
|
What are the possible side effects of DYSPORT? DYSPORT can cause serious side effects. See "What is the most important information I should know about DYSPORT?" The most common side effects of DYSPORT in people with cervical dystonia include: |
||||
|
|
|
||
|
The most common side effects of DYSPORT in people with glabellar lines include: |
||||
|
|
|
||
|
The most common side effect of DYSPORT in adults with upper limb spasticity include: |
||||
| ||||
|
The most common side effects of DYSPORT in adults with lower limb spasticity include: |
||||
|
|
|
||
|
The most common side effects of DYSPORT in children (2 to 17 years of age) with upper limb spasticity include: |
||||
|
| |||
|
The most common side effects of DYSPORT in children (2 to 17 years of age) with lower limb spasticity include: |
||||
|
|
|
||
|
Tell your doctor if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of DYSPORT. For more information, ask your doctor or pharmacist. Tell your doctor if you have dry eye or changes in vision following use of DYSPORT. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||||
|
General information about DYSPORT: Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. This Medication Guide summarizes the most important information about DYSPORT. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information about DYSPORT that is written for healthcare professionals. |
||||
|
What are the ingredients in DYSPORT? Active ingredient: (botulinum toxin Type A) Inactive ingredients: human albumin and lactose. DYSPORT may contain cow's milk protein. |
||||
|
Distributed by: Ipsen Biopharmaceuticals, Inc. Cambridge, MA 02142 and Galderma Laboratories, L.P. Fort Worth, TX 76177; Manufactured by: Ipsen Biopharm Ltd., Wrexham, LL13 9UF, UK U.S. License No. 1787 For more information about DYSPORT, call 855-463-5127 or go to www.dysport.com or www.DysportUSA.com. |
||||
DYSPORT is a registered trademark of Ipsen Biopharm Limited. Botox, Xeomin and Myobloc are registered trademarks of their respective owners.
© 2020. All rights reserved.
| DYSPORT
botulinum toxin type a injection, powder, lyophilized, for solution |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| DYSPORT
botulinum toxin type a injection, powder, lyophilized, for solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Ipsen Biopharmaceuticals, Inc. (118461578) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| IPSEN BIOPHARM LTD | 365113203 | MANUFACTURE(15054-0500, 15054-0530) | |