Drug Detail:Nucynta er (Tapentadol [ ta-pen-ta-dol ])
Drug Class: Opioids (narcotic analgesics)
Highlights of Prescribing Information
NUCYNTA® ER (tapentadol) extended-release tablets for oral use C-II
Initial U.S. Approval: 2008
WARNING: ADDICTION, ABUSE, AND MISUSE; RISK EVALUATION AND MITIGATION STRATEGY (REMS); LIFE- THREATENING RESPIRATORY DEPRESSION; ACCIDENTAL INGESTION; NEONATAL OPIOID WITHDRAWAL SYNDROME; INTERACTION WITH ALCOHOL and RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
See full prescribing information for complete boxed warning.
- NUCYNTA ER exposes users to risks of addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient's risk before prescribing, and monitor regularly for development of these behaviors or conditions. (5.1)
- To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the Food and Drug Administration (FDA) has required a Risk Evaluation and Mitigation Strategy (REMS) for these products. (5.2)
- Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely, especially upon initiation or following a dose increase. Instruct patients to swallow NUCYNTA ER tablets whole to avoid exposure to a potentially fatal dose of tapentadol. (5. 3)
- Accidental ingestion of NUCYNTA ER, especially in children, can result in fatal overdose of tapentadol. (5.3)
- Prolonged use of NUCYNTA ER during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available. (5.4)
- Instruct patients not to consume alcohol or any products containing alcohol while taking NUCYNTA ER because co-ingestion can result in fatal plasma tapentadol levels. (5.5)
- Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing for use in patients for whom alternative treatment options are inadequate; limit dosages and durations to the minimum required; and follow patients for signs and symptoms of respiratory depression and sedation. (5.5), (7)
Recent Major Changes
| Dosage and Administration (2.2) | 03/2021 |
| Warnings and Precautions (5.1, 5.3 5.5) | 03/2021 |
Indications and Usage for Nucynta ER
NUCYNTA ER is an opioid agonist indicated for the management of:
- pain severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate. (1)
- neuropathic pain associated with diabetic peripheral neuropathy (DPN) in adults severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate. (1)
Limitations of Use
- Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses, and because of the greater risks of overdose and death with extended-release opioid formulations, reserve NUCYNTA ER for use in patients for whom alternative treatment options (e.g., non- opioid analgesics or immediate-release opioids) are ineffective, not tolerated, or would be otherwise inadequate to provide sufficient management of pain.
- NUCYNTA ER is not indicated as an as-needed (prn) analgesic. (1)
Nucynta ER Dosage and Administration
- To be prescribed only by healthcare providers knowledgeable in use of potent opioids for management of chronic pain. (2.1)
- Use the lowest effective dosage for the shortest duration consistent with individual patient treatment goals (2.1).
- Individualize dosing based on the severity of pain, patient response, prior analgesic experience, and risk factors for addiction, abuse, and misuse. (2.1)
- Instruct patients to swallow NUCYNTA ER tablets intact, and not to cut, break, chew, crush, or dissolve the tablets (risk of potentially fatal overdose). (2.1, 5.1)
- Instruct patients to take tablets one at a time, with enough water to ensure complete swallowing immediately after placing in mouth. (2.1)
- Do not exceed a total daily dose of NUCYNTA ER of 500 mg. (2.1)
- Discuss availability of naloxone with the patient and caregiver and assess each patient's need for access to naloxone, both when initiating and renewing treatment with NUCYNTA ER. Consider prescribing naloxone based on the patient's risk factors for overdose. (2.2, 5.1, 5.3, 5.5)
- For opioid-naïve and opioid non-tolerant patients, initiate treatment with 50 mg tablet orally twice daily (approximately every 12 hours). See full prescribing information for instructions on conversion, titration, and maintenance of therapy. (2.3, 2.4)
- Titrate patients with dose increases of 50 mg no more than twice daily every three days. (2.4)
- Moderate Hepatic Impairment: Initiate treatment with 50 mg NUCYNTA ER no more than every 24 hours. Do not exceed 100 mg per day. Monitor closely for respiratory and central nervous system depression (2.5)
- Do not abruptly discontinue NUCYNTA ER in a physically-dependent patient because rapid discontinuation of opioid analgesics has resulted in serious withdrawal symptoms, uncontrolled pain, and suicide.(2.6)
Dosage Forms and Strengths
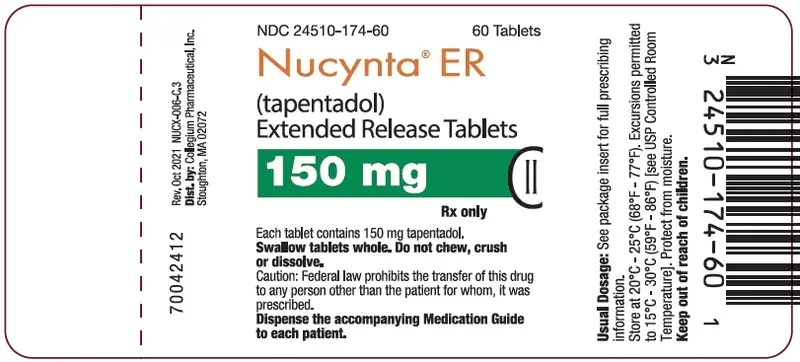
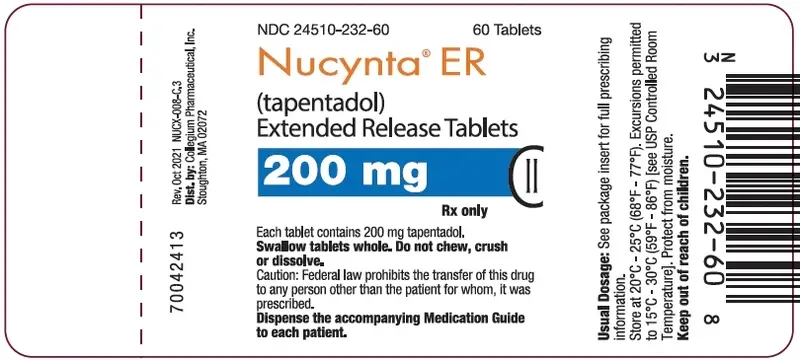
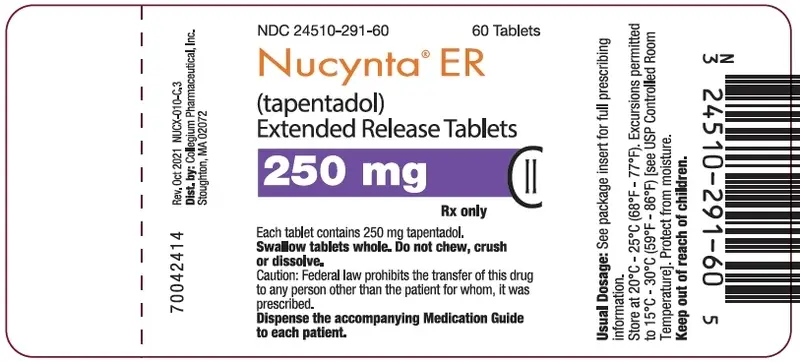
Extended-release tablets: 50 mg, 100 mg, 150 mg, 200 mg, 250 mg (3)
Contraindications
- Significant respiratory depression (4)
- Acute or severe bronchial asthma (4)
- Known or suspected paralytic ileus (4)
- Hypersensitivity to tapentadol or to any other ingredients of the product (4)
- Concurrent use of monoamine oxidase inhibitors (MAOIs) or use of MAOIs within the last 14 days. (4)
Warnings and Precautions
- Risk of Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients: Monitor closely, particularly during initiation and titration. (5.1)
- Serotonin Syndrome: Potentially life-threatening condition could result from concomitant serotonergic drug administration. Discontinue NUCYNTA ER if serotonin syndrome is suspected. (5.7)
- Adrenal Insufficiency: If diagnosed, treat with physiologic replacement of corticosteroids, and wean patient off of the opioid. (5.8)
- Severe Hypotension: Monitor during dosage initiation and titration. Avoid use of NUCYNTA ER in patients with circulatory shock. (5.9)
- Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness: Monitor for sedation and respiratory depression. Avoid use of NUCYNTA ER in patients with impaired consciousness or coma. (5.10)
Adverse Reactions/Side Effects
The most common (≥10%) adverse reactions were nausea, constipation, dizziness, headache, and somnolence. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Collegium Pharmaceutical, Inc. at 1-855-331-5615 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Mixed Agonist/Antagonist and Partial Agonist Opioid Analgesics: Avoid use with NUCYNTA ER because they may reduce analgesic effect of NUCYNTA ER or precipitate withdrawal symptoms. (5.13, 7)
Use In Specific Populations
- Pregnancy: Based on animal data, may cause fetal harm. (8.1)
- Nursing mothers: Nursing is not recommended. (8.2)
- Severe Hepatic or Renal Impairment: Use not recommended. (8.6, 8.7)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 3/2021
Full Prescribing Information
WARNING: ADDICTION, ABUSE, AND MISUSE; RISK EVALUATION AND MITIGATION STRATEGY (REMS); LIFE-THREATENING RESPIRATORY DEPRESSION; ACCIDENTAL INGESTION; NEONATAL OPIOID WITHDRAWAL SYNDROME; INTERACTION WITH ALCOHOL and RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
1. Indications and Usage for Nucynta ER
NUCYNTA ER (tapentadol) is indicated for the management of:
- pain severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate.
- neuropathic pain associated with diabetic peripheral neuropathy (DPN) severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate.
2. Nucynta ER Dosage and Administration
2.1 Important Dosage and Administration Instructions
NUCYNTA ER should be prescribed only by healthcare professionals who are knowledgeable in the use of potent opioids for the management of chronic pain.
- Use the lowest effective dosage for the shortest duration consistent with individual patient treatment goals [see Warnings and Precautions (5)].
- Initiate the dosing regimen for each patient individually, taking into account the patient's severity of pain, patient response, prior analgesic treatment experience, and risk factors for addiction, abuse, and misuse [see Warnings and Precautions (5.1)]
- Monitor patients closely for respiratory depression, especially within the first 24-72 hours of initiating therapy and following dosage increases with NUCYNTA ER and adjust the dosage accordingly [see Warnings and Precautions (5.3)].
Instruct patients to swallow NUCYNTA ER tablets whole, one tablet at a time, with enough water to ensure complete swallowing immediately after placing in the mouth [see Patient Counseling Information (17)]. Crushing, chewing, or dissolving NUCYNTA ER tablets will result in uncontrolled delivery of tapentadol and can lead to overdose or death [see Warnings and Precautions (5.1)].
Discontinue all other tapentadol and tramadol products when beginning and while taking NUCYNTA ER [see Warnings and Precautions (5.7)]. Although the maximum approved total daily dose of NUCYNTA immediate-release formulation is 600 mg per day, the maximum total daily dose of NUCYNTA ER is 500 mg. Do not exceed a total daily dose of NUCYNTA ER of 500 mg.
2.2 Patient Access to Naloxone for the Emergency Treatment of Opioid Overdose
Discuss the availability of naloxone for the emergency treatment of opioid overdose with the patient and caregiver and assess the potential need for access to naloxone, both when initiating and renewing treatment with NUCYNTA ER [see Warnings and Precautions (5.3), Patient Counseling Information (17)].
Inform patients and caregivers about the various ways to obtain naloxone as permitted by individual state naloxone dispensing and prescribing requirements or guidelines (e.g., by prescription, directly from a pharmacist, or as part of a community-based program).
Consider prescribing naloxone, based on the patient's risk factors for overdose, such as concomitant use of CNS depressants, a history of opioid use disorder, or prior opioid overdose. The presence of risk factors for overdose should not prevent the proper management of pain in any given patient [see Warnings and Precautions (5.1, 5.3, 5.5)].
Consider prescribing naloxone if the patient has household members (including children) or other close contacts at risk for accidental ingestion or overdose.
2.4 Titration and Maintenance of Therapy
Individually titrate NUCYNTA ER to a dose that provides adequate analgesia and minimizes adverse reactions. Continually reevaluate patients receiving NUCYNTA ER to assess the maintenance of pain control and the relative incidence of adverse reactions, as well as monitoring for the development of addiction, abuse, or misuse [see Warnings and Precautions (5.1)]. Frequent communication is important among the prescriber, other members of the healthcare team, the patient, and the caregiver/family during periods of changing analgesic requirements, including initial titration. During chronic therapy, periodically reassess the continued need for opioid analgesics.
Patients who experience breakthrough pain may require a dosage adjustment of NUCYNTA ER, or may need rescue medication with an appropriate dose of an immediate-release analgesic. If the level of pain increases after dose stabilization, attempt to identify the source of increased pain before increasing the NUCYNTA ER dosage. Titrate patients to adequate analgesia with dose increases of 50 mg no more than twice daily every three days. In clinical studies, efficacy with NUCYNTA ER was demonstrated relative to placebo in the dosage range of 100 mg to 250 mg twice daily [see Clinical Studies (14)].
If unacceptable opioid-related adverse reactions are observed, consider reducing the dosage. Adjust the dosage to obtain an appropriate balance between management of pain and opioid-related adverse reactions.
2.5 Dosage Modification in Patients with Hepatic Impairment
The use of NUCYNTA ER in patients with severe hepatic impairment (Child-Pugh Score 10-15) is not recommended [see Warnings and Precautions (5.15)].
In patients with moderate hepatic impairment (Child-Pugh Score 7 to 9), initiate treatment using 50 mg NUCYNTA ER, administer no more frequently than once every 24 hours, and monitor closely for respiratory and central nervous system depression, particularly during initiation and titration of NUCYNTA ER. The maximum recommended dose for patients with moderate hepatic impairment is 100 mg of NUCYNTA ER per day. Monitor closely for respiratory and central nervous system depression [see Clinical Pharmacology (12.2)].
No dosage adjustment is recommended in patients with mild hepatic impairment (Child-Pugh Score 5 to 6) [see Warnings and Precautions (5.15), Use in Specific Populations (8.6), Clinical Pharmacology (12.3)].
2.6 Safe Reduction or Discontinuation of NUCYNTA ER
Do not abruptly discontinue NUCYNTA ER in patients who may be physically dependent on opioids. Rapid discontinuation of opioid analgesics in patients who are physically dependent on opioids has resulted in serious withdrawal symptoms, uncontrolled pain, and suicide. Rapid discontinuation has also been associated with attempts to find other sources of opioid analgesics, which may be confused with drug-seeking for abuse. Patients may also attempt to treat their pain or withdrawal symptoms with illicit opioids, such as heroin, and other substances.
When a decision has been made to decrease the dose or discontinue therapy in an opioid-dependent patient taking NUCYNTA ER, there are a variety of factors that should be considered, including the dose of NUCYNTA ER the patient has been taking, the duration of treatment, the type of pain being treated, and the physical and psychological attributes of the patient. It is important to ensure ongoing care of the patient and to agree on an appropriate tapering schedule and follow-up plan so that patient and provider goals and expectations are clear and realistic. When opioid analgesics are being discontinued due to a suspected substance use disorder, evaluate and treat the patient, or refer for evaluation and treatment of the substance use disorder. Treatment should include evidence-based approaches, such as medication assisted treatment of opioid use disorder. Complex patients with comorbid pain and substance use disorders may benefit from referral to a specialist.
There are no standard opioid tapering schedules that are suitable for all patients. Good clinical practice dictates a patient-specific plan to taper the dose of the opioid gradually. For patients on NUCYNTA ER who are physically opioid-dependent, initiate the taper by a small enough increment (e.g., no greater than 10% to 25% of the total daily dose) to avoid withdrawal symptoms, and proceed with dose-lowering at an interval of every 2 to 4 weeks. Patients who have been taking opioids for briefer periods of time may tolerate a more rapid taper.
It may be necessary to provide the patient with lower dosage strengths to accomplish a successful taper. Reassess the patient frequently to manage pain and withdrawal symptoms, should they emerge. Common withdrawal symptoms include restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other signs and symptoms also may develop, including irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate. If withdrawal symptoms arise, it may be necessary to pause the taper for a period of time or raise the dose of the opioid analgesic to the previous dose, and then proceed with a slower taper. In addition, monitor patients for any changes in mood, emergence of suicidal thoughts, or use of other substances.
When managing patients taking opioid analgesics, particularly those who have been treated for a long duration and/or with high doses for chronic pain, ensure that a multimodal approach to pain management, including mental health support (if needed), is in place prior to initiating an opioid analgesic taper. A multimodal approach to pain management may optimize the treatment of chronic pain, as well as assist with the successful tapering of the opioid analgesic [see Warnings and Precautions (5.13), Drug Abuse and Dependence (9.3)].
3. Dosage Forms and Strengths
NUCYNTA ER 50 mg, 100 mg, 150 mg, 200 mg and 250 mg extended-release tablets are available in the following colors and prints:
- 50 mg extended-release tablets are white oblong-shaped with a black print "OMJ 50" on one side
- 100 mg extended-release tablets are light-blue oblong-shaped with a black print "OMJ 100" on one side
- 150 mg extended-release tablets are blue-green oblong-shaped with a black print "OMJ 150" on one side
- 200 mg extended-release tablets are blue oblong-shaped with a depression in the middle running lengthwise on each side and a black print "OMJ 200" on one side
- 250 mg extended-release tablets are dark blue oblong-shaped with a depression in the middle running lengthwise on each side and a white print "OMJ 250" on one side.
4. Contraindications
NUCYNTA ER is contraindicated in patients with:
- Significant respiratory depression
- Acute or severe bronchial asthma or hypercarbia in an unmonitored setting or in the absence of resuscitative equipment
- Known or suspected gastrointestinal obstruction, including paralytic ileus
- Hypersensitivity (e.g. anaphylaxis, angioedema) to tapentadol or to any other ingredients of the product [see Adverse Reactions (6.2)].
- Concurrent use of monoamine oxidase inhibitors (MAOIs) or use of MAOIs within the last 14 days [see Drug Interactions (7)].
5. Warnings and Precautions
5.1 Addiction, Abuse, and Misuse
NUCYNTA ER contains tapentadol, a Schedule II controlled substance. As an opioid, NUCYNTA ER exposes users to the risks of addiction, abuse, and misuse. Because extended-release products such as NUCYNTA ER deliver the opioid over an extended period of time, there is a greater risk for overdose and death due to the larger amount of tapentadol present [see Drug Abuse and Dependence (9)].
Although the risk of addiction in any individual is unknown, it can occur in patients appropriately prescribed NUCYNTA ER. Addiction can occur at recommended doses and if the drug is misused or abused.
Assess each patient's risk for opioid addiction, abuse, or misuse prior to prescribing NUCYNTA ER, and monitor all patients receiving NUCYNTA ER for the development of these behaviors and conditions. Risks are increased in patients with a personal or family history of substance abuse (including drug or alcohol abuse or addiction) or mental illness (e.g., major depression). The potential for these risks should not, however, prevent the prescribing of NUCYNTA ER for the proper management of pain in any given patient. Patients at increased risk may be prescribed opioids such as NUCYNTA ER, but use in such patients necessitates intensive counseling about the risks and proper use of NUCYNTA ER along with intensive monitoring for signs of addiction, abuse, and misuse. Consider prescribing naloxone for the emergency treatment of opioid overdose [see Dosage and Administration (2.2), Warnings and Precautions (5.3)].
Abuse or misuse of NUCYNTA ER by crushing, chewing, snorting, or injecting the dissolved product will result in the uncontrolled delivery of tapentadol and can result in overdose and death [see Overdosage (10)].
Opioid are sought by drug abusers and people with addiction disorders and are subject to criminal diversion. Consider these risks when prescribing or dispensing NUCYNTA ER. Strategies to reduce these risks include prescribing the drug in the smallest appropriate quantity and advising the patient on the proper disposal of unused drug [see Patient Counseling Information (17)]. Contact the local state professional licensing board or state controlled substances authority for information on how to prevent and detect abuse or diversion of this product.
5.2 Opioid Analgesic Risk Evaluation and Mitigation Strategy (REMS)
To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the Food and Drug Administration (FDA) has required a Risk Evaluation and Mitigation Strategy (REMS) for these products. Under the requirements of the REMS, drug companies with approved opioid analgesic products must make REMS-compliant education programs available to healthcare providers. Healthcare providers are strongly encouraged to do all of the following:
- Complete a REMS-compliant education program offered by an accredited provider of continuing education (CE) or another education program that includes all the elements of the FDA Education Blueprint for Health Care Providers Involved in the Management or Support of Patients with Pain.
- Discuss the safe use, serious risks, and proper storage and disposal of opioid analgesics with patients and/or their caregivers every time these medicines are prescribed. The Patient Counseling Guide (PCG) can be obtained at this link: www.fda.gov/OpioidAnalgesicREMSPCG.
- Emphasize to patients and their caregivers the importance of reading the Medication Guide that they will receive from their pharmacist every time an opioid analgesic is dispensed to them.
- Consider using other tools to improve patient, household, and community safety, such as patient-prescriber agreements that reinforce patient-prescriber responsibilities.
To obtain further information on the opioid analgesic REMS and for a list of accredited REMS CME/CE, call 1-800-503-0784, or log on to www.opioidanalgesicrems.com. The FDA Blueprint can be found at www.fda.gov/OpioidAnalgesicREMSBlueprint.
5.3 Life-Threatening Respiratory Depression
Serious, life-threatening, or fatal respiratory depression has been reported with the use of opioids, even when used as recommended. Respiratory depression, if not immediately recognized and treated, may lead to respiratory arrest and death. Management of respiratory depression may include close observation, supportive measures, and use of opioid antagonists, depending on the patient's clinical status [see Overdosage (10)]. Carbon dioxide (CO2) retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids.
While serious, life-threatening, or fatal respiratory depression can occur at any time during the use of NUCYNTA ER, the risk is greatest during the initiation of therapy or following a dosage increase. Monitor patients closely for respiratory depression especially within the first 24-72 hours of initiating therapy with and following dosage increases of NUCYNTA ER.
To reduce the risk of respiratory depression, proper dosing and titration of NUCYNTA ER are essential [see Dosage and Administration (2)]. Overestimating the NUCYNTA ER dosage when converting patients from another opioid product can result in fatal overdose with the first dose.
Accidental ingestion of even one dose of NUCYNTA ER, especially by children, can result in respiratory depression and death due to an overdose of tapentadol.
Educate patients and caregivers on how to recognize respiratory depression and emphasize the importance of calling 911 or getting emergency medical help right away in the event of a known or suspected overdose [see Patient Counseling Information (17)].
Opioids can cause sleep-related breathing disorders including central sleep apnea (CSA) and sleep-related hypoxemia. Opioid use increases the risk of CSA in a dose-dependent fashion. In patients who present with CSA, consider decreasing the opioid dosage using best practices for opioid taper [see Dosage and Administration (2.6)].
5.4 Neonatal Opioid Withdrawal Syndrome
Prolonged use of NUCYNTA ER during pregnancy can result in withdrawal in the neonate. Neonatal opioid withdrawal syndrome, unlike opioid withdrawal syndrome in adults, may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. Observe newborns for signs of neonatal opioid withdrawal syndrome and manage accordingly. Advise pregnant women using opioids for a prolonged period of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available [see Use in Specific Populations (8.1), Patient Counseling Information (17)].
5.5 Risk from Concomitant Use with Benzodiazepines or Other CNS Depressants
Patients must not consume alcoholic beverages or prescription or non-prescription products containing alcohol while on NUCYNTA ER therapy. The co-ingestion of alcohol with NUCYNTA ER may result in increased plasma tapentadol levels and a potentially fatal overdose of tapentadol [see Clinical Pharmacology (12.3)].
Profound sedation, respiratory depression, coma, and death may result from the concomitant use of NUCYNTA ER with benzodiazepines or other CNS depressants (e.g., non-benzodiazepine sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opioids, alcohol). Because of these risks, reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioid analgesics alone. Because of similar pharmacological properties, it is reasonable to expect similar risk with the concomitant use of other CNS depressant drugs with opioid analgesics [see Drug Interactions (7)].
If the decision is made to prescribe a benzodiazepine or other CNS depressant concomitantly with an opioid analgesic, prescribe the lowest effective dosages and minimum durations of concomitant use. In patients already receiving an opioid analgesic, prescribe a lower initial dose of the benzodiazepine or other CNS depressant than indicated in the absence of an opioid, and titrate based on clinical response. If an opioid analgesic is initiated in a patient already taking a benzodiazepine or other CNS depressant, prescribe a lower initial dose of the opioid analgesic, and titrate based on clinical response. Follow patients closely for signs and symptoms of respiratory depression and sedation.
If concomitant use is warranted, consider prescribing naloxone for the emergency treatment of opioid overdose [see Dosage and Administration (2.2), Warnings and Precautions (5.3)].
Advise both patients and caregivers about the risks of respiratory depression and sedation when NUCYNTA ER is used with benzodiazepines or other CNS depressants (including alcohol and illicit drugs). Advise patients not to drive or operate heavy machinery until the effects of concomitant use of the benzodiazepine or other CNS depressant have been determined. Screen patients for risk of substance use disorders, including opioid abuse and misuse, and warn them of the risk for overdose and death associated with the use of additional CNS depressants including alcohol and illicit drugs [see Drug Interactions (7) and Patient Counseling Information (17)].
5.6 Risk of Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients
The use of NUCYNTA ER in patients with acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment is contraindicated.
5.7 Serotonin Syndrome with Concomitant Use of Serotonergic Drugs
Cases of serotonin syndrome, a potentially life-threatening condition, have been reported during concomitant use of tapentadol with serotonergic drugs. Serotonergic drugs include selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), triptans, 5-HT3 receptor antagonists, drugs that affect the serotonergic neurotransmitter system (e.g., mirtazapine, trazodone, tramadol), certain muscle relaxants (i.e., cyclobenzaprine, metaxalone), and drugs that impair metabolism of serotonin (including MAO inhibitors, both those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue) [see Drug Interactions (7)]. This may occur within the recommended dosage range.
Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile blood pressure, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination, rigidity), and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). The onset of symptoms generally occurs within several hours to a few days of concomitant use, but may occur later than that. Discontinue NUCYNTA ER if serotonin syndrome is suspected.
5.8 Adrenal Insufficiency
Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use. Presentation of adrenal insufficiency may include non-specific symptoms and signs including nausea, vomiting, anorexia, fatigue, weakness, dizziness, and low blood pressure. If adrenal insufficiency is suspected, confirm the diagnosis with diagnostic testing as soon as possible. If adrenal insufficiency is diagnosed, treat with physiologic replacement doses of corticosteroids. Wean the patient off of the opioid to allow adrenal function to recover and continue corticosteroid treatment until adrenal function recovers. Other opioids may be tried as some cases reported use of a different opioid without recurrence of adrenal insufficiency. The information available does not identify any particular opioids as being more likely to be associated with adrenal insufficiency.
5.9 Severe Hypotension
NUCYNTA ER may cause severe hypotension including orthostatic hypotension and syncope in ambulatory patients. There is an increased risk in patients whose ability to maintain blood pressure has already been compromised by a reduced blood volume or concurrent administration of certain CNS depressant drugs (e.g., phenothiazines or general anesthetics) [see Drug Interactions (7)]. Monitor these patients for signs of hypotension after initiating or titrating the dosage of NUCYNTA ER. In patients with circulatory shock, NUCYNTA ER may cause vasodilation that can further reduce cardiac output and blood pressure. Avoid the use of NUCYNTA ER in patients with circulatory shock.
5.10 Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness
In patients who may be susceptible to the intracranial effects of CO2 retention (e.g., those with evidence of increased intracranial pressure or brain tumors), NUCYNTA ER may reduce respiratory drive, and the resultant CO2 retention can further increase intracranial pressure. Monitor such patients for signs of sedation and respiratory depression, particularly when initiating therapy with NUCYNTA ER.
Opioids may also obscure the clinical course in a patient with a head injury. Avoid the use of NUCYNTA ER in patients with impaired consciousness or coma.
5.11 Risks of Use in Patients with Gastrointestinal Conditions
NUCYNTA ER is contraindicated in patients with known or suspected gastrointestinal obstruction, including paralytic ileus.
The tapentadol in NUCYNTA ER may cause spasm of the sphincter of Oddi. Opioids may cause increases in serum amylase. Monitor patients with biliary tract disease, including acute pancreatitis, for worsening symptoms.
5.12 Increased Risk of Seizures in Patients with Seizure Disorders
The tapentadol in NUCYNTA ER may increase the frequency of seizures in patients with seizure disorders, and may increase the risk of seizures occurring in other clinical settings associated with seizures. Monitor patients with a history of seizure disorders for worsened seizure control during NUCYNTA ER therapy.
5.13 Withdrawal
Do not abruptly discontinue NUCYNTA ER in a patient physically dependent on opioids. When discontinuing NUCYNTA ER in a physically dependent patient, gradually taper the dosage. Rapid tapering of tapentadol in a patient physically dependent on opioids may lead to a withdrawal syndrome and return of pain [see Dosage and Administration (2.6), Drug Abuse and Dependence (9.3)].
Additionally, avoid the use of mixed agonist/antagonist (e.g., pentazocine, nalbuphine, and butorphanol) or partial agonist (e.g., buprenorphine) analgesics in patients who have received or are receiving a course of therapy with a full opioid agonist analgesic, including NUCYNTA ER. In these patients, mixed agonists/antagonists and partial agonist analgesics may reduce the analgesic effect and/or may precipitate withdrawal symptoms [see Drug Interactions (7)].
5.14 Risks of Driving and Operating Machinery
NUCYNTA ER may impair the mental or physical abilities needed to perform potentially hazardous activities such as driving a car or operating machinery. Warn patients not to drive or operate dangerous machinery unless they are tolerant to the effects of NUCYNTA ER and know how they will react to the medication [see Patient Counseling Information (17)].
5.15 Risk of Toxicity in Patients with Hepatic Impairment
A study with an immediate-release formulation of tapentadol in subjects with hepatic impairment showed higher serum concentrations of tapentadol than in those with normal hepatic function. Avoid use of NUCYNTA ER in patients with severe hepatic impairment. Reduce the dose of NUCYNTA ER in patients with moderate hepatic impairment [see Dosage and Administration (2.5) and Clinical Pharmacology (12.3)]. Closely monitor patients with moderate hepatic impairment for respiratory and central nervous system depression when initiating and titrating NUCYNTA ER.
5.16 Risk of Toxicity in Patients with Renal Impairment
Use of NUCYNTA ER in patients with severe renal impairment is not recommended due to accumulation of a metabolite formed by glucuronidation of tapentadol. The clinical relevance of the elevated metabolite is not known [see Clinical Pharmacology (12.3)].
6. Adverse Reactions/Side Effects
The following serious adverse reactions are described, or described in greater detail, in other sections:
- Addiction, Abuse, and Misuse [see Warnings and Precautions (5.1)]
- Life-Threatening Respiratory Depression [see Warnings and Precautions (5.3)]
- Neonatal Opioid Withdrawal Syndrome [see Warnings and Precautions (5.4)]
- Interaction with Benzodiazepine or Other CNS Depressants [see Warnings and Precautions (5.5)]
- Serotonin Syndrome [see Warnings and Precautions 5.7]
- Adrenal Insufficiency [see Warnings and Precautions (5.8)]
- Severe Hypotension [see Warnings and Precautions (5.9)]
- Gastrointestinal Adverse Reactions [see Warnings and Precautions (5.11)]
- Seizures [see Warnings and Precautions (5.12)]
- Withdrawal [see Warnings and Precautions (5.13)]
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of tapentadol. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Psychiatric disorders: hallucination, suicidal ideation, panic attack
Serotonin syndrome: Cases of serotonin syndrome, a potentially life-threatening condition, have been reported during concomitant use of opioids with serotonergic drugs.
Adrenal insufficiency: Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use.
Anaphylaxis: Anaphylaxis has been reported with ingredients contained in NUCYNTA ER.
Androgen deficiency: Cases of androgen deficiency have occurred with chronic use of opioids [see Clinical Pharmacology (12.2)].
7. Drug Interactions
Table 3 includes clinically significant drug interactions with NUCYNTA ER.
| Alcohol | |
| Clinical Impact: | Concomitant use of alcohol with NUCYNTA ER can result in an increase of tapentadol plasma levels and potentially fatal overdose of tapentadol. |
| Intervention: | Instruct patients not to consume alcoholic beverages or use prescription or non-prescription products containing alcohol while on NUCYNTA ER therapy. |
| Benzodiazepines and Other Central Nervous System (CNS) Depressants | |
| Clinical Impact: | Due to additive pharmacologic effect, the concomitant use of benzodiazepines or other CNS depressants, including alcohol, can increase the risk of hypotension, respiratory depression, profound sedation, coma, and death. |
| Intervention: | Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients closely for signs of respiratory depression and sedation If concomitant use is warranted, consider prescribing naloxone for the emergency treatment of opioid overdose [see Dosage and Administration (2.2), Warnings and Precautions (5.1, 5.3, 5.5)]. |
| Examples: | Benzodiazepines and other sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opioids, alcohol |
| Serotonergic Drugs | |
| Clinical Impact: | The concomitant use of opioids with other drugs that affect the serotonergic neurotransmitter system has resulted in serotonin syndrome [see Warnings and Precautions 5.7]. |
| Intervention: | If concomitant use is warranted, carefully observe the patient, particularly during treatment initiation and dose adjustment. Discontinue NUCYNTA ER if serotonin syndrome is suspected. |
| Examples: | Selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), triptans, 5-HT3 receptor antagonists, drugs that affect the serotonin neurotransmitter system (e.g., mirtazapine, trazodone, tramadol), certain muscle relaxants (i.e., cyclobenzaprine, metaxalone), monoamine oxidase (MAO) inhibitors (those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue) |
| Monoamine Oxidase Inhibitors (MAOIs) | |
| Clinical Impact: | MAOI interactions with opioids may manifest as serotonin syndrome or opioid toxicity (e.g., respiratory depression, coma) [see Warnings and Precautions (5.3)]. |
| Intervention: | Do not use NUCYNTA ER in patients taking MAOIs or within 14 days of stopping such treatment |
| Examples: | phenelzine, tranylcypromine, linezolid |
| Mixed Agonist/Antagonist and Partial Agonist Opioid Analgesics | |
| Clinical Impact: | May reduce the analgesic effect of NUCYNTA ER and/or precipitate withdrawal symptoms. |
| Intervention: | Avoid concomitant use. |
| Examples: | butorphanol, nalbuphine, pentazocine, buprenorphine |
| Muscle Relaxants | |
| Clinical Impact: | Tapentadol may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression. |
| Intervention: | Monitor patients for signs of respiratory depression that may be greater than otherwise expected and decrease the dosage of NUCYNTA ER and/or the muscle relaxant as necessary. Due to the risk of respiratory depression with concomitant use of skeletal muscle relaxants and opioids, consider prescribing naloxone for the emergency treatment of opioid overdose [see Dosage and Administration (2.2), Warnings and Precautions (5.3, 5.5)] |
| Examples: | cyclobenzaprine, metaxalone |
| Diuretics | |
| Clinical Impact: | Opioids can reduce the efficacy of diuretics by inducing the release of antidiuretic hormone. |
| Intervention: | Monitor patients for signs of diminished diuresis and/or effects on blood pressure and increase the dosage of the diuretic as needed. |
| Anticholinergic Drugs | |
| Clinical Impact: | The concomitant use of anticholinergic drugs may increase risk of urinary retention and/or severe constipation, which may lead to paralytic ileus. |
| Intervention: | Monitor patients for signs of urinary retention or reduced gastric motility when NUCYNTA ER is used concomitantly with anticholinergic drugs. |
8. Use In Specific Populations
8.4 Pediatric Use
The safety and efficacy of NUCYNTA ER in pediatric patients less than 18 years of age have not been established.
8.5 Geriatric Use
Of the total number of patients in Phase 2/3 double-blind, multiple-dose clinical studies of NUCYNTA ER, 28% (1023/3613) were 65 years and over, while 7% (245/3613) were 75 years and over. No overall differences in effectiveness or tolerability were observed between these patients and younger patients.
Elderly patients (aged 65 or older) may have increased sensitivity to tapentadol. In general, use caution when selecting a dosage for an elderly patient, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy [see Clinical Pharmacology (12.3)].
Respiratory depression is the chief risk for elderly patients treated with opioids, and has occurred after large initial doses were administered to patients who were not opioid-tolerant or when opioids were co-administered with other agents that depress respiration. Titrate the dosage of NUCYNTA ER slowly in geriatric patients and monitor closely for signs of central nervous system and respiratory depression [see Warnings and Precautions (5.6)].
Tapentadol is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
8.6 Hepatic Impairment
Use of NUCYNTA ER in patients with severe hepatic impairment (Child-Pugh Score 10-15) is not recommended. In patients with moderate hepatic impairment (Child-Pugh Score 7 to 9), dosage reduction of NUCYNTA ER is recommended [see Dosage and Administration (2.5)]. No dosage adjustment is recommended in patients with mild hepatic impairment (Child-Pugh Score 5 to 6) [see Warnings and Precautions (5.15), Clinical Pharmacology (12.3)].
8.7 Renal Impairment
Use of NUCYNTA ER in patients with severe renal impairment (creatinine clearance less than 30 mL/minute) is not recommended. No dosage adjustment is recommended in patients with mild or moderate renal impairment (creatinine clearance 30-90 mL/minute) [see Warnings and Precautions (5.15), Clinical Pharmacology (12.3)].
9. Drug Abuse and Dependence
9.2 Abuse
NUCYNTA ER contains tapentadol, a substance with a high potential for abuse similar to other opioids including fentanyl, hydrocodone, hydromorphone, methadone, morphine, oxycodone, and oxymorphone. NUCYNTA ER can be abused and is subject to misuse, addiction, and criminal diversion [see Warnings and Precautions (5.3)].
The high drug content in extended-release formulations adds to the risk of adverse outcomes from abuse and misuse.
All patients treated with opioids require careful monitoring for signs of abuse and addiction, because use of opioid analgesic products carries the risk of addiction even under appropriate medical use.
Prescription drug abuse is the intentional non-therapeutic use of a prescription drug, even once, for its rewarding psychological or physiological effects.
Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that develop after repeated substance use and includes: a strong desire to take the drug, difficulties in controlling its use, persisting in its use despite harmful consequences, a higher priority given to drug use than to other activities and obligations, increased tolerance, and sometimes a physical withdrawal.
"Drug-seeking" behavior is very common in persons with substance use disorders. Drug-seeking tactics include emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing, or referral, repeated "loss" of prescriptions, tampering with prescriptions, and reluctance to provide prior medical records or contact information for other treating healthcare provider(s). "Doctor shopping" (visiting multiple prescribers to obtain additional prescriptions) is common among drug abusers, and people suffering from untreated addiction. Preoccupation with achieving adequate pain relief can be appropriate behavior in a patient with poor pain control.
Abuse and addiction are separate and distinct from physical dependence and tolerance. Healthcare providers should be aware that addiction may not be accompanied by concurrent tolerance and symptoms of physical dependence in all addicts. In addition, abuse of opioids can occur in the absence of true addiction.
NUCYNTA ER, like other opioids, can be diverted for non-medical use into illicit channels of distribution. Careful record-keeping of prescribing information, including quantity, frequency, and renewal requests, as required by state and federal law, is strongly advised.
Proper assessment of the patient, proper prescribing practices, periodic re-evaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs.
9.3 Dependence
Both tolerance and physical dependence can develop during chronic opioid therapy. Tolerance is the need for increasing doses of opioids to maintain a defined effect such as analgesia (in the absence of disease progression or other external factors). Tolerance may occur to both the desired and undesired effects of drugs, and may develop at different rates for different effects.
Physical dependence is a physiological state in which the body adapts to the drug after a period of regular exposure, resulting in withdrawal symptoms after abrupt discontinuation or a significant dosage reduction of a drug. Withdrawal also may be precipitated through the administration of drugs with opioid antagonist activity, (e.g., naloxone, nalmefene), mixed agonist/antagonist analgesics (e.g., pentazocine, butorphanol, nalbuphine), or partial agonists (e.g., buprenorphine). Physical dependence may not occur to a clinically significant degree until after several days to weeks of continued opioid usage.
Do not abruptly discontinue NUCYNTA ER in a patient physically dependent on opioids. Rapid tapering of NUCYNTA ER in a patient physically dependent on opioids may lead to serious withdrawal symptoms, uncontrolled pain, and suicide. Rapid discontinuation has also been associated with attempts to find other sources of opioid analgesics, which may be confused with drug-seeking for abuse.
When discontinuing NUCYNTA ER, gradually taper the dosage using a patient specific plan that considers the following: the dose of NUCYNTA ER the patient has been taking, the duration of treatment, and the physical and psychological attributes of the patient. To improve the likelihood of a successful taper and minimize withdrawal symptoms, it is important that the opioid tapering schedule is agreed upon by the patient. In patients taking opioids for a long duration at high doses, ensure that a multimodal approach to pain management, including mental health support (if needed), is in place prior to initiating an opioid analgesic taper [see Dosage and Administration (2.6), Warnings and Precautions (5.13)].
Infants born to mothers physically dependent on opioids will also be physically dependent and may exhibit respiratory difficulties and withdrawal symptoms [see Use in Specific Populations (8.1)].
11. Nucynta ER Description
NUCYNTA ER (tapentadol) is an opioid agonist, supplied in extended-release film-coated tablets for oral administration, containing 58.24, 116.48, 174.72, 232.96, and 291.20 mg of tapentadol hydrochloride in each tablet strength, corresponding to 50, 100, 150, 200, and 250 mg of tapentadol free-base, respectively. The chemical name is 3-[(1R,2R)-3-(dimethylamino)-1-ethyl-2-methylpropyl]phenol monohydrochloride. The structural formula is:
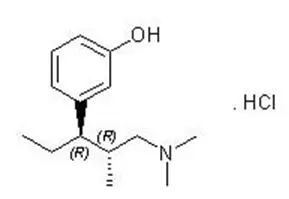
The molecular weight of tapentadol HCl is 257.80, and the molecular formula is C14H23NO∙HCl. The n- octanol: water partition coefficient log P value is 2.89. The pKa values are 9.36 and 10.45. In addition to the active ingredient tapentadol HCl, tablets also contain the following inactive ingredients: alpha-tocopherol (vitamin E), hypromellose, polyethylene glycol, and polyethylene oxide. The film coating is comprised of polyvinyl alcohol, polyethylene glycol, talc, titanium dioxide, and the colorant FD&C Blue #2 aluminum lake is used for 100, 150, 200, and 250 mg strengths; and additionally, yellow iron oxide is used in 150 mg tablets. Printing inks contain shellac glaze and propylene glycol for all strengths, and black iron oxide (50, 100, 150 and 200 mg tablets) or titanium dioxide (250 mg tablets).
12. Nucynta ER - Clinical Pharmacology
12.1 Mechanism of Action
Tapentadol is a centrally-acting synthetic analgesic. The exact mechanism of action is unknown. Although the clinical relevance is unclear, preclinical studies have shown that tapentadol is a mu-opioid receptor (MOR) agonist and a norepinephrine reuptake inhibitor (NRI). Analgesia in animal models is derived from both of these properties.
12.3 Pharmacokinetics
13. Nonclinical Toxicology
13.2 Animal Toxicology and/or Pharmacology
In toxicological studies with tapentadol, the most common systemic effects of tapentadol were related to the mu-opioid receptor agonist and norepinephrine reuptake inhibition pharmacodynamic properties of the compound. Transient, dose-dependent and predominantly CNS-related findings were observed, including impaired respiratory function and convulsions, the latter occurring in the dog at plasma levels (Cmax), which are in the range associated with the maximum recommended human dose (MRHD).
14. Clinical Studies
14.1 Clinical Trials Summary
The efficacy of NUCYNTA ER was studied in five studies in patients with chronic pain and DPN. Efficacy was demonstrated in one randomized, double-blind, placebo- and active-controlled study in patients with chronic low back pain (LBP), and two randomized, double-blind, placebo-controlled studies in patients with pain related to diabetic peripheral neuropathy (DPN-1 and DPN-2).
14.2 Moderate to Severe Chronic Low Back Pain
In the LBP study, patients 18 years of age or older with chronic low back pain and a baseline pain score of ≥5 on an 11-point numerical rating scale (NRS), ranging from 0 to 10 were enrolled and randomized to 1 of 3 treatments: NUCYNTA ER, active-control (an extended-release Schedule II opioid analgesic), or placebo.
Patients randomized to NUCYNTA ER initiated therapy with a dose of 50 mg twice daily for three days. After three days, the dose was increased to 100 mg twice daily. Subsequent titration was allowed over a 3- week titration period to a dose up to 250 mg twice daily, followed by a 12-week maintenance period. There were 981 patients randomized. The mean age of the study population was 50 (range 18 to 89) years; the mean baseline pain intensity score was 8 (SD 1). Approximately half of the patients were opioid-naïve (had not taken opioids during the three months prior to the screening visit).
The number of patients completing the study was 51% in the placebo group, 54% in the NUCYNTA ER group and 43% in the active-control group. Lack of efficacy was the most common reason for discontinuation among placebo-treated patients (21%), whereas adverse events were the most common reason for discontinuation among the active treatment groups (17% and 32% for NUCYNTA ER and active-control, respectively).
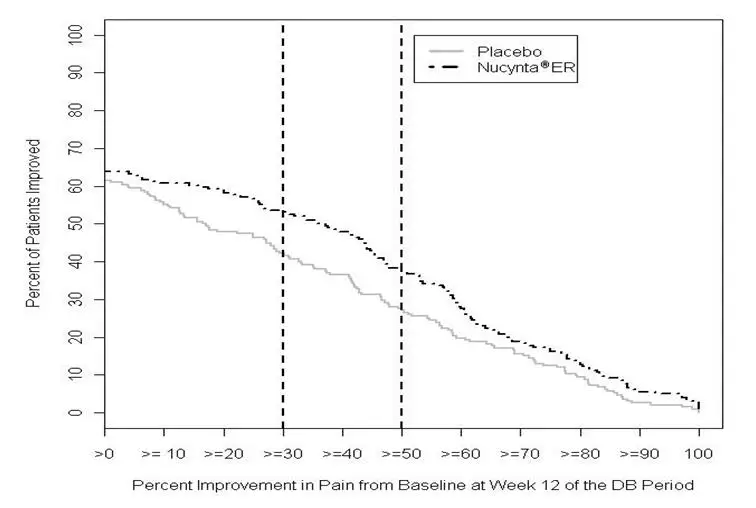
After 15 weeks of treatment, patients taking NUCYNTA ER had a significantly greater pain reduction compared to placebo. The proportion of patients with various degrees of improvement is shown in Figure 1. The figure is cumulative, such that patients, whose change from baseline is, for example 50%, are also included at every level of improvement below 50%. Patients who did not complete the study were assigned 0% improvement.
Figure 1: Percentage of Patients Achieving Various Levels of Improvement in Pain Intensity - Study LBP1
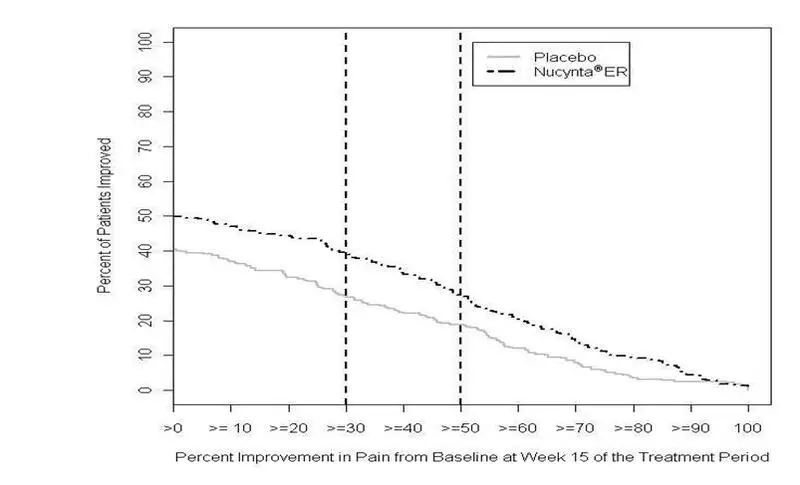
- 1
- The last week of Study LBP was Week 15.
14.3 Neuropathic Pain Associated with Diabetic Peripheral Neuropathy
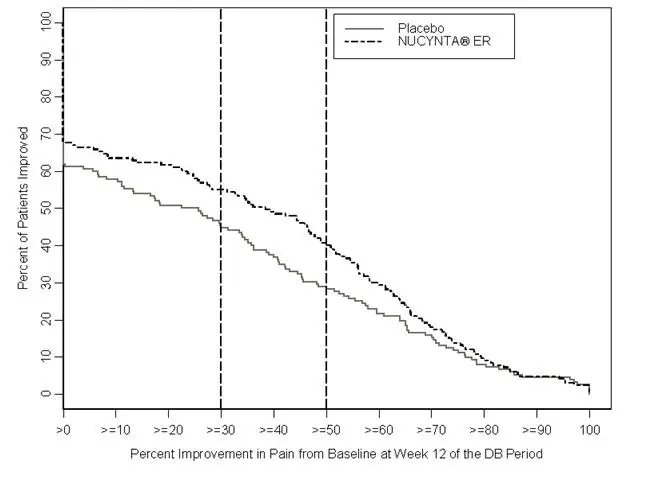
In the two DPN studies, patients 18 years of age or older with pain due to diabetic peripheral neuropathy and a pain score of ≥5 on an 11-point numerical rating scale (NRS) ranging from 0 (no pain) to 10 (worst possible pain) were enrolled. Following an open-label treatment period in which NUCYNTA ER was administered to all patients for three weeks and titrated to an individually stable dose, patients who had tolerated the drug and demonstrated at least a 1-point improvement in pain intensity on the NRS at the end of the open-label titration period were randomized to either continue the NUCYNTA ER dose (100 mg to 250 mg twice a day) reached during the open-label titration period, or receive placebo for 12 weeks of maintenance treatment. During the first 4 days of the double-blind maintenance period patients were permitted to take tapentadol ER 25 mg up to two times a day as additional medication. After the first 4 days, patients were allowed to take tapentadol ER 25 mg once daily as needed for pain, in addition to the patient's assigned study drug. Patients recorded their pain in a diary twice daily.
16. How is Nucynta ER supplied
NUCYNTA ER tablets are available in the following strengths and packages:
50 mg extended-release tablets are white oblong-shaped with a black print "OMJ 50" on one side and are available in bottles of 60 with child-resistant closure (NDC 24510-058-60) and unit dose blister packs of 100 (10 blister strips of 10 tablets each), for hospital use only (NDC 24510-058-01).
100 mg extended-release tablets are light-blue oblong-shaped with a black print "OMJ 100" on one side and are available in bottles of 60 with child-resistant closure (NDC 24510-116-60) and unit dose blister packs of 100 (10 blister strips of 10 tablets each), for hospital use only (NDC 24510-116-01).
150 mg extended-release tablets are blue-green oblong-shaped with a black print "OMJ 150" on one side and are available in bottles of 60 with child-resistant closure (NDC 24510-174-60) and unit dose blister packs of 100 (10 blister strips of 10 tablets each), for hospital use only (NDC 24510-174-01).
200 mg extended-release tablets are blue oblong-shaped with a depression in the middle running lengthwise on each side and with a black print "OMJ 200" on one side, and are available in bottles of 60 with child- resistant closure (NDC 24510-232-60) and unit dose blister packs of 100 (10 blister strips of 10 tablets each), for hospital use only (NDC 24510-232-01).
250 mg extended-release tablets are dark blue oblong-shaped with a depression in the middle running lengthwise on each side and with a white print "OMJ 250" on one side, and are available in bottles of 60 with child-resistant closure (NDC 24510-291-60) and unit dose blister packs of 100 (10 blister strips of 10 tablets each), for hospital use only (NDC 24510-291-01).
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
| NUCYNTA
ER
tapentadol hydrochloride tablet, film coated, extended release |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| NUCYNTA
ER
tapentadol hydrochloride tablet, film coated, extended release |
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
| NUCYNTA
ER
tapentadol hydrochloride tablet, film coated, extended release |
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
| NUCYNTA
ER
tapentadol hydrochloride tablet, film coated, extended release |
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
| NUCYNTA
ER
tapentadol hydrochloride tablet, film coated, extended release |
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
| Labeler - Collegium Pharmaceutical, Inc. (032531241) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Janssen Pharmaceuticals, Inc. | 080236951 | API MANUFACTURE(24510-058, 24510-116, 24510-174, 24510-232, 24510-291) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Janssen Ortho, LLC | 805887986 | ANALYSIS(24510-058, 24510-116, 24510-174, 24510-232, 24510-291) , MANUFACTURE(24510-058, 24510-116, 24510-174, 24510-232, 24510-291) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Patheon Pharmaceuticals, Inc. | 005286822 | MANUFACTURE(24510-058, 24510-116, 24510-174, 24510-232, 24510-291) | |