Drug Detail:Kazano (Alogliptin and metformin [ al-oh-glip-tin-and-met-for-min ])
Drug Class: Antidiabetic combinations
Highlights of Prescribing Information
KAZANO (alogliptin and metformin hydrochloride) tablets, for oral use
Initial U.S. Approval: 2013
WARNING: LACTIC ACIDOSIS
See full prescribing information for complete boxed warning.
- Postmarketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. Symptoms included malaise, myalgias, respiratory distress, somnolence, and abdominal pain. Laboratory abnormalities included elevated blood lactate levels, anion gap acidosis, increased lactate/pyruvate ratio; and metformin plasma levels generally greater than 5 mcg/mL. (5.1)
- Risk factors include renal impairment, concomitant use of certain drugs, age ≥65 years old, radiological studies with contrast, surgery and other procedures, hypoxic states, excessive alcohol intake, and hepatic impairment. Steps to reduce the risk of and manage metformin-associated lactic acidosis in these high risk groups are provided in the Full Prescribing Information. (5.1)
- If lactic acidosis is suspected, discontinue KAZANO and institute general supportive measures in a hospital setting. Prompt hemodialysis is recommended. (5.1)
Indications and Usage for Kazano
KAZANO is a combination of alogliptin, a dipeptidyl-peptidase-4 (DPP-4) inhibitor and metformin hydrochloride (HCl), a biguanide, indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. (1)
Limitations of Use: Should not be used in patients with type 1 diabetes mellitus. (1)
Kazano Dosage and Administration
- Individualize the starting dosage based on the patient's current regimen. (2.1)
- Given orally twice daily with food. (2.1)
- Adjust the dosage based on effectiveness and tolerability while not exceeding the maximum recommended daily dosage of 25 mg alogliptin and 2000 mg metformin HCl. (2.1)
- Prior to initiation, assess renal function with estimated glomerular filtration rate (eGFR). (2.2)
- Do not use in patients with eGFR below 60 mL/min/1.73 m2.
- KAZANO may need to be discontinued at time of, or prior to, iodinated contrast imaging procedures. (2.3)
Dosage Forms and Strengths
Tablets:12.5 mg alogliptin and 500 mg metformin HCl, 12.5 mg alogliptin and 1000 mg metformin HCl. (3)
Contraindications
- Severe renal impairment: eGFR below 30 mL/min/1.73 m2. (4)
- Metabolic acidosis, including diabetic ketoacidosis. (4)
- History of serious hypersensitivity to alogliptin or metformin, components of KAZANO or any of the excipients. (4)
Warnings and Precautions
- Lactic acidosis: See boxed warning. (5.1)
- Pancreatitis: There have been postmarketing reports of acute pancreatitis. If pancreatitis is suspected, promptly discontinue KAZANO. (5.2)
- Heart failure: Consider the risks and benefits of KAZANO prior to initiating treatment in patients at risk for heart failure. If heart failure develops, evaluate and manage according to current standards of care and consider discontinuation of KAZANO. (5.3)
- Hypersensitivity: There have been postmarketing reports of serious hypersensitivity reactions in patients treated with alogliptin such as anaphylaxis, angioedema and severe cutaneous adverse reactions, including Stevens-Johnson syndrome. If hypersensitivity reactions occur, discontinue KAZANO, treat promptly, and monitor until signs and symptoms resolve. (5.4)
- Hepatic effects: Postmarketing reports of hepatic failure, sometimes fatal. Causality cannot be excluded. If liver injury is detected, promptly interrupt KAZANO and assess patient for probable cause, then treat cause if possible, to resolution or stabilization. Do not restart KAZANO if liver injury is confirmed and no alternative etiology can be found. (5.5)
- Vitamin B12 deficiency: Metformin may lower vitamin B12 levels. Measure hematologic parameters annually and B12 at 2 to 3 year intervals and manage any abnormalties. (5.6)
- Hypoglycemia: Consider lowering the dosage of insulin secretagogue or insulin to reduce the risk of hypoglycemia when initiating KAZANO. (5.7)
- Arthralgia: Severe and disabling arthralgia has been reported in patients taking DPP-4 inhibitors. Consider as a possible cause for severe joint pain and discontinue drug if appropriate. (5.8)
- Bullous pemphigoid: There have been postmarketing reports of bullous pemphigoid requiring hospitalization in patients taking DPP-4 inhibitors. Tell patients to report development of blisters or erosions. If bullous pemphigoid is suspected, discontinue KAZANO. (5.9)
Adverse Reactions/Side Effects
Most common adverse reactions (incidence ≥4%) are upper respiratory tract infection, nasopharyngitis, diarrhea, hypertension, headache, back pain and urinary tract infection. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Takeda Pharmaceuticals America, Inc. at 1-877-TAKEDA-7 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
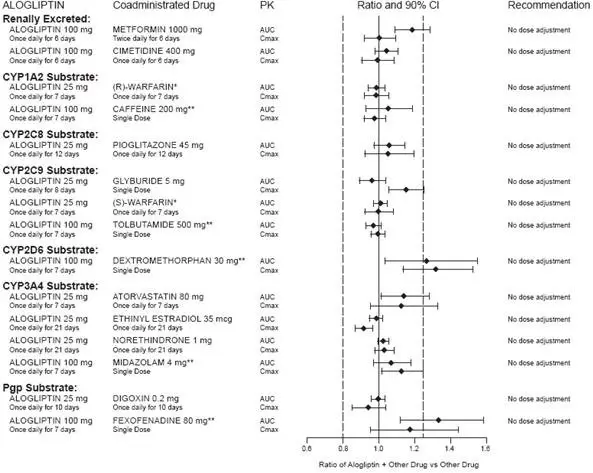
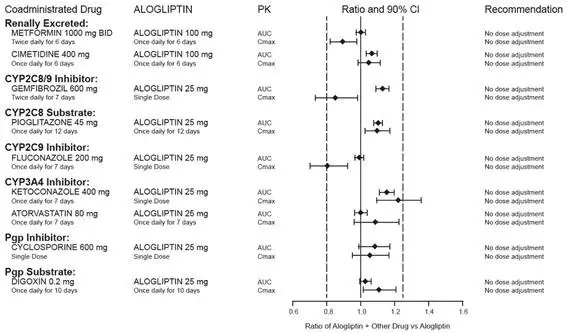
Drug Interactions
- Carbionic anhydrase inhibitors may increase risk of lactic acidosis. Consider more frequent monitoring. (7)
- Drugs that reduce metformin clearance (such as ranolazine, vandetanib, dolutegravir, and cimetidine), may increase the accumulation of metformin. Consider the benefits and risks of concomitant use. (7)
- Alcohol can potentiate the effect of metformin on lactate metabolism. Warn patients against excessive alcohol intake. (7)
Use In Specific Populations
- Females and Males of Reproductive Potential: Advise premenopausal females of the potential for an unintended pregnancy. (8.3)
- Pediatrics: Safety and effectiveness of KAZANO in pediatric patients have not been established. (8.4)
- Geriatric Use: Assess renal function more frequently. (8.5)
- Hepatic Impairment: Avoid use in patients with hepatic impairment. (8.7)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 7/2023
Related/similar drugs
Mounjaro, metformin, Trulicity, Lantus, Victoza, Levemir, TresibaFull Prescribing Information
WARNING: LACTIC ACIDOSIS
Postmarketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. The onset of metformin-associated lactic acidosis is often subtle, accompanied only by nonspecific symptoms such as malaise, myalgias, respiratory distress, somnolence, and abdominal pain. Metformin-associated lactic acidosis was characterized by elevated blood lactate levels (greater than 5 mmol/L), anion gap acidosis (without evidence of ketonuria or ketonemia), an increased lactate/pyruvate ratio; and metformin plasma levels generally greater than 5 mcg/mL [see Warnings and Precautions (5.1)].
Risk factors for metformin-associated lactic acidosis include renal impairment, concomitant use of certain drugs (e.g., carbonic anhydrase inhibitors such as topiramate), age 65 years old or greater, having a radiological study with contrast, surgery and other procedures, hypoxic states (e.g., acute congestive heart failure), excessive alcohol intake, and hepatic impairment.
Steps to reduce the risk of and manage metformin-associated lactic acidosis in these high risk groups are provided in the Full Prescribing Information [see Dosage and Administration (2.2), Contraindications (4), Warnings and Precautions (5.1), Drug Interactions (7), Use in Specific Populations (8.6, 8.7)].
If metformin-associated lactic acidosis is suspected, immediately discontinue KAZANO and institute general supportive measures in a hospital setting. Prompt hemodialysis is recommended [see Warnings and Precautions (5.1)].
1. Indications and Usage for Kazano
KAZANO is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus.
2. Kazano Dosage and Administration
2.1 Recommended Dosage
- Individualize the starting dosage of KAZANO based on the patient's current regimen.
- KAZANO should be taken orally twice daily with food with gradual dose escalation to reduce the gastrointestinal (GI) side effects due to metformin. Do not split tablets.
- Adjust the dosage based on effectiveness and tolerability while not exceeding the maximum recommended daily dose of 25 mg alogliptin and 2000 mg metformin hydrochloride (HCl).
2.2 Recommendations for Use in Renal Impairment
Assess renal function prior to initiation of KAZANO and periodically thereafter.
KAZANO is contraindicated in patients with an estimated glomerular filtration rate (eGFR) below 30 mL/min/1.73 m2 [see Contraindications (4), Warnings and Precautions (5.1)].
KAZANO is not recommended in patients with an eGFR between 30 and 59 mL/min/1.73 m2 because these patients require a lower daily dosage of alogliptin than what is available in the fixed combination KAZANO product.
Kazano requires no dose adjustment in patients with an eGFR of 60 mL/min/1.73 m2 or greater.
2.3 Discontinuation for Iodinated Contrast Imaging Procedures
Discontinue KAZANO at the time of, or prior to, an iodinated contrast imaging procedure in patients with an eGFR between 30 and 60 mL/min/1.73 m2; in patients with a history of liver disease, alcoholism or heart failure; or in patients who will be administered intra-arterial iodinated contrast. Re-evaluate eGFR 48 hours after the imaging procedure; restart KAZANO if renal function is stable [see Warnings and Precautions (5.1)].
3. Dosage Forms and Strengths
- 12.5 mg/500 mg tablets are pale yellow, oblong, film-coated tablets with "12.5/500" debossed on one side and "322M" debossed on the other side
- 12.5 mg/1000 mg tablets are pale yellow, oblong, film-coated tablets with "12.5/1000" debossed on one side and "322M" debossed on the other side
4. Contraindications
KAZANO is contraindicated in patients with:
- Severe renal impairment (eGFR below 30 mL/min/1.73 m2) [see Warnings and Precautions (5.1)].
- Acute or chronic metabolic acidosis, including diabetic ketoacidosis with or without coma.
- History of serious hypersensitivity reaction to alogliptin or metformin or any of the excipients in KAZANO, such as anaphylaxis, angioedema and severe cutaneous adverse reactions [see Warnings and Precautions (5.4), Adverse Reactions (6.2)].
5. Warnings and Precautions
5.2 Pancreatitis
Acute pancreatitis has been reported in the postmarketing setting and in randomized clinical trials. In glycemic control trials in patients with type 2 diabetes mellitus, acute pancreatitis was reported in 6 (0.2%) patients treated with alogliptin 25 mg and 2 (<0.1%) patients treated with active comparators or placebo. In the EXAMINE trial (a cardiovascular outcomes trial of patients with type 2 diabetes mellitus and high cardiovascular (CV) risk), acute pancreatitis was reported in 10 (0.4%) patients treated with alogliptin and in 7 (0.3%) patients treated with placebo.
It is unknown whether patients with a history of pancreatitis are at increased risk for pancreatitis while using KAZANO.
After initiation of KAZANO, patients should be observed for signs and symptoms of pancreatitis. If pancreatitis is suspected, alogliptin should promptly be discontinued and appropriate management should be initiated.
5.3 Heart Failure
In the EXAMINE trial which enrolled patients with type 2 diabetes mellitus and recent acute coronary syndrome, 106 (3.9%) of patients treated with alogliptin and 89 (3.3%) of patients treated with placebo were hospitalized for congestive heart failure.
Consider the risks and benefits of KAZANO prior to initiating treatment in patients at risk for heart failure, such as those with a prior history of heart failure and a history of renal impairment, and observe these patients for signs and symptoms of heart failure during therapy. Patients should be advised of the characteristic symptoms of heart failure and should be instructed to immediately report such symptoms. If heart failure develops, evaluate and manage according to current standards of care and consider discontinuation of KAZANO.
5.4 Hypersensitivity Reactions
There have been postmarketing reports of serious hypersensitivity reactions in patients treated with alogliptin [see Adverse Reactions (6.2)]. These reactions include anaphylaxis, angioedema and severe cutaneous adverse reactions, including Stevens-Johnson syndrome. If a serious hypersensitivity reaction is suspected, discontinue KAZANO, assess for other potential causes for the event and institute alternative treatment for diabetes mellitus. Use caution in patients with a history of angioedema with another dipeptidyl peptidase-4 (DPP-4) inhibitor because it is unknown whether such patients will be predisposed to angioedema with KAZANO.
5.5 Hepatic Effects
There have been postmarketing reports of fatal and nonfatal hepatic failure in patients taking alogliptin, although some of the reports contain insufficient information necessary to establish the probable cause [see Adverse Reactions (6.2)].
In glycemic control trials in patients with type 2 diabetes mellitus, serum alanine aminotransferase (ALT) elevations greater than three times the upper limit of normal (ULN) were reported in 1.3% of patients treated with alogliptin 25 mg and 1.7% of patients treated with active comparators or placebo. In the EXAMINE trial (a cardiovascular outcomes trial of patients with type 2 diabetes mellitus and high cardiovascular (CV) risk), increases in serum alanine aminotransferase three times the upper limit of the reference range occurred in 2.4% of patients treated with alogliptin and in 1.8% of patients treated with placebo.
Measure liver tests promptly in patients who report symptoms that may indicate liver injury, including fatigue, anorexia, right upper abdominal discomfort, dark urine or jaundice. In this clinical context, if the patient is found to have clinically significant liver enzyme elevations and if abnormal liver tests persist or worsen, KAZANO should be interrupted and investigation done to establish the probable cause. KAZANO should not be restarted in these patients without another explanation for the liver test abnormalities.
5.6 Vitamin B12 Levels
In metformin clinical trials of 29 week duration, a decrease to subnormal levels of previously normal serum vitamin B12 levels was observed in approximately 7% of patients. Such decrease, possibly due to interference with B12 absorption from the B12-intrinsic factor complex, may be associated with anemia but appears to be rapidly reversible with discontinuation of metformin or vitamin B12 supplementation. Certain individuals (those with inadequate vitamin B12 or calcium intake or absorption) appear to be predisposed to developing subnormal vitamin B12 levels. Measure hematologic parameters on an annual basis and vitamin B12 at 2 to 3 year intervals in patients on KAZANO and manage any abnormalities [see Adverse Reactions (6.1)].
5.7 Hypoglycemia with Concomitant Use with Insulin or Insulin Secretagogues
Insulin and insulin secretagogues, such as sulfonylureas, are known to cause hypoglycemia. Therefore, a lower dosage of insulin or insulin secretagogue may be required to minimize the risk of hypoglycemia when used in combination with KAZANO.
5.8 Severe and Disabling Arthralgia
There have been postmarketing reports of severe and disabling arthralgia in patients taking DPP-4 inhibitors. The time to onset of symptoms following initiation of drug therapy varied from one day to years. Patients experienced relief of symptoms upon discontinuation of the medication. A subset of patients experienced a recurrence of symptoms when restarting the same drug or a different DPP-4 inhibitor. Consider DPP-4 inhibitors as a possible cause for severe joint pain and discontinue drug if appropriate.
5.9 Bullous Pemphigoid
Postmarketing cases of bullous pemphigoid requiring hospitalization have been reported with DPP-4 inhibitor use. In reported cases, patients typically recovered with topical or systemic immunosuppressive treatment and discontinuation of DPP-4 inhibitor. Tell patients to report development of blisters or erosions while receiving KAZANO. If bullous pemphigoid is suspected, KAZANO should be discontinued and referral to a dermatologist should be considered for diagnosis and appropriate treatment.
6. Adverse Reactions/Side Effects
The following serious adverse reactions are described below or elsewhere in the prescribing information:
- Pancreatitis [see Warnings and Precautions (5.2)]
- Heart Failure [see Warnings and Precautions (5.3)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.4)]
- Hepatic Effects [see Warnings and Precautions (5.5)]
- Severe and Disabling Arthralgia [see Warnings and Precautions (5.8)]
- Bullous Pemphigoid [see Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postmarketing use. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
8. Use In Specific Populations
8.2 Lactation
Data
Published clinical lactation studies report that metformin is present in human milk which resulted in infant doses approximately 0.11% to 1% of the maternal weight-adjusted dosage and a milk/plasma ratio (based on AUC) ranging between 0.13 and 1. However, the studies were not designed to definitely establish the risk of use of metformin during lactation because of small sample size and limited adverse event data collected in infants.
8.3 Females and Males of Reproductive Potential
There is the potential for unintended pregnancy with premenopausal women as therapy with metformin may result in ovulation in some premenopausal anovulatory women.
8.4 Pediatric Use
The safety and effectiveness of KAZANO have not been established in pediatric patients.
Effectiveness of alogliptin was not demonstrated in a 52 week, randomized, double-blind, placebo-controlled trial (NCT02856113) in 151 pediatric patients aged 10 to 17 years with inadequately controlled type 2 diabetes mellitus.
8.6 Renal Impairment
Metformin is substantially excreted by the kidney, and the risk of metformin accumulation and lactic acidosis increases with the degree of renal impairment. KAZANO is contraindicated in severe renal impairment, patients with an eGFR below 30 mL/min/1.73 m2 [see Dosage and Administration (2.2), Contraindications (4), Warnings and Precautions (5.1), Clinical Pharmacology (12.3)].
10. Overdosage
Overdose of metformin has occurred, including ingestion of amounts greater than 50 grams. Hypoglycemia was reported in approximately 10% of cases, but no causal association with metformin has been established. Lactic acidosis has been reported in approximately 32% of metformin overdose cases [see Warnings and Precautions (5.1)].
In the event of an overdose, it is reasonable to institute the necessary clinical monitoring and supportive therapy as dictated by the patient's clinical status. Per clinical judgment, it may be reasonable to initiate removal of unabsorbed material from the gastrointestinal tract.
Alogliptin is minimally dialyzable; over a three-hour hemodialysis session, approximately 7% of the drug was removed. Therefore, hemodialysis is unlikely to be beneficial in an overdose situation. It is not known if alogliptin is dialyzable by peritoneal dialysis.
Metformin is dialyzable with a clearance of up to 170 mL/min under good hemodynamic conditions. Hemodialysis may be useful for removal of accumulated drug from patients in whom metformin overdosage is suspected.
In the event of an overdose, contact the Poison Help Line, (1-800-222-1222) or a medical toxicologist for additional overdosage management recommendations.
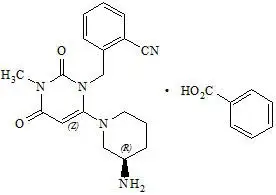
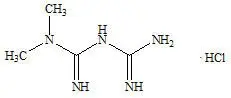
11. Kazano Description
KAZANO tablets contain two oral antihyperglycemic drugs used in the management of type 2 diabetes mellitus: alogliptin and metformin HCl.
12. Kazano - Clinical Pharmacology
12.3 Pharmacokinetics
Specific Populations
14. Clinical Studies
14.1 Overview of Clinical Trials in Adults with Type 2 Diabetes Mellitus
The coadministration of alogliptin and metformin has been studied in patients with type 2 diabetes mellitus inadequately controlled on either diet and exercise alone, on metformin alone or metformin in combination with a thiazolidinedione.
A total of 2,114 patients with type 2 diabetes mellitus were randomized in three double-blind, placebo- or active-controlled clinical safety and efficacy trials conducted to evaluate the effects of alogliptin co-administered with metformin HCl on glycemic control. Among those, 2,095 patients were exposed to the trial medication. The racial distribution of patients exposed to trial medication was 69% White, 16% Asian, 7% Black or African American, 2% American Indian or Alaska Native, 0% Native Hawaiian/Other Pacific Islander and 6% Multiracial or other racial groups. The ethnic distribution was 24% Hispanic or Latino. Patients had an overall mean age of approximately 54.4 years (range 22 to 80 years). In patients with type 2 diabetes mellitus, treatment with alogliptin co-administered with metformin HCl produced clinically meaningful and statistically significant improvements in A1C versus comparator. As is typical for trials of agents to treat type 2 diabetes mellitus, the mean reduction in hemoglobin A1c (A1C) with alogliptin co-administered with metformin HCl appears to be related to the degree of A1C elevation at baseline.
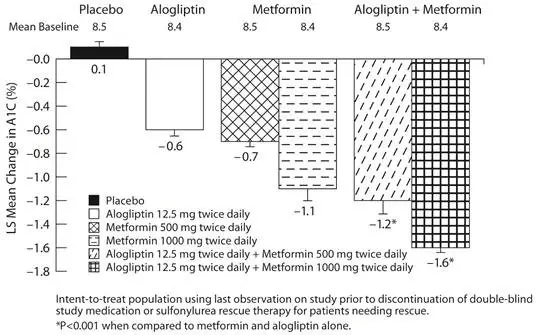
14.2 Alogliptin and Metformin Coadministration in Patients with Type 2 Diabetes Mellitus Inadequately Controlled on Diet and Exercise
In a 26 week, double-blind, placebo-controlled trial, a total of 784 patients inadequately controlled on diet and exercise alone (mean baseline A1C = 8.4%) were randomized to one of seven treatment groups: placebo; metformin HCl 500 mg or metformin HCl 1000 mg twice daily, alogliptin 12.5 mg twice daily, or alogliptin 25 mg daily; alogliptin 12.5 mg in combination with metformin HCl 500 mg or metformin HCl 1000 mg twice daily. Both coadministration treatment arms (alogliptin 12.5 mg + metformin HCl 500 mg and alogliptin 12.5 mg + metformin HCl 1000 mg) resulted in significant improvements in A1C (Figure 3) and FPG when compared with their respective individual alogliptin and metformin component regimens (Table 6). Coadministration treatment arms demonstrated improvements in two-hour postprandial glucose (PPG) compared to alogliptin alone or metformin alone (Table 6). A total of 12% of patients receiving alogliptin 12.5 mg + metformin HCl 500 mg, 3% of patients receiving alogliptin 12.5 mg + metformin HCl 1000 mg, 17% of patients receiving alogliptin 12.5 mg, 23% of patients receiving metformin HCl 500 mg, 11% of patients receiving metformin HCl 1000 mg and 39% of patients receiving placebo required glycemic rescue.
Improvements in A1C were not affected by gender, age, race or baseline BMI. The mean decrease in body weight was similar between metformin alone and alogliptin when co-administered with metformin HCl. Lipid effects were neutral.
| Placebo | Alogliptin 12.5 mg twice daily | Metformin HCl 500 mg twice daily | Metformin HCl 1000 mg twice daily | Alogliptin 12.5 mg + Metformin HCl 500 mg twice daily | Alogliptin 12.5 mg + Metformin HCl 1000 mg twice daily | |
|---|---|---|---|---|---|---|
|
||||||
| A1C (%)* | N=102 | N=104 | N=103 | N=108 | N=102 | N=111 |
| Baseline (mean) | 8.5 | 8.4 | 8.5 | 8.4 | 8.5 | 8.4 |
| Change from baseline (adjusted mean†) | 0.1 | -0.6 | -0.7 | -1.1 | -1.2 | -1.6 |
| Difference from metformin (adjusted mean† with 95% confidence interval) | - | - | - | - | -0.6‡
(-0.9, -0.3) | -0.4‡
(-0.7, -0.2) |
| Difference from alogliptin (adjusted mean† with 95% confidence interval) | - | - | - | - | -0.7‡
(-1.0, -0.4) | -1.0‡
(-1.3, -0.7) |
| % of Patients (n/N) achieving A1C <7%§ | 4% (4/102) | 20% (21/104) | 27% (28/103) | 34% (37/108) | 47%‡
(48/102) | 59%‡
(66/111) |
| FPG (mg/dL)* | N=105 | N=106 | N=106 | N=110 | N=106 | N=112 |
| Baseline (mean) | 187 | 177 | 180 | 181 | 176 | 185 |
| Change from baseline (adjusted mean†) | 12 | -10 | -12 | -32 | -32 | -46 |
| Difference from metformin (adjusted mean† with 95% confidence interval) | - | - | - | - | -20‡
(-33, -8) | -14‡
(-26, -2) |
| Difference from alogliptin (adjusted mean† with 95% confidence interval) | - | - | - | - | -22‡
(-35, -10) | -36‡
(-49, -24) |
| 2-Hour PPG (mg/dL)¶ | N=26 | N=34 | N=28 | N=37 | N=31 | N=37 |
| Baseline (mean) | 263 | 272 | 247 | 266 | 261 | 268 |
| Change from baseline (adjusted mean†) | -21 | -43 | -49 | -54 | -68 | -86‡ |
| Difference from metformin (adjusted mean† with 95% confidence interval) | - | - | - | - | -19 (-49, 11) | -32‡
(-58, -5) |
| Difference from alogliptin (adjusted mean† with 95% confidence interval) | - | - | - | - | -25 (-53, 3) | -43‡
(-70, -16) |
| Figure 3. Change from Baseline A1C at Week 26 with Alogliptin and Metformin Alone and Alogliptin in Combination with Metformin |
 |
14.3 Alogliptin and Metformin Coadministration in Patients with Type 2 Diabetes Mellitus Inadequately Controlled on Metformin Alone
In a 26 week, double-blind, placebo-controlled trial, a total of 527 patients already on metformin (mean baseline A1C = 8%) were randomized to receive alogliptin 12.5 mg, alogliptin 25 mg, or placebo once daily. Patients were maintained on a stable dose of metformin HCl (median daily dose = 1700 mg) during the treatment period. Alogliptin 25 mg in combination with metformin resulted in statistically significant improvements from baseline in A1C and FPG at Week 26, when compared to placebo (Table 7). A total of 8% of patients receiving alogliptin 25 mg and 24% of patients receiving placebo required glycemic rescue. Improvements in A1C were not affected by gender, age, race, baseline BMI or baseline metformin dose.
The mean decrease in body weight was similar between alogliptin 25 mg and placebo when given in combination with metformin. Lipid effects were also neutral.
| Alogliptin 25 mg + Metformin | Placebo + Metformin | |
|---|---|---|
|
||
| A1C (%) | N=203 | N=103 |
| Baseline (mean) | 7.9 | 8.0 |
| Change from baseline (adjusted mean†) | -0.6 | -0.1 |
| Difference from placebo (adjusted mean† with 95% confidence interval) | -0.5‡ (-0.7, -0.3) | ˗ |
| % of patients (n/N) achieving A1C ≤7%‡ | 44% (92/207)‡ | 18% (19/104) |
| FPG (mg/dL) | N=204 | N=104 |
| Baseline (mean) | 172 | 180 |
| Change from baseline (adjusted mean†) | -17 | 0 |
| Difference from placebo (adjusted mean† with 95% confidence interval) | -17‡ (-26, -9) | ˗ |
14.4 Alogliptin Add-On Therapy in Patients with Type 2 Diabetes Mellitus Inadequately Controlled on the Combination of Metformin and Pioglitazone
In a 52 week, active-comparator trial, a total of 803 patients inadequately controlled (mean baseline A1C = 8.2%) on a current regimen of pioglitazone 30 mg and metformin were randomized to either receive the addition of once-daily alogliptin 25 mg or the titration of pioglitazone 30 mg to 45 mg following a four week single-blind, placebo run-in period. Patients were maintained on a stable dose of metformin HCl (median daily dose = 1700 mg). Patients who failed to meet prespecified hyperglycemic goals during the 52 week treatment period received glycemic rescue therapy.
In combination with pioglitazone and metformin, alogliptin 25 mg was shown to be statistically superior in lowering A1C and FPG compared with the titration of pioglitazone from 30 to 45 mg at Week 26 and at Week 52 (Table 8). A total of 11% of patients in the alogliptin 25 mg in combination with pioglitazone 30 mg and metformin treatment group and 22% of patients in the up titration of pioglitazone in combination with metformin treatment group required glycemic rescue. Improvements in A1C were not affected by gender, age, race or baseline BMI.
The mean increase in body weight was similar in both treatment arms. Lipid effects were neutral.
| Alogliptin 25 mg + Pioglitazone 30 mg + Metformin | Pioglitazone 45 mg + Metformin | |
|---|---|---|
|
||
| A1C (%) | N=397 | N=394 |
| Baseline (mean) | 8.2 | 8.1 |
| Change from baseline (adjusted mean†) | -0.7 | -0.3 |
| Difference from pioglitazone 45 mg + metformin* (adjusted mean† with 95% confidence interval) | -0.4‡ (-0.5, -0.3) | - |
| % of Patients (n/N) achieving A1C ≤7% | 33% (134/404)§ | 21% (85/399) |
| Fasting Plasma Glucose (mg/dL)‡ | N=399 | N=396 |
| Baseline (mean) | 162 | 162 |
| Change from baseline (adjusted mean†) | -15 | -4 |
| Difference from pioglitazone 45 mg + metformin (adjusted mean† with 95% confidence interval) | -11§ (-16, -6) | - |
14.5 Cardiovascular Safety Trial
A randomized, double-blind, placebo-controlled cardiovascular outcomes trial (EXAMINE) was conducted to evaluate the cardiovascular risk of alogliptin. The trial compared the risk of major adverse cardiovascular events (MACE) between alogliptin (N=2701) and placebo (N=2679) when added to standard of care therapies for diabetes mellitus and atherosclerotic vascular disease (ASCVD). The trial was event driven and patients were followed until a sufficient number of primary outcome events accrued.
Eligible patients were adults with type 2 diabetes mellitus who had inadequate glycemic control at baseline (e.g., HbA1c >6.5%) and had been hospitalized for an acute coronary syndrome event (e.g., acute myocardial infarction or unstable angina requiring hospitalization) 15 to 90 days prior to randomization. The dose of alogliptin was based on estimated renal function at baseline per dosage and administration recommendations. The average time between an acute coronary syndrome event and randomization was approximately 48 days.
The mean age of the population was 61 years. Most patients were male (68%), White (73%), and were recruited from outside of the United States (86%). Asian and Black or African American patients contributed 20% and 4% of the total population, respectively. At the time of randomization patients had a diagnosis of type 2 diabetes mellitus for approximately 9 years, 87% had a prior myocardial infarction and 14% were current smokers. Hypertension (83%) and renal impairment (27% with an eGFR ≤60 mL/min/1.73 m2) were prevalent co-morbid conditions. Use of medications to treat diabetes mellitus (e.g., metformin 73%, sulfonylurea 54%, insulin 41%), and ASCVD (e.g., statin 94%, aspirin 93%, renin-angiotensin system blocker 88%, beta-blocker 87%) was similar between patients randomized to alogliptin and placebo at baseline. During the trial, medications to treat diabetes mellitus and ASCVD could be adjusted to ensure care for these conditions adhered to standard of care recommendations set by local practice guidelines.
The primary endpoint in EXAMINE was the time to first occurrence of a MACE defined as the composite of cardiovascular death, nonfatal myocardial infarction (MI), or nonfatal stroke. The trial was designed to exclude a pre-specified risk margin of 1.3 for the hazard ratio of MACE. The median exposure to trial drug was 526 days and 95% of the patients were followed to trial completion or death.
Table 9 shows the trial results for the primary MACE composite endpoint and the contribution of each component to the primary MACE endpoint. The upper bound of the confidence interval was 1.16 and excluded a risk margin larger than 1.3.
| Composite of first event of CV death, nonfatal MI or nonfatal stroke (MACE) | Alogliptin | Placebo | Hazard Ratio | ||
|---|---|---|---|---|---|
| Number of Patients (%) | Rate per 100 PY* | Number of Patients (%) | Rate per 100 PY* | (98% CI) | |
| N=2701 | N=2679 | ||||
| 305 (11.3) | 7.6 | 316 (11.8) | 7.9 | 0.96 (0.80, 1.16) | |
|
|||||
| CV Death | 89 (3.3) | 2.2 | 111 (4.1) | 2.8 | |
| Non-fatal MI | 187 (6.9) | 4.6 | 173 (6.5) | 4.3 | |
| Non-fatal stroke | 29 (1.1) | 0.7 | 32 (1.2) | 0.8 | |
The Kaplan-Meier based cumulative event probability is presented in Figure 4 for the time to first occurrence of the primary MACE composite endpoint by treatment arm. The curves for placebo and alogliptin overlap throughout the duration of the trial. The observed incidence of MACE was highest within the first 60 days after randomization in both treatment arms (14.8 MACE per 100 PY), decreased from day 60 to the end of the first year (8.4 per 100 PY) and was lowest after 1 year of follow-up (5.2 per 100 PY).
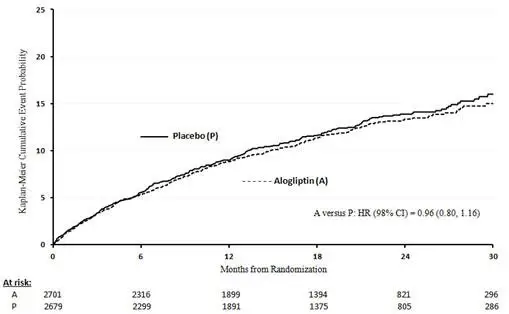 |
The rate of all cause death was similar between treatment arms with 153 (3.6 per 100 PY) recorded among patients randomized to alogliptin and 173 (4.1 per 100 PY) among patients randomized to placebo. A total of 112 deaths (2.9 per 100 PY) among patients on alogliptin and 130 among patients on placebo (3.5 per 100 PY) were adjudicated as cardiovascular deaths.
16. How is Kazano supplied
KAZANO tablets are available in the following strengths and packages:
12.5 mg/500 mg tablet: pale yellow, oblong, film-coated tablets with "12.5/500" debossed on one side and "322M" debossed on the other side, available in:
| NDC 64764-335-60 | Bottles of 60 tablets |
| NDC 64764-335-80 | Bottles of 180 tablets |
| NDC 64764-335-77 | Bottles of 500 tablets |
12.5 mg/1000 mg tablet: pale yellow, oblong, film-coated tablets with "12.5/1000" debossed on one side and "322M" debossed on the other side, available in:
| NDC 64764-337-60 | Bottles of 60 tablets |
| NDC 64764-337-80 | Bottles of 180 tablets |
| NDC 64764-337-77 | Bottles of 500 tablets |
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
| MEDICATION GUIDE KAZANO [Kah-ZAHN-oh] (alogliptin and metformin HCl) tablets |
||||||
|---|---|---|---|---|---|---|
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | ALM143 R14 July 2023 | |||||
| Read this Medication Guide carefully before you start taking KAZANO and each time you get a refill. There may be new information. This information does not take the place of talking with your doctor about your medical condition or treatment. If you have any questions about KAZANO, ask your doctor or pharmacist. | ||||||
| What is the most important information I should know about KAZANO? KAZANO can cause serious side effects, including:
KAZANO can have other serious side effects. See "What are the possible side effects of KAZANO?"
Tell your doctor if you have ever had: |
||||||
|
|
|
||||
Stop taking KAZANO and call your doctor right away if you have pain in your stomach area (abdomen) that is severe and will not go away. The pain may be felt going from your abdomen through to your back. The pain may happen with or without vomiting. These may be symptoms of pancreatitis.
Tell your healthcare provider if you have ever had heart failure or have problems with your kidneys. Contact your healthcare provider right away if you have any of the following symptoms: |
||||||
|
|
|
||||
| These may be symptoms of heart failure. | ||||||
What is KAZANO?
|
||||||
| Who should not take KAZANO? Do not take KAZANO if you:
|
||||||
|
|
|||||
| If you have any of these symptoms, stop taking KAZANO and contact your doctor or go to the nearest hospital emergency room right away. | ||||||
| What should I tell my doctor before and during treatment with KAZANO?
Before you take KAZANO, tell your doctor if you:
KAZANO may affect the way other medicines work, and other medicines may affect how KAZANO works. Contact your doctor before you start or stop other types of medicines. |
||||||
How should I take KAZANO?
|
||||||
| What are the possible side effects of KAZANO? KAZANO can cause serious side effects, including:
|
||||||
|
|
|||||
If you have these symptoms, stop taking KAZANO and contact your doctor right away or go to the nearest hospital emergency room.
|
||||||
|
|
|
||||
|
||||||
|
|
|
|
| ||
|
||||||
|
|
|
||||
| Taking KAZANO with food can help lessen the common stomach side effects of metformin that usually happen at the beginning of treatment. If you have unexplained stomach problems, tell your doctor. Stomach problems that start later, during treatment, may be a sign of something more serious. Tell your doctor if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of KAZANO. For more information, ask your doctor or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||||||
How should I store KAZANO?
|
||||||
| General information about the safe and effective use of KAZANO
Medicines are sometimes prescribed for purposes other than those listed in the Medication Guide. Do not take KAZANO for a condition for which it was not prescribed. Do not give KAZANO to other people, even if they have the same symptoms you have. It may harm them. This Medication Guide summarizes the most important information about KAZANO. If you would like to know more information, talk with your doctor. You can ask your doctor or pharmacist for information about KAZANO that is written for health professionals. For more information go to www.kazano.com or call 1-877-TAKEDA-7 (1-877-825-3327). |
||||||
| What are the ingredients in KAZANO?
Active ingredients: alogliptin and metformin hydrochloride Inactive ingredients: crospovidone, magnesium stearate, mannitol, microcrystalline cellulose, and povidone; the tablets are film-coated with ferric oxide yellow, hypromellose 2910, talc, and titanium dioxide. Distributed by Takeda Pharmaceuticals America, Inc., Lexington, MA 02421. KAZANO and NESINA are trademarks of Takeda Pharmaceutical Company Limited registered with the U.S. Patent and Trademark Office and are used under license by Takeda Pharmaceuticals America, Inc. ©2023 Takeda Pharmaceuticals America, Inc. |
||||||
| KAZANO
alogliptin and metformin hydrochloride tablet, film coated |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| KAZANO
alogliptin and metformin hydrochloride tablet, film coated |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| Labeler - Takeda Pharmaceuticals America, Inc. (039997266) |