Drug Detail:Hemgenix (Etranacogene dezaparvovec-drlb)
Drug Class: Miscellaneous uncategorized agents
Highlights of Prescribing Information
HEMGENIX (etranacogene dezaparvovec-drlb) suspension, for intravenous infusion
Initial U.S. Approval: 2022
Indications and Usage for Hemgenix
HEMGENIX is an adeno-associated virus vector-based gene therapy indicated for the treatment of adults with Hemophilia B (congenital Factor IX deficiency) who: (1)
- Currently use Factor IX prophylaxis therapy, or
- Have current or historical life-threatening hemorrhage, or
- Have repeated, serious spontaneous bleeding episodes.
Hemgenix Dosage and Administration
For single-use intravenous infusion only. (2)
- Perform baseline testing to select patients, including testing for Factor IX inhibitor presence and liver health tests. (2.1)
- The recommended dose of HEMGENIX is 2 × 1013 genome copies (gc) per kg of body weight. (2.1)
- Administer HEMGENIX as an intravenous infusion after dilution with 0.9% normal saline at a constant infusion rate of 500 ml/hour (8 mL/min). (2.1)
Dosage Forms and Strengths
HEMGENIX is a suspension for intravenous infusion. (3)
HEMGENIX is provided in kits containing 10 to 48 single-use vials, each kit constituting a dosage unit based on the patient's body weight. (3)
HEMGENIX has a nominal concentration of 1 × 1013 gc/mL, and each vial contains an extractable volume of not less than 10 mL (3)
Contraindications
None. (4)
Warnings and Precautions
- Infusion reactions: Monitor during administration and for at least 3 hours after end of infusion. If symptoms occur, slow or interrupt administration. Re-start administration at a slower infusion once resolved. (2.3, 5.1)
- Hepatotoxicity: Closely monitor transaminase levels once per week for 3 months after HEMGENIX administration to mitigate the risk of potential hepatotoxicity. Continue to monitor transaminases in all patients who developed liver enzyme elevations until liver enzymes return to baseline. Consider corticosteroid treatment should elevations occur. (5.2)
- Hepatocellular carcinogenicity: For patients with preexisting risk factors (e.g., cirrhosis, advanced hepatic fibrosis, hepatitis B or C, non-alcoholic fatty liver disease (NAFLD), chronic alcohol consumption, non-alcoholic steatohepatitis (NASH), and advanced age), perform regular (e.g., annual) liver ultrasound and alpha-fetoprotein testing following administration. (5.4)
- Monitoring Laboratory tests: Monitor for Factor IX activity and Factor IX inhibitors. (5.5)
Adverse Reactions/Side Effects
The most common adverse reactions (incidence ≥5%) were elevated ALT, headache, blood creatine kinase elevations, flu-like symptoms, infusion-related reactions, fatigue, malaise and elevated AST. (6)
To report SUSPECTED ADVERSE REACTIONS, contact CSL Behring at 1-866-915-6958 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Use In Specific Populations
No dose adjustment is required in geriatric, hepatic, or renal impaired patients. (8.5, 8.6, 8.7)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 12/2022
Related/similar drugs
BeneFix, NovoSeven RT, Alprolix, Ixinity, Sevenfact, IdelvionFull Prescribing Information
1. Indications and Usage for Hemgenix
HEMGENIX is an adeno-associated virus vector-based gene therapy indicated for treatment of adults with Hemophilia B (congenital Factor IX deficiency) who:
- Currently use Factor IX prophylaxis therapy, or
- Have current or historical life-threatening hemorrhage, or
- Have repeated, serious spontaneous bleeding episodes.
2. Hemgenix Dosage and Administration
For single-use intravenous infusion only.
For patient selection:
- Perform Factor IX inhibitor titer testing.
In case of a positive test result for human Factor IX inhibitors, perform a re-test within approximately 2 weeks. If both the initial test and re-test results are positive, do not administer HEMGENIX to this patient. - Perform liver health assessments, including:
- Enzyme testing [alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP) and total bilirubin)],
- Hepatic ultrasound and elastography.
2.1 Dose
The recommended dose of HEMGENIX is 2 × 1013 genome copies (gc) per kilogram (kg) of body weight (or 2 mL/kg body weight) administered as an intravenous infusion after dilution with 0.9% sodium chloride solution (normal saline) [see Dosage and Administration (2.2)].
Calculate the dose as follows:
| HEMGENIX dose (in mL) = patient body weight (in kilogram) × 2 |
The multiplication factor 2 represents the per kilogram dose (2 × 1013 gc/kg) divided by the amount of genome copies per mL of the HEMGENIX solution (1 × 1013 gc/mL).
Number of HEMGENIX vials needed = HEMGENIX dose (in mL) divided by 10 (round up to next whole number of vials).
The division factor 10 represents the extractable volume of HEMGENIX from each vial (10 mL).
The total volume of the patient's HEMGENIX dose to be diluted may be less than the total volume of vials needed.
Example calculation for 72 kg patient
| Patient Weight | HEMGENIX dose (mL) (body weight multiplied by 2) | Number of Vials needed [HEMGENIX dose (mL) divided by 10, then rounded up] |
|---|---|---|
| 72 kg | 144 mL | 15 |
HEMGENIX can be administered only once.
2.3 Administration
Monitoring Post-Administration
Conduct the following tests after HEMGENIX administration [see Warnings and Precautions (5.2, 5.3, 5.4)]:
- Perform regular liver enzyme testing to monitor for liver enzyme elevations which may indicate immune-mediated hepatotoxicity:
- Monitor ALT and AST (transaminase) levels by testing weekly for 3 months following administration of HEMGENIX. Continue to monitor transaminases in all patients who developed liver enzyme elevations until liver enzymes return to baseline.
- In the event of ALT increase to above normal limits or to twice the patient`s baseline in the first 3 months post-dose, consider implementing a course of corticosteroids. For patients with clinically relevant ALT increases who need corticosteroid treatment, administer the recommended starting dose of 60 mg/day of oral prednisolone or prednisone, with a subsequent taper in response to normalization of the ALT levels (see Table 1):
Table 1. Prednisolone Treatment Applied in Clinical Studies With HEMGENIX: Timeline *Prednisolone Oral Dose (mg/day) - *
- Medications equivalent to prednisolone may also be used. A combined immunosuppressant regimen or the use of other products can be considered in case of prednisolone treatment failure or contraindication.
Week 1 60 Week 2 40 Week 3 30 Week 4 30 Maintenance dose until ALT level returns to baseline level 20 Taper dose after ALT baseline level has been reached Reduce daily dose by 5 mg/week
In the clinical studies, the mean duration of corticosteroid use for elevated transaminases was 81.4 days [Standard Deviation (SD) 28.6] and ranged from 51 to 130 days [see Warnings and Precautions (5.2)]. - Monitor Factor IX activity (e.g., weekly for 3 months).
- Monitor patients regularly for their Factor IX activity, in particular when exogenous Factor IX is administered. It may take several weeks before improved hemostatic control becomes apparent after HEMGENIX infusion; therefore, continued hemostatic support with exogenous human Factor IX may be needed during the first weeks after HEMGENIX infusion [see Clinical Pharmacology (12.3)].
- The use of different assays may impact the test results; therefore, use the same assay and reagents to monitor patients over time, if feasible [see Monitoring Laboratory Tests (5.5)].
- Use of exogenous Factor IX concentrates before and after HEMGENIX administration may impede assessment of endogenous, HEMGENIX-derived Factor IX activity.
- Perform regular alpha-fetoprotein (AFP) level testing and abdominal ultrasound (e.g., annually) in patients with preexisting risk factors for hepatocellular carcinoma (e.g., in patients with cirrhosis, advanced hepatic fibrosis, hepatitis B or C, non-alcoholic fatty liver disease (NAFLD), chronic alcohol consumption, non-alcoholic steatohepatitis (NASH), and advanced age).
- Monitor patients for human Factor IX inhibitors. Post-dose inhibitor testing should be performed if bleeding is not controlled, or plasma Factor IX activity levels decrease [see Warnings and Precautions (5.5)].
3. Dosage Forms and Strengths
HEMGENIX is a clear and colorless suspension for intravenous infusion.
HEMGENIX is provided in a kit containing 10 to 48 vials. Each kit constitutes a dosage unit based on the patient's body weight.
HEMGENIX has a nominal concentration of 1 × 1013 gc/mL, and each vial contains an extractable volume of not less than 10 mL.
5. Warnings and Precautions
5.1 Infusion Reactions
Infusion reactions, including hypersensitivity reactions and anaphylaxis, may occur. Symptoms may include chest tightness, headaches, abdominal pain, lightheadedness, flu-like symptoms, shivering, flushing, rash, and hypertension. Closely monitor patients for signs or symptoms of an infusion reaction throughout the infusion period and for at least 3 hours after end of infusion. Do not infuse the product faster than 500 mL/hour [see Adverse Reactions (6)].
In the event of an infusion reaction during administration, the infusion may be slowed or stopped. If the infusion is stopped, restart at a slower rate when the infusion reaction has resolved. Consider treatment with a corticosteroid or antihistamine for management of an infusion reaction [see Dosage and Administration (2.1)].
5.2 Hepatotoxicity
Intravenous administration of a liver-directed AAV vector could potentially lead to liver transaminase elevations (transaminitis). Transaminitis, particularly when observed in the first 3 months after HEMGENIX administration, is presumed to occur due to immune-mediated injury of transduced hepatocytes and may reduce the therapeutic efficacy of the AAV-vector based gene therapy.
In clinical studies with HEMGENIX, most subjects had asymptomatic, and predominantly mild elevations in transaminases. Elevated ALT levels occurred most often in the first 4 months after HEMGENIX administration. There were some subjects who had a late onset of elevated ALT levels between Months 6-24 (range = 42 IU/L-193 IU/L); however, all of these ALT values were <2× ULN with the exception of one subject. Three additional subjects had AST elevations with onset and resolution between Months 6 and 12 (range = 41 IU/L – 96 IU/L).
In one subject, an ALT elevation >5× ULN occurred 24 days after HEMGENIX administration and resolved by 51 days post-HEMGENIX administration. There was one subject who had an AST elevation > 5× ULN that occurred 11 months post-HEMGENIX administration and resolved to <2× ULN eight days later.
The majority of the elevated ALT values returned to baseline, however 9 subjects' ALT values never resolved to normal (range at 2-year follow up = 48 IU/L – 193 IU/L) [see Adverse Reactions (6)].
Closely monitor transaminase levels once per week for 3 months after HEMGENIX administration to mitigate the risk of potential hepatotoxicity. Continue to monitor transaminases in all patients who developed liver enzyme elevations until liver enzymes return to baseline [see Dosage and Administration (2.3)].
In case of increased ALT levels above the upper limit of normal or double baseline levels, consider implementing a course of corticosteroid, along with human Factor IX activity monitoring [see Dosage and Administration (2.3)].
5.3 Immune-mediated neutralization of the AAV5 vector capsid
In AAV-vector based gene therapies, preexisting neutralizing anti-AAV antibodies may impede transgene expression at desired therapeutic levels. Following treatment with HEMGENIX all subjects developed neutralizing anti-AAV antibodies. Currently, there is no validated neutralizing anti-AAV5 antibody assay.
In the clinical studies with HEMGENIX, an unvalidated clinical trial assay was utilized to assess preexisting neutralizing anti-AAV5 antibodies. The subject sub-group with detectable preexisting neutralizing anti-AAV5 antibodies up to titers of 1:678 showed mean Factor IX activity that was numerically lower compared to that subject sub-group without detectable preexisting neutralizing anti-AAV5 antibodies. Subjects, with and without preexisting neutralizing anti-AAV5 antibodies, demonstrated hemostatic protection. In one subject with a preexisting neutralizing anti-AAV5 antibody titer of 1:3212, no human Factor IX expression was observed, and restart of the exogenous Factor IX prophylaxis was needed for bleeding events. [see Clinical Studies (14)].
5.4 Hepatocellular carcinogenicity
The integration of liver-targeting AAV vector DNA into the genome may carry the theoretical risk of hepatocellular carcinoma development.
HEMGENIX is composed of a non-replicating AAV5 vector whose DNA persists largely in episomal form. Random integration of HEMGENIX vector DNA to the human DNA at low frequency is possible. No HEMGENIX-associated clonal expansion or carcinogenicity was observed in clinical studies [see Clinical Studies (14)]. One subject with preexisting risk factors for developing hepatic cancer developed a hepatocellular carcinoma, which was assessed as not likely related to HEMGENIX treatment based on vector integration site analyses and whole genome sequencing.
Patients with preexisting risk factors for hepatocellular carcinoma (e.g., patients with cirrhosis, advanced hepatic fibrosis, hepatitis C or B, non-alcoholic fatty liver disease (NAFLD), chronic alcohol consumption, non-alcoholic steatohepatitis (NASH), and advanced age) should receive abdominal ultrasound screenings and be monitored regularly (e.g., annually) for alpha-fetoprotein (AFP) elevations in the 5 years following administration [see Dosage and Administration (2.3)].
5.5 Monitoring Laboratory Tests
After HEMGENIX administration, regularly monitor patient's Factor IX activity levels.
When using an in vitro activated partial thromboplastin time (aPTT)-based one-stage clotting assay (OSA) for determining Factor IX activity, plasma Factor IX activity results can be affected by both the type of aPTT reagent and the reference standard used in the assay. This is important to consider particularly when changing the laboratory and/or reagents used in the assay. Therefore, the same assay and reagents are recommended to be used to monitor Factor IX activity over time.
The results of Factor IX activity tests are lower if measured with chromogenic substrate assay (CSA) compared to OSA.
In the clinical efficacy study with HEMGENIX, the post-dose Factor IX activity measured with CSA returned lower values with the mean CSA to OSA Factor IX activity ratio ranging from 0.41 to 0.55.
Monitor patients through appropriate clinical observations and laboratory tests for the development of inhibitors to Factor IX after HEMGENIX administration. Perform an assay that detects Factor IX inhibitors if bleeding is not controlled, or plasma Factor IX activity levels decrease.
6. Adverse Reactions/Side Effects
The most common adverse reactions (incidence ≥5%) reported in clinical studies were ALT elevations, headache, blood creatine kinase elevations, flu-like symptoms, infusion-related reactions, fatigue, malaise, and AST elevations.
The following adverse reactions are discussed in greater detail in other sections of the label:
- Infusion related reactions [see Warnings and Precautions (5.1)].
- Hepatotoxicity [see Warnings and Precautions (5.2)].
- Immune-mediated neutralization of the AAV5 vector capsid [see Warnings and Precautions (5.3)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The safety of HEMGENIX was evaluated in two clinical studies (the first study enrolled 3 subjects and the second study 54 subjects). Both studies enrolled adult male subjects with moderately severe or severe Hemophilia B (N = 57), who received a single intravenous dose of 2 × 1013 gc/kg body weight of HEMGENIX. All subjects entered a follow-up period of 5 years.
No serious adverse reactions were reported [see Clinical Studies (14)]. The most common adverse reactions observed in ≥5% of subjects post-dose are listed in Table 2:
| Adverse Reactions ≥5% | Subjects (%) (N = 57) |
|---|---|
|
|
| Alanine aminotransferase increased | 24 (42%) |
| Headache | 10 (18%) |
| Blood creatine kinase increased | 24 (42%) |
| Flu-like symptoms | 8 (14%) |
| Infusion-related reactions* (see below) | 19* (33%) |
| Hypersensitivity | 2† (4%) |
| Fatigue | 7 (12%) |
| Aspartate aminotransferase increased | 24 (42%) |
| Nausea | 4 (7%) |
| Malaise | 7 (12%) |
Infusion-related reactions were observed in 19 subjects. Infusions were temporarily interrupted in 3 subjects and resumed at a slower infusion rate after treatment with antihistamines and/or corticosteroids. In one subject, infusion was stopped and not resumed (see footnote of Table 2).
There were 24 subjects who had elevated ALT values from Day 8 to 731 post-administration.
Five subjects had ALT elevations >2-3× ULN (range = 89 IU/L – 130 IU/L), one subject had an ALT elevation > 3-5× ULN (193 IU/L) and one subject had an ALT elevation > 5× ULN (275 IU/L). The subject who had the ALT elevation >5× ULN occurred 3 weeks after HEMGENIX administration.
Five subjects had AST elevations > 2-3× ULN (range = 71 IU/L – 118 IU/L), three subjects had AST elevations > 3-5× ULN (range = 127 IU/L – 163 IU/L) and one subject had an AST elevation > 5× ULN (327 IU/L). The subject who had the AST elevation > 5× ULN occurred 11 months post-HEMGENIX administration.
Seventeen subjects had elevations in ALT levels within the first 4 months after HEMGENIX infusion (range = 41 IU/L – 275 IU/L), eleven of these subjects' ALT levels resolved within 4 months post-infusion (range = 41 IU/L – 275 IU/L) and five of these subjects' ALT levels never normalized as of last follow-up (range of values at 2-year follow-up = 48 IU/L – 110 IU/L). Seven additional subjects had ALT elevations with onset between Months 6 to 24 (range = 42 IU/L-193 IU/L), five of these subjects had additional risk factors for having elevated transaminase levels including Hepatitis C and Human Immunodeficiency Virus (HIV). ALT levels never normalized as of last follow-up (range of values at 2-year follow-up = (59 IU/L- 193 IU/L) in three of the subjects with ALT elevations with onset between Months 6 to 24.
Nineteen subjects had elevations in AST levels within 3 months after HEMGENIX infusion (range = 32 IU/L- 163 IU/L). Nine of these subjects' AST elevations resolved within 4 months post-infusion (range = 35 IU/L – 163 IU/L), three resolved within 7 to 13 months post-infusion (range = 35 IU/L – 62 IU/L), and seven of these subjects' AST levels never normalized as of last follow-up (range of values at 2-year follow-up = 36 IU/L – 327 IU/L). The remaining 5 subjects with AST elevation had onset of between 6 months and 2 years post-infusion (range = 36 IU/L – 127 IU/L), and AST levels had not normalized as of the last follow-up for one subject (AST at 2-year follow-up = 127 IU/L) who had additional risk factors for having elevated transaminase levels.
Nine subjects with ALT elevations received a tapered course of corticosteroids. The mean duration of corticosteroid treatment for the elevated ALT was 81.4 days. Nineteen of the 24 subjects with ALT elevations also had a related AST elevation. Twenty-one subjects had elevated transaminase levels and were not treated with corticosteroids. [see Clinical Studies (14)].
8. Use In Specific Populations
8.4 Pediatric Use
The safety and efficacy of HEMGENIX in pediatric patients have not been established.
8.5 Geriatric Use
The clinical studies included a total of 6 geriatric subjects with Hemophilia B, aged 68 to 75 years at time of enrollment. No meaningful differences in the safety and efficacy profile were observed in these subjects compared to subjects aged 18 to 65 years, and no dose adjustment was made [see Clinical Studies (14)].
8.6 Hepatic Impairment
Limited clinical data in subjects with liver impairment indicate numerically lower FIX activity as compared to subjects without hepatic impairment [see Clinical Pharmacology (12.3)]. In the clinical studies, no dose adjustment was made in subjects with hepatic pathologies. The safety and efficacy in subjects with advanced hepatic impairment, including cirrhosis, advanced liver fibrosis, or uncontrolled Hepatitis B and C, have not been studied.
8.7 Renal Impairment
Limited clinical data are available in subjects with mild and moderate renal impairment [see Clinical Pharmacology (12.3)]. In the clinical studies, no dose adjustment was made in these subjects. The safety and efficacy in subjects with severe renal impairment and end-stage renal disease have not been studied.
11. Hemgenix Description
HEMGENIX (etranacogene dezaparvovec-drlb) is an adeno-associated viral vector-based gene therapy for intravenous infusion after dilution. HEMGENIX is a non-replicating recombinant AAV5 containing a codon-optimized DNA sequence of the gain-of-function Padua variant of human Factor IX (variant R338L), under control of a liver-specific promotor 1 (LP1).
HEMGENIX has a nominal concentration of 1 × 1013 gc/mL. Each vial contains an extractable volume of no less than 10 mL of HEMGENIX and the following excipients: sucrose (50 mg/mL), polysorbate-20 (0.22 mg/mL), potassium chloride (0.2 mg/mL), potassium phosphate (0.2 mg/mL), sodium chloride (8 mg/mL), and sodium phosphate (1.2 mg/mL).
HEMGENIX is sterile, clear and colorless suspension, and contains no preservative. After dilution, HEMGENIX should be clear and colorless suspension.
12. Hemgenix - Clinical Pharmacology
12.1 Mechanism of Action
HEMGENIX is an adeno-associated virus serotype 5 (AAV5) based gene therapy designed to deliver a copy of a gene encoding the Padua variant of human coagulation Factor IX (hFIX-Padua). Single intravenous infusion of HEMGENIX results in cell transduction and increase in circulating Factor IX activity in patients with Hemophilia B.
12.3 Pharmacokinetics
12.6 Immunogenicity
In clinical studies sustained humoral immune response to infused AAV5 capsid was observed in all subjects following treatment with HEMGENIX. The neutralizing anti-AAV5 antibody levels raised above the upper limit of quantification by week 3 post-administration and remained elevated, as measured at month 24 post-dose. Re-administration of HEMGENIX in the presence of high anti-AAV5 antibody titer has not been evaluated. Currently, there is no validated neutralizing anti-AAV5 antibody assay.
13. Nonclinical Toxicology
Nonclinical studies were initiated with a predecessor of HEMGENIX product, rAAV5 expressing the wild type human coagulation factor IX (rAAV5-hFIX). HEMGENIX was developed by introducing a 2-nucleotide change in the transgene for hFIX, generating the naturally occurring Padua variant of Factor IX (rAAV5-hFIX-Padua).
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No traditional nonclinical carcinogenicity or mutagenicity studies were conducted with HEMGENIX; such studies were not indicated. No adverse effects were observed in mating rates and fertility indices in healthy naïve female mice following mating with males that were administered the predecessor of HEMGENIX [see Use in specific populations (8.3)]. To evaluate vector integration, host genomic DNA was isolated from liver tissue obtained from healthy mice and NHPs following intravenous administration of the predecessor of HEMGENIX. For both species, the identified rAAV5-hFIX vector DNA sequences represented episomal forms that were not integrated into the host DNA. A low level of integrated rAAV5-hFIX DNA was distributed throughout the host genome with no predilection to specific integration sites, including in genes associated with malignant transformation in humans.
13.2 Animal Toxicology and/or Pharmacology
A pharmacology study was conducted in a murine model of Hemophilia B (B6.129P2-F9tm1Dws. Intravenous administration of the predecessor of HEMGENIX at dose levels ranging from 5×1011 to 2.3×1014 gc/kg, resulted in dose-dependent increases in plasma hFIX protein levels, plasma hFIX clotting activity, and vector transduction in the liver at 4 weeks post-dose.
Intravenous administration of HEMGENIX resulted in a no-observed-adverse-effect-level of 5 × 1013 gc/kg (the maximum dose level administered) in healthy mice and 9 × 1013 gc/kg in NHPs. Vector biodistribution to the liver and hFIX protein levels in the plasma occurred in a dose-dependent manner in both species. Anti-hFIX antibodies developed in 5 out of 12 NHPs administered HEMGENIX, which correlated with a decline in circulating hFIX protein levels beginning at 13 weeks post-dose.
One out of 10 healthy mice administered 5 × 1013 gc/kg of HEMGENIX or the predecessor of HEMGENIX developed pulmonary thrombi at 13 weeks post-dose. This dose level is 2.5-fold higher than the recommended dose level for HEMGENIX. Compared to concurrent controls, prolonged prothrombin time, decreased activated partial thromboplastin time and decreased heart rates were observed in NHPs administered 9 × 1013 gc/kg of HEMGENIX during the 26-week study. This dose level is 4.5-fold higher than the recommended dose level for HEMGENIX.
14. Clinical Studies
The efficacy of HEMGENIX was evaluated in a prospective, open-label, single-dose, single-arm, multi-national study (N = 54). The study enrolled adult male subjects aged 19 to 75 years, with severe or moderately severe Hemophilia B, who received a single intravenous dose of 2 × 1013 gc/kg body weight of HEMGENIX and entered a follow-up period of 5 years. The study is on-going.
The 54 subjects prospectively completed a lead-in period of at least six months with the intent to receive standard of care routine Factor IX prophylaxis. These 54 subjects then received the indicated single intravenous dose of HEMGENIX. Subjects were then followed up monthly until Month 12, and then at 6-month intervals until Year 5. For the efficacy evaluation, data up to 18 months post-treatment were used. Of the 54 subjects, 53 subjects completed at least 18 months of follow-up in the ongoing study. One subject with numerous cardiovascular and urologic risk factors, aged 75 years at screening, died of urosepsis and cardiogenic shock at Month 15 post-dose (at age 77 years) unrelated to treatment. Another subject received around 10% of the intended dose of HEMGENIX due to an infusion-related hypersensitivity reaction.
The main efficacy outcome was a non-inferiority test of annualized bleeding rate (ABR) during Months 7 to 18 after HEMGENIX treatment compared with ABR during the lead-in period. All bleeding episodes, regardless of investigator assessment, were counted. Subjects were allowed to continue prophylaxis during Months 0 to 6. The estimated mean ABR during Months 7 to 18 after HEMGENIX treatment was 1.9 bleeds/year with a 95% confidence interval (CI) of (1.0, 3.4), compared with an estimated mean ABR of 4.1 [95% CI: 3.2, 5.4] during the lead-in period. The ABR ratio (Months 7 to 18 post-treatment / lead-in) was 0.46 [95% CI: 0.26, 0.81], demonstrating non-inferiority of ABR during Months 7 to 18 compared to the lead-in period.
Two subjects were not able to stop routine prophylaxis after HEMGENIX treatment. During Months 7 to 18, an additional subject received prophylaxis from Days 396-534 [approximately 20 weeks].
| Lead-in Period* | Months 7 to 18† after HEMGENIX treatment | |
|---|---|---|
| Abbreviations: ABR = Annualized Bleeding Rate; CI = Confidence Interval | ||
|
||
| All Bleeds | 136 | 96‡ |
| Follow-up time (Person-Year) | 33 | 52 |
| Mean Adjusted ABR (95% CI)§ | 4.1 (3.2, 5.4) | 1.9 (1.0, 3.4) |
| Subjects with Bleeds | 40 (74%) | 20 (37%) |
| Subjects with Zero Bleeds | 14 (26%) | 34 (63%) |
| Observed Spontaneous Bleed Count (Proportion of total bleeds)¶ | 50 (37%) | 14 (26%) |
| Observed Joint Bleed Count (Proportion of total bleeds)¶ | 77 (57%) | 19 (35%) |
After a single-dose of HEMGENIX, increases in Factor IX activity were observed [see Pharmacokinetics (12.3)].
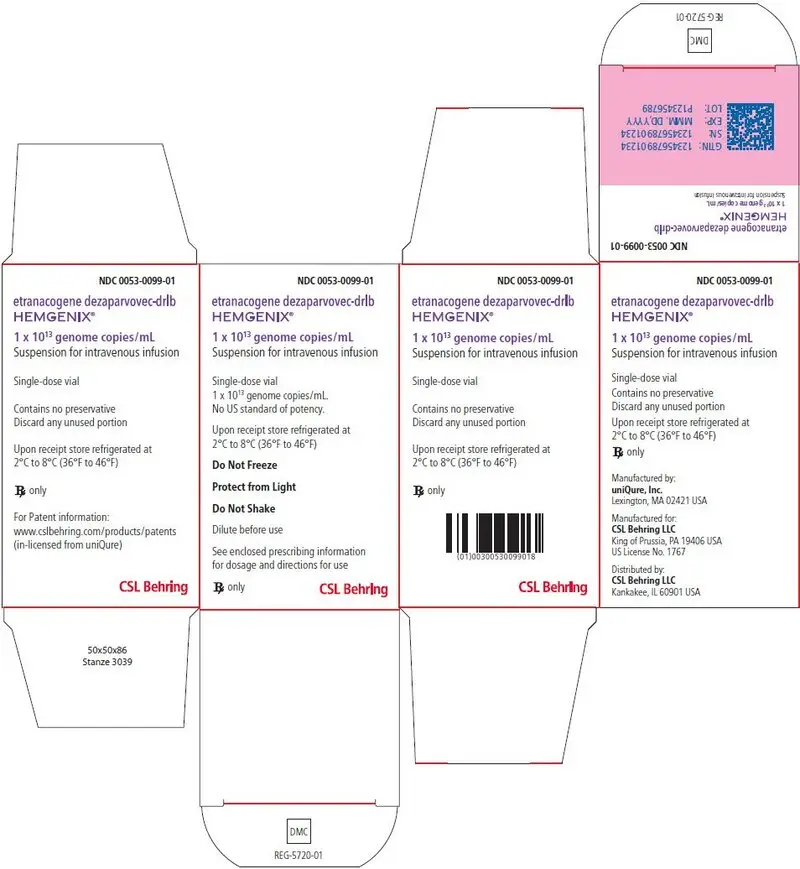
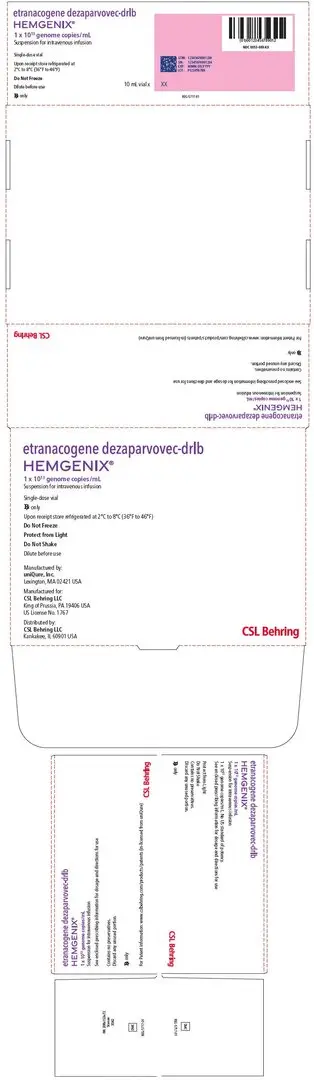
16. How is Hemgenix supplied
16.1 How Supplied
HEMGENIX is supplied as sterile, preservative-free, clear, and colorless suspension. HEMGENIX has a nominal concentration of 1 × 1013 gc/mL.
HEMGENIX is provided as a customized kit to meet dosing requirements for each patient [see Dosage and Administration (2.1)], with each kit containing 10 (ten) to 48 (forty-eight) single-use vials (NDC 0053-0099-01), each with an extractable volume of no less than 10 mL of HEMGENIX (see5). The total number of vials in each kit corresponds to the dosing requirement for the individual patient depending on the patient`s body weight [see Dosage and Administration (2.1)]. The customized kit is accompanied with patient`s specific identifier number (Lot) on the outer carton. Each HEMGENIX kit may contain different drug product lots.
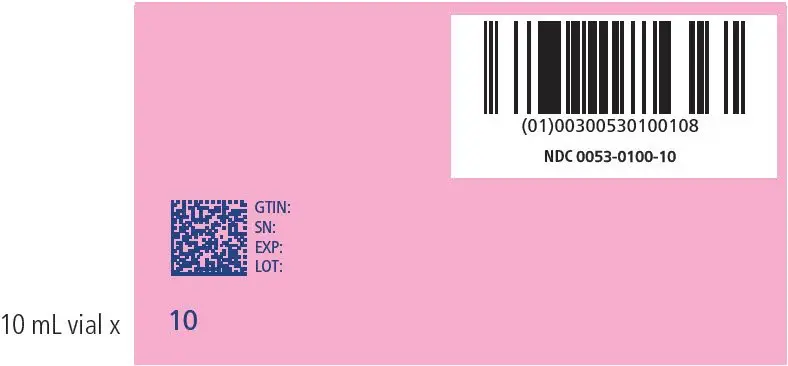
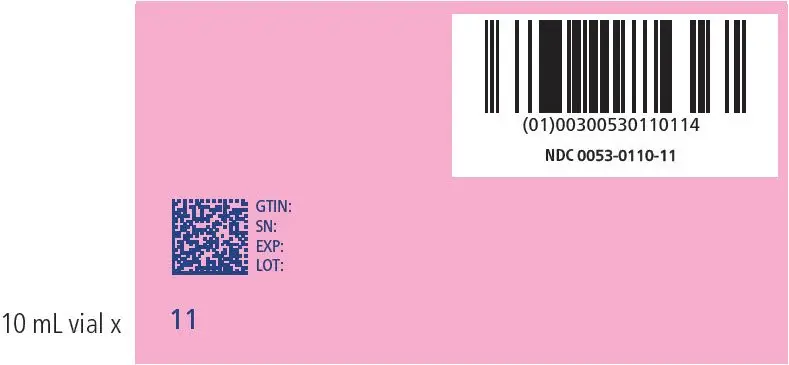
Kit sizes and National Drug Codes (NDC) are provided in Table 5:
| Total Number of Vials per Kit | Patient Body Weight (kg) | Total Volume per Kit (mL) | NDC Number |
|---|---|---|---|
| 10 | 46-50 | 100 | 0053-0100-10 |
| 11 | 51-55 | 110 | 0053-0110-11 |
| 12 | 56-60 | 120 | 0053-0120-12 |
| 13 | 61-65 | 130 | 0053-0130-13 |
| 14 | 66-70 | 140 | 0053-0140-14 |
| 15 | 71-75 | 150 | 0053-0150-15 |
| 16 | 76-80 | 160 | 0053-0160-16 |
| 17 | 81-85 | 170 | 0053-0170-17 |
| 18 | 86-90 | 180 | 0053-0180-18 |
| 19 | 91-95 | 190 | 0053-0190-19 |
| 20 | 96-100 | 200 | 0053-0200-20 |
| 21 | 101-105 | 210 | 0053-0210-21 |
| 22 | 106-110 | 220 | 0053-0220-22 |
| 23 | 111-115 | 230 | 0053-0230-23 |
| 24 | 116-120 | 240 | 0053-0240-24 |
| 25 | 121-125 | 250 | 0053-0250-25 |
| 26 | 126-130 | 260 | 0053-0260-26 |
| 27 | 131-135 | 270 | 0053-0270-27 |
| 28 | 136-140 | 280 | 0053-0280-28 |
| 29 | 141-145 | 290 | 0053-0290-29 |
| 30 | 146-150 | 300 | 0053-0300-30 |
| 31 | 151-155 | 310 | 0053-0310-31 |
| 32 | 156-160 | 320 | 0053-0320-32 |
| 33 | 161-165 | 330 | 0053-0330-33 |
| 34 | 166-170 | 340 | 0053-0340-34 |
| 35 | 171-175 | 350 | 0053-0350-35 |
| 36 | 176-180 | 360 | 0053-0360-36 |
| 37 | 181-185 | 370 | 0053-0370-37 |
| 38 | 186-190 | 380 | 0053-0380-38 |
| 39 | 191-195 | 390 | 0053-0390-39 |
| 40 | 196-200 | 400 | 0053-0400-40 |
| 41 | 201-205 | 410 | 0053-0410-41 |
| 42 | 206-210 | 420 | 0053-0420-42 |
| 43 | 211-215 | 430 | 0053-0430-43 |
| 44 | 216-220 | 440 | 0053-0440-44 |
| 45 | 221-225 | 450 | 0053-0450-45 |
| 46 | 226-230 | 460 | 0053-0460-46 |
| 47 | 231-235 | 470 | 0053-0470-47 |
| 48 | 236-240 | 480 | 0053-0480-48 |
17. Patient Counseling Information
Inform patients that:
- Pre-infusion blood tests will be necessary to look for Factor IX inhibitors. If these exist, the patient may not be a good candidate for HEMGENIX [see Dosage and Administration (2)].
- Prior to HEMGENIX treatment, a liver ultrasound and elastography will be performed. Patients found to have pre-existing risk factors for hepatocellular carcinoma will be monitored annually in the 5 years following infusion [see Warnings and Precautions (5.4)].
- Infusion reactions can occur. Patients will be monitored during and for at least 3 hours following administration. If a reaction occurs, the infusion rate may be slowed or interrupted, then started at a slower rate [see Warnings and Precautions (5.1)].
- HEMGENIX can elevate certain liver enzymes. Weekly blood tests will be required to monitor for this for 3 months after treatment. Corticosteroid treatment may be necessary if this occurs [see Warnings and Precautions (5.2)].
- If post-infusion bleeding is not controlled or if bleeding returns, then blood tests will be performed for Factor IX activity and neutralizing Factor IX inhibitors [see Warnings and Precautions (5.5)].
- Vector distribution in blood (within the body), and vector shedding in semen and other excreta and secreta can occur post-infusion. It is not known how long this will continue. Patients should not donate blood, organs, tissues, or cells for transplantation [see Pharmacokinetics (12.3)].
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| HEMGENIX
etranacogene dezaparvovec kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| Labeler - CSL Behring (058268293) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| CSL Behring LLC | 058268293 | MANUFACTURE(0053-0100, 0053-0110, 0053-0120, 0053-0130, 0053-0140, 0053-0150, 0053-0160, 0053-0170, 0053-0180, 0053-0190, 0053-0200, 0053-0210, 0053-0220, 0053-0230, 0053-0240, 0053-0250, 0053-0260, 0053-0270, 0053-0280, 0053-0290, 0053-0300, 0053-0310, 0053-0320, 0053-0330, 0053-0340, 0053-0350, 0053-0360, 0053-0370, 0053-0380, 0053-0390, 0053-0400, 0053-0410, 0053-0420, 0053-0430, 0053-0440, 0053-0450, 0053-0460, 0053-0470, 0053-0480) | |