Drug Detail:Harvoni (Ledipasvir and sofosbuvir [ le-dip-as-vir-and-soe-fos-bue-vir ])
Drug Class: Antiviral combinations
Highlights of Prescribing Information
HARVONI® (ledipasvir and sofosbuvir) tablets, for oral use
HARVONI® (ledipasvir and sofosbuvir) oral pellets
Initial U.S. Approval: 2014
WARNING: RISK OF HEPATITIS B VIRUS REACTIVATION IN PATIENTS COINFECTED WITH HCV AND HBV
See full prescribing information for complete boxed warning.
Hepatitis B virus (HBV) reactivation has been reported, in some cases resulting in fulminant hepatitis, hepatic failure, and death. (5.1)
Recent Major Changes
| Indications and Usage (1) | 8/2019 |
| Dosage and Administration | |
| Recommended Treatment Regimen and Duration in Patients 3 Years of Age and Older with Genotype 1, 4, 5, or 6 HCV (2.2) | 8/2019 |
| Recommended Dosage in Pediatric Patients 3 Years of Age and Older (2.4) | 8/2019 |
| Preparation and Administration of Oral Pellets (2.5) | 8/2019 |
| Renal Impairment (2.6) | 11/2019 |
Indications and Usage for Harvoni
HARVONI is a fixed-dose combination of ledipasvir, a hepatitis C virus (HCV) NS5A inhibitor, and sofosbuvir, an HCV nucleotide analog NS5B polymerase inhibitor, and is indicated for the treatment of chronic hepatitis C virus (HCV) in adults and pediatric patients 3 years of age and older:
- Genotype 1, 4, 5, or 6 infection without cirrhosis or with compensated cirrhosis
- Genotype 1 infection with decompensated cirrhosis, in combination with ribavirin
- Genotype 1 or 4 infection who are liver transplant recipients without cirrhosis or with compensated cirrhosis, in combination with ribavirin. (1)
Harvoni Dosage and Administration
- Testing prior to the initiation of therapy: Test all patients for HBV infection by measuring HBsAg and anti-HBc. (2.1)
- Recommended treatment regimen and duration in patients 3 years of age and older: (2.2)
| HCV Genotype | Patient Population | Regimen and Duration |
|---|---|---|
| Genotype 1 | Treatment-naïve without cirrhosis or with compensated cirrhosis (Child-Pugh A) | HARVONI 12 weeks |
| Treatment-experienced without cirrhosis | HARVONI 12 weeks |
|
| Treatment-experienced with compensated cirrhosis (Child-Pugh A) | HARVONI 24 weeks |
|
| Treatment-naïve and treatment-experienced with decompensated cirrhosis (Child-Pugh B or C) | HARVONI + ribavirin 12 weeks |
|
| Genotype 1 or 4 | Treatment-naïve and treatment-experienced liver transplant recipients without cirrhosis, or with compensated cirrhosis (Child-Pugh A) | HARVONI + ribavirin 12 weeks |
| Genotype 4, 5, or 6 | Treatment-naïve and treatment-experienced without cirrhosis or with compensated cirrhosis (Child-Pugh A) | HARVONI 12 weeks |
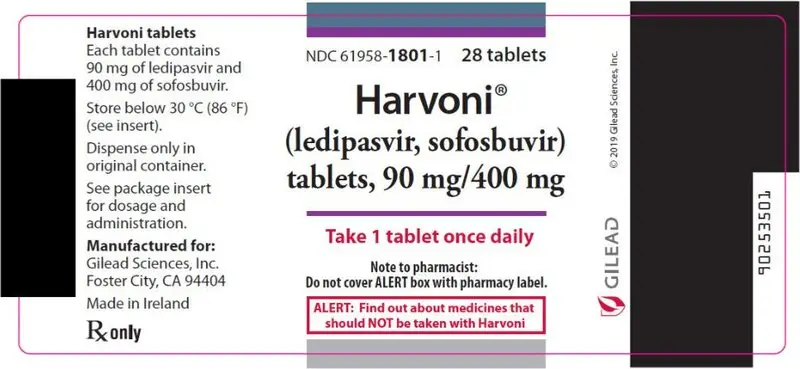
- Recommended dosage in adults: One tablet (90 mg of ledipasvir and 400 mg of sofosbuvir) taken orally once daily with or without food. (2.3)
- Recommended dosage in pediatric patients 3 years and older: Recommended dosage of HARVONI in pediatric patients 3 years of age and older is based on weight. Refer to Table 2 of the full prescribing information for specific dosing guidelines based on body weight. (2.4)
- Instructions for Use should be followed for preparation and administration of HARVONI oral pellets. (2.5)
- HCV/HIV-1 coinfection: For adult and pediatric patients with HCV/HIV-1 coinfection, follow the dosage recommendations in the tables in the full prescribing information. (2.3, 2.4)
- If used in combination with ribavirin, follow the recommendations for ribavirin dosing and dosage modifications. (2.3, 2.4)
- For patients with any degree of renal impairment, including end stage renal disease on dialysis, no HARVONI dosage adjustment is recommended. (2.6)
Dosage Forms and Strengths
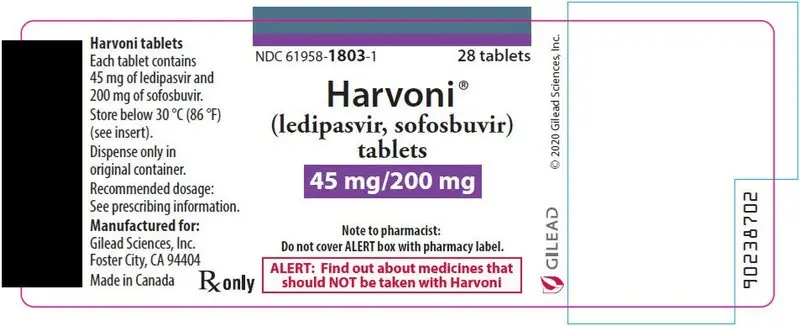
- Tablets: 90 mg of ledipasvir and 400 mg of sofosbuvir; 45 mg of ledipasvir and 200 mg of sofosbuvir. (3)
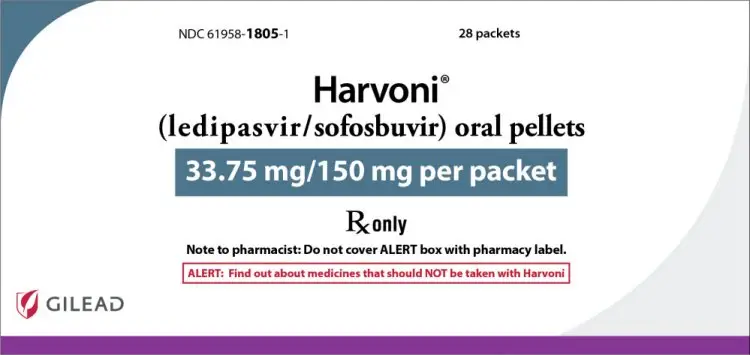
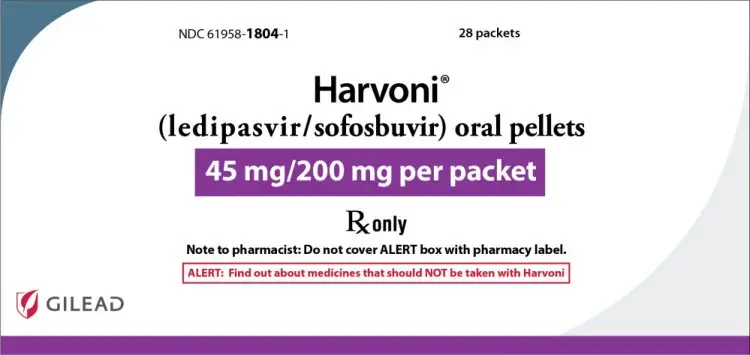
- Oral Pellets: 45 mg of ledipasvir and 200 mg of sofosbuvir; 33.75 mg of ledipasvir and 150 mg of sofosbuvir. (3)
Contraindications
If used in combination with ribavirin, all contraindications to ribavirin also apply to HARVONI combination therapy. (4)
Warnings and Precautions
- Risk of Hepatitis B Virus Reactivation: Test all patients for evidence of current or prior HBV infection before initiation of HCV treatment. Monitor HCV/HBV coinfected patients for HBV reactivation and hepatitis flare during HCV treatment and post-treatment follow-up. Initiate appropriate patient management for HBV infection as clinically indicated. (5.1)
- Bradycardia with amiodarone coadministration: Serious symptomatic bradycardia may occur in patients taking amiodarone, particularly in patients also receiving beta blockers, or those with underlying cardiac comorbidities and/or advanced liver disease. Coadministration of amiodarone with HARVONI is not recommended. In patients without alternative, viable treatment options, cardiac monitoring is recommended. (5.2, 6.2, 7.2)
Adverse Reactions/Side Effects
- The most common adverse reactions (incidence greater than or equal to 10%, all grades) observed with treatment with HARVONI were fatigue, headache, and asthenia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Gilead Sciences, Inc. at 1-800-GILEAD-5 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Coadministration with amiodarone may result in serious symptomatic bradycardia. Use of HARVONI with amiodarone is not recommended. (5.2, 6.2, 7.2)
- P-gp inducers (e.g., rifampin, St. John's wort): May alter concentrations of ledipasvir and sofosbuvir. Use of HARVONI with P-gp inducers is not recommended. (5.3, 7, 12.3)
- Consult the full prescribing information prior to use for potential drug interactions. (5.2, 5.3, 7, 12.3)
- Clearance of HCV infection with direct acting antivirals may lead to changes in hepatic function, which may impact safe and effective use of concomitant medications. Frequent monitoring of relevant laboratory parameters (INR or blood glucose) and dose adjustments of certain concomitant medications may be necessary. (7.2)
Use In Specific Populations
- Pediatric Use: No data are available regarding the safety of HARVONI in pediatric patients with renal impairment. (8.4)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 3/2020
Related/similar drugs
Epclusa, Sovaldi, Vosevi, Mavyret, ribavirin, sofosbuvirFull Prescribing Information
WARNING: RISK OF HEPATITIS B VIRUS REACTIVATION IN PATIENTS COINFECTED WITH HCV AND HBV
Test all patients for evidence of current or prior hepatitis B virus (HBV) infection before initiating treatment with HARVONI. HBV reactivation has been reported in HCV/HBV coinfected patients who were undergoing or had completed treatment with HCV direct acting antivirals and were not receiving HBV antiviral therapy. Some cases have resulted in fulminant hepatitis, hepatic failure, and death. Monitor HCV/HBV coinfected patients for hepatitis flare or HBV reactivation during HCV treatment and post-treatment follow-up. Initiate appropriate patient management for HBV infection as clinically indicated [see Warnings and Precautions (5.1)].
1. Indications and Usage for Harvoni
HARVONI is indicated for the treatment of adults and pediatric patients 3 years of age and older with chronic hepatitis C virus (HCV) [see Dosage and Administration (2.2 and 2.3) and Clinical Studies (14)]:
- genotype 1, 4, 5, or 6 infection without cirrhosis or with compensated cirrhosis
- genotype 1 infection with decompensated cirrhosis, for use in combination with ribavirin
- genotype 1 or 4 infection who are liver transplant recipients without cirrhosis or with compensated cirrhosis, for use in combination with ribavirin
2. Harvoni Dosage and Administration
2.1 Testing Prior to the Initiation of Therapy
Test all patients for evidence of current or prior HBV infection by measuring hepatitis B surface antigen (HBsAg) and hepatitis B core antibody (anti-HBc) before initiating HCV treatment with HARVONI [see Warnings and Precautions (5.1)].
2.2 Recommended Treatment Regimen and Duration in Patients 3 Years of Age and Older with Genotype 1, 4, 5, or 6 HCV
Table 1 shows the recommended HARVONI treatment regimen and duration based on patient population. Relapse rates are affected by baseline host and viral factors and differ between treatment durations for certain subgroups [see Clinical Studies (14)].
For patients with HCV/HIV-1 coinfection, follow the dosage recommendations in Table 1 [see Clinical Studies (14)]. Refer to Drug Interactions (7) for dosage recommendations for concomitant HIV-1 antiviral drugs.
| HCV Genotype | Patient Population | Treatment Regimen and Duration |
|---|---|---|
|
||
| Genotype 1 | Treatment-naïve without cirrhosis or with compensated cirrhosis (Child-Pugh A) | HARVONI 12 weeks* |
| Treatment-experienced† without cirrhosis | HARVONI 12 weeks | |
| Treatment-experienced† with compensated cirrhosis (Child-Pugh A) | HARVONI 24 weeks‡ | |
| Treatment-naïve and treatment-experienced† with decompensated cirrhosis (Child-Pugh B or C) | HARVONI + ribavirin§ 12 weeks | |
| Genotype 1 or 4 | Treatment-naïve and treatment-experienced† liver transplant recipients without cirrhosis, or with compensated cirrhosis (Child-Pugh A) | HARVONI + ribavirin§ 12 weeks |
| Genotype 4, 5, or 6 | Treatment-naïve and treatment-experienced†, without cirrhosis or with compensated cirrhosis (Child-Pugh A) | HARVONI 12 weeks |
2.3 Recommended Dosage in Adults
The recommended dosage of HARVONI in adults with genotype 1, 4, 5, or 6 HCV is one tablet (90 mg ledipasvir and 400 mg sofosbuvir) taken orally once daily with or without food [see Clinical Pharmacology (12.3)].
The daily dosage of ribavirin is weight-based (1000 mg for patients <75 kg and 1200 mg for those ≥75 kg) administered orally in two divided doses with food.
In patients with decompensated cirrhosis, the starting dosage of ribavirin is 600 mg and can be titrated up to 1000 mg for patients <75 kg and 1200 mg for those ≥75 kg in two divided doses with food. If the starting dosage of ribavirin is not well tolerated, the dosage should be reduced as clinically indicated based on hemoglobin levels.
For further information on ribavirin dosing and dosage modifications, refer to the ribavirin prescribing information [see Dosage and Administration (2.4), Use in Specific Populations (8.6), and Clinical Studies (14.5)].
2.4 Recommended Dosage in Pediatric Patients 3 Years of Age and Older
The recommended dosage of HARVONI in pediatric patients 3 years of age and older with genotype 1, 4, 5, or 6 HCV using HARVONI tablets or oral pellets is based on weight (Table 2). Table 3 provides the weight-based dosage of ribavirin when used in combination with HARVONI for pediatric patients. Take HARVONI tablets or pellets (with or without food) once daily [see Dosage and Administration (2.5), Clinical Pharmacology (12.3), and Clinical Studies (14.7)]. HARVONI pellets can be taken in pediatric patients who cannot swallow the tablet formulation.
| Body Weight (kg) | Dosing of HARVONI Tablets or Oral Pellets | HARVONI Daily Dose |
|---|---|---|
| at least 35 | one 90 mg/400 mg tablet once daily or two 45 mg/200 mg tablets once daily or two 45 mg/200 mg packets of pellets once daily | 90 mg/400 mg per day |
| 17 to less than 35 | one 45 mg/200 mg tablet once daily or one 45 mg/200 mg packet of pellets once daily | 45 mg/200 mg per day |
| less than17 | one 33.75 mg/150 mg packet of pellets once daily | 33.75 mg/150 mg per day |
| Body Weight (kg) | Oral Ribavirin Daily Dosage* |
|---|---|
|
|
| less than 47 | 15 mg per kg per day (divided dose AM and PM) |
| 47–49 | 600 mg per day (1 × 200 mg AM, 2 × 200 mg PM) |
| 50–65 | 800 mg per day (2 × 200 mg AM, 2 × 200 mg PM) |
| 66–80 | 1000 mg per day (2 × 200 mg AM, 3 × 200 mg PM) |
| greater than 80 | 1200 mg per day (3 × 200 mg AM, 3 × 200 mg PM) |
2.5 Preparation and Administration of Oral Pellets
See the HARVONI oral pellets full Instructions for Use for details on the preparation and administration of HARVONI pellets.
Do not chew HARVONI pellets. If HARVONI pellets are administered with food, sprinkle the pellets on one or more spoonfuls of non-acidic soft food at or below room temperature. Examples of non-acidic foods include pudding, chocolate syrup, mashed potato, and ice cream. Take HARVONI pellets within 30 minutes of gently mixing with food and swallow the entire contents without chewing to avoid a bitter aftertaste.
2.6 Renal Impairment
No dosage adjustment of HARVONI is recommended in patients with any degree of renal impairment, including end stage renal disease (ESRD) on dialysis [see Dosage and Administration (2.3)]. Take HARVONI with or without ribavirin according to the recommendations in Table 1 [see Adverse Reactions (6.1), Use in Specific Populations (8.6), and Clinical Studies (14.6)]. Refer to ribavirin tablet prescribing information for ribavirin dosage modification for patients with CrCl less than or equal to 50 mL per minute.
3. Dosage Forms and Strengths
HARVONI is available as tablets or pellets for oral use. Each dosage form is available in two dose strengths.
- 90 mg/400 mg Tablets: orange, diamond-shaped, film-coated tablet debossed with "GSI" on one side and "7985" on the other side of the tablet. Each tablet contains 90 mg ledipasvir and 400 mg sofosbuvir.
- 45 mg/200 mg Tablets: white, capsule-shaped, film-coated tablets, debossed with "GSI" on one side and "HRV" on the other side. Each tablet contains 45 mg ledipasvir and 200 mg sofosbuvir.
- 45 mg/200 mg Pellets: orange pellets in unit-dose packets. Each packet contains 45 mg ledipasvir and 200 mg sofosbuvir.
- 33.75 mg/150 mg Pellets: orange pellets in unit-dose packets. Each packet contains 33.75 mg ledipasvir and 150 mg sofosbuvir.
4. Contraindications
If HARVONI is administered with ribavirin, the contraindications to ribavirin also apply to this combination regimen. Refer to the ribavirin prescribing information for a list of contraindications for ribavirin [see Dosage and Administration (2.2)].
5. Warnings and Precautions
5.1 Risk of Hepatitis B Virus Reactivation in Patients Coinfected with HCV and HBV
Hepatitis B virus (HBV) reactivation has been reported in HCV/HBV coinfected patients who were undergoing or had completed treatment with HCV direct acting antivirals, and who were not receiving HBV antiviral therapy. Some cases have resulted in fulminant hepatitis, hepatic failure, and death. Cases have been reported in patients who are HBsAg positive and also in patients with serologic evidence of resolved HBV infection (i.e., HBsAg negative and anti-HBc positive). HBV reactivation has also been reported in patients receiving certain immunosuppressants or chemotherapeutic agents; the risk of HBV reactivation associated with treatment with HCV direct-acting antivirals may be increased in these patients.
HBV reactivation is characterized as an abrupt increase in HBV replication manifesting as a rapid increase in serum HBV DNA level. In patients with resolved HBV infection, reappearance of HBsAg can occur. Reactivation of HBV replication may be accompanied by hepatitis, i.e., increases in aminotransferase levels and, in severe cases, increases in bilirubin levels, liver failure, and death can occur.
Test all patients for evidence of current or prior HBV infection by measuring HBsAg and anti-HBc before initiating HCV treatment with HARVONI. In patients with serologic evidence of HBV infection, monitor for clinical and laboratory signs of hepatitis flare or HBV reactivation during HCV treatment with HARVONI and during post-treatment follow-up. Initiate appropriate patient management for HBV infection as clinically indicated.
5.2 Serious Symptomatic Bradycardia When Coadministered with Amiodarone
Postmarketing cases of symptomatic bradycardia, as well as fatal cardiac arrest and cases requiring pacemaker intervention, have been reported when amiodarone is coadministered with HARVONI. Bradycardia has generally occurred within hours to days, but cases have been observed up to 2 weeks after initiating HCV treatment. Patients also taking beta blockers, or those with underlying cardiac comorbidities and/or advanced liver disease, may be at increased risk for symptomatic bradycardia with coadministration of amiodarone. Bradycardia generally resolved after discontinuation of HCV treatment. The mechanism for this effect is unknown.
Coadministration of amiodarone with HARVONI is not recommended. For patients taking amiodarone who have no other alternative, viable treatment options and who will be coadministered HARVONI:
- Counsel patients about the risk of serious symptomatic bradycardia
- Cardiac monitoring in an in-patient setting for the first 48 hours of coadministration is recommended, after which outpatient or self-monitoring of the heart rate should occur on a daily basis through at least the first 2 weeks of treatment.
Patients who are taking HARVONI who need to start amiodarone therapy due to no other alternative, viable treatment options should undergo similar cardiac monitoring as outlined above.
Due to amiodarone's long half-life, patients discontinuing amiodarone just prior to starting HARVONI should also undergo similar cardiac monitoring as outlined above.
Patients who develop signs or symptoms of bradycardia should seek medical evaluation immediately. Symptoms may include near-fainting or fainting, dizziness or lightheadedness, malaise, weakness, excessive tiredness, shortness of breath, chest pains, confusion, or memory problems [see Adverse Reactions (6.2), Drug Interactions (7.2)].
5.3 Risk of Reduced Therapeutic Effect Due to Use with P-gp Inducers
The concomitant use of HARVONI and P-gp inducers may significantly decrease ledipasvir and sofosbuvir plasma concentrations and may lead to a reduced therapeutic effect of HARVONI. Therefore, the use of HARVONI with P-gp inducers (e.g., rifampin, St. John's wort) is not recommended [see Drug Interactions (7.2)].
5.4 Risks Associated with Ribavirin Combination Treatment
If HARVONI is administered with ribavirin, the warnings and precautions for ribavirin, in particular the pregnancy avoidance warning, apply to this combination regimen. Refer to the ribavirin prescribing information for a full list of the warnings and precautions for ribavirin [see Dosage and Administration (2.2)].
6. Adverse Reactions/Side Effects
The following serious adverse reactions are described below and elsewhere in labeling:
- Serious Symptomatic Bradycardia When Coadministered with Amiodarone [see Warnings and Precautions (5.2)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
If HARVONI is administered with ribavirin to adults, refer to the prescribing information for ribavirin for a description of ribavirin-associated adverse reactions.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of HARVONI. Because postmarketing reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
7. Drug Interactions
7.1 Potential for Drug Interaction
As HARVONI contains ledipasvir and sofosbuvir, any interactions that have been identified with these agents individually may occur with HARVONI.
After oral administration of HARVONI, sofosbuvir is rapidly absorbed and subject to extensive first-pass hepatic extraction. In clinical pharmacology studies, both sofosbuvir and the inactive metabolite GS-331007 were monitored for purposes of pharmacokinetic analyses.
Ledipasvir is an inhibitor of the drug transporters P-gp and breast cancer resistance protein (BCRP) and may increase intestinal absorption of coadministered substrates for these transporters.
Ledipasvir and sofosbuvir are substrates of drug transporters P-gp and BCRP while GS-331007 is not. P-gp inducers (e.g., rifampin, St. John's wort) may decrease ledipasvir and sofosbuvir plasma concentrations, leading to reduced therapeutic effect of HARVONI, and the use with P-gp inducers is not recommended with HARVONI [see Warnings and Precautions (5.3)].
7.2 Established and Potentially Significant Drug Interactions
Clearance of HCV infection with direct acting antivirals may lead to changes in hepatic function, which may impact the safe and effective use of concomitant medications. For example, altered blood glucose control resulting in serious symptomatic hypoglycemia has been reported in diabetic patients in postmarketing case reports and published epidemiological studies. Management of hypoglycemia in these cases required either discontinuation or dose modification of concomitant medications used for diabetes treatment.
Frequent monitoring of relevant laboratory parameters (e.g., International Normalized Ratio [INR] in patients taking warfarin, blood glucose levels in diabetic patients) or drug concentrations of concomitant medications such as cytochrome P450 substrates with a narrow therapeutic index (e.g., certain immunosuppressants) is recommended to ensure safe and effective use. Dose adjustments of concomitant medications may be necessary.
Table 6 provides a listing of established or potentially clinically significant drug interactions. The drug interactions described are based on studies conducted with either HARVONI, the components of HARVONI (ledipasvir and sofosbuvir) as individual agents, or are predicted drug interactions that may occur with HARVONI [see Warnings and Precautions (5.2, 5.3) and Clinical Pharmacology (12.3)].
| Concomitant Drug Class: Drug Name | Effect on Concentration† | Clinical Comment |
|---|---|---|
| tenofovir DF = tenofovir disoproxil fumarate | ||
|
||
| Acid Reducing Agents: | ↓ ledipasvir | Ledipasvir solubility decreases as pH increases. Drugs that increase gastric pH are expected to decrease concentration of ledipasvir. |
| Antacids (e.g., aluminum and magnesium hydroxide) | It is recommended to separate antacid and HARVONI administration by 4 hours. | |
| H2-receptor antagonists‡ (e.g., famotidine) | H2-receptor antagonists may be administered simultaneously with or 12 hours apart from HARVONI at a dose that does not exceed doses comparable to famotidine 40 mg twice daily. | |
| Proton-pump inhibitors‡ (e.g., omeprazole) | Proton-pump inhibitor doses comparable to omeprazole 20 mg or lower can be administered simultaneously with HARVONI under fasted conditions. | |
| Antiarrhythmics:
amiodarone | Effect on amiodarone, ledipasvir, and sofosbuvir concentrations unknown | Coadministration of amiodarone with HARVONI may result in serious symptomatic bradycardia. The mechanism of this effect is unknown. Coadministration of amiodarone with HARVONI is not recommended; if coadministration is required, cardiac monitoring is recommended [see Warnings and Precautions (5.2), Adverse Reactions (6.2)]. |
| digoxin | ↑ digoxin | Coadministration of HARVONI with digoxin may increase the concentration of digoxin. Therapeutic concentration monitoring of digoxin is recommended when coadministered with HARVONI. |
| Anticonvulsants:
carbamazepine‡ phenytoin phenobarbital | ↓ ledipasvir ↓ sofosbuvir | Coadministration of HARVONI with carbamazepine, phenytoin, or phenobarbital is expected to decrease the concentration of ledipasvir and sofosbuvir, leading to reduced therapeutic effect of HARVONI. Coadministration is not recommended. |
| Antimycobacterials:
rifabutin‡ rifampin‡ rifapentine | ↓ ledipasvir ↓ sofosbuvir | Coadministration of HARVONI with rifampin, rifabutin, or rifapentine is not recommended [see Warnings and Precautions (5.3)]. |
| HIV Antiretrovirals: | ||
| Regimens containing tenofovir DF without an HIV protease inhibitor/ ritonavir or cobicistat | ↑ tenofovir | Monitor for tenofovir-associated adverse reactions in patients receiving HARVONI concomitantly with a regimen containing tenofovir DF without an HIV protease inhibitor/ritonavir or cobicistat. Refer to VIREAD or TRUVADA prescribing information for recommendations on renal monitoring. |
Regimens containing tenofovir DF and an HIV protease inhibitor/ ritonavir or cobicistat
| ↑ tenofovir | The safety of increased tenofovir concentrations in the setting of HARVONI and an HIV protease inhibitor/ritonavir or cobicistat has not been established. Consider alternative HCV or antiretroviral therapy to avoid increases in tenofovir exposures. If coadministration is necessary, monitor for tenofovir-associated adverse reactions. Refer to VIREAD or TRUVADA prescribing information for recommendations on renal monitoring. |
| elvitegravir, cobicistat, emtricitabine, tenofovir DF | ↑ tenofovir | The safety of increased tenofovir concentrations in the setting of HARVONI and the combination of elvitegravir, cobicistat, emtricitabine, and tenofovir DF has not been established. Coadministration is not recommended. |
| tipranavir/ritonavir | ↓ ledipasvir ↓ sofosbuvir | Coadministration of HARVONI with tipranavir/ritonavir is expected to decrease the concentration of ledipasvir and sofosbuvir, leading to reduced therapeutic effect of HARVONI. Coadministration is not recommended. |
| HCV Products:
simeprevir‡ | ↑ ledipasvir ↑ simeprevir | Concentrations of ledipasvir and simeprevir are increased when simeprevir is coadministered with ledipasvir. Coadministration of HARVONI with simeprevir is not recommended. |
| Herbal Supplements:
St. John's wort (Hypericum perforatum) | ↓ ledipasvir ↓ sofosbuvir | Coadministration of HARVONI with St. John's wort, a P-gp inducer, is not recommended [see Warnings and Precautions (5.3)]. |
| HMG-CoA Reductase Inhibitors:
rosuvastatin | ↑ rosuvastatin | Coadministration of HARVONI with rosuvastatin may significantly increase the concentration of rosuvastatin, which is associated with increased risk of myopathy, including rhabdomyolysis. Coadministration of HARVONI with rosuvastatin is not recommended. |
| atorvastatin | ↑ atorvastatin | Coadministration of HARVONI with atorvastatin may be associated with increased risk of myopathy, including rhabdomyolysis. Monitor closely for HMG-CoA reductase inhibitor-associated adverse reactions, such as myopathy and rhabdomyolysis. |
7.3 Drugs without Clinically Significant Interactions with HARVONI
Based on drug interaction studies conducted with the components of HARVONI (ledipasvir or sofosbuvir) or HARVONI, no clinically significant drug interactions have been either observed or are expected when HARVONI is used with the following drugs [see Clinical Pharmacology (12.3)]: abacavir, atazanavir/ritonavir, cyclosporine, darunavir/ritonavir, dolutegravir, efavirenz, elvitegravir/cobicistat/emtricitabine/tenofovir alafenamide, emtricitabine, lamivudine, methadone, midazolam, oral contraceptives, pravastatin, raltegravir, rilpivirine, tacrolimus, or verapamil. See Table 6 for use of HARVONI with certain HIV antiretroviral regimens [see Drug Interactions (7.2)].
8. Use In Specific Populations
8.3 Females and Males of Reproductive Potential
If HARVONI is administered with ribavirin, the information for ribavirin with regard to pregnancy testing, contraception, and infertility also applies to this combination regimen. Refer to ribavirin prescribing information for additional information.
8.4 Pediatric Use
The safety, pharmacokinetics, and efficacy of HARVONI for treatment of HCV genotype 1 and 4 infection in treatment-naïve and treatment-experienced pediatric patients 3 years of age and older without cirrhosis or with compensated cirrhosis have been established in an open-label, multicenter clinical trial (Study 1116, N=226; 186 treatment-naïve, 40 treatment-experienced) and are comparable to that observed in adults.
The safety and efficacy of HARVONI for treatment of HCV genotypes 5 or 6 infection in pediatric patients 3 years of age and older are supported by comparable ledipasvir, sofosbuvir, and GS-331007 exposures between adults and pediatric patients [see Dosage and Administration (2.2 and 2.4), Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies (14.3, 14.6, 14.7)]. Similar rationale is used to support dosing recommendations for pediatric patients with HCV genotype 1 infection who have decompensated cirrhosis (Child-Pugh B or C) and for pediatric patients with HCV genotype 1 and 4 infection who are liver transplant recipients without cirrhosis or with compensated cirrhosis.
In patients with severe renal impairment, including those requiring dialysis, exposures of GS-331007, the inactive metabolite of sofosbuvir, are increased [see Clinical Pharmacology (12.3)]. No data are available regarding the safety of HARVONI in pediatric patients with renal impairment [see Use in Specific Populations (8.6)].
The safety and efficacy of HARVONI have not been established in pediatric patients less than 3 years of age.
8.5 Geriatric Use
Clinical trials of HARVONI included 225 subjects aged 65 and over (9% of total number of subjects in the clinical studies). No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. No dosage adjustment of HARVONI is warranted in geriatric patients [see Clinical Pharmacology (12.3)].
8.6 Renal Impairment
No dosage adjustment of HARVONI is recommended for patients with mild, moderate, or severe renal impairment, including ESRD requiring dialysis [see Dosage and Administration (2.4), Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies (14.6)]. No safety data are available in subjects with both decompensated cirrhosis and severe renal impairment, including those on dialysis. Additionally, no safety data are available in pediatric patients with renal impairment [see Use in Specific Populations (8.4)]. Refer to ribavirin tablet prescribing information regarding use in patients with renal impairment.
8.7 Hepatic Impairment
No dosage adjustment of HARVONI is recommended for patients with mild, moderate, or severe hepatic impairment (Child-Pugh Class A, B, or C) [see Dosage and Administration (2.3), Clinical Pharmacology (12.3) and Clinical Studies (14.5)].
Clinical and hepatic laboratory monitoring, as clinically indicated, is recommended for patients with decompensated cirrhosis receiving treatment with HARVONI and ribavirin [see Adverse Reactions (6.1)].
10. Overdosage
No specific antidote is available for overdose with HARVONI. If overdose occurs, the patient must be monitored for evidence of toxicity. Treatment of overdose with HARVONI consists of general supportive measures including monitoring of vital signs as well as observation of the clinical status of the patient. Hemodialysis is unlikely to result in significant removal of ledipasvir since ledipasvir is highly bound to plasma protein. Hemodialysis can efficiently remove the predominant circulating metabolite of sofosbuvir, GS-331007, with an extraction ratio of 53%.
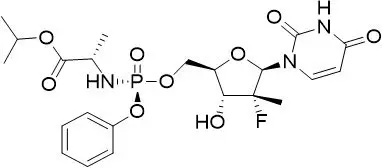
11. Harvoni Description
12. Harvoni - Clinical Pharmacology
12.1 Mechanism of Action
HARVONI is a fixed-dose combination of ledipasvir and sofosbuvir, which are direct-acting antiviral agents against the hepatitis C virus [see Microbiology (12.4)].
13. Nonclinical Toxicology
14. Clinical Studies
14.1 Description of Clinical Trials
The efficacy and safety of HARVONI were evaluated in four trials in genotype 1 HCV mono-infected subjects including one trial exclusively in treatment-experienced subjects with compensated cirrhosis (Child-Pugh A); one trial in genotype 1 or 4 HCV/HIV-1 coinfected subjects; two trials in genotype 4, 5, or 6 HCV mono-infected subjects; two trials in genotype 1 or 4 HCV infected pretransplant subjects with decompensated cirrhosis (Child-Pugh B and C) or post-transplant with Metavir F0–F3 fibrosis, compensated cirrhosis, decompensated cirrhosis, or fibrosing cholestatic hepatitis (FCH); two trials in subjects with severe renal impairment (one of which included subjects requiring dialysis); and one trial in genotype 1 or 4 HCV pediatric subjects 3 years of age and older without cirrhosis or with compensated cirrhosis, as summarized in Table 10 [see Clinical Studies (14.2, 14.3, 14.4, 14.5, 14.6, and 14.7)]:
| Trial | Population | Study Arms (Number of Subjects Treated) |
|---|---|---|
| ESRD = End stage renal disease; RBV = ribavirin; RI = Renal impairment; TN = Treatment-naïve subjects. | ||
|
||
| ION-3 *
(NCT01851330) | GT1, TN without cirrhosis | HARVONI 8 weeks (215) HARVONI + RBV 8 weeks (216) HARVONI 12 weeks (216) |
| ION-1 *
(NCT01701401) | GT1, TN with or without cirrhosis | HARVONI 12 weeks (214) HARVONI + RBV 12 weeks (217) HARVONI 24 weeks (217) HARVONI + RBV 24 weeks (217) |
| ION-2 *
(NCT01768286) | GT1, TE† with or without cirrhosis | HARVONI 12 weeks (109) HARVONI + RBV 12 weeks (111) HARVONI 24 weeks (109) HARVONI + RBV 24 weeks (111) |
| SIRIUS ‡
(NCT01965535) | GT1, TE† with cirrhosis | HARVONI + RBV 12 Weeks (77) HARVONI 24 weeks (77) |
| ION-4 *
(NCT02073656) | GT1 and GT4 HCV/HIV-1 coinfected TN and TE† with or without cirrhosis | HARVONI 12 Weeks (N=327 for GT1; N=8 for GT4) |
| 1119 *
(NCT02081079) | GT4 and GT5, TN and TE† with or without cirrhosis | HARVONI 12 Weeks (N=44 for GT4; N=41 for GT5) |
| ELECTRON-2 *
(NCT01826981) | GT6, TN and TE† with or without cirrhosis | HARVONI 12 Weeks (25) |
| SOLAR-1 * and SOLAR-2 *
(NCT01938430 and NCT02010255) | GT1 and GT4 pre-transplant with decompensated cirrhosis or post-transplant with Metavir F0–F3 fibrosis, compensated cirrhosis, decompensated cirrhosis, or FCH | HARVONI + RBV 12 Weeks (336) HARVONI + RBV 24 weeks (334) |
| 1116 *
(NCT02249182) | GT1 or 4 TN and TE with or without cirrhosis in pediatric subjects 3 years of age and older | HARVONI 12 Weeks (223) HARVONI 24 Weeks (1) |
| 0154 *
(NCT01958281) | GT1 TN and TE† with severe RI without dialysis | HARVONI 12 weeks (18) |
| 4063 *
(NCT03036839) | GT1, 5, or 6 TN and TE§ with or without compensated cirrhosis, with ESRD requiring dialysis | HARVONI 8 Weeks (45) HARVONI 12 Weeks (12) HARVONI 24 Weeks (6) |
HARVONI was administered once daily by mouth in these trials. For subjects without cirrhosis or with compensated cirrhosis who received ribavirin, the ribavirin dosage was 1000 mg per day for subjects weighing less than 75 kg or 1200 mg per day for subjects weighing at least 75 kg. For subjects with decompensated cirrhosis in SOLAR-1 and SOLAR-2 studies, the starting ribavirin dosage was 600 mg per day regardless of transplantation status. Ribavirin dose adjustments were performed according to the ribavirin labeling.
Serum HCV RNA values were measured during the clinical trials using the COBAS TaqMan HCV test (version 2.0), for use with the High Pure System in ION-3, ION-1, ION-2, SIRIUS, and ION-4 studies or the COBAS AmpliPrep/COBAS Taqman HCV test (version 2.0) in ELECTRON-2, 1119, SOLAR-1, SOLAR-2, and 1116 studies. The COBAS TaqMan HCV test (version 2.0) for use with the High Pure System has a lower limit of quantification (LLOQ) of 25 IU per mL and the COBAS AmpliPrep/COBAS Taqman HCV test (version 2.0) has a LLOQ of 15 IU per mL. Sustained virologic response (SVR12), defined as HCV RNA less than LLOQ at 12 weeks after the cessation of treatment, was the primary endpoint in studies in adults and the key efficacy endpoint in the study in pediatric subjects 12 years of age and older. Relapse was a secondary endpoint, which was defined as HCV RNA greater than or equal to LLOQ with 2 consecutive values or last available post-treatment measurement during the post-treatment period after achieving HCV RNA less than LLOQ at end of treatment.
14.3 Clinical Trials in Subjects with Genotype 4, 5, or 6 HCV
Below are trial descriptions, SVR12, and relapse data in the genotype 4, 5, and 6 HCV populations. Trial results in the genotype 4, 5, and 6 HCV populations are based upon limited number of subjects in some subgroups, particularly in subjects who have been previously treated and subjects with cirrhosis.
14.4 Clinical Trials in Subjects Coinfected with HCV and HIV-1
ION-4 was an open-label clinical trial that evaluated the safety and efficacy of 12 weeks of treatment with HARVONI without ribavirin in HCV treatment-naïve and previously treated adult subjects with genotype 1 or 4 HCV infection who were coinfected with HIV-1. Treatment-experienced subjects had failed prior treatment with Peg-IFN + ribavirin, Peg-IFN + ribavirin + an HCV protease inhibitor, or sofosbuvir + ribavirin. Subjects were on a stable HIV-1 antiretroviral therapy that included emtricitabine + tenofovir disoproxil fumarate, administered with efavirenz, rilpivirine, or raltegravir.
Of the 335 treated subjects, the median age was 52 years (range: 26 to 72); 82% of the subjects were male; 61% were White; 34% were Black; mean body mass index was 27 kg/m2 (range: 18 to 66 kg/m2); 75% had genotype 1a HCV infection; 2% had genotype 4 infection; 76% had non-C/C IL28B alleles (CT or TT); and 20% had compensated cirrhosis. Fifty-five percent (55%) of the subjects were treatment-experienced.
Table 18 presents the SVR12 in the ION-4 trial after 12 weeks of HARVONI treatment.
| HARVONI 12 Weeks (N=335) |
|
|---|---|
|
|
| SVR12 | 96% (321/335) |
| Outcome for Subjects without SVR | |
| On-Treatment Virologic Failure | <1% (2/335) |
| Relapse* | 3% (10/333) |
| Other† | <1% (2/335) |
SVR12 rates were 94% (63/67) in subjects with cirrhosis and 98% (46/47) in subjects who were previously treated and had cirrhosis. The relapse rate in the ION-4 trial in Black subjects was 9% (10/115), all of whom were IL28B non-CC genotype, and none in non-Black subjects (0/220). In the ION-1, ION-2, and ION-3 HCV mono-infection studies, relapse rates were 3% (10/305) in Black subjects and 2% (26/1637) in non-Black subjects.
No subject had HIV-1 rebound during the study. The percentage of CD4+ cells did not change during treatment. Median CD4+ cell count increase of 29 cells/mm3 was observed at the end of treatment with HARVONI for 12 weeks.
14.5 Clinical Trials in Liver Transplant Recipients and/or Subjects with Decompensated Cirrhosis
SOLAR-1 and SOLAR-2 were two open-label trials that evaluated 12 and 24 weeks of treatment with HARVONI in combination with ribavirin in HCV treatment-naïve and previously treated adult subjects with genotype 1 and 4 infection who had undergone liver transplantation and/or who had decompensated liver disease. The two trials were identical in study design. Subjects were enrolled in one of the seven groups in the trials based on liver transplantation status and severity of hepatic impairment (see Table 19). Subjects with a CPT score greater than 12 were excluded. Within each group, subjects were randomized in a 1:1 ratio to receive HARVONI + ribavirin for 12 weeks or HARVONI + ribavirin for 24 weeks. For subjects with decompensated cirrhosis in SOLAR-1 and SOLAR-2 studies, the starting ribavirin dosage was 600 mg per day regardless of transplantation status. Ribavirin dose adjustments were performed according to the ribavirin labeling [see Clinical Studies (14.1)].
Demographics and baseline characteristics were balanced across the treatment groups. Of the 670 treated subjects, the median age was 59 years (range: 21 to 81); 77% of the subjects were male; 91% were White; mean body mass index was 28 kg/m2 (range: 18 to 49 kg/m2); 94% and 6% had genotype 1 and 4 HCV infection, respectively; 78% of the subjects failed a prior HCV therapy.
Table 19 presents the pooled SVR12 rates for SOLAR-1 and SOLAR-2 in subjects with genotype 1 HCV treated with HARVONI + ribavirin for 12 weeks. The SVR12 rates observed with 24 weeks of HARVONI + ribavirin were similar to the SVR12 rates observed with 12 weeks of treatment. Therefore, the results for the HARVONI + ribavirin 24 weeks arm are not presented in Table 19.
| HARVONI + RBV 12 weeks (N=307) |
||
|---|---|---|
| SVR12 (N=300)*,† | Relapse (N=288)*,†,‡ | |
|
||
| Pre-transplant | ||
| CPT B | 87% (45/52) | 12% (6/51) |
| CPT C | 88% (35/40) | 5% (2/37) |
| Post-transplant | ||
| Metavir score F0–F3 | 95% (94/99) | 3% (3/97) |
| CPT A | 98% (55/56) | 0% (0/55) |
| CPT B | 89% (41/46) | 2% (1/42) |
| CPT C | 57% (4/7) | 33% (2/6) |
There were 7 subjects with fibrosing cholestatic hepatitis in the 12-week treatment arm, and all subjects achieved SVR12.
In genotype 4 HCV post-transplant subjects without cirrhosis or with compensated cirrhosis treated with HARVONI + ribavirin for 12 weeks (N=12), the SVR12 rate was similar to rates reported with genotype 1; no subjects relapsed. Available data in subjects with genotype 4 HCV who had decompensated cirrhosis (pre- and post-liver transplantation) were insufficient for dosing recommendations; therefore, these results are not presented.
14.6 Clinical Trials in Adults with Severe Renal Impairment, Including those Requiring Dialysis
Trial 0154 was an open-label clinical trial that evaluated 12 weeks of treatment with HARVONI in 18 treatment-naïve and treatment-experienced (subjects with prior exposure to an HCV NS5B polymerase inhibitor were excluded) genotype 1 HCV-infected adults with severe renal impairment not requiring dialysis. At baseline, two subjects (11%) had cirrhosis and the mean eGFR was 24.9 mL/min (range: 9.0 to 39.6). The SVR rate was 100% (18/18).
As shown in the table below, Trial 4063 was an open-label three-arm clinical trial that evaluated 8, 12, and 24 weeks of treatment with HARVONI in a total of 63 adults with chronic HCV infection and ESRD requiring dialysis. Of the 63 subjects, 10% had cirrhosis, 24% were treatment-experienced, 95% were on hemodialysis, and 5% were on peritoneal dialysis; mean duration on dialysis was 12 years (range: 0.2 to 43 years). The SVR rates for the 8, 12, and 24 week HARVONI treatment groups are shown in Table 20.
| HARVONI 8 Weeks (N=45) | HARVONI 12 Weeks (N=12) | HARVONI 24 Weeks (N=6) |
|
|---|---|---|---|
|
|||
| Population | Treatment-naïve, GT 1 HCV Non-cirrhotic | Treatment-naïve and treatment- experienced* GT 1, 5, 6† HCV Non-cirrhotic | Treatment-experienced, GT 1 HCV with compensated cirrhosis |
| SVR12 | 93% (42/45) | 100% (12/12) | 83% (5/6) |
| Outcome for Subjects without SVR | |||
| On-Treatment Virologic Failure | 0/45 | 0/12 | 0/6 |
| Relapse | 0/44 | 0/12 | 0/6 |
| Other‡ | 7% (3/45) | 0/12 | 17% (1/6) |
14.7 Clinical Trial in Pediatric Subjects
The efficacy of HARVONI was evaluated in an open-label trial (Study 1116) in 224 HCV treatment-naïve (N=186) and treatment-experienced (N=38) pediatric subjects 3 years of age or older. This study evaluated 12 weeks of treatment with HARVONI once daily in genotype 1 (N=183) or genotype 4 (N=3) treatment-naive subjects without cirrhosis or with compensated cirrhosis; genotype 1 treatment-experienced subjects without cirrhosis (N=37); and evaluated 24 weeks of treatment with HARVONI once daily in one genotype 1 subject who was both treatment-experienced and cirrhotic.
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
| This Patient Information has been approved by the U.S. Food and Drug Administration | Revised: 03/2020 | |||
| Patient Information | ||||
| HARVONI® (har-VOE-nee) (ledipasvir and sofosbuvir) tablets | HARVONI® (har-VOE-nee) (ledipasvir and sofosbuvir) oral pellets |
|||
| Important: If you take HARVONI with ribavirin, you should also read the Medication Guide for ribavirin. | ||||
| What is the most important information I should know about HARVONI? | ||||
| HARVONI can cause serious side effects, including, Hepatitis B virus reactivation: Before starting treatment with HARVONI, your healthcare provider will do blood tests to check for hepatitis B virus infection. If you have ever had hepatitis B virus infection, the hepatitis B virus could become active again during or after treatment of hepatitis C virus with HARVONI. Hepatitis B virus becoming active again (called reactivation) may cause serious liver problems including liver failure and death. Your healthcare provider will monitor you if you are at risk for hepatitis B virus reactivation during treatment and after you stop taking HARVONI. |
||||
| For more information about side effects, see the section "What are the possible side effects of HARVONI?" | ||||
| What is HARVONI? | ||||
| HARVONI is a prescription medicine used to treat adults and children 3 years of age and older with chronic (lasting a long time) hepatitis C virus (HCV): | ||||
|
||||
| It is not known if HARVONI is safe and effective in children with HCV under 3 years of age. | ||||
| Before taking HARVONI, tell your healthcare provider about all of your medical conditions, including if you: | ||||
|
||||
| Tell your healthcare provider about all of the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. HARVONI and other medicines may affect each other. This can cause you to have too much or not enough HARVONI or other medicines in your body. This may affect the way HARVONI or your other medicines work, or may cause side effects. Keep a list of your medicines to show your healthcare provider and pharmacist. | ||||
|
||||
| Do not start taking a new medicine without telling your healthcare provider. Your healthcare provider can tell you if it is safe to take HARVONI with other medicines. | ||||
| How should I take HARVONI? | ||||
|
||||
| If you take too much HARVONI, call your healthcare provider or go to the nearest hospital emergency room right away. | ||||
| How should I give HARVONI oral pellets to my child?
See the detailed Instructions for Use for information about how to give or take a dose of HARVONI oral pellets. |
||||
|
||||
| What are the possible side effects of HARVONI? | ||||
| HARVONI can cause serious side effects, including: | ||||
|
||||
|
|
|
||
| The most common side effects of HARVONI include: | ||||
|
|
|
||
| These are not all the possible side effects of HARVONI. For more information, ask your healthcare provider or pharmacist. | ||||
| Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. | ||||
| How should I store HARVONI? | ||||
|
||||
| Keep HARVONI and all medicines out of the reach of children. | ||||
| General information about the safe and effective use of HARVONI | ||||
| Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use HARVONI for a condition for which it was not prescribed. Do not give HARVONI to other people, even if they have the same symptoms you have. It may harm them. | ||||
| You can ask your healthcare provider or pharmacist for information about HARVONI that is written for health professionals. | ||||
| What are the ingredients in HARVONI? | ||||
| Active ingredients: ledipasvir and sofosbuvir | ||||
| Inactive ingredients, Tablets 90/400 mg: colloidal silicon dioxide, copovidone, croscarmellose sodium, lactose monohydrate, magnesium stearate, and microcrystalline cellulose. | ||||
| The tablet film-coat contains: FD&C yellow #6/sunset yellow FCF aluminum lake, polyethylene glycol, polyvinyl alcohol, talc, and titanium dioxide. | ||||
| Inactive ingredients, Tablets 45/200 mg: colloidal silicon dioxide, copovidone, croscarmellose sodium, lactose monohydrate, magnesium stearate, and microcrystalline cellulose. | ||||
| The tablet film-coat contains: polyethylene glycol, polyvinyl alcohol partially hydrolyzed, talc, and titanium dioxide. | ||||
| Inactive ingredients, Oral Pellets: amino-methacrylate copolymer, colloidal silicon dioxide, copovidone, croscarmellose sodium, hypromellose, iron oxide red, iron oxide yellow, lactose monohydrate, magnesium stearate, microcrystalline cellulose, polyethylene glycol, talc, and titanium dioxide. | ||||
| Manufactured and distributed by: Gilead Sciences, Inc., Foster City, CA 94404 For more information, call 1-800-445-3235 or go to www.HARVONI.com. HARVONI is a trademark of Gilead Sciences, Inc. All other trademarks referenced herein are the property of their respective owners. ©2020 Gilead Sciences, Inc. All rights reserved. 205834-GS-011 |
||||
INSTRUCTIONS FOR USE HARVONI® (har-VOE-nee) (ledipasvir and sofosbuvir) pellets, for oral use
Read the Patient Information that comes with HARVONI oral pellets for important information about HARVONI.
This Instructions for Use contains information on how to take HARVONI oral pellets. Be sure you understand and follow the instructions. If you have any questions, ask your healthcare provider or pharmacist.
Important Information You Need to Know Before Taking HARVONI oral pellets
- For oral use only (take by mouth with or without food).
- Do not open the HARVONI oral pellet packet(s) until ready to use.
- HARVONI oral pellets are orange pellets supplied as single-use packets in cartons. Each carton contains 28 packets.
- Do not use HARVONI oral pellets if the carton tamper-evident seal, or the pellets packet seal, is broken or damaged.
| Preparing a dose of HARVONI oral pellets to be taken with food: |
Before you prepare a dose of HARVONI oral pellets to be taken with food, gather the following supplies:
- Daily HARVONI oral pellet packet(s), as prescribed by your healthcare provider
- One or more spoonfuls of non-acidic soft food such as pudding, chocolate syrup, mashed potato, or ice cream
- Bowl
- Spoon
- Scissors (optional)
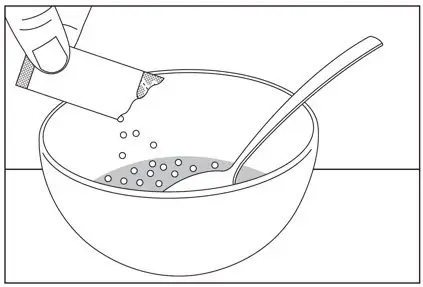
Step 1: Add one or more spoonfuls of non-acidic soft food to the bowl first.
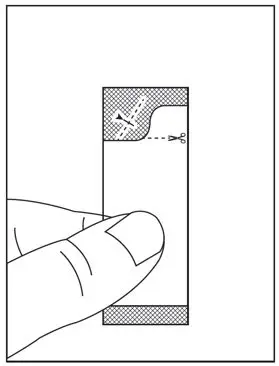
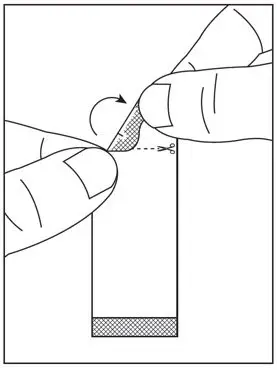
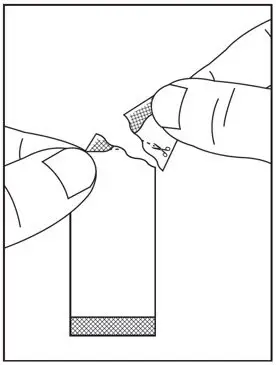
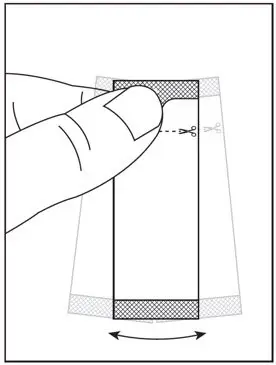
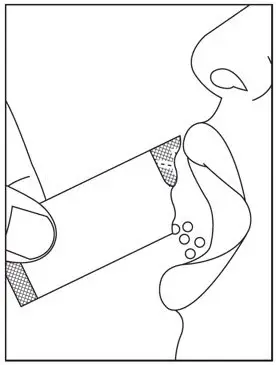
| Step 2: Hold the HARVONI oral pellets packet with the cut line on top (see Figure A). | Step 3: Shake the packet gently to settle the pellets to the bottom of the packet (see Figure B). |
| Figure A | Figure B |
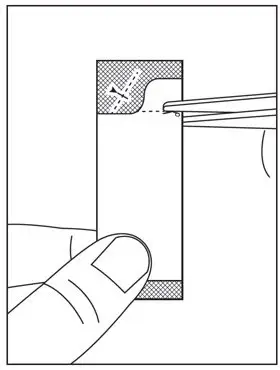
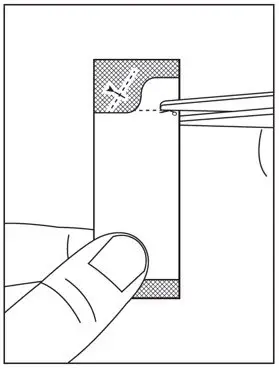
Step 4: Cut the packet along the cut line with scissors (see Figure C), or fold the packet back at the tear line (see Figure D) and tear open (see Figure E).
Step 5: Carefully pour the entire contents of the prescribed number of HARVONI oral pellet packet(s) onto the food in the bowl and gently mix with a spoon (see Figure F). Make sure that no HARVONI oral pellets remain in the packet(s).
Step 6: Take the HARVONI oral pellets and food mixture within 30 minutes without chewing to avoid a bitter taste. Ensure all of the HARVONI oral pellets are taken.
| Preparing a dose of HARVONI oral pellets to be taken without food: |
Before you prepare a dose of HARVONI oral pellets to be taken without food, gather the following supplies:
- Daily HARVONI oral pellet packet(s), as prescribed by your healthcare provider
- Scissors (optional)
- Water (optional)
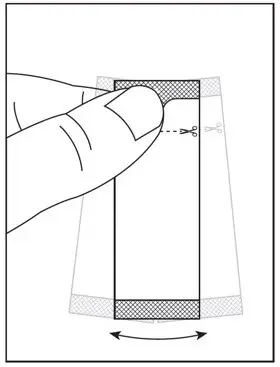
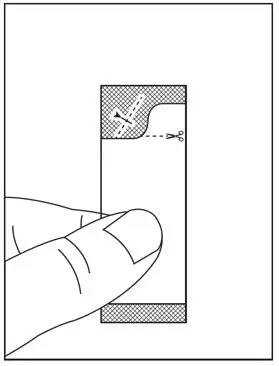
| Step 1: Hold the HARVONI oral pellets packet with the cut line on top (see Figure G). | Step 2: Shake the packet gently to settle the pellets to the bottom of the packet (see Figure H). |
| Figure G | Figure H |
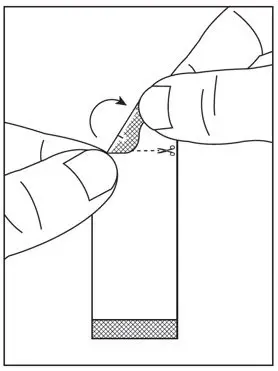
Step 3: Cut the packet along the cut line with scissors (see Figure I), or fold the packet back at the tear line (see Figure J) and tear open (see Figure K).
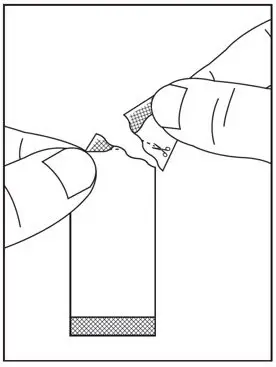
Step 4: Pour the entire contents of the HARVONI oral pellets packet directly in the mouth and swallow without chewing to avoid a bitter taste (see Figure L). Water may be taken after swallowing the pellets, if needed. Make sure that no HARVONI oral pellets remain in the packet. If your healthcare provider prescribed more than one HARVONI oral pellets packet, repeat Steps 1 through 4.
 |
| Figure L |
Storing HARVONI oral pellets
- Store HARVONI pellets below 86°F (30°C).
- Keep HARVONI oral pellets and all medicines out of the reach of children.
Disposing of HARVONI oral pellets
- Throw away any unused portion. Do not store and reuse any leftover HARVONI mixture (pellets mixed with food).
For more information, call 1-800-445-3235 or go to www.HARVONI.com.
Manufactured for and distributed by: Gilead Sciences, Inc., Foster City, CA 94404
HARVONI is a trademark of Gilead Sciences, Inc., or its related companies.
© 2020 Gilead Sciences, Inc. All rights reserved.
205834-GS-011
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Issued: March 2020
| HARVONI
ledipasvir and sofosbuvir tablet, film coated |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| HARVONI
ledipasvir and sofosbuvir tablet, film coated |
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
| HARVONI
ledipasvir and sofosbuvir pellet |
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
| HARVONI
ledipasvir and sofosbuvir pellet |
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
| Labeler - Gilead Sciences, Inc (185049848) |