Drug Detail:Mannitol (monograph) (Osmitrol)
Drug Class:
Highlights of Prescribing Information
MANNITOL Injection, for intravenous use
Initial U.S. Approval: 1964
Recent Major Changes
Indications and Usage (removed, revised) (1) 09/2019
Contraindications (4) 09/2019
Warnings and Precautions (5.1, 5.3, 5.7) 09/2019
Indications and Usage for Mannitol Injection
Mannitol Injection is an osmotic diuretic, indicated for the reduction of: (1)
• intracranial pressure and treatment of cerebral edema. (1)
• elevated intraocular pressure. (1)
Mannitol Injection Dosage and Administration
Administration Instructions (2.1):
- For intravenous infusion preferably into a large central vein.
- Prior to administration, evaluate renal, cardiac and pulmonary status, and correct fluid and electrolyte imbalances.
Recommended Dosage (2.2):
- The dosage, concentration and rate of administration depend on the age, weight and condition of the patient, including fluid requirement, urinary output and concomitant therapy.
- Reduction of Intracranial Pressure: 0.25 gram/kg administered every 6 to 8 hours as an intravenous infusion over 30 minutes.
- Reduction of Intraocular Pressure: 1.5 to 2 grams/kg of a 15% or 20% w/v solution as a single dose administered intravenously over at least 30 minutes.
Dosage Forms and Strengths
Injection: 20% (0.2 grams/mL): 20 grams of mannitol, USP per 100 mL in single-dose 250 mL and 500 mL flexible containers. (3)
Contraindications
- Known hypersensitivity to mannitol. (4, 5.1)
- Anuria. (4, 5.2)
- Severe hypovolemia. (4, 5.4)
- Pre-existing severe pulmonary vascular congestion or pulmonary edema. (4, 5.5)
- Active intracranial bleeding except during craniotomy. (4)
Warnings and Precautions
- Hypersensitivity Reactions, including anaphylaxis: Stop infusion immediately if hypersensitivity reactions develop. (5.1)
-
Renal Complications Including Renal Failure: Risk factors include preexisting renal failure, concomitant use of nephrotoxic drugs or
other diuretics. Avoid use of nephrotoxic drugs. Discontinue Mannitol Injection if renal function worsens. (5.2, 8.6) - Central Nervous System (CNS) Toxicity: Confusion, lethargy and coma may occur during or after infusion. Concomitant neurotoxic drugs may potentiate toxicity. Avoid use of neurotoxic drugs. Discontinue Mannitol Injection if CNS toxicity develops. (5.3)
- Fluid and Electrolyte Imbalances, Hyperosmolarity: Hypervolemia may exacerbate congestive heart failure, hyponatremia can lead to encephalopathy; hypo/hyperkalemia can result in cardiac adverse reactions in sensitive patients. Discontinue Mannitol Injection if fluid and/or electrolyte imbalances occur. (5.4)
- Monitoring/Laboratory Tests: Monitor fluid and electrolytes, serum osmolarity and renal, cardiac and pulmonary function. Discontinue if toxicity develops. (5.5)
- Infusion Site Reactions: May include irritation and inflammation, as well as severe reactions (compartment syndrome) when associated with extravasation. (5.6)
- Interference with Laboratory Tests: High concentrations of mannitol may cause false low results of inorganic phosphorus blood concentrations. Mannitol may produce false positive results for blood ethylene glycol. (5.7, 7.6)
Adverse Reactions/Side Effects
The most common adverse reactions are hypersensitivity reactions, renal failure, CNS toxicity, hypo/hypervolemia, hypo/hypernatremia, hypo/hyperkalemia, and infusion site reactions. (6)
To report SUSPECTED ADVERSE REACTIONS, contact B. Braun Medical Inc. at 1-800-854-6851 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. (6)
Drug Interactions
- Nephrotoxic Drugs and Diuretics: May increase the risk of renal failure; avoid concomitant use. (7.1, 7.2)
- Neurotoxic Drugs: May potentiate CNS toxicity of mannitol; avoid concomitant use. (7.3)
- Drugs Affected by Electrolyte Imbalances: May result in cardiac adverse reactions; monitor serum electrolytes and discontinue Mannitol Injection if cardiac status worsens. (7.4)
- Renally Eliminated Agents: Concomitant use may decrease the effectiveness of agents that undergo significant renal elimination. However, concomitant use of mannitol and lithium may increase risk of lithium toxicity. If concomitant use is necessary, frequently monitor lithium concentrations and for signs of toxicity. (7.5)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 8/2023
Related/similar drugs
furosemide, azithromycin, Lasix, dexamethasone, Zithromax, gentamicin, CreonFull Prescribing Information
1. Indications and Usage for Mannitol Injection
Mannitol Injection is indicated for:
- Reduction of intracranial pressure and treatment of cerebral edema.
- Reduction of elevated intraocular pressure.
2. Mannitol Injection Dosage and Administration
2.1 Important Preparation and Administration Instructions
- Mannitol Injection is for intravenous use only, preferably into a large central vein [see Warnings and Precautions (5.6), Description (11)].
- Prior to administration of Mannitol Injection, evaluate renal, cardiac and pulmonary status of the patient and correct fluid and electrolyte imbalances [see Dosage and Administration (2.2)].
- Do not administer Mannitol Injection simultaneously with blood products through the same administration set because of the possibility of pseudoagglutination or hemolysis. If it is essential that blood be given simultaneously, at least 20 mEq of sodium chloride should be added to each liter of mannitol solution to avoid pseudoagglutination.
Preparation
- Tear overwrap and remove solution container.
- Visually inspect the container. The closure system has two ports; the one for the administration set has a tamper evident plastic protector and the other is a medication addition site. Use only if solution is clear and container and seals are intact.
- Check for minute leaks by squeezing inner bag firmly. If leaks are found, discard solution as sterility may be impaired.
- Invert container and carefully inspect the solution in good light for cloudiness, haze, or particulate matter. Any container which is suspect should not be used.
- Admixing Mannitol Injection with other medications is not recommended. The addition of sodium chloride to 20% mannitol solution may result in precipitation of mannitol.
- Inspect Mannitol Injection visually for particulate matter and discoloration prior to administration and periodically during administration. If particulates or discoloration are present, discard the bag.
- Solutions of mannitol may crystallize when exposed to low temperatures. Concentrations greater than 15% have a greater tendency to crystallization. Inspect for crystals prior to administration. If crystals are observed, the container should be warmed by appropriate means to not greater than 60°C, shaken, then cooled to body temperature before administering. If all crystals cannot be completely redissolved, the container must be discarded.
Administration
-
Administer intravenously using sterile, filter-type administration set. It is recommended that Mannitol Injection be administered through a blood filter set to ensure against infusion of mannitol crystals.
- When administered peripherally, infuse slowly through a small bore needle, placed well within the lumen of a large vein to minimize venous irritation. Carefully avoid infiltration.
- Do not admix with other drugs. The use of supplemental additive medication is not recommended.
- To prevent air embolism, use a non-vented infusion set or close the vent on a vented set, avoid multiple connections, do not connect flexible containers in series, fully evacuate residual gas in the container prior to administration, do not pressurize the flexible container to increase flow rates, and if administration is controlled by a pumping device, turn off pump before the container runs dry.
-
For single use only; discard unused portion.
2.2 Recommended Dosage
Prior to administration of Mannitol Injection, evaluate renal, cardiac and pulmonary status of the patient and correct fluid and electrolyte imbalances.
The total dosage, concentration, and rate of administration depend on the age, weight, and condition of the patient being treated, including fluid requirement, electrolyte balance, serum osmolality, urinary output, and concomitant therapy.
The following outline of administration and dosage is only a general guide to therapy.
Reduction of Intracranial Pressure
Usually a maximum reduction in intracranial pressure in adults can be achieved with a dose of 0.25 g/kg infused intravenously over 30 minutes, which may be repeated every six to eight hours.
During and following Mannitol Injection infusion, monitor fluid and electrolytes, serum osmolarity, and renal, cardiac and pulmonary function. Discontinue Mannitol Injection if renal, cardiac, or pulmonary status worsens or CNS toxicity develops [see Warnings and Precautions (5.2, 5.3, 5.4, 5.5)].
Reduction of Intraocular Pressure
The recommended dosage is 1.5 to 2 g/kg of a 20% solution (7.5 to 10 mL/kg) as a single dose infused intravenously over a period of at least 30 minutes. When used preoperatively, administer one to one and one-half hours before surgery to achieve maximal reduction of intraocular pressure before operation.
3. Dosage Forms and Strengths
Mannitol Injection 20%, USP is a clear and colorless solution of 20 grams of mannitol, USP per 100 mL (0.2 grams/mL) in single-dose 250 mL and 500 mL flexible containers.
4. Contraindications
Mannitol Injection is contraindicated in patients with:
- Hypersensitivity to mannitol [see Warnings and Precautions (5.1)]
- Anuria [see Warnings and Precautions (5.2)]
- Severe hypovolemia [see Warnings and Precautions (5.4)]
- Pre-existing severe pulmonary vascular congestion or pulmonary edema [see Warnings and Precautions (5.5)]
- Active intracranial bleeding except during craniotomy.
5. Warnings and Precautions
5.1 Hypersensitivity Reactions
Serious hypersensitivity reactions, including anaphylaxis, hypotension and dyspnea resulting in cardiac arrest and death have been reported with Mannitol Injection [see Adverse Reactions (6)]. Stop the infusion immediately if signs or symptoms of a suspected hypersensitivity reaction develop. Initiate appropriate therapeutic countermeasures as clinically indicated.
5.2 Renal Complications Including Renal Failure
Renal complications, including irreversible renal failure have been reported in patients receiving mannitol.
Reversible, oliguric acute kidney injury (AKI) has occurred in patients with normal pretreatment renal function who received large intravenous doses of mannitol.
Although the osmotic nephrosis associated with mannitol administration is in principle reversible, osmotic nephrosis in general is known to potentially proceed to chronic or even end-stage renal failure. Monitor renal function closely during infusion of Mannitol Injection. Patients with pre-existing renal disease, patients with conditions that put them at high risk for renal failure, or those receiving potentially nephrotoxic drugs or other diuretics, are at increased risk of renal failure following administration of Mannitol Injection. Avoid concomitant administration of nephrotoxic drugs (e.g., aminoglycosides) or, other diuretics with Mannitol Injection, if possible [see Drug Interactions (7.1, 7.2)].
Patients with oliguric AKI who subsequently develop anuria while receiving mannitol are at risk of congestive heart failure, pulmonary edema, hypertensive crisis, coma and death.
During and following Mannitol Injection infusion for reduction in intracranial pressure, monitor the patient clinically and review laboratory tests for changes in fluid and electrolyte status. Discontinue Mannitol Injection if renal function worsens [see Warnings and Precautions (5.5)].
5.3 Central Nervous System (CNS) Toxicity
CNS toxicity manifested by, e.g., confusion, lethargy, or coma has been reported in patients treated with mannitol, with fatal outcomes identified, in particular in the presence of impaired renal function CNS toxicity may result from high serum mannitol concentrations, serum hyperosmolarity resulting in intracellular dehydration within CNS, hyponatremia or other disturbances of electrolyte and acid/base balance secondary to mannitol administration [see Warnings and Precautions (5.4)].
At high concentrations, mannitol may cross the blood brain barrier and interfere with the ability of the brain to maintain the pH of the cerebrospinal fluid especially in the presence of acidosis.
In patients with preexisting compromise of the blood brain barrier, the risk of increasing cerebral edema (general and focal) associated with repeated or continued use of 20% Mannitol Injection USP must be individually weighed against the expected benefits.
A rebound increase of intracranial pressure may occur several hours after the infusion. Patients with a compromised blood brain barrier are at increased risk.
Concomitant administration of nephrotoxic drugs (e.g., aminoglycosides) with Mannitol Injection may potentiate neurotoxicity. Avoid concomitant use of neurotoxic drugs, if possible [see Drug Interactions (7.3)].
During and following infusion of Mannitol Injection for the reduction in intracranial pressure, monitor the patient clinically and laboratory tests for changes in fluid and electrolyte status. Discontinue Mannitol Injection if CNS toxicity develops. [see Warnings and Precautions (5.5)].
5.4 Fluid and Electrolyte Imbalances, Hyperosmolarity
Depending on dosage and duration, administration of Mannitol Injection may result in hypervolemia leading to or exacerbating existing congestive heart failure. Accumulation of mannitol due to insufficient renal excretion increases the risk of hypervolemia.
Mannitol-induced osmotic diuresis may cause or worsen dehydration/hypovolemia and hemoconcentration. Administration of Mannitol Injection may also cause hyperosmolarity [see Description (11)].
The obligatory diuretic response following rapid infusion of Mannitol Injection may further aggravate preexisting hemoconcentration. Excessive loss of water and electrolytes may lead to serious imbalances. Serum sodium and potassium should be carefully monitored during mannitol administration.
Depending on dosage and duration of administration, electrolyte and acid/base imbalances may also result from transcellular shifts in water and electrolytes, osmotic diuresis and/or other mechanisms. Such imbalances may be severe and potentially fatal.
Imbalances that may result from Mannitol Injection administration include:
• Hypernatremia, dehydration and hemoconcentration
• Hyponatremia, which can lead to headache, nausea, seizures, lethargy, coma, cerebral edema, and death. Acute symptomatic hyponatremic encephalopathy is considered a medical emergency.
• Hypo/hyperkalemia. The development of electrolyte imbalances (e.g., hyperkalemia, hypokalemia) associated with mannitol administration may result in cardiac adverse reactions in patients receiving drugs that are sensitive to such imbalances (e.g., digoxin, agents that may cause QT prolongation, neuromuscular blocking agents) [see Drug Interactions (7.4)].
• Other electrolyte disturbances
• Metabolic acidosis/alkalosis
Pediatric patients less than two years of age, particularly preterm and term neonates, may be at higher risk for fluid and electrolyte abnormalities following Mannitol Injection administration due to decreased glomerular filtration rate and limited ability to concentrate urine [see Use in Specific Populations (8.4)]
During and following Mannitol Injection infusion for the reduction in intracranial pressure, monitor fluid, acid-base balance and electrolyte status and discontinue Mannitol Injection if imbalances occur [see Warnings and Precautions (5.5)].
5.5 Monitoring/Laboratory Tests
During and following infusion of Mannitol Injection for the reduction in intracranial pressure, monitor:
• serum osmolarity, serum electrolytes (including sodium, potassium, calcium and phosphate) and acid base balance
• the osmol gap
• signs of hypo- or hypervolemia, including urine output
• renal, cardiac and pulmonary function
• intracranial pressure
Discontinue Mannitol Injection if renal, cardiac, or pulmonary status worsens, or CNS toxicity develops [see Contraindications (4)].
5.6 Infusion Site Reactions
The infusion of hypertonic solutions through a peripheral vein, including Mannitol Injection, may result in peripheral venous irritation, including phlebitis. Other severe infusion site reactions, such as compartment syndrome and swelling associated with extravasation, can occur with administration of Mannitol Injection [see Adverse Reactions (6)]. Mannitol Injection is preferably for administration into a large central vein [see Dosage and Administration (2.1)].
5.7 Interference with Laboratory Tests
High concentrations of mannitol can cause false low results for inorganic phosphorus blood concentrations [see Drug Interactions (7.6)].
Mannitol may produce false positive results in tests for blood ethylene glycol concentrations [see Drug Interactions (7.6)].
6. Adverse Reactions/Side Effects
The following adverse reactions from voluntary reports or clinical studies have been reported with mannitol injection. Because many of these reactions were reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
• Hypersensitivity Reactions: cardiac arrest, anaphylaxis, hypotension, dyspnea, hypertension, pyrexia, chills, sweating, cough, musculoskeletal stiffness, myalgia, urticarial/rash, pruritus, generalized pain, discomfort, nausea, vomiting, and headache [see Warnings and Precautions (5.1)]
• Renal Failure: acute kidney injury, osmotic nephrosis, azotemia, anuria, hematuria, oliguria, polyuria [see Warnings and Precautions (5.2)]
• CNS Toxicity: headache, coma, seizures, confusion, lethargy; rebound increase in intracranial pressure; dizziness [see Warnings and Precautions (5.3)]
• Fluid and Electrolyte Imbalances: hypovolemia, hypervolemia, peripheral edema, dehydration, hyponatremia, hypernatremia, hyperkalemia, hypokalemia; metabolic acidosis [see Warnings and Precautions (5.4)]
• Infusion Site Reactions: infection, venous thrombosis or phlebitis, inflammation, pain, rash, erythema, pruritus, compartment syndrome and swelling associated with extravasation [see Warnings and Precautions (5.6)]
• Cardiac and Respiratory Disorders: rhinitis, congestive cardiac failure, pulmonary edema, palpitations, hypotension, hypertension, tachycardia, and angina-like chest pains.
• Gastrointestinal Disorders: thirst, dry mouth, nausea, vomiting
• Other: asthenia, malaise, fever, chills, urticaria
7. Drug Interactions
7.1 Nephrotoxic Drugs
Concomitant administration of nephrotoxic drugs (e.g., cyclosporine, aminoglycosides) increases the risk of renal failure following administration of mannitol. Avoid use of nephrotoxic drugs with Mannitol Injection, if possible [see Warnings and Precautions (5.2)].
7.2 Diuretics
Concomitant administration of other diuretics may potentiate the renal toxicity of mannitol. Avoid use of other diuretics with Mannitol Injection, if possible [see Warnings and Precautions (5.2)].
7.3 Neurotoxic Drugs
Concomitant administration of systemic neurotoxic drugs (e.g., aminoglycosides) with Mannitol Injection may potentiate the CNS toxicity of mannitol. Avoid use of systemic neurotoxic drugs with Mannitol Injection, if possible [see Warnings and Precautions (5.3)].
7.4 Drugs Affected by Electrolyte Imbalances
The development of electrolyte imbalances (e.g., hyperkalemia, hypokalemia) associated with mannitol administration may result in cardiac adverse reactions in patients receiving drugs that are sensitive to such imbalances (e.g., digoxin, drugs that prolong the QT interval, neuromuscular blocking agents) [see Warnings and Precautions (5.4)]. During and following infusion of Mannitol Injection, monitor serum electrolytes and discontinue Mannitol Injection if cardiac status worsens [see Warnings and Precautions (5.5)].
7.5 Renally Eliminated Drugs
Mannitol therapy may increase the elimination and decrease the effectiveness of treatment with drugs that undergo significant renal elimination. Concomitant administration of mannitol with lithium may initially increase the elimination of lithium but may also increase the risk of lithium toxicity if patients develop hypovolemia or renal impairment. In patients receiving lithium, consider holding lithium doses during treatment with Mannitol Injection. In patients requiring concomitant administration of lithium and Mannitol Injection, frequently monitor serum lithium concentrations and for signs of lithium toxicity.
7.6 Interference with Laboratory Tests
High concentrations of mannitol can cause false low results for inorganic phosphorus blood concentrations when an assay based on the conversion of phosphate (orthophosphate) to the phosphomolybdate complex is used.
Mannitol may produce false positive results in tests for blood ethylene glycol concentrations in which mannitol is initially oxidized to an aldehyde.
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
The available case report data with mannitol over decades of use have not identified a drug-associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes. Mannitol crosses the placenta and may cause fluid shifts that could potentially result in adverse effects in the fetus (see Data). No adverse developmental effects from mannitol were reported in published animal studies; however, fluid shifts occurred in fetal ewes in response to maternal infusion of mannitol.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
8.2 Lactation
Risk Summary
There are no data on the presence of mannitol in either human or animal milk, the effects of on the breastfed infant, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Mannitol Injection and any potential adverse effects on the breastfed infant from Mannitol Injection or from the underlying maternal condition.
8.4 Pediatric Use
Mannitol Injection is approved for use in the pediatric population for the reduction of intracranial and intraocular pressure. Studies have not defined the optimal dose of Mannitol Injection in the pediatric population. The safety profile for mannitol use in pediatric patients is similar to adults at dosages described in labeling. However, pediatric patients less than two years of age, particularly preterm and term neonates, may be at higher risk for fluid and electrolyte abnormalities following Mannitol Injection administration due to decreased glomerular filtration rate and limited ability to concentrate urine [see Warnings and Precautions (5.4)].
8.5 Geriatric Use
Mannitol is known to be substantially excreted by the kidney and the risk of adverse reactions to this drug may be greater in elderly patients with impaired renal function. Evaluate the renal, cardiac and pulmonary status of the patient and correct fluid and electrolyte imbalances prior to administration of Mannitol Injection [see Warnings and Precautions (5.2, 5.3, 5.4, 5.5)].
8.6 Renal Impairment
Patients with pre-existing renal disease, patients with conditions that put them at risk for renal failure, or those receiving potentially nephrotoxic drugs or other diuretics, are at increased risk of renal failure with administration of mannitol. Evaluate the renal, cardiac and pulmonary status of the patient and correct fluid and electrolyte imbalances prior to administration of Mannitol Injection [see Warnings and Precautions (5.2, 5.3, 5.4, 5.5)].
10. Overdosage
Signs and symptoms of overdose with Mannitol Injection include renal failure and acute kidney injury, hypo/hypervolemia, hyperosmolarity and electrolyte imbalances, CNS toxicity (e.g., coma, seizures), some of which can be fatal [see Warnings and Precautions (5.2, 5.3, 5.4)].
Management of overdosage with Mannitol Injection is symptomatic and supportive. Discontinue the infusion and institute appropriate corrective measures with particular attention to renal, cardiac and pulmonary systems. Correct fluid and electrolyte imbalances.
Mannitol Injection is dialyzable (hemodialysis and peritoneal dialysis): dialysis may increase Mannitol Injection elimination.
11. Mannitol Injection Description
Mannitol Injection 20%, USP is a sterile, nonpyrogenic solution of Mannitol, USP in 250 mL and 500 mL single-dose EXCEL® flexible containers for intravenous administration as an osmotic diuretic. It contains no antimicrobial agents. Mannitol is a six-carbon sugar alcohol prepared commercially by the reduction of dextrose.
Each 100 mL contains:
Mannitol USP 20 g; Water for Injection USP qs
pH: 5.3 (4.5-7.0); Calculated Osmolarity 1100 mOsmol/liter
Normal physiologic osmolarity range is approximately 280 to 310 mOsmol/L.
The formula of the active ingredient is:
| Ingredient | Molecular Formula | Molecular Weight |
| Mannitol USP | 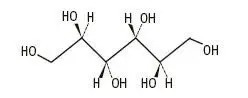 | 182.17 |
The EXCEL® plastic container is made from a multilayered film specifically developed for parenteral drugs. It contains no plasticizers. The solution contact layer is a rubberized copolymer of ethylene and propylene. Solutions in contact with the plastic container may leach out certain chemical components from the plastic in very small amounts; however, biological testing was supportive of the safety of the plastic container materials. The container-solution unit is a closed system and is not dependent upon entry of external air during administration. The container is overwrapped to provide protection from the physical environment and to provide an additional moisture barrier when necessary. Exposure to temperatures above 25°C/77°F during transport and storage will lead to minor losses in moisture content. Higher temperatures lead to greater losses. It is unlikely that these minor losses will lead to clinically significant changes within the expiration period.
12. Mannitol Injection - Clinical Pharmacology
12.1 Mechanism of Action
Mannitol, when administered intravenously, exerts its osmotic effect as a solute of relatively small molecular size being largely confined to the extracellular space. Mannitol hinders tubular reabsorption of water and enhances excretion of sodium and chloride by elevating the osmolarity of the glomerular filtrate.
This increase in extracellular osmolarity effected by the intravenous administration of mannitol will induce the movement of intracellular water to the extracellular and vascular spaces. This action underlies the role of mannitol in reducing intracranial pressure, intracranial edema, and elevated intraocular pressure.
12.3 Pharmacokinetics
Distribution
Mannitol distributes largely in the extracellular space in 20 to 40 minutes after intravenous administration. The volume of distribution of mannitol is approximately 17 L in adults.
Elimination
In subjects with normal renal function, the total clearance is 87 to 109 mL/min. The elimination half-life of mannitol is 0.5 to 2.5 hours.
Metabolism
Only relatively small amount of the dose administered is metabolized after intravenous administration of mannitol to healthy subjects.
Excretion
Mannitol is eliminated primarily via the kidneys in unchanged form. Mannitol is filtered by the glomeruli, exhibits less than 10% of tubular reabsorption, and is not secreted by tubular cells. Following intravenous administration, approximately 80% of an administered dose of mannitol is estimated to be excreted in the urine in three hours with lesser amounts thereafter.
Specific Populations
Patients with Renal Impairment
In patients with renal impairment, the elimination half-life of mannitol is prolonged. In a published study, in patients with renal impairment including acute renal failure and end stage renal failure, the elimination half-life of mannitol was estimated at about 36 hours, based on serum osmolarity. In patients with renal impairment on dialysis, the elimination half-life of mannitol was reduced to 6 and 21 hours during hemodialysis and peritoneal dialysis, respectively [see Use in Specific Populations (8.6), Overdosage (10)].
16. How is Mannitol Injection supplied
Mannitol Injection USP, 20% (0.2 grams/mL) as a clear and colorless solution is supplied in sterile and nonpyrogenic 250 mL and 500 mL single-dose EXCEL® Containers.
Not made with natural rubber latex, PVC or DEHP.
|
NDC |
REF |
Size |
|
0264-7578-10 |
L5781 |
500 mL |
|
0264-7578-20 |
L5782 |
250 mL |
The 500 mL and 250 mL containers are packaged 24 per case.
Store at room temperature (25°C).
Exposure of pharmaceutical products to heat should be minimized. Avoid excessive heat. Protect from freezing.
17. Patient Counseling Information
Inform patients or caregivers of the following risks of Mannitol Injection:
• Hypersensitivity Reactions [see Warnings and Precautions (5.1)]
• Renal Failure [see Warnings and Precautions (5.2)]
• CNS Toxicity [see Warnings and Precautions (5.3)]
• Fluid and Electrolyte Imbalances, Hyperosmolarity [see Warnings and Precautions (5.4)]
• Infusion Site Reactions [see Warnings and Precautions (5.6)]
Rx only
Manufactured by:
B. Braun Medical Inc.
Bethlehem, PA 18018-3524 USA
1-800-227-2862
Produced in USA with API from Germany
EXCEL® is a registered trademark of B. Braun Medical Inc.
Y36-002-994 LD-496-3
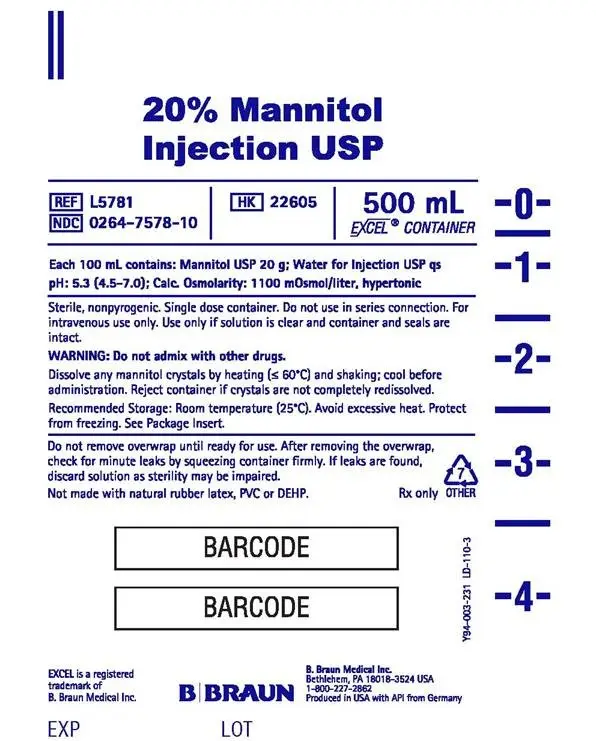
PRINCIPAL DISPLAY PANEL - 500 mL
20% Mannitol
Injection USP
REF L5781
NDC 0264-7578-10
HK 22605
500 mL
EXCEL® CONTAINER
Each 100 mL contains: Mannitol USP 20 g; Water for Injection USP qs
pH: 5.3 (4.5-7.0); Calc. Osmolarity: 1100 mOsmol/liter, hypertonic
Sterile, nonpyrogenic. Single dose container. Do not use in series connection. For
intravenous use only. Use only if solution is clear and container and seals are
intact.
WARNING: Do not admix with other drugs.
Dissolve any mannitol crystals by heating (< 60°C) and shaking; cool before
administration. Reject container if crystals are not completely redissolved.
Recommended Storage: Room temperature (25°C). Avoid excessive heat. Protect
from freezing. See Package Insert.
Do not remove overwrap until ready for use. After removing the overwrap,
check for minute leaks by squeezing container firmly. If leaks are found,
discard solution as sterility may be impaired.
Not made with natural rubber latex, PVC or DEHP.
Rx only

EXCEL is a registered
trademark of
B. Braun Medical Inc.
B. Braun Medical Inc.
Bethlehem, PA 18018-3524 USA
1-800-227-2862
Produced in USA with API from Germany
Y94-003-231 LD-110-3
EXP
LOT
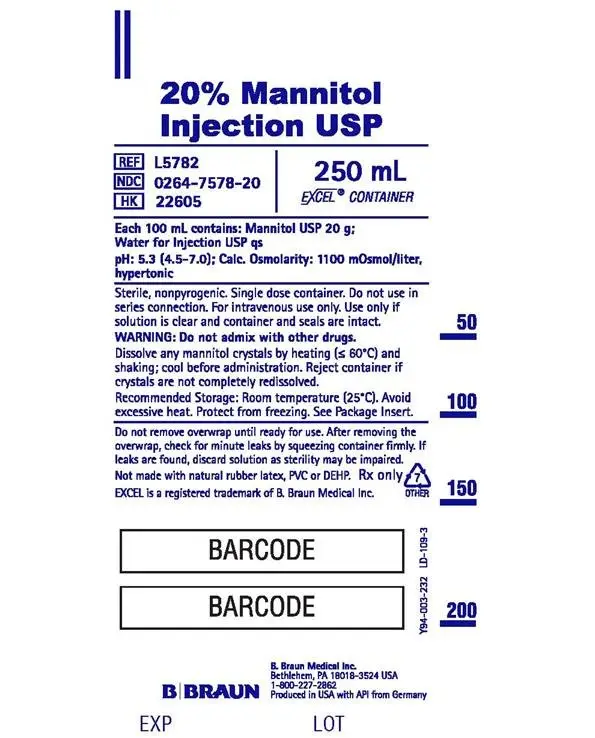
PRINCIPAL DISPLAY PANEL - 250 mL
20% Mannitol
Injection USP
REF L5782
NDC 0264-7578-20
HK 22605
250 mL
EXCEL® CONTAINER
Each 100 mL contains: Mannitol USP 20 g;
Water for Injection USP qs
pH: 5.3 (4.5-7.0); Calc. Osmolarity: 1100 mOsmol/liter,
hypertonic
Sterile, nonpyrogenic. Single dose container. Do not use in
series connection. For intravenous use only. Use only if
solution is clear and container and seals are intact.
WARNING: Do not admix with other drugs.
Dissolve any mannitol crystals by heating (< 60°C) and
shaking; cool before administration. Reject container if
crystals are not completely redissolved.
Recommended Storage: Room temperature (25°C). Avoid
excessive heat. Protect from freezing. See Package Insert.
Do not remove overwrap until ready for use. After removing the
overwrap, check for minute leaks by squeezing container firmly. If
leaks are found, discard solution as sterility may be impaired.
Not made with natural rubber latex, PVC or DEHP.
EXCEL is a registered trademark of B. Braun Medical Inc.
Rx only

B. Braun Medical Inc.
Bethlehem, PA 18018-3524 USA
1-800-227-2862
Produced in USA with API from Germany
Y94-003-232 LD-109-3
EXP
LOT
| MANNITOL
mannitol injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - B. Braun Medical Inc. (002397347) |




