Drug Detail:Letairis (Ambrisentan [ am-bri-sen-tan ])
Drug Class: Agents for pulmonary hypertension
Highlights of Prescribing Information
Letairis (ambrisentan) tablets, for oral use
Initial U.S. Approval: 2007
WARNING: EMBRYO-FETAL TOXICITY
See full prescribing information for complete boxed warning.
- Do not administer Letairis to a pregnant female because it may cause fetal harm ( 4.1, 5.1, 8.1).
- Females of reproductive potential: Exclude pregnancy before the start of treatment, monthly during treatment, and 1 month after stopping treatment. Prevent pregnancy during treatment and for one month after stopping treatment by using acceptable methods of contraception ( 2.2, 8.3).
- Because of the risk of embryo-fetal toxicity, for all female patients, Letairis is only available through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the Ambrisentan REMS ( 5.2).
Indications and Usage for Letairis
Letairis is an endothelin receptor antagonist indicated for the treatment of pulmonary arterial hypertension (PAH) (WHO Group 1):
- To improve exercise ability and delay clinical worsening.
- In combination with tadalafil to reduce the risks of disease progression and hospitalization for worsening PAH, and to improve exercise ability.
Studies establishing effectiveness included trials predominantly in patients with WHO Functional Class II–III symptoms and etiologies of idiopathic or heritable PAH (60%) or PAH associated with connective tissue diseases (34%) ( 1).
Letairis Dosage and Administration
- Initiate treatment at 5 mg once daily ( 2.1).
- May be started with tadalafil ( 2.1).
- Titrate at 4-week intervals as needed and tolerated ( 2.1).
- Do not split, crush, or chew tablets ( 2.1).
Dosage Forms and Strengths
Tablet: 5 mg and 10 mg ( 3)
Contraindications
- Pregnancy ( 4.1)
- Idiopathic Pulmonary Fibrosis ( 4.2)
Warnings and Precautions
- Fluid retention may require intervention ( 5.3).
- If patients develop acute pulmonary edema during initiation of therapy with Letairis, consider underlying pulmonary veno-occlusive disease and discontinue treatment if necessary ( 5.4).
- Decreases in sperm count have been observed in patients taking endothelin receptor antagonists ( 5.5).
- Decreases in hemoglobin have been observed within the first few weeks; measure hemoglobin at initiation, at 1 month, and periodically thereafter ( 5.6).
Adverse Reactions/Side Effects
- Most common adverse reactions (>3% compared to placebo) are peripheral edema, nasal congestion, sinusitis, and flushing ( 6.1).
- When used in combination with tadalafil, most common adverse reactions (>5% compared with either monotherapy) are peripheral edema, headache, nasal congestion, cough, anemia, dyspepsia, and bronchitis ( 6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Gilead Sciences, Inc. at (1-800-445-3235, Option 3) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
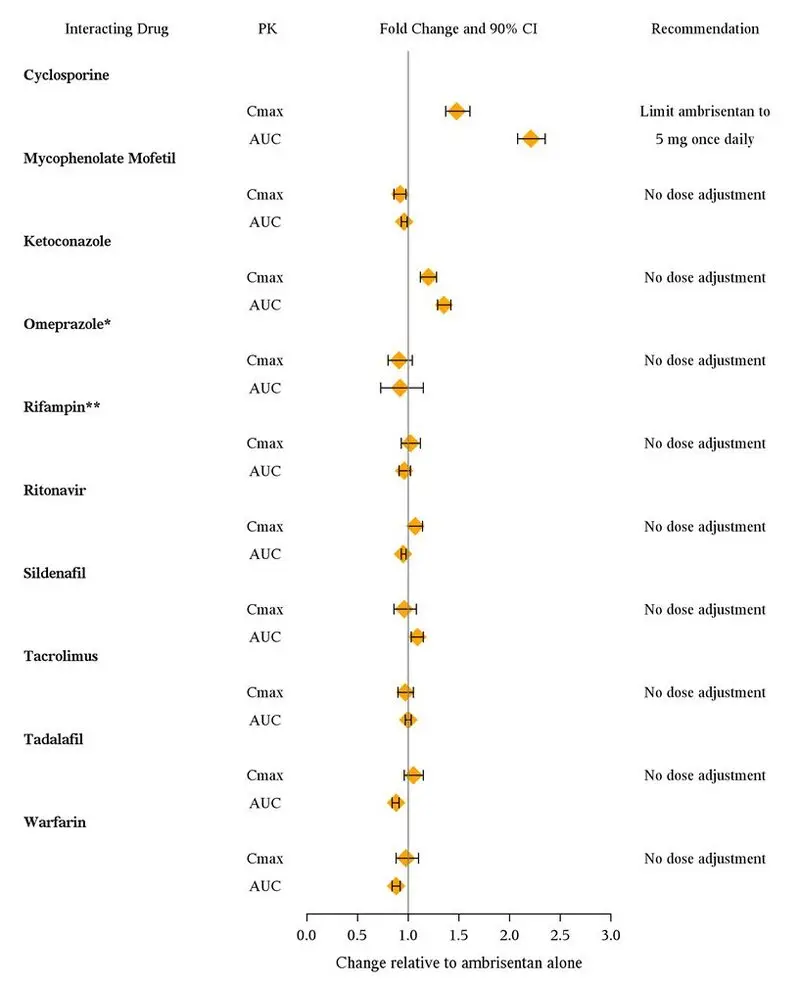
Cyclosporine increases ambrisentan exposure; limit ambrisentan dose to 5 mg once daily ( 7).
Use In Specific Populations
- Breastfeeding: Choose Letairis or breastfeeding ( 8.2).
- Not recommended in patients with moderate or severe hepatic impairment ( 8.7).
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 8/2019
Related/similar drugs
sildenafil, tadalafil, Adcirca, Revatio, Opsumit, ambrisentanFull Prescribing Information
WARNING: EMBRYO-FETAL TOXICITY
Do not administer Letairis to a pregnant female because it may cause fetal harm. Letairis is very likely to produce serious birth defects if used by pregnant females, as this effect has been seen consistently when it is administered to animals [see Contraindications (4.1), Warnings and Precautions (5.1), and Use in Specific Populations (8.1)].
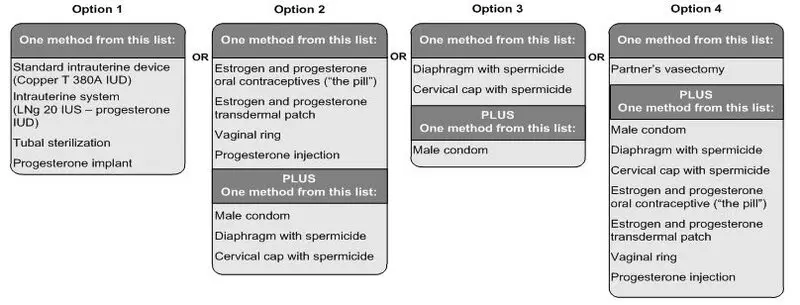
Exclude pregnancy before the initiation of treatment with Letairis. Females of reproductive potential must use acceptable methods of contraception during treatment with Letairis and for one month after treatment. Obtain monthly pregnancy tests during treatment and 1 month after discontinuation of treatment [see Dosage and Administration (2.2) and Use in Specific Populations (8.3)] .
Because of the risk of embryo-fetal toxicity, for all female patients, Letairis is only available through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the Ambrisentan REMS [see Warnings and Precautions (5.2)] .
1. Indications and Usage for Letairis
Letairis is indicated for the treatment of pulmonary arterial hypertension (PAH) (WHO Group 1):
- To improve exercise ability and delay clinical worsening.
- In combination with tadalafil to reduce the risks of disease progression and hospitalization for worsening PAH, and to improve exercise ability [see Clinical Studies (14.2)].
Studies establishing effectiveness included predominantly patients with WHO Functional Class II–III symptoms and etiologies of idiopathic or heritable PAH (60%) or PAH associated with connective tissue diseases (34%).
2. Letairis Dosage and Administration
3. Dosage Forms and Strengths
5 mg and 10 mg film -coated tablets for oral administration
- Each 5 mg tablet is square convex, pale pink, with "5" on one side and "GSI" on the other side.
- Each 10 mg tablet is oval convex, deep pink, with "10" on one side and "GSI" on the other side.
4. Contraindications
4.1 Pregnancy
Letairis may cause fetal harm when administered to a pregnant female. Letairis is contraindicated in females who are pregnant. Letairis was consistently shown to have teratogenic effects when administered to animals. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus [see Warnings and Precautions (5.1, 5.2) and Use in Specific Populations (8.1)] .
5. Warnings and Precautions
5.1 Embryo-fetal Toxicity
Letairis may cause fetal harm when administered during pregnancy and is contraindicated for use in females who are pregnant. In females of reproductive potential, exclude pregnancy prior to initiation of therapy, ensure use of acceptable contraceptive methods, and obtain monthly pregnancy tests [see Dosage and Administration (2.2), and Use in Specific Populations (8.1, 8.3)] .
Letairis is only available for females through a restricted program under a REMS [see Warnings and Precautions (5.2)] .
5.2 Ambrisentan Risk Evaluation and Mitigation Strategy (REMS)
For all females, Letairis is available only through a restricted program under a REMS called the Ambrisentan REMS because of the risk of embryo-fetal toxicity [see Contraindications (4.1), Warnings and Precautions (5.1), and Use in Specific Populations (8.1, 8.3)].
Important requirements of the Ambrisentan REMS include the following:
- Prescribers must be certified with the Ambrisentan REMS by enrolling and completing training.
- All females, regardless of reproductive potential, must enroll in the Ambrisentan REMS prior to initiating Letairis. Male patients are not enrolled in the REMS.
- Females of reproductive potential must comply with the pregnancy testing and contraception requirements [see Use in Specific Populations (8.3)].
- Pharmacies that dispense Letairis must be certified with the Ambrisentan REMS and must dispense to female patients who are authorized to receive Letairis.
Further information is available at www.ambrisentanrems.us.com or 1-888-417-3172.
5.3 Fluid Retention
Peripheral edema is a known class effect of endothelin receptor antagonists, and is also a clinical consequence of PAH and worsening PAH. In the placebo-controlled studies, there was an increased incidence of peripheral edema in patients treated with doses of 5 or 10 mg Letairis compared to placebo [see Adverse Reactions (6.1)] . Most edema was mild to moderate in severity.
In addition, there have been postmarketing reports of fluid retention in patients with pulmonary hypertension, occurring within weeks after starting Letairis. Patients required intervention with a diuretic, fluid management, or, in some cases, hospitalization for decompensating heart failure.
If clinically significant fluid retention develops, with or without associated weight gain, further evaluation should be undertaken to determine the cause, such as Letairis or underlying heart failure, and the possible need for specific treatment or discontinuation of Letairis therapy.
Peripheral edema/fluid retention is more common with Letairis plus tadalafil than with Letairis or tadalafil alone.
5.4 Pulmonary Edema with Pulmonary Veno-occlusive Disease (PVOD)
If patients develop acute pulmonary edema during initiation of therapy with vasodilating agents such as Letairis, the possibility of PVOD should be considered, and if confirmed Letairis should be discontinued.
5.5 Decreased Sperm Counts
Decreased sperm counts have been observed in human and animal studies with another endothelin receptor antagonist and in animal fertility studies with ambrisentan. Letairis may have an adverse effect on spermatogenesis. Counsel patients about potential effects on fertility [see Use in Specific Populations (8.6) and Nonclinical Toxicology (13.1)].
5.6 Hematological Changes
Decreases in hemoglobin concentration and hematocrit have followed administration of other endothelin receptor antagonists and were observed in clinical studies with Letairis. These decreases were observed within the first few weeks of treatment with Letairis, and stabilized thereafter. The mean decrease in hemoglobin from baseline to end of treatment for those patients receiving Letairis in the 12-week placebo-controlled studies was 0.8 g/dL.
Marked decreases in hemoglobin (>15% decrease from baseline resulting in a value below the lower limit of normal) were observed in 7% of all patients receiving Letairis (and 10% of patients receiving 10 mg) compared to 4% of patients receiving placebo. The cause of the decrease in hemoglobin is unknown, but it does not appear to result from hemorrhage or hemolysis.
In the long-term open-label extension of the two pivotal clinical studies, mean decreases from baseline (ranging from 0.9 to 1.2 g/dL) in hemoglobin concentrations persisted for up to 4 years of treatment.
There have been postmarketing reports of decreases in hemoglobin concentration and hematocrit that have resulted in anemia requiring transfusion.
Measure hemoglobin prior to initiation of Letairis, at one month, and periodically thereafter. Initiation of Letairis therapy is not recommended for patients with clinically significant anemia. If a clinically significant decrease in hemoglobin is observed and other causes have been excluded, consider discontinuing Letairis.
6. Adverse Reactions/Side Effects
Clinically significant adverse reactions that appear in other sections of the labeling include:
- Embryo-fetal Toxicity [see Warnings and Precautions (5.1), Use in Specific Populations (8.1)]
- Fluid Retention [see Warnings and Precautions (5.3)]
- Pulmonary Edema with PVOD [see Warnings and Precautions (5.4)]
- Decreased Sperm Count [see Warnings and Precautions (5.5)]
- Hematologic Changes [see Warnings and Precautions (5.6)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Safety data for Letairis are presented from two 12-week, placebo-controlled studies (ARIES-1 and ARIES-2) in patients with pulmonary arterial hypertension (PAH), and one randomized, double-blind, active-controlled trial in 605 patients with PAH (AMBITION) comparing Letairis plus tadalafil to Letairis or tadalafil alone. The exposure to Letairis in these studies ranged from 1 day to 4 years (N=357 for at least 6 months and N=279 for at least 1 year).
In ARIES-1 and ARIES-2, a total of 261 patients received Letairis at doses of 2.5, 5, or 10 mg once daily and 132 patients received placebo. The adverse reactions that occurred in >3% more patients receiving Letairis than receiving placebo are shown in Table 1.
| Placebo
(N=132) | Letairis
(N=261) |
||
|---|---|---|---|
| Adverse Reaction | n (%) | n (%) | Placebo-adjusted (%) |
| Peripheral edema | 14 (11) | 45 (17) | 6 |
| Nasal congestion | 2 (2) | 15 (6) | 4 |
| Sinusitis | 0 (0) | 8 (3) | 3 |
| Flushing | 1 (1) | 10 (4) | 3 |
Most adverse drug reactions were mild to moderate and only nasal congestion was dose-dependent.
Few notable differences in the incidence of adverse reactions were observed for patients by age or sex. Peripheral edema was similar in younger patients (<65 years) receiving Letairis (14%; 29/205) or placebo (13%; 13/104), and was greater in elderly patients (≥65 years) receiving Letairis (29%; 16/56) compared to placebo (4%; 1/28). The results of such subgroup analyses must be interpreted cautiously.
The incidence of treatment discontinuations due to adverse events other than those related to PAH during the clinical trials in patients with PAH was similar for Letairis (2%; 5/261 patients) and placebo (2%; 3/132 patients). The incidence of patients with serious adverse events other than those related to PAH during the clinical trials in patients with PAH was similar for placebo (7%; 9/132 patients) and for Letairis (5%; 13/261 patients).
During 12-week controlled clinical trials, the incidence of aminotransferase elevations >3 × upper limit of normal (ULN) were 0% on Letairis and 2.3% on placebo. In practice, cases of hepatic injury should be carefully evaluated for cause.
Combination Use with Tadalafil
The mean exposure to Letairis + tadalafil in the AMBITION study was 78.7 weeks. The adverse reactions that occurred in >5% more patients receiving Letairis + tadalafil than receiving Letairis or tadalafil monotherapy in AMBITION are shown in Table 2.
| Adverse Reactions | Letairis + Tadalafil Combination Therapy
(N=302) n (%) | Letairis Monotherapy
(N=152) n (%) | Tadalafil Monotherapy
(N=151) n (%) |
|---|---|---|---|
| Peripheral edema | 135 (45%) | 58 (38%) | 43 (28%) |
| Headache | 125 (41%) | 51 (34%) | 53 (35%) |
| Nasal congestion | 58 (19%) | 25 (16%) | 17 (11%) |
| Cough | 53 (18%) | 20 (13%) | 24 (16%) |
| Anemia | 44 (15%) | 11 (7%) | 17 (11%) |
| Dyspepsia | 32 (11%) | 5 (3%) | 18 (12%) |
| Bronchitis | 31 (10%) | 6 (4%) | 13 (9%) |
Peripheral edema was more frequent on combination therapy; however, there was no notable difference observed in the incidence of peripheral edema in elderly patients (≥65 years) versus younger patients (<65 years) on combination therapy (44% vs. 45%) or Letairis monotherapy (37% vs. 39%) in AMBITION.
Treatment discontinuations due to adverse events while on randomized treatment were similar across treatment groups: 16% for Letairis + tadalafil, 14% for Letairis alone, and 13% for tadalafil alone.
6.2 Postmarketing Experience
The following adverse reactions were identified during post-approval use of Letairis. Because these reactions were reported voluntarily from a population of uncertain size, it is not possible to estimate reliably the frequency or to establish a causal relationship to drug exposure: anemia requiring transfusion [see Warnings and Precautions (5.6)] heart failure (associated with fluid retention), symptomatic hypotension, and hypersensitivity (e.g., angioedema, rash).
Elevations of liver aminotransferases (ALT, AST) have been reported with Letairis use; in most cases alternative causes of the liver injury could be identified (heart failure, hepatic congestion, hepatitis, alcohol use, hepatotoxic medications). Other endothelin receptor antagonists have been associated with elevations of aminotransferases, hepatotoxicity, and cases of liver failure [see Adverse Reactions (6.1)].
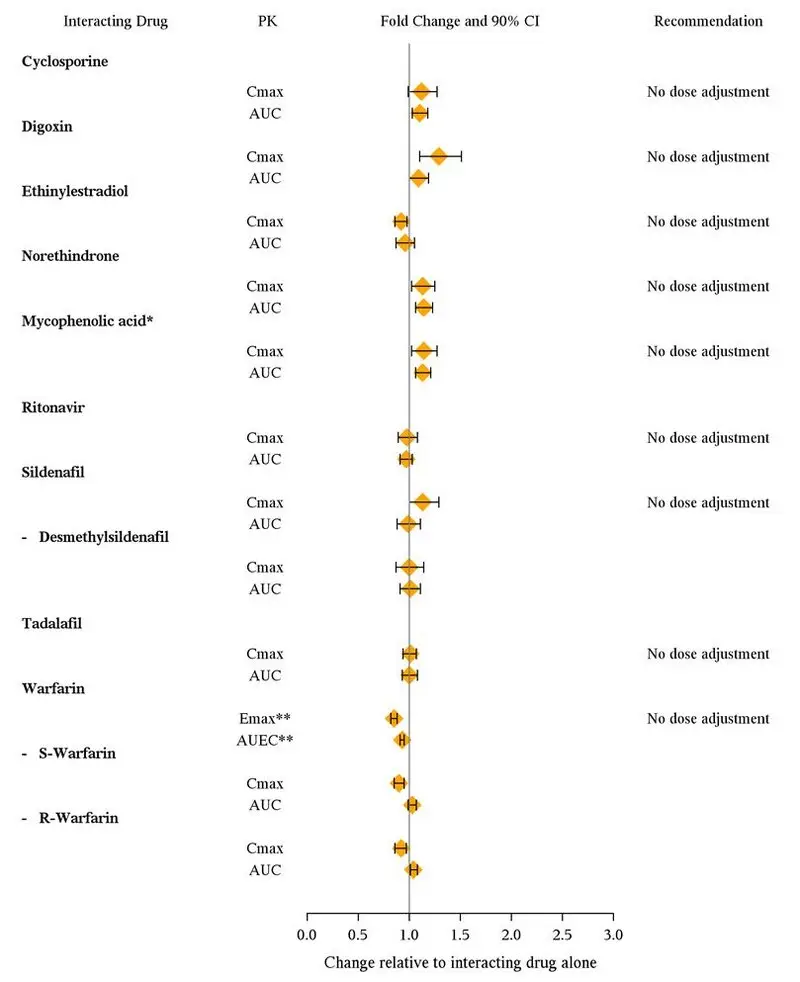
7. Drug Interactions
Multiple dose coadministration of ambrisentan and cyclosporine resulted in an approximately 2-fold increase in ambrisentan exposure in healthy volunteers; therefore, limit the dose of ambrisentan to 5 mg once daily when coadministered with cyclosporine [see Clinical Pharmacology (12.3)] .
8. Use In Specific Populations
8.1 Pregnancy
Data
Animal Data
Letairis was teratogenic at oral dosages of ≥15 mg/kg/day (AUC 51.7 h∙µg/mL) in rats and ≥7 mg/kg/day (24.7 h∙µg/mL) in rabbits; it was not studied at lower dosages. These dosages are of 3.5 and 1.7 times, respectively, the human dose of 10 mg per day (14.8 h∙µg/mL) based on AUC. In both species, there were abnormalities of the lower jaw and hard and soft palate, malformation of the heart and great vessels, and failure of formation of the thymus and thyroid.
A preclinical study in rats has shown decreased survival of newborn pups (mid and high dosages) and effects on testicle size and fertility of pups (high dosage) following maternal treatment with ambrisentan from late gestation through weaning. The mid and high dosages were 51 ×, and 170 × (on a mg/m 2 body surface area basis) the maximum oral human dose of 10 mg and an average adult body weight of 70 kg. These effects were absent at a maternal dosage 17 × the human dose based on mg/m 2.
8.4 Pediatric Use
Safety and effectiveness of Letairis in pediatric patients have not been established .
8.5 Geriatric Use
In the two placebo-controlled clinical studies of Letairis, 21% of patients were ≥65 years old and 5% were ≥75 years old. The elderly (age ≥65 years) showed less improvement in walk distances with Letairis than younger patients did, but the results of such subgroup analyses must be interpreted cautiously. Peripheral edema was more common in the elderly than in younger patients.
8.6 Renal Impairment
The impact of renal impairment on the pharmacokinetics of ambrisentan has been examined using a population pharmacokinetic approach in PAH patients with creatinine clearances ranging between 20 and 150 mL/min. There was no significant impact of mild or moderate renal impairment on exposure to ambrisentan [see Clinical Pharmacology (12.3)] . Dose adjustment of Letairis in patients with mild or moderate renal impairment is therefore not required. There is no information on the exposure to ambrisentan in patients with severe renal impairment.
The impact of hemodialysis on the disposition of ambrisentan has not been investigated.
10. Overdosage
There is no experience with overdosage of Letairis. The highest single dose of Letairis administered to healthy volunteers was 100 mg, and the highest daily dose administered to patients with PAH was 10 mg once daily. In healthy volunteers, single doses of 50 mg and 100 mg (5 to 10 times the maximum recommended dose) were associated with headache, flushing, dizziness, nausea, and nasal congestion. Massive overdosage could potentially result in hypotension that may require intervention.
11. Letairis Description
Letairis is the brand name for ambrisentan, an endothelin receptor antagonist that is selective for the endothelin type-A (ET A) receptor. The chemical name of ambrisentan is (+)-(2 S)-2-[(4,6-dimethylpyrimidin-2-yl)oxy]-3-methoxy-3,3-diphenylpropanoic acid. It has a molecular formula of C 22H 22N 2O 4 and a molecular weight of 378.42. It contains a single chiral center determined to be the ( S) configuration and has the following structural formula:
Figure 1 Ambrisentan Structural Formula
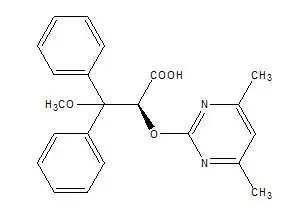
Ambrisentan is a white to off-white, crystalline solid. It is a carboxylic acid with a pKa of 4.0. Ambrisentan is practically insoluble in water and in aqueous solutions at low pH. Solubility increases in aqueous solutions at higher pH. In the solid state ambrisentan is very stable, is not hygroscopic, and is not light sensitive.
Letairis is available as 5 mg and 10 mg film-coated tablets for once daily oral administration. The tablets include the following inactive ingredients: croscarmellose sodium, lactose monohydrate, magnesium stearate and microcrystalline cellulose. The tablets are film-coated with a coating material containing FD&C Red #40 aluminum lake, lecithin, polyethylene glycol, polyvinyl alcohol, talc, and titanium dioxide. Each square, pale pink Letairis tablet contains 5 mg of ambrisentan. Each oval, deep pink Letairis tablet contains 10 mg of ambrisentan. Letairis tablets are unscored.
12. Letairis - Clinical Pharmacology
12.1 Mechanism of Action
Endothelin-1 (ET-1) is a potent autocrine and paracrine peptide. Two receptor subtypes, ET A and ET B, mediate the effects of ET-1 in the vascular smooth muscle and endothelium. The primary actions of ET A are vasoconstriction and cell proliferation, while the predominant actions of ET B are vasodilation, antiproliferation, and ET-1 clearance.
In patients with PAH, plasma ET-1 concentrations are increased as much as 10-fold and correlate with increased mean right atrial pressure and disease severity. ET-1 and ET-1 mRNA concentrations are increased as much as 9-fold in the lung tissue of patients with PAH, primarily in the endothelium of pulmonary arteries. These findings suggest that ET-1 may play a critical role in the pathogenesis and progression of PAH.
Ambrisentan is a high-affinity (K i=0.011 nM) ET A receptor antagonist with a high selectivity for the ET A versus ET B receptor (>4000-fold). The clinical impact of high selectivity for ET A is not known.
12.3 Pharmacokinetics
The pharmacokinetics of ambrisentan (S-ambrisentan) in healthy subjects is dose proportional. The absolute bioavailability of ambrisentan is not known. Ambrisentan is absorbed with peak concentrations occurring approximately 2 hours after oral administration in healthy subjects and PAH patients. Food does not affect its bioavailability. In vitro studies indicate that ambrisentan is a substrate of P-gp. Ambrisentan is highly bound to plasma proteins (99%). The elimination of ambrisentan is predominantly by non-renal pathways, but the relative contributions of metabolism and biliary elimination have not been well characterized. In plasma, the AUC of 4-hydroxymethyl ambrisentan accounts for approximately 4% relative to parent ambrisentan AUC. The in vivo inversion of S-ambrisentan to R-ambrisentan is negligible. The mean oral clearance of ambrisentan is 38 mL/min and 19 mL/min in healthy subjects and in PAH patients, respectively. Although ambrisentan has a 15-hour terminal half-life, the mean trough concentration of ambrisentan at steady-state is about 15% of the mean peak concentration and the accumulation factor is about 1.2 after long-term daily dosing, indicating that the effective half-life of ambrisentan is about 9 hours.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Oral carcinogenicity studies of up to two years duration were conducted at starting doses of 10, 30, and 60 mg/kg/day in rats (8 to 48 times the maximum recommended human dose [MRHD] on a mg/m 2 basis) and at 50, 150, and 250 mg/kg/day in mice (28 to 140 times the MRHD). In the rat study, the high- and mid-dose male and female groups had their doses lowered to 40 and 20 mg/kg/day, respectively, in week 51 because of effects on survival. The high-dose males and females were taken off drug completely in weeks 69 and 93, respectively. The only evidence of ambrisentan-related carcinogenicity was a positive trend in male rats, for the combined incidence of benign basal cell tumor and basal cell carcinoma of skin/subcutis in the mid-dose group (high-dose group excluded from analysis), and the occurrence of mammary fibroadenomas in males in the high-dose group. In the mouse study, high-dose male and female groups had their doses lowered to 150 mg/kg/day in week 39 and were taken off drug completely in week 96 (males) or week 76 (females). In mice, ambrisentan was not associated with excess tumors in any dosed group.
Positive findings of clastogenicity were detected, at drug concentrations producing moderate to high toxicity, in the chromosome aberration assay in cultured human lymphocytes. There was no evidence for genetic toxicity of ambrisentan when tested in vitro in bacteria (Ames test) or in vivo in rats (micronucleus assay, unscheduled DNA synthesis assay).
The development of testicular tubular atrophy and impaired fertility has been linked to the chronic administration of endothelin receptor antagonists in rodents. Testicular tubular degeneration was observed in rats treated with ambrisentan for two years at doses ≥10 mg/kg/day (8-fold MRHD). Increased incidences of testicular findings were also observed in mice treated for two years at doses ≥50 mg/kg/day (28-fold MRHD). Effects on sperm count, sperm morphology, mating performance, and fertility were observed in fertility studies in which male rats were treated with ambrisentan at oral doses of 300 mg/kg/day (236-fold MRHD). At doses of ≥10 mg/kg/day, observations of testicular histopathology in the absence of fertility and sperm effects were also present.
14. Clinical Studies
14.1 Pulmonary Arterial Hypertension (PAH)
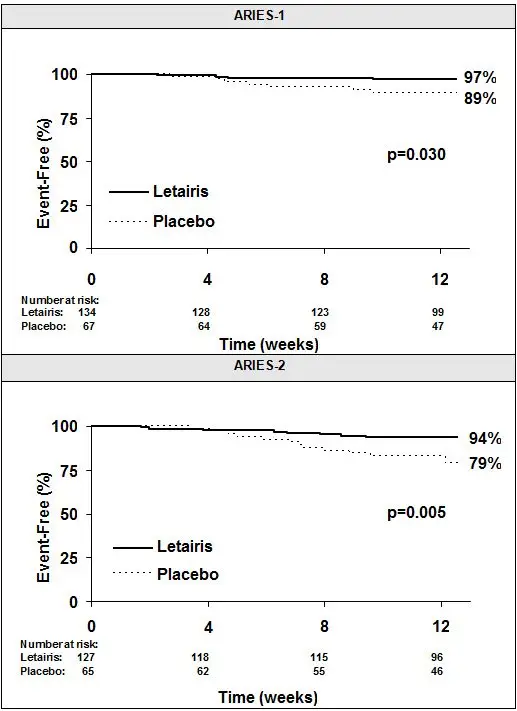
Two 12-week, randomized, double-blind, placebo-controlled, multicenter studies were conducted in 393 patients with PAH (WHO Group 1). The two studies were identical in design except for the doses of Letairis and the geographic region of the investigational sites. ARIES-1 compared once-daily doses of 5 mg and 10 mg Letairis to placebo, while ARIES-2 compared once-daily doses of 2.5 mg and 5 mg Letairis to placebo. In both studies, Letairis or placebo was added to current therapy, which could have included a combination of anticoagulants, diuretics, calcium channel blockers, or digoxin, but not epoprostenol, treprostinil, iloprost, bosentan, or sildenafil. The primary study endpoint was 6-minute walk distance. In addition, clinical worsening, WHO functional class, dyspnea, and SF-36 ® Health Survey were assessed.
Patients had idiopathic or heritable PAH (64%) or PAH associated with connective tissue diseases (32%), HIV infection (3%), or anorexigen use (1%). There were no patients with PAH associated with congenital heart disease.
Patients had WHO functional class I (2%), II (38%), III (55%), or IV (5%) symptoms at baseline. The mean age of patients was 50 years, 79% of patients were female, and 77% were Caucasian.
Submaximal Exercise Ability
Results of the 6-minute walk distance at 12 weeks for the ARIES-1 and ARIES-2 studies are shown in Table 3 and Figure 4.
| ARIES-1 | ARIES-2 | |||||
|---|---|---|---|---|---|---|
| Placebo
(N=67) | 5 mg
(N=67) | 10 mg
(N=67) | Placebo
(N=65) | 2.5 mg
(N=64) | 5 mg
(N=63) |
|
| Mean ± standard deviation | ||||||
|
||||||
| Baseline | 342 ± 73 | 340 ± 77 | 342 ± 78 | 343 ± 86 | 347 ± 84 | 355 ± 84 |
| Mean change from baseline | -8 ± 79 | 23 ± 83 | 44 ± 63 | -10 ± 94 | 22 ± 83 | 49 ± 75 |
| Placebo-adjusted mean change from baseline | – | 31 | 51 | – | 32 | 59 |
| Placebo-adjusted median change from baseline | – | 27 | 39 | – | 30 | 45 |
| p-value * | – | 0.008 | <0.001 | – | 0.022 | <0.001 |
Figure 4 Mean Change in 6-Minute Walk Distance (ARIES-1 and ARIES-2)
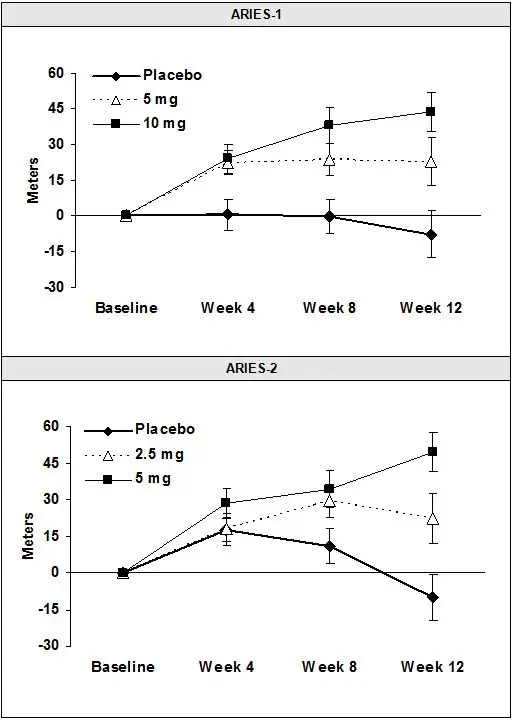
Mean change from baseline in 6-minute walk distance in the placebo and Letairis groups.
Values are expressed as mean ± standard error of the mean.
In both studies, treatment with Letairis resulted in a significant improvement in 6-minute walk distance for each dose of Letairis and the improvements increased with dose. An increase in 6-minute walk distance was observed after 4 weeks of treatment with Letairis, with a dose-response observed after 12 weeks of treatment. Improvements in walk distance with Letairis were smaller for elderly patients (age ≥65) than younger patients and for patients with secondary PAH than for patients with idiopathic or heritable PAH. The results of such subgroup analyses must be interpreted cautiously.
14.2 Combination Treatment of PAH
In a randomized, double-blind, active-controlled trial (AMBITION), 605 patients with WHO Functional Class II or III PAH were randomized 2:1:1 to once daily Letairis plus tadalafil or to Letairis or tadalafil alone. Treatment was initiated with Letairis 5 mg and tadalafil 20 mg. If tolerated, tadalafil was increased to 40 mg at 4 weeks and Letairis was increased to 10 mg at 8 weeks.
The primary endpoint was time to first occurrence of (a) death, (b) hospitalization for worsening PAH, (c) >15% decrease from baseline in 6MWD combined with WHO Functional Class III or IV symptoms sustained over 14 days (short term clinical worsening), or (d) reduction in 6MWD sustained over 14 days combined with WHO Functional Class III or IV symptoms sustained over 6 months (inadequate long term clinical response).
Patients had idiopathic PAH (55%), heritable PAH (3%), or PAH associated with connective tissue diseases, congenital heart disease, stable HIV infection, or drugs or toxins (APAH, 43%). Median time from diagnosis to first study drug administration was 25 days. Approximately 32% and 68% of patients were in WHO Functional Class II and III, respectively. The mean patient age was 55.7 years (34% were ≥65 years old). Most patients were white (90%) and female (76%); 45% were North American.
Principal results are shown in Figures 6 and 7.
Figure 6 Time to Primary Endpoint Event (AMBITION)
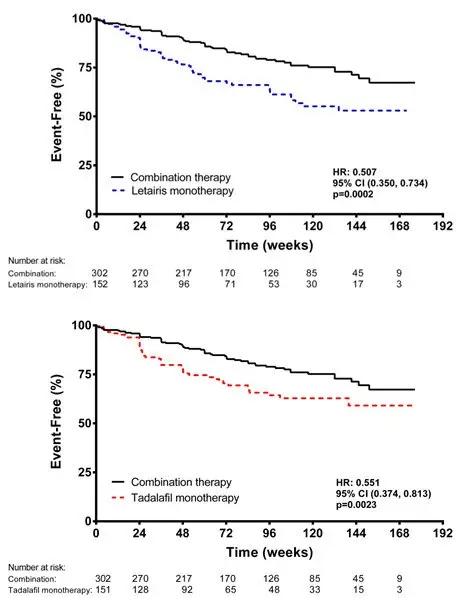
Figure 7 Primary Endpoint Events and First Occurrences of Each Component at Any Time (AMBITION)
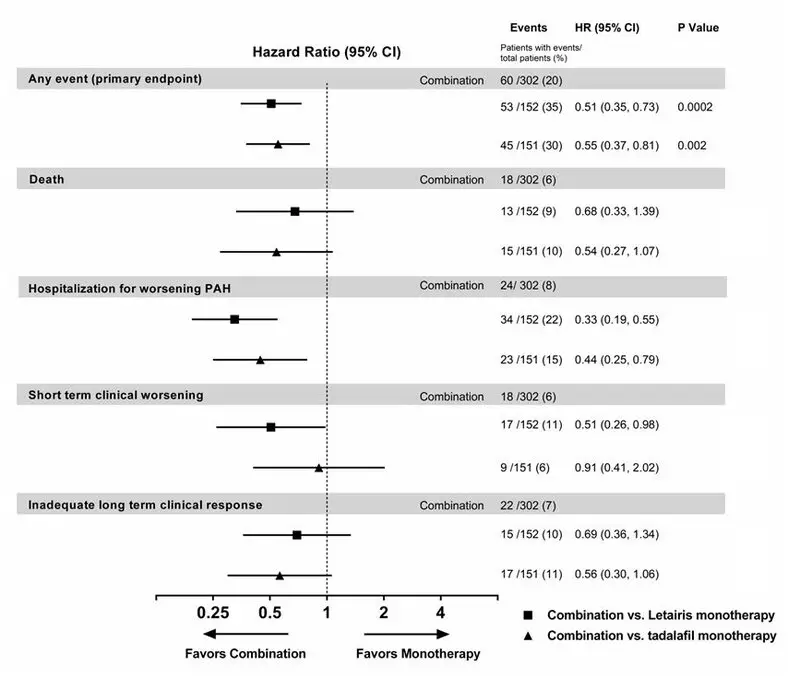
The treatment effect of Letairis plus tadalafil compared with individual monotherapy on time to first primary endpoint event was consistent across subgroups. (Figure 8).
Figure 8 Primary Endpoint by Subgroups (AMBITION)
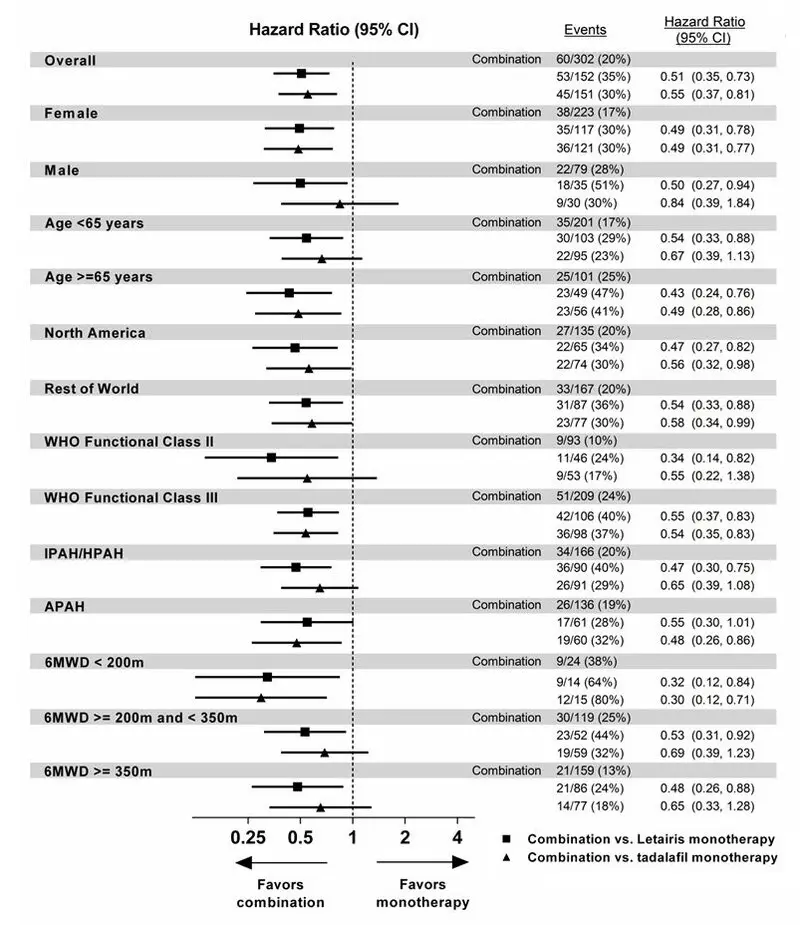
Note: The figure above presents effects in various subgroups all of which are baseline characteristics and all of which were pre-specified, if not the groupings. The 95% confidence limits that are shown do not take into account how many comparisons were made, nor do they reflect the effect of a particular factor after adjustment for all other factors. Apparent homogeneity or heterogeneity among groups should not be over interpreted.
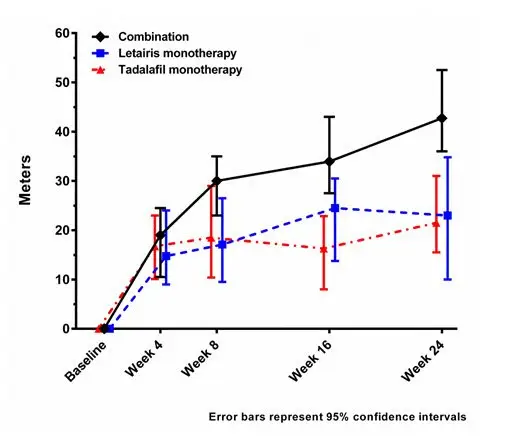
Exercise Ability
Results of the 6MWD at 24 weeks for the AMBITION study are shown in Table 5 and Figure 9.
| Letairis + Tadalafil
(N=302) | Letairis Monotherapy
(N=152) | Tadalafil Monotherapy
(N=151) |
|
|---|---|---|---|
|
|||
| Baseline (median) | 356 | 366 | 352 |
| Change from baseline (median) | 43 | 23 | 22 |
| Median difference from Letairis + Tadalafil
(95% CI) | 24
(11, 37) | 20
(8, 32) |
|
| P-Value | 0.0004 | 0.0016 | |
Figure 9 Median Change in 6-Minute Walk Distance (meters) in AMBITION
14.4 Adverse Effects in Idiopathic Pulmonary Fibrosis (IPF)
A randomized controlled study in patients with IPF, with or without pulmonary hypertension (WHO Group 3), compared Letairis (N=329) to placebo (N=163). The study was terminated after 34 weeks for lack of efficacy, and was found to demonstrate a greater risk of disease progression or death on Letairis. More patients taking Letairis died (8% vs. 4%), had a respiratory hospitalization (13% vs. 6%), and had a decrease in FVC/DLCO (17% vs. 12%) [see Contraindications (4.2)] .
16. How is Letairis supplied
Letairis film -coated tablets are supplied as follows:
| Tablet Strength | Package Configuration | NDC No. | Description of Tablet;
Debossed on Tablet; Size |
|---|---|---|---|
| 5 mg | 30 count blister | 61958 -0801 -2 | Square convex; pale pink;
"5" on side 1 and "GSI" on side 2; 6.6 mm Square |
| 30 count bottle | 61958 -0801 -1 | ||
| 10 count blister | 61958 -0801 -3 | ||
| 10 count bottle | 61958 -0801 -5 | ||
| 10 mg | 30 count blister | 61958 -0802 -2 | Oval convex; deep pink;
"10" on side 1 and "GSI" on side 2; 9.8 mm × 4.9 mm Oval |
| 30 count bottle | 61958 -0802 -1 | ||
| 10 count blister | 61958 -0802 -3 | ||
| 10 count bottle | 61958 -0802 -5 |
17. Patient Counseling Information
Advise patients to read the FDA-approved patient labeling (Medication Guide).
| LETAIRIS
ambrisentan tablet, film coated |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
| LETAIRIS
ambrisentan tablet, film coated |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| Labeler - Gilead Sciences, Inc (185049848) |