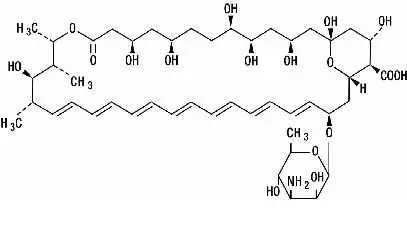
Drug Detail:Fungizone (Amphotericin b [ am-foe-ter-i-sin ])
Drug Class: Polyenes
Fungizone - Clinical Pharmacology
Related/similar drugs
fluconazole, nystatin, clotrimazole, ketoconazole, Diflucan, itraconazole, miconazoleIndications and Usage for Fungizone
FUNGIZONE Intravenous (Amphotericin B for Injection, USP) should be administered primarily to patients with progressive, potentially life-threatening fungal infections. This potent drug should not be used to treat noninvasive fungal infections, such as oral thrush, vaginal candidiasis, and esophageal candidiasis in patients with normal neutrophil counts.
FUNGIZONE Intravenous is specifically intended to treat potentially life-threatening fungal infections: aspergillosis, cryptococcosis (torulosis), North American blastomycosis, systemic candidiasis, coccidioido-mycosis, histoplasmosis, zygomycosis including mucormycosis due to susceptible species of the genera Absidia, Mucor, and Rhizopus, and infections due to related susceptible species of Conidiobolus and Basidiobolus, and sporotrichosis.
Amphotericin B may be useful in the treatment of American mucocutaneous leishmaniasis, but it is not the drug of choice as primary therapy.
Warnings
Amphotericin B is frequently the only effective treatment available for potentially life-threatening fungal disease. In each case, its possible life-saving benefit must be balanced against its untoward and dangerous side effects.
EXERCISE CAUTION to prevent inadvertent FUNGIZONE Intravenous overdose, which can result in potentially fatal cardiac or cardiorespiratory arrest. Verify the product name and dosage pre-administration, especially if dose prescribed exceeds 1.5 mg/kg (see OVERDOSAGE and DOSAGE AND ADMINISTRATION).
Precautions
General
Amphotericin B should be administered intravenously under close clinical observation by medically trained personnel. It should be reserved for treatment of patients with progressive, potentially life-threatening fungal infections due to susceptible organisms (see INDICATIONS AND USAGE).
Acute reactions including fever, shaking chills, hypotension, anorexia, nausea, vomiting, headache, and tachypnea are common 1 to 3 hours after starting an intravenous infusion. These reactions are usually more severe with the first few doses of amphotericin B and usually diminish with subsequent doses.
Rapid intravenous infusion has been associated with hypotension, hypokalemia, arrhythmias, and shock and should, therefore, be avoided (see DOSAGE AND ADMINISTRATION).
Amphotericin B should be used with care in patients with reduced renal function; frequent monitoring of renal function is recommended (see PRECAUTIONS: Laboratory Tests and ADVERSE REACTIONS). In some patients hydration and sodium repletion prior to amphotericin B administration may reduce the risk of developing nephrotoxicity. Supplemental alkali medication may decrease renal tubular acidosis complications.
Since acute pulmonary reactions have been reported in patients given amphotericin B during or shortly after leukocyte transfusions, it is advisable to temporarily separate these infusions as far as possible and to monitor pulmonary function (see PRECAUTIONS: Drug Interactions).
Leukoencephalopathy has been reported following use of amphotericin B. Literature reports have suggested that total body irradiation may be a predisposition.
Whenever medication is interrupted for a period longer than 7 days, therapy should be resumed by starting with the lowest dosage level, e.g., 0.25 mg/kg of body weight, and increased gradually as outlined under DOSAGE AND ADMINISTRATION.
Laboratory Tests
Renal function should be monitored frequently during amphotericin B therapy (see ADVERSE REACTIONS). It is also advisable to monitor on a regular basis liver function, serum electrolytes (particularly magnesium and potassium), blood counts, and hemoglobin concentrations. Laboratory test results should be used as a guide to subsequent dosage adjustments.
Drug Interactions
When administered concurrently, the following drugs may interact with amphotericin B:
Antineoplastic agents: may enhance the potential for renal toxicity, bronchospasm and hypotension. Antineoplastic agents (e.g., nitrogen mustard, etc.) should be given concomitantly only with great caution.
Corticosteroids and Corticotropin (ACTH): may potentiate amphotericin B-induced hypokalemia which may predispose the patient to cardiac dysfunction. Avoid concomitant use unless necessary to control side effects of amphotericin B. If used concomitantly, closely monitor serum electrolytes and cardiac function (see ADVERSE REACTIONS).
Digitalis glycosides: amphotericin B-induced hypokalemia may potentiate digitalis toxicity. Serum potassium levels and cardiac function should be closely monitored and any deficit promptly corrected.
Flucytosine: while a synergistic relationship with amphotericin B has been reported, concomitant use may increase the toxicity of flucytosine by possibly increasing its cellular uptake and/or impairing its renal excretion.
Imidazoles (e.g., ketoconazole, miconazole, clotrimazole, fluconazole, etc.): in vitro and animal studies with the combination of amphotericin B and imidazoles suggest that imidazoles may induce fungal resistance to amphotericin B. Combination therapy should be administered with caution, especially in immunocompromised patients.
Other nephrotoxic medications: agents such as aminoglycosides, cyclosporine, and pentamidine may enhance the potential for drug-induced renal toxicity, and should be used concomitantly only with great caution. Intensive monitoring of renal function is recommended in patients requiring any combination of nephrotoxic medications (see PRECAUTIONS: Laboratory Tests).
Skeletal muscle relaxants: amphotericin B-induced hypokalemia may enhance the curariform effect of skeletal muscle relaxants (e.g., tubocurarine). Serum potassium levels should be monitored and deficiencies corrected.
Leukocyte transfusions: acute pulmonary toxicity has been reported in patients receiving intravenous amphotericin B and leukocyte transfusions (see PRECAUTIONS: General).
Adverse Reactions/Side Effects
Although some patients may tolerate full intravenous doses of amphotericin B without difficulty, most will exhibit some intolerance, often at less than the full therapeutic dose.
Tolerance may be improved by treatment with aspirin, antipyretics (e.g., acetaminophen), antihistamines, or antiemetics. Meperidine (25 to 50 mg IV) has been shown in some patients to decrease the duration of shaking chills and fever that may accompany the infusion of amphotericin B.
Administration of amphotericin B on alternate days may decrease anorexia and phlebitis.
Intravenous administration of small doses of adrenal corticosteroids just prior to or during the amphotericin B infusion may help decrease febrile reactions. Dosage and duration of such corticosteroid therapy should be kept to a minimum (see PRECAUTIONS: Drug Interactions).
Addition of heparin (1000 units per infusion), and the use of pediatric scalp-vein needle may lessen the incidence of thrombophlebitis. Extravasation may cause chemical irritation.
The adverse reactions most commonly observed are:
General (body as a whole): fever (sometimes accompanied by shaking chills usually occurring within 15 to 20 minutes after initiation of treatment); malaise; weight loss.
Cardiopulmonary: hypotension; tachypnea.
Gastrointestinal: anorexia; nausea; vomiting; diarrhea; dyspepsia; cramping epigastric pain.
Hematologic: normochromic, normocytic anemia.
Local: pain at the injection site with or without phlebitis or thrombophlebitis.
Musculoskeletal: generalized pain, including muscle and joint pains.
Neurologic: headache.
Renal: decreased renal function and renal function abnormalities including: azotemia, hypokalemia, hyposthenuria, renal tubular acidosis; and nephrocalcinosis. These usually improve with interruption of therapy. However, some permanent impairment often occurs, especially in those patients receiving large amounts (over 5 g) of amphotericin B or receiving other nephrotoxic agents. In some patients hydration and sodium repletion prior to amphotericin B administration may reduce the risk of developing nephrotoxicity. Supplemental alkali medication may decrease renal tubular acidosis.
The following adverse reactions have also been reported:
General (body as a whole): flushing.
Allergic: anaphylactoid and other allergic reactions; bronchospasm; wheezing.
Cardiopulmonary: cardiac arrest; shock; cardiac failure; pulmonary edema; hypersensitivity pneumonitis; arrhythmias, including ventricular fibrillation; dyspnea; hypertension.
Dermatologic: rash, in particular maculopapular; pruritus. Skin exfoliation, toxic epidermal necrolysis, and Stevens-Johnson syndrome have been reported during post-marketing surveillance.
Gastrointestinal: acute liver failure; hepatitis; jaundice; hemorrhagic gastroenteritis; melena.
Hematologic: agranulocytosis; coagulation defects; thrombocytopenia; leukopenia; eosinophilia; leukocytosis.
Neurologic: convulsions; hearing loss; tinnitus; transient vertigo; visual impairment; diplopia; peripheral neuropathy; encephalopathy (see PRECAUTIONS); other neurologic symptoms.
Renal: acute renal failure; anuria; oliguria. Nephrogenic diabetes insipidus has been reported during post-marketing surveillance.
Overdosage
Amphotericin B overdoses can result in potentially fatal cardiac or cardiorespiratory arrest (see WARNINGS and DOSAGE AND ADMINISTRATION). If an overdose is suspected, discontinue therapy and monitor the patient’s clinical status (e.g., cardiorespiratory, renal, and liver function, hematologic status, serum electrolytes) and administer supportive therapy, as required. Amphotericin B is not hemodialyzable.
Prior to reinstituting therapy, the patient’s condition should be stabilized (including correction of electrolyte deficiencies, etc.).
Fungizone Dosage and Administration
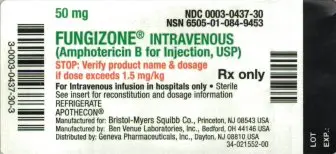
**VERIFY PRODUCT NAME AND DOSAGE.**
CAUTION: Under no circumstances should a total daily dose of 1.5 mg/kg be exceeded. Amphotericin B overdoses can result in potentially fatal cardiac or cardiorespiratory arrest (see WARNINGS and OVERDOSAGE).
FUNGIZONE Intravenous (Amphotericin B for Injection) should be administered by slow intravenous infusion. Intravenous infusion should be given over a period of approximately 2 to 6 hours (depending on the dose) observing the usual precautions for intravenous therapy (see PRECAUTIONS: General). The recommended concentration for intravenous infusion is 0.1 mg/mL (1 mg/10 mL).
Since patient tolerance varies greatly, the dosage of amphotericin B must be individualized and adjusted according to the patient’s clinical status (e.g., site and severity of infection, etiologic agent, cardio-renal function, etc.).
A single intravenous test dose (1 mg in 20 mL of 5% dextrose solution) administered over 20 to 30 minutes may be preferred. The patient’s temperature, pulse, respiration, and blood pressure should be recorded every 30 minutes for 2 to 4 hours.
In patients with good cardio-renal function and a well tolerated test dose, therapy is usually initiated with a daily dose of 0.25 mg/kg of body weight. However, in those patients having severe and rapidly progressive fungal infection, therapy may be initiated with a daily dose of 0.3 mg/kg of body weight. In patients with impaired cardio-renal function or a severe reaction to the test dose, therapy should be initiated with smaller daily doses (i.e., 5 to 10 mg).
Depending on the patient’s cardio-renal status (see PRECAUTIONS: Laboratory Tests), doses may gradually be increased by 5 to 10 mg per day to final daily dosage of 0.5 to 0.7 mg/kg.
There are insufficient data presently available to define total dosage requirements and duration of treatment necessary for eradication of specific mycoses. The optimal dose is unknown. Total daily dosage may range up to 1.0 mg/kg per day or up to 1.5 mg/kg when given on alternate days.
Sporotrichosis: Therapy with intravenous amphotericin B for sporotrichosis has ranged up to 9 months with a total dose up to 2.5 g.
Aspergillosis: Aspergillosis has been treated with amphotericin B intravenously for a period up to 11 months with a total dose up to 3.6 g.
Rhinocerebral phycomycosis: This fulminating disease generally occurs in association with diabetic ketoacidosis. It is, therefore, imperative that diabetic control be restored in order for treatment with FUNGIZONE Intravenous to be successful. In contradistinction, pulmonary phycomycosis, which is more common in association with hematologic malignancies, is often an incidental finding at autopsy. A cumulative dose of at least 3 g of amphotericin B is recommended to treat rhinocerebral phycomycosis. Although a total dose of 3 to 4 g will infrequently cause lasting renal impairment, this would seem a reasonable minimum where there is clinical evidence of invasion of deep tissue. Since rhinocerebral phycomycosis usually follows a rapidly fatal course, the therapeutic approach must necessarily be more aggressive than that used in more indolent mycoses.
-----------------------------------------
REPRESENTATIVE PACKAGING
See How Supplied section for a complete list of available packages of FUNGIZONE.
50 mg
NDC 0003-0437-30
NSN 6505-01-084-9453
FUNGIZONE® INTRAVENOUS
(Amphotericin B for Injection, USP)
STOP: Verify product name & dosage if dose exceeds 1.5 mg/kg
Rx only
For Intravenous infusion in hospitals only
Sterile
See insert for reconstitution and dosage information
REFRIGERATE
APOTHECON®
Manufactured for: Bristol-Myers Squibb Co., Princeton, NJ 08543 USA
Manufactured by: Ben Venue Laboratories, Inc., Bedford, OH 44146 USA
Distributed by: Geneva Pharmaceuticals, Inc., Dayton, NJ 08810 USA
34-021552-00
| FUNGIZONE
amphotericin b injection, powder, lyophilized, for solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - E.R. Squibb & Sons, L.L.C. (011550092) |