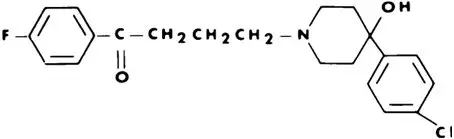
Drug Detail:Haldol (Haloperidol (oral) [ hal-oh-per-i-dol ])
Drug Class: Miscellaneous antipsychotic agents
Indications and Usage for Haldol
HALDOL (haloperidol) is indicated for the treatment of patients with schizophrenia.
Contraindications
HALDOL (haloperidol) is contraindicated in patients with:
- Severe toxic central nervous system depression or comatose states from any cause.
- Hypersensitivity to this drug – hypersensitivity reactions have included anaphylactic reaction and angioedema (see WARNINGS, Hypersensitivity Reactions and ADVERSE REACTIONS).
- Parkinson's disease (see WARNINGS, Neurological Adverse Reactions in Patients with Parkinson's Disease or Dementia with Lewy Bodies).
- Dementia with Lewy bodies (see WARNINGS, Neurological Adverse Reactions in Patients with Parkinson's Disease or Dementia with Lewy Bodies).
Warnings
Cardiovascular Effects
Cases of sudden death, QTc interval-prolongation, and Torsades de Pointes have been reported in patients receiving HALDOL (see ADVERSE REACTIONS). Higher than recommended doses of any formulation and intravenous administration of HALDOL appear to be associated with a higher risk of QTc interval-prolongation and Torsades de Pointes. Also, a QTc-interval that exceeds 500 msec is associated with an increased risk of Torsades de Pointes. Although cases have been reported even in the absence of predisposing factors, particular caution is advised in treating patients with other QTc-prolonging conditions (including electrolyte imbalance [particularly hypokalemia and hypomagnesemia], drugs known to prolong QTc, underlying cardiac abnormalities, hypothyroidism, and familial long QT-syndrome). HALDOL INJECTION IS NOT APPROVED FOR INTRAVENOUS ADMINISTRATION. If HALDOL is administered intravenously, the ECG should be monitored for QTc-prolongation and arrhythmias.
Tachycardia and hypotension (including orthostatic hypotension) have also been reported in occasional patients (see ADVERSE REACTIONS).
Tardive Dyskinesia
A syndrome consisting of potentially irreversible, involuntary, dyskinetic movements may develop in patients treated with antipsychotic drugs (see ADVERSE REACTIONS). Although the prevalence of the syndrome appears to be highest among the elderly, especially elderly women, it is impossible to rely upon prevalence estimates to predict, at the inception of antipsychotic treatment, which patients are likely to develop the syndrome. Whether antipsychotic drug products differ in their potential to cause tardive dyskinesia is unknown.
Both the risk of developing tardive dyskinesia and the likelihood that it will become irreversible are believed to increase as the duration of treatment and the total cumulative dose of antipsychotic drugs administered to the patient increase. However, the syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses.
Ttardive dyskinesia may remit, partially or completely, if antipsychotic treatment is discontinued. Antipsychotic treatment, itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome and thereby may possibly mask the underlying process. The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.
Given these considerations, antipsychotic drugs should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that, 1) is known to respond to antipsychotic drugs, and, 2) for whom alternative, equally effective, but potentially less harmful treatments are not available or appropriate. In patients who do require chronic treatment, the smallest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. The need for continued treatment should be reassessed periodically.
If signs and symptoms of tardive dyskinesia appear in a patient on antipsychotics, drug discontinuation should be considered. However, some patients may require treatment despite the presence of the syndrome.
Neurological Adverse Reactions in Patients with Parkinson's Disease or Dementia with Lewy Bodies
Patients with Parkinson's Disease or Dementia with Lewy Bodies are reported to have an increased sensitivity to antipsychotic medication. Manifestations of this increased sensitivity with haloperidol treatment include severe extrapyramidal symptoms, confusion, sedation, and falls. In addition, haloperidol may impair the antiparkinson effects of levodopa and other dopamine agonists. HALDOL is contraindicated in patients with Parkinson's Disease or Dementia with Lewy Bodies (see CONTRAINDICATIONS).
Hypersensitivity Reactions
There have been postmarketing reports of hypersensitivity reactions with haloperidol. These include anaphylactic reaction, angioedema, dermatitis exfoliative, hypersensitivity vasculitis, rash, urticaria, face edema, laryngeal edema, bronchospasm, and laryngospasm (see ADVERSE REACTIONS). HALDOL is contraindicated in patients with hypersensitivity to this drug (see CONTRAINDICATIONS).
Usage in Pregnancy
Rats or rabbits administered oral haloperidol doses of 0.5 to 7.5 mg/kg, which are approximately 0.2 to 7 times the maximum recommended human dose (MRHD) of 20 mg/day based on mg/m2 body surface area, showed an increase in incidence of resorption, reduced fertility, delayed delivery and pup mortality. No fetal abnormalities were observed at these doses in rats or rabbits. Cleft palate has been observed in mice administered oral haloperidol at a dose of 0.5 mg/kg, which is approximately 0.1 times the MRHD based on mg/m2 body surface area.
There are no well controlled studies with HALDOL (haloperidol) in pregnant women. There are reports, however, of cases of limb malformations observed following maternal use of HALDOL along with other drugs which have suspected teratogenic potential during the first trimester of pregnancy. Causal relationships were not established in these cases. Since such experience does not exclude the possibility of fetal damage due to HALDOL, this drug should be used during pregnancy or in women likely to become pregnant only if the benefit clearly justifies a potential risk to the fetus. Infants should not be nursed during drug treatment.
Precautions
Drug Interactions
Drug-drug interactions can be pharmacodynamic (combined pharmacologic effects) or pharmacokinetic (alteration of plasma levels). The risks of using haloperidol in combination with other drugs have been evaluated as described below.
Pharmacokinetic Interactions
Adverse Reactions/Side Effects
The following adverse reactions are discussed in more detail in other sections of the labeling:
- WARNINGS, Increased mortality in Elderly Patients with Dementia-Related Psychosis
- WARNINGS, Cardiovascular Effects
- WARNINGS, Tardive Dyskinesia
- WARNINGS, Neuroleptic Malignant Syndrome
- WARNINGS, Hypersensitivity Reactions
- WARNINGS, Falls
- WARNINGS, Usage in Pregnancy
- WARNINGS, Combined Use of HALDOL and Lithium
- WARNINGS, General
- PRECAUTIONS, Leukopenia, Neutropenia, and Agranulocytosis
- PRECAUTIONS, Withdrawal Emergent Dyskinesia
- PRECAUTIONS, Other
Haldol Dosage and Administration
There is considerable variation from patient to patient in the amount of medication required for treatment. As with all drugs used to treat schizophrenia, dosage should be individualized according to the needs and response of each patient. Dosage adjustments, either upward or downward, should be carried out as rapidly as practicable to achieve optimum therapeutic control.
To determine the initial dosage, consideration should be given to the patient's age, severity of illness, previous response to other antipsychotic drugs, and any concomitant medication or disease state. Debilitated or geriatric patients, as well as those with a history of adverse reactions to antipsychotic drugs, may require less HALDOL (haloperidol). The optimal response in such patients is usually obtained with more gradual dosage adjustments and at lower dosage levels.
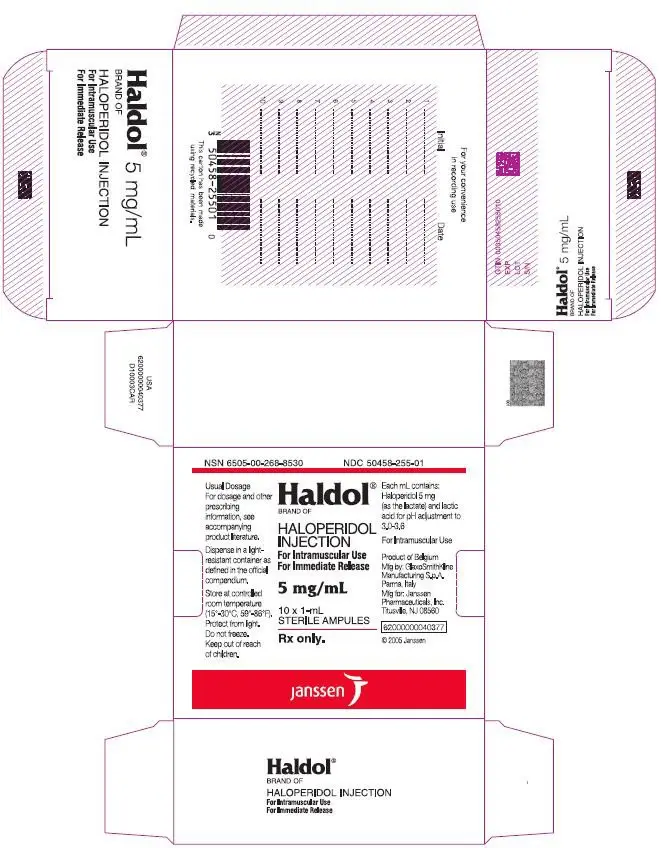
Parenteral medication, administered intramuscularly in doses of 2 to 5 mg, is utilized for prompt control of the acutely agitated schizophrenic patient with moderately severe to very severe symptoms. Depending on the response of the patient, subsequent doses may be given, administered as often as every hour, although 4 to 8 hour intervals may be satisfactory. The maximum dose is 20 mg/day.
Controlled trials to establish the safety and effectiveness of intramuscular administration in children have not been conducted.
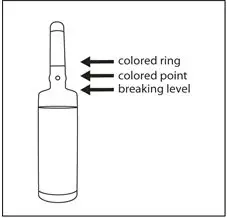
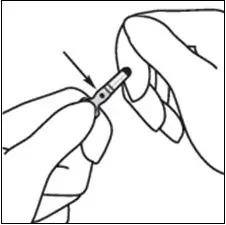
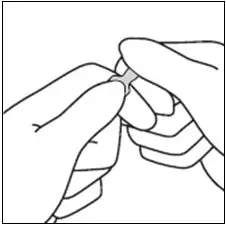
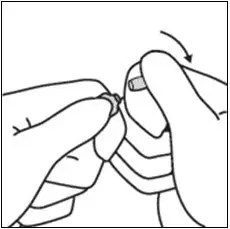
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
| HALDOL
haloperidol injection |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Janssen Pharmaceuticals, Inc. (063137772) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Janssen Pharmaceutica N.V. | 400345889 | API MANUFACTURE(50458-255) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| GlaxoSmithKline | 338471078 | MANUFACTURE(50458-255) , ANALYSIS(50458-255) | |