Drug Detail:Enjaymo (Sutimlimab-jome)
Drug Class: Selective immunosuppressants
Highlights of Prescribing Information
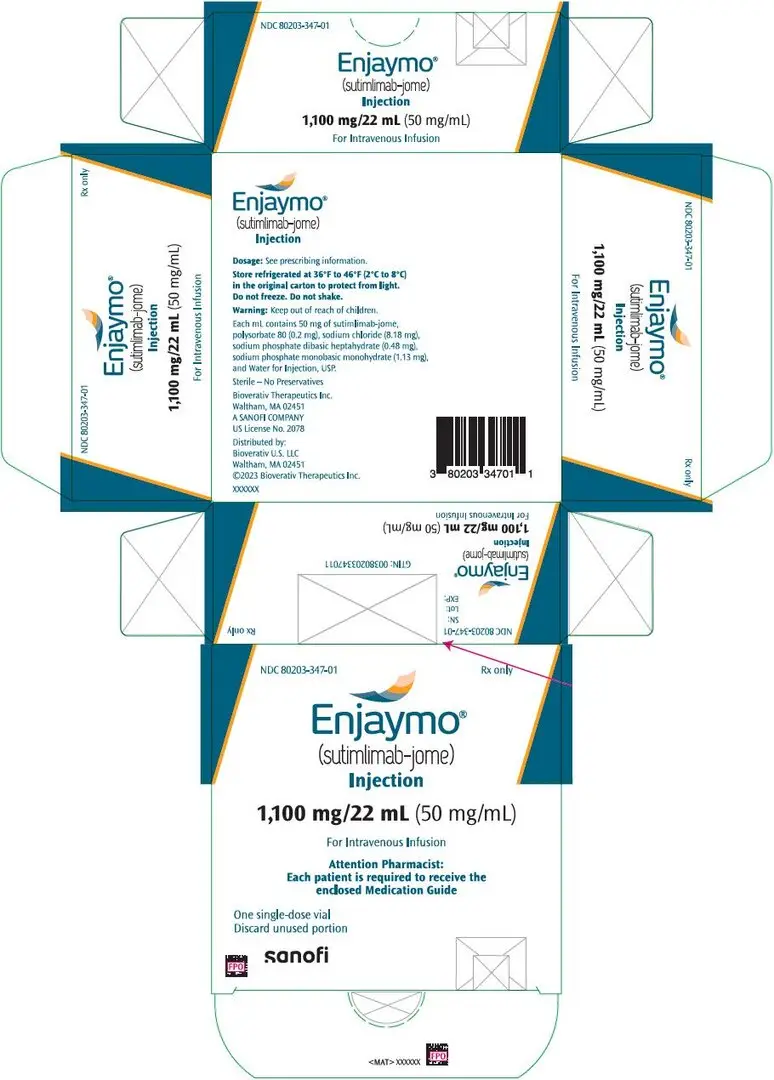
ENJAYMO ® (sutimlimab-jome) injection, for intravenous use
Initial U.S. Approval: 2022
Recent Major Changes
| Indications and Usage ( 1) | 01/2023 |
| Dosage and Administration ( 2.3) | 01/2023 |
| Warnings and Precautions ( 5.1, 5.2) | 01/2023 |
Indications and Usage for Enjaymo
ENJAYMO is a classical complement inhibitor indicated for the treatment of hemolysis in adults with cold agglutinin disease (CAD). ( 1)
Enjaymo Dosage and Administration
- Vaccinate against encapsulated bacteria at least two weeks prior to treatment. ( 2.1)
- Weight-based dosage weekly for two weeks then every two weeks:
- For patients weighing 39 kg to less than 75 kg: 6,500 mg by intravenous infusion. ( 2.2)
- For patients weighing 75 kg or more: 7,500 mg by intravenous infusion. ( 2.2)
- See Full Prescribing Information for important preparation and administration instructions. ( 2.2, 2.3)
Dosage Forms and Strengths
Injection: 1,100 mg/22 mL (50 mg/mL) in a single-dose vial ( 3)
Contraindications
ENJAYMO is contraindicated in patients with known hypersensitivity to sutimlimab-jome or any of the inactive ingredients. ( 4)
Warnings and Precautions
- Serious Infections: Ensure patients are vaccinated against encapsulated bacteria. Monitor patients for early signs and symptoms of infections. ( 5.1)
- Infusion-Related Reactions: Monitor patients for infusion-related reactions, interrupt if reaction occurs, and institute appropriate medical management as needed. ( 5.2)
- Risk of Autoimmune Disease: Monitor patients for signs and symptoms and manage medically. ( 5.3)
- Recurrent Hemolysis After ENJAYMO Discontinuation: Monitor patients for signs and symptoms of hemolysis if treatment with ENJAYMO is interrupted. ( 5.4)
Adverse Reactions/Side Effects
Most common adverse reactions in the CADENZA study (Part A) (incidence ≥18%) are rhinitis, headache, hypertension, acrocyanosis, and Raynaud's phenomenon. The most common adverse reactions in the CARDINAL study (incidence ≥25%) are urinary tract infection, respiratory tract infection, bacterial infection, dizziness, fatigue, peripheral edema, arthralgia, cough, hypertension, and nausea. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Bioverativ Therapeutics Inc. (A SANOFI COMPANY) at 1-800-745-4447 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 3/2023
Full Prescribing Information
2. Enjaymo Dosage and Administration
2.1 Recommended Vaccinations
Vaccinate patients against encapsulated bacteria at least 2 weeks prior to initiation of ENJAYMO therapy according to the most current Advisory Committee on Immunization Practices (ACIP) recommendations for patients with persistent complement deficiencies [see Warnings and Precautions (5.1)]. If urgent ENJAYMO therapy is indicated in an unvaccinated patient, administer vaccine(s) as soon as possible.
2.2 Recommended Dosage Regimen
The recommended dosage of ENJAYMO for patients with CAD is based on body weight. For patients weighing 39 kg to less than 75 kg, the recommended dose is 6,500 mg and for patients weighing 75 kg or more, the recommended dose is 7,500 mg. Administer ENJAYMO intravenously weekly for the first two weeks, with administration every two weeks thereafter. Administer ENJAYMO at the recommended dosage regimen time points, or within two days of these time points.
If a dose is missed, administer as soon as possible; thereafter, resume dosing every two weeks. If the duration after the last dose exceeds 17 days, administer ENJAYMO weekly for two weeks, with administration every two weeks thereafter.
2.3 Preparation and Administration
ENJAYMO is for intravenous infusion only.
Each vial of ENJAYMO is intended for single dose only.
ENJAYMO can either be used as an undiluted or diluted preparation.
Undiluted preparation of ENJAYMO
Use aseptic technique to prepare ENJAYMO as follows:
- Remove ENJAYMO from the refrigerator. To minimize foaming, do not shake ENJAYMO.
- Inspect vials visually for particulate matter and discoloration prior to administration. ENJAYMO solution is a clear to slightly opalescent and colorless to slightly yellow liquid. Do not administer if discolored or if other foreign particulate matter is present.
- Withdraw the calculated volume of ENJAYMO from the appropriate number of vials based on the recommended dosage (see Table 1) and add to an empty infusion bag.
- Prior to administration, allow the infusion solution to adjust to room temperature (59°F to 77°F (15°C to 25°C). Refer to Table 1 for infusion rate. The infusion should be administered over 1 hour. Administer ENJAYMO infusion solution only through a 0.2 micron in-line filter with a polyethersulfone (PES) membrane.
- The infusion catheter and tubing should be primed with the dosing solution immediately before infusion and flushed immediately following completion of the infusion with a sufficient quantity (approximately 20 mL) of sterile 0.9% Sodium Chloride Injection, USP.
- If the ENJAYMO infusion solution is not used immediately, store refrigerated at 36°F to 46°F (2°C to 8°C).
- Once removed from refrigeration, allow the ENJAYMO infusion solution to adjust to room temperature 59°F to 77°F (15°C to 25°C) and administer within 8 hours. Total time from the time of preparation, including refrigeration, adjustment to room temperature and the expected infusion time should not exceed 36 hours. In-line infusion warmers may be used, do not exceed a temperature of 104°F (40°C).
- No incompatibilities have been observed between ENJAYMO infusion solution and infusion bags made of Di-(2-ethylhexyl)phthalate (DEHP) plasticized polyvinyl chloride (PVC), Ethyl Vinyl Acetate (EVA) and polyolefin (PO); administration sets made of DEHP-plasticized PVC, DEHP-free polypropylene (PP) and polyethylene (PE); and vial adapters made of polycarbonate (PC) and acrylonitrile-butadiene-styrene (ABS).
| Body Weight Range | Dose | Number of ENJAYMO Vials Needed | ENJAYMO Volume | Maximum Infusion Rate |
|---|---|---|---|---|
|
||||
| Greater than or equal to 39 kg to less than 75 kg | 6,500 mg | 6 | 130 mL | 130 mL/hour * |
| 75 kg or greater | 7,500 mg | 7 | 150 mL | 150 mL/hour * |
Diluted preparation of ENJAYMO
Use aseptic technique to prepare ENJAYMO as follows:
- Remove ENJAYMO from the refrigerator. To minimize foaming, do not shake ENJAYMO.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
- ENJAYMO solution is a clear to slightly opalescent and colorless to slightly yellow solution. Do not administer if discolored or if foreign particulate matter is present.
- Withdraw the calculated volume of ENJAYMO from the appropriate number of vials based on the recommended dosage (see Table 1). Dilute the calculated volume with 0.9% Sodium Chloride Injection, USP to a total volume of 500 mL.
- Refer to Table 2 for infusion rate. Administer the infusion over 1 to 2 hours depending on the patient's body weight. Administer ENJAYMO infusion solution only through a 0.2 micron in-line filter with a polyethersulfone (PES) membrane.
- Prime the infusion tubing with the dosing solution immediately before infusion and flush immediately following completion of the infusion with a sufficient quantity (approximately 20 mL) of 0.9% Sodium Chloride Injection, USP.
- If the ENJAYMO infusion solution is not used immediately, store refrigerated at 36°F to 46°F (2°C to 8°C).
- Once removed from refrigeration, allow the ENJAYMO infusion solution to adjust to room temperature 59°F to 77°F (15°C to 25°C) and administer within 8 hours. Total time from the time of preparation, including refrigeration, adjustment to room temperature and the expected infusion time should not exceed 36 hours. In-line infusion warmers may be used; do not exceed a temperature of 104°F (40°C).
- No incompatibilities have been observed between ENJAYMO infusion solution and infusion bags made of Di-(2-ethylhexyl)phthalate (DEHP) plasticized polyvinyl chloride (PVC), Ethyl Vinyl Acetate (EVA) and polyolefin (PO); administration sets made of DEHP-plasticized PVC, DEHP-free polypropylene (PP) and polyethylene (PE); and vial adapters made of polycarbonate (PC) and acrylonitrile-butadiene-styrene (ABS).
| Body Weight Range | Dose | Number of ENJAYMO Vials Needed | ENJAYMO Volume | Volume of NaCl Diluent | Total Volume | Maximum Infusion Rate |
|---|---|---|---|---|---|---|
|
||||||
| 39 kg to less than 70 kg | 6,500 mg | 6 | 130 mL | 370 mL | 500 mL | 250 mL/hour |
| 70 kg to less than 75 kg | 6,500 mg | 6 | 130 mL | 370 mL | 500 mL | 500 mL/hour * |
| 75 kg or greater | 7,500 mg | 7 | 150 mL | 350 mL | 500 mL | 500 mL/hour * |
Slow or stop the infusion in case of infusion reaction during ENJAYMO administration. Monitor the patient for at least two hours following completion of the initial infusion for signs or symptoms of an infusion and/or hypersensitivity reaction. Monitor the patient for one hour following completion of subsequent infusions for signs or symptoms of an infusion reaction.
3. Dosage Forms and Strengths
Injection: 1,100 mg/22 mL (50 mg/mL) as a clear to slightly opalescent, colorless to slightly yellow solution in a single-dose vial.
4. Contraindications
ENJAYMO is contraindicated in patients with known hypersensitivity to sutimlimab-jome or any of the inactive ingredients [see Warnings and Precautions (5.2) and Adverse Reactions (6.1)] .
5. Warnings and Precautions
5.1 Serious Infections
ENJAYMO may increase susceptibility to serious infections, including infections caused by encapsulated bacteria such as Neisseria meningitidis (any serogroup), Streptococcus pneumoniae, and Haemophilus influenzae.
Serious infections (bacterial and viral) were reported in 15% (10/66) of patients receiving ENJAYMO from the two phase 3 studies. These infections included urinary tract infection with sepsis, respiratory tract infection, pneumonia, otomastoiditis, and skin infections One patient (1.5%) died due to klebsiella pneumonia.
Vaccinate patients for encapsulated bacteria according to the most current ACIP recommendations for patients with persistent complement deficiencies. Revaccinate patients in accordance with ACIP recommendations.
Immunize patients without a history of vaccination against encapsulated bacteria at least two weeks prior to receiving the first dose of ENJAYMO. If urgent ENJAYMO therapy is indicated in an unvaccinated patient, administer vaccine(s) as soon as possible.
Vaccination reduces, but does not eliminate, the risk of encapsulated bacterial infections.
If ENJAYMO treatment is administered to patients with active systemic infections, monitor closely for signs and symptoms of worsening infection. Some infections may become rapidly life-threatening or fatal if not recognized and treated promptly. Inform patients of these signs and symptoms and steps to be taken to seek immediate medical care. Consider interruption of ENJAYMO treatment in patients who are undergoing treatment for serious infection. ENJAYMO has not been studied in patients with chronic systemic infections such as hepatitis B, hepatitis C, or HIV. Consider patients' immune status when initiating treatment with ENJAYMO.
5.2 Infusion-Related Reactions
ENJAYMO is contraindicated in patients with known hypersensitivity to sutimlimab-jome or any of the inactive ingredients [see Contraindications (4)] . Administration of ENJAYMO may result in infusion-related reactions. In the two phase 3 studies, 19 of 66 (29%) patients treated with ENJAYMO experienced infusion-related reactions (e.g., shortness of breath, rapid heartbeat, nausea, flushing, headache, hypotension, chest discomfort, pruritus, rash, injection site reaction, and dizziness) were reported in patients from the two clinical studies. One patient permanently discontinued ENJAYMO due to an infusion-related reaction.
Monitor patients for infusion-related reactions and interrupt if a reaction occurs. Discontinue ENJAYMO infusion and institute appropriate supportive measures if signs of hypersensitivity reactions, such as cardiovascular instability or respiratory compromise, occur.
5.3 Risk of Autoimmune Disease
Based on its mechanism of action, ENJAYMO may potentially increase the risk for developing autoimmune diseases such as systemic lupus erythematosus (SLE). Development of systemic lupus erythematosus (SLE) has been associated with inherited classical complement deficiency. Patients with SLE or autoimmune disease with positive anti-nuclear antibody were excluded from clinical trials with ENJAYMO. In clinical trials, 3/66 (4.5%) patients developed a relapse or worsening of preexisting autoimmune disease. Monitor patients being treated with ENJAYMO for signs and symptoms and manage medically.
5.4 Recurrent Hemolysis After ENJAYMO Discontinuation
If treatment with ENJAYMO is interrupted, closely monitor patients for signs and symptoms of recurrent hemolysis, e.g., elevated levels of total bilirubin or lactate dehydrogenase (LDH) accompanied by a decrease in hemoglobin, or reappearance of symptoms such as fatigue, dyspnea, palpitations, or hemoglobinuria. Consider restarting ENJAYMO if signs and symptoms of hemolysis occur after discontinuation.
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions are discussed in greater detail in other sections of the labeling:
- Serious Infections [see Warnings and Precautions (5.1)]
- Infusion-Related Reactions [see Warnings and Precautions (5.2)]
- Risk of Autoimmune Disease [see Warnings and Precautions (5.3)]
- Recurrent Hemolysis After ENJAYMO Discontinuation [see Warnings and Precautions (5.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of ENJAYMO in patients with a confirmed diagnosis of CAD was evaluated in a placebo-controlled study (CADENZA) in Part A (n=42) followed by an open-label single-arm study in Part B (n=39) and an open-label single-arm study (CARDINAL) (n=24) [see Clinical Studies (14)] . The median duration of treatment exposure to ENJAYMO was 104 weeks (patients randomized to ENJAYMO in CADENZA Part A) and 93 weeks (patients randomized to placebo in CADENZA Part A) and 143 weeks for CARDINAL.
CADENZA (Part A)
Serious adverse reaction occurred in 2/22 (9%) patients who received ENJAYMO. Serious adverse reactions included Raynaud's phenomenon (n=1) and febrile infection (n=1).
Permanent discontinuation of ENJAYMO due to an adverse reaction occurred in 2/22 (9%) patients. Adverse reactions which resulted in permanent discontinuation of ENJAYMO included Raynaud's phenomenon (n=1), acrocyanosis (n=1), and infusion related reactions (n=1).
Dosage interruptions of ENJAYMO due to an adverse reaction occurred in 3/22 patients. Adverse reactions which required dosage interruption included nasopharyngitis (n=1) and infusion related reaction (n=1), including pruritis (n=1) and chest discomfort (n=1).
The most common adverse reactions (≥18%) reported in the CADENZA study were rhinitis, headache, hypertension, acrocyanosis, and Raynaud's phenomenon.
| Adverse Reactions | ENJAYMO
(N=22) | Placebo
(N=20) |
|---|---|---|
| Headache | 5 (23%) | 2 (10%) |
| Hypertension | 5 (23%) | 0 |
| Rhinitis | 4 (18%) | 0 |
| Acrocyanosis | 4 (18%) | 0 |
| Raynaud's phenomenon | 4 (18%) | 0 |
CARDINAL
Serious adverse reactions occurred in 10/24 (42%) patients who received ENJAYMO. The most common adverse reaction (>5%) was acrocyanosis (n=2). A fatal adverse reaction of pneumonia klebsiella occurred in one patient who received ENJAYMO.
Permanent discontinuation of ENJAYMO due to an adverse reaction occurred in 2/24 (8%) patients. Adverse reactions which resulted in permanent discontinuation of ENJAYMO included pneumonia klebsiella (n=1) and acrocyanosis (n=2).
Dosage interruptions of ENJAYMO due to an adverse reaction occurred in 7/24 patients. Adverse reactions which required dosage interruption included pneumonia, COVID-19 pneumonia, abdominal pain upper, urinary tract infection bacterial, urosepsis, acrocyanosis, viral infection, blood creatinine increased and infusion-related reaction.
The most common adverse reaction (≥25%) reported in the CARDINAL study were urinary tract infection, respiratory tract infection, bacterial infection, dizziness, fatigue, peripheral edema, arthralgia, cough, hypertension, and nausea.
| Adverse Reaction/Body System | n (%)
(N=24) |
|---|---|
| Please note: if a subject has multiple events in a grouped term the subject is only counted once. | |
| The following terms were combined for the analysis: | |
|
|
| INFECTIONS AND INFESTATIONS | |
| Urinary tract infection * | 9 (38%) |
| Respiratory tract infection † | 6 (25%) |
| Bacterial infection ‡ | 6 (25%) |
| Nasopharyngitis | 5 (21%) |
| Viral infection § | 5 (21%) |
| NERVOUS SYSTEM DISORDERS | |
| Dizziness ¶ | 7 (29%) |
| Headache | 5 (21%) |
| GENERAL DISORDERS | |
| Fatigue # | 8 (33%) |
| Peripheral edema Þ | 6 (25%) |
| Pyrexia | 5 (21%) |
| MUSCULOSKELETAL AND CONNECTIVE TISSUE DISORDERS | |
| Arthralgia | 6 (25%) |
| VASCULAR DISORDERS | |
| Hypertension ß | 6 (25%) |
| Acrocyanosis | 5 (21%) |
| GASTROINTESTINAL DISORDERS | |
| Nausea | 6 (25%) |
| Abdominal pain à | 5 (21%) |
| RESPIRATORY, THORACIC, AND MEDIASTINAL DISORDERS | |
| Cough è | 6 (25%) |
| INJURY, POISONING AND PROCEDURAL COMPLICATIONS | |
| Infusion-related reaction ð | 4 (17%) |
8. Use In Specific Populations
8.5 Geriatric Use
Of the 66 patients with CAD in clinical studies of ENJAYMO, 65% were 65 years of age and over, including 27% who were 75 years of age and over. No overall differences in safety or effectiveness were observed between these patients and younger patients, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
11. Enjaymo Description
Sutimlimab-jome, a classical complement inhibitor, is a humanized monoclonal antibody expressed by recombinant in Chinese hamster ovary (CHO) cells and produced in vitro using standard mammalian cell culture methods. Sutimlimab-jome is composed of two heterodimers. Each heterodimer is composed of a heavy and a light polypeptide chain. Each heavy chain (H-chain) is composed of 445 amino acids and each light chain (L-chain) contains 216 amino acids. Sutimlimab-jome has a molecular weight of approximately 147 kDa.
ENJAYMO (sutimlimab-jome) injection is a sterile, clear to slightly opalescent, colorless to slightly yellow, preservative-free solution for intravenous use. Each single-dose vial contains 1,100 mg sutimlimab-jome at a concentration of 50 mg/mL with a pH of 6.1. Each mL contains 50 mg of sutimlimab-jome and also contains polysorbate 80 (0.2 mg), sodium chloride (8.18 mg), sodium phosphate dibasic heptahydrate (0.48 mg), sodium phosphate monobasic monohydrate (1.13 mg), and Water for Injection, USP.
12. Enjaymo - Clinical Pharmacology
12.1 Mechanism of Action
Sutimlimab-jome is an immunoglobulin G (IgG), subclass 4 (IgG4) monoclonal antibody (mAb) that inhibits the classical complement pathway (CP) and specifically binds to complement protein component 1, s subcomponent (C1s), a serine protease which cleaves C4. Sutimlimab-jome does not inhibit the lectin and alternative pathways. Inhibition of the classical complement pathway at the level of C1s prevents deposition of complement opsonins on the surface of RBCs, resulting in inhibition of hemolysis in patients with CAD.
12.2 Pharmacodynamics
Greater than 90% inhibition of CP was observed following a single sutimlimab-jome infusion and sustained in patients with CAD when sutimlimab-jome concentrations were greater than or equal to 100 mcg/mL. C4 levels returned to normal levels (0.2 g/L) in patients with CAD within one week following the first dose of sutimlimab-jome. Complete CP inhibition following initiation of sutimlimab-jome treatment led to inhibition of hemolysis as evidenced by normalization of bilirubin, decrease in LDH, increase in haptoglobin, and decrease in reticulocytes.
After the first treatment with sutimlimab-jome, near normalization of bilirubin associated with a greater than 1 g/dL increase in hemoglobin was observed, demonstrating the effect of CP inhibition. The extent and duration of the pharmacodynamic response in patients with CAD were exposure dependent for sutimlimab-jome.
12.3 Pharmacokinetics
Following administration of the approved weight-based recommended dosages, the exposure of sutimlimab-jome increases proportionally over a dosage range of 60 mg/kg to 100 mg/kg by intravenous infusion (0.3 to 1.5 times the maximum approved recommended dosage based on 75 kg body weight). Steady state was achieved by Week 7 after starting sutimlimab-jome treatment, with an accumulation ratio of less than 2.
12.6 Immunogenicity
The observed incidence of anti-drug antibodies is highly dependent on the sensitivity and specificity of the assay. Differences in assay methods preclude meaningful comparisons of the incidence of anti-drug antibodies in the studies described below with the incidence of anti-drug antibodies in other studies, including those of sutimlimab-jome or of other sutimlimab products.
During the treatment period in CARDINAL and CADENZA, 8/66 (12%) ENJAYMO-treated patients developed anti-sutimlimab-jome antibodies (duration of exposure up to 177 weeks). There was no identified clinically significant effect of anti-drug antibodies on pharmacokinetics, pharmacodynamics, safety, or effectiveness of ENJAYMO over the treatment duration [see Clinical Studies (14)] .
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity and mutagenicity studies have not been conducted with sutimlimab-jome.
Effects of sutimlimab-jome on male and female fertility have not been studied in animals. In repeat-dose studies in cynomolgus monkeys with sutimlimab-jome administered once-weekly at exposures 3 to 4 times the human exposures at the maximum recommended human doses of sutimlimab-jome, no effects on male or female reproductive tissues were observed.
14. Clinical Studies
14.1 CADENZA
The efficacy of ENJAYMO was assessed in a placebo-controlled 6-month trial in 42 patients (CADENZA, NCT 03275454). Following the completion of the 6-month treatment period (Part A) in which 22 patients received ENJAYMO and 20 patients received placebo, 39 patients (19 patients on ENJAYMO and 20 patients on placebo) continued to receive ENJAYMO in a long-term safety and durability of response extension phase (Part B) for an additional 12 months following last patient out from Part A. The trial included a 9 week safety follow-up after the last dose of ENJAYMO. Patients with a confirmed diagnosis of CAD based on chronic hemolysis, polyspecific direct antiglobulin test (DAT), monospecific DAT specific for C3d, cold agglutinin titer ≥64 at 4°C, an IgG DAT ≤1+ and no history of transfusion within 6 months, or more than one blood transfusion in the 12 months prior to enrollment in the trial were administered 6.5 g or 7.5 g ENJAYMO (based on body weight) intravenously over approximately 60 minutes on Day 0, Day 7, and every 14 days thereafter; or placebo. Patients with cold agglutinin disease secondary to infection, rheumatologic disease, systemic lupus erythematosus, or overt hematologic malignancy were excluded, whereas patients with a history of or concomitant low-grade lymphoproliferative disease were not excluded.
Major baseline characteristics of the study population are summarized in Table 5.
| Parameter | Statistic | CADENZA | |
|---|---|---|---|
| Placebo | ENJAYMO | ||
| N=20 | N=22 | ||
|
|||
| Age | Mean | 68.2 | 65.3 |
| Min, Max | 51, 83 | 46, 88 | |
| Sex | |||
| Male | n (%) | 4 (20.0) | 5 (22.7) |
| Female | 16 (80.0) | 17 (77.3) | |
| Body weight | Mean, Kg | 64.9 | 66.8 |
| Min, Max | 48, 95 | 39, 100 | |
| Hemoglobin | Mean, g/dL | 9.33 | 9.15 |
| Bilirubin (total) * | µmol/L | 35.77 | 41.17 |
| (1.75 × ULN) | (2 × ULN) | ||
| LDH | U/L | 380.8 | 421.5 |
| History of transfusion | Mean number of transfusions (range) | ||
| Within last 6 months | 0 | 0 | |
| Within last 12 months | 0 | 0.14 (0, 1) | |
| FACIT †-Fatigue scale | Mean | 32.99 | 31.67 |
Efficacy was based on the proportion of patients who met the following criteria: an increase from baseline in Hgb level ≥1.5 g/dL at the treatment assessment time point (mean value from Weeks 23, 25, and 26), no blood transfusion from Week 5 through Week 26, and no treatment for CAD beyond what was permitted per protocol from Week 5 through Week 26. Efficacy was further assessed based on the effect of ENJAYMO on Hgb, laboratory measures of hemolysis including mean change from baseline in total bilirubin and LDH. Supportive efficacy data collected included transfusion usage after five weeks of treatment. In addition, mean change from baseline in symptoms and impacts of fatigue were assessed using a patient-reported outcome instrument, the FACIT-Fatigue (score range from 0 to 52 with higher scores indicating less fatigue).
The data from this study demonstrated a statistically significant treatment effect of ENJAYMO over placebo in terms of the rate of patients who met the efficacy criteria (responder) as well as improving symptoms and impacts of fatigue (FACIT-Fatigue). The responder rate difference between ENJAYMO and placebo was 58.78% (95% CI: 34.6% to 82.96%) with a p-value of 0.0004. At the treatment assessment timepoint (TAT), 16 of 22 patients on ENJAYMO (72.7%; 95% CI: 49.8% to 89.3%) and 3 of 20 patients on placebo (15.0%; 95% CI: 3.2% to 37.9%) met primary criteria. Efficacy of ENJAYMO in the inhibition of hemolysis in patients with CAD was demonstrated across multiple end points as described in the table below (see Table 6).
| Parameter | Statistic | Placebo
N=20 | ENJAYMO
N=22 | Treatment Effect |
|---|---|---|---|---|
|
||||
| Responder* | n (%) | 3 (15) | 16 (72.7) | 58.78 (34.6, 82.96) † |
| p-value: | <0.001 | |||
| Hemoglobin | Mean change from baseline (LS ‡ Mean), g/dL | 0.09 | 2.66 | 2.56 |
| 95% CI of LS Mean | (1.75, 3.38) | |||
| p-value: | <0.001 | |||
| Patients with mean change from baseline of:
greater than or equal to 1.5 g/dL | n (%) | 3 (15) | 16 (72.7) | NC |
| Patients not receiving blood transfusion from Week 5 through Week 26 (transfusion avoidance) | n (%) | 16 (80) | 18 (81.8) | NC |
| Patients not receiving protocol-prohibited CAD medications from Week 5 through Week 26 § | n (%) | 20 (100) | 19 (86.4) | NC |
| FACIT ‡-Fatigue | Mean change from baseline (LS ‡ Mean) | 1.91 | 10.83 | 8.93 |
| 95% CI of LS Mean | (4, 13.85) | |||
| p-value: | <0.001 | |||
During Part A, an increase in mean hemoglobin level of 2.02 g/dL was observed in patients on ENJAYMO at Week 3; in the placebo group the mean hemoglobin level decreased by 0.31g/dL. At treatment assessment timepoint, a mean decrease in bilirubin of 1.29 mg/dL compared to baseline was reported in patients on ENJAYMO (n=17) versus 0.11 mg/dL on placebo (n=18). In the ENJAYMO group, bilirubin levels normalized in 88.2% (n=15) of patients compared to 22.2% (n=4) of patients in the placebo arm. At treatment assessment timepoint, a mean decrease in LDH of 150.83 U/L compared to baseline was reported in patients on ENJAYMO (n=19) versus an increase of 7.6 U/L on placebo (n=20). In the ENJAYMO group, LDH levels were < 1.5 × ULN in 94.7% (n=18) of patients compared to 70% (n=14) in the placebo arm.
In Part B, mean hemoglobin levels were maintained at >10.5 g/dL. Sustained normalization of mean bilirubin levels was also observed indicating a sustained decrease in hemolysis. Mean hemoglobin level of 11.58 g/dL (range: 6.90–15.30) and 1.01 mg/dL (range: 0.29–5.54) for bilirubin was observed at the last on-treatment visit.
After the last dose of ENJAYMO in the study, signs and symptoms of recurrent hemolysis were observed, nine weeks after the last dose in Part B; mean hemoglobin decreased by 2.41 g/dL (SE: 0.373) and mean bilirubin increased by 1.27 mg/dL (SE: 0.182) from the last available values during treatment.
14.2 CARDINAL
The efficacy of ENJAYMO was assessed in an open-label, single-arm, 6-month trial in 24 patients (CARDINAL, NCT03347396). Following the completion of the 6-month treatment period (Part A), patients continued to receive ENJAYMO in a long-term safety and durability of response extension phase (Part B) for an additional 24 months following last patient out from Part A. The trial included a 9 week safety follow-up after the last dose of ENJAYMO.
Patients with a confirmed diagnosis of CAD based on chronic hemolysis, polyspecific direct antiglobulin test (DAT), monospecific DAT specific for C3d, cold agglutinin titer ≥64 at 4°C, and IgG DAT ≤1+ and a recent blood transfusion in the 6 months prior to enrollment were administered 6.5 g or 7.5 g ENJAYMO (based on body weight) intravenously over approximately 60 minutes on Day 0, Day 7, and every 14 days thereafter. Patients with cold agglutinin syndrome secondary to infection, rheumatologic disease, systemic lupus erythematosus, or overt hematologic malignancy were excluded, whereas patients with a history of or concomitant low-grade lymphoproliferative disease were not excluded. Major baseline characteristics of the trial population are summarized in Table 7.
| Parameter | Statistic | ENJAYMO
N=24 |
|---|---|---|
|
||
| Age | Mean (SD)
Range | 71.3 (8.2)
55 to 85 years |
| Sex | ||
| Female | n (%) | 15 (63) |
| Male | 9 (38) | |
| Body weight | Mean (SD)
Range | 67.8 (15.8)
40 to 112 kg |
| Hemoglobin | Mean (SD), g/dL | 8.6 (1.16) |
| Bilirubin (total) * | Mean (SD), mg/dL | 3.1 (1.41)
(2.6 × ULN †) |
| LDH † | Mean (SD), U/L | 438 (484.60) |
| Blood transfusion | Median number of transfusions (range) | |
| Within last 6 months | 2.0 (1, 19) | |
| Within last 12 months | 2.0 (1, 23) | |
Efficacy was based on the proportion of patients who met the following criteria: an increase from baseline in Hgb level ≥2 g/dL or a Hgb level ≥12 g/dL at the treatment assessment time point (mean value from Weeks 23, 25, and 26), no blood transfusion from Week 5 through Week 26, and no treatment for CAD beyond what was permitted per protocol from Week 5 through Week 26.
Efficacy of ENJAYMO in patients with CAD is described in Table 8.
| Parameter | Statistic | ENJAYMO
N=24 |
|---|---|---|
|
||
| Responder * | n (%) | 13 (54) |
| Hemoglobin level ≥12 g/dL or
Increase in Hemoglobin level of ≥2 g/dL | n (%) | 15 (63) |
| Hemoglobin level ≥12 g/dL | n (%) | 9 (38) |
| Increase in Hemoglobin level of ≥2 g/dL | n (%) | 15 (63) |
| Patients not receiving RBC transfusion from Week 5 through Week 26 (transfusion avoidance) | n (%) | 17 (71) |
| Patients not receiving protocol-prohibited CAD medications † from Week 5 through Week 26 | n (%) | 22 (92) |
In Part A, among 14 patients with baseline and follow-up bilirubin values, the mean was 3.23 mg/dL (2.7-fold ULN) at baseline and 0.91 mg/dL (0.8-fold ULN) at the treatment assessment time point. The least-squares (LS) mean change was reduction of -2.23 mg/dL (95% CI: -2.49 to -1.98). Among 17 patients with baseline and follow-up LDH values, the mean LDH was 424 U/L (1.7-fold ULN) at baseline and 301 U/L (1.2-fold ULN) at the follow-up time point. The least squared mean change in LDH at the treatment assessment time point was reduction of -126 (95% CI: -218 to -35).
In CARDINAL, an increase in mean hemoglobin level of 2.29 g/dL (SE: 0.308) was observed at Week 3 and 3.18 g/dL (SE: 0.476) at treatment assessment time point. The observed model mean change in hemoglobin level from baseline at treatment assessment time point was an improvement of 2.60 g/dL (95% CI: 0.74, 4.46).
In Part B, mean hemoglobin levels were maintained at >10 g/dL. Sustained normalization of mean bilirubin levels was also observed indicating a sustained decrease in hemolysis. Mean hemoglobin level of 12.23 g/dL (range: 9.20–14.40) and 0.96 mg/dL (range: 0.4–1.7) for bilirubin was observed at the last on-treatment visit.
After the last dose of ENJAYMO in the study, signs and symptoms of recurrent hemolysis were observed, nine weeks after the last dose in Part B; mean hemoglobin decreased by 2.28 g/dL (SE: 0.402) and mean bilirubin increased by 1.42 mg/dL (SE: 0.192) from the last available values during treatment.
| ENJAYMO
sutimlimab-jome injection, solution, concentrate |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Bioverativ Therapeutics Inc. (080521844) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Biogen MA Inc. | 841087823 | analysis(80203-347) , api manufacture(80203-347) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Vetter Pharma Fertigung GmbH & Co. KG (Ravensburg Mooswiesen) | 312670654 | analysis(80203-347) , manufacture(80203-347) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| KBI Biopharma, Inc. | 034248380 | analysis(80203-347) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Genzyme Corporation | 050424395 | pack(80203-347) , label(80203-347) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Eurofins Biopharma Product Testing Munich GmbH | 313046917 | analysis(80203-347) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Sanofi-Aventis Deutschland GmbH | 313218430 | pack(80203-347) , label(80203-347) | |