Drug Detail:Menveo (Meningococcal conjugate vaccine [ me-nin-je-kok-al-kon-je-gate-vax-een ])
Drug Class: Bacterial vaccines
Highlights of Prescribing Information
MENVEO [Meningococcal (Groups A, C, Y, and W-135) Oligosaccharide Diphtheria CRM197 Conjugate Vaccine] solution for injection, for intramuscular use
Initial U.S. Approval: 2010
Recent Major Changes
|
Dosage and Administration (2.1, 2.2, 2.3) |
10/2022 |
Indications and Usage for Menveo
MENVEO is a vaccine indicated for active immunization to prevent invasive meningococcal disease caused by Neisseria meningitidis serogroups A, C, Y, and W-135 in individuals 2 months through 55 years of age.
MENVEO does not prevent N. meningitidis serogroup B infections. (1)
Menveo Dosage and Administration
- •
- For intramuscular injection only (0.5 mL). (2)
- MENVEO is supplied as either:
- •
- Two vials: A vial containing the MenCYW-135 liquid conjugate component (gray cap) and a vial containing the MenA lyophilized conjugate component (orange cap). The contents of the vials must be combined to form MENVEO prior to administration. This presentation is for use in individuals 2 months through 55 years of age. (2.1, 2.2),
- OR
- •
- One vial containing MENVEO (pink cap). This presentation does not require reconstitution before use. This presentation is for use in individuals 10 through 55 years of age. (2.1, 2.2)
Primary Vaccination
- •
- In children initiating vaccination at 2 months of age, administer as a 4-dose series at 2, 4, 6, and 12 months of age. (2.4)
- •
- In children initiating vaccination at 7 months through 23 months of age, administer as a 2-dose series with the second dose administered in the second year of life and at least 3 months after the first dose. (2.4)
- •
- In individuals aged 2 through 55 years, administer as a single dose. (2.4)
Booster Vaccination
- •
- A single booster dose of MENVEO may be administered to individuals aged 15 through 55 years who are at continued risk for meningococcal disease if at least 4 years have elapsed since a prior dose of a meningococcal (serogroups A, C, Y, W-135) conjugate vaccine. (2.4)
Dosage Forms and Strengths
Solution for injection. A single dose is 0.5 mL. (3)
Contraindications
Severe allergic reaction (e.g., anaphylaxis) to a previous dose of MENVEO, to any component of this vaccine, or to any other diphtheria toxoid-containing vaccine. (4)
Warnings and Precautions
- •
- Syncope (fainting) has occurred in association with administration of MENVEO. Procedures should be in place to avoid injury from fainting. (5.2)
- •
- Apnea following intramuscular vaccination has been observed in some infants born prematurely. A decision about when to administer MENVEO to an infant born prematurely should be based on consideration of the individual infant's medical status and the potential benefits and possible risks of vaccination. (5.5)
Adverse Reactions/Side Effects
- •
- Common solicited adverse reactions (≥10%) among children initiating vaccination at 2 months of age and receiving the 4-dose series were tenderness (24% to 41%) and erythema at injection site (11% to 15%), irritability (42% to 57%), sleepiness (29% to 50%), persistent crying (21% to 41%), change in eating habits (17% to 23%), vomiting (5% to 11%), and diarrhea (8% to 16%). (6.1)
- •
- Common solicited adverse reactions (≥10%) among children initiating vaccination at 7 months through 23 months of age and receiving the 2-dose series were tenderness (10% to 16%) and erythema at injection site (12% to 15%), irritability (27% to 40%), sleepiness (17% to 29%), persistent crying (12-21%), change in eating habits (12% to 20%), and diarrhea (10% to 16%). (6.1)
- •
- Common solicited adverse reactions (≥10%) among children aged 2 through 10 years who received MENVEO were injection site pain (31%), erythema (23%), irritability (18%), induration (16%), sleepiness (14%), malaise (12%), and headache (11%). (6.1)
- •
- Common solicited adverse reactions (≥10%) among adolescents and adults who received a single dose of MENVEO were pain at the injection site (41%), headache (30%), myalgia (18%), malaise (16%), and nausea (10%). Similar rates of solicited adverse reactions were observed following a single booster dose. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact GlaxoSmithKline at 1-888-825-5249 or VAERS at 1-800-822-7967 or www.vaers.hhs.gov.
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 10/2022
Related/similar drugs
ciprofloxacin, ceftriaxone, Rocephin, rifampin, meningococcal conjugate vaccineFull Prescribing Information
1. Indications and Usage for Menveo
MENVEO is a vaccine indicated for active immunization to prevent invasive meningococcal disease caused by Neisseria meningitidis serogroups A, C, Y, and W-135 in individuals 2 months through 55 years of age.
MENVEO does not prevent N. meningitidis serogroup B infections.
2. Menveo Dosage and Administration
For intramuscular injection only.
2.1 MENVEO Presentations
MENVEO is supplied in two presentations, a two-vial presentation and a one-vial presentation.
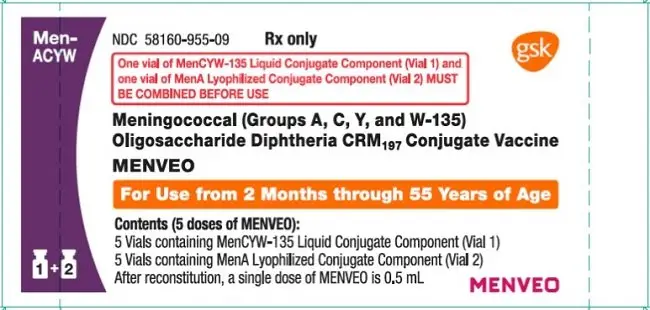
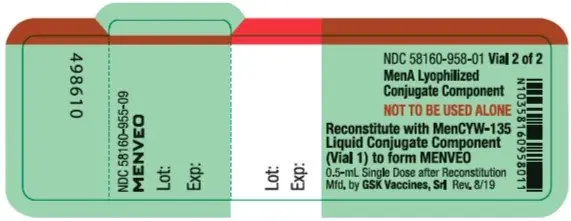
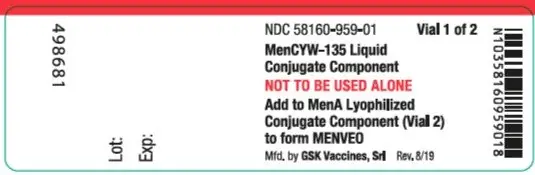
Two-Vial Presentation
The two-vial presentation includes a vial with a gray cap containing the MenCYW-135 liquid conjugate component and a vial with an orange cap containing the MenA lyophilized conjugate component. The contents of the vials must be combined to form MENVEO prior to administration. This presentation is for use in individuals 2 months through 55 years of age.
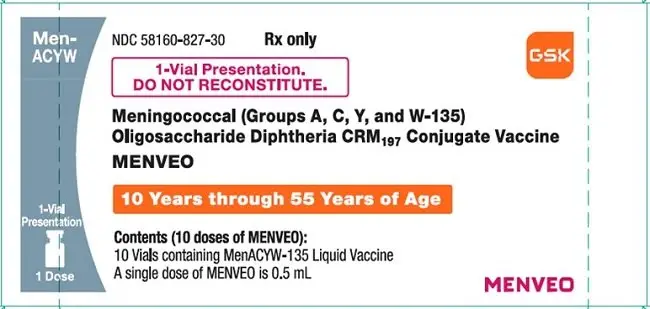
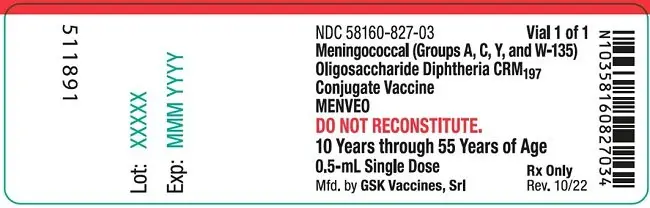
One-Vial Presentation
The one-vial presentation contains MENVEO in a single vial with a pink cap and does not require reconstitution before use. This presentation is for use in individuals 10 through 55 years of age.
2.2 Preparation
Reconstitution Instructions for MENVEO Two-Vial Presentation
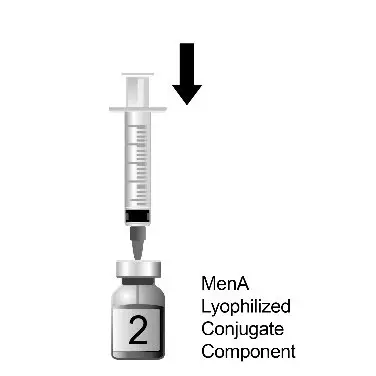
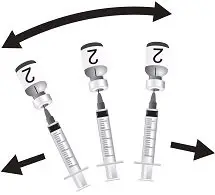
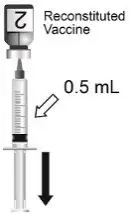
Use the MenCYW-135 liquid conjugate component (Vial 1, gray cap) to reconstitute the MenA lyophilized conjugate component (Vial 2, orange cap) to form MENVEO. Invert Vial 2 and shake well until the lyophilized conjugate component is dissolved. After reconstitution, withdraw 0.5 mL from the vial containing the reconstituted vaccine. See Figures 1 through 4.
Administer MENVEO immediately or store between 36°F and 77°F (2°C and 25°C) for up to 8 hours. Shake well before using. Discard reconstituted vaccine if it has been frozen or not used within 8 hours.
Instructions for MENVEO One-Vial Presentation
The MENVEO presentation that is supplied in a single vial with a pink cap does NOT require reconstitution. Withdraw 0.5 mL from the vial.
2.3 Administration
MENVEO is a clear, colorless solution, free from visible foreign particles. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. If any of these conditions exist, MENVEO should not be administered.
Administer a single 0.5-mL dose by intramuscular injection.
2.4 Dosing Schedule
The dosing schedule is as follows:
Primary Vaccination
Table 1. Dosing Schedule for MENVEO Primary Vaccination
| MENVEO Two-Vial Presentation | |
|---|---|
|
Infants Aged 2 Months |
4-dose series at 2, 4, 6, and 12 months of age |
|
Children Aged 7 through 23 Months |
2-dose series with the second dose administered in the second year of life and at least 3 months after the first dose |
|
Children Aged 2 through 10 Years |
A single dose For children aged 2 through 5 years at continued high risk of meningococcal disease, a second dose may be administered 2 months after the first dose. |
|
Adolescents and Adults Aged 11 through 55 Years |
A single dose |
|
MENVEO One-Vial Presentation |
|
|
Adolescents and Adults Aged 10 through 55 Years |
A single dose |
Booster Vaccination
Adolescents and Adults Aged 15 through 55 Years: A single booster dose of MENVEO using either the two-vial presentation or the one-vial presentation may be administered to individuals who are at continued risk for meningococcal disease if at least 4 years have elapsed since a prior dose of a meningococcal (serogroups A, C, Y, W-135) conjugate vaccine.
3. Dosage Forms and Strengths
MENVEO is a solution for intramuscular injection. A single dose is 0.5 mL.
4. Contraindications
Do not administer MENVEO to individuals with a severe allergic reaction (e.g., anaphylaxis) to a previous dose of MENVEO, to any component of this vaccine, or to any other diphtheria toxoid-containing vaccine. [See Description (11).]
5. Warnings and Precautions
5.1 Management of Acute Allergic Reactions
Appropriate medical treatment must be available should an acute allergic reaction, including an anaphylactic reaction, occur following administration of MENVEO.
5.2 Syncope
Syncope (fainting) has occurred in association with administration of MENVEO. Procedures should be in place to avoid injury from fainting.
5.3 Altered Immunocompetence
Reduced Immune Response
Some individuals with altered immunocompetence, including some individuals receiving immunosuppressant therapy, may have reduced immune responses to MENVEO.
Complement Deficiency
Persons with certain complement deficiencies and persons receiving treatment that inhibits terminal complement activation (for example, eculizumab) are at increased risk for invasive disease caused by N. meningitidis, including invasive disease caused by serogroups A, C, Y, and W, even if they develop antibodies following vaccination with MENVEO. [See Clinical Pharmacology (12.1).]
5.4 Guillain-Barré Syndrome
Guillain-Barré syndrome (GBS) has been reported in temporal relationship following administration of another U.S.-licensed meningococcal quadrivalent polysaccharide conjugate vaccine. The decision by the healthcare professional to administer MENVEO to persons with a history of GBS should take into account the expected benefits and potential risks.
5.5 Apnea in Premature Infants
Apnea following intramuscular vaccination has been observed in some infants born prematurely. A decision about when to administer MENVEO to an infant born prematurely should be based on consideration of the individual infant's medical status and the potential benefits and possible risks of vaccination.
6. Adverse Reactions/Side Effects
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of a vaccine cannot be directly compared with rates in the clinical trials of another vaccine and may not reflect the rates observed in practice.
Overall, in clinical studies, 36,146 individuals 2 months through 55 years of age were administered at least one dose of MENVEO supplied in the two-vial presentation and 1,337 individuals 10 through 44 years of age were administered one dose of MENVEO supplied in the one-vial presentation. The safety data for the two-vial presentation are relevant to the safety of the one-vial presentation because each presentation contains the same meningococcal conjugated oligosaccharides. [See Description (11).]
Primary Vaccination Studies
Children Aged 2 through 23 Months: The safety of MENVEO in infants vaccinated at 2, 4, 6, and 12 months of age was evaluated in 3 randomized multicenter clinical studies (NCT00474526, NCT00806195, NCT01000311) conducted in the U.S., Australia, Canada, Taiwan, and several countries of Latin America in which 8,735 infants received at least 1 dose of MENVEO and routine infant vaccines (diphtheria toxoid; acellular pertussis; tetanus toxoid [DTaP]; inactivated polio types 1, 2, and 3 [IPV]; hepatitis B; Haemophilus influenzae type b (Hib) antigens; pentavalent rotavirus; and 7-valent pneumococcal conjugate [PCV7]). With Dose 4 of MENVEO, toddlers received concomitantly the following vaccines: 7-valent pneumococcal conjugate; measles, mumps, rubella, and varicella; and inactivated hepatitis A. A total of 2,864 infants in these studies received the routine infant/toddler vaccines only. The infants who received MENVEO were Caucasian (33%), Hispanic (44%), African American (8%), Asian (8%), and other racial/ethnic groups (7%); 51% were male, with a mean age of 65.1 days (Standard Deviation [SD]: 7.5 days) at the time of first vaccination.
Safety data for administration of 2 doses of MENVEO in children aged 6 through 23 months are available from 3 randomized studies (NCT00474526, NCT00310856, NCT00626327) conducted in the U.S., Latin America, and Canada, of which one U.S. study specifically addressed the safety of MENVEO administered concomitantly with measles, mumps, rubella, and varicella vaccine (MMRV). The 1,985 older infants and toddlers who received 2 doses of MENVEO were Caucasian (49%), Hispanic (32%), African American (11%), and other racial/ethnic groups (8%), 51% male, with a mean age of 10.1 months (SD: 2.0 months).
Children Aged 2 through 10 Years: The safety of MENVEO in children aged 2 through 10 years was evaluated in 4 clinical trials (NCT00310817, NCT00262028, NCT00329849, NCT00616421) conducted in North America (66%), Latin America (28%), and Europe (6%) in which 3,181 subjects received MENVEO and 2,116 subjects received comparator vaccines (either Meningococcal Polysaccharide Vaccine, Groups A, C, Y, and W-135 Combined - MENOMUNE, Sanofi Pasteur [n = 861], or Meningococcal (Groups A, C, Y, and W-135) Polysaccharide Diphtheria Toxoid Conjugate Vaccine - MENACTRA, Sanofi Pasteur [n = 1,255]). The subjects aged 2 through 10 years who received MENVEO were Caucasian (69%), Hispanic (13%), African American (7%), and other racial/ethnic groups (6%), 51% male, with a mean age of 5.2 years. The safety of a second dose of MENVEO administered 2 months following a first dose was studied in 351 children aged 2 through 5 years.
Adolescents and Adults: The safety of MENVEO in individuals aged 11 through 55 years was evaluated in 5 randomized controlled clinical trials (NCT01018732, NCT00329901, NCT00450437, NCT00474487, NCT00518180) in which 6,185 participants received MENVEO alone (5,286 participants), MENVEO concomitant with other vaccine(s) (899 participants), or a U.S.-licensed comparator vaccine (1,966 participants). In the concomitant trials (NCT00329901, NCT00518180) MENVEO was given with vaccines containing: tetanus toxoid, diphtheria toxoid, and pertussis (Tdap), or Tdap with human papillomavirus (HPV). The comparator vaccine was either MENOMUNE (209 participants) or MENACTRA (1,757 participants). The trials were conducted in North America (46%), Latin America (41%), and Europe (13%). In 2 of the studies, subjects received concomitant vaccination with Tdap or with Tdap plus HPV. Overall, in these studies, subjects were Caucasian (50%), followed by Hispanic (40%), African American (7%), and other racial/ethnic groups (3%). Among recipients of MENVEO, 61%, 17%, and 22% were in the 11- through 18-year, 19- through 34-year, and 35- through 55-year age groups, respectively, with a mean age of 23.5 years (SD: 12.9 years). Among recipients of MENACTRA, 31%, 32%, and 37% were in the 11- through 18-year, 19- through 34-year, and 35- through 55-year age groups, respectively, with a mean age of 29.2 years (SD: 13.4 years). Among MENOMUNE recipients, 100% were in the 11- through 18-year age group, and the mean age was 14.2 years (SD: 1.8 years).
The safety of MENVEO one-vial presentation was evaluated in 2 randomized clinical trials (NCT03652610, NCT03433482). In these studies, 1,337 subjects aged 10 through 44 years were administered a single dose of MENVEO supplied in the one‑vial presentation and contributed to study analyses and 1,332 subjects 10 through 40 years of age were administered MENVEO supplied in the two-vial presentation. The studies were conducted in Australia, Belgium, Canada, Germany, and Italy (NCT03652610), and in Brazil, Estonia, Finland, France, Mexico, Russian Federation, South Africa, Spain, and Turkey (NCT03433482). Overall, in these studies, subjects were White (80.8%), followed by Hispanic or Latino ethnicity (12.8%), other racial groups (11.4%), African American (4.3%), Asian (3.0%), American Indian or Alaskan Native (0.3%), and Native Hawaiian or other Pacific Islander (0.1%). Overall, 25.6% of individuals were aged 10 through 17 years, and 74.4% were aged 18 through 44 years.
Booster Vaccination Study
In a multicenter, open-label trial (NCT02986854) conducted in the U.S., 601 subjects aged 15 to 51 years received a single booster dose of MENVEO 4 to 6 years after prior vaccination with MENVEO (n = 301; median age: 16 years) or MENACTRA (n = 300; median age: 16 years). Across booster groups of MENVEO, 81% of subjects were White and 50% were female.
In most trials, solicited local and systemic adverse reactions were monitored daily for 7 days following each (one or more) vaccination and recorded on a diary card. Participants were monitored for unsolicited adverse events which included adverse events requiring a physician visit or Emergency Department visit (i.e., medically-attended) or which led to a subject’s withdrawal from the study. Among children, adolescents, and adults aged 2 to 55 years, medically significant adverse events and serious adverse events (SAEs) were monitored for 6 months after vaccination. Across the studies of infants and toddlers aged 2 through 23 months, either all medically-attended or all medically-significant adverse events were collected in the period between the infant dose(s) and the toddler doses and during the 6-month period after the toddler dose.
Solicited Adverse Reactions in the Primary Vaccination Studies
The reported frequencies of solicited local and systemic adverse reactions from U.S. infants in the largest multinational safety study of MENVEO (NCT00806195) are presented in Table 2. Among the U.S. participants in the group receiving MENVEO with routine vaccines, 51% were female; 64% were Caucasian, 12% were African American, 15% were Hispanic, 2% were Asian, and 7% were of other racial/ethnic groups.
In infants initiating vaccination at 2 months of age and receiving the 4-dose series, common solicited adverse reactions (>10%) were tenderness (24% to 41%) and erythema at injection site (11% to 15%), irritability (42% to 57%), sleepiness (29% to 50%), persistent crying (21% to 41%), change in eating habits (17% to 23%), vomiting (5% to 11%), and diarrhea (8% to 16%). The rates of solicited adverse reactions reported for subjects aged 2 months and older receiving MENVEO with routine vaccines at 2, 4, 6, and 12 months of age were comparable to rates among subjects who only received routine vaccines.
| Adverse Reactions | Dose 1 | Dose 2 | Dose 3 | Dose 4 | ||||
|---|---|---|---|---|---|---|---|---|
| MENVEO
with Routineb % | Routine
Vaccinesb % | MENVEO
with Routineb % | Routine
Vaccinesb % | MENVEO
with Routineb % | Routine
Vaccinesb % | MENVEO
with Routineb % | Routine
Vaccinesb % |
|
| Clinicaltrials.gov Identifier NCT00806195. n = Number of subjects who completed the diary card for a given symptom at the specified vaccination. a As-Treated Safety Subpopulation = U.S. children who received at least 1 dose of study vaccine and whose diary cards were completed per protocol and returned to the site. b Routine infant/toddler vaccines include DTaP-IPV-Hib and PCV7 at Doses 1, 2, 3, and PCV7, MMRV, and Hepatitis A vaccines at Dose 4. HBV and rotavirus vaccines were allowed according to Advisory Committee on Immunization Practices (ACIP) recommendations. c Local reactogenicity of MENVEO and PCV7 was assessed. d Tenderness, severe = Cried when injected limb moved. e Irritability, severe = Unable to console. f Sleepiness, severe = Sleeps most of the time, hard to arouse. g Change in eating habits, severe = Missed >2 feeds. h Vomiting, severe = Little/no intake for more prolonged time. i Diarrhea, severe = ≥6 liquid stools, no solid consistency. j Rash was assessed only as present or not present, without a grading for severity. k Axillary temperature. |
||||||||
|
Local Adverse Reactionsc |
n = 1,250-1,252 |
n = 428 |
n = 1,205-1,207 |
n = 399 |
n = 1,056-1,058 |
n = 351-352 |
n = 1,054-1,055 |
n = 334-337 |
|
Tenderness, any |
41 |
45 |
31 |
36 |
24 |
32 |
29 |
39 |
|
Tenderness, severed |
3 |
5 |
2 |
2 |
1 |
3 |
1 |
1 |
|
Erythema, any |
11 |
14 |
12 |
21 |
14 |
23 |
15 |
25 |
|
Erythema, >50 mm |
<1 |
<1 |
0 |
0 |
0 |
0 |
0 |
0 |
|
Induration, any |
8 |
16 |
9 |
17 |
8 |
19 |
8 |
21 |
|
Induration, >50 mm |
0 |
<1 |
0 |
0 |
0 |
0 |
0 |
0 |
|
Systemic Adverse Reactions |
n = 1,246-1,251 |
n = 427-428 |
n = 1,119-1,202 |
n = 396-398 |
n = 1,050-1,057 |
n = 349-350 |
n = 1,054-1,056 |
n = 333-337 |
|
Irritability, any |
57 |
59 |
48 |
46 |
42 |
38 |
43 |
42 |
|
Irritability, severee |
2 |
2 |
1 |
3 |
1 |
1 |
2 |
1 |
|
Sleepiness, any |
50 |
50 |
37 |
36 |
30 |
30 |
29 |
27 |
|
Sleepiness, severef |
2 |
1 |
1 |
1 |
<1 |
<1 |
1 |
0 |
|
Persistent crying, any |
41 |
38 |
28 |
24 |
22 |
17 |
21 |
18 |
|
Persistent crying, ≥3 hours |
2 |
2 |
2 |
2 |
1 |
1 |
1 |
1 |
|
Change in eating habits, any |
23 |
24 |
18 |
17 |
17 |
13 |
19 |
16 |
|
Change in eating habits, severeg |
1 |
1 |
1 |
1 |
1 |
<1 |
1 |
0 |
|
Vomiting, any |
11 |
9 |
7 |
6 |
6 |
4 |
5 |
4 |
|
Vomiting, severeh |
<1 |
0 |
<1 |
0 |
<1 |
0 |
<1 |
0 |
|
Diarrhea, any |
16 |
11 |
11 |
8 |
8 |
6 |
13 |
9 |
|
Diarrhea, severei |
<1 |
<1 |
<1 |
<1 |
1 |
<1 |
1 |
1 |
|
Rashj |
3 |
3 |
3 |
4 |
3 |
3 |
4 |
3 |
|
Fever ≥38.0°Ck |
3 |
2 |
4 |
6 |
7 |
6 |
9 |
7 |
|
Fever 38.0-38.9°C |
3 |
2 |
4 |
5 |
7 |
6 |
6 |
5 |
|
Fever 39.0-39.9°C |
0 |
0 |
1 |
1 |
<1 |
0 |
2 |
2 |
|
Fever ≥40.0°C |
0 |
<1 |
0 |
<1 |
0 |
0 |
<1 |
0 |
The safety of a second dose of MENVEO administered at 12 months of age concomitantly with MMRV was investigated in a randomized, controlled, multicenter study (NCT00626327) conducted in the U.S. The rates of solicited adverse reactions reported were comparable between the concomitantly administered group (MENVEO with MMRV) and the group which received MMRV alone or MENVEO alone. The frequency and severity of solicited local and systemic reactions occurring within 7 days following vaccination at 12 months of age are shown in Table 3. In subjects who received both MENVEO and MMRV at 12 months of age local reactions at both injection sites were evaluated separately. Body temperature measurements were collected for 28 days following the 12-months-of-age visit, when MMRV was administered to the vaccinees. Common solicited adverse reactions (≥10%) among children initiating vaccination at 7 months through 23 months of age and receiving the 2-dose series were tenderness (10% to 16%) and erythema at injection site (12% to 15%), irritability (27% to 40%), sleepiness (17% to 29%), persistent crying (12% to 21%), change in eating habits (12% to 20%), and diarrhea (10% to 16%). An examination of the fever profile during this period showed that MENVEO administered with MMRV did not increase the frequency or intensity of fever above that observed for the MMRV-only group.
| Adverse Reactions | MENVEO | MENVEO + MMRV | MMRV | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MENVEO
7-9 Months % | MENVEO
12 Months % | MENVEO
7-9 Months % | MENVEO with MMRV
12 Months % | MMRV
12 Months % |
||||||||||
| Clinicaltrials.gov Identifier NCT00626327. n = Number of subjects who completed the diary card for a given symptom at the specified vaccination. a As-Treated Safety Subpopulation = U.S. children who received at least 1 dose of study vaccine and whose diary cards were completed per protocol and returned to the site. b Tenderness, severe = Cried when injected limb moved. c Irritability, severe = Unable to console. d Sleepiness, severe = Sleeps most of the time, hard to arouse. e Change in eating habits, severe = Missed >2 feeds. f Vomiting, severe = Little/no intake for more prolonged time. g Diarrhea, severe = ≥6 liquid stools, no solid consistency. h Rash was assessed only as present or not present, without a grading for severity. i Axillary temperature. |
||||||||||||||
|
Local Adverse Reactions– MENVEO |
n = 460-462 |
n = 381-384 |
n = 430-434 |
n = 386-387 | ||||||||||
|
Tenderness, any |
11 |
10 |
11 |
16 |
N/A |
|||||||||
|
Tenderness, severeb |
<1 |
<1 |
<1 |
0 |
N/A |
|||||||||
|
Erythema, any |
15 |
13 |
13 |
12 |
N/A |
|||||||||
|
Erythema, >50 mm |
<1 |
<1 |
0 |
1 |
N/A |
|||||||||
|
Induration, any |
8 |
8 |
7 |
8 |
N/A |
|||||||||
|
Induration, >50 mm |
<1 |
<1 |
0 |
1 |
N/A |
|||||||||
|
Local Adverse Reactions– MMRV |
n = 382-383 |
n = 518-520 |
||||||||||||
|
Tenderness, any |
N/A |
N/A |
N/A |
16 |
19 |
|||||||||
|
Tenderness, severeb |
N/A |
N/A |
N/A |
0 |
<1 |
|||||||||
|
Erythema, any |
N/A |
N/A |
N/A |
15 |
14 |
|||||||||
|
Erythema, >50 mm |
N/A |
N/A |
N/A |
1 |
<1 |
|||||||||
|
Induration, any |
N/A |
N/A |
N/A |
13 |
8 |
|||||||||
|
Induration, >50 mm |
N/A |
N/A |
N/A |
<1 |
0 |
|||||||||
|
Systemic Adverse Reactions |
n = 461-463 |
n = 385-386 |
n = 430-434 |
n = 387-389 |
n = 522-524 |
|||||||||
|
Irritability, any |
40 |
27 |
37 |
37 |
44 |
|||||||||
|
Irritability, severec |
2 |
2 |
2 |
1 |
3 |
|||||||||
|
Sleepiness, any |
26 |
17 |
29 |
26 |
32 |
|||||||||
|
Sleepiness, severed |
2 |
1 |
1 |
1 |
2 |
|||||||||
|
Persistent crying, any |
21 |
12 |
20 |
19 |
20 |
|||||||||
|
Persistent crying, ≥3 hours |
2 |
1 |
1 |
1 |
2 |
|||||||||
|
Change in eating habits, any |
17 |
12 |
17 |
20 |
20 |
|||||||||
|
Change in eating habits, severee |
<1 |
1 |
1 |
2 |
1 |
|||||||||
|
Vomiting, any |
9 |
6 |
9 |
6 |
6 |
|||||||||
|
Vomiting, severef |
<1 |
<1 |
<1 |
<1 |
<1 |
|||||||||
|
Diarrhea, any |
16 |
10 |
15 |
15 |
20 |
|||||||||
|
Diarrhea, severeg |
2 |
1 |
<1 |
1 |
2 |
|||||||||
|
Rashh |
3 |
5 |
6 |
6 |
8 |
|||||||||
|
Fever ≥38.0°Ci |
5 |
5 |
6 |
9 |
7 |
|||||||||
|
Fever 38.0-38.9°C |
3 |
3 |
5 |
7 |
7 |
|||||||||
|
Fever 39.0-39.9°C |
2 |
2 |
1 |
1 |
1 |
|||||||||
|
Fever ≥40.0°C |
<1 |
1 |
<1 |
<1 |
0 |
|||||||||
In clinical trials of children aged 2 through 10 years (NCT00310817, NCT00262028, NCT00329849, NCT00616421), the most frequently occurring adverse reactions (>10%) among all subjects who received MENVEO were injection site pain (31%), erythema (23%), irritability (18%), induration (16%), sleepiness (14%), malaise (12%), and headache (11%). Among subjects aged 11 through 55 years, the most frequently occurring adverse reactions (>10%) among all subjects who received MENVEO were pain at the injection site (41%), headache (30%), myalgia (18%), malaise (16%), and nausea (10%).
The rates of solicited adverse reactions reported for subjects aged 2 through 5 years and 6 through 10 years who received a single dose of MENVEO or MENACTRA in a randomized, controlled, multicenter study (NCT00616421) conducted in the U.S. and Canada are shown in Table 4. Following a second dose of MENVEO administered to children aged 2 through 5 years, the most common solicited adverse reactions (≥10%) were pain at injection site (28%), erythema (22%), irritability (16%), induration (13%), and sleepiness (12%). The solicited adverse reactions from a separate randomized, controlled, multicenter study conducted in the U.S. in adolescents and adults (NCT00450437) are provided in Tables 5 and 6, respectively. In neither study were concomitant vaccines administered with the study vaccines.
| Adverse Reactions | Participants Aged 2 through 5 Years | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MENVEO
n = 693 % | MENACTRA
n = 684 % |
||||||||||||||||||||
| Any | Moderate | Severe | Any | Moderate | Severe | ||||||||||||||||
| Clinicaltrials.gov Identifier NCT00616421. a Moderate: Some limitation in normal daily activity, Severe: Unable to perform normal daily activity. b Moderate: ≥50-100 mm, Severe: >100 mm. c Rash was assessed only as present or not present, without a grading for severity. d Fever grading: Any: ≥38°C, Moderate: 39-39.9°C, Severe: ≥40°C. Parents reported the use of antipyretic medication to treat or prevent symptoms in 11% and 13% of subjects aged 2 through 5 years, 9% and 10% of subjects aged 6 through 10 years for MENVEO and MENACTRA, respectively. e Different systemic reactions were solicited in different age groups. |
|||||||||||||||||||||
|
Local Adverse Reactions |
|||||||||||||||||||||
|
Injection site paina |
33 |
6 |
1 |
35 |
8 |
0.4 |
|||||||||||||||
|
Erythemab |
27 |
5 |
1 |
25 |
3 |
0.3 |
|||||||||||||||
|
Indurationb |
18 |
2 |
0.4 |
18 |
2 |
0.3 |
|||||||||||||||
|
Systemic Adverse Reactionse |
|||||||||||||||||||||
|
Irritabilitya |
21 |
6 |
1 |
22 |
7 |
1 |
|||||||||||||||
|
Sleepinessa |
16 |
3 |
1 |
18 |
5 |
1 |
|||||||||||||||
|
Change in eatinga |
9 |
2 |
1 |
10 |
2 |
0.3 |
|||||||||||||||
|
Diarrheaa |
7 |
1 |
0.1 |
8 |
1 |
0 |
|||||||||||||||
|
Headachea |
5 |
1 |
0 |
6 |
1 |
0.3 |
|||||||||||||||
|
Rashc |
4 |
- |
- |
5 |
- |
- |
|||||||||||||||
|
Arthralgiaa |
3 |
1 |
0.1 |
4 |
1 |
0 |
|||||||||||||||
|
Vomitinga |
3 |
1 |
0.1 |
3 |
1 |
0 |
|||||||||||||||
|
Feverd |
2 |
0.4 |
0 |
2 |
0.3 |
0 |
|||||||||||||||
|
Participants Aged 6 through 10 Years |
|||||||||||||||||||||
|
Adverse Reactions |
MENVEO n = 582 % |
MENACTRA n = 571 % |
|||||||||||||||||||
|
Any |
Moderate |
Severe |
Any |
Moderate |
Severe |
||||||||||||||||
|
Local Adverse Reactions |
|||||||||||||||||||||
|
Injection site paina |
39 |
8 |
1 |
45 |
10 |
2 |
|||||||||||||||
|
Erythemab |
28 |
5 |
1 |
22 |
2 |
0.2 |
|||||||||||||||
|
Indurationb |
17 |
2 |
0.3 |
13 |
2 |
0 |
|||||||||||||||
|
Systemic Adverse Reactionse |
|||||||||||||||||||||
|
Headachea |
18 |
3 |
1 |
13 |
2 |
1 |
|||||||||||||||
|
Malaisea |
14 |
3 |
1 |
11 |
3 |
1 |
|||||||||||||||
|
Myalgiaa |
10 |
2 |
1 |
10 |
2 |
1 |
|||||||||||||||
|
Nauseaa |
8 |
2 |
1 |
6 |
2 |
0.4 |
|||||||||||||||
|
Arthralgiaa |
6 |
1 |
0 |
4 |
1 |
0.4 |
|||||||||||||||
|
Chillsa |
5 |
1 |
0 |
5 |
1 |
0.4 |
|||||||||||||||
|
Rashc |
5 |
- |
- |
3 |
- |
- |
|||||||||||||||
|
Feverd |
2 |
1 |
0 |
2 |
0 |
0.4 |
|||||||||||||||
| Adverse Reactions | MENVEO
n = 1,631 % | MENACTRA
n = 539 % |
||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Any | Moderate | Severe | Any | Moderate | Severe | |||||||||||||||||||||||
| Clinicaltrials.gov Identifier NCT00450437. a Moderate: Some limitation in normal daily activity, Severe: Unable to perform normal daily activity. b Moderate: ≥50-100 mm, Severe: >100 mm. c Rash was assessed only as present or not present, without a grading for severity. d Fever grading: Any: ≥38°C, Moderate: 39-39.9°C, Severe: ≥40°C. |
||||||||||||||||||||||||||||
|
Local Adverse Reactions |
||||||||||||||||||||||||||||
|
Injection site paina |
44 |
9 |
1 |
53 |
11 |
1 |
||||||||||||||||||||||
|
Erythemab |
15 |
2 |
0.4 |
16 |
1 |
0 |
||||||||||||||||||||||
|
Indurationb |
12 |
2 |
0.2 |
11 |
1 |
0 |
||||||||||||||||||||||
|
Systemic Adverse Reactions |
||||||||||||||||||||||||||||
|
Headachea |
29 |
8 |
2 |
28 |
7 |
1 |
||||||||||||||||||||||
|
Myalgiaa |
19 |
4 |
1 |
18 |
5 |
0.4 |
||||||||||||||||||||||
|
Nauseaa |
12 |
3 |
1 |
9 |
2 |
1 |
||||||||||||||||||||||
|
Malaisea |
11 |
3 |
1 |
12 |
5 |
1 |
||||||||||||||||||||||
|
Chillsa |
8 |
2 |
1 |
7 |
1 |
0.2 |
||||||||||||||||||||||
|
Arthralgiaa |
8 |
2 |
0.4 |
6 |
1 |
0 |
||||||||||||||||||||||
|
Rashc |
3 |
- |
- |
3 |
- |
- |
||||||||||||||||||||||
|
Feverd |
1 |
0.4 |
0 |
1 |
0 |
0 |
||||||||||||||||||||||
| Adverse Reactions | MENVEO
n = 1,018 % | MENACTRA
n = 336 % |
|||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Any | Moderate | Severe | Any | Moderate | Severe | ||||||||||||||||||||||||||||||
| Clinicaltrials.gov Identifier NCT00450437. a Moderate: Some limitation in normal daily activity, Severe: Unable to perform normal daily activity. b Moderate: ≥50-100 mm, Severe: >100 mm. c Rash was assessed only as present or not present, without a grading for severity. d Fever grading: Any: ≥38°C, Moderate: 39-39.9°C, Severe: ≥40°C. |
|||||||||||||||||||||||||||||||||||
|
Local Adverse Reactions |
|||||||||||||||||||||||||||||||||||
|
Injection site paina |
38 |
7 |
0.3 |
41 |
6 |
0 |
|||||||||||||||||||||||||||||
|
Erythemab |
16 |
2 |
1 |
12 |
1 |
0 |
|||||||||||||||||||||||||||||
|
Indurationb |
13 |
1 |
0.4 |
9 |
0.3 |
0 |
|||||||||||||||||||||||||||||
|
Systemic Adverse Reactions |
|||||||||||||||||||||||||||||||||||
|
Headachea |
25 |
7 |
2 |
25 |
7 |
1 |
|||||||||||||||||||||||||||||
|
Myalgiaa |
14 |
4 |
0.5 |
15 |
3 |
1 |
|||||||||||||||||||||||||||||
|
Malaisea |
10 |
3 |
1 |
10 |
2 |
1 |
|||||||||||||||||||||||||||||
|
Nauseaa |
7 |
2 |
0.4 |
5 |
1 |
0.3 |
|||||||||||||||||||||||||||||
|
Arthralgiaa |
6 |
2 |
0.4 |
6 |
1 |
1 |
|||||||||||||||||||||||||||||
|
Chillsa |
4 |
1 |
0.1 |
4 |
1 |
0 |
|||||||||||||||||||||||||||||
|
Rashc |
2 |
- |
- |
1 |
- |
- |
|||||||||||||||||||||||||||||
|
Feverd |
1 |
0.3 |
0 |
1 |
0.3 |
0 |
|||||||||||||||||||||||||||||
In studies NCT03652610 and NCT03433482, there were no notable differences in frequency and severity of solicited adverse reactions within 7 days following vaccination in individuals who received the one-vial presentation compared to individuals who received the two-vial presentation.
Solicited Adverse Reactions in the Booster Vaccination Study (Adolescents and Adults)
A multicenter, open-label clinical trial (NCT02986854) was conducted in the U.S. in subjects aged 15 through 55 years [see Clinical Studies (14.1)]. The methodology for evaluating solicited adverse reactions, unsolicited adverse events, and SAEs after a booster dose of MENVEO was similar to the primary vaccination studies. The most common solicited local and systemic adverse reactions within 7 days of vaccination were pain at injection site (36%) and fatigue (38%), respectively.
Solicited Adverse Reactions following Concomitant Vaccine Administration
The safety of 4-dose series of MENVEO administered concomitantly with U.S.-licensed routine infant and toddler vaccines was evaluated in one pivotal trial (NCT00806195). The safety of a 2-dose series of MENVEO initiated at 7-9 months of age, with the second dose administered concomitantly with U.S.-licensed MMRV vaccine at 12 months of age, was evaluated in one pivotal trial (NCT00626327). Rates of solicited adverse reactions which occurred 7 days following vaccination are shown in Tables 2 and 3, respectively. There was no significant increase in the rates of solicited systemic or local reactions observed in recipients of routine childhood vaccines when concomitantly vaccinated with MENVEO. [See Drug Interactions (7.1).]
The safety of MENVEO administered concomitantly with Tdap and HPV was evaluated in a single-center study (NCT00518180) conducted in Costa Rica. Solicited local and systemic adverse reactions were reported as noted above. In this study, subjects aged 11 through 18 years received MENVEO concomitantly with Tdap and HPV (n = 540), or MENVEO followed 1 month later by Tdap and then 1 month later by HPV (n = 541), or Tdap followed 1 month later by MENVEO and then 1 month later by HPV (n = 539). Some solicited systemic adverse reactions were more frequently reported in the group that received MENVEO, Tdap, and HPV concomitantly, (headache 40%, malaise 25%, myalgia 27%, and arthralgia 17%) compared with the group that first received MENVEO alone (headache 36%, malaise 20%, myalgia 19%, and arthralgia 11%). Among subjects administered MENVEO alone (1 month prior to Tdap), 36% reported headache, 20% malaise, and 16% myalgia. Among subjects administered MENVEO 1 month after Tdap, 27% reported headache, 18% malaise, and 16% myalgia.
Serious Adverse Events in All Safety Studies
SAEs in subjects receiving a 4-dose series of MENVEO at 2, 4, 6, and 12 months were evaluated in 3 randomized, multicenter clinical studies (NCT00474526, NCT00806195, NCT01000311). In the 2 controlled studies (NCT00806195, NCT01000311), the proportions of infants randomized to receive the 4-dose series of MENVEO concomitantly with routine vaccinations and infants who received routine vaccinations alone that reported SAEs during different study periods were, respectively: a) 2.7% and 2.2% during the infant series, b) 2.5% and 2.5% between the infant series and the toddler dose, c) 0.3% and 0.3% in the 1 month following the toddler dose, and d) 1.6% and 2.2% during the 6-month follow-up period after the last dose. In the third study (NCT00474526), which was controlled up to the toddler dose, the proportions of infants randomized to dosing regimens that included receiving 4 doses of MENVEO concomitantly with routine vaccinations at 2, 4, 6, and 12 months and infants who received routine vaccinations alone that reported SAEs during different study periods were, respectively: a) 3.5% and 3.6% during the infant series, and b) 2.8% and 3.3% between the infant series and the toddler dose, and c) 0.5% and 0.7% in the 1 month following the toddler dose. In the same study, 1.9% of infants randomized to receive the 4-dose series of MENVEO concomitantly with routine vaccinations reported SAEs during the 6-month follow-up period after the toddler dose. The most common SAEs reported in these 3 studies were wheezing, pneumonia, gastroenteritis, and convulsions, and most occurred at highest frequency after the infant series.
In a study of older infants (NCT00626327) randomized to receive the 2-dose series of MENVEO concomitantly with MMRV at 12 months of age, the rates of SAEs during the study, including the 6-month follow-up period after the last dose, were 3.6% and 3.8% for the groups receiving MENVEO with MMRV and MENVEO only, respectively. Infants receiving MMRV alone, who had a shorter period of study participation as they were enrolled at 12 months of age, had a lower rate of SAEs (1.5%). Among 1,597 study subjects included in the safety population, the most commonly reported SAEs in all study arms combined were dehydration (0.4%) and gastroenteritis (0.3%). Across the submitted studies of individuals aged 2 through 23 months within 28 days of vaccination, 2 deaths were reported in the groups receiving MENVEO (one case of sudden death and one case of sepsis), while no deaths were reported in the control group. None of the deaths was assessed as related to vaccination. Among subjects with symptom onset within 42 days of vaccination (Days 12, 25, 29), 3/12,049 (0.02%, 95% CI: [0.01%, 0.07%]) recipients of MENVEO and 0/2,877 (0%, 95% CI: [0%, 0.13%]) control recipients were diagnosed with Kawasaki Disease. One case of acute disseminated encephalomyelitis with symptom onset 29 days post Dose 4 was observed in a participant given MENVEO coadministered with routine U.S. childhood vaccines at 12 months of age (including measles, mumps, and rubella vaccine [MMR] and varicella vaccine).
The information regarding SAEs in subjects aged 2 through 10 years was derived from 3 randomized, controlled clinical trials (NCT00262028, NCT00329849, NCT00616421). Safety follow-up ranged from 6 through 12 months and included 2,883 subjects administered MENVEO. SAEs reported during the safety follow-up periods occurred in 21/2,883 (0.7%) subjects receiving MENVEO, in 7/1,255 (0.6%) MENACTRA subjects, and 2/861 (0.2%) MENOMUNE subjects. In the subjects receiving either 1 or 2 doses of MENVEO, there were 6 subjects with pneumonia, 3 subjects with appendicitis, and 2 subjects with dehydration; all other events were reported to occur in one subject. Among 1,255 subjects administered a single dose of MENACTRA and 861 subjects administered MENOMUNE, there were no events reported to occur in more than 1 subject. The SAEs occurring within the first 30 days after receipt of each vaccine were as follows: MENVEO (6/2,883 [0.2%]) — appendicitis, pneumonia, staphylococcal infection, dehydration, febrile convulsion, and tonic convulsion; MENACTRA (1/1255 [0.1%]) — inguinal hernia; MENOMUNE (2/861 [0.2%]) — abdominal pain, lobar pneumonia. In a supportive study (NCT00310817), 298 subjects received 1 or 2 doses of MENVEO and 22 (7%) had SAEs over a 13-month follow-up period including 13 subjects with varicella and 2 subjects with laryngitis. All other events were reported to occur in 1 subject. During the 30 days post vaccination in this study, 1 limb injury and 1 case of varicella were reported.
The information regarding SAEs in subjects aged 11 through 55 years was derived from 5 randomized, controlled clinical trials (NCT01018732, NCT00329901, NCT00450437, NCT00474487, NCT00518180). SAEs reported within 6 months of vaccination occurred in 40/6,185 (0.6%) subjects receiving MENVEO, 13/1,757 (0.7%) MENACTRA subjects, and 5/209 (2.4%) MENOMUNE subjects. During the 6 months following immunization, SAEs reported by more than 1 subject were as follows: MENVEO - appendicitis (3 subjects), road traffic accident (3 subjects), and suicide attempt (5 subjects); MENACTRA - intervertebral disc protrusion (2 subjects); MENOMUNE - none. SAEs that occurred within 30 days of vaccination were reported by 7 of 6,185 (0.1%) subjects in the group receiving MENVEO, 4 of 1,757 (0.2%) subjects in the MENACTRA group, and by none of 209 subjects in the MENOMUNE group. The events that occurred during the first 30 days post immunization with MENVEO were: vitello-intestinal duct remnant, Cushing’s syndrome, viral hepatitis, pelvic inflammatory disease, intentional multiple-drug overdose, simple partial seizure, and suicidal depression. The events that occurred during the first 30 days post immunization with MENACTRA were: herpes zoster, fall, intervertebral disc protrusion, and angioedema.
In the 2 clinical studies (NCT03652610, NCT03433482) which evaluated the safety of the one-vial presentation of MENVEO, SAEs were reported by 14 subjects (1.0%) who received the one-vial presentation of MENVEO and 14 subjects (1.1%) who received the two-vial presentation of MENVEO within the 6-month follow-up period after vaccination. No deaths were reported. None of the SAEs were related to the study vaccines.
6.2 Postmarketing Experience
In addition to reports in clinical trials, the following adverse reactions have been identified during postapproval use of MENVEO. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to the vaccine.
Blood and Lymphatic System Disorders
Local lymphadenopathy.
Ear and Labyrinth Disorders
Hearing impaired, ear pain, vertigo, vestibular disorder.
Eye Disorders
Eyelid ptosis.
General Disorders and Administration Site Conditions
Injection site pruritus; pain; erythema; inflammation; and swelling, including extensive swelling of the vaccinated limb; fatigue; malaise; pyrexia.
Immune System Disorders
Hypersensitivity reactions, including anaphylaxis.
Infections and Infestations
Vaccination site cellulitis.
Injury, Poisoning, and Procedural Complications
Fall, head injury.
Investigation
Alanine aminotransferase increased, body temperature increased.
Musculoskeletal and Connective Tissue Disorders
Arthralgia, bone pain.
Nervous System Disorders
Dizziness, syncope, tonic convulsion, headache, facial paresis, balance disorder.
Respiratory, Thoracic, and Mediastinal Disorders
Oropharyngeal pain.
Skin and Subcutaneous Tissue Disorders
Skin exfoliation.
Postmarketing Observational Safety Study
In a postmarketing observational safety study conducted in a U.S. health maintenance organization, data from electronic health records of 48,899 persons aged 11 through 21 years were used to evaluate pre-specified events of interest following vaccination with MENVEO. Using a self-controlled case series method, Bell’s palsy showed a statistically significant increased risk in the period 1 to 84 days post vaccination compared with the control period, with an overall adjusted relative incidence of 2.9 (95% CI: 1.1-7.5). Among the 8 reported cases of Bell’s palsy, 6 cases occurred in persons who received MENVEO concomitantly with one or more of the following vaccines: Tdap, HPV, and Influenza vaccine. All reported Bell’s palsy cases resolved.
7. Drug Interactions
7.1 Concomitant Administration with Other Vaccines
Do not mix MENVEO or any of its components with any other vaccine or diluent in the same syringe or vial.
In 2 clinical trials of infants initiating vaccination at 2 months of age (NCT00474526, NCT01000311), MENVEO was given concomitantly at 2, 4, and 6 months with routine infant vaccines: diphtheria toxoid; acellular pertussis; tetanus toxoid; inactivated polio types 1, 2, and 3; hepatitis B; Haemophilus influenzae type b antigens; pentavalent rotavirus; and 7-valent pneumococcal conjugate vaccine. For Dose 4 given at 12 months of age, MENVEO was given concomitantly with the following vaccines: 7-valent pneumococcal conjugate, MMRV, or measles, mumps, and rubella vaccine and varicella vaccine (MMR+V), and inactivated hepatitis A. In a clinical trial of older infants (aged 7 months and older) and toddlers (NCT00626327), MENVEO was administered concomitantly with MMRV or MMR+V vaccine(s) at 12 months of age. No immune interference was observed for the concomitantly administered vaccines, including most pneumococcal vaccine serotypes (post Dose 3); no immune interference was observed post Dose 4 for any pneumococcal vaccine serotypes (NCT00474526, NCT01000311). [See Clinical Studies (14.1).]
For children aged 2 through 10 years, no data are available to evaluate safety and immunogenicity of other childhood vaccines when administered concomitantly with MENVEO.
In a clinical trial in adolescents (NCT00518180), MENVEO was given concomitantly with the following: Tdap and HPV; no interference was observed in meningococcal immune responses when compared with MENVEO given alone. Lower geometric mean antibody concentrations (GMCs) for antibodies to the pertussis antigens filamentous hemagglutinin (FHA) and pertactin were observed when MENVEO was administered concomitantly with Tdap and HPV as compared with Tdap alone. [See Clinical Studies (14.1).]
7.2 Immunosuppressive Treatments
Immunosuppressive therapies, such as irradiation, antimetabolite medications, alkylating agents, cytotoxic drugs, and corticosteroids (when used in greater than physiologic doses) may reduce the immune response to MENVEO. [See Warnings and Precautions (5.3).] The immunogenicity of MENVEO has not been evaluated in persons receiving such therapies.
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
All pregnancies have a risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
There are no adequate and well-controlled studies of MENVEO in pregnant women in the U.S. There was a pregnancy exposure registry conducted from 2014-2017 that included 82 subjects. Available data do not suggest an increased risk of major birth defects and miscarriage in women who received MENVEO within 28 days prior to conception or during pregnancy (see Data).
A developmental toxicity study was performed in female rabbits administered 0.5 mL (at each occasion) of MENVEO prior to mating and during gestation. A single human dose is 0.5 mL. This study revealed no adverse effects on fetal or pre-weaning development (see Data).
Data
Human Data: A pregnancy exposure registry (2014 to 2017) included 82 pregnancies with known outcomes with exposure within 28 days prior to conception or during pregnancy. Miscarriage was reported for 12.2% of pregnancies with exposure to MENVEO within 28 days prior to conception or during pregnancy (10/82). Major birth defects were reported for 3.6% of live born infants whose mothers were exposed within 28 days prior to conception or during pregnancy (2/55). The rates of miscarriage and major birth defects were consistent with estimated background rates.
Animal Data: In a developmental toxicity study, female rabbits were administered MENVEO by intramuscular injection on Days 29, 15, and 1 prior to mating and on Gestation Days 7 and 20. The total dose was 0.5 mL at each occasion (a single human dose is 0.5 mL). No adverse effects on pre-weaning development up to Postnatal Day 29 were observed. There were no vaccine-related fetal malformations or variations observed.
8.2 Lactation
Risk Summary
It is not known whether the vaccine components of MENVEO are excreted in human milk. Data are not available to assess the effects of MENVEO in the breastfed infant or on milk production/excretion.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for MENVEO and any potential adverse effects on the breastfed child from MENVEO or from the underlying maternal condition. For preventive vaccines, the underlying maternal condition is susceptibility to disease prevented by the vaccine.
8.4 Pediatric Use
Safety and effectiveness of MENVEO in children aged younger than 2 months have not been established.
Safety and effectiveness of the one-vial presentation of MENVEO in children aged younger than 10 years have not been established. [See Dosage and Administration (2).]
For children 2 months through 9 years of age, only the two-vial presentation is approved for use. [See Dosage and Administration (2).]
11. Menveo Description
MENVEO [Meningococcal (Groups A, C, Y, and W-135) Oligosaccharide Diphtheria CRM197 Conjugate Vaccine] is a sterile liquid vaccine administered by intramuscular injection that contains N. meningitidis serogroup A, C, Y, and W-135 oligosaccharides conjugated individually to Corynebacterium diphtheriae CRM197 protein. The polysaccharides are produced by bacterial fermentation of N. meningitidis (serogroups A, C, Y, or W-135). N. meningitidis strains A, C, Y, and W-135 are each cultured and grown on Franz Complete medium and treated with formaldehyde. MenA, MenW-135, and MenY polysaccharides are purified by several extraction and precipitation steps. MenC polysaccharide is purified by a combination of chromatography and precipitation steps.
The protein carrier (CRM197) is produced by bacterial fermentation and is purified by a series of chromatography and ultrafiltration steps. C. diphtheriae is cultured and grown on CY medium containing yeast extracts and amino acids.
The oligosaccharides are prepared for conjugation from purified polysaccharides by hydrolysis, sizing, and reductive amination. After activation, each oligosaccharide is covalently linked to the CRM197 protein. The resulting glycoconjugates are purified to yield the 4 drug substances, which compose the final vaccine. The vaccine contains no preservative or adjuvant. Each dose of vaccine contains 10 mcg MenA oligosaccharide; 5 mcg of each of MenC, MenY, and MenW-135 oligosaccharides; and 25.4 to 65.5 mcg CRM197 protein. Residual formaldehyde per dose is estimated to be not more than 0.30 mcg.
The vials in which the vaccine components are contained are composed of Type I glass, USP.
The container closures (synthetic rubber stoppers) are not made with natural rubber latex.
12. Menveo - Clinical Pharmacology
12.1 Mechanism of Action
Neisseria meningitidis is a gram-negative diplococcus that causes life-threatening invasive disease such as meningitis and sepsis. Globally, 5 serogroups, A, B, C, Y, and W-135 cause almost all invasive meningococcal infections. The presence of serum bactericidal antibodies protects against invasive meningococcal disease.1 Vaccination with MENVEO leads to the production of bactericidal antibodies directed against the capsular polysaccharides of serogroups A, C, Y, and W-135.
14. Clinical Studies
For all age groups, effectiveness has been inferred from the measurement of serogroup-specific anticapsular antibodies with bactericidal activity using pooled human serum that lacked bactericidal activity as the source of exogenous complement (hSBA).
14.1 Primary Vaccination Studies
In the absence of a licensed comparator vaccine for use in infants, the pre-specified endpoint for effectiveness of MENVEO in U.S. infants receiving a 4-dose series at 2, 4, 6, and 12 months of age was the proportion of subjects achieving an hSBA ≥1:8, with the lower limit of the 2-sided 95% CI for the point estimate being ≥80% of vaccinees for serogroup A, and ≥85% of vaccinees for serogroups C, W-135, and Y 1 month following the final dose.
The effectiveness of MENVEO in subjects aged 2 through 55 years was assessed by comparing the hSBA responses to immunization with MENVEO to those following immunization with the licensed meningococcal quadrivalent conjugate vaccine MENACTRA.
The primary effectiveness endpoint was hSBA seroresponse to each serogroup 28 days after vaccination. Seroresponse was defined as: a) post-vaccination hSBA ≥1:8 for subjects with a baseline hSBA <1:4; or, b) at least 4-fold higher than baseline titers for subjects with a pre-vaccination hSBA ≥1:4. Secondary endpoints included the proportion of subjects with post-vaccination hSBA ≥1:8 and the hSBA Geometric Mean Titer (GMT) for each serogroup. In a separate group of children aged 2 through 5 years randomized to receive 2 doses of MENVEO administered 2 months apart, seroresponse rate, proportion with post-vaccination hSBA ≥1:8, and GMT were determined for each serogroup.
Immunogenicity in Infants/Toddlers Aged 2 Months through 12 Months
The effectiveness of MENVEO in infants was assessed in a randomized, controlled, multicenter study (NCT01000311). Among the subjects receiving MENVEO who were included in the per-protocol analysis, the mean age at enrollment was 65 days, 51% were male, 67% were Caucasian, 6% were African American, 15% were Hispanic, 2% were Asian, and 9% were noted as other racial/ethnic groups. The pre-defined criteria for immunogenicity were met for all 4 serogroups A, C, W-135, and Y at 1 month following completion of a 4-dose series at 2, 4, 6, and 12 months of age (Table 7).
The percentage of subjects with hSBA ≥1:8 at 7 months was 94% to 98% for serogroups C, W-135, and Y and 76% for serogroup A.
| Serogroup | Post 3rd Dose | Post 4th Dose | |
|---|---|---|---|
| Clinicaltrials.gov Identifier NCT01000311. % ≥1:8 = Proportions of subjects with hSBA ≥1:8 against a given serogroup; CI = Confidence interval; GMT = Geometric mean antibody titer; n = Number of infants eligible for inclusion in the Per-Protocol Immunogenicity population for whom serological results were available for the post-Dose 3 and post-Dose 4 evaluations. Serum Bactericidal Assay with exogenous human complement source (hSBA). a Pre-specified criteria for adequacy of immune response were met (lower limit of the 95% CI >80% for serogroup A and >85% for serogroups C, W, and Y). |
|||
|
A |
n = 202 |
n = 168 |
|
|
% ≥1:8 95% CI |
76 |
89 |
|
|
GMT 95% CI |
21 (17, 26) |
54 (44, 67) |
|
|
C |
n = 199 |
n = 156 |
|
|
% ≥1:8 95% CI |
94 |
95 |
|
|
GMT 95% CI |
74 (62, 87) |
135 (107, 171) |
|
|
W-135 |
n = 194 |
n = 153 |
|
|
% ≥1:8 95% CI |
98 |
97 |
|
|
GMT 95% CI |
79 (67, 92) |
215 (167, 227) |
|
|
Y |
n = 188 |
n = 153 |
|
|
% ≥1:8 95% CI |
94 |
96 |
|
|
GMT 95% CI |
51 (43, 61) |
185 (148, 233) |
|
The effectiveness of 2 doses of MENVEO given at 7-9 months and 12 months of age was assessed in a randomized, multicenter, controlled clinical trial (NCT00626327) conducted in the U.S. This study also investigated the concomitant administration of MENVEO and MMRV. The per-protocol population for assessing the response to 2 doses of MENVEO consisted of 386 subjects. Among subjects who completed the per-protocol analysis, their mean age at enrollment was 8.5 months (SD: 0.8 months), 50% were male; 61% were Caucasian, 15% were Hispanic, 10% were African American, 4% were Asian, and 10% were noted as other racial/ethnic groups.
Among the per-protocol population, after MENVEO administered at 7-9 and at 12 months, the proportions of subjects with hSBA ≥1:8 for serogroups A, C, W-135, and Y were respectively: 88% (84-91), 100% (98-100), 98% (96-100), 96% (93-99).
Immunogenicity in Children Aged 2 Years through 10 Years
Effectiveness in subjects aged 2 through 10 years was evaluated in a randomized, multicenter, active-controlled clinical study (NCT00616421) comparing hSBA responses following 1 dose of MENVEO or MENACTRA. The study was conducted in the U.S. and Canada and was stratified by age (2 through 5 years and 6 through 10 years). The per-protocol population evaluated after a single dose of vaccine consisted of 1,170 subjects who received MENVEO and 1,161 who received MENACTRA (Table 8) and included serological results for 89% to 95% of subjects, depending on serogroup and age group. Demographics for the 616 and 619 subjects aged 2 through 5 years for MENVEO and MENACTRA were as follows: mean age 3.6 years (SD: 1.1) vs. 3.6 years (SD: 1.1), 51% vs. 52% male, 62% vs. 62% Caucasian, 14% vs. 13% Hispanic, 12% vs. 13% African American, 6% vs. 4% Asian, and 7% vs. 8% other racial/ethnic groups, respectively. Demographics were for 554 and 542 per-protocol subjects aged 6 through 10 years for MENVEO and MENACTRA were as follows: mean age 7.9 years (SD: 1.4) vs. 8.1 years (SD: 1.4), 52% vs. 56% male, 66% vs. 66% Caucasian, 14% vs. 14% African American, 7% vs. 7% Hispanic, 5% vs. 6% Asian, and 8% vs. 8% other racial/ethnic groups, respectively. In a separate group of children aged 2 through 5 years randomized to receive 2 doses of MENVEO administered 2 months apart, the per-protocol population evaluated after 2 doses of MENVEO consisted of 297 subjects and included serologic results for 96% to 99% of subjects, depending on serogroup.
In study participants aged 2 through 5 years and 6 through 10 years, non-inferiority of MENVEO to MENACTRA for the proportion of subjects with a seroresponse was demonstrated for serogroups C, W-135, and Y, but not for serogroup A (Table 8).
| Endpoint by Serogroup | 2-5 Years | 6-10 Years | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| MENVEO
(95% CI) | MENACTRA
(95% CI) | Percent Difference (MENVEO – MENACTRA) or GMT Ratio (MENVEO/
MENACTRA) (95% CI) | MENVEO
(95% CI) | MENACTRA
(95% CI) | Percent Difference (MENVEO – MENACTRA) or GMT Ratio (MENVEO/
MENACTRA) (95% CI) |
|||||
| Clinicaltrials.gov Identifier NCT00616421. a Serum Bactericidal Assay with exogenous human complement source (hSBA). CI = Confidence interval; GMT = Geometric mean antibody titer. b Seroresponse was defined as: Subjects with a pre-vaccination hSBA <1:4, a post-vaccination titer of >1:8 and among subjects with a pre-vaccination hSBA ≥1:4, a post-vaccination titer at least 4-fold higher than baseline. c Non-inferiority criterion not met (the lower limit of the 2-sided 95% CI ≤-10% for vaccine group differences). d Non-inferiority criterion met (the lower limit of the 2-sided 95% CI >-10% for vaccine group differences [MENVEO minus MENACTRA]). |
||||||||||
|
A |
n = 606 |
n = 611 |
n = 551 |
n = 541 | ||||||
|
% Seroresponseb |
72 |
77 |
-5 |
77 |
83 |
-6 |
||||
|
% ≥1:8 |
72 |
78 |
-6 |
77 |
83 |
-6 |
||||
|
GMT |
26 |
25 |
1.04 |
35 |
35 |
1.01 |
||||
|
C |
n = 607 |
n = 615 |
n = 554 |
n = 539 | ||||||
|
% Seroresponseb |
60 |
56 |
4 |
63 |
57 |
6 |
||||
|
% ≥1:8 |
68 |
64 |
4 |
77 |
74 |
3 |
||||
|
GMT |
18 |
13 |
1.33 |
36 |
27 |
1.36 |
||||
|
W-135 |
n = 594 |
n = 605 |
n = 542 |
n = 533 | ||||||
|
% Seroresponseb |
72 (68, 75) |
58 (54, 62) |
14 (9, 19)d |
57 |
44 |
13 |
||||
|
% ≥1:8 |
90 (87, 92) |
75 (71, 78) |
15 (11, 19) |
91 (88, 93) |
84 (81, 87) |
7 (3, 11) |
||||
|
GMT |
43 (38, 50) |
21 (19, 25) |
2.02 (1.71, 2.39) |
61 (52, 72) |
35 (30, 42) |
1.72 (1.44, 2.06) |
||||
|
Y |
n = 593 |
n = 600 |
n = 545 |
n = 539 | ||||||
|
% Seroresponseb |
66 |
45 |
21 |
58 |
39 |
19 |
||||
|
% ≥1:8 |
76 |
57 |
19 |
79 |
63 |
16 |
||||
|
GMT |
24 |
10 |
2.36 |
34 |
14 |
2.41 |
||||
In the 297 per-protocol subjects aged 2 through 5 years observed at 1 month after the second dose of MENVEO, the proportions of subjects with seroresponse (95% CI) were: 91% (87-94), 98% (95-99), 89% (85-92), and 95% (91-97) for serogroups A, C, W-135, and Y, respectively. The proportion of subjects with hSBA ≥1:8 (95% CI) were 91% (88-94), 99% (97-100), 99% (98-100), and 98% (95-99) for serogroups A, C, W-135, and Y, respectively. The hSBA GMTs (95% CI) for this group were 64 (51-81), 144 (118-177), 132 (111-157), and 102 (82-126) for serogroups A, C, W-135, and Y, respectively.
Immunogenicity in Adolescents Aged 11 Years through 18 Years
Effectiveness in subjects aged 11 through 55 years was evaluated in a randomized, multicenter, active-controlled clinical study (NCT00450437) comparing the hSBA responses following 1 dose of MENVEO or MENACTRA. The study was conducted in the U.S. and stratified by age (11 through 18 years and 19 through 55 years). This study enrolled 3,539 participants, who were randomized to receive a dose of MENVEO (n = 2,663) or MENACTRA (n = 876). Among subjects who completed the per-protocol evaluation for immunogenicity (n = 3,393, MENVEO = 2,549, MENACTRA = 844), demographics for subjects receiving MENVEO and MENACTRA, respectively, were as follows: mean age 23.9 (SD: 13.6) vs. 23.7 (SD: 13.7), 42% vs. 42% male, 79% vs. 78% Caucasian, 8% vs. 9% African American, 7% vs. 7% Hispanic, 3% vs. 3% Asian, 2% vs. 3% other racial/ethnic groups. Immunogenicity for each serogroup was assessed in a subset of study participants (Tables 9 and 10).
In study participants aged 11 through 18 years, non-inferiority of MENVEO to MENACTRA was demonstrated for all 4 serogroups for the proportion of subjects with a seroresponse (Table 9).
| Endpoint by Serogroup | Bactericidal Antibody Responsea | Comparison of MENVEO and MENACTRA | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MENVEO
(95% CI) | MENACTRA
(95% CI) | MENVEO/
MENACTRA (95% CI) | MENVEO minus MENACTRA
(95% CI) |
||||||||||||
| Clinicaltrials.gov Identifier NCT00450437. CI = Confidence interval; GMT = Geometric mean antibody titer. a Serum Bactericidal Assay with exogenous human complement source (hSBA). b Seroresponse was defined as: a) post-vaccination hSBA ≥1:8 for subjects with a pre-vaccination hSBA <1:4; or, b) at least 4-fold higher than baseline titers for subjects with a pre-vaccination hSBA ≥1:4. c Non-inferiority criterion for the primary endpoint met (the lower limit of the 2-sided 95% CI >-10% for vaccine group differences [MENVEO minus MENACTRA]). |
|||||||||||||||
|
A |
n = 1,075 |
n = 359 | |||||||||||||
|
% Seroresponseb |
75 (72, 77) |
66 (61, 71) |
8 (3, 14)c |
||||||||||||
|
% >1:8 |
75 |
67 |
- |
8 (3, 14) |
|||||||||||
|
GMT |
29 (24, 35) |
18 (14, 23) |
1.63 (1.31, 2.02) |
- |
|||||||||||
|
C |
n = 1,396 |
n = 460 | |||||||||||||
|
% Seroresponseb |
76 (73, 78) |
73 (69, 77) |
2 (-2, 7)c |
||||||||||||
|
% >1:8 |
85 |
85 |
- |
0 (-4, 4) |
|||||||||||
|
GMT |
50 |
41 |
1.22 (0.97, 1.55) |
- |
|||||||||||
|
W-135 |
n = 1,024 |
n = 288 | |||||||||||||
|
% Seroresponseb |
75 (72, 77) |
63 (57, 68) |
12 (6, 18)c |
||||||||||||
|
% >1:8 |
96 |
88 |
- |
8 (4, 12) |
|||||||||||
|
GMT |
87 |
44 |
2.00 (1.66, 2.42) |
- |
|||||||||||
|
Y |
n = 1,036 |
n = 294 | |||||||||||||
|
% Seroresponseb |
68 (65, 71) |
41 (35, 47) |
27 (20, 33)c |
||||||||||||
|
% >1:8 |
88 |
69 |
- |
19 (14, 25) |
|||||||||||
|
GMT |
51 |
18 |
2.82 (2.26, 3.52) |
- |
|||||||||||
Immunogenicity in Adults Aged 19 Years through 55 Years
The study in subjects aged 11 through 55 years was a randomized, multicenter, active-controlled clinical trial (NCT00450437) conducted in the U.S. and stratified by age (11 through 18 years and 19 through 55 years) as described above.
In study participants aged 19 through 55 years, non-inferiority of MENVEO to MENACTRA was demonstrated for all 4 serogroups for the proportion of subjects with a seroresponse (Table 10).
| Endpoint by Serogroup | Bactericidal Antibody Responsea | Comparison of MENVEO and MENACTRA | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MENVEO
(95% CI) | MENACTRA
(95% CI) | MENVEO/
MENACTRA (95% CI) | MENVEO minus MENACTRA
(95% CI) |
|||||||||||||||||
| Clinicaltrials.gov Identifier NCT00450437. CI = Confidence interval; GMT = Geometric mean antibody titer. a Serum Bactericidal Assay with exogenous human complement source (hSBA). b Seroresponse was defined as: a) post-vaccination hSBA >1:8 for subjects with a pre-vaccination hSBA <1:4; or, b) at least 4-fold higher than baseline titers for subjects with a pre-vaccination hSBA ≥1:4. c Non-inferiority criterion for the primary endpoint met (the lower limit of the 2-sided 95% CI >-10% for vaccine group differences [MENVEO minus MENACTRA]). |
||||||||||||||||||||
|
A |
n = 963 |
n = 321 | ||||||||||||||||||
|
% Seroresponseb |
67 (64, 70) |
68 (63, 73) |
-1 (-7, 5)c |
|||||||||||||||||
|
% >1:8 |
69 |
71 |
- |
-2 (-7, 4) |
||||||||||||||||
|
GMT |
31 |
30 |
1.06 (0.82, 1.37) |
- |
||||||||||||||||
|
C |
n = 902 |
n = 300 | ||||||||||||||||||
|
% Seroresponseb |
68 (64, 71) |
60 (54, 65) |
8 (2, 14)c |
|||||||||||||||||
|
% >1:8 |
80 |
74 |
- |
6 (1, 12) |
||||||||||||||||
|
GMT |
50 |
34 |
1.50 (1.14, 1.97) |
- |
||||||||||||||||
|
W-135 |
n = 484 |
n = 292 | ||||||||||||||||||
|
% Seroresponseb |
50 (46, 55) |
41 (35, 47) |
9 (2, 17)c |
|||||||||||||||||
|
% >1:8 |
94 |
90 |
- |
4 (0, 9) |
||||||||||||||||
|
GMT |
111 |
69 |
1.61 (1.24, 2.1) |
- |
||||||||||||||||
|
Y |
n = 503 |
n = 306 | ||||||||||||||||||
|
% Seroresponseb |
56 (51, 60) |
40 (34, 46) |
16 (9, 23)c |
|||||||||||||||||
|
% >1:8 |
79 |
70 |
- |
9 (3, 15) |
||||||||||||||||
|
GMT |
44 |
21 |
2.10 (1.60, 2.75) |
- |
||||||||||||||||
Immunogenicity of MENVEO One-Vial Presentation in Individuals Aged 10 Years through 40 Years
Immunogenicity of MENVEO one-vial presentation was evaluated in an observer-blind randomized, multicenter, controlled clinical trial in individuals aged 10 to 40 years (NCT03433482). The study compared the immune response of the MENVEO one-vial presentation to the MENVEO two-vial presentation.
The primary analysis demonstrated non-inferiority of MenA serogroup hSBA GMTs at 28 days post-vaccination for the MENVEO one-vial presentation group compared to the MENVEO two-vial presentation group (lower limit of the two-sided 95% CI for the ratio of hSBA GMTs against serogroup A between the MENVEO one-vial presentation group and the MENVEO two-vial presentation group was greater than 0.5). Secondary analyses showed comparable immune responses against N. meningitidis serogroups C, W-135 and Y as measured by hSBA GMTs. Additional secondary analyses demonstrated comparable percentages of subjects with hSBA titers ≥8, and percentages of subjects with a ≥4-fold rise in titers compared to baseline for serogroups A, C, W-135 and Y.
14.2 Booster Vaccination Study
Immunogenicity in Adolescents and Adults Aged 15 Years through 55 Years
For a description of study design and number of participants, see section 6.1 Booster Vaccination Study. The co-primary immunogenicity endpoints were hSBA seroresponse to each serogroup 29 days a) following a booster vaccination with MENVEO given to subjects who received a prior dose of MENVEO, and b) following a booster vaccination with MENVEO given to subjects who received a prior dose of MENACTRA. Seroresponse was defined as: a) post-vaccination hSBA ≥1:16 for subjects with a baseline hSBA <1:4 or b) at least 4-fold higher than baseline titers for subjects with a pre-vaccination hSBA ≥1:4. Secondary endpoints included the proportions of subjects with post-vaccination hSBA ≥1:8, the hSBA GMTs for each serogroup, and antibody titers against each serogroup 4 to 6 years after a prior dose (as measured by percentages of subjects with hSBA titers ≥1:8 and hSBA GMTs prior to booster vaccination).
Seroresponse rates at Day 29 following a booster vaccination with MENVEO were 97% for serogroup A, 95% for serogroup C, 96% for serogroup W-135, and 97% for serogroup Y, in subjects who had received a prior dose of MENVEO (n = 290). At Day 6, following a booster vaccination, seroresponse rates were 39%, 51%, 50%, and 49% for serogroups A, C, W-135, and Y, respectively, in subjects who had received a prior dose of MENVEO.
The hSBA GMTs were 13, 92, 112, and 63 for serogroups A, C, W-135, and Y at Day 6, and 210, 1160, 1395, and 1067, respectively, for the 4 serogroups at Day 29 following a booster dose of MENVEO.
Overall, similar seroresponse rates and GMTs were observed for those subjects who received a booster vaccination with MENVEO following a prior dose of MENACTRA (n = 282).
Prior to booster vaccination, the percentage of subjects with hSBA titers >1:8 for serogroups A, C, W-135, and Y were 12%, 62%, 76%, and 54% for those who received a prior dose of MENVEO 4 to 6 years earlier, and 15%, 54%, 77%, and 47% for those who received a prior dose of MENACTRA 4 to 6 years earlier. The hSBA GMTs for serogroups A, C, W-135, and Y prior to booster vaccination were 3, 16, 23, and 9 following a prior vaccination with MENVEO and 3, 11, 23, and 8 following a prior vaccination with MENACTRA.
14.3 Immunogenicity of Concomitantly Administered Vaccines
In U.S. infants (NCT00474526, NCT01000311) who received MENVEO concomitantly with DTaP-IPV-Hib and PCV7 at 2, 4, and 6 months of age and HBV administered according to ACIP recommendations, there was no evidence for reduced antibody response to pertussis antigens (GMC to pertussis toxin, filamentous hemagglutinin, fimbriae, and pertactin), diphtheria toxoid (antibody levels ≥0.1 IU/mL), tetanus toxoid (antibody levels ≥0.1 IU/mL), poliovirus types 1, 2, and 3 (neutralizing antibody levels ≥1:8 to each virus), Haemophilus influenzae type b (anti-PRP antibody ≥0.15 mcg/mL), hepatitis B (anti-hepatitis B surface antigen ≥10 mIU/mL), or most serotypes of PCV7 (antibody levels ≥0.35 mcg/mL) relative to the response in infants administered DTaP-IPV-Hib, PCV7, and HBV. The immune responses to DTaP-IPV-Hib, PCV7, and HBV were evaluated 1 month following Dose 3. No interference was observed for pertussis based on GMC ratios, or for the other concomitantly administered vaccines, with the exception of pneumococcal serotype 6B and 23F, for which interference was suggested post Dose 3. No interference was observed post Dose 4 for these serotypes.
There was no evidence for interference in the immune response to MMR and varicella vaccines (among initially seronegative children) in terms of percentages of children with anti-measles antibodies ≥255 mIU/mL, anti-mumps ≥10 ELISA antibody units, anti-rubella ≥10 IU/mL, and anti-varicella ≥5 gp ELISA units/mL, administered at 12 months of age (NCT00626327) concomitantly with MENVEO relative to these vaccines administered alone. The immune responses to MMR and varicella vaccines were evaluated 6 weeks post vaccination.
For children aged 2 through 10 years, no data are available for evaluating safety and immunogenicity of other childhood vaccines when administered concomitantly with MENVEO.
For individuals aged 11 through 18 years, the effect of concomitant administration of MENVEO with Tdap and HPV was evaluated in a study (NCT00518180) conducted in Costa Rica (see also section 6.1 for the safety results from this trial). Subjects were randomized to receive one of the following regimens at the start of the trial: MENVEO plus Tdap plus HPV (n = 540); MENVEO alone (n = 541); Tdap alone (n = 539). Subjects were healthy adolescents aged 11 through 18 years (mean age between groups was 13.8 to 13.9 years). For antigens of MENVEO, the proportion (95% CI) of subjects achieving an hSBA seroresponse among those who received MENVEO plus Tdap plus HPV vs. MENVEO alone, respectively, were: serogroup A 80% (76, 84) vs. 82% (78, 85); serogroup C 83% (80, 87) vs. 84% (80, 87); serogroup W-135 77% (73, 80) vs. 81% (77, 84); serogroup Y 83% (79, 86) vs. 82% (79, 86). Among subjects who received Tdap plus MENVEO plus HPV, compared with Tdap alone, the proportions (95% CI) of subjects who achieved an anti-tetanus or anti-diphtheria toxoids levels ≥1.0 IU/mL in the 2 groups, respectively, were 100% (99, 100) vs. 98% (96, 99) and 100% (99, 100) vs. 100% (99, 100). For pertussis antigens, among subjects who received Tdap plus MENVEO plus HPV, compared with Tdap alone, the responses respectively for anti-pertussis toxin GMCs (95% CI) were 51 (47, 55) vs. 63 (58, 69) ELISA Units (EU)/mL, for anti-filamentous hemagglutinin were 342 (310, 376) vs. 511 (464, 563) EU/mL, and for anti-pertactin were 819 (727, 923) vs. 1,197 (1,061, 1,350) EU/mL. Because there are no established serological correlates of protection for pertussis, the clinical implications of the lower pertussis antigen responses are unknown.
15. References
1. Goldschneider I, Gotschlich EC, Artenstein MS. Human immunity to the meningococcus. I. The role of humoral antibodies. J Exp Med. (1969);129:1307-1326.
16. How is Menveo supplied
16.1 MENVEO Two-Vial Presentation
MENVEO two-vial presentation is supplied in cartons containing:
- •
- 5 Vials containing MenCYW-135 Liquid Conjugate Component (Vial 1; gray cap)
- •
- 5 Vials containing MenA Lyophilized Conjugate Component (Vial 2; orange cap)
One vial of MenCYW-135 liquid conjugate component (Vial 1) and one vial of MenA lyophilized conjugate component (Vial 2) must be combined before use to form a single dose (0.5 mL) of MENVEO (packaged without syringes or needles). Each carton contains 5 doses of MENVEO.
The container closures (synthetic rubber stoppers) are not made with natural rubber latex.
| Presentation | Carton NDC Number | ||
|---|---|---|---|
| MenCYW-135 Liquid Conjugate Component
(Vial 1; gray cap) NDC Number | MenA Lyophilized Conjugate Component
(Vial 2; orange cap) NDC Number |
||
|
Carton of 10 vials (5 doses) |
NDC 58160-955-09 |
5 Vials NDC 58160-959-01 |
5 Vials NDC 58160-958-01 |
Storage before Reconstitution
Do not freeze. Frozen/previously frozen product should be discarded.
Store refrigerated, away from the freezer compartment, at 36°F to 46°F (2°C to 8°C).
Protect from light. Vaccine must be maintained at 36°F to 46°F (2°C to 8°C) during transport.
Do not use after the expiration date.
Storage after Reconstitution
The reconstituted vaccine should be used immediately but may be held at 36°F to 77°F (2°C to 25°C) for up to 8 hours. Do not freeze. Discard reconstituted vaccine if it has been frozen or not used within 8 hours.
16.2 MENVEO One-Vial Presentation
MENVEO one-vial presentation is supplied in cartons containing:
- •
- 10 Vials containing MENVEO (pink cap)
Each carton contains 10 single dose vials of MENVEO. Each dose is 0.5 mL.
The container closures (synthetic rubber stoppers) are not made with natural rubber latex.
Table 12. MENVEO: One-Vial Presentation
| Presentation | Carton NDC Number | MENVEO
(pink cap) NDC Number |
|---|---|---|
|
Carton of 10 vials (10 doses) |
NDC 58160-827-30 |
10 Vials NDC 58160-827-03 |
Do not freeze. Frozen/previously frozen product should be discarded.
Store refrigerated, away from the freezer compartment, at 36°F to 46°F (2°C to 8°C).
Protect from light. Vaccine must be maintained at 36°F to 46°F (2°C to 8°C) during transport.
Do not use after the expiration date.
17. Patient Counseling Information
Give the recipient, parent, or guardian the Vaccine Information Statements, which are required by the National Childhood Vaccine Injury Act of 1986 to be given prior to immunization. These materials are available free of charge at the Centers for Disease Control and Prevention (CDC) website (www.cdc.gov/vaccines).
Provide the following information to the vaccine recipient, parent, or guardian:
- •
- Potential benefits and risks of immunization with MENVEO.
- •
- The importance of completing the immunization series.
- •
- Potential for adverse reactions that have been temporally associated with administration of MENVEO or other vaccines containing similar components.
- •
- Reporting any adverse reactions to their healthcare provider.
MENVEO is a trademark owned by or licensed to the GSK group of companies.
The other brands listed are trademarks owned by or licensed to their respective owners and are not owned by or licensed to the GSK group of companies. The makers of these brands are not affiliated with and do not endorse the GSK group of companies or its products.
Manufactured by:
GSK Vaccines, Srl
Bellaria-Rosia 53018, Sovicille (SI), Italy
US License No. 1617
Distributed by:
GlaxoSmithKline
Durham, NC 27701
©2022 GSK group of companies or its licensor.
MNV:7PI
PRINCIPAL DISPLAY PANEL
NDC 58160-955-09
MENVEO
MENINGOCOCCAL (GROUPS A, C, Y AND W-135)
OLIGOSACCHARIDEDIPHTHERIA CRM197 CONJUGATE VACCINE
Men-ACYW
Rx Only
One vial of MenCYW-135 Liquid Conjugate Component (Vial 1) and one vial of MenA Lyophilized Conjugate Component (Vial 2) MUST BE COMBINED BEFORE USE
For Use from 2 Months through 55 Years of Age
Contents (5 doses of MENVEO):
5 Vials containing MenCYW-135 Liquid Conjugate Component (Vial 1)
5 Vials containing MenA Lyophilized Conjugate Component (Vial 2)
After reconstitution, a single dose of MENVEO is 0.5 mL
Made in Italy
©2019 GSK group of companies or its licensor.
Rev. 8/19
498608
PRINCIPAL DISPLAY PANEL
NDC 58160-827-30
MENVEO
Meningococcal (Groups A, C, Y AND W-135)
Oligosaccharide Diphtheria CRM197 Conjugate Vaccine
Men-ACYW
1-Vial Presentation
1Dose
Rx Only
1-Vial Presentation
DO NOT RECONSTITUTE.
10 Years through 55 Years of Age
Contents (10 doses of MENVEO):
10 Vials containing MenACYW-135 Liquid Vaccine
A single dose of MENVEO is 0.5 mL
GSK
MENVEO
Made in Italy
©2022 GSK group of companies or its licensor.
Rev. 10/22
511975
| MENVEO
meningococcal (groups a, c, y and w-135) oligosaccharide diphtheria crm197 conjugate vaccine kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| MENVEO
meningococcal (groups a, c, y and w-135) oligosaccharide diphtheria crm197 conjugate vaccine injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - GlaxoSmithKline Biologicals SA (372748392) |