Drug Detail:Janumet xr (Metformin and sitagliptin [ met-for-min-and-si-ta-glip-tin ])
Drug Class: Antidiabetic combinations
Highlights of Prescribing Information
JANUMET® XR (sitagliptin and metformin hydrochloride extended-release) tablets, for oral use
Initial U.S. Approval: 2012
WARNING: LACTIC ACIDOSIS
See full prescribing information for complete boxed warning.
- Postmarketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. Symptoms included malaise, myalgias, respiratory distress, somnolence, and abdominal pain. Laboratory abnormalities included elevated blood lactate levels, anion gap acidosis, increased lactate/pyruvate ratio, and metformin plasma levels generally >5 mcg/mL. (5.1)
- Risk factors include renal impairment, concomitant use of certain drugs, age ≥65 years old, radiological studies with contrast, surgery and other procedures, hypoxic states, excessive alcohol intake, and hepatic impairment. Steps to reduce the risk of and manage metformin-associated lactic acidosis in these highrisk groups are provided in the Full Prescribing Information. (5.1)
- If lactic acidosis is suspected, discontinue JANUMET XR and institute general supportive measures in a hospital setting. Prompt hemodialysis is recommended. (5.1)
Indications and Usage for Janumet XR
JANUMET XR is a combination of sitagliptin, a dipeptidyl peptidase-4 (DPP-4) inhibitor, and metformin hydrochloride (HCl), a biguanide indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. (1)
Limitations of Use:
- Not for the treatment of type 1 diabetes. (1)
- Has not been studied in patients with a history of pancreatitis. (1, 5.2)
Janumet XR Dosage and Administration
- Take JANUMET XR orally once daily with a meal. Patients taking two JANUMET XR tablets should take the tablets together. (2.1)
- Individualize the dosage of JANUMET XR on the basis of the patient’s current regimen, effectiveness, and tolerability. (2.1)
- The maximum recommended daily dose is 100 mg of sitagliptin and 2000 mg of metformin HCl extended-release. (2.1)
- The recommended starting dose in patients not currently treated with metformin is 100 mg sitagliptin and 1000 mg metformin HCl once daily, with gradual dose escalation recommended to reduce the gastrointestinal effects due to metformin. (2.1)
- The starting dose in patients already treated with metformin should provide sitagliptin dosed as 100 mg and the dose of metformin already being taken once daily. For patients taking metformin HCl 850 mg twice daily or 1000 mg twice daily, the recommended starting dose of JANUMET XR is two 50 mg sitagliptin and 1000 mg metformin HCl extended-release tablets once daily. (2.1)
- Maintain the same total daily dose of sitagliptin and metformin when changing between JANUMET and JANUMET XR. (2.1)
- Prior to initiation, assess renal function with estimated glomerular filtration rate (eGFR) (2.2)
- Do not use in patients with eGFR below 30 mL/min/1.73 m2.
- Discontinue if eGFR later falls below 30 mL/min/1.73 m2.
- Initiation is not recommended in patients with eGFR between 30 – 45 mL/min/1.73 m2.
- Assess risk/benefit of continuing if eGFR falls below 45 mL/min/1.73 m2.
- Limit dose of sitagliptin to 50 mg once daily if eGFR falls below 45 mL/min/1.73 m2.
- JANUMET XR may need to be discontinued at time of, or prior to, iodinated contrast imaging procedures. (2.3)
Dosage Forms and Strengths
JANUMET XR Tablets:
- sitagliptin 100 mg and metformin HCl 1000 mg extended-release
- sitagliptin 50 mg and metformin HCl 500 mg extended-release
- sitagliptin 50 mg and metformin HCl 1000 mg extended-release (3)
Contraindications
- Severe renal impairment: eGFR below 30 mL/min/1.73 m2. (4)
- Metabolic acidosis, including diabetic ketoacidosis. (4)
- History of a serious hypersensitivity reaction (e.g., anaphylaxis or angioedema) to JANUMET XR, sitagliptin, or metformin. (5.7, 6.2)
Warnings and Precautions
- Lactic Acidosis: See boxed warning. (5.1)
- Pancreatitis: There have been postmarketing reports of acute pancreatitis, including fatal and non-fatal hemorrhagic or necrotizing pancreatitis in patients treated with sitagliptin. If pancreatitis is suspected, promptly discontinue JANUMET XR. (5.2)
- Heart Failure: Has been observed with two other members of the DPP-4 inhibitor class. Consider risks and benefits of JANUMET XR in patients who have known risk factors for heart failure. Monitor patients for signs and symptoms. (5.3)
- Acute Renal Failure: Has been reported postmarketing sometimes requiring dialysis. Before initiating JANUMET XR and at least annually thereafter, assess renal function. (5.4)
- Vitamin B12 Deficiency: Metformin may lower vitamin B12 levels. Measure hematologic parameters annually and vitamin B12 at 2 to 3 year intervals and manage any abnormalities. (5.5)
- Hypoglycemia with Concomitant Use with Insulin or Insulin Secretagogues: Increased risk of hypoglycemia when used in combination with insulin and/or an insulin secretagogue. A lower dose of insulin or insulin secretagogue may be required. (5.6)
- Hypersensitivity Reactions: There have been postmarketing reports of serious allergic and hypersensitivity reactions in patients treated with sitagliptin, such as anaphylaxis, angioedema, and exfoliative skin conditions including Stevens-Johnson syndrome. Promptly stop JANUMET XR, assess for other potential causes, institute appropriate monitoring and treatment. (5.7)
- Severe and Disabling Arthralgia: Has been reported in patients taking DPP-4 inhibitors. Consider as a possible cause for severe joint pain and discontinue drug if appropriate. (5.8)
- Bullous Pemphigoid: There have been postmarketing reports requiring hospitalization in patients taking DPP-4 inhibitors. Tell patients to report development of blisters or erosions. If bullous pemphigoid is suspected, discontinue JANUMET XR. (5.9)
Adverse Reactions/Side Effects
- The most common adverse reactions reported in ≥5% of patients simultaneously started on sitagliptin and metformin and more commonly than in patients treated with placebo were diarrhea, upper respiratory tract infection, and headache. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Merck Sharp & Dohme LLC at 1-877-888-4231 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Carbonic anhydrase inhibitors may increase risk of lactic acidosis. Consider more frequent monitoring. (7)
- Drugs that reduce metformin clearance (such as ranolazine, vandetanib, dolutegravir, and cimetidine) may increase the accumulation of metformin. Consider the benefits and risks of concomitant use. (7)
- Alcohol can potentiate the effect of metformin on lactate metabolism. Warn patients against excessive alcohol intake. (7)
Use In Specific Populations
- Females and Males of Reproductive Potential: Advise premenopausal females of the potential for an unintended pregnancy. (8.3)
- Geriatric Use: Assess renal function more frequently. (8.5)
- Hepatic Impairment: Avoid use in patients with hepatic impairment. (8.7)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 7/2022
Related/similar drugs
metformin, Trulicity, Lantus, Victoza, Tresiba, LevemirFull Prescribing Information
WARNING: LACTIC ACIDOSIS
Postmarketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. The onset of metformin-associated lactic acidosis is often subtle, accompanied only by nonspecific symptoms such as malaise, myalgias, respiratory distress, somnolence, and abdominal pain. Metformin-associated lactic acidosis was characterized by elevated blood lactate levels (>5 mmol/Liter), anion gap acidosis (without evidence of ketonuria or ketonemia), an increased lactate/pyruvate ratio, and metformin plasma levels generally >5 mcg/mL [see Warnings and Precautions (5.1)].
Risk factors for metformin-associated lactic acidosis include renal impairment, concomitant use of certain drugs (e.g., carbonic anhydrase inhibitors such as topiramate), age 65 years old or greater, having a radiological study with contrast, surgery and other procedures, hypoxic states (e.g., acute congestive heart failure), excessive alcohol intake, and hepatic impairment.
Steps to reduce the risk of and manage metformin-associated lactic acidosis in these high risk groups are provided in the full prescribing information [see Dosage and Administration (2.2), Contraindications (4), Warnings and Precautions (5.1), Drug Interactions (7), and Use in Specific Populations (8.6, 8.7)].
If metformin-associated lactic acidosis is suspected, immediately discontinue JANUMET XR and institute general supportive measures in a hospital setting. Prompt hemodialysis is recommended [see Warnings and Precautions (5.1)].
1. Indications and Usage for Janumet XR
JANUMET® XR is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus.
2. Janumet XR Dosage and Administration
2.1 Recommended Dosing
- Take JANUMET XR orally once daily with a meal. Patients taking two JANUMET XR tablets should take the two tablets together once daily.
- Individualize the dosage of JANUMET XR on the basis of the patient’s current regimen, effectiveness, and tolerability.
- The maximum recommended daily dose is 100 mg of sitagliptin and 2000 mg of metformin hydrochloride (HCl) extended-release.
- The recommended starting dose in patients not currently treated with metformin is 100 mg sitagliptin and 1000 mg metformin HCl extended-release once daily, with gradual dose escalation recommended to reduce gastrointestinal side effects associated with metformin.
- The starting dose in patients already treated with metformin should provide 100 mg sitagliptin and the previously prescribed dose of metformin.
- For patients taking metformin HCl immediate-release 850 mg twice daily or 1000 mg twice daily, the recommended starting dose of JANUMET XR is two 50 mg sitagliptin and 1000 mg metformin HCl extended-release tablets taken together once daily.
- Maintain the same total daily dose of sitagliptin and metformin when changing between JANUMET (sitagliptin and metformin HCl immediate-release) and JANUMET XR.
- Do not split, crush or chew JANUMET XR tablets.
2.2 Recommendations for Use in Renal Impairment
- Assess renal function prior to initiation of JANUMET XR and periodically thereafter.
- JANUMET XR is contraindicated in patients with an estimated glomerular filtration rate (eGFR) below 30 mL/min/1.73 m2. Discontinue JANUMET XR if the patient's eGFR later falls below 30 mL/min/1.73 m2 [see Contraindications (4) and Warnings and Precautions (5.1)].
- Initiation of JANUMET XR in patients with an eGFR between 30 and 45 mL/min/1.73 m2 is not recommended.
- In patients taking JANUMET XR whose eGFR later falls below 45 mL/min/1.73 m2, assess the benefit risk of continuing therapy and limit dose of the sitagliptin component to 50 mg once daily.
2.3 Discontinuation for Iodinated Contrast Imaging Procedures
Discontinue JANUMET XR at the time of, or prior to, an iodinated contrast imaging procedure in patients with an eGFR between 30 and 60 mL/min/1.73 m2; in patients with a history of liver disease, alcoholism, or heart failure; or in patients who will be administered intra-arterial iodinated contrast. Re-evaluate eGFR 48 hours after the imaging procedure; restart JANUMET XR if renal function is stable [see Warnings and Precautions (5.1)].
3. Dosage Forms and Strengths
Tablets:
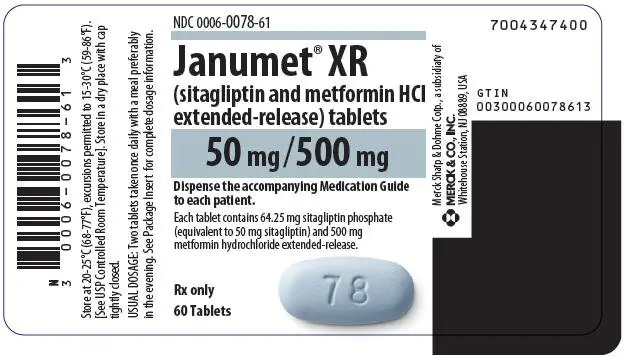
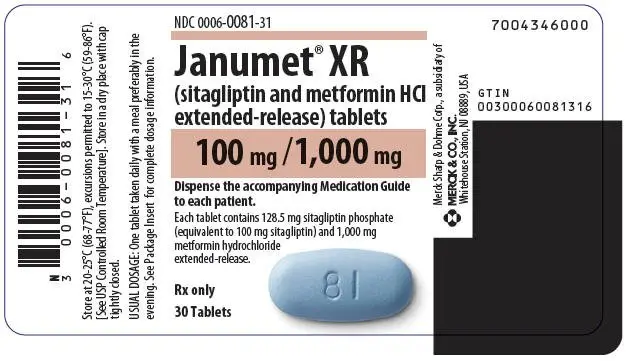
- sitagliptin 100 mg and metformin HCl 1000 mg extended-release tablets are blue, bi-convex oval, film-coated tablets with “81” debossed on one side.
- sitagliptin 50 mg and metformin HCl 500 mg extended-release tablets are light blue, bi-convex oval, film-coated tablets with “78” debossed on one side.
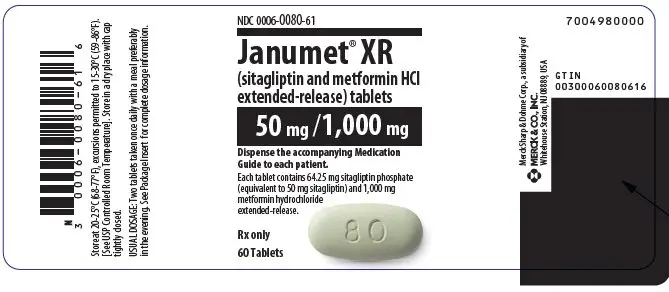
- sitagliptin 50 mg and metformin HCl 1000 mg extended-release tablets are light green, bi-convex oval, film-coated tablets with “80” debossed on one side.
4. Contraindications
JANUMET XR is contraindicated in patients with:
- Severe renal impairment (eGFR below 30 mL/min/1.73 m2) [see Warnings and Precautions (5.1)].
- Acute or chronic metabolic acidosis, including diabetic ketoacidosis.
- History of a serious hypersensitivity reaction to JANUMET XR, sitagliptin, or metformin such as anaphylaxis or angioedema. [See Warnings and Precautions (5.7); Adverse Reactions (6.2).]
5. Warnings and Precautions
5.1 Lactic Acidosis
There have been postmarketing cases of metformin-associated lactic acidosis, including fatal cases. These cases had a subtle onset and were accompanied by nonspecific symptoms such as malaise, myalgias, abdominal pain, respiratory distress, or increased somnolence; however, hypothermia, hypotension and resistant bradyarrhythmias have occurred with severe acidosis. Metformin-associated lactic acidosis was characterized by elevated blood lactate concentrations (>5 mmol/Liter), anion gap acidosis (without evidence of ketonuria or ketonemia), and an increased lactate/pyruvate ratio; metformin plasma levels were generally >5 mcg/mL. Metformin decreases liver uptake of lactate increasing lactate blood levels which may increase the risk of lactic acidosis, especially in patients at risk.
If metformin-associated lactic acidosis is suspected, general supportive measures should be instituted promptly in a hospital setting, along with immediate discontinuation of JANUMET XR. In JANUMET XR-treated patients with a diagnosis or strong suspicion of lactic acidosis, prompt hemodialysis is recommended to correct the acidosis and remove accumulated metformin (metformin is dialyzable, with a clearance of up to 170 mL/min under good hemodynamic conditions). Hemodialysis has often resulted in reversal of symptoms and recovery.
Educate patients and their families about the symptoms of lactic acidosis, and if these symptoms occur instruct them to discontinue JANUMET XR and report these symptoms to their health care provider.
For each of the known and possible risk factors for metformin-associated lactic acidosis, recommendations to reduce the risk of and manage metformin-associated lactic acidosis are provided below:
5.2 Pancreatitis
There have been postmarketing reports of acute pancreatitis, including fatal and non-fatal hemorrhagic or necrotizing pancreatitis, in patients taking sitagliptin with or without metformin. After initiation of JANUMET XR, patients should be observed carefully for signs and symptoms of pancreatitis. If pancreatitis is suspected, JANUMET XR should promptly be discontinued and appropriate management should be initiated. It is unknown whether patients with a history of pancreatitis are at increased risk for the development of pancreatitis while using JANUMET XR.
5.3 Heart Failure
An association between dipeptidyl peptidase-4 (DPP-4) inhibitor treatment and heart failure has been observed in cardiovascular outcomes trials for two other members of the DPP-4 inhibitor class. These trials evaluated patients with type 2 diabetes mellitus and atherosclerotic cardiovascular disease.
Consider the risks and benefits of JANUMET XR prior to initiating treatment in patients at risk for heart failure, such as those with a prior history of heart failure and a history of renal impairment, and observe these patients for signs and symptoms of heart failure during therapy. Advise patients of the characteristic symptoms of heart failure and to immediately report such symptoms. If heart failure develops, evaluate and manage according to current standards of care and consider discontinuation of JANUMET XR.
5.4 Acute Renal Failure
There have been postmarketing reports of worsening renal function in patients taking sitagliptin with or without metformin, including acute renal failure, sometimes requiring dialysis. Before initiation of therapy with JANUMET XR and at least annually thereafter, renal function should be assessed. In patients in whom development of renal dysfunction is anticipated, particularly in elderly patients, renal function should be assessed more frequently and JANUMET XR discontinued if evidence of renal impairment is present. JANUMET XR is contraindicated in patients with severe renal impairment [see Contraindications (4) and Warnings and Precautions (5.1)].
5.5 Vitamin B12 Deficiency
In controlled clinical trials of metformin of 29 weeks duration, a decrease to subnormal levels of previously normal serum vitamin B12 levels was observed in approximately 7% of patients. Such decrease, possibly due to interference with B12 absorption from the B12-intrinsic factor complex, may be associated with anemia but appears to be rapidly reversible with discontinuation of metformin or vitamin B12 supplementation. Certain individuals (those with inadequate vitamin B12 or calcium intake or absorption) appear to be predisposed to developing subnormal vitamin B12 levels. Measure hematologic parameters on an annual basis and vitamin B12 measurements at 2- to 3-year intervals in patients on JANUMET XR and manage any abnormalities [see Adverse Reactions (6.1)].
5.6 Hypoglycemia with Concomitant Use with Insulin or Insulin Secretagogues
JANUMET XR may increase the risk of hypoglycemia when combined with insulin and/or an insulin secretagogue (e.g., sulfonylurea) [see Adverse Reactions (6)]. A lower dose of insulin or insulin secretagogue may be required to minimize the risk of hypoglycemia when used in combination with JANUMET XR [see Drug Interactions (7)].
5.7 Hypersensitivity Reactions
There have been postmarketing reports of serious hypersensitivity reactions in patients treated with sitagliptin, one of the components of JANUMET XR. These reactions include anaphylaxis, angioedema, and exfoliative skin conditions including Stevens-Johnson syndrome. Onset of these reactions occurred within the first 3 months after initiation of treatment with sitagliptin, with some reports occurring after the first dose. If a hypersensitivity reaction is suspected, discontinue JANUMET XR, assess for other potential causes for the event, and institute alternative treatment for diabetes. [See Adverse Reactions (6.2).]
Use caution in a patient with a history of angioedema to another DPP-4 inhibitor because it is unknown whether such patients will be predisposed to angioedema with JANUMET XR.
5.8 Severe and Disabling Arthralgia
There have been postmarketing reports of severe and disabling arthralgia in patients taking DPP-4 inhibitors. The time to onset of symptoms following initiation of drug therapy varied from one day to years. Patients experienced relief of symptoms upon discontinuation of the medication. A subset of patients experienced a recurrence of symptoms when restarting the same drug or a different DPP-4 inhibitor. Consider DPP-4 inhibitors as a possible cause for severe joint pain and discontinue drug if appropriate.
5.9 Bullous Pemphigoid
Postmarketing cases of bullous pemphigoid requiring hospitalization have been reported with DPP-4 inhibitor use. In reported cases, patients typically recovered with topical or systemic immunosuppressive treatment and discontinuation of the DPP-4 inhibitor. Tell patients to report development of blisters or erosions while receiving JANUMET XR. If bullous pemphigoid is suspected, JANUMET XR should be discontinued and referral to a dermatologist should be considered for diagnosis and appropriate treatment.
6. Adverse Reactions/Side Effects
The following adverse reactions are also discussed elsewhere in the labeling:
- Lactic Acidosis [see Warnings and Precautions (5.1)]
- Pancreatitis [see Warnings and Precautions (5.2)]
- Heart Failure [see Warnings and Precautions (5.3)]
- Acute Renal Failure [see Warnings and Precautions (5.4)]
- Vitamin B12 Deficiency [see Warnings and Precautions (5.5)]
- Hypoglycemia with Concomitant Use with Insulin or Insulin Secretagogues [see Warnings and Precautions (5.6)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.7)]
- Severe and Disabling Arthralgia [see Warnings and Precautions (5.8)]
- Bullous Pemphigoid [see Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Sitagliptin and Metformin Immediate-Release Coadministration in Patients with Type 2 Diabetes Inadequately Controlled on Diet and Exercise
Table 1 summarizes the most common (≥5% of patients) adverse reactions reported (regardless of investigator assessment of causality) in a 24-week placebo-controlled factorial study in which sitagliptin and metformin immediate-release were coadministered to patients with type 2 diabetes inadequately controlled on diet and exercise.
| Number of Patients (%) | ||||
|---|---|---|---|---|
|
Placebo |
Sitagliptin 100 mg once daily |
Metformin HCl Immediate-Release 500 mg or 1000 mg twice daily † | Sitagliptin 50 mg twice daily + Metformin HCl Immediate- Release 500 mg or 1000 mg twice daily † |
|
| N = 176 | N = 179 | N = 364† | N = 372† | |
|
||||
| Diarrhea | 7 (4.0) | 5 (2.8) | 28 (7.7) | 28 (7.5) |
| Upper Respiratory Tract Infection | 9 (5.1) | 8 (4.5) | 19 (5.2) | 23 (6.2) |
| Headache | 5 (2.8) | 2 (1.1) | 14 (3.8) | 22 (5.9) |
Gastrointestinal Adverse Reactions
The incidences of pre-selected gastrointestinal adverse experiences in patients treated with sitagliptin and metformin immediate-release were similar to those reported for patients treated with metformin immediate-release alone. See Table 2.
| Number of Patients (%) | ||||||
|---|---|---|---|---|---|---|
| Study of Sitagliptin and Metformin Immediate-Release in Patients Inadequately Controlled on Diet and Exercise | Study of Sitagliptin Add-on in Patients Inadequately Controlled on Metformin Immediate-Release Alone | |||||
|
Placebo |
Sitagliptin 100 mg once daily |
Metformin HCl Immediate-Release 500 mg or 1000 mg twice daily * | Sitagliptin 50 mg bid + Metformin HCl Immediate- Release 500 mg or 1000 mg twice daily * | Placebo and Metformin HCL Immediate- Release ≥1500 mg daily | Sitagliptin 100 mg once daily and Metformin HCl Immediate- Release ≥1500 mg daily |
|
| N = 176 | N = 179 | N = 364 | N = 372 | N = 237 | N = 464 | |
|
||||||
| Diarrhea | 7 (4.0) | 5 (2.8) | 28 (7.7) | 28 (7.5) | 6 (2.5) | 11 (2.4) |
| Nausea | 2 (1.1) | 2 (1.1) | 20 (5.5) | 18 (4.8) | 2 (0.8) | 6 (1.3) |
| Vomiting | 1 (0.6) | 0 (0.0) | 2 (0.5) | 8 (2.2) | 2 (0.8) | 5 (1.1) |
| Abdominal Pain† | 4 (2.3) | 6 (3.4) | 14 (3.8) | 11 (3.0) | 9 (3.8) | 10 (2.2) |
Hypoglycemia
In the above studies (N=5), adverse reactions of hypoglycemia were based on all reports of symptomatic hypoglycemia; a concurrent glucose measurement was not required although most (77%) reports of hypoglycemia were accompanied by a blood glucose measurement ≤70 mg/dL. When the combination of sitagliptin and metformin immediate-release was coadministered with a sulfonylurea or with insulin, the percentage of patients reporting at least one adverse reaction of hypoglycemia was higher than that observed with placebo and metformin immediate-release coadministered with a sulfonylurea or with insulin (Table 3).
|
||
| Add-On to Glimepiride + Metformin Immediate-Release (24 weeks) | Sitagliptin 100 mg + Metformin Immediate-Release + Glimepiride | Placebo + Metformin Immediate-Release + Glimepiride |
| N = 116 | N = 113 | |
| Overall (%) | 19 (16.4) | 1 (0.9) |
| Rate (episodes/patient-year) † | 0.82 | 0.02 |
| Severe (%)‡ | 0 (0.0) | 0 (0.0) |
| Add-On to Insulin + Metformin Immediate-Release (24 weeks) | Sitagliptin 100 mg + Metformin Immediate-Release + Insulin | Placebo + Metformin Immediate-Release + Insulin |
| N = 229 | N = 233 | |
| Overall (%) | 35 (15.3) | 19 (8.2) |
| Rate (episodes/patient-year) † | 0.98 | 0.61 |
| Severe (%)‡ | 1 (0.4) | 1 (0.4) |
The overall incidence of reported adverse reactions of hypoglycemia in patients with type 2 diabetes inadequately controlled on diet and exercise was 0.6% in patients given placebo, 0.6% in patients given sitagliptin alone, 0.8% in patients given metformin immediate-release alone, and 1.6% in patients given sitagliptin in combination with metformin immediate-release. In patients with type 2 diabetes inadequately controlled on metformin immediate-release alone, the overall incidence of adverse reactions of hypoglycemia was 1.3% in patients given add-on sitagliptin and 2.1% in patients given add-on placebo.
In the study of sitagliptin and add-on combination therapy with metformin immediate-release and rosiglitazone, the overall incidence of hypoglycemia was 2.2% in patients given add-on sitagliptin and 0.0% in patients given add-on placebo through Week 18. Through Week 54, the overall incidence of hypoglycemia was 3.9% in patients given add-on sitagliptin and 1.0% in patients given add-on placebo.
In an additional 30-week placebo-controlled study of patients with type 2 diabetes inadequately controlled with metformin comparing the maintenance of sitagliptin 100 mg versus withdrawal of sitagliptin when initiating basal insulin therapy, the event rate and incidence of documented symptomatic hypoglycemia (blood glucose measurement ≤70 mg/dL) did not differ between the sitagliptin and placebo groups.
6.2 Postmarketing Experience
Additional adverse reactions have been identified during postapproval use of sitagliptin with metformin, sitagliptin, or metformin. Because these reactions are reported voluntarily from a population of uncertain size, it is generally not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Hypersensitivity reactions including anaphylaxis, angioedema, rash, urticaria, cutaneous vasculitis, and exfoliative skin conditions including Stevens-Johnson syndrome; upper respiratory tract infection; hepatic enzyme elevations; acute pancreatitis, including fatal and non-fatal hemorrhagic and necrotizing pancreatitis [see Indications and Usage (1)]; worsening renal function, including acute renal failure (sometimes requiring dialysis) and tubulointerstitial nephritis; severe and disabling arthralgia; bullous pemphigoid; constipation; vomiting; headache; myalgia; pain in extremity; back pain; pruritus; mouth ulceration; stomatitis; cholestatic, hepatocellular, and mixed hepatocellular liver injury; rhabdomyolysis.
7. Drug Interactions
Table 4 presents clinically significant drug interactions with JANUMET XR:
| Carbonic Anhydrase Inhibitors | |
|---|---|
| Clinical Impact: | Carbonic anhydrase inhibitors frequently cause a decrease in serum bicarbonate and induce non-anion gap, hyperchloremic metabolic acidosis. Concomitant use of these drugs with JANUMET XR may increase the risk for lactic acidosis. |
| Intervention: | Consider more frequent monitoring of these patients. |
| Examples: | Topiramate, zonisamide, acetazolamide or dichlorphenamide. |
| Drugs that Reduce Metformin Clearance | |
| Clinical Impact: | Concomitant use of drugs that interfere with common renal tubular transport systems involved in the renal elimination of metformin (e.g., organic cationic transporter-2 [OCT2] / multidrug and toxin extrusion [MATE] inhibitors) could increase systemic exposure to metformin and may increase the risk for lactic acidosis [see Clinical Pharmacology (12.3)]. |
| Intervention: | Consider the benefits and risks of concomitant use with JANUMET XR. |
| Examples: | Ranolazine, vandetanib, dolutegravir, and cimetidine. |
| Alcohol | |
| Clinical Impact: | Alcohol is known to potentiate the effect of metformin on lactate metabolism. |
| Intervention: | Warn patients against alcohol intake while receiving JANUMET XR. |
| Insulin Secretagogues or Insulin | |
| Clinical Impact: | Coadministration of JANUMET XR with an insulin secretagogue (e.g., sulfonylurea) or insulin may increase the risk of hypoglycemia. |
| Intervention: | Patients receiving an insulin secretagogue or insulin may require lower doses of the insulin secretagogue or insulin. |
| Drugs Affecting Glycemic Control | |
| Clinical Impact: | Certain drugs tend to produce hyperglycemia and may lead to loss of glycemic control. |
| Intervention: | When such drugs are administered to a patient receiving JANUMET XR, observe the patient closely for loss of blood glucose control. When such drugs are withdrawn from a patient receiving JANUMET XR, observe the patient closely for hypoglycemia. |
| Examples: | Thiazides and other diuretics, corticosteroids, phenothiazines, thyroid products, estrogens, oral contraceptives, phenytoin, nicotinic acid, sympathomimetics, calcium channel blockers, and isoniazid. |
8. Use In Specific Populations
8.3 Females and Males of Reproductive Potential
Discuss the potential for unintended pregnancy with premenopausal women as therapy with metformin may result in ovulation in some anovulatory women.
8.4 Pediatric Use
The safety and effectiveness of JANUMET XR have not been established in pediatric patients.
Three 20-week double-blind, placebo-controlled studies each with 34-week extensions were conducted to evaluate the efficacy and safety of sitagliptin in 410 pediatric patients aged 10 to 17 years with inadequately controlled type 2 diabetes, with or without insulin therapy (HbA1c 6.5-10% for patients not on insulin, HbA1c 7-10% for patients on insulin). At study entry, patients in study 1 were not treated with oral antihyperglycemic agents; patients in studies 2 and 3 were on maximally tolerated metformin therapy. The primary efficacy endpoint was the change from baseline in HbA1c after 20 weeks of therapy. The pre-specified primary efficacy analyses included data from study 1 and pooled data from studies 2 and 3, regardless of glycemic rescue or treatment discontinuation.
In both efficacy analyses, the effect of treatment with sitagliptin was not significantly different from placebo. In study 1, the mean baseline HbA1c was 7.5%, and 12% of patients were on insulin therapy. At week 20, the change from baseline in HbA1c in patients treated with sitagliptin (N=95) was 0.06% compared to 0.23% in patients treated with placebo (N=95), a difference of -0.17% (95% CI: -0.62, 0.28). In studies 2 and 3, the mean baseline HbA1c was 8.0%, 15% of patients were on insulin and 72% were on metformin HCl doses of greater than 1,500 mg daily. At week 20, the change from baseline in HbA1c in patients treated with sitagliptin (N=107) was -0.23% compared to 0.09% in patients treated with placebo (N=113), a difference of -0.33% (95% CI: -0.70, 0.05).
10. Overdosage
In the event of overdose with JANUMET XR, contact the Poison Control Center.
In the event of an overdose, it is reasonable to employ supportive measures, e.g., remove unabsorbed material from the gastrointestinal tract, employ clinical monitoring (including obtaining an electrocardiogram), and institute supportive therapy as indicated by the patient's clinical status.
Sitagliptin is modestly dialyzable. In clinical studies, approximately 13.5% of the dose was removed over a 3- to 4-hour hemodialysis session. Prolonged hemodialysis may be considered if clinically appropriate. It is not known if sitagliptin is dialyzable by peritoneal dialysis.
Overdose of metformin has occurred, including ingestion of amounts greater than 50 grams. Hypoglycemia was reported in approximately 10% of cases, but no causal association with metformin has been established. Lactic acidosis has been reported in approximately 32% of metformin overdose cases [see Warnings and Precautions (5.1)]. Metformin is dialyzable with a clearance of up to 170 mL/min under good hemodynamic conditions. Therefore, hemodialysis may be useful for removal of accumulated drug from patients in whom metformin overdosage is suspected.
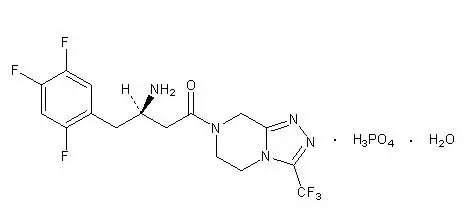
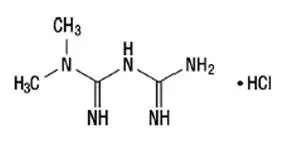
11. Janumet XR Description
JANUMET XR tablets for oral use contain two antihyperglycemic medications: sitagliptin and metformin extended-release.
12. Janumet XR - Clinical Pharmacology
12.3 Pharmacokinetics
JANUMET XR
After administration of two JANUMET XR 50 mg/1000 mg tablets once daily with the evening meal for 7 days in healthy adult subjects, steady-state for sitagliptin and metformin is reached by Day 4 and 5, respectively.
Effect of Food
Food decreases the extent of and slightly delays the absorption of metformin, as shown by approximately a 40% lower mean peak plasma concentration (Cmax), a 25% lower area under the plasma concentration versus time curve (AUC), and a 35-minute prolongation of time to peak plasma concentration (Tmax) following administration of a single 850-mg tablet of metformin HCl with food, compared to the same tablet strength administered fasting. The clinical relevance of these decreases is unknown.
Specific Populations
Patients with Renal Impairment
Patients with Hepatic Impairment
Drug Interaction Studies
JANUMET XR
Coadministration of multiple doses of sitagliptin (50 mg) and metformin HCl (1000 mg) given twice daily did not meaningfully alter the pharmacokinetics of either sitagliptin or metformin in patients with type 2 diabetes.
Pharmacokinetic drug interaction studies with JANUMET XR have not been performed; however, such studies have been conducted with the individual components of JANUMET XR (sitagliptin and metformin extended-release).
Sitagliptin
In Vivo Assessment of Drug Interactions
Effects of Sitagliptin on Other Drugs
In clinical studies, sitagliptin did not meaningfully alter the pharmacokinetics of metformin, glyburide, simvastatin, rosiglitazone, digoxin, warfarin, or an oral contraception (ethinyl estradiol and norethindrone) (Table 5), providing in vivo evidence of a low propensity for causing drug interactions with substrates of CYP3A4, CYP2C8, CYP2C9, P-gp, and organic cationic transporter (OCT).
| Coadministered Drug | Dose of Coadministered Drug* | Dose of Sitagliptin * | Geometric Mean Ratio (ratio with/without sitagliptin) No Effect = 1.00 |
||
|---|---|---|---|---|---|
| AUC† | Cmax | ||||
|
|||||
| Digoxin | 0.25 mg‡ once daily for 10 days | 100 mg‡ once daily for 10 days | Digoxin | 1.11§ | 1.18 |
| Glyburide | 1.25 mg | 200 mg‡ once daily for 6 days | Glyburide | 1.09 | 1.01 |
| Simvastatin | 20 mg | 200 mg‡ once daily for 5 days | Simvastatin | 0.85¶ | 0.80 |
| Simvastatin Acid | 1.12¶ | 1.06 | |||
| Rosiglitazone | 4 mg | 200 mg‡ once daily for 5 days | Rosiglitazone | 0.98 | 0.99 |
| Warfarin | 30 mg single dose on day 5 | 200 mg‡ once daily for 11 days | S(-) Warfarin | 0.95 | 0.89 |
| R(+) Warfarin | 0.99 | 0.89 | |||
| Ethinyl estradiol and norethindrone | 21 days once daily of 35 µg ethinyl estradiol with norethindrone 0.5 mg × 7 days, 0.75 mg × 7 days, 1.0 mg × 7 days | 200 mg‡ once daily for 21 days | Ethinyl estradiol | 0.99 | 0.97 |
| Norethindrone | 1.03 | 0.98 | |||
| Metformin HCl | 1000 mg‡ twice daily for 14 days | 50 mg‡ twice daily for 7 days | Metformin | 1.02# | 0.97 |
Effects of Other Drugs on Sitagliptin
Clinical data described below suggest that sitagliptin is not susceptible to clinically meaningful interactions by coadministered medications (Table 6).
| Coadministered Drug | Dose of Coadministered Drug* | Dose of Sitagliptin* | Geometric Mean Ratio (ratio with/without coadministered drug) No Effect = 1.00 |
||
|---|---|---|---|---|---|
| AUC† | Cmax | ||||
|
|||||
| Cyclosporine | 600 mg once daily | 100 mg once daily | Sitagliptin | 1.29 | 1.68 |
| Metformin HCl | 1000 mg‡ twice daily for 14 days | 50 mg‡ twice daily for 7 days | Sitagliptin | 1.02§ | 1.05 |
14. Clinical Studies
The coadministration of sitagliptin and metformin immediate-release has been studied in patients with type 2 diabetes inadequately controlled on diet and exercise and in combination with other antidiabetic medications.
There have been no clinical efficacy or safety studies conducted with JANUMET XR to characterize its effect on hemoglobin A1c (A1C) reduction. Bioequivalence of JANUMET XR tablets with coadministered sitagliptin and extended-release metformin tablets has been demonstrated for all tablet strengths [see Clinical Pharmacology (12.3)].
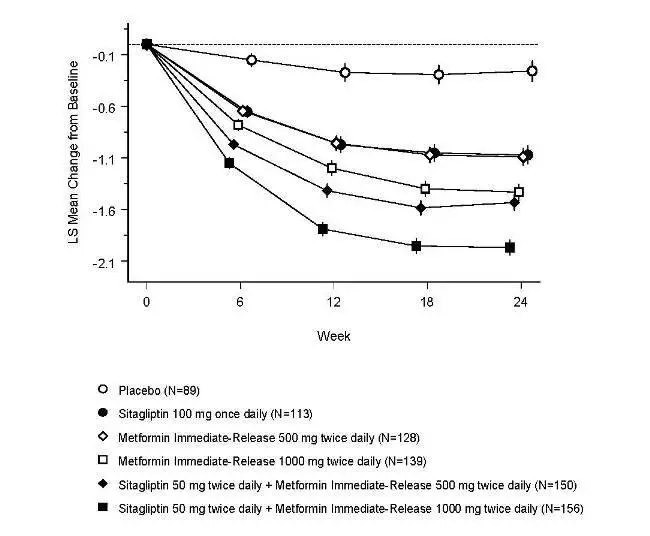
Sitagliptin and Metformin Immediate-Release Coadministration in Patients with Type 2 Diabetes Inadequately Controlled on Diet and Exercise
A total of 1091 patients with type 2 diabetes and inadequate glycemic control on diet and exercise participated in a 24-week, randomized, double-blind, placebo-controlled factorial study designed to assess the efficacy of sitagliptin and metformin immediate-release coadministration. Patients on an antihyperglycemic agent (N=541) underwent a diet, exercise, and drug washout period of up to 12 weeks duration. After the washout period, patients with inadequate glycemic control (A1C 7.5% to 11%) were randomized after completing a 2-week single-blind placebo run-in period. Patients not on antihyperglycemic agents at study entry (N=550) with inadequate glycemic control (A1C 7.5% to 11%) immediately entered the 2-week single-blind placebo run-in period and then were randomized. Approximately equal numbers of patients were randomized to receive placebo, 100 mg of sitagliptin once daily, 500 mg or 1000 mg of metformin HCl immediate-release twice daily, or 50 mg of sitagliptin twice daily in combination with 500 mg or 1000 mg of metformin HCl immediate-release twice daily. Patients who failed to meet specific glycemic goals during the study were treated with glyburide (glibenclamide) rescue.
Sitagliptin and metformin immediate-release coadministration provided significant improvements in A1C, FPG, and 2-hour PPG compared to placebo, to metformin immediate-release alone, and to sitagliptin alone (Table 9, Figure 1). For patients not on an antihyperglycemic agent at study entry, mean reductions from baseline in A1C were: sitagliptin 100 mg once daily, -1.1%; metformin HCl immediate-release 500 mg bid, -1.1%; metformin HCl immediate-release 1000 mg bid, -1.2%; sitagliptin 50 mg bid with metformin HCl immediate-release 500 mg bid, -1.6%; sitagliptin 50 mg bid with metformin HCl immediate-release 1000 mg bid, -1.9%; and for patients receiving placebo, -0.2%. Lipid effects were generally neutral. The decrease in body weight in the groups given sitagliptin in combination with metformin immediate-release was similar to that in the groups given metformin alone or placebo.
|
Placebo |
Sitagliptin 100 mg once daily |
Metformin HCl Immediate-Release 500 mg twice daily |
Metformin HCl Immediate-Release 1000 mg twice daily | Sitagliptin 50 mg bid + Metformin HCl Immediate-Release 500 mg twice daily | Sitagliptin 50 mg bid + Metformin HCl Immediate-Release 1000 mg twice daily |
|
|---|---|---|---|---|---|---|
|
||||||
| A1C (%) | N = 165 | N = 175 | N = 178 | N = 177 | N = 183 | N = 178 |
| Baseline (mean) | 8.7 | 8.9 | 8.9 | 8.7 | 8.8 | 8.8 |
| Change from baseline (adjusted mean†) | 0.2 | -0.7 | -0.8 | -1.1 | -1.4 | -1.9 |
| Difference from placebo (adjusted mean†) (95% CI) | -0.8‡
(-1.1, -0.6) | -1.0‡
(-1.2, -0.8) | -1.3‡
(-1.5, -1.1) | -1.6‡
(-1.8, -1.3) | -2.1‡
(-2.3, -1.8) |
|
| Patients (%) achieving A1C <7% | 15 (9%) | 35 (20%) | 41 (23%) | 68 (38%) | 79 (43%) | 118 (66%) |
| % Patients receiving rescue medication | 32 | 21 | 17 | 12 | 8 | 2 |
| FPG (mg/dL) | N = 169 | N = 178 | N = 179 | N = 179 | N = 183 | N = 180 |
| Baseline (mean) | 196 | 201 | 205 | 197 | 204 | 197 |
| Change from baseline (adjusted mean†) | 6 | -17 | -27 | -29 | -47 | -64 |
| Difference from placebo (adjusted mean†) (95% CI) | -23‡
(-33, -14) | -33‡
(-43, -24) | -35‡
(-45, -26) | -53‡
(-62, -43) | -70‡
(-79, -60) |
|
| 2-hour PPG (mg/dL) | N = 129 | N = 136 | N = 141 | N = 138 | N = 147 | N = 152 |
| Baseline (mean) | 277 | 285 | 293 | 283 | 292 | 287 |
| Change from baseline (adjusted mean†) | 0 | -52 | -53 | -78 | -93 | -117 |
| Difference from placebo (adjusted mean†) (95% CI) | -52‡
(-67, -37) | -54‡
(-69, -39) | -78‡
(-93, -63) | -93‡
(-107, -78) | -117‡
(-131, -102) |
|
|
| Figure 1: Mean Change from Baseline for A1C (%) over 24 Weeks with Sitagliptin and Metformin Immediate-Release, Alone and in Combination in Patients with Type 2 Diabetes Inadequately Controlled with Diet and Exercise* |
 |
Initial combination therapy or maintenance of combination therapy should be individualized and are left to the discretion of the health care provider.
Sitagliptin Add-on Therapy in Patients with Type 2 Diabetes Inadequately Controlled on Metformin Immediate-Release Alone
A total of 701 patients with type 2 diabetes participated in a 24-week, randomized, double-blind, placebo-controlled study designed to assess the efficacy of sitagliptin in combination with metformin immediate-release. Patients already on metformin HCl immediate-release (N=431) at a dose of at least 1500 mg per day were randomized after completing a 2-week, single-blind placebo run-in period. Patients on metformin immediate-release and another antihyperglycemic agent (N=229) and patients not on any antihyperglycemic agents (off therapy for at least 8 weeks, N=41) were randomized after a run-in period of approximately 10 weeks on metformin HCl immediate-release (at a dose of at least 1500 mg per day) in monotherapy. Patients were randomized to the addition of either 100 mg of sitagliptin or placebo, administered once daily. Patients who failed to meet specific glycemic goals during the studies were treated with pioglitazone rescue.
In combination with metformin immediate-release, sitagliptin provided significant improvements in A1C, FPG, and 2-hour PPG compared to placebo with metformin immediate-release (Table 10). Rescue glycemic therapy was used in 5% of patients treated with sitagliptin 100 mg and 14% of patients treated with placebo. A similar decrease in body weight was observed for both treatment groups.
| Sitagliptin 100 mg once daily + Metformin Immediate-Release | Placebo + Metformin Immediate-Release |
|
|---|---|---|
|
||
| A1C (%) | N = 453 | N = 224 |
| Baseline (mean) | 8.0 | 8.0 |
| Change from baseline (adjusted mean†) | -0.7 | -0.0 |
| Difference from placebo + metformin immediate- release (adjusted mean†) (95% CI) | -0.7‡
(-0.8, -0.5) | |
| Patients (%) achieving A1C <7% | 213 (47%) | 41 (18%) |
| FPG (mg/dL) | N = 454 | N = 226 |
| Baseline (mean) | 170 | 174 |
| Change from baseline (adjusted mean†) | -17 | 9 |
| Difference from placebo + metformin immediate- release (adjusted mean†) (95% CI) | -25‡
(-31, -20) | |
| 2-hour PPG (mg/dL) | N = 387 | N = 182 |
| Baseline (mean) | 275 | 272 |
| Change from baseline (adjusted mean†) | -62 | -11 |
| Difference from placebo + metformin immediate- release (adjusted mean†) (95% CI) | -51‡
(-61, -41) | |
Sitagliptin Add-on Therapy in Patients with Type 2 Diabetes Inadequately Controlled on the Combination of Metformin Immediate-Release and Glimepiride
A total of 441 patients with type 2 diabetes participated in a 24-week, randomized, double-blind, placebo-controlled study designed to assess the efficacy of sitagliptin in combination with glimepiride, with or without metformin immediate-release. Patients entered a run-in treatment period on glimepiride (≥4 mg per day) alone or glimepiride in combination with metformin HCl immediate-release (≥1500 mg per day). After a dose-titration and dose-stable run-in period of up to 16 weeks and a 2-week placebo run-in period, patients with inadequate glycemic control (A1C 7.5% to 10.5%) were randomized to the addition of either 100 mg of sitagliptin or placebo, administered once daily. Patients who failed to meet specific glycemic goals during the studies were treated with pioglitazone rescue.
Patients receiving sitagliptin with metformin immediate-release and glimepiride had significant improvements in A1C and FPG compared to patients receiving placebo with metformin immediate-release and glimepiride (Table 11), with mean reductions from baseline relative to placebo in A1C of -0.9% and in FPG of -21 mg/dL. Rescue therapy was used in 8% of patients treated with add-on sitagliptin 100 mg and 29% of patients treated with add-on placebo. The patients treated with add-on sitagliptin had a mean increase in body weight of 1.1 kg vs. add-on placebo (+0.4 kg vs. -0.7 kg). In addition, add-on sitagliptin resulted in an increased rate of hypoglycemia compared to add-on placebo. [See Warnings and Precautions (5.6); Adverse Reactions (6.1).]
| Sitagliptin 100 mg + Metformin Immediate-Release and Glimepiride | Placebo + Metformin Immediate-Release and Glimepiride |
|
|---|---|---|
|
||
| A1C (%) | N = 115 | N = 105 |
| Baseline (mean) | 8.3 | 8.3 |
| Change from baseline (adjusted mean†) | -0.6 | 0.3 |
| Difference from placebo (adjusted mean†) (95% CI) | -0.9‡
(-1.1, -0.7) | |
| Patients (%) achieving A1C <7% | 26 (23%) | 1 (1%) |
| FPG (mg/dL) | N = 115 | N = 109 |
| Baseline (mean) | 179 | 179 |
| Change from baseline (adjusted mean†) | -8 | 13 |
| Difference from placebo (adjusted mean†) (95% CI) | -21‡
(-32, -10) | |
Sitagliptin Add-on Therapy in Patients with Type 2 Diabetes Inadequately Controlled on the Combination of Metformin Immediate-Release and Rosiglitazone
A total of 278 patients with type 2 diabetes participated in a 54-week, randomized, double-blind, placebo-controlled study designed to assess the efficacy of sitagliptin in combination with metformin immediate-release and rosiglitazone. Patients on dual therapy with metformin HCl immediate-release ≥1500 mg/day and rosiglitazone ≥4 mg/day or with metformin HCl immediate-release ≥1500 mg/day and pioglitazone ≥30 mg/day (switched to rosiglitazone ≥4 mg/day) entered a dose-stable run-in period of 6 weeks. Patients on other dual therapy were switched to metformin HCl immediate-release ≥1500 mg/day and rosiglitazone ≥4 mg/day in a dose titration/stabilization run-in period of up to 20 weeks in duration. After the run-in period, patients with inadequate glycemic control (A1C 7.5% to 11%) were randomized 2:1 to the addition of either 100 mg of sitagliptin or placebo, administered once daily. Patients who failed to meet specific glycemic goals during the studies were treated with glipizide (or other sulfonylurea) rescue. The primary time point for evaluation of glycemic parameters was Week 18.
In combination with metformin immediate-release and rosiglitazone, sitagliptin provided significant improvements in A1C, FPG, and 2-hour PPG compared to placebo with metformin immediate-release and rosiglitazone (Table 12) at Week 18. At Week 54, mean reduction in A1C was -1.0% for patients treated with sitagliptin and -0.3% for patients treated with placebo in an analysis based on the intent-to-treat population. Rescue therapy was used in 18% of patients treated with sitagliptin 100 mg and 40% of patients treated with placebo. There was no significant difference between sitagliptin and placebo in body weight change.
| Week 18 | ||
|---|---|---|
| Sitagliptin 100 mg + Metformin Immediate-Release + Rosiglitazone | Placebo + Metformin Immediate-Release + Rosiglitazone |
|
|
||
| A1C (%) | N = 176 | N = 93 |
| Baseline (mean) | 8.8 | 8.7 |
| Change from baseline (adjusted mean†) | -1.0 | -0.4 |
| Difference from placebo + rosiglitazone + metformin immediate-release (adjusted mean†) (95% CI) | -0.7‡
(-0.9, -0.4) | |
| Patients (%) achieving A1C <7% | 39 (22%) | 9 (10%) |
| FPG (mg/dL) | N = 179 | N = 94 |
| Baseline (mean) | 181 | 182 |
| Change from baseline (adjusted mean†) | -30 | -11 |
| Difference from placebo + rosiglitazone + metformin immediate-release (adjusted mean†) (95% CI) | -18‡
(-26, -10) | |
| 2-hour PPG (mg/dL) | N = 152 | N = 80 |
| Baseline (mean) | 256 | 248 |
| Change from baseline (adjusted mean†) | -59 | -21 |
| Difference from placebo + rosiglitazone + metformin immediate-release (adjusted mean†) (95% CI) | -39‡
(-51, -26) | |
Sitagliptin Add-on Therapy in Patients with Type 2 Diabetes Inadequately Controlled on the Combination of Metformin Immediate-Release and Insulin
A total of 641 patients with type 2 diabetes participated in a 24-week, randomized, double-blind, placebo-controlled study designed to assess the efficacy of sitagliptin as add-on to insulin therapy. Approximately 75% of patients were also taking metformin immediate-release. Patients entered a 2-week, single-blind run-in treatment period on pre-mixed, long-acting, or intermediate-acting insulin, with or without metformin HCl immediate-release (≥1500 mg per day). Patients using short-acting insulins were excluded unless the short-acting insulin was administered as part of a pre-mixed insulin. After the run-in period, patients with inadequate glycemic control (A1C 7.5% to 11%) were randomized to the addition of either 100 mg of sitagliptin (N=229) or placebo (N=233), administered once daily. Patients were on a stable dose of insulin prior to enrollment with no changes in insulin dose permitted during the run-in period. Patients who failed to meet specific glycemic goals during the double-blind treatment period were to have uptitration of the background insulin dose as rescue therapy.
Among patients also receiving metformin immediate-release, the median daily insulin (pre-mixed, intermediate or long acting) dose at baseline was 40 units in the sitagliptin-treated patients and 42 units in the placebo-treated patients. The median change from baseline in daily dose of insulin was zero for both groups at the end of the study. Patients receiving sitagliptin with metformin immediate-release and insulin had significant improvements in A1C, FPG and 2-hour PPG compared to patients receiving placebo with metformin immediate-release and insulin (Table 13). The adjusted mean change from baseline in body weight was -0.3 kg in patients receiving sitagliptin with metformin immediate-release and insulin and -0.2 kg in patients receiving placebo with metformin immediate-release and insulin. There was an increased rate of hypoglycemia in patients treated with sitagliptin. [See Warnings and Precautions (5.6); Adverse Reactions (6.1).]
| Sitagliptin 100 mg + Metformin Immediate-Release + Insulin | Placebo + Metformin Immediate-Release + Insulin |
|
|---|---|---|
|
||
| A1C (%) | N = 223 | N = 229 |
| Baseline (mean) | 8.7 | 8.6 |
| Change from baseline (adjusted mean†, ‡) | -0.7 | -0.1 |
| Difference from placebo (adjusted mean†) (95% CI) | -0.5§ (-0.7, -0.4) | |
| Patients (%) achieving A1C <7% | 32 (14%) | 12 (5%) |
| FPG (mg/dL) | N = 225 | N = 229 |
| Baseline (mean) | 173 | 176 |
| Change from baseline (adjusted mean†) | -22 | -4 |
| Difference from placebo (adjusted mean†) (95% CI) | -18§ (-28, -8.4) | |
| 2-hour PPG (mg/dL) | N = 182 | N = 189 |
| Baseline (mean) | 281 | 281 |
| Change from baseline (adjusted mean†) | -39 | 1 |
| Difference from placebo (adjusted mean†) (95% CI) | -40§ (-53, -28) | |
Maintenance of Sitagliptin During Initiation and Titration of Insulin Glargine
A total of 746 patients with type 2 diabetes (mean baseline HbA1C 8.8%, disease duration 10.8 years) participated in a 30-week, randomized, double-blind, placebo-controlled study to assess the efficacy and safety of continuing sitagliptin during the initiation and uptitration of insulin glargine. Patients who were on a stable dose of metformin HCl (≥1500 mg/day) in combination with a DPP-4 inhibitor and/or sulfonylurea but with inadequate glycemic control (A1C 7.5% to 11%) were enrolled in the study. Those on metformin and sitagliptin (100 mg/day) directly entered the double-blind treatment period; those on another DPP-4 inhibitor and/or on a sulfonylurea entered a 4-8 week run-in period in which they were maintained on metformin and switched to sitagliptin (100 mg); other DPP-4 inhibitors and sulfonylureas were discontinued. At randomization patients were randomized either to continue sitagliptin or to discontinue sitagliptin and switch to a matching placebo. On the day of randomization, insulin glargine was initiated at a dose of 10 units subcutaneously in the evening. Patients were instructed to uptitrate their insulin dose in the evening based on fasting blood glucose measurements to achieve a target of 72-100 mg/dL.
At 30 weeks, the mean reduction in A1C was greater in the sitagliptin group than in the placebo group (Table 14). At the end of the trial, 27.3% of patients in the sitagliptin group and 27.3% in the placebo group had a fasting plasma glucose (FPG) in the target range; there was no significant difference in insulin dose between arms.
| Sitagliptin 100 mg+Metformin+ Insulin Glargine | Placebo+Metformin+ Insulin Glargine | |
|---|---|---|
|
||
| A1C (%) | N = 373* | N = 370* |
| Baseline (mean) | 8.8 | 8.8 |
| Week 30 (mean) | 6.9 | 7.3 |
| Change from baseline (adjusted mean)† | -1.9 | -1.4 |
| Difference from placebo (adjusted mean) (95% CI)† | -0.4 (-0.6, -0.3)‡ | |
| Patients (%) with A1C <7% | 202 (54.2%) | 131 (35.4%) |
| FPG (mg/dL) | N = 373* | N = 370* |
| Baseline (mean) | 199 | 201 |
| Week 30 (mean) | 118 | 123 |
| Change from baseline (adjusted mean)† | -81 | -76 |
Sitagliptin Add-on Therapy vs. Glipizide Add-on Therapy in Patients with Type 2 Diabetes Inadequately Controlled on Metformin Immediate-Release
The efficacy of sitagliptin was evaluated in a 52-week, double-blind, glipizide-controlled noninferiority trial in patients with type 2 diabetes. Patients not on treatment or on other antihyperglycemic agents entered a run-in treatment period of up to 12 weeks duration with metformin HCl immediate-release monotherapy (dose of ≥1500 mg per day) which included washout of medications other than metformin immediate-release, if applicable. After the run-in period, those with inadequate glycemic control (A1C 6.5% to 10%) were randomized 1:1 to the addition of sitagliptin 100 mg once daily or glipizide for 52 weeks. Patients receiving glipizide were given an initial dosage of 5 mg/day and then electively titrated over the next 18 weeks to a maximum dosage of 20 mg/day as needed to optimize glycemic control. Thereafter, the glipizide dose was to be kept constant, except for down-titration to prevent hypoglycemia. The mean dose of glipizide after the titration period was 10 mg.
After 52 weeks, sitagliptin and glipizide had similar mean reductions from baseline in A1C in the intent-to-treat analysis (Table 15). These results were consistent with the per protocol analysis (Figure 2). A conclusion in favor of the non-inferiority of sitagliptin to glipizide may be limited to patients with baseline A1C comparable to those included in the study (over 70% of patients had baseline A1C <8% and over 90% had A1C <9%).
| Sitagliptin 100 mg + Metformin Immediate-Release | Glipizide + Metformin Immediate-Release |
|
|---|---|---|
|
||
| A1C (%) | N = 576 | N = 559 |
| Baseline (mean) | 7.7 | 7.6 |
| Change from baseline (adjusted mean†) | -0.5 | -0.6 |
| FPG (mg/dL) | N = 583 | N = 568 |
| Baseline (mean) | 166 | 164 |
| Change from baseline (adjusted mean†) | -8 | -8 |
|
| Figure 2: Mean Change from Baseline for A1C (%) Over 52 Weeks in a Study Comparing Sitagliptin to Glipizide as Add-On Therapy in Patients Inadequately Controlled on Metformin Immediate-Release (Per Protocol Population)* |
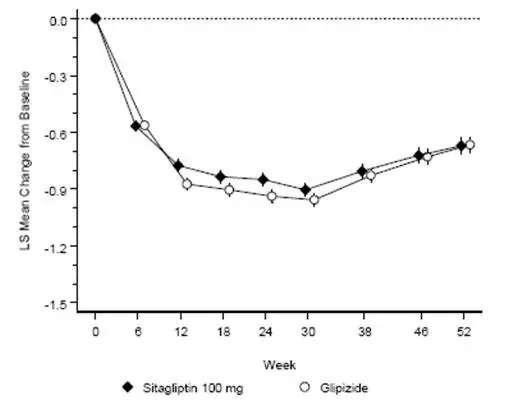 |
The incidence of hypoglycemia in the sitagliptin group (4.9%) was significantly (p<0.001) lower than that in the glipizide group (32.0%). Patients treated with sitagliptin exhibited a significant mean decrease from baseline in body weight compared to a significant weight gain in patients administered glipizide (-1.5 kg vs. +1.1 kg).
16. How is Janumet XR supplied
Tablets supplied as follows:
| Contents | Description | How Supplied | NDC |
|---|---|---|---|
| 50 mg sitagliptin and 500 mg metformin HCl extended-release | light blue, bi-convex oval, film-coated tablets with “78” debossed on one side | unit-of-use bottles of 60 | NDC 0006-0078-61 |
| unit-of-use bottles of 180 | NDC 0006-0078-62 | ||
| bulk bottles of 1000 | NDC 0006-0078-82 | ||
| 50 mg sitagliptin and 1000 mg metformin HCl extended-release | light green, bi-convex oval, film-coated tablets with “80” debossed on one side | unit-of-use bottles of 60 | NDC 0006-0080-61 |
| unit-of-use bottles of 180 | NDC 0006-0080-62 | ||
| bulk bottles of 1000 | NDC 0006-0080-82 | ||
| 100 mg sitagliptin and 1000 mg metformin HCl extended-release | blue, bi-convex oval, film-coated tablets with “81” debossed on one side | unit-of-use bottles of 30 | NDC 0006-0081-31 |
| unit-of-use bottles of 90 | NDC 0006-0081-54 | ||
| bulk bottles of 1000 | NDC 0006-0081-82 |
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised: 07/2022 | |||||
| Medication Guide JANUMET® XR (JAN-you-met XR) (sitagliptin and metformin hydrochloride extended-release) tablets, for oral use |
||||||
| Read this Medication Guide carefully before you start taking JANUMET XR and each time you get a refill. There may be new information. This information does not take the place of talking with your doctor about your medical condition or your treatment. If you have any questions about JANUMET XR, ask your doctor or pharmacist. | ||||||
| What is the most important information I should know about JANUMET XR? JANUMET XR can cause serious side effects, including:
Stop taking JANUMET XR and call your doctor right away if you have any of the following symptoms, which could be signs of lactic acidosis:
Most people who have had lactic acidosis with metformin have other things that, combined with the metformin, led to the lactic acidosis. Tell your doctor if you have any of the following, because you have a higher chance for getting lactic acidosis with JANUMET XR if you:
The best way to keep from having a problem with lactic acidosis from metformin is to tell your doctor if you have any of the problems in the list above. Your doctor may decide to stop your JANUMET XR for a while if you have any of these things. JANUMET XR can have other serious side effects. See "What are the possible side effects of JANUMET XR?"
Before you start taking JANUMET XR, tell your doctor if you have ever had:
Stop taking JANUMET XR and call your doctor right away if you have pain in your stomach area (abdomen) that is severe and will not go away. The pain may be felt going from your abdomen through to your back. The pain may happen with or without vomiting. These may be symptoms of pancreatitis.
|
||||||
What is JANUMET XR?
|
||||||
| Who should not take JANUMET XR? Do not take JANUMET XR if you:
Symptoms of a serious allergic reaction to JANUMET XR may include rash, raised red patches on your skin (hives) or swelling of the face, lips, tongue, and throat that may cause difficulty in breathing or swallowing. |
||||||
| What should I tell my doctor before taking JANUMET XR? Before you take JANUMET XR, tell your doctor about all of your medical conditions, including if you:
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. JANUMET XR may affect the way other medicines work and other medicines may affect how JANUMET XR works. |
||||||
How should I take JANUMET XR?
|
||||||
| What are the possible side effects of JANUMET XR? JANUMET XR may cause serious side effects, including:
|
||||||
|
|
|
|
|
||
The most common side effects of JANUMET XR include: |
||||||
|
|
|
||||
| Taking JANUMET XR with meals can help lessen the common stomach side effects of metformin that usually happen at the beginning of treatment. If you have unusual or sudden stomach problems, talk with your doctor. Stomach problems that start later during treatment may be a sign of something more serious. JANUMET XR may have other side effects, including swelling of the hands or legs. Swelling of the hands and legs can happen if you take JANUMET XR in combination with rosiglitazone (Avandia). Rosiglitazone is another type of diabetes medicine. Tell your doctor if you have any side effect that bothers you or does not go away. These are not all the possible side effects of JANUMET XR. For more information, ask your doctor or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||||||
How should I store JANUMET XR?
|
||||||
| General information about the safe and effective use of JANUMET XR.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use JANUMET XR for a condition for which it was not prescribed. Do not give JANUMET XR to other people, even if they have the same symptoms you have. It may harm them. This Medication Guide summarizes the most important information about JANUMET XR. If you would like to know more information, talk with your doctor. You can ask your doctor or pharmacist for information about JANUMET XR that is written for health professionals. |
||||||
| What are the ingredients in JANUMET XR? Active ingredients: sitagliptin and metformin hydrochloride extended-release Inactive ingredients:
|
||||||
| Dist. by: Merck Sharp & Dohme LLC Rahway, NJ 07065, USA For more information go to www.janumetxr.com or call 1-800-622-4477. For patent information: www.msd.com/research/patent The trademarks depicted herein are owned by their respective companies. Copyright © 2012-2022 Merck & Co., Inc., Rahway, NJ, USA, and its affiliates. All rights reserved. usmg-mk0431a-xrt-2207r011 |
||||||
| JANUMET
XR
sitagliptin and metformin hydrochloride tablet, film coated, extended release |
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
| JANUMET
XR
sitagliptin and metformin hydrochloride tablet, film coated, extended release |
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
| JANUMET
XR
sitagliptin and metformin hydrochloride tablet, film coated, extended release |
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
| Labeler - Merck Sharp & Dohme LLC (118446553) |