Drug Detail:Imfinzi (Durvalumab [ dur-val-ue-mab ])
Drug Class: Anti-PD-1 and PD-L1 monoclonal antibodies (immune checkpoint inhibitors)
Highlights of Prescribing Information
IMFINZI® (durvalumab) injection, for intravenous use
Initial U.S. Approval: 2017
Recent Major Changes
Indications and Usage (1.3) 09/2022
Indications and Usage (1.4) 10/2022
Indications and Usage (1.1) 11/2022
Dosage and Administration (2.1) 09/2022
Dosage and Administration (2.1, 2.2, 2.3) 10/2022
Dosage and Administration (2.1, 2.3) 11/2022
Warnings and Precautions (5.1, 5.2) 10/2022
Warnings and Precautions (5.1, 5.2) 11/2022
Indications and Usage for Imfinzi
IMFINZI is a programmed death-ligand 1 (PD-L1) blocking antibody indicated:
- •
- for the treatment of adult patients with unresectable, Stage III non-small cell lung cancer (NSCLC) whose disease has not progressed following concurrent platinum-based chemotherapy and radiation therapy. (1.1)
- •
- in combination with tremelimumab-actl and platinum-based chemotherapy, for the treatment of adult patients with metastatic non-small cell lung cancer (NSCLC) with no sensitizing epidermal growth factor receptor (EGFR) mutations or anaplastic lymphoma kinase (ALK) genomic tumor aberrations. (1.1)
- •
- in combination with etoposide and either carboplatin or cisplatin, as first-line treatment of adult patients with extensive-stage small cell lung cancer (ES-SCLC). (1.2)
- •
- in combination with gemcitabine and cisplatin, as treatment of adult patients with locally advanced or metastatic biliary tract cancer (BTC). (1.3)
- •
- in combination with tremelimumab-actl, for the treatment of adult patients with unresectable hepatocellular carcinoma (uHCC). (1.4)
Imfinzi Dosage and Administration
- •
- Administer IMFINZI as an intravenous infusion over 60 minutes after dilution. (2.3)
- •
- Stage III NSCLC:
- ∘
- Weight ≥ 30 kg: 10 mg/kg every 2 weeks or 1,500 mg every 4 weeks (2.1)
- ∘
- Weight < 30 kg: 10 mg/kg every 2 weeks (2.1)
- •
- Metastatic NSCLC:
- ∘
- Weight ≥ 30 kg: 1,500 mg every 3 weeks in combination with tremelimumab-actl 75 mg and platinum-based chemotherapy for 4 cycles, and then administer IMFINZI 1,500 mg every 4 weeks as a single agent with histology-based pemetrexed maintenance therapy every 4 weeks, and a fifth dose of tremelimumab-actl 75 mg in combination with IMFINZI dose 6 at week 16 (2.1)
- ∘
- Weight < 30 kg: 20 mg/kg every 3 weeks in combination with tremelimumab-actl 1 mg/kg and platinum-based chemotherapy, and then administer IMFINZI 20 mg/kg every 4 weeks as a single agent with histology-based pemetrexed therapy every 4 weeks, and a fifth dose of tremelimumab-actl 1 mg/kg in combination with IMFINZI dose 6 at week 16 (2.1)
- •
- ES-SCLC:
- ∘
- Weight ≥ 30 kg: With etoposide and either carboplatin or cisplatin, administer IMFINZI 1,500 mg every 3 weeks in combination with chemotherapy, and then 1,500 mg every 4 weeks as a single agent (2.1)
- ∘
- Weight < 30 kg: With etoposide and either carboplatin or cisplatin, administer IMFINZI 20 mg/kg every 3 weeks in combination with chemotherapy, and then 10 mg/kg every 2 weeks as a single agent (2.1)
- •
- BTC:
- ∘
- Weight ≥ 30 kg: administer IMFINZI 1,500 mg every 3 weeks in combination with chemotherapy, and then 1,500 mg every 4 weeks as a single agent (2.1)
- ∘
- Weight < 30 kg: administer IMFINZI 20 mg/kg every 3 weeks in combination with chemotherapy, and then 20 mg/kg every 4 weeks as a single agent (2.1)
- •
- uHCC:
- ∘
- Weight ≥ 30 kg: IMFINZI 1,500 mg in combination with tremelimumab-actl 300 mg as a single dose at Cycle 1/Day 1, followed by IMFINZI as a single agent every 4 weeks (2.1)
- ∘
- Weight < 30 kg: IMFINZI 20 mg/kg in combination with tremelimumab-actl 4 mg/kg as a single dose at Cycle 1/Day 1, followed by IMFINZI as a single agent every 4 weeks (2.1)
- •
- See full Prescribing Information for preparation and administration instructions and dosage modifications for adverse reactions.
Dosage Forms and Strengths
- •
- Injection: 500 mg/10 mL (50 mg/mL) solution in a single-dose vial. (3)
- •
- Injection: 120 mg/2.4 mL (50 mg/mL) solution in a single-dose vial. (3)
Contraindications
None. (4)
Warnings and Precautions
- •
- Immune-Mediated Adverse Reactions (5.1)
- ∘
- Immune-mediated adverse reactions, which may be severe or fatal, can occur in any organ system or tissue, including the following: immune-mediated pneumonitis, immune-mediated colitis, immune-mediated hepatitis, immune-mediated endocrinopathies, immune-mediated dermatologic adverse reactions, immune-mediated nephritis and renal dysfunction, solid organ transplant rejection, and immune-mediated pancreatitis.
- o
- Monitor for early identification and management. Evaluate liver enzymes, creatinine, and thyroid function at baseline and periodically during treatment.
- o
- Withhold or permanently discontinue based on severity and type of reaction.
- •
- Infusion-Related Reactions: Interrupt, slow the rate of infusion, or permanently discontinue IMFINZI based on the severity of the reaction. (5.2)
- •
- Complications of Allogeneic HSCT: Fatal and other serious complications can occur in patients who receive allogeneic HSCT before or after being treated with a PD-1/PD-L1 blocking antibody. (5.3)
- •
- Embryo-Fetal Toxicity: Can cause fetal harm. Advise females of reproductive potential of the potential risk to a fetus and use of effective contraception. (5.4, 8.1, 8.3)
Adverse Reactions/Side Effects
IMFINZI as a Single Agent
- •
- Most common adverse reactions (≥ 20% of patients with unresectable, Stage III NSCLC) are cough, fatigue, pneumonitis/radiation pneumonitis, upper respiratory tract infections, dyspnea, and rash. (6.1)
IMFINZI in Combination with Platinum-Based Chemotherapy
- •
- Most common adverse reactions (≥ 20% of patients with extensive-stage SCLC) are nausea, fatigue/asthenia, and alopecia. (6.1)
IMFINZI in Combination with gemcitabine and cisplatin
- •
- Most common adverse reactions (≥ 20% of patients with BTC) are fatigue, nausea, constipation, decreased appetite, abdominal pain, rash, and pyrexia. (6.1)
IMFINZI in Combination with Tremelimumab-actl
- •
- Most common adverse reactions (≥ 20%) of patients with uHCC are rash, diarrhea, fatigue, pruritis, musculoskeletal pain, and abdominal pain. (6.1)
IMFINZI in Combination with Tremelimumab-actl and Platinum-Based Chemotherapy
Most common adverse reactions (≥ 20% of patients with metastatic NSCLC) were nausea, fatigue, musculoskeletal pain, decreased appetite, rash, and diarrhea. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca at 1-800-236-9933 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Use In Specific Populations
Lactation: Advise not to breastfeed. (8.2)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 6/2023
Related/similar drugs
Opdivo, Retevmo, methotrexate, Keytruda, Avastin, pembrolizumab, cisplatinFull Prescribing Information
1. Indications and Usage for Imfinzi
1.1 Non-Small Cell Lung Cancer
- •
- IMFINZI is indicated for the treatment of adult patients with unresectable Stage III non-small cell lung cancer (NSCLC) whose disease has not progressed following concurrent platinum-based chemotherapy and radiation therapy.
- •
- IMFINZI, in combination with tremelimumab-actl and platinum-based chemotherapy, is indicated for the treatment of adult patients with metastatic NSCLC with no sensitizing epidermal growth factor receptor (EGFR) mutations or anaplastic lymphoma kinase (ALK) genomic tumor aberrations.
1.2 Small Cell Lung Cancer
IMFINZI, in combination with etoposide and either carboplatin or cisplatin, is indicated for the first-line treatment of adult patients with extensive-stage small cell lung cancer (ES-SCLC).
2. Imfinzi Dosage and Administration
2.1 Recommended Dosage
The recommended dosages for IMFINZI as a single agent and IMFINZI in combination with other therapeutic agents are presented in Tables 1, 2 and 3.
Administer IMFINZI as an intravenous infusion after dilution as recommended [see Dosage and Administration (2.3)].
|
||
|
Indication |
Recommended IMFINZI Dosage |
Duration of Therapy |
|
Single Agent |
||
|
Unresectable stage III NSCLC |
Patients with a body weight of ≥ 30 kg: 10 mg/kg every 2 weeks or 1,500 mg every 4 weeks Patients with a body weight of < 30 kg: 10 mg/kg every 2 weeks |
Until disease progression, unacceptable toxicity, or a maximum of 12 months |
|
Combination with Other Therapeutic Agents |
||
|
ES-SCLC |
Patients with a body weight of ≥ 30 kg: 1,500 mg in combination with chemotherapy* every 3 weeks (21 days) for 4 cycles, followed by 1,500 mg every 4 weeks as a single agent Patients with a body weight of < 30 kg: 20 mg/kg in combination with chemotherapy* every 3 weeks (21 days) for 4 cycles, followed by 10 mg/kg every 2 weeks as a single agent |
Until disease progression or unacceptable toxicity |
|
BTC |
Patients with a body weight of ≥ 30 kg: 1,500 mg in combination with chemotherapy* every 3 weeks (21 days) up to 8 cycles followed by 1,500 mg every 4 weeks as a single agent Patients with a body weight of < 30 kg: 20 mg/kg in combination with chemotherapy* every 3 weeks (21 days) up to 8 cycles followed by 20 mg/kg every 4 weeks as a single agent |
Until disease progression or until unacceptable toxicity |
|
uHCC |
Patients with a body weight of ≥ 30 kg and more:
|
After Cycle 1 of combination therapy, administer IMFINZI as a single agent every 4 weeks until disease progression or unacceptable toxicity |
IMFINZI in Combination with Tremelimumab-actl and Platinum-Based Chemotherapy
The recommended dosage schedule and regimens for IMFINZI for the treatment of metastatic non-small cell lung cancer (NSCLC) are provided in Tables 2 and 3.
Weigh patients prior to each infusion.
Calculate the appropriate dose using Table 3 below based on the patient’s weight and tumor histology.
| Week*,† | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | |
| Cycle: | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||||||||||||||||
|
|||||||||||||||||||||||||
|
IMFINZI*,‡ |
X |
X |
X |
X |
X |
X |
X |
X |
|||||||||||||||||
|
Tremelimumab-actl‡,§ |
X |
X |
X |
X |
X | ||||||||||||||||||||
|
Chemotherapy |
X |
X |
X |
X |
X¶ |
X¶ |
X¶ |
XÞ |
|||||||||||||||||
| Tumor Histology | Patient Weight | IMFINZI Dosage | Tremelimumab-actl Dosage* | Platinum-based Chemotherapy Regimen* |
|---|---|---|---|---|
|
||||
|
Non-Squamous |
≥30kg |
1,500 mg |
75 mg |
OR
|
|
<30kg |
20 mg/kg |
1 mg/kg |
||
|
Squamous |
≥30kg |
1,500 mg |
75 mg |
OR
|
|
<30kg |
20 mg/kg |
1 mg/kg |
||
2.2 Dosage Modifications for Adverse Reactions
No dose reduction for IMFINZI is recommended. In general, withhold IMFINZI for severe (Grade 3) immune-mediated adverse reactions. Permanently discontinue IMFINZI for life-threatening (Grade 4) immune-mediated adverse reactions, recurrent severe (Grade 3) immune-mediated reactions that require systemic immunosuppressive treatment, or an inability to reduce corticosteroid dose to 10 mg or less of prednisone or equivalent per day within 12 weeks of initiating corticosteroids.
Dosage modifications for IMFINZI or IMFINZI in combination with tremelimumab-actl and platinum-based chemotherapy for adverse reactions that require management different from these general guidelines are summarized in Table 4.
| Adverse Reaction | Severity* | Dosage Modification |
|---|---|---|
|
||
|
||
|
Grade 2 |
Withhold† |
|
Grade 3 or 4 |
Permanently discontinue |
|
|
Grade 2 |
Withhold† |
|
Grade 3 |
Withhold† or permanently discontinue‡ |
|
|
Grade 4 |
Permanently discontinue |
|
|
Any grade |
Permanently discontinue |
|
ALT or AST increases to more than 3 and up to 8 times the ULN or total bilirubin increases to more than 1.5 and up to 3 times ULN |
Withhold† |
|
ALT or AST increases to more than 8 times ULN or total bilirubin increases to more than 3 times the ULN |
Permanently discontinue |
|
|
AST or ALT is more than 1 and up to 3 times ULN at baseline and increases to more than 5 and up to 10 times ULN or AST or ALT is more than 3 and up to 5 times ULN at baseline and increases to more than 8 and up to 10 times ULN |
Withhold† |
|
AST or ALT increases to more than 10 times ULN or total bilirubin increases to more than 3 times ULN |
Permanently discontinue |
|
|
Grade 3 or 4 |
Withhold until clinically stable or permanently discontinue depending on severity |
|
Grade 2 or 3 increased blood creatinine |
Withhold† |
|
Grade 4 increased blood creatinine |
Permanently discontinue |
|
|
Suspected SJS, TEN, or DRESS |
Withhold† |
|
Confirmed SJS, TEN, or DRESS |
Permanently discontinue |
|
|
Grade 2, 3, or 4 |
Permanently discontinue |
|
Grade 2 |
Withhold† |
|
Grade 3 or 4 |
Permanently discontinue |
|
|
Other Adverse Reactions |
||
|
Grade 1 or 2 |
Interrupt or slow the rate of infusion |
|
Grade 3 or 4 |
Permanently discontinue |
|
|
ALT = alanine aminotransferase, AST = aspartate aminotransferase, DRESS = Drug Rash with Eosinophilia and Systemic Symptoms, SJS = Stevens Johnson Syndrome, TEN = toxic epidermal necrolysis, ULN = upper limit normal. |
||
2.3 Preparation and Administration
Preparation
- •
- Visually inspect drug product for particulate matter and discoloration prior to administration, whenever solution and container permit. Discard the vial if the solution is cloudy, discolored, or visible particles are observed.
- •
- Do not shake the vial.
- •
- Withdraw the required volume from the vial(s) of IMFINZI and transfer into an intravenous bag containing 0.9% Sodium Chloride Injection, USP or 5% Dextrose Injection, USP. Mix diluted solution by gentle inversion. Do not shake the solution. The final concentration of the diluted solution should be between 1 mg/mL and 15 mg/mL.
- •
- Discard partially used or empty vials of IMFINZI.
Storage of Infusion Solution
- •
- IMFINZI does not contain a preservative.
- •
- Administer infusion solution immediately once prepared. If the infusion solution is not administered immediately and needs to be stored, the time from preparation until the completion of the infusion should not exceed:
- ∘
- 28 days in a refrigerator at 2°C to 8°C (36°F to 46°F)
- ∘
- 8 hours at room temperature up to 25°C (77°F)
- •
- Do not freeze.
- •
- Do not shake.
Administration
- •
- Administer infusion solution intravenously over 60 minutes through an intravenous line containing a sterile, low-protein binding 0.2 or 0.22 micron in-line filter.
- •
- Use separate infusion bags and filters for each drug product.
IMFINZI in Combination with Other Products
- •
- Administer all drug products as separate intravenous infusions.
- •
- Do not co-administer other drugs through the same infusion line.
- •
- For platinum-based chemotherapy, refer to Prescribing Information for administration information.
- •
- For pemetrexed therapy, refer to Prescribing Information for administration information.
Combination Regimens: Order of Infusions
IMFINZI in Combination with Tremelimumab-actl
- •
- Infuse tremelimumab-actl first, followed by IMFINZI on the same day of dosing.
IMFINZI in Combination with Tremelimumab-actl and Platinum-Based Chemotherapy
- •
- Infuse tremelimumab-actl first, followed by IMFINZI and then platinum-based chemotherapy on the day of dosing.
IMFINZI in Combination with Tremelimumab-actl and Pemetrexed Therapy
- •
- Infuse tremelimumab-actl first, followed by IMFINZI and then pemetrexed therapy on the day of dosing.
Combination Regimens: Infusion Instructions
IMFINZI in Combination with Tremelimumab-actl
- •
- Administer tremelimumab-actl over 60 minutes followed by a 60 minute observation period. Then administer IMFINZI as a separate intravenous infusion over 60 minutes.
IMFINZI in Combination with Tremelimumab-actl and Platinum-Based Chemotherapy/ Pemetrexed Therapy
Cycle 1
- •
- Infuse tremelimumab-actl over 1 hour. One to two hours after completion of tremelimumab-actl infusion, infuse IMFINZI over 1 hour. One to two hours after completion of IMFINZI infusion, administer platinum-based chemotherapy.
Subsequent Cycles
- •
- If there are no infusion reactions during cycle 1, subsequent cycles of IMFINZI can be given immediately after tremelimumab-actl. The time between the end of the IMFINZI infusion and the start of chemotherapy can be reduced to 30 minutes.
3. Dosage Forms and Strengths
Injection: 120 mg/2.4 mL (50 mg/mL) and 500 mg/10 mL (50 mg/mL) clear to opalescent, colorless to slightly yellow solution in a single-dose vial.
5. Warnings and Precautions
5.1 Immune-Mediated Adverse Reactions
IMFINZI is a monoclonal antibody that belongs to a class of drugs that bind to either the programmed death-receptor 1 (PD-1) or the PD-ligand 1 (PD-L1), blocking the PD-1/PD-L1 pathway, thereby removing inhibition of the immune response, potentially breaking peripheral tolerance and inducing immune-mediated adverse reactions. Important immune-mediated adverse reactions listed under Warnings and Precautions may not include all possible severe and fatal immune-mediated reactions.
The incidence and severity of immune-mediated adverse reactions were similar when IMFINZI was administered as a single agent or in combination with chemotherapy or in combination with tremelimumab-actl and platinum-based chemotherapy, unless otherwise noted.
Immune-mediated adverse reactions, which may be severe or fatal, can occur in any organ system or tissue. Immune-mediated adverse reactions can occur at any time after starting treatment with a PD 1/PD-L1 blocking antibody. While immune-mediated adverse reactions usually manifest during treatment with PD-1/PD-L1 blocking antibodies, immune-mediated adverse reactions can also manifest after discontinuation of PD-1/PD-L1 blocking antibodies.
Early identification and management of immune-mediated adverse reactions are essential to ensure safe use of PD-1/PD-L1 blocking antibodies. Monitor patients closely for symptoms and signs that may be clinical manifestations of underlying immune-mediated adverse reactions. Evaluate liver enzymes, creatinine, and thyroid function at baseline and periodically during treatment. In cases of suspected immune-mediated adverse reactions, initiate appropriate workup to exclude alternative etiologies, including infection. Institute medical management promptly, including specialty consultation as appropriate.
Withhold or permanently discontinue IMFINZI depending on severity [see Dosage and Administration (2.2)]. In general, if IMFINZI requires interruption or discontinuation, administer systemic corticosteroid therapy (1 mg to 2 mg/kg/day prednisone or equivalent) until improvement to Grade 1 or less. Upon improvement to Grade 1 or less, initiate corticosteroid taper and continue to taper over at least 1 month. Consider administration of other systemic immunosuppressants in patients whose immune-mediated adverse reactions are not controlled with corticosteroid therapy.
Toxicity management guidelines for adverse reactions that do not necessarily require systemic steroids (e.g., endocrinopathies and dermatologic reactions) are discussed below.
Immune-Mediated Pneumonitis
IMFINZI can cause immune-mediated pneumonitis. The incidence of pneumonitis is higher in patients who have received prior thoracic radiation.
IMFINZI as a Single Agent
In Patients Who did Not Receive Recent Prior Radiation
In patients who received IMFINZI on clinical trials in which radiation therapy was generally not administered immediately prior to initiation of IMFINZI, the incidence of immune-mediated pneumonitis was 2.4% (34/1414), including fatal (< 0.1%), and Grade 3-4 (0.4%) adverse reactions. Events resolved in 19 of the 34 patients and resulted in permanent discontinuation in 5 patients. Systemic corticosteroids were required in 19 patients (19/34) with pneumonitis who did not receive chemoradiation prior to initiation of IMFINZI.
In Patients Who Received Recent Prior Radiation
The incidence of pneumonitis (including radiation pneumonitis) in patients with unresectable Stage III NSCLC following definitive chemoradiation within 42 days prior to initiation of IMFINZI in PACIFIC was 18.3% (87/475) in patients receiving IMFINZI and 12.8% (30/234) in patients receiving placebo. Of the patients who received IMFINZI (475) 1.1% were fatal and 2.7% were Grade 3 adverse reactions. Events resolved in 50 of the 87 patients and resulted in permanent discontinuation in 27 patients.
Systemic corticosteroids were required in 64 patients (64/87) with pneumonitis who had received chemoradiation prior to initiation of IMFINZI, while 2 patients required use of infliximab with high-dose steroids.
The frequency and severity of immune-mediated pneumonitis in patients who did not receive definitive chemoradiation prior to IMFINZI were similar whether IMFINZI was given as a single agent in patients with various cancers in a pooled data set or in patients with ES-SCLC or BTC when given in combination with chemotherapy.
IMFINZI with Tremelimumab-actl
Immune-mediated pneumonitis occurred in 1.3% (5/388) of patients receiving IMFINZI in combination with tremelimumab-actl, including fatal (0.3%) and Grade 3 (0.2%) adverse reactions. Events resolved in 3 of the 5 patients and resulted in permanent discontinuation in 1 patient. Systemic corticosteroids were required in all patients; of these, 4 patients required high-dose corticosteroid treatment (at least 40 mg prednisone or equivalent per day). One patient (1/5) required other immunosuppressants.
IMFINZI with Tremelimumab-actl and Platinum-Based Chemotherapy
Immune-mediated pneumonitis occurred in 3.5% (21/596) of patients receiving IMFINZI in combination with tremelimumab-actl and platinum-based chemotherapy, including fatal (0.5%), and Grade 3 (1%) adverse reactions. Events resolved in 11 of the 21 patients and resulted in permanent discontinuation in 7 patients. Systemic corticosteroids were required in all patients with immune-mediated pneumonitis, while 1 patient (1/21) required other immunosuppressants.
Immune-Mediated Colitis
IMFINZI can cause immune-mediated colitis that is frequently associated with diarrhea. Cytomegalovirus (CMV) infection/reactivation has been reported in patients with corticosteroid-refractory immune-mediated colitis. In cases of corticosteroid-refractory colitis, consider repeating infectious workup to exclude alternative etiologies.
IMFINZI as a Single Agent
Immune-mediated colitis occurred in 2% (37/1889) of patients receiving IMFINZI, including Grade 4 (<0.1%) and Grade 3 (0.4%) adverse reactions. Events resolved in 27 of the 37 patients and resulted in permanent discontinuation in 8 patients. Systemic corticosteroids were required in all patients with immune-mediated colitis, while 2 patients (2/37) required other immunosuppressants (e.g., infliximab, mycophenolate).
IMFINZI with Tremelimumab-actl
Immune-mediated colitis or diarrhea occurred in 6% (23/388) of patients receiving IMFINZI in combination with tremelimumab-actl, including Grade 3 (3.6%) adverse reactions. Events resolved in 22 of the 23 patients and resulted in permanent discontinuation in 5 patients. All patients received systemic corticosteroids, and 20 of the 23 patients received high-dose corticosteroid treatment (at least 40 mg prednisone or equivalent per day). Three patients also received other immunosuppressants.
Intestinal perforation has been observed in other studies of IMFINZI in combination with tremelimumab-actl.
IMFINZI with Tremelimumab-actl and Platinum-Based Chemotherapy
Immune-mediated colitis occurred in 6.5% (39/596) of patients receiving IMFINZI in combination with tremelimumab-actl including fatal (0.2%) and Grade 3 (2.5%) adverse reactions. Events resolved in 33 of 39 patients and resulted in permanent discontinuation in 11 patients. Systemic corticosteroids were required in all patients with immune-mediated colitis, while 4 patients (4/39) required other corticosteroids.
Intestinal perforation and large intestine perforation were reported in 0.1% of patients receiving IMFINZI in combination with tremelimumab-actl.
Immune-Mediated Hepatitis
IMFINZI can cause immune-mediated hepatitis.
IMFINZI as a Single Agent
Immune-mediated hepatitis occurred in 2.8% (52/1889) of patients receiving IMFINZI, including fatal (0.2%), Grade 4 (0.3%) and Grade 3 (1.4%) adverse reactions. Events resolved in 21 of the 52 patients and resulted in permanent discontinuation of IMFINZI in 6 patients. Systemic corticosteroids were required in all patients with immune-mediated hepatitis, while 2 patients (2/52) required use of mycophenolate with high-dose steroids.
IMFINZI with Tremelimumab-actl
Immune-mediated hepatitis occurred in 7.5% (29/388) of patients receiving IMFINZI in combination with tremelimumab-actl, including fatal (0.8%), Grade 4 (0.3%), and Grade 3 (4.1%) adverse reactions. Events resolved in 12 of the 29 patients and resulted in permanent discontinuation in 9 patients. Systemic corticosteroids were required in all 29 patients and all 29 patients required high-dose corticosteroid treatment (at least 40 mg prednisone or equivalent per day). Eight patients (8/29) required other immunosuppressants.
IMFINZI with Tremelimumab-actl and Platinum-Based Chemotherapy
Immune-mediated hepatitis occurred in 3.9% (23/596) of patients receiving IMFINZI in combination with tremelimumab-actl, including fatal (0.3%), Grade 4 (0.5%), and Grade 3 (2.0%) adverse reactions. Events resolved in 12 of the 23 patients and resulted in permanent discontinuation in 10 patients. Systemic corticosteroids were required in all patients with immune-mediated hepatitis, while 2 patients (2/23) required use of other immunosuppressants.
Immune-Mediated Endocrinopathies
Adrenal Insufficiency
IMFINZI can cause primary or secondary adrenal insufficiency. For Grade 2 or higher adrenal insufficiency, initiate symptomatic treatment, including hormone replacement as clinically indicated. Withhold or permanently discontinue IMFINZI based on the severity [see Dosage and Administration (2.2)].
IMFINZI as a Single Agent
Immune-mediated adrenal insufficiency occurred in 0.5% (9/1889) of patients receiving IMFINZI, including Grade 3 (<0.1%) adverse reactions. Events resolved in 1 of the 9 patients and did not lead to permanent discontinuation of IMFINZI in any patients. Systemic corticosteroids were required in all patients with adrenal insufficiency; of these, the majority remained on systemic corticosteroids.
IMFINZI with Tremelimumab-actl
Immune-mediated adrenal insufficiency occurred in 1.5% (6/388) of patients receiving IMFINZI in combination with tremelimumab-actl, including Grade 3 (0.3%) adverse reactions. Events resolved in 2 of the 6 patients. Systemic corticosteroids were required in all 6 patients, and of these, 1 patient required high-dose corticosteroid treatment (at least 40 mg prednisone or equivalent per day).
IMFINZI with Tremelimumab-actl and Platinum-Based Chemotherapy
Immune-mediated adrenal insufficiency occurred in 2.2% (13/596) of patients receiving IMFINZI in combination with tremelimumab-actl, including Grade 3 (0.8%) adverse reactions. Events resolved in 2 of the 13 patients and resulted in permanent discontinuation in 1 patient. Systemic corticosteroids were required in all patients with adrenal insufficiency. One patient also required endocrine therapy.
Hypophysitis
IMFINZI can cause immune-mediated hypophysitis. Hypophysitis can present with acute symptoms associated with mass effect such as headache, photophobia, or visual field cuts. Hypophysitis can cause hypopituitarism. Initiate symptomatic treatment including hormone replacement as clinically indicated. Withhold or permanently discontinue IMFINZI depending on severity [see Dosage and Administration (2.2)].
IMFINZI as a Single Agent
Grade 3 hypophysitis/hypopituitarism occurred in <0.1% (1/1889) of patients who received IMFINZI. Treatment with systemic corticosteroids was administered in this patient. The event did not lead to permanent discontinuation of IMFINZI.
IMFINZI with Tremelimumab-actl
Immune-mediated hypophysitis/hypopituitarism occurred in 1% (4/388) of patients receiving IMFINZI in combination with tremelimumab-actl. Events resolved in 2 of the 4 patients. Systemic corticosteroids were required in 3 patients, and of these, 1 patient received high-dose corticosteroid treatment (at least 40 mg prednisone or equivalent per day). Two patients also required endocrine therapy.
IMFINZI with Tremelimumab-actl and Platinum-Based Chemotherapy
Immune-mediated hypophysitis occurred in 1.3% (8/596) of patients receiving IMFINZI in combination with tremelimumab-actl, including Grade 3 (0.5%) adverse reactions. Events resulted in permanent discontinuation in 1 patient. Systemic corticosteroids were required in 6 patients with immune-mediated hypophysitis; of these, 2 of the 8 patients received high-dose corticosteroid treatment (at least 40 mg prednisone or equivalent per day). Four patients also required endocrine therapy.
Thyroid Disorders
IMFINZI can cause immune-mediated thyroid disorders. Thyroiditis can present with or without endocrinopathy. Hypothyroidism can follow hyperthyroidism. Initiate hormone replacement therapy for hypothyroidism or institute medical management of hyperthyroidism as clinically indicated. Withhold or discontinue IMFINZI based on the severity [see Dosage and Administration (2.2)].
Thyroiditis
IMFINZI as a Single Agent
Immune-mediated thyroiditis occurred in 0.5% (9/1889) of patients receiving IMFINZI, including Grade 3 (<0.1%) adverse reactions. Events resolved in 4 of the 9 patients and resulted in permanent discontinuation in 1 patient. Systemic corticosteroids were required in 3 patients (3/9) with immune-mediated thyroiditis, while 8 patients (8/9) required endocrine therapy.
IMFINZI with Tremelimumab-actl
Immune-mediated thyroiditis occurred in 1.5% (6/388) of patients receiving IMFINZI in combination with tremelimumab-actl. Events resolved in 2 of the 6 patients. Systemic corticosteroids were required in 2 patients (2/6) with immune-mediated thyroiditis; of these, 1 patient required high-dose corticosteroid treatment (at least 40 mg prednisone or equivalent per day). All patients required other therapy including hormone replacement therapy, thiamazole, carbimazole, propylthiouracil, perchlorate, calcium channel blocker, or beta-blocker.
IMFINZI with Tremelimumab-actl and Platinum-Based Chemotherapy
Immune-mediated thyroiditis occurred in 1.2% (7/596) of patients receiving IMFINZI in combination with tremelimumab-actl. Events resolved in 2 of the 7 patients and one resulted in permanent discontinuation. Systemic corticosteroids were required in 2 patients (2/7) with immune-mediated thyroiditis, while all patients required endocrine therapy.
Hyperthyroidism
IMFINZI as a Single Agent
Immune-mediated hyperthyroidism occurred in 2.1% (39/1889) of patients receiving IMFINZI. Events resolved in 30 of the 39 patients and did not lead to permanent discontinuation of IMFINZI in any patients. Systemic corticosteroids were required in 9 patients (9/39) with immune-mediated hyperthyroidism, while 35 patients (35/39) required endocrine therapy.
IMFINZI with Tremelimumab-actl
Immune-mediated hyperthyroidism occurred in 4.6% (18/388) of patients receiving IMFINZI in combination with tremelimumab-actl, including Grade 3 (0.3%) adverse reactions. Events resolved in 15 of the 18 patients. Two patients (2/18) required high-dose corticosteroid treatment (at least 40 mg prednisone or equivalent per day). Seventeen patients required other therapy (thiamazole, carbimazole, propylthiouracil, perchlorate, calcium channel blocker, or beta-blocker).
IMFINZI with Tremelimumab-actl and Platinum-Based Chemotherapy
Immune-mediated hyperthyroidism occurred in 5% (30/596) of patients receiving IMFINZI in combination with tremelimumab-actl, including Grade 3 (0.2%) adverse reactions. Events resolved in 21 of the 30 patients. Systemic corticosteroids were required in 5 patients (5/30) with immune-mediated hyperthyroidism, while 28 patients (28/30) required endocrine therapy.
Hypothyroidism
IMFINZI as a Single Agent
Immune-mediated hypothyroidism occurred in 8.3% (156/1889) of patients receiving IMFINZI, including Grade 3 (<0.1%) adverse reactions. Events resolved in 31 of the 156 patients and did not lead to permanent discontinuation of IMFINZI in any patients. Systemic corticosteroids were required in 11 patients (11/156) and the majority of patients (152/156) required long-term thyroid hormone replacement.
IMFINZI with Tremelimumab-actl
Immune-mediated hypothyroidism occurred in 11% (42/388) of patients receiving IMFINZI in combination with tremelimumab-actl. Events resolved in 5 of the 42 patients. One patient received high-dose corticosteroid treatment (at least 40 mg prednisone or equivalent per day). All patients required other therapy (thiamazole, carbimazole, propylthiouracil, perchlorate, calcium channel blocker, or beta-blocker).
IMFINZI with Tremelimumab-actl and Platinum-Based Chemotherapy
Immune-mediated hypothyroidism occurred in 8.6% (51/596) of patients receiving IMFINZI in combination with tremelimumab-actl, including Grade 3 (0.5%) adverse reactions. Systemic corticosteroids were required in 2 patients (2/51) and all patients required endocrine therapy.
Type 1 Diabetes Mellitus, which can present with diabetic ketoacidosis
Monitor patients for hyperglycemia or other signs and symptoms of diabetes. Initiate treatment with insulin as clinically indicated. Withhold or permanently discontinue IMFINZI based on the severity [see Dosage and Administration (2.2)].
IMFINZI as a Single Agent
Grade 3 immune-mediated type 1 diabetes mellitus occurred in < 0.1% (1/1889) of patients receiving IMFINZI. This patient required long-term insulin therapy and IMFINZI was permanently discontinued. Two additional patients (0.1%, 2/1889) had events of hyperglycemia requiring insulin therapy that did not resolve at the time of reporting.
IMFINZI with Tremelimumab-actl
Two patients (0.5%, 2/388) had events of hyperglycemia requiring insulin therapy that had not resolved at last follow-up.
IMFINZI with Tremelimumab-actl and Platinum-Based Chemotherapy
Immune-mediated Type 1 diabetes mellitus occurred in 0.5% (3/596) of patients receiving IMFINZI in combination with tremelimumab-actl, including Grade 3 (0.3%) adverse reactions. All patients required endocrine therapy.
Immune-Mediated Nephritis with Renal Dysfunction
IMFINZI can cause immune-mediated nephritis.
IMFINZI as a Single Agent
Immune-mediated nephritis occurred in 0.5% (10/1889) of patients receiving IMFINZI, including Grade 3 (< 0.1%) adverse reactions. Events resolved in 5 of the 10 patients and resulted in permanent discontinuation in 3 patients. Systemic corticosteroids were required in all patients with immune-mediated nephritis.
IMFINZI with Tremelimumab-actl
Immune-mediated nephritis occurred in 1% (4/388) of patients receiving IMFINZI in combination with tremelimumab-actl, including Grade 3 (0.5%) adverse reactions. Events resolved in 3 of the 4 patients and resulted in permanent discontinuation in 2 patients. Systemic corticosteroids were required in all patients with immune-mediated nephritis; of these, 3 patients required high-dose corticosteroid treatment (at least 40 mg prednisone or equivalent per day).
IMFINZI with Tremelimumab-actl and Platinum-Based Chemotherapy
Immune-mediated nephritis occurred in 0.7% (4/596) of patients receiving IMFINZI in combination with tremelimumab-actl, including Grade 3 (0.2%) adverse reactions. Events resolved in 1 of the 4 patients and resulted in permanent discontinuation in 3 patients. Systemic corticosteroids were required in all patients with immune-mediated nephritis.
Immune-Mediated Dermatology Reactions
IMFINZI can cause immune-mediated rash or dermatitis. Exfoliative dermatitis, including Stevens Johnson Syndrome (SJS), drug rash with eosinophilia and systemic symptoms (DRESS), and toxic epidermal necrolysis (TEN), has occurred with PD-1/L-1 blocking antibodies. Topical emollients and/or topical corticosteroids may be adequate to treat mild to moderate non-exfoliative rashes. Withhold or permanently discontinue IMFINZI depending on severity [see Dosage and Administration (2.2)].
IMFINZI as a Single Agent
Immune-mediated rash or dermatitis occurred in 1.8% (34/1889) of patients receiving IMFINZI, including Grade 3 (0.4%) adverse reactions. Events resolved in 19 of the 34 patients and resulted in permanent discontinuation in 2 patients. Systemic corticosteroids were required in all patients with immune-mediated rash or dermatitis.
IMFINZI with Tremelimumab-actl
Immune-mediated rash or dermatitis occurred in 4.9% (19/388) of patients receiving IMFINZI in combination with tremelimumab-actl, including Grade 4 (0.3%) and Grade 3 (1.5%) adverse reactions. Events resolved in 13 of the 19 patients and resulted in permanent discontinuation in 2 patients. Systemic corticosteroids were required in all patients with immune-mediated rash or dermatitis; of these, 12 patients required high-dose corticosteroid treatment (at least 40 mg prednisone or equivalent per day). One patient received other immunosuppressants.
IMFINZI with Tremelimumab-actl and Platinum-Based Chemotherapy
Immune-mediated rash or dermatitis occurred in 7.2% (43/596) of patients receiving IMFINZI in combination with tremelimumab-actl, including Grade 3 (0.3%) adverse reactions. Events resolved in 32 of the 43 patients and resulted in permanent discontinuation in 2 patients. Systemic corticosteroids were required in all patients with immune-mediated rash or dermatitis.
Immune-Mediated Pancreatitis
IMFINZI in combination with tremelimumab-actl can cause immune-mediated pancreatitis.
IMFINZI with Tremelimumab-actl
Immune-mediated pancreatitis occurred in 2.3% (9/388) of patients receiving IMFINZI in combination with tremelimumab-actl, including Grade 4 (0.3%) and Grade 3 (1.5%) adverse reactions. Events resolved in 6 of the 9 patients. Systemic corticosteroids were required in all 9 patients and of these 7 patients required high-dose corticosteroid treatment (at least 40 mg prednisone or equivalent per day).
Other Immune-Mediated Adverse Reactions
The following clinically significant, immune-mediated adverse reactions occurred at an incidence of less than 1% each in patients who received IMFINZI or IMFINZI in combination with tremelimumab-actl, or were reported with the use of other PD-1/PD-L1 blocking antibodies.
Cardiac/vascular: Myocarditis, pericarditis, vasculitis.
Nervous system: Meningitis, encephalitis, myelitis and demyelination, myasthenic syndrome/myasthenia gravis (including exacerbation), Guillain-Barré syndrome, nerve paresis, autoimmune neuropathy.
Ocular: Uveitis, iritis, and other ocular inflammatory toxicities can occur. Some cases can be associated with retinal detachment. Various grades of visual impairment to include blindness can occur. If uveitis occurs in combination with other immune-mediated adverse reactions, consider a Vogt-Koyanagi-Harada-like syndrome, as this may require treatment with systemic steroids to reduce the risk of permanent vision loss.
Gastrointestinal: Pancreatitis including increases in serum amylase and lipase levels, gastritis, duodenitis.
Musculoskeletal and connective tissue disorders: Myositis/polymyositis, rhabdomyolysis and associated sequelae including renal failure, arthritis, polymyalgia rheumatic.
Endocrine: Hypoparathyroidism.
Other (hematologic/immune): Hemolytic anemia, aplastic anemia, hemophagocytic lymphohistiocytosis, systemic inflammatory response syndrome, histiocytic necrotizing lymphadenitis (Kikuchi lymphadenitis), sarcoidosis, immune thrombocytopenia, solid organ transplant rejection.
5.2 Infusion-Related Reactions
IMFINZI can cause severe or life-threatening infusion-related reactions.
Monitor for signs and symptoms of infusion-related reactions. Interrupt, slow the rate of, or permanently discontinue IMFINZI based on the severity [see Dosage and Administration (2.2)]. For Grade 1 or 2 infusion-related reactions, consider using pre-medications with subsequent doses.
IMFINZI as a Single Agent
Infusion-related reactions occurred in 2.2% (42/1889) of patients receiving IMFINZI, including Grade 3 (0.3%) adverse reactions.
IMFINZI in Combination with Tremelimumab-actl
Infusion-related reactions occurred in 10 (2.6%) patients receiving IMFINZI in combination with tremelimumab-actl.
IMFINZI with Tremelimumab-actl and Platinum-Based Chemotherapy
Infusion-related reactions occurred in 2.9% (17/596) of patients receiving IMFINZI in combination with tremelimumab-actl, including Grade 3 (0.3%) adverse reactions.
5.3 Complications of Allogeneic HSCT after IMFINZI
Fatal and other serious complications can occur in patients who receive allogeneic hematopoietic stem cell transplantation (HSCT) before or after being treated with a PD-1/L-1 blocking antibody. Transplant-related complications include hyperacute graft-versus-host-disease (GVHD), acute GVHD, chronic GVHD, hepatic veno-occlusive disease (VOD) after reduced intensity conditioning, and steroid-requiring febrile syndrome (without an identified infectious cause). These complications may occur despite intervening therapy between PD-1/L-1 blockade and allogeneic HSCT.
Follow patients closely for evidence of transplant-related complications and intervene promptly. Consider the benefit versus risks of treatment with a PD-1/L-1 blocking antibody prior to or after an allogeneic HSCT.
5.4 Embryo-Fetal Toxicity
Based on its mechanism of action and data from animal studies, IMFINZI can cause fetal harm when administered to a pregnant woman. In animal reproduction studies, administration of durvalumab to cynomolgus monkeys from the onset of organogenesis through delivery resulted in increased premature delivery, fetal loss and premature neonatal death. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with IMFINZI and for 3 months after the last dose of IMFINZI [see Use in Specific Populations (8.1, 8.3)].
6. Adverse Reactions/Side Effects
The following adverse reactions are discussed in greater detail in other sections of the labeling.
- •
- Immune-Mediated Adverse Reactions [see Warnings and Precautions (5.1)].
- •
- Infusion-Related Reactions [see Warnings and Precautions (5.2)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
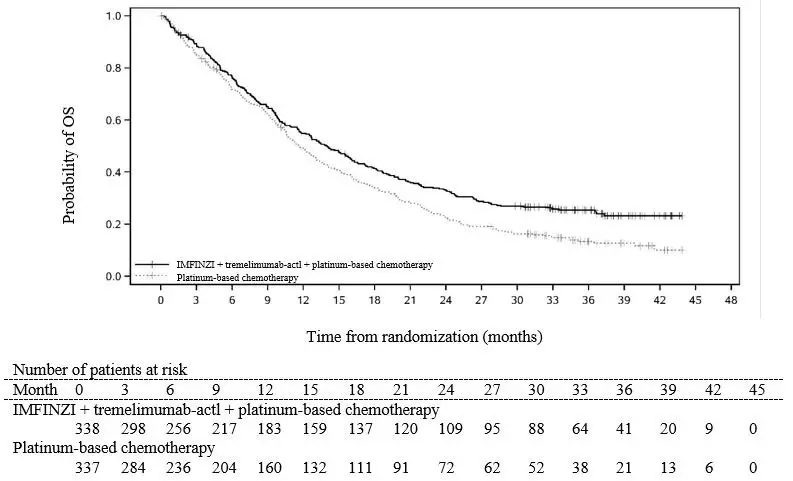
The data described in the Warnings and Precautions section reflect exposure to IMFINZI as a single agent in a total of 1889 patients enrolled in the PACIFIC study (a randomized, placebo-controlled study that enrolled 475 patients with Stage III NSCLC), Study 1108 (an open-label, single-arm, multicohort study that enrolled 970 patients with advanced solid tumors), and an additional open-label, single-arm trial (ATLANTIC Study) that enrolled 444 patients with advanced solid tumors, including NSCLC. In these trials, IMFINZI was administered at a dose of 10 mg/kg every 2 weeks. Among the 1889 patients, 38% were exposed for 6 months or more and 18% were exposed for 12 months or more. The data also reflect exposure to IMFINZI in combination with chemotherapy in 265 patients from the CASPIAN study (a randomized, open-label study in patients with ES-SCLC), in 338 patients from the TOPAZ-1 study (a randomized, double-blind study in patients with BTC). In the CASPIAN and TOPAZ-1 studies, IMFINZI was administered at a dose of 1,500 mg every 3 or 4 weeks.
The data described in the Warnings and Precautions also reflect exposure to IMFINZI 1,500 mg in combination with tremelimumab-actl 300 mg in 388 patients in HIMALAYA. In the HIMALAYA study patients received IMFINZI 1,500 mg in combination with tremelimumab-actl as a single intravenous infusion of 300 mg, followed by IMFINZI 1,500 mg every 4 weeks. The pooled safety population (N = 596) described in the Warnings and Precautions section reflect exposure to IMFINZI 1,500 mg in combination with tremelimumab-actl 75 mg and histology-based platinum chemotherapy regimens in 330 patients in POSEIDON [see Clinical Studies (14.1)] and 266 patients with ES-SCLC in CASPIAN who received up to four cycles of platinum-etoposide plus IMFINZI 1,500 mg with tremelimumab-actl 75 mg every 3 weeks followed by IMFINZI 1,500 mg every 4 weeks (an unapproved regimen for extensive stage small cell lung cancer). Among the 596 patients, 55% were exposed to IMFINZI for 6 months or more and 24% were exposed for 12 months or more.
The data described in this section reflect exposure to IMFINZI in patients with Stage III NSCLC enrolled in the PACIFIC study, in patients with metastatic NSCLC enrolled in the POSEIDON study, in patients with ES-SCLC enrolled in the CASPIAN study, in patients with BTC enrolled in the TOPAZ-1 study and in patients with uHCC included in the HIMALAYA study.
Non-Small Cell Lung Cancer
Stage III NSCLC - PACIFIC
The safety of IMFINZI in patients with Stage III NSCLC who completed concurrent platinum-based chemoradiotherapy within 42 days prior to initiation of study drug was evaluated in the PACIFIC study, a multicenter, randomized, double-blind, placebo-controlled study. A total of 475 patients received IMFINZI 10 mg/kg intravenously every 2 weeks. The study excluded patients who had disease progression following chemoradiation, with active or prior autoimmune disease within 2 years of initiation of the study or with medical conditions that required systemic immunosuppression [see Clinical Studies (14.1)].
The study population characteristics were: median age of 64 years (range: 23 to 90), 45% age 65 years or older, 70% male, 69% White, 27% Asian, 75% former smoker, 16% current smoker, and 51% had WHO performance status of 1. All patients received definitive radiotherapy as per protocol, of which 92% received a total radiation dose of 54 Gy to 66 Gy. The median duration of exposure to IMFINZI was 10 months (range: 0.2 to 12.6).
IMFINZI was discontinued due to adverse reactions in 15% of patients. The most common adverse reactions leading to IMFINZI discontinuation were pneumonitis or radiation pneumonitis in 6% of patients. Serious adverse reactions occurred in 29% of patients receiving IMFINZI. The most frequent serious adverse reactions reported in at least 2% of patients were pneumonitis or radiation pneumonitis (7%) and pneumonia (6%). Fatal pneumonitis or radiation pneumonitis and fatal pneumonia occurred in < 2% of patients and were similar across arms. The most common adverse reactions (occurring in ≥ 20% of patients) were cough, fatigue, pneumonitis or radiation pneumonitis, upper respiratory tract infections, dyspnea, and rash. Table 5 summarizes the adverse reactions that occurred in at least 10% of patients treated with IMFINZI.
| IMFINZI
N = 475 | Placebo
N = 234 |
||||
|---|---|---|---|---|---|
| Adverse Reaction | All Grades
(%) | Grades 3-4 (%) | All Grades
(%) | Grades 3-4 (%) | |
|
|||||
|
Respiratory, Thoracic, and Mediastinal Disorders |
|||||
|
Cough/Productive Cough |
40 |
0.6 |
30 |
0.4 |
|
|
Pneumonitis* /Radiation Pneumonitis |
34 |
3.4 |
25 |
3 |
|
|
Dyspnea† |
25 |
1.5 |
25 |
2.6 |
|
|
Gastrointestinal Disorders |
|||||
|
Diarrhea |
18 |
0.6 |
19 |
1.3 |
|
|
Abdominal pain‡ |
10 |
0.4 |
6 |
0.4 |
|
|
Endocrine Disorders |
|||||
|
Hypothyroidism§ |
12 |
0.2 |
1.7 |
0 |
|
|
Skin and Subcutaneous Tissue Disorders |
|||||
|
Rash¶ |
23 |
0.6 |
12 |
0 |
|
|
Pruritus# |
12 |
0 |
6 |
0 |
|
|
General Disorders |
|||||
|
FatigueÞ |
34 |
0.8 |
32 |
1.3 |
|
|
Pyrexia |
15 |
0.2 |
9 |
0 |
|
|
Infections |
|||||
|
Upper respiratory tract infectionsß |
26 |
0.4 |
19 |
0 |
|
|
Pneumoniaà |
17 |
7 |
12 |
6 |
|
Other adverse reactions occurring in less than 10% of patients treated with IMFINZI were dysphonia, dysuria, night sweats, peripheral edema, and increased susceptibility to infections.
Table 6 summarizes the laboratory abnormalities that occurred in at least 20% of patients treated with IMFINZI.
|
||||
|
IMFINZI |
Placebo |
|||
|
Laboratory Abnormality |
All Grades* (%)† |
Grade 3 or 4 (%) |
All Grades* (%)† |
Grade 3 or 4 (%) |
|
Chemistry |
||||
|
Hyperglycemia |
52 |
8 |
51 |
8 |
|
Hypocalcemia |
46 |
0.2 |
41 |
0 |
|
Increased ALT |
39 |
2.3 |
22 |
0.4 |
|
Increased AST |
36 |
2.8 |
21 |
0.4 |
|
Hyponatremia |
33 |
3.6 |
30 |
3.1 |
|
Hyperkalemia |
32 |
1.1 |
29 |
1.8 |
|
Increased GGT |
24 |
3.4 |
22 |
1.7 |
|
Hematology |
||||
|
Lymphopenia |
43 |
17 |
39 |
18 |
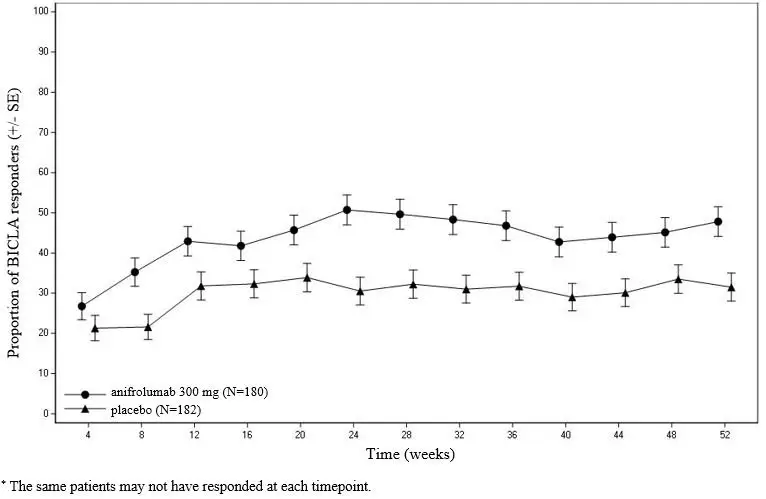
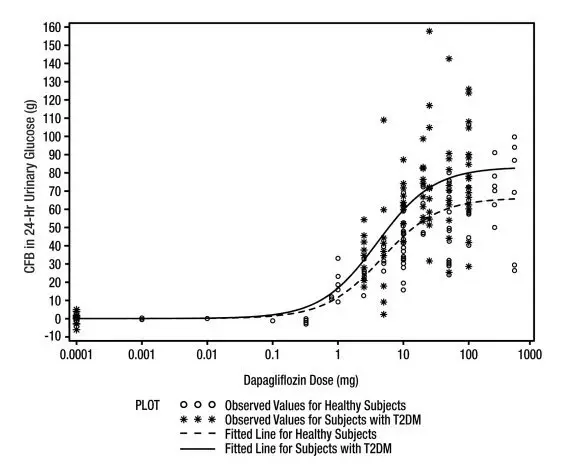
Metastatic NSCLC - POSEIDON
The safety of IMFINZI in combination with tremelimumab-actl and platinum-based chemotherapy in patients with metastatic NSCLC was evaluated in POSEIDON (NCT03164616), a randomized, open-label, multicenter, active-controlled trial. A total of 330 patients received IMFINZI 1,500 mg in combination with tremelimumab-actl (≥ 30 kg body weight received 75 mg and < 30 kg body weight received 1 mg/kg) and histology-based platinum chemotherapy regimens [see Clinical Studies (14.1)]. Of these patients, 66% received the maximum 5 doses of tremelimumab-actl and 79% received at least 4 doses. Treatment was continued with IMFINZI as a single agent (or with IMFINZI and histologically-based pemetrexed for non-squamous patients based on the investigator’s decision) until disease progression or unacceptable toxicity. The trial excluded patients with active or prior autoimmune disease or with medical conditions that required systemic corticosteroids or immunosuppressants [see Clinical Studies (14.1)].
The median age of patients who received IMFINZI in combination with tremelimumab-actl and platinum-based chemotherapy was 63 years (range: 27 to 87); 80% male; 61% White, 29% Asian, 58% former smoker, 25% current smoker, and 68% ECOG performance of 1.
Serious adverse reactions occurred in 44% of patients receiving IMFINZI in combination with tremelimumab-actl and platinum-based chemotherapy. The most frequent serious adverse reactions reported in at least 2% of patients were pneumonia (11%), anemia (5%), diarrhea (2.4%), thrombocytopenia (2.4%), pyrexia (2.4%), and febrile neutropenia (2.1%). Fatal adverse reactions occurred in a total of 4.2% of patients receiving IMFINZI in combination with tremelimumab-actl and platinum-based chemotherapy. These include hepatitis, nephritis, myocarditis, pancreatitis (all in the same patient), death (2 patients), sepsis (2 patients), pneumonitis (2 patients), acute kidney injury (2 patients), febrile neutropenia (1 patient), chronic obstructive pulmonary disease (1 patient), dyspnea (1 patient), sudden death (1 patient), and ischemic stroke (1 patient).
Permanent discontinuation of IMFINZI or tremelimumab-actl due to an adverse reaction occurred in 17% of the patients. Adverse reactions which resulted in permanent discontinuation of IMFINZI or tremelimumab-actl in > 2% of patients included pneumonia.
Dosage interruption or delay of IMFINZI and tremelimumab-actl due to an adverse reaction occurred in 41% of patients. Adverse reactions which required dosage interruption or delay of IMFINZI and tremelimumab-actl in > 1% of patients included anemia, leukopenia/white blood cell count decreased, pneumonia, pneumonitis, colitis, diarrhea, hepatitis, rash, asthenia, amylase increased, alanine aminotransferase increased, aspartate aminotransferase increased, lipase increased, neutropenia/ neutrophil count decreased, and thrombocytopenia/platelet count decreased.
The most common adverse reactions (occurring in ≥ 20% of patients) were nausea, fatigue, musculoskeletal pain, decreased appetite, rash, and diarrhea. Grade 3 or 4 laboratory abnormalities (≥ 10%) were neutropenia, anemia, leukopenia, lymphocytopenia, lipase increased, hyponatremia and thrombocytopenia.
Table 7 summarizes the adverse reactions in POSEIDON.
| IMFINZI with tremelimumab-actl and platinum-based chemotherapy
N = 330 | Platinum-based chemotherapy
N = 333 |
|||
|---|---|---|---|---|
| Adverse Reaction | All Grades (%) | Grade 3 or 4 (%) | All Grades (%) | Grade 3 or 4 (%) |
|
||||
|
Respiratory, thoracic and mediastinal disorders |
||||
|
Cough/Productive Cough* |
12 |
0 |
8 |
0.3 |
|
Gastrointestinal disorders |
||||
|
Nausea |
42 |
1.8 |
37 |
2.1 |
|
Diarrhea |
22 |
1.5 |
15 |
1.5 |
|
Constipation |
19 |
0 |
24 |
0.6 |
|
Vomiting |
18 |
1.2 |
14 |
1.5 |
|
Stomatitis† |
10 |
0 |
6 |
0.3 |
|
Endocrine disorders |
||||
|
Hypothyroidism‡ |
13 |
0 |
2.1 |
0 |
|
Skin and subcutaneous tissue disorders |
||||
|
Rash§ |
27 |
2.4 |
10 |
0.6 |
|
Alopecia |
10 |
0 |
6 |
0 |
|
Pruritus |
11 |
0 |
4.5 |
0 |
|
General disorders and administration site conditions |
||||
|
Fatigue/Asthenia¶ |
36 |
5 |
32 |
4.5 |
|
Pyrexia# |
19 |
0 |
8 |
0 |
|
EdemaÞ |
10 |
0 |
10 |
0.6 |
|
Musculoskeletal and connective tissue disorders |
||||
|
Musculoskeletal Painß |
29 |
0.6 |
22 |
1.5 |
|
Metabolism and nutrition disorders |
||||
|
Decreased appetite |
28 |
1.5 |
25 |
1.2 |
|
Infections and Infestations |
||||
|
Pneumoniaà |
17 |
8 |
12 |
4.2 |
|
Upper respiratory tract infectionsè |
15 |
0.6 |
9 |
0.9 |
|
Nervous system disorders |
||||
|
Headacheð |
11 |
0 |
8 |
0.6 |
Table 8 summarizes the laboratory abnormalities in POSEIDON.
| Laboratory Abnormality* | IMFINZI with tremelimumab-actl and platinum-based chemotherapy† | Platinum-based chemotherapy‡ | ||
|---|---|---|---|---|
| All Grades
(%) | Grade 3 or 4
(%) | All Grades
(%) | Grade 3 or 4
(%) |
|
|
||||
|
Chemistry | ||||
|
Lipase increased |
35 |
14 |
25 |
5 |
|
Hyponatremia |
55 |
13 |
50 |
11 |
|
Hypernatremia |
15 |
0 |
14 |
0 |
|
Amylase increased |
41 |
9 |
25 |
6 |
|
Hypokalemia |
21 |
7 |
17 |
2.8 |
|
Hyperglycemia |
42 |
6 |
37 |
3.1 |
|
Increased ALT |
64 |
6 |
56 |
4.7 |
|
Increased AST |
63 |
5 |
55 |
2.2 |
|
Blood creatinine increased |
89 |
4.0 |
83 |
1.9 |
|
Increased Alkaline Phosphatase |
33 |
3.4 |
26 |
1.2 |
|
Gamma Glutamyl Transferase increased |
38 |
2.2 |
35 |
4.7 |
|
Hyperkalemia |
49 |
2.2 |
35 |
2.8 |
|
Albumin decreased |
27 |
1.9 |
18 |
0.9 |
|
Hypocalcemia |
58 |
0.9 |
49 |
0.9 |
|
Hypomagnesemia |
12 |
4 |
23 |
0 |
|
Bilirubinemia |
16 |
0.9 |
8 |
0.3 |
|
Hematology | ||||
|
Neutropenia |
71 |
37 |
69 |
32 |
|
Anemia |
84 |
24 |
84 |
25 |
|
Leukopenia |
77 |
21 |
81 |
18 |
|
Lymphocytopenia |
67 |
20 |
60 |
19 |
|
Thrombocytopenia |
53 |
11 |
54 |
12 |
Small Cell Lung Cancer
Extensive Stage Small Cell Lung Cancer – CASPIAN
The safety of IMFINZI in combination with etoposide and either carboplatin or cisplatin in previously untreated ES-SCLC was evaluated in CASPIAN, a randomized, open-label, multicenter, active-controlled trial. A total of 265 patients received IMFINZI 1,500 mg in combination with chemotherapy every 3 weeks for 4 cycles followed by IMFINZI 1,500 mg every 4 weeks until disease progression or unacceptable toxicity. The trial excluded patients with active or prior autoimmune disease or with medical conditions that required systemic corticosteroids or immunosuppressants [see Clinical Studies (14.2)]. Among 265 patients receiving IMFINZI, 49% were exposed for 6 months or longer and 19% were exposed for 12 months or longer.
Among 266 patients receiving chemotherapy alone, 57% of the patients received 6 cycles of chemotherapy and 8% of the patients received prophylactic cranial irradiation (PCI) after chemotherapy.
IMFINZI was discontinued due to adverse reactions in 7% of the patients receiving IMFINZI plus chemotherapy. These include pneumonitis, hepatotoxicity, neurotoxicity, sepsis, diabetic ketoacidosis and pancytopenia (1 patient each). Serious adverse reactions occurred in 31% of patients receiving IMFINZI plus chemotherapy. The most frequent serious adverse reactions reported in at least 1% of patients were febrile neutropenia (4.5%), pneumonia (2.3%), anemia (1.9%), pancytopenia (1.5%), pneumonitis (1.1%) and COPD (1.1%). Fatal adverse reactions occurred in 4.9% of patients receiving IMFINZI plus chemotherapy. These include pancytopenia, sepsis, septic shock, pulmonary artery thrombosis, pulmonary embolism, and hepatitis (1 patient each) and sudden death (2 patients). The most common adverse reactions (occurring in ≥ 20% of patients) were nausea, fatigue/asthenia and alopecia.
Table 9 summarizes the adverse reactions that occurred in patients treated with IMFINZI plus chemotherapy.
| IMFINZI with etoposide and either carboplatin or cisplatin
N = 265 | Etoposide and either carboplatin or cisplatin
N = 266 |
|||
|---|---|---|---|---|
| Adverse Reaction | All Grades (%) | Grade 3-4 (%) | All Grades (%) | Grade 3-4 (%) |
|
||||
|
Respiratory, thoracic and mediastinal disorders |
||||
|
Cough/Productive Cough |
15 |
0.8 |
9 |
0 |
|
Gastrointestinal disorders |
||||
|
Nausea |
34 |
0.4 |
34 |
1.9 |
|
Constipation |
17 |
0.8 |
19 |
0 |
|
Vomiting |
15 |
0 |
17 |
1.1 |
|
Diarrhea |
10 |
1.1 |
11 |
1.1 |
|
Endocrine disorders |
||||
|
Hyperthyroidism* |
10 |
0 |
0.4 |
0 |
|
Skin and subcutaneous tissue disorders |
||||
|
Alopecia |
31 |
1.1 |
34 |
0.8 |
|
Rash† |
11 |
0 |
6 |
0 |
|
General disorders and administration site conditions |
||||
|
Fatigue/Asthenia |
32 |
3.4 |
32 |
2.3 |
|
Metabolism and nutrition disorders |
||||
|
Decreased appetite |
18 |
0.8 |
17 |
0.8 |
Table 10 summarizes the laboratory abnormalities that occurred in at least 20% of patients treated with IMFINZI plus chemotherapy.
|
||
|
IMFINZI with Etoposide and either Carboplatin or Cisplatin |
Etoposide and either Carboplatin or Cisplatin |
|
|
Laboratory Abnormality |
Grade† 3 or 4 (%)‡ |
Grade†3 or 4 (%)‡ |
|
Chemistry |
||
|
Hyponatremia |
11 |
13 |
|
Hypomagnesemia |
11 |
6 |
|
Hyperglycemia |
5 |
5 |
|
Increased Alkaline Phosphatase |
4.9 |
3.5 |
|
Increased ALT |
4.9 |
2.7 |
|
Increased AST |
4.6 |
1.2 |
|
Hypocalcemia |
3.5 |
2.4 |
|
Blood creatinine increased |
3.4 |
1.1 |
|
Hyperkalemia |
1.5 |
3.1 |
|
TSH decreased < LLN§ and ≥ LLN at baseline |
NA |
NA |
|
Hematology |
||
|
Neutropenia |
41 |
48 |
|
Lymphopenia |
14 |
13 |
|
Anemia |
13 |
22 |
|
Thrombocytopenia |
12 |
15 |
Biliary Tract Cancer
Locally advanced or metastatic BTC - TOPAZ-1
The safety of IMFINZI in combination with gemcitabine and cisplatin in locally advanced or metastatic BTC was evaluated in TOPAZ-1, a randomized, double-blind, placebo-controlled, multicenter trial. A total of 338 patients received IMFINZI 1,500 mg in combination with gemcitabine and cisplatin every 3 weeks up to 8 cycles followed by IMFINZI 1,500 mg every 4 weeks until disease progression or unacceptable toxicity. Patients with active or prior documented autoimmune or inflammatory disorders, HIV infection or other active infections, including tuberculosis or hepatitis C were ineligible [see Clinical Studies (14.3)].
IMFINZI was discontinued due to adverse reactions in 6% of the patients receiving IMFINZI plus chemotherapy. The most frequently reported events resulting in discontinuation were sepsis (3 patients) and ischemic stroke (2 patients). The remaining events were dispersed across system organ classes and reported in 1 patient each. Serious adverse reactions occurred in 47% of patients receiving IMFINZI plus chemotherapy. The most frequent serious adverse reactions reported in at least 2% of patients were cholangitis (7%), pyrexia (3.8%), anemia (3.6%), sepsis (3.3%) and acute kidney injury (2.4%). Fatal adverse reactions occurred in 3.6% of patients receiving IMFINZI plus chemotherapy. These include ischemic or hemorrhagic stroke (4 patients), sepsis (2 patients) and upper gastrointestinal hemorrhage (2 patients). The most common adverse reactions (occurring in ≥ 20% of patients) were fatigue, nausea, constipation, decreased appetite, abdominal pain, rash and pyrexia. Table 11 summarizes the adverse reactions that occurred in patients treated with IMFINZI plus chemotherapy.
|
||||
|
IMFINZI with Gemcitabine and Cisplatin N = 338 |
Placebo with Gemcitabine and Cisplatin N = 342 |
|||
|
Adverse Reaction |
All Grades* (%) |
Grade* 3-4 (%) |
All Grades* (%) |
Grade* 3-4 (%) |
|
General disorders and administration site conditions |
||||
|
Fatigue† |
42 |
6 |
43 |
6 |
|
Pyrexia |
20 |
1.5 |
16 |
0.6 |
|
Gastrointestinal disorders |
||||
|
Nausea |
40 |
1.5 |
34 |
1.8 |
|
Constipation |
32 |
0.6 |
29 |
0.3 |
|
Abdominal pain‡ |
24 |
0.6 |
23 |
2.9 |
|
Vomiting |
18 |
1.5 |
18 |
2.0 |
|
Diarrhea |
17 |
1.2 |
15 |
1.8 |
|
Metabolism and nutrition disorders |
||||
|
Decreased appetite |
26 |
2.1 |
23 |
0.9 |
|
Skin and subcutaneous tissue disorders |
||||
|
Rash§ |
23 |
0.9 |
14 |
0 |
|
Pruritus |
11 |
0 |
8 |
0 |
|
Psychiatric disorders |
||||
|
Insomnia |
10 |
0 |
11 |
0 |
Table 12 summarizes the laboratory abnormalities in patients treated with IMFINZI plus chemotherapy.
|
||
|
IMFINZI with Gemcitabine and Cisplatin |
Placebo with Gemcitabine and Cisplatin |
|
|
Laboratory Abnormality |
Grade† 3 or 4 (%) |
Grade† 3 or 4 (%) |
|
Chemistry |
||
|
Hyponatremia |
18 |
13 |
|
Gamma-glutamyltransferase increased |
12 |
13 |
|
Increased bilirubin |
10 |
14 |
|
Hypokalemia |
8 |
4.4 |
|
Increased AST |
8 |
8 |
|
Increased ALT |
7 |
6 |
|
Blood creatinine increased |
5 |
2.1 |
|
Hypomagnesemia |
4.5 |
2.2 |
|
Hypoalbuminemia |
3.6 |
2.9 |
|
Hyperkalemia |
2.1 |
2.1 |
|
Increased Alkaline Phosphatase |
1.8 |
3.8 |
|
Hypocalcemia |
1.8 |
2.4 |
|
Hematology |
||
|
Neutropenia |
48 |
49 |
|
Anemia |
31 |
28 |
|
Leukopenia |
28 |
28 |
|
Lymphopenia |
23 |
15 |
|
Thrombocytopenia |
18 |
18 |
Hepatocellular Carcinoma
Unresectable HCC - HIMALAYA
The safety of IMFINZI in combination with tremelimumab-actl was evaluated in a total of 388 patients with uHCC in HIMALAYA, a randomized, open-label, multicenter study [see Clinical Studies (14.1)]. Patients received IMFINZI 1,500 mg administered as a single intravenous infusion in combination with tremelimumab-actl 300 mg on the same day, followed by IMFINZI every 4 weeks or sorafenib 400 mg given orally twice daily.
Serious adverse reactions occurred in 41% of patients who received IMFINZI in combination with tremelimumab-actl. Serious adverse reactions in > 1% of patients included hemorrhage (6%), diarrhea (4%), sepsis (2.1%), pneumonia (2.1%), rash (1.5%), vomiting (1.3%), acute kidney injury (1.3%), and anemia (1.3%). Fatal adverse reactions occurred in 8% of patients who received IMFINZI in combination with tremelimumab-actl, including death (1%), hemorrhage intracranial (0.5%), cardiac arrest (0.5%), pneumonitis (0.5%), hepatic failure (0.5%), and immune-mediated hepatitis (0.5%). The most common adverse reactions (occurring in ≥ 20% of patients) were rash, diarrhea, fatigue, pruritis, musculoskeletal pain, and abdominal pain.
Permanent discontinuation of treatment regimen due to an adverse reaction occurred in 14% of patients; the most common adverse reactions leading to treatment discontinuation (≥ 1%) were hemorrhage (1.8%), diarrhea (1.5%), AST increased (1%), and hepatitis (1%).
Dosage interruptions or delay of the treatment regimen due to an adverse reaction occurred in 35% of patients. Adverse reactions which required dosage interruption or delay in ≥ 1% of patients included ALT increased (3.6%), diarrhea (3.6%), rash (3.6%), amylase increased (3.4%), AST increased (3.1%), lipase increased (2.8%), pneumonia (1.5%), hepatitis (1.5%), pyrexia (1.5%), anemia (1.3%), thrombocytopenia (1%), hyperthyroidism (1%), pneumonitis (1%), and blood creatinine increased (1%).
Table 13 summarizes the adverse reactions that occurred in patients treated with IMFINZI in combination with tremelimumab-actl in the HIMALAYA study.
| IMFINZI and Tremelimumab-actl
(N = 388) | Sorafenib
(N = 374) |
|||
|---|---|---|---|---|
| Adverse Reaction | All Grades (%) | Grade 3-4 (%) | All Grades (%) | Grade 3-4 (%) |
|
||||
|
Gastrointestinal disorders | ||||
|
Diarrhea* |
27 |
6 |
45 |
4.3 |
|
Abdominal pain* |
20 |
1.8 |
24 |
4 |
|
Nausea |
12 |
0 |
14 |
0 |
|
Skin and subcutaneous tissue disorders |
||||
|
Rash* |
32 |
2.8 |
57 |
12 |
|
Pruritus |
23 |
0 |
6 |
0.3 |
|
Metabolism and nutrition disorders |
||||
|
Decreased appetite |
17 |
1.3 |
18 |
0.8 |
|
General disorders and administration site conditions |
||||
|
Fatigue* |
26 |
3.9 |
30 |
6 |
|
Pyrexia* |
13 |
0.3 |
9 |
0.3 |
|
Psychiatric disorders | ||||
|
Insomnia |
10 |
0.3 |
4.3 |
0 |
|
Endocrine disorders |
||||
|
Hypothyroidism* |
14 |
0 |
6 |
0 |
|
Musculoskeletal and Connective Tissue Disorders |
||||
|
Musculoskeletal pain* |
22 |
2.6 |
17 |
0.8 |
Table 14 summarizes the laboratory abnormalities that occurred in patients treated with IMFINZI in combination with tremelimumab-actl in the HIMALAYA study.
| IMFINZI and Tremelimumab-actl | Sorafenib | |||
|---|---|---|---|---|
| Laboratory Abnormality | Any grade*(%)† | Grade 3* or 4 (%)† | Any grade*(%)† | Grade 3* or 4 (%)† |
|
||||
|
Chemistry | ||||
|
Aspartate Aminotransferase increased |
63 |
27 |
55 |
21 |
|
Alanine Aminotransferase increased |
56 |
18 |
53 |
12 |
|
Sodium decreased |
46 |
15 |
40 |
11 |
|
Bilirubin increased |
41 |
8 |
47 |
11 |
|
Alkaline Phosphatase increased |
41 |
8 |
44 |
5 |
|
Glucose increased |
39 |
14 |
29 |
4 |
|
Calcium decreased |
34 |
0 |
43 |
0.3 |
|
Albumin decreased |
31 |
0.5 |
37 |
1.7 |
|
Potassium increased |
28 |
3.8 |
21 |
2.6 |
|
Creatinine increased |
21 |
1.3 |
15 |
0.9 |
|
Hematology | ||||
|
Hemoglobin decreased |
52 |
4.8 |
40 |
6 |
|
Lymphocytes decreased |
41 |
11 |
39 |
10 |
|
Platelets decreased |
29 |
1.6 |
35 |
3.1 |
|
Leukocytes decreased |
20 |
0.8 |
30 |
1.1 |
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
Based on findings from animal studies and its mechanism of action, IMFINZI can cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (12.1)]. There are no available data on the use of IMFINZI in pregnant women.
In animal reproduction studies, administration of durvalumab to pregnant cynomolgus monkeys from the confirmation of pregnancy through delivery at exposure levels approximately 6 to 20 times higher than those observed at the clinical dose of 10 mg/kg based on area under the curve (AUC), resulted in an increase in premature delivery, fetal loss, and premature neonatal death (see Data). Human immunoglobulin G1 (IgG1) is known to cross the placental barrier; therefore, durvalumab has the potential to be transmitted from the mother to the developing fetus. Apprise pregnant women of the potential risk to a fetus.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Animal Data
As reported in the literature, the PD-1/PD-L1 pathway plays a central role in preserving pregnancy by maintaining maternal immune tolerance to the fetus. In mouse allogeneic pregnancy models, disruption of PD-L1 signaling was shown to result in an increase in fetal loss. The effects of durvalumab on prenatal and postnatal development were evaluated in reproduction studies in cynomolgus monkeys. Durvalumab was administered from the confirmation of pregnancy through delivery at exposure levels approximately 6 to 20 times higher than those observed at a clinical dose of 10 mg/kg (based on AUC). Administration of durvalumab resulted in premature delivery, fetal loss (abortion and stillbirth), and increase in neonatal deaths. Durvalumab was detected in infant serum on postpartum Day 1, indicating the presence of placental transfer of durvalumab. Based on its mechanism of action, fetal exposure to durvalumab may increase the risk of developing immune-mediated disorders or altering the normal immune response and immune-mediated disorders have been reported in PD-1 knockout mice.
8.2 Lactation
Risk Summary
There are no data on the presence of durvalumab in human milk, its effects on the breastfed child, or the effects on milk production. Maternal IgG is known to be present in human milk. The effects of local gastrointestinal exposure and limited systemic exposure in the breastfed child to IMFINZI are unknown. Durvalumab was present in the milk of lactating cynomolgus monkeys and was associated with premature neonatal death (see Data).
Because of the potential for adverse reactions in a breastfed child, advise women not to breastfeed during treatment with IMFINZI and for 3 months after the last dose. Refer to the Prescribing Information for the agents administered in combination with IMFINZI for recommended duration to not breastfeed, as appropriate.
Data
In lactating cynomolgus monkeys, durvalumab was present in breast milk at about 0.15% of maternal serum concentrations after administration of durvalumab from the confirmation of pregnancy through delivery at exposure levels approximately 6 to 20 times higher than those observed at the recommended clinical dose of 10 mg/kg (based on AUC). Administration of durvalumab resulted in premature neonatal death.
8.3 Females and Males of Reproductive Potential
Pregnancy testing
Verify pregnancy status of females of reproductive potential prior to initiating treatment with IMFINZI.
Contraception
Females
IMFINZI can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)]. Advise females of reproductive potential to use effective contraception during treatment with IMFINZI and for 3 months following the last dose of IMFINZI. Refer to the Prescribing Information for the agents administered in combination with IMFINZI for recommended contraception duration, as appropriate.
8.4 Pediatric Use
The safety and effectiveness of IMFINZI have not been established in pediatric patients.
8.5 Geriatric Use
Of the 476 patients treated with IMFINZI in the PACIFIC study, 45% were 65 years or older, while 7.6% were 75 years or older. No overall differences in safety or effectiveness were observed between patients 65 years or older and younger patients. The PACIFIC study did not include sufficient numbers of patients aged 75 years and over to determine whether they respond differently from younger patients.
Of the 265 patients with ES-SCLC treated with IMFINZI in combination with chemotherapy 101 (38%) patients were 65 years or older and 19 (7.2%) patients were 75 years or older. There were no clinically meaningful differences in safety or efficacy between patients 65 years or older and younger patients.
Of the 330 patients with metastatic NSCLC treated with IMFINZI in combination with tremelimumab-actl and platinum-based chemotherapy, 143 (43%) patients were 65 years or older and 35 (11%) patients were 75 years or older. There were no clinically meaningful differences in safety or efficacy between patients 65 years or older and younger patients.
Of the 338 patients with BTC treated with IMFINZI in combination with chemotherapy in the TOPAZ-1 study, 158 (47%) patients were 65 years or older and 38 (11%) patients were 75 years or older. No overall differences in safety or effectiveness of IMFINZI have been observed between patients 65 years of age and older and younger adult patients.
Of the 393 patients with uHCC treated with IMFINZI in combination with tremelimumab-actl, 50% of patients were 65 years of age or older and 13% of patients were 75 years of age or older. No overall differences in safety or effectiveness of IMFINZI have been observed between patients 65 years of age and older and younger adult patients.
11. Imfinzi Description
Durvalumab is a programmed cell death ligand 1 (PD-L1) blocking antibody. Durvalumab is a human immunoglobulin G1 kappa (IgG1κ) monoclonal antibody that is produced by recombinant DNA technology in Chinese Hamster Ovary (CHO) cell suspension culture.
IMFINZI (durvalumab) Injection for intravenous use is a sterile, preservative-free, clear to opalescent, colorless to slightly yellow solution, free from visible particles.
Each 500 mg vial of IMFINZI contains 500 mg of durvalumab in 10 mL solution. Each mL contains durvalumab, 50 mg, L-histidine (2 mg), L-histidine hydrochloride monohydrate (2.7 mg), α,α-trehalose dihydrate (104 mg), Polysorbate 80 (0.2 mg), and Water for Injection, USP.
Each 120 mg vial of IMFINZI contains 120 mg of durvalumab in 2.4 mL solution. Each mL contains durvalumab, 50 mg, L-histidine (2 mg), L-histidine hydrochloride monohydrate (2.7 mg), α,α-trehalose dihydrate (104 mg), Polysorbate 80 (0.2 mg), and Water for Injection, USP.
12. Imfinzi - Clinical Pharmacology
12.1 Mechanism of Action
Expression of programmed cell death ligand-1 (PD-L1) can be induced by inflammatory signals (e.g., IFN-gamma) and can be expressed on both tumor cells and tumor-associated immune cells in the tumor microenvironment. PD-L1 blocks T-cell function and activation through interaction with PD-1 and CD80 (B7.1). By binding to its receptors, PD-L1 reduces cytotoxic T-cell activity, proliferation, and cytokine production.
Durvalumab is a human immunoglobulin G1 kappa (IgG1κ) monoclonal antibody that binds to PD-L1 and blocks the interaction of PD-L1 with PD-1 and CD80 (B7.1). Blockade of PD-L1/PD-1 and PD-L1/CD80 interactions releases the inhibition of immune responses, without inducing antibody dependent cell-mediated cytotoxicity (ADCC).
PD-L1 blockade with durvalumab led to increased T-cell activation in vitro and decreased tumor size in co-engrafted human tumor and immune cell xenograft mouse models.
12.2 Pharmacodynamics
The steady state AUC, Ctrough, and Cmax in patients administered with 1,500 mg every 4 weeks are 6% higher, 19% lower, and 55% higher than those administered with 10 mg/kg every 2 weeks, respectively. Based on the modeling of pharmacokinetic data and exposure relationships for safety, there are no anticipated clinically meaningful differences in efficacy and safety for the doses of 1,500 mg every 4 weeks compared to 10 mg/kg every 2 weeks in patients weighing > 30 kg with NSCLC.
12.3 Pharmacokinetics
The pharmacokinetics of durvalumab as a single agent was studied in patients with doses ranging from 0.1 mg/kg (0.01 times the approved recommended dosage) to 20 mg/kg (2 times the approved recommended dosage) administered once every two, three, or four weeks.
PK exposure increased more than dose-proportionally at doses < 3 mg/kg (0.3 times the approved recommended dosage) and dose proportionally at doses ≥ 3 mg/kg every 2 weeks. Steady state was achieved at approximately 16 weeks.
The pharmacokinetics of durvalumab is similar when assessed as a single agent, when in combination with chemotherapy, when in combination with tremelimumab-actl and when in combination with tremelimumab-actl and platinum-based chemotherapy.
Distribution
The geometric mean (% coefficient of variation [CV%]) steady state volume of distribution (Vss) was 5.4 (13.1%) L.
Elimination
Durvalumab clearance decreases over time, with a mean maximal reduction (CV%) from baseline values of approximately 23% (57%) resulting in a geometric mean (CV%) steady state clearance (CLss) of 8 mL/h (39%) at day 365; the decrease in CLss is not considered clinically relevant. The geometric mean (CV%) terminal half-life, based on baseline CL was approximately 21 (26%) days.
Specific Populations
There were no clinically significant differences in the pharmacokinetics of durvalumab based on body weight (31 to 175 kg), age (18 to 96 years), sex, race (White, Black, Asian, Native Hawaiian, Pacific Islander, or Native American), albumin levels (4 to 57 g/L), lactate dehydrogenase levels (18 to 15,800 U/L), soluble PD-L1 (67 to 3,470 pg/mL), tumor type (NSCLC, SCLC, BTC and HCC), mild or moderate renal impairment (CLcr 30 to 89 mL/min), and mild or moderate hepatic impairment (bilirubin ≤ 3x ULN and any AST). The effect of severe renal impairment (CLcr 15 to 29 mL/min) or severe hepatic impairment (bilirubin > 3x ULN and any AST) on the pharmacokinetics of durvalumab is unknown.
12.6 Immunogenicity
The observed incidence of anti-drug antibodies (ADA) is highly dependent on the sensitivity and specificity of the assay. Differences in assay methods preclude meaningful comparison of the incidence of ADAs in the studies described below with the incidence of ADAs in other studies including those of IMFINZI.
Of the 2,280 patients who received IMFINZI 10 mg/kg every 2 weeks or 20 mg/kg every 4 weeks as a single-agent, 69 patients (3%) tested positive for ADAs and 12 (0.5%) tested positive for neutralizing antibodies. The development of ADAs against durvalumab appears to have no clinically relevant effect on its pharmacokinetics or safety.
Of the 201 patients in the CASPIAN study who received IMFINZI 1,500 mg every 3 weeks in combination with chemotherapy for four doses followed by IMFINZI 1,500 mg every 4 weeks, no patients tested positive for ADAs.
Of the 240 patients in the TOPAZ-1 study who received IMFINZI 1,500 mg every 3 weeks in combination with chemotherapy up to 8 cycles followed by IMFINZI 1,500 mg every 4 weeks, 2 (0.8%) patients tested positive for treatment-emergent ADAs and neutralizing antibodies, respectively. There were insufficient numbers of patients with ADAs or neutralizing antibodies (2 patients each) to determine whether ADAs have an impact on pharmacokinetics, pharmacodynamics, safety and/or effectiveness of IMFINZI.
During the 12 week treatment period in the HIMALAYA study, of the 294 patients who received IMFINZI once every 4 weeks in combination with a single dose of tremelimumab-actl and who were evaluated for the presence of ADAs against IMFINZI at predose week 0, week 4 and week 12, 3.1% (9/294) of patients tested positive for anti-durvalumab-antibodies. Among the 9 patients who tested positive for ADA, 55.6% (5/9) tested positive for neutralizing antibodies against durvalumab. There was no identified clinically significant effect of anti-durvalumab antibodies on the safety of durvalumab; however, the effect of ADAs on the pharmacokinetics and effectiveness of durvalumab is unknown.
During 16 weeks of treatment during the POSEIDON study, among 286 patients who received IMFINZI 1,500 mg in combination with tremelimumab-actl 75 mg every 3 weeks for five doses and chemotherapy for four cycles followed by IMFINZI 1,500 mg every 4 weeks 10% (29/286) of patients tested positive for anti-durvalumab antibodies with predose sampling at week 0, week 3 and week 12. Among the 29 patients who tested positive for ADAs, 10% (3/29) tested positive for neutralizing antibodies against durvalumab. The geometric mean of durvalumab concentration in patients with ADA positive was 46 mcg/mL compared to 89 mcg/mL in patients with ADA negative. There was no clinically significant effect of anti-durvalumab antibodies on the safety of durvalumab; however, there is insufficient data to assess whether the observed ADA associated pharmacokinetic changes reduce effectiveness of durvalumab.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
The carcinogenic and genotoxic potential of durvalumab have not been evaluated.
Animal fertility studies have not been conducted with durvalumab. In repeat-dose toxicology studies with durvalumab in sexually mature cynomolgus monkeys of up to 3 months duration, there were no notable effects on the male and female reproductive organs.
13.2 Animal Toxicology and/or Pharmacology
In animal models, inhibition of PD-L1/PD-1 signaling increased the severity of some infections and enhanced inflammatory responses. Mycobacterium tuberculosis-infected PD-1 knockout mice exhibit markedly decreased survival compared with wild-type controls, which correlated with increased bacterial proliferation and inflammatory responses in these animals. PD-1 blockade using a primate anti-PD-1 antibody was also shown to exacerbate M. tuberculosis infection in rhesus macaques. PD-L1 and PD-1 knockout mice have also shown decreased survival following infection with lymphocytic choriomeningitis virus.
14. Clinical Studies
14.1 Non-Small Cell Lung Cancer (NSCLC)
Unresectable Stage III NSCLC - PACIFIC
The efficacy of IMFINZI was evaluated in the PACIFIC study (NCT02125461), a multicenter, randomized, double-blind, placebo-controlled study in patients with unresectable Stage III NSCLC who completed at least 2 cycles of concurrent platinum-based chemotherapy and definitive radiation within 42 days prior to initiation of the study drug and had a WHO performance status of 0 or 1. The study excluded patients who had progressed following concurrent chemoradiation, patients with active or prior documented autoimmune disease within 2 years of initiation of the study or patients with medical conditions that required systemic immunosuppression. Randomization was stratified by sex, age (< 65 years vs. ≥ 65 years), and smoking history (smoker vs. non-smoker). Patients were randomized 2:1 to receive IMFINZI 10 mg/kg or placebo intravenously every 2 weeks for up to 12 months or until unacceptable toxicity or confirmed RECIST v1.1-defined progression. Assessment of tumor status was performed every 8 weeks. The major efficacy outcome measures were progression-free survival (PFS) as assessed by a BICR RECIST v1.1, and overall survival (OS). Additional efficacy outcome measures included ORR and DoR assessed by BICR.
A total of 713 patients were randomized: 476 patients to the IMFINZI arm and 237 to the placebo arm. The study population characteristics were: median age of 64 years (range: 23 to 90); 70% male; 69% White and 27% Asian; 16% current smokers, 75% former smokers, and 9% never smokers; 51% WHO performance status of 1; 53% with Stage IIIA and 45% were Stage IIIB; 46% with squamous and 54% with non-squamous histology. All patients received definitive radiotherapy as per protocol, of which 92% received a total radiation dose of 54 Gy to 66 Gy; 99% of patients received concomitant platinum-based chemotherapy (55% cisplatin-based, 42% carboplatin-based chemotherapy, and 2% switched between cisplatin and carboplatin).
At a pre-specified interim analysis for OS based on 299 events (61% of total planned events), the study demonstrated a statistically significant improvement in OS in patients randomized to IMFINZI compared to placebo. The pre-specified interim analysis of PFS based on 371 events (81% of total planned events) demonstrated a statistically significant improvement in PFS in patients randomized to IMFINZI compared to placebo. Table 15 and Figure 1 summarizes the efficacy results for PACIFIC.
| Endpoint | IMFINZI (N = 476)* | Placebo (N = 237)* |
|---|---|---|
| Overall Survival (OS)† | ||
| Number of deaths | 183 (38%) | 116 (49%) |
| Median in months (95% CI) | NR (34.7, NR) | 28.7 (22.9, NR) |
| Hazard Ratio (95% CI)‡ | 0.68 (0.53, 0.87) | |
| p-value‡, | 0.0025 | |
|
||
|
||
|
|
|
|
|
|
|
|
|
|
|
|
Figure 1. Kaplan-Meier Curves of Overall Survival in the PACIFIC Study
Metastatic NSCLC - POSEIDON
The efficacy of IMFINZI in combination with tremelimumab-actl and platinum-based chemotherapy in previously untreated metastatic NSCLC patients with no sensitizing epidermal growth factor receptor (EGFR) mutation or anaplastic lymphoma kinase (ALK) genomic tumor aberrations was investigated in POSEIDON, a randomized, multicenter, active-controlled, open-label trial (NCT03164616). Eligible patients had Eastern Cooperative Oncology Group (ECOG) Performance Status of 0 or 1 and must have had no prior chemotherapy or any other systemic therapy for metastatic NSCLC. Choice of platinum-based chemotherapy was at the investigator’s discretion, taking into consideration the calculated creatinine clearance. Patients with active and/or untreated brain metastases; a history of active primary immunodeficiency; autoimmune disorders including active or prior documented autoimmune or inflammatory disorders; use of systemic immunosuppressants within 14 days before the first dose of the treatment except physiological dose of systemic corticosteroids were ineligible.
Randomization was stratified by tumor cells (TC) PD-L1 expression (TC ≥ 50% vs. TC < 50%), disease stage (Stage IVA vs. Stage IVB), and histology (non-squamous vs. squamous).
Patients were randomized 1:1:1 to receive IMFINZI in combination with tremelimumab-actl and platinum-based chemotherapy according to the regimens listed below, IMFINZI and platinum-based chemotherapy (an unapproved regimen for metastatic NSCLC), or platinum-based chemotherapy. The evaluation of efficacy for metastatic NSCLC relied on comparison between:
- •
- IMFINZI 1,500 mg with tremelimumab-actl 75 mg (or 1 mg/kg for patients < 30 kg) and platinum-based chemotherapy every 3 weeks for 4 cycles, followed by IMFINZI 1,500 mg every 4 weeks as a single agent. A fifth dose of tremelimumab-actl 75 mg (or 1 mg/kg for patients < 30 kg) was given at Week 16 in combination with IMFINZI dose 6.
- •
- Platinum-based chemotherapy every 3 weeks as monotherapy for 4 cycles. Patients could receive an additional 2 cycles (a total of 6 cycles post-randomization), as clinically indicated, at investigator’s discretion.
Patients received IMFINZI in combination with tremelimumab-actl with one of the following platinum-based chemotherapy regimens:
- •
- Non-squamous NSCLC
- •
- Pemetrexed 500 mg/m2 with carboplatin AUC 5-6 or cisplatin 75 mg/m2 every 3 weeks for 4 cycles.
- •
- Squamous NSCLC
- •
- Gemcitabine 1,000 or 1,250 mg/m2 on Days 1 and 8 with cisplatin 75 mg/m2 or carboplatin AUC 5-6 on Day 1 every 3 weeks for 4 cycles.
- •
- Non-squamous and Squamous NSCLC
- •
- Nab-paclitaxel 100 mg/m2 on Days 1, 8, and 15 with carboplatin AUC 5-6 on Day 1 every 3 weeks for 4 cycles.
Tremelimumab-actl was given up to a maximum of 5 doses. IMFINZI and histology-based pemetrexed continued every 4 weeks until disease progression or unacceptable toxicity. Administration of IMFINZI monotherapy was permitted beyond disease progression if the patient was clinically stable and deriving clinical benefit as determined by the investigator. Patients with disease progression during IMFINZI monotherapy were given the option to be retreated with 4 additional cycles of tremelimumab-actl in combination with IMFINZI. Tumor assessments were performed at Week 6, Week 12, and then every 8 weeks thereafter.
The major efficacy outcome measures were progression free survival (PFS) and overall survival (OS) of IMFINZI and tremelimumab-actl in combination with platinum-based chemotherapy compared to platinum-based chemotherapy alone. Additional efficacy outcome measures were overall response rate (ORR) and duration of response (DoR). PFS, ORR, and DoR were assessed using Blinded Independent Central Review (BICR) according to RECIST v1.1.
A total of 675 patients were randomized to receive either IMFINZI with tremelimumab-actl and platinum-based-chemotherapy (n = 338) or platinum-based chemotherapy (n = 337). The median age was 63 years (range: 27 to 87), 46% of patients age ≥ 65 years, 77% male, 57% White, 34% Asian, 0.3% Native Hawaiian or Other Pacific Islander, 3% American Indian or Alaska Native, 2% Black or African American, 4% Other Race, 79% former or current smoker, 34% ECOG PS 0, and 66% ECOG PS 1. Thirty-six percent had squamous histology, 63% non-squamous histology, 29% PD-L1 expression TC ≥ 50%, 71% PD-L1 expression TC < 50%.
Efficacy results are summarized in Table 16 and Figure 2.
| IMFINZI with tremelimumab-actl and platinum-based chemotherapy (n = 338) | Platinum-based chemotherapy (n = 337) |
|
|---|---|---|
|
||
|
OS* | ||
|
251 (74) |
285 (85) |
|
14.0 (11.7, 16.1) |
11.7 (10.5, 13.1) |
|
0.77 (0.65, 0.92) |
|
|
0.00304 |
|
|
PFS† | ||
|
238 (70) |
258 (77) |
|
6.2 (5.0, 6.5) |
4.8 (4.6, 5.8) |
|
0.72 (0.60, 0.86) |
|
|
0.00031 |
|
|
ORR % (95% CI)‡ |
39 (34, 44) |
24 (20, 29) |
|
Median DoR (months)
|
9.5 (7.2, NR) |
5.1 (4.4, 6.0) |
|
NR=Not Reached, CI=Confidence Interval |
||
Figure 2. Kaplan-Meier curves of OS in POSEIDON
14.2 Small Cell Lung Cancer (SCLC)
Extensive-stage SCLC – CASPIAN
The efficacy of IMFINZI in combination with etoposide and either carboplatin or cisplatin in previously untreated ES-SCLC was investigated in CASPIAN, a randomized, multicenter, active-controlled, open-label trial (NCT03043872). Eligible patients had WHO Performance Status of 0 or 1 and were suitable to receive a platinum-based chemotherapy regimen as first-line treatment for SCLC. Patients with asymptomatic or treated brain metastases were eligible. Choice of platinum agent was at the investigator’s discretion, taking into consideration the calculated creatinine clearance. Patients with history of chest radiation therapy; a history of active primary immunodeficiency; autoimmune disorders including paraneoplastic syndrome; active or prior documented autoimmune or inflammatory disorders; use of systemic immunosuppressants within 14 days before the first dose of the treatment except physiological dose of systemic corticosteroids were ineligible.
Randomization was stratified by the planned platinum-based therapy in cycle 1 (carboplatin or cisplatin).
The evaluation of efficacy for ES-SCLC relied on comparison between:
IMFINZI 1,500 mg, and investigator’s choice of carboplatin (AUC 5 or 6 mg/mL/min) or cisplatin (75-80 mg/m2) on Day 1 and etoposide (80-100 mg/m2) intravenously on Days 1, 2, and 3 of each 21 day cycle for 4 cycles, followed by IMFINZI 1,500 mg every 4 weeks until disease progression or unacceptable toxicity, or
Investigator’s choice of carboplatin (AUC 5 or 6 mg/mL/min) or cisplatin (75-80 mg/m2) on Day 1 and etoposide (80-100 mg/m2) intravenously on Days 1, 2, and 3 of each 21-day cycle, up to 6 cycles. After completion of chemotherapy, PCI as administered per investigator discretion.
Administration of IMFINZI as a single agent was permitted beyond disease progression if the patient was clinically stable and deriving clinical benefit as determined by the investigator.
The major efficacy outcome measure was overall survival (OS) of IMFINZI plus chemotherapy vs. chemotherapy alone. Additional efficacy outcome measures were investigator-assessed progression-free survival (PFS) and objective response rate (ORR), per RECIST v1.1.
The study population characteristics were: median age of 63 years (range: 28 to 82); 40% age 65 or older; 70% male; 84% White, 15% Asian, and 0.9% Black; 65% WHO/ECOG PS of 1; and 93% were former/current smokers. Ninety percent of patients had Stage IV disease and 10% had brain metastasis at baseline. A total of 25% of the patients received cisplatin and 74% of the patients received carboplatin. In the chemotherapy alone arm, 57% of the patients received 6 cycles of chemotherapy, and 8% of the patients received PCI.
The OS results are summarized in Table 17 and Figure 3.
|
||
|
Endpoint |
IMFINZI with Etoposide and either Carboplatin or Cisplatin (n = 268) |
Etoposide and either Carboplatin or Cisplatin (n = 269) |
|
Overall Survival (OS) |
||
|
Number of deaths (%)* |
155 (58) |
181 (67) |
|
Median OS (months) (95% CI) |
13.0 (11.5, 14.8) |
10.3 (9.3, 11.2) |
|
Hazard Ratio (95% CI)† |
0.73 (0.59, 0.91) |
|
|
p-value* |
0.0047 |
|
Figure 3. Kaplan-Meier Curves of Overall Survival in the CASPIAN Study
Investigator-assessed PFS (96% of total planned events) showed a HR of 0.78 (95% CI: 0.65, 0.94), with median PFS of 5.1 months (95% CI: 4.7, 6.2) in the IMFINZI plus chemotherapy arm and 5.4 months (95% CI: 4.8, 6.2) in the chemotherapy alone arm. The investigator-assessed confirmed ORR was 68% (95% CI: 62%, 73%) in the IMFINZI plus chemotherapy arm and 58% (95% CI: 52%, 63%) in the chemotherapy alone arm.
In the exploratory subgroup analyses of OS based on the planned platinum chemotherapy received at cycle 1, the HR was 0.70 (95% CI 0.55, 0.89) in patients who received carboplatin, and the HR was 0.88 (95% CI 0.55, 1.41) in patients who received cisplatin.
14.3 Biliary Tract Cancer (BTC)
Locally advanced or metastatic BTC - TOPAZ-1
The efficacy of IMFINZI in combination with gemcitabine and cisplatin in patients with locally advanced or metastatic BTC was investigated in TOPAZ-1 (NCT03875235), a randomized, double-blind, placebo-controlled, multicenter trial that enrolled 685 patients with histologically confirmed locally advanced unresectable or metastatic BTC who have not previously received systemic therapy. Patients with recurrent disease > 6 months after surgery and/or completion of adjuvant therapy were eligible. Patients had an ECOG Performance status of 0 and 1 and at least one target lesion by RECIST 1.1. Patients with ampullary carcinoma; active or prior documented autoimmune or inflammatory disorders; HIV infection or active infections, including tuberculosis or hepatitis C; current or prior use of immunosuppressive medication within 14 days before the first dose of IMFINZI were ineligible.
Randomization was stratified by disease status (recurrent vs. initially unresectable) and primary tumor location (intrahepatic cholangiocarcinoma [ICCA] vs. extrahepatic cholangiocarcinoma [ECCA] vs. gallbladder cancer [GBC]). Patients were randomized 1:1 to receive:
- •
- IMFINZI 1,500 mg on Day 1+ gemcitabine 1,000 mg/m2 and cisplatin 25 mg/m2 on Days 1 and 8 of each 21-day cycle up to 8 cycles, followed by IMFINZI 1,500 mg every 4 weeks, or
- •
- Placebo on Day 1+ gemcitabine 1,000 mg/m2 and cisplatin 25 mg/m2 on Days 1 and 8 of each 21-day cycle up to 8 cycles, followed by placebo every 4 weeks.
Treatment with IMFINZI or placebo continued until disease progression, or unacceptable toxicity. Treatment beyond disease progression was permitted if the patient was clinically stable and deriving clinical benefit as determined by the investigator.
The major efficacy outcome measure was overall survival (OS). Additional efficacy outcome measures were investigator-assessed progression-free survival (PFS), objective response rate (ORR) and duration of response (DoR). Tumor assessments were conducted every 6 weeks for the first 24 weeks after the date of randomization, and then every 8 weeks until confirmed objective disease progression.
The study population characteristics were: 50% male, median age of 64 years (range 20-85), 47% age 65 or older; 56% Asian, 37% White, 2% Black or African American, 0.1% American Indian or Alaskan Native, and 4% other; 51% had an ECOG PS of 1; primary tumor location was ICCA 56%, ECCA 18% and GBC 25%; 20% of patients had recurrent disease; 86% of patients had metastatic and 14% had locally advanced disease.
At a pre-specified interim analysis, the trial demonstrated a statistically significant improvement in OS and PFS in patients randomized to IMFINZI in combination with chemotherapy compared to placebo in combination with chemotherapy. Table 18 summarizes the efficacy results for TOPAZ-1.
| Endpoint | IMFINZI with Gemcitabine and Cisplatin
(n = 341) | Placebo with Gemcitabine and Cisplatin
(n = 344) |
|---|---|---|
|
||
|
Overall Survival (OS) | ||
|
198 (58) |
226 (66) |
|
12.8 |
11.5 |
|
0.80 (0.66, 0.97) |
|
|
0.021 |
|
|
Progression-Free Survival (PFS) | ||
|
276 (81) |
297 (86) |
|
7.2 |
5.7 |
|
0.75 (0.63, 0.89) | |
|
0.001 | |
The investigator-assessed ORR was 27% (95% CI: 22% - 32%) in the IMFINZI plus chemotherapy arm and 19% (95% CI: 15%-23%) in the chemotherapy alone arm.
Figure 4: Kaplan-Meier Curve of OS in TOPAZ-1 Study
14.4 Hepatocellular Carcinoma (HCC)
The efficacy of IMFINZI in combination with tremelimumab-actl was evaluated in the HIMALAYA study (NCT03298451), a randomized (1:1:1), open-label, multicenter study in patients with confirmed uHCC who had not received prior systemic treatment for HCC. Patients were randomized to one of two investigational arms (IMFINZI plus trememlimumab-actl or IMFINZI) or sorafenib. Study treatment consisted of IMFINZI 1,500 mg in combination with tremelimumab-actl as a one-time single intravenous infusion of 300 mg on the same day, followed by IMFINZI every 4 weeks; IMFINZI 1,500 mg every 4 weeks; or sorafenib 400 mg given orally twice daily, until disease progression or unacceptable toxicity. The efficacy assessment of IMFINZI is based on patients randomized to the IMFINZI plus tremelimumab-actl arm versus the sorafenib arm. Randomization was stratified by macrovascular invasion (MVI) (yes or no), etiology of liver disease (hepatitis B virus vs. hepatitis C virus vs. others) and ECOG performance status (0 vs. 1).
The study enrolled patients with BCLC Stage C or B (not eligible for locoregional therapy). The study excluded patients with co-infection of viral hepatitis B and hepatitis C; active or prior documented gastrointestinal (GI) bleeding within 12 months; ascites requiring non-pharmacologic intervention within 6 months; hepatic encephalopathy within 12 months before the start of treatment; active or prior documented autoimmune or inflammatory disorders. Esophagogastroduodenoscopy was not mandated prior to enrollment but adequate endoscopic therapy, according to institutional standards, was required for patients with history of esophageal variceal bleeding or those assessed as high risk for esophageal variceal bleeding by the treating physician.
Study treatment was permitted beyond disease progression if the patient was clinically stable and deriving clinical benefit as determined by the investigator.
The major efficacy outcome measure was overall survival (OS) between the IMFINZI plus tremelimumab-actl arm versus the sorafenib arm. Additional efficacy outcomes were investigator-assessed progression-free survival (PFS), objective response rate (ORR) and duration of response (DoR) according to RECIST v1.1. Tumor assessments were conducted every 8 weeks for the first 12 months and then every 12 weeks thereafter.
The baseline demographics of the IMFINZI plus tremelimumab-actl and sorafenib arms were as follows: male (85%), age < 65 years (50%), median age of 65 years (range: 18 to 88 years), White (46%), Asian (49%), Black or African American (2%), Native Hawaiian or other Pacific Islander (0.1%), race Unknown (2%), Hispanic or Latino (5%), Not Hispanic or Latino (94%), ethnicity Unknown (1%), ECOG PS 0 (62%); Child-Pugh Class score A (99%), macrovascular invasion (26%), extrahepatic spread (53%), viral etiology; hepatitis B (31%), hepatitis C (27%), and uninfected (42%).
Efficacy results are presented in Table 19 and Figure 5.
| Endpoint | IMFINZI and Tremelimumab-actl
(N = 393) | Sorafenib
(N = 389) |
|---|---|---|
|
||
|
OS |
||
|
Number of deaths (%) |
262 (66.7) |
293 (75.3) |
|
16.4 (14.2, 19.6) |
13.8 (12.3, 16.1) |
|
0.78 (0.66, 0.92) |
|
|
0.0035 |
|
|
PFS |
||
|
Number of events (%) |
335 (85.2) |
327 (84.1) |
|
Median PFS (months) (95% CI) |
3.8 (3.7, 5.3) |
4.1 (3.7, 5.5) |
|
HR (95% CI)* |
0.90 (0.77, 1.05) |
|
|
ORR |
||
|
20.1 (16.3, 24.4) |
5.1 (3.2, 7.8) |
|
12 (3.1) |
0 |
|
67 (17.0) |
20 (5.1) |
|
DoR |
||
|
22.3 (13.7, NR) |
18.4 (6.5, 26.0) |
|
82.3 |
78.9 |
|
65.8 |
63.2 |
|
CI=Confidence Interval, HR=Hazard Ratio, NR=Not Reached |
||
Figure 5. Kaplan-Meier curve of OS
16. How is Imfinzi supplied
IMFINZI (durvalumab) Injection is a clear to opalescent, colorless to slightly yellow solution supplied in a carton containing one single-dose vial either as:
- •
- 500 mg/10 mL (50 mg/mL) (NDC 0310-4611-50)
- •
- 120 mg/2.4 mL (50 mg/mL) (NDC 0310-4500-12)
Store in a refrigerator at 2°C to 8°C (36°F to 46°F) in original carton to protect from light.
Do not freeze. Do not shake.
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Immune-Mediated Adverse Reactions
Inform patients of the risk of immune-mediated adverse reactions that may require corticosteroid treatment and interruption or discontinuation of IMFINZI [see Warnings and Precautions (5.1)], including:
- •
- Pneumonitis: Advise patients to contact their healthcare provider immediately for any new or worsening cough, chest pain, or shortness of breath.
- •
- Hepatitis: Advise patients to contact their healthcare provider immediately for jaundice, severe nausea or vomiting, pain on the right side of abdomen, lethargy, or easy bruising or bleeding.
- •
- Colitis: Advise patients to contact their healthcare provider immediately for diarrhea, blood or mucus in stools, or severe abdominal pain.
- •
- Endocrinopathies: Advise patients to contact their healthcare provider immediately for signs or symptoms of hypothyroidism, hyperthyroidism, adrenal insufficiency, type 1 diabetes mellitus, or hypophysitis.
- •
- Nephritis: Advise patients to contact their healthcare provider immediately for signs or symptoms of nephritis.
- •
- Dermatological Reactions: Advise patients to contact their healthcare provider immediately for signs or symptoms of severe dermatological reactions.
- •
- Pancreatitis: Advise patients to contact their healthcare provider immediately for signs or symptoms of pancreatitis.
- •
- Other Immune-Mediated Adverse Reactions: Advise patients to contact their healthcare provider immediately for signs or symptoms of pancreatitis, aseptic meningitis, encephalitis, immune thrombocytopenia, myocarditis, hemolytic anemia, myositis, uveitis, keratitis, and myasthenia gravis.
Infusion-Related Reactions:
- •
- Advise patients to contact their healthcare provider immediately for signs or symptoms of infusion-related reactions [see Warnings and Precautions (5.2)].
Complications of Allogeneic HSCT:
- •
- Advise patients of potential risk of post-transplant complications [see Warnings and Precautions (5.3)].
Embryo-Fetal Toxicity:
- •
- Advise females of reproductive potential that IMFINZI can cause harm to a fetus and to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.4) and Use in Specific Populations (8.1,8.3)].
- •
- Advise females of reproductive potential to use effective contraception during treatment and for 3 months after the last dose of IMFINZI [see Use in Specific Populations (8.3)].
Lactation:
- •
- Advise female patients not to breastfeed while taking IMFINZI and for 3 months after the last dose [see Warnings and Precautions (5.4) and Use in Specific Populations (8.2)].
Manufactured for:
AstraZeneca Pharmaceuticals LP
Wilmington, DE 19850
By: AstraZeneca UK Limited
1 Francis Crick Ave.
Cambridge, England CB2 0AA
US License No. 2043
IMFINZI is a registered trademark of AstraZeneca group of companies.
© AstraZeneca 2022
|
MEDICATION GUIDE
|
|||
|
What is the most important information I should know about IMFINZI? IMFINZI is a medicine that may treat certain cancers by working with your immune system. IMFINZI can cause your immune system to attack normal organs and tissues in any area of your body and can affect the way they work. These problems can sometimes become severe or life-threatening and can lead to death. You can have more than one of these problems at the same time. These problems may happen anytime during treatment or even after your treatment has ended. Call or see your healthcare provider right away if you develop any new or worsening signs or symptoms, including: Lung problems. |
|||
|
|
|
|
|
Intestinal problems. |
|||
|
|
||
|
Liver problems. |
|||
|
|
||
|
Hormone gland problems. |
|||
|
|
||
|
Kidney problems. |
|||
|
|
||
|
Skin problems. |
|||
|
|
||
|
Pancreas problems |
|||
|
|
||
|
Problems can also happen in other organs and tissues. These are not all of the signs and symptoms of immune system problems that can happen with IMFINZI. Call or see your healthcare provider right away for any new or worsening signs or symptoms, which may include:
|
|||
|
Infusion reactions that can sometimes be severe or life-threatening. Signs and symptoms of infusion reactions may include: |
|||
|
|
||
|
Complications, including graft-versus-host disease (GVHD), in people who have received a bone marrow (stem cell) transplant that uses donor stem cells (allogeneic). These complications can be serious and can lead to death. These complications may happen if you underwent transplantation either before or after being treated with IMFINZI. Your healthcare provider will monitor you for these complications. Getting medical treatment right away may help keep these problems from becoming more serious. Your healthcare provider will check you for these problems during your treatment with IMFINZI. Your healthcare provider may treat you with corticosteroid or hormone replacement medicines. Your healthcare provider may also need to delay or completely stop treatment with IMFINZI, if you have severe side effects. |
|||
|
What is IMFINZI? IMFINZI is a prescription medicine used to treat adults with:
It is not known if IMFINZI is safe and effective in children. |
|||
|
Before you receive IMFINZI, tell your healthcare provider about all of your medical conditions, including if you:
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. |
|||
|
How will I receive IMFINZI?
|
|||
|
What are the possible side effects of IMFINZI? IMFINZI can cause serious side effects, including: See “What is the most important information I should know about IMFINZI?” |
|||
|
The most common side effects of IMFINZI in adults with NSCLC include: |
|||
|
|
||
|
The most common side effects of IMFINZI when used with tremelimumab-actl and platinum-containing chemotherapy in adults with metastatic NSCLC include: |
|||
|
|
||
|
The most common side effects of IMFINZI when used with other anticancer medicines in adults with ES-SCLC include: |
|||
|
|
||
|
The most common side effects of IMFINZI when used with other anticancer medicines in adults with BTC include: |
|||
|
|
||
|
The most common side effects of IMFINZI when used with tremelimumab-actl in adults with uHCC include: |
|||
|
|
||
|
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of IMFINZI. Ask your healthcare provider or pharmacist for more information. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
|||
|
General information about the safe and effective use of IMFINZI. Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. If you would like more information about IMFINZI, talk with your healthcare provider. You can ask your healthcare provider for information about IMFINZI that is written for health professionals. |
|||
|
What are the ingredients in IMFINZI? Active ingredient: durvalumab Inactive ingredients: L-histidine, L-histidine hydrochloride monohydrate, α,α-trehalose dihydrate, polysorbate 80, water for injection, USP. |
|||
|
Manufactured for: AstraZeneca Pharmaceuticals LP, Wilmington, DE 19850 By: AstraZeneca UK Limited, 1 Francis Crick Ave. Cambridge, England CB2 0AA US License No. 2043 IMFINZI is a registered trademark of AstraZeneca group of companies. For more information, call 1-800-236-9933 or go to www.IMFINZI.com © AstraZeneca 2022 |
|||
This Medication Guide has been approved by the U.S. Food and Drug Administration. Revised: 6/2023
PACKAGE/LABEL PRINCIPAL DISPLAY PANEL
NDC 0310-4500-12
Rx only
IMFINZI™
(durvalumab)
Injection
120 mg/2.4 mL
(50 mg/mL)
For Intravenous Infusion After Dilution
Single-dose vial. Discard unused portion.
Store at 2° to 8°C (36° to 46°F).
Do not freeze or shake.
Keep vial in original carton to protect from light.
Attention Pharmacist: Dispense the accompanying Medication Guide to each patient.
Do not use if vial seal is broken or missing.
Must dilute before use.
See prescribing information.
AstraZeneca
PACKAGE/LABEL DISPLAY PANEL
NDC 0310-4611-50
Rx only
IMFINZI™
(durvalumab)
Injection
500 mg/10 mL
(50 mg/mL)
For Intravenous Infusion After Dilution
Single-dose vial. Discard unused portion.
Store at 2° to 8°C (36° to 46°F).
Do not freeze or shake.
Keep vial in original carton to protect from light.
Attention Pharmacist: Dispense the accompanying Medication Guide to each patient.
Do not use if vial seal is broken or missing.
Must dilute before use.
See prescribing information.
AstraZeneca
| IMFINZI
durvalumab injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| IMFINZI
durvalumab injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - AstraZeneca Pharmaceuticals LP (054743190) |
| Registrant - AstraZeneca PLC (230790719) |