Drug Detail:Ioflupane i-123 (Ioflupane i-123 [ eye-oh-floo-payne ])
Drug Class: Diagnostic radiopharmaceuticals
Highlights of Prescribing Information
IOFLUPANE I 123 injection, for intravenous use
Initial U.S. Approval: 2011
Recent Major Changes
| Indications and Usage (1) | 11/2022 |
| Contraindications (4) | 11/2022 |
| Warnings and Precautions, Radiation Risk (5.3) | 11/2022 |
Indications and Usage for Ioflupane I-123
Ioflupane I 123 Injection is a radioactive diagnostic agent indicated as an adjunct to other diagnostic evaluations for striatal dopamine transporter visualization using single photon emission computed tomography (SPECT) brain imaging in adult patients with:
- suspected Parkinsonian syndromes (PS) or
- suspected dementia with Lewy bodies (DLB). (1)
Ioflupane I-123 Dosage and Administration
- Administer a thyroid-blocking agent at least one hour before the dose of Ioflupane I 123 Injection. (2.2)
- The recommended dose of Ioflupane I 123 Injection in adult patients is 111 MBq to 185 MBq (3 mCi to 5 mCi) administered intravenously over at least 20 seconds. (2.3)
- Measure patient dose using a dose calibrator immediately prior to administration. (2.4)
- Begin SPECT imaging between 3 hours and 6 hours post-injection. (2.6)
Dosage Forms and Strengths
Injection: 185 MBq (5 mCi) in 2.5 mL at a concentration of 74 MBq/mL (2 mCi/mL) of ioflupane I 123 at calibration date and time supplied in single-dose vials. (3)
Contraindications
Known serious hypersensitivity to ioflupane I 123 (4)
Warnings and Precautions
- Hypersensitivity Reactions: Hypersensitivity reactions including dyspnea, edema, rash, erythema, and pruritus have been reported. Have treatment measures available prior to Ioflupane I 123 Injection administration. (5.1)
- Thyroid Accumulation of Iodine-123: Thyroid uptake of iodine-123 may result in an increased long-term risk for thyroid neoplasia. (2.2, 5.2)
- Radiation Risk: Ensure safe handling to minimize radiation exposure to the patient and healthcare providers. Advise patients to hydrate before and after administration and to void frequently after administration. (2.1, 5.3)
Adverse Reactions/Side Effects
The following adverse reactions were reported at ≤1%: headache, nausea, vertigo, dry mouth and dizziness. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact CURIUM US LLC at 1-866-789-2211 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
Amoxapine, amphetamine, armodafinil, benztropine, bupropion, buspirone, cocaine, mazindol, methamphetamine, methylphenidate, modafinil norephedrine, phentermine, phenylpropanolamine, selegiline, sertraline, citalopram and paroxetine may interfere with Ioflupane I 123 Injection imaging. The effects of dopamine agonists and antagonists on Ioflupane I 123 Injection imaging have not been established. (7)
Use In Specific Populations
- Pregnancy: May cause fetal harm. (8.1)
- Lactation: Advise a lactating woman to interrupt breastfeeding and pump and discard breastmilk for at least 6 days after Ioflupane I 123 Injection administration. (8.2)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 12/2022
Related/similar drugs
Lexiscan, glucagon, mannitol, arginine, barium sulfate, Ceretec, DaTscanFull Prescribing Information
1. Indications and Usage for Ioflupane I-123
Ioflupane I 123 Injection is indicated as an adjunct to other diagnostic evaluations for striatal dopamine transporter visualization using single photon emission computed tomography (SPECT) brain imaging in adult patients with:
● suspected Parkinsonian syndromes (PS) or
● suspected dementia with Lewy bodies (DLB).
2. Ioflupane I-123 Dosage and Administration
2.1 Radiation Safety
Ioflupane I 123 Injection emits radiation and must be handled with safety measures to minimize radiation exposure to healthcare providers and patients [see Warnings and Precautions (5.3)]. Radiopharmaceuticals should be used by or under the control of healthcare providers who are qualified by specific training and experienced in the safe use and handling of radionuclides, and whose experience and training have been approved by the appropriate government agency authorized to license the use of radionuclides.
To minimize radiation exposure, encourage hydration prior to and following Ioflupane I 123 Injection administration in order to permit frequent voiding. Encourage the patient to void frequently for the first 48 hours following Ioflupane I 123 Injection administration [see Dosage and Administration (2.5)].
2.2 Thyroid Blockade Before Ioflupane I 123 Injection Administration
Administer Potassium Iodide Oral Solution or Strong Iodine Solution (e.g., Lugol's Solution) equivalent to 100 mg iodide to block uptake of iodine-123 by the patient's thyroid at least one hour before the dose of Ioflupane I 123 Injection [see Warnings and Precautions (5.2)].
2.3 Recommended Dosage
The recommended dose of Ioflupane I 123 Injection in adult patients is 111 MBq to 185 MBq (3 mCi to 5 mCi) administered intravenously over at least 20 seconds.
2.4 Preparation and Administration
- Assess pregnancy status before administering Ioflupane I 123 Injection to a female of reproductive potential [see Use in Specific Populations (8.1)].
- Use aseptic procedures and radiation shielding during preparation and administration.
- Inspect the Ioflupane I 123 Injection vial for particulate matter and discoloration prior to administration and do not use it if the vial contains particulate matter or discoloration.
- Measure patient dose using a dose calibrator immediately prior to administration.
- Discard unused portion.
2.5 Radiation Dosimetry
The estimated radiation absorbed doses to an adult from intravenous injection of Ioflupane I 123 Injection are shown in Table 1. The values are calculated assuming urinary bladder emptying at 4.8-hour intervals and appropriate thyroid blocking (iodine-123 is a known Auger electron emitter).
| ORGAN / TISSUE | ABSORBED DOSE PER UNIT ADMINISTERED ACTIVITY (μGy / MBq) | |
| Adrenals | 12.9 | |
| Brain | 17.8 | |
| Striata | 230 | |
| Breasts | 7.8 | |
| Gallbladder Wall | 26.4 | |
| GI Tract | Esophagus | 10 |
| Stomach Wall | 11.2 | |
| Small Intestine Wall | 21.2 | |
| Colon Wall a | 39.8 | |
| Upper Large Intestine Wall | 38.1 | |
| Lower Large Intestine Wall | 42 | |
| Heart Wall | 12.9 | |
| Kidneys | 10.9 | |
| Liver | 27.9 | |
| Lungs | 41.2 | |
| Muscle | 9.4 | |
| Osteogenic Cells | 28.2 | |
| Ovaries | 16.8 | |
| Pancreas | 13 | |
| Red Marrow | 9.2 | |
| Skin | 6 | |
| Spleen | 10.4 | |
| Testes | 8.5 | |
| Thymus | 10 | |
| Thyroid | 9 | |
| Urinary Bladder Wall | 53.1 | |
| Uterus | 16.1 | |
| Total Body | 11.3 | |
| EFFECTIVE DOSE PER UNIT ADMINISTERED ACTIVITY (µSv/MBq) | 21.3 | |
a The absorbed dose to the colon wall is the mass-weighted sum of the absorbed doses to the upper and lower large intestine walls, Dcolon = 0.57DULI + 0.43DLLI [Publication 80 of the ICRP (International Commission on Radiological Protection); Annals of the ICRP 28 (3). Oxford: Pergamon Press; 1998]
The Effective Dose resulting from a Ioflupane I 123 Injection administration with an administered activity of 185 MBq (5 mCi) is 3.94 mSv in an adult.
2.6 Imaging Instructions
Begin SPECT imaging 3 hours to 6 hours following Ioflupane I 123 Injection administration.
Use a gamma camera fitted with high-resolution collimators and set to a photopeak of 159 keV with a ± 10% energy window. Angular sampling should be at least 120 views over 360 degrees.
Position the patient supine with the head on an off-the-table headrest, use a flexible head restraint such as a strip of tape across the chin or forehead if necessary to help avoid movement, and set a circular orbit for the detector heads with the radius as small as possible (typically 11 cm to 15 cm).
Obtain images with matrix size and zoom factors selected to give a pixel size of 3.5 mm to 4.5 mm. Collect a minimum of 1.5 million counts for optimal images.
2.7 Image Interpretation
Interpret Ioflupane I 123 Injection images visually, based upon the appearance of the striata. Reconstructed pixel size should be between 3.5 mm and 4.5 mm with slices 1 pixel thick. Optimum presentation of the reconstructed images for visual interpretation is transaxial slices parallel to the anterior commissure-posterior commissure (AC-PC) line.
Determine whether an image is normal or abnormal by assessing the extent (as indicated by shape) and intensity of the striatal signal. Image interpretation does not involve integration of the striatal image appearance with clinical signs and/or symptoms.
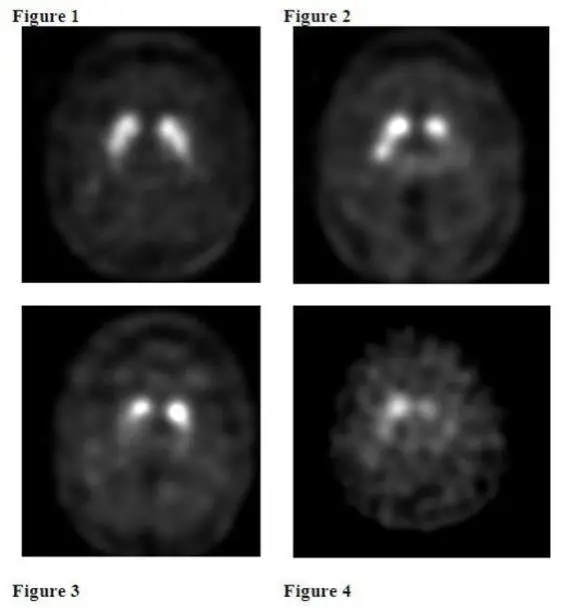
Normal: In transaxial images, normal images are characterized by two symmetric comma- or crescent-shaped focal regions of activity mirrored about the median plane. Striatal activity is distinct, relative to surrounding brain tissue (Figure 1).
Abnormal: Abnormal Ioflupane I 123 Injection images fall into at least one of the following three categories (all are considered abnormal).
- Activity is asymmetric, e.g., activity in the region of the putamen of one hemisphere is absent or greatly reduced with respect to the other. Activity is still visible in the caudate nuclei of both hemispheres resulting in a comma or crescent shape in one and a circular or oval focus in the other. There may be reduced activity between at least one striatum and surrounding tissues (Figure 2).
- Activity is absent in the putamen of both hemispheres and confined to the caudate nuclei. Activity is relatively symmetric and forms two roughly circular or oval foci. Activity of one or both is generally reduced (Figure 3).
- Activity is absent in the putamen of both hemispheres and greatly reduced in one or both caudate nuclei. Activity of the striata with respect to the background is reduced (Figure 4).
3. Dosage Forms and Strengths
Injection: clear, colorless solution containing 185 MBq (5 mCi) in 2.5 mL at a concentration of 74 MBq/mL (2 mCi/mL) of ioflupane I-123 at calibration date and time supplied in single-dose vials.
4. Contraindications
Ioflupane I 123 Injection is contraindicated in patients with known serious hypersensitivity to ioflupane I-123 [see Warnings and Precautions (5.1)].
5. Warnings and Precautions
5.1 Hypersensitivity Reactions
Hypersensitivity reactions, including dyspnea, edema, rash, erythema, and pruritus, have been reported following Ioflupane I 123 Injection administration [see Adverse Reactions (6.2)]. The reactions have generally occurred within minutes of Ioflupane I 123 Injection administration and have either resolved spontaneously or following the administration of corticosteroids and antihistamines.
Ioflupane I 123 Injection is contraindicated in patients with known serious hypersensitivity to ioflupane I-123 [see Contraindications (4)]. Have treatment measures available and monitor patients for symptoms or signs of a hypersensitivity reaction.
5.2 Thyroid Accumulation of Iodine-123
Ioflupane I 123 Injection may contain up to 6% of free iodide (iodine-123). Thyroid uptake of iodine-123 may result in an increased long-term risk for thyroid neoplasia. To decrease thyroid accumulation of iodine-123, block the thyroid gland before administration of Ioflupane I 123 Injection [see Dosage and Administration (2.2)].
5.3 Radiation Risk
Ioflupane I 123 Injection contributes to a patient’s overall long-term cumulative radiation exposure. Long-term cumulative radiation exposure is associated with an increased risk for cancer. Ensure safe handling to minimize radiation exposure to patients and healthcare providers. Advise patients to hydrate before and after administration and to void frequently after administration [see Dosage and Administration (2.1)].
6. Adverse Reactions/Side Effects
The following clinically significant adverse reaction is described elsewhere in the labeling:
• Hypersensitivity Reactions [see Warnings and Precautions (5.1)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of Ioflupane I 123 Injection cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The data from clinical trials reflect exposure to Ioflupane I 123 Injection in 942 subjects with a mean age of 66 years (range 25 years to 90 years). Among these subjects, 42% were female and 99% White. Subjects received 88 MBq to 287 MBq (2 mCi to 8 mCi) [median 173 MBq (4.7 mCi)] intravenously as a single dose. The recommended dose of Ioflupane I 123 Injection is 111 MBq to 185 MBq (3 mCi to 5 mCi) [see Dosage and Administration (2.3)].
The following adverse reactions were reported at a rate of 1% or less: headache, nausea, vertigo, dry mouth, and dizziness.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of Ioflupane I 123 Injection. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Immune system disorders: Hypersensitivity, including dyspnea, edema, rash, erythema, and pruritus
General disorders and administration site conditions: Injection site pain
7. Drug Interactions
Ioflupane I 123 binds to the dopamine transporter [see Clinical Pharmacology (12.1)]. Drugs that bind to the dopamine transporter with high affinity may interfere with the image obtained following Ioflupane I 123 Injection administration. These potentially interfering drugs consist of: amoxapine, amphetamine, armodafinil, benztropine, bupropion, buspirone, cocaine, mazindol, methamphetamine, methylphenidate, modafinil, norephedrine, phentermine, phenylpropanolamine, selegiline, and sertraline. Selective serotonin reuptake inhibitors (paroxetine and citalopram) may increase or decrease ioflupane binding to the dopamine transporter. Whether discontinuation of these drugs prior to Ioflupane I 123 Injection administration may minimize the interference with a Ioflupane I 123 Injection image is unknown.
The impact of dopamine agonists and antagonists upon Ioflupane I 123 Injection imaging results has not been established.
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
Radioactive iodine products cross the placenta and can permanently impair fetal thyroid function. Administration of an appropriate thyroid blocking agent is recommended before use of Ioflupane I 123 Injection in a pregnant woman to protect the woman and fetus from accumulation of iodine-123 [see Dosage and Administration (2.2)].
There are no available data on Ioflupane I 123 Injection use in pregnant women to evaluate for a drug-associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes. Animal reproduction studies have not been conducted with ioflupane I-123. All radiopharmaceuticals have the potential to cause fetal harm depending on the fetal stage of development and the magnitude of the radiation dose. Administration of Ioflupane I 123 Injection at a dose of 185 MBq (5 mCi) results in an absorbed radiation dose to the uterus of 0.3 rad (3.0 mGy). Radiation doses greater than 15 rad (150 mGy) have been associated with congenital anomalies but doses under 5 rad (50 mGy) generally have not. Advise pregnant women of the potential risks of fetal exposure to radiation doses with administration of Ioflupane I 123 Injection.
The estimated background risk of major birth defects and miscarriage for the indicated population(s) is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
8.2 Lactation
Risk Summary
Iodine-123, the radionuclide in Ioflupane I 123 Injection, is present in human milk. There is no information on the effects on the breastfed infant or on milk production. Advise a lactating woman to interrupt breastfeeding and pump and discard breastmilk for at least 6 days (>10 physical half-lives) after Ioflupane I 123 Injection administration in order to minimize radiation exposure to a breastfed infant.
12. Ioflupane I-123 - Clinical Pharmacology
12.1 Mechanism of Action
The active drug substance in Ioflupane I 123 Injection is N-ω-fluoropropyl-2β-carbomethoxy-3β-(4-[123I]iodophenyl)nortropane or ioflupane I-123.
In vitro, ioflupane binds reversibly to the human dopamine transporter (DaT) (Ki = 0.62 nM; IC50 = 0.71 nM). Autoradiography of post-mortem human brain slices exposed to radiolabeled ioflupane shows concentration of the radiolabel in striatum (caudate nucleus and putamen). The specificity of the binding of ioflupane I-125 to dopamine transporter was demonstrated by competition studies with the DaT inhibitor GBR 12909 (a dopamine reuptake inhibitor), the serotonin reuptake inhibitor citalopram, and the norepinephrine reuptake inhibitor desipramine in post-mortem human brain slices exposed to radiolabeled ioflupane. Citalopram reduced binding in the neocortex and thalamus with only minor effects in the striatum. This indicated that the binding in the cortex and thalamus is mainly to the serotonin reuptake sites. Desipramine showed no effect on the level of striatal binding of ioflupane I- 125, but reduced extrastriatal binding by 60 to 85%. The binding of ioflupane I-125 to the striatum was abolished in the presence of high concentrations of GBR 12909, indicating selectivity of ioflupane binding for the pre-synaptic DaT.
Following administration of Ioflupane I 123 Injection to humans, radioactive decay of the iodine-123 emits gamma radiation which can be detected externally using gamma detectors, allowing visualization of the brain striata through SPECT imaging [see Clinical Pharmacology (12.3)].
12.3 Pharmacokinetics
The pharmacokinetics of ioflupane I-123 were studied by monitoring radioactivity following intravenous injection; only 5% of the administered radioactivity remained in whole blood at 5 minutes post-injection. Uptake in the brain reached approximately 7% of injected radioactivity at 10 minutes post-injection and decreased to 3% after 5 hours; striata to background ratios were relatively constant between 3 hours and 6 hours post-injection. About 30% of the whole brain radioactivity was attributed to striatal uptake. By 48 hours post-injection, approximately 60% of the injected radioactivity has been excreted in the urine, with fecal excretion estimated to be approximately 14%.
14. Clinical Studies
14.1 Suspected Parkinsonian Syndromes
The safety and efficacy of Ioflupane I 123 Injection were evaluated in two multicenter, single-arm, open-label studies (Study 1 and Study 2) that enrolled 284 adult patients with suspected PS.
In these studies, Ioflupane I 123 Injection image interpretation was compared to a reference clinical diagnostic standard of "PS" or "non-PS". PS consisted of Parkinson's disease (PD), multiple system atrophy (MSA), and progressive supranuclear palsy (PSP). These conditions have been associated with dopaminergic neurodegeneration and Ioflupane I 123 Injection imaging was not designed to distinguish among the conditions. Among the non-PS population, subjects with a history of the following conditions were included: vascular parkinsonism, psychogenic parkinsonism, essential tremor (ET), various forms of tremor, and other non-PS diagnoses; Ioflupane I 123 Injection imaging was not designed to distinguish among these conditions.
Patients underwent SPECT imaging with a variety of multi-headed cameras or multi-detector single- slice systems 3 to 6 hours after Ioflupane I 123 Injection administration. The Ioflupane I 123 Injection activity in these two clinical studies ranged from 111 MBq to 201 MBq (3 mCi to 5.4 mCi) [median 167.8 MBq (4.5 mCi)]. Readers blinded to clinical information interpreted Ioflupane I 123 Injection imaging as normal or abnormal [see Dosage and Administration (2.7)]. A normal image is inconsistent with clinical conditions associated with PS and an abnormal image is consistent with clinical conditions associated with PS.
Study 1 consisted of 99 patients with early features of Parkinsonism; patients with features suggestive of MSA or PSP were excluded. The baseline clinical diagnoses consisted of: probable PD (44%), possible PD (31%), “benign” PD (6%), possible ET (11%), and other diagnoses (7%). The patients were 44% female, 42% of age 65 years or over, and all were White. Study 1 readers had no other role in patient assessment. The reference clinical diagnostic standard consisted of the clinical diagnoses established by a consensus panel of movement disorder specialists that evaluated data inclusive through 36 months of follow-up.
Study 2 consisted of 185 patients with clinically established diagnosis of PS (PD, MSA, PSP) or ET. The baseline clinical diagnoses consisted of: PD (70%), MSA (10%), PSP (5%), and ET (15%). The patients were 35% female, 48% of age 65 years or over, and 99% were White. Study 2 readers included site investigators. The reference clinical diagnostic standard consisted of the investigator-determined baseline clinical diagnosis.
Table 4 shows the positive percent agreement and negative percent agreement of the Ioflupane I 123 Injection image results with the reference clinical diagnostic standard. Positive percent agreement represents the percent of patients with abnormal Ioflupane I 123 Injection images among all the patients with a clinical diagnostic reference standard of PS. Negative percent agreement represents the percent of patients with normal Ioflupane I 123 Injection images among the patients with a non-PS clinical diagnostic reference standard.
| Positive percent agreement
(95 % CI) | Negative percent agreement
(95 % CI)) |
|
| Study 1 (patients with early signs and/or symptoms of PS) | ||
| Reader A, n = 99 | 77 (66, 87) | 96 (82, 100) |
| Reader B, n = 96 | 78 (66, 87) | 96 (82, 100) |
| Reader C, n = 98 | 79 (67, 87) | 96 (82, 100) |
| Study 2 (patients with established diagnoses of PS or ET) | ||
| Reader A, n = 185 | 93 (88, 97) | 96 (81, 100) |
| Reader B, n = 185 | 97 (93, 99) | 74 (54, 89) |
| Reader C, n = 185 | 96 (92, 99) | 85 (66, 96) |
| Reader D, n = 185 | 92 (87, 96) | 93 (76, 99) |
| Reader E, n = 185 | 94 (90, 97) | 93 (76, 99) |
| IOFLUPANE I 123
ioflupane i-123 injection, solution |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| Labeler - Curium US LLC (079875617) |




![The chemical name for ioflupane I-123 is N-ω-fluoropropyl-2β-carbomethoxy-3β-(4- [123I]iodophenyl)nortropane and it has the following structural formula:](https://cdn.themeditary.com/images/2023/09/08/ioflupane-i-123-02.webp)
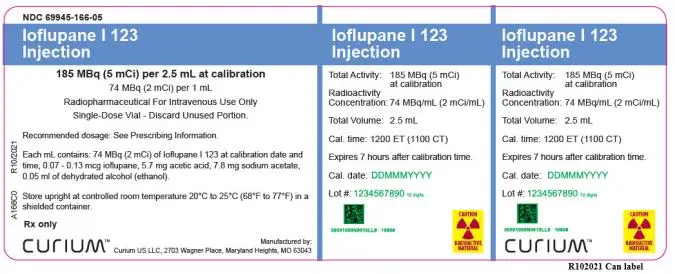
![PRINCIPAL DISPLAY PANEL
NDC 69945-166-05
Ioflupane I 123 Injection
185 MBq (5 mCi) per 2.5 mL at calibration
[74 MBq (2 mCi) per 1 mL]
Radiopharmaceutical - For Intravenous Use Only
Single-Dose Vial – Discard Unused Portion.
Cal. time:
1200 ET (1100 CT)
Cal. date:
Lot #:
Volume: 2.5 mL
Radioactive Concentration:
74 MBq/mL (2 mCi/mL)
Total Activity:
185 MBq (5 mCi)
Recommended Dosage:
See Prescribing Information
Rx only
Store upright at controlled
room temperature 20°C to
25°C (68°F to 77°F) in a
shielded container. Expires
7 hours after calibration time.
Each mL contains 74 MBq
(2 mCi) of Ioflupane I 123 at
calibration, 0.07 - 0.13 mcg
ioflupane, 5.7 mg acetic acid,
7.8 mg sodium acetate,
0.05 mL ethanol.
CAUTION
RADIOACTIVE MATERIAL
Manufactured by:
Curium US LLC
2703 Wagner Place
Maryland Heights, MO
63043
A166V0 R12/2021](https://cdn.themeditary.com/images/2023/09/08/ioflupane-i-123-04.webp)
