Drug Detail:Nutropin aq nuspin 10 (Somatropin [ soe-ma-troe-pin ])
Drug Class: Growth hormones
Highlights of Prescribing Information
Nutropin AQ (somatropin) injection, for subcutaneous use
Initial U.S. Approval: 1987
Recent Major Changes
| Contraindications (4) | 12/2016 |
| Warnings and Precautions, (5) | 12/2016 |
Indications and Usage for Nutropin AQ
Nutropin AQ is a recombinant human growth hormone indicated for:
- Pediatric Patients: Treatment of children with growth failure due to growth hormone deficiency (GHD), idiopathic short stature (ISS), Turner syndrome (TS), and chronic kidney disease (CKD) up to the time of renal transplantation (1.1).
- Adult Patients: Treatment of adults with either childhood-onset or adult-onset GHD (1.2).
Nutropin AQ Dosage and Administration
Nutropin AQ should be administered subcutaneously (2).
Injection sites should always be rotated to avoid lipoatrophy (2.3).
|
|
|
|
|
|
|
|
|
|
|
|
Dosage Forms and Strengths
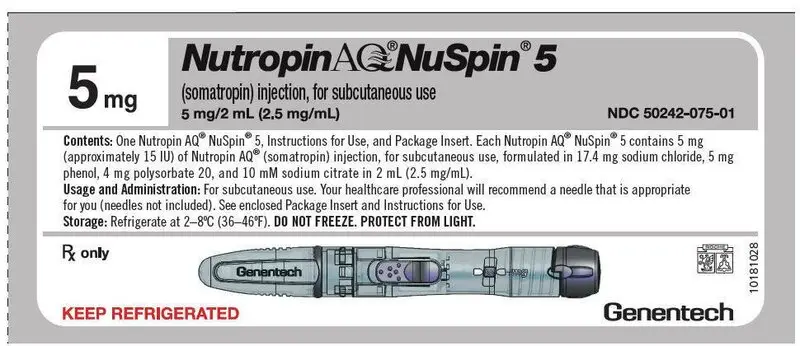
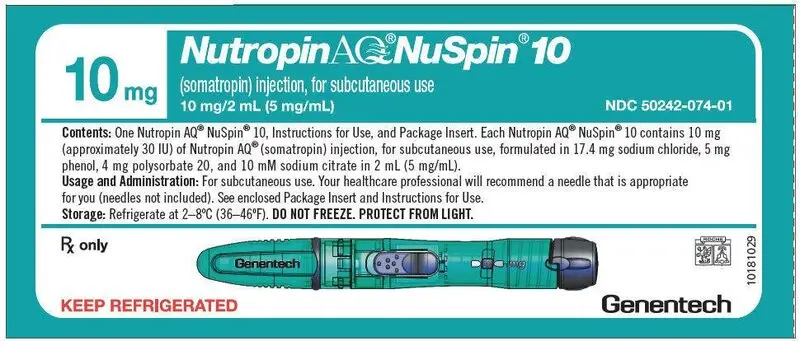
Nutropin AQ is a sterile liquid available in the following pen cartridge and NuSpin forms (3):
- Pen Cartridge: 10 mg/2 mL (yellow color band), and 20 mg/2 mL (purple color band).
- NuSpin: 5 mg/2 mL (clear device), 10 mg/2 mL (green device), and 20 mg/2 mL (blue device).
Contraindications
- Acute critical illness (4).
- Children with Prader-Willi syndrome (PWS) who are severely obese or have severe respiratory impairment – reports of sudden death (4).
- Active malignancy (4).
- Hypersensitivity to somatropin or excipients (4).
- Active proliferative or severe non-proliferative diabetic retinopathy (4).
- Children with closed epiphysis (4).
Warnings and Precautions
- Acute critical illness: Evaluate potential benefit of treatment continuation against potential risk (5.1).
- PWS: Evaluate for signs of upper airway obstruction and sleep apnea before initiating therapy. Discontinue treatment if these signs occur. (5.2).
- Neoplasm: Monitor patients with preexisting tumors for progression or reoccurrence. Increased risk of a second neoplasm in childhood cancer survivors treated with somatropin - in particular meningiomas in patients treated with radiation to the head for their first neoplasm. (5.3).
- Impaired glucose tolerance (IGT) and Diabetes Mellitus (DM): Periodically monitor glucose levels in all patients, as IGT and DM may be unmasked during somatropin therapy. Doses of concurrent antihyperglycemic drugs in patients with DM may require adjustment. (5.4).
- Intracranial hypertension (IH): Exclude preexisting papilledema. IH may develop, but is usually reversible after discontinuation or dose reduction (5.5).
- Hypersensitivity: Serious hypersensitivity reactions may occur. In the event of an allergic reaction, seek prompt medical attention (5.6).
- Fluid retention (e.g., edema, arthralgia, carpal tunnel syndrome- especially in adults): Reduce dose as necessary if such signs develop (5.7).
- Hypoadrenalism: Monitor patients for reduced serum cortisol levels and/or need for glucocorticoid dose increase in those with known hypoadrenalism (5.8).
- Hypothyroidism: Monitor thyroid function periodically as it may first become evident or worsen after initiation of somatropin (5.9).
- Slipped capital femoral epiphysis (SCFE): Evaluate any child with onset of a limp or hip/knee pain for possible SCFE (5.10).
- Progression of preexisting scoliosis: Monitor any child with scoliosis for progression of the curve (5.11).
- Pancreatitis: Consider pancreatitis in patients with persistent severe abdominal pain (5.16)
Adverse Reactions/Side Effects
Common somatropin-related adverse reactions include injection site reactions. Additional common adverse reactions in adults include edema, arthralgias, and carpal tunnel syndrome (6.1, 6.2).
To report SUSPECTED ADVERSE REACTIONS, contact Genentech at 1-888-835-2555 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Inhibition of 11 β-Hydroxysteroid Dehydrogenase Type 1: May require the initiation of glucocorticoid replacement therapy. Patients treated with glucocorticoid replacement for previously diagnosed hypoadrenalism may require an increase in their maintenance doses (7.1, 7.2).
- Glucocorticoid replacement: Should be carefully adjusted (7.2).
- Cytochrome P450 - Metabolized Drugs: Monitor carefully if used with somatropin (7.3).
- Oral estrogen: Larger doses of somatropin may be required in women (7.4).
- Insulin and/or other hypoglycemic agents: May require adjustment (7.5).
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 12/2016
Full Prescribing Information
1. Indications and Usage for Nutropin AQ
2. Nutropin AQ Dosage and Administration
For subcutaneous injection.
Therapy with Nutropin AQ should be supervised by a physician who is experienced in the diagnosis and management of pediatric patients with short stature associated with growth hormone deficiency (GHD), chronic kidney disease, Turner syndrome, idiopathic short stature, or adult patients with either childhood-onset or adult-onset GHD.
2.1 Dosing for Pediatric Patients
Nutropin AQ dosage and administration schedule should be individualized for each patient. Response to growth hormone (GH) therapy in pediatric patients tends to decrease with time. However, in pediatric patients failure to increase growth rate, particularly during the first year of therapy, suggests the need for close assessment of compliance and evaluation of other causes of growth failure, such as hypothyroidism, under-nutrition, advanced bone age and antibodies to recombinant human GH (rhGH).
Treatment with Nutropin AQ for short stature should be discontinued when the epiphyses are fused.
2.2 Dosing for Adult Patients
2.3 Preparation and Administration
The solution should be clear immediately after removal from the refrigerator. Occasionally, after refrigeration, you may notice that small colorless particles of protein are present in the solution. This is not unusual for solutions containing proteins. Allow the pen cartridge or NuSpin® to come to room temperature and gently swirl. If the solution is cloudy, the contents MUST NOT be injected.
Parenteral drug products should always be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Injection sites, which may be located on the thigh, upper arm, abdomen or buttock, should always be rotated to avoid lipoatrophy.
3. Dosage Forms and Strengths
Nutropin AQ is available in the following pen cartridge and NuSpin forms:
- Pen Cartridge: 10 mg/2 mL (yellow color band), and 20 mg/2 mL (purple color band)
- NuSpin: 5 mg/2 mL (clear device), 10 mg/2 mL (green device), and 20 mg/2 mL (blue device)
5. Warnings and Precautions
5.1 Acute Critical Illness
Increased mortality in patients with acute critical illnesses due to complications following open heart surgery, abdominal surgery or multiple accidental trauma, or those with acute respiratory failure has been reported after treatment with pharmacologic amounts of somatropin [see Contraindications (4)]. Two placebo-controlled clinical trials in non-GHD adult patients (n = 522) with these conditions in intensive care units revealed a significant increase in mortality (42% vs. 19%) among somatropin-treated patients (doses 5.3–8 mg/day) compared to those receiving placebo. The safety of continuing somatropin treatment in patients receiving replacement doses for approved indications who concurrently develop these illnesses has not been established. Therefore, the potential benefit of treatment continuation with somatropin in patients having acute critical illnesses should be weighed against the potential risk.
5.2 Prader-Willi Syndrome (PWS) in Children
There have been reports of fatalities after initiating therapy with somatropin in pediatric patients with PWS who had one or more of the following risk factors: severe obesity, history of upper airway obstruction or sleep apnea, or unidentified respiratory infection. Male patients with one or more of these factors may be at greater risk than females. Patients with PWS syndrome should be evaluated for signs of upper airway obstruction and sleep apnea before initiation of treatment with somatropin. If during treatment with somatropin, patients show signs of upper airway obstruction (including onset of or increased snoring) and/or new onset sleep apnea, treatment should be interrupted. All patients with PWS treated with somatropin should also have effective weight control and be monitored for signs of respiratory infection, which should be diagnosed as early as possible and treated aggressively [see Contraindications (4)]. Nutropin AQ is not indicated for the treatment of pediatric patients who have growth failure due to genetically confirmed PWS.
5.3 Neoplasms
In childhood cancer survivors who were treated with radiation to the brain/head for their first neoplasm and who developed subsequent GHD and were treated with somatropin, an increased risk of a second neoplasm has been reported. Intracranial tumors, in particular meningiomas, were the most common of these second neoplasms. In adults, it is unknown whether there is any relationship between somatropin replacement therapy and CNS tumor recurrence [see Contraindications (4)]. Monitor all patients with a history of GHD secondary to an intracranial neoplasm routinely while on somatropin therapy for progression or recurrence of the tumor.
Because children with certain rare genetic causes of short stature have an increased risk of developing malignancies, practitioners should thoroughly consider the risks and benefits of starting somatropin in these patients. If treatment with somatropin is initiated, these patients should be carefully monitored for development of neoplasms.
Monitor patients on somatropin therapy carefully for increased growth, or potential malignant changes, of preexisting nevi.
5.4 Glucose Intolerance and Diabetes Mellitus
Treatment with somatropin may decrease insulin sensitivity, particularly at higher doses in susceptible patients. As a result, previously undiagnosed impaired glucose tolerance (IGT) and overt diabetes mellitus may be unmasked during somatropin treatment, and new onset type 2 diabetes mellitus has been reported in patients taking somatropin. Therefore, glucose levels should be monitored periodically in all patients treated with somatropin, especially in those with risk factors for diabetes, such as obesity, Turner syndrome (TS), or a family history of diabetes mellitus. Patients with preexisting type 1 or type 2 diabetes mellitus or IGT should be monitored closely during somatropin therapy. The doses of antihyperglycemic drugs (i.e. insulin or oral/injectable agents) may require adjustment when somatropin therapy is instituted in these patients.
5.5 Intracranial Hypertension
Intracranial Hypertension (IH) with papilledema, visual changes, headache, nausea, and/or vomiting has been reported in a small number of patients treated with somatropin products. Symptoms usually occurred within the first eight (8) weeks after the initiation of somatropin therapy. In all reported cases, IH-associated signs and symptoms rapidly resolved after cessation of therapy or a reduction of the somatropin dose. Funduscopic examination should be performed routinely before initiating treatment with somatropin to exclude preexisting papilledema, and periodically during the course of somatropin therapy. If papilledema is observed by funduscopy during somatropin treatment, treatment should be stopped. If somatropin-induced IH is diagnosed, treatment with somatropin can be restarted at a lower dose after IH-associated signs and symptoms have resolved. Patients with TS, chronic kidney disease (CKD), and PWS may be at increased risk for the development of IH.
5.6 Severe Hypersensitivity
Serious systemic hypersensitivity reactions including anaphylactic reaction and angioedema have been reported with postmarketing use of somatropin products. Patients and caregivers should be informed that such reactions are possible and that prompt medical attention should be sought if an allergic reaction occurs.
5.7 Fluid Retention
Fluid retention during somatropin replacement therapy in adults may occur. Clinical manifestations of fluid retention (e.g., edema, arthralgia, myalgia, nerve compression syndromes including carpal tunnel syndrome/paraesthesias) are usually transient and dose dependent.
5.8 Hypoadrenalism
Patients receiving somatropin therapy who have or are at risk for pituitary hormone deficiency(s) may be at risk for reduced serum cortisol levels and/or unmasking of central (secondary) hypoadrenalism. In addition, patients treated with glucocorticoid replacement for previously diagnosed hypoadrenalism may require an increase in their maintenance or stress doses following initiation of somatropin treatment [see Section 7.1, 11-β Hydroxysteroid Dehydrogenase Type 1].
5.9 Hypothyroidism
Undiagnosed/untreated hypothyroidism may prevent an optimal response to somatropin, in particular, the growth response in children. Patients with TS have an inherently increased risk of developing autoimmune thyroid disease and primary hypothyroidism. In patients with GHD, central (secondary) hypothyroidism may first become evident or worsen during somatropin treatment. Therefore, patients treated with somatropin should have periodic thyroid function tests and thyroid hormone replacement therapy should be initiated or appropriately adjusted when indicated.
5.10 Slipped Capital Femoral Epiphysis (SCFE) in Pediatric Patients
SCFE may occur more frequently in patients with endocrine disorders (including GHD and TS) or in patients undergoing rapid growth. Any pediatric patient with the onset of a limp or complaints of hip or knee pain during somatropin therapy should be carefully evaluated.
5.11 Progression of Preexisting Scoliosis in Pediatric Patients
Progression of scoliosis can occur in patients who experience rapid growth. Because somatropin increases growth rate, patients with a history of scoliosis who are treated with somatropin should be monitored for progression of scoliosis. However, somatropin has not been shown to increase the occurrence of scoliosis. Skeletal abnormalities including scoliosis are commonly seen in untreated TS patients. Scoliosis is also commonly seen in untreated patients with PWS. Physicians should be alert to these abnormalities, which may manifest during somatropin therapy.
5.12 Otitis Media and Cardiovascular Disorders in Patients with Turner Syndrome
Patients with TS should be evaluated carefully for otitis media and other ear disorders, as these patients have an increased risk of ear and hearing disorders. Somatropin treatment may increase the occurrence of otitis media in patients with TS. In addition, patients with TS should be monitored closely for cardiovascular disorders (e.g., hypertension, aortic aneurysm or dissection, stroke) as these patients are also at increased risk for these conditions.
5.13 Osteodystrophy in Pediatric Patients with Chronic Kidney Disease
Children with growth failure secondary to CKD should be examined periodically for evidence of progression of renal osteodystrophy. SCFE or avascular necrosis of the femoral head may be seen in children with advanced renal osteodystrophy, and it is uncertain whether these problems are affected by somatropin therapy. X-rays of the hip should be obtained prior to initiating somatropin therapy in CKD patients and physicians and parents should be alert to the development of a limp or complaints of hip or knee pain in these patients treated with Nutropin AQ. No studies have been completed evaluating Nutropin AQ therapy in patients who have received renal transplants. Currently, treatment of patients with functioning renal allografts is not indicated.
5.14 Lipoatrophy
When somatropin is administered subcutaneously at the same site over a long period of time, tissue atrophy may result. This can be avoided by rotating the injection site [see Dosage and Administration (2.3)].
5.15 Laboratory Tests
Serum levels of inorganic phosphorus, alkaline phosphatase, and parathyroid hormone (PTH), and IGF-1 may increase during somatropin therapy.
5.16 Pancreatitis
Cases of pancreatitis have been reported rarely in children and adults receiving somatropin treatment, with some evidence supporting a greater risk in children compared with adults. Published literature indicates that girls who have TS may be at greater risk than other somatropin-treated children. Pancreatitis should be considered in any somatropin–treated patient, especially a child, who develops persistent severe abdominal pain.
6. Adverse Reactions/Side Effects
The following important adverse reactions are also described elsewhere in the labeling:
- Increased mortality in patients with acute critical illness [see Warnings and Precautions (5.1)]
- Fatalities in children with Prader-Willi syndrome [see Warnings and Precautions (5.2)]
- Neoplasms in pediatric patients [see Warnings and Precautions (5.3)]
- Glucose intolerance and diabetes mellitus [see Warnings and Precautions (5.4)]
- Intracranial hypertension [see Warnings and Precautions (5.5)]
- Severe hypersensitivity [see Warnings and Precautions (5.6)]
- Fluid retention [see Warnings and Precautions (5.7)]
- Hypoadrenalism [see Warnings and Precautions (5.8)]
- Hypothyroidism [see Warnings and Precautions (5.9)]
- Slipped capital femoral epiphysis in pediatric patients [see Warnings and Precautions (5.10)]
- Progression of preexisting scoliosis in pediatric patients [see Warnings and Precautions (5.11)]
- Otitis media and cardiovascular disorders in patients with Turner syndrome [see Warnings and Precautions (5.12)]
- Osteodystrophy in pediatric patients with chronic kidney disease [see Warnings and Precautions (5.13)]
- Lipoatrophy [see Warnings and Precautions (5.14)]
- Pancreatitis [see Warnings and Precautions (5.16)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under varying conditions, adverse reaction rates observed during the clinical trials performed with one somatropin formulation cannot always be directly compared to the rates observed during the clinical trials performed with a second somatropin formulation, and may not reflect the adverse reaction rates observed in practice.
Pediatric Patients
Idiopathic Short Stature (ISS)
In a post-marketing surveillance study, the National Cooperative Growth Study (NCGS), the pattern of adverse events in over 8,000 patients with ISS was consistent with the known safety profile of growth hormone (GH), and no new safety signals attributable to GH were identified. The frequency of protocol-defined targeted adverse events is described in the table, below.
| Reported Events | NCGS (N = 8018) |
|---|---|
| AVN = avascular necrosis; SCFE = slipped capital femoral epiphysis. Data obtained with several rhGH products (Nutropin, Nutropin AQ, Nutropin Depot and Protropin). |
|
| Any Adverse Event | |
| Overall | 103 (1.3%) |
| Targeted Adverse Event | |
| Overall | 103 (1.3%) |
| Injection-site reaction | 28 (0.3%) |
| New onset or progression of scoliosis | 16 (0.2%) |
| Gynecomastia | 12 (0.1%) |
| Any new onset or recurring tumor (benign) | 12 (0.1%) |
| Arthralgia or arthritis | 10 (0.1%) |
| Diabetes mellitus | 5 (0.1%) |
| Edema | 5 (0.1%) |
| Cancer, neoplasm (new onset or recurrence) | 4 (0.0%) |
| Fracture | 4 (0.0%) |
| Intracranial hypertension | 4 (0.0%) |
| Abnormal bone or other growth | 3 (0.0%) |
| Central nervous system tumor | 2 (0.0%) |
| New or recurrent SCFE or AVN | 2 (0.0%) |
| Carpal tunnel syndrome | 1 (0.0%) |
In subjects treated in a long-term study of Nutropin for ISS, mean fasting and postprandial insulin levels increased, while mean fasting and postprandial glucose levels remained unchanged. Mean hemoglobin A1c (A1C) levels rose slightly from baseline as expected during adolescence; sporadic values outside normal limits occurred transiently.
6.2 Immunogenicity
As with all therapeutic proteins, there is potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to Nutropin with the incidence of antibodies to other products may be misleading. In the case of GH, antibodies with binding capacities lower than 2 mg/L have not been associated with growth attenuation. In a very small number of patients treated with somatropin, when binding capacity was greater than 2 mg/L, interference with the growth response was observed.
In clinical studies of pediatric patients that were treated with Nutropin for the first time, 0/107 GHD patients, 0/125 CKD patients, 0/112 TS, and 0/117 ISS patients screened for antibody production developed antibodies with binding capacities ≥ 2 mg/L at six months. In a clinical study of patients that were treated with Nutropin AQ for the first time, 0/38 GHD patients screened for antibody production for up to 15 months developed antibodies with binding capacities ≥ 2 mg/L.
Additional short-term immunologic and renal function studies were carried out in a group of pediatric patients with CKD after approximately one year of treatment to detect other potential adverse effects of antibodies to GH. Testing included measurements of C1q, C3, C4, rheumatoid factor, creatinine, creatinine clearance, and blood urea nitrogen (BUN). No adverse effects of GH antibodies were noted.
6.3 Post-Marketing Experience
Because these adverse events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The adverse events reported during post-marketing surveillance do not differ from those listed/discussed above in Sections 6.1 and 6.2 in children and adults.
Serious systemic hypersensitivity reactions including anaphylactic reactions and angioedema have been reported with postmarketing use of somatropin products [see Warnings and Precautions (5.6)].
Leukemia has been reported in a small number of GHD children treated with somatropin, somatrem (methionylated rhGH) and GH of pituitary origin. It is uncertain whether these cases of leukemia are related to GH therapy, the pathology of GHD itself, or other associated treatments such as radiation therapy. On the basis of current evidence, experts have not been able to conclude that GH therapy per se was responsible for these cases of leukemia. The risk for children with GHD, CKD, or TS, if any, remains to be established [see Contraindications (4) and Warnings and Precautions (5.3)].
The following additional adverse reactions have been reported in GH-treated patients: gynecomastia (children), and pancreatitis [(Children and adults, see Warnings and Precautions (5.16)].
7. Drug Interactions
7.1 11 β-Hydroxysteroid Dehydrogenase Type 1 (11βHSD-1)
The microsomal enzyme 11βHSD-1 is required for conversion of cortisone to its active metabolite, cortisol, in hepatic and adipose tissue. Growth hormone (GH) and somatropin inhibit 11βHSD-1. Consequently, individuals with untreated GH deficiency have relative increases in 11βHSD-1 and serum cortisol. Introduction of somatropin treatment may result in inhibition of 11βHSD-1 and reduced serum cortisol concentrations. As a consequence, previously undiagnosed central (secondary) hypoadrenalism may be unmasked and glucocorticoid replacement may be required in patients treated with somatropin. In addition, patients treated with glucocorticoid replacement for previously diagnosed hypoadrenalism may require an increase in their maintenance or stress doses following initiation of somatropin treatment; this may be especially true for patients treated with cortisone acetate and prednisone since conversion of these drugs to their biologically active metabolites is dependent on the activity of 11βHSD-1.
7.2 Pharmacologic Glucocorticoid Therapy and Supraphysiologic Glucocorticoid Treatment
Pharmacologic glucocorticoid therapy and supraphysiologic glucocorticoid treatment may attenuate the growth-promoting effects of somatropin in children. Therefore, glucocorticoid replacement therapy should be carefully adjusted in children with concomitant GH and glucocorticoid deficiency to avoid both hypoadrenalism and an inhibitory effect on growth.
The use of Nutropin AQ in patients with Chronic Kidney Disease (CKD) requiring glucocorticoid therapy has not been evaluated. Concomitant glucocorticoid therapy may inhibit the growth promoting effect of Nutropin AQ. Therefore, if glucocorticoid replacement is required for CKD, the glucocorticoid dose should be carefully adjusted to avoid an inhibitory effect on growth. In the clinical trials there was no evidence of drug interactions with Nutropin and commonly used drugs used in the management of CKD.
7.3 Cytochrome P450 (CYP450)-Metabolized Drugs
Limited published data indicate that somatropin treatment increases CYP450-mediated antipyrine clearance in man. These data suggest that somatropin administration may alter the clearance of compounds known to be metabolized by CYP450 liver enzymes (e.g., corticosteroids, sex steroids, anticonvulsants, cyclosporine). Careful monitoring is advisable when somatropin is administered in combination with other drugs known to be metabolized by CYP450 liver enzymes. However, formal drug interaction studies have not been conducted.
8. Use In Specific Populations
8.3 Nursing Mothers
There have been no studies conducted with Nutropin AQ in nursing mothers. It is not known whether Nutropin AQ is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Nutropin AQ is administered to a nursing mother.
8.5 Geriatric Use
Clinical studies of Nutropin AQ did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Elderly patients may be more sensitive to the action of somatropin, and therefore may be more prone to develop adverse reactions. A lower starting dose and smaller dose increments should be considered for older patients [see Dosage and Administration (2.2)].
8.6 Hepatic Impairment
No studies have been conducted for Nutropin AQ in patients with hepatic impairment. [see Clinical Pharmacology (12.3)].
11. Nutropin AQ Description
Nutropin AQ (somatropin) injection, for subcutaneous use is a human growth hormone (hGH) produced by recombinant DNA technology. Nutropin AQ has 191 amino acid residues and a molecular weight of 22,125 daltons. The amino acid sequence of the product is identical to that of pituitary-derived hGH. Nutropin AQ may contain not more than fifteen percent deamidated GH at expiration. The deamidated form of GH has been extensively characterized and has been shown to be safe and fully active.
Nutropin AQ is a sterile liquid intended for subcutaneous administration. The product is nearly isotonic at a concentration of 5 mg of GH per mL and has a pH of approximately 6.0.
Each pen cartridge or NuSpin contain either 5 mg, 10 mg or 20 mg of somatropin formulated in 17.4 mg sodium chloride, 5 mg phenol, 4 mg polysorbate 20, and 10 mM sodium citrate [see How Supplied/Storage and Handling (16)].
12. Nutropin AQ - Clinical Pharmacology
12.1 Mechanism of Action
Somatropin (as well as endogenous growth hormone) binds to dimeric growth hormone receptors located within the cell membranes of target tissue cells resulting in intracellular signal transduction and a host of pharmacodynamic effects. Some of these pharmacodynamic effects are primarily mediated by insulin-like growth factor (IGF-1) produced in the liver and also locally (e.g., skeletal growth, protein synthesis), while others are primarily a consequence of the direct effects of somatropin (e.g., lipolysis) [see Clinical Pharmacology (12.2)].
12.2 Pharmacodynamics
In vitro and in vivo preclinical and clinical testing have demonstrated that Nutropin AQ is therapeutically equivalent to pituitary-derived hGH. Pediatric patients who lack adequate endogenous growth hormone (GH) secretion, patients with chronic kidney disease (CKD), and patients with Turner syndrome (TS) that were treated with Nutropin AQ or Nutropin resulted in an increase in growth rate and an increase in IGF-1 levels similar to that seen with pituitary-derived hGH.
12.3 Pharmacokinetics
Special Populations
Gender: No gender-specific pharmacokinetic studies have been done with Nutropin AQ. The available literature indicates that the pharmacokinetics of somatropin are similar in men and women.
| Cmax
(µg/L) | Tmax
(hr) | t1/2
(hr) | AUC0-∞
(μg ∙ hr/L) | CL/Fsc
(mL/[hr ∙ kg]) |
|
|---|---|---|---|---|---|
| Abbreviations: AUC0-∞ = area under the curve, Cmax = maximum concentration, CL/Fsc = systemic clearance, CV% = coefficient of variation in %; SC = subcutaneous, Fsc = subcutaneous bioavailability (not determined), t1/2 = half-life. | |||||
|
|||||
| MEAN† | 71.1 | 3.9 | 2.3 | 677 | 150 |
| CV% | 17 | 56 | 18 | 13 | 13 |
| Figure 1
Single Dose Mean Growth Hormone Concentrations in Healthy Adult Males |
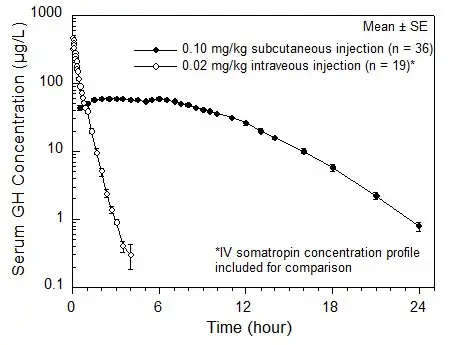 |
14. Clinical Studies
14.1 Pubertal Patients with Growth Hormone Deficiency (GHD)
One open label, multicenter, randomized clinical trial of two dosages of Nutropin was performed in pubertal patients with GHD. Ninety-seven patients (mean age 13.9 years, 83 male, 14 female) currently being treated with approximately 0.3 mg/kg/wk of GH were randomized to 0.3 mg/kg/wk or 0.7 mg/kg/wk Nutropin doses. All patients were already in puberty (Tanner stage ≥ 2) and had bone ages ≤ 14 years in males or ≤ 12 years in females. Mean baseline height standard deviation score (SDS) was –1.3.
The mean last measured height in all 97 patients after a mean duration of 2.7 ± 1.2 years, by analysis of covariance (ANCOVA) adjusting for baseline height, is shown below.
| Last Measured Height* (cm) | Height Difference Between Groups (cm) | |||
|---|---|---|---|---|
| Age (yr) | 0.3 mg/kg/wk | 0.7 mg/kg/wk | ||
| Mean ± SD (range) | Mean ± SD | Mean ± SD | Mean ± SE | |
|
||||
| Male | 17.2 ± 1.3 (13.6 to 19.4) | 170.9 ± 7.9 (n = 42) | 174.5 ± 7.9 (n = 41) | 3.6 ± 1.7 |
| Female | 15.8 ± 1.8 (11.9 to 19.3) | 154.7 ± 6.3 (n = 7) | 157.6 ± 6.3 (n = 7) | 2.9 ± 3.4 |
The mean height SDS at last measured height (n = 97) was –0.7 ± 1.0 in the 0.3 mg/kg/wk group and – 0.1 ± 1.2 in the 0.7 mg/kg/wk group. For patients completing 3.5 or more years (mean 4.1 years) of Nutropin treatment (15/49 patients in the 0.3 mg/kg/wk group and 16/48 patients in the 0.7 mg/kg/wk group), the mean last measured height was 166.1 ± 8.0 cm in the 0.3 mg/kg/wk group and 171.8 ± 7.1 cm in the 0.7 mg/kg/wk group, adjusting for baseline height and sex.
The mean change in bone age was approximately one year for each year in the study in both dose groups. Patients with baseline height SDS above –1.0 were able to attain normal adult heights with the 0.3 mg/kg/wk dose of Nutropin (mean height SDS at near-adult height = –0.1, n = 15).
Thirty-one patients had bone mineral density (BMD) determined by dual energy x-ray absorptiometry (DEXA) scans at study conclusion. The two dose groups did not differ significantly in mean SDS for total body BMD (–0.9 ± 1.9 in the 0.3 mg/kg/wk group vs. –0.8 ± 1.2 in the 0.7 mg/kg/wk group, n = 20) or lumbar spine BMD (–1.0 ± 1.0 in the 0.3 mg/kg/wk group vs. –0.2 ± 1.7 in the 0.7 mg/kg/wk group, n = 21).
Over a mean duration of 2.7 years, patients in the 0.7 mg/kg/wk group were more likely to have IGF-I values above the normal range than patients in the 0.3 mg/kg/wk group (27.7% vs. 9.0% of IGF-I measurements for individual patients). The clinical significance of elevated IGF-I values is unknown.
14.2 Pediatric Patients with Growth Failure Secondary to Chronic Kidney Disease (CKD)
Two multicenter, randomized, controlled clinical trials were conducted to determine whether treatment with Nutropin prior to renal transplantation in patients with CKD could improve their growth rates and height deficits. One study was a double-blind, placebo-controlled trial and the other was an open-label, randomized trial. The dose of Nutropin in both controlled studies was 0.05 mg/kg/day (0.35 mg/kg/week) administered daily by subcutaneous injection. Combining the data from those patients completing two years in the two controlled studies results in 62 patients treated with Nutropin and 28 patients in the control groups (either placebo-treated or untreated). The mean first year growth rate was 10.8 cm/yr for Nutropin-treated patients, compared with a mean growth rate of 6.5 cm/yr for placebo/untreated controls (p < 0.00005). The mean second year growth rate was 7.8 cm/yr for the Nutropin-treated group, compared with 5.5 cm/yr for controls (p < 0.00005). There was a significant increase in mean height SDS in the Nutropin group (–2.9 at baseline to –1.5 at Month 24, n = 62) but no significant change in the controls (-2.8 at baseline to –2.9 at Month 24, n = 28). The mean third year growth rate of 7.6 cm/yr in the Nutropin-treated patients (n = 27) suggests that Nutropin stimulates growth beyond two years. However, there are no control data for the third year because control patients crossed over to Nutropin treatment after two years of participation. The gains in height were accompanied by appropriate advancement of skeletal age. These data demonstrate that Nutropin therapy improves growth rate and corrects the acquired height deficit associated with CKD.
The North American Pediatric Renal Transplant Cooperative Study (NAPRTCS) has reported data for growth post-transplant in children who did not receive GH prior to transplantation as well as children who did receive Nutropin during the clinical trials prior to transplantation. The average change in height SDS during the initial two years post-transplant was 0.15 for the 2,391 patients who did not receive GH pre-transplant and 0.28 for the 57 patients who did1. For patients who were followed for 5 years post-transplant, the corresponding changes in height SDS were also similar between groups.
14.3 Pediatric Patients with Turner Syndrome (TS)
Three US studies, two long-term, open-label, multicenter, historically controlled studies (Studies 1 and 2), and one long-term, randomized, dose-response study (Study 3) and one Canadian, long-term, randomized, open-label, multicenter, concurrently controlled study, were conducted to evaluate the efficacy of somatropin treatment of short stature due to TS.
In the US Studies 1 and 2, the effect of long-term GH treatment (0.375 mg/kg/week given either 3 times per week or daily) on adult height was determined by comparing adult heights in the treated patients with those of age-matched historical controls with TS who received no growth-promoting therapy. In Study 1, estrogen treatment was delayed until patients were at least age 14. GH therapy resulted in a mean adult height gain of 7.4 cm (mean duration of GH therapy of 7.6 years) vs. matched historical controls by ANCOVA.
In Study 2, patients treated with early Nutropin therapy (before 11 years of age) were randomized to receive estrogen-replacement therapy (conjugated estrogens, 0.3 mg escalating to 0.625 mg daily) at either age 12 or 15 years. Compared with matched historical controls, early Nutropin therapy (mean duration of 5.6 years) combined with estrogen replacement at age 12 years resulted in an adult height gain of 5.9 cm (n = 26), whereas girls who initiated estrogen at age 15 years (mean duration of Nutropin therapy 6.1 years) had a mean adult height gain of 8.3 cm (n = 29). Patients who initiated Nutropin after age 11 (mean age 12.7 years; mean duration of Nutropin therapy 3.8 years) had a mean adult height gain of 5.0 cm (n = 51).
Thus, in Studies 1 and 2, the greatest improvement in adult height was observed in patients who received early GH treatment and estrogen after age 14 years.
In Study 3, a randomized, blinded dose-response study, patients were treated from a mean age of 11.1 years for a mean duration of 5.3 years with a weekly GH dose of either 0.27 mg/kg or 0.36 mg/kg administered in divided doses 3 or 6 times weekly. The mean near-final height of GH-treated patients was 148.7 ± 6.5 cm (n = 31). When compared to historical control data, the mean gain in adult height was approximately 5 cm.
The Canadian randomized study compared near-adult height outcomes for GH-treated patients to those of a concurrent control group who received no injections. The somatropin-treated patients received a dosage of 0.3 mg/kg/week given in divided doses 6 times per week from a mean age of 11.7 years for a mean duration of 4.7 years. Puberty was induced with a standardized estrogen regimen initiated at 13 years of age for both treatment groups. The somatropin-treated group (n = 27) attained a mean (± SD) near final height of 146.0 ± 6.2 cm; the untreated control group (n = 19) attained a near final height of 142.1 ± 4.8 cm. By ANCOVA (with adjustments for baseline height and mid-parental height), the effect of GH-treatment was a mean height increase of 5.4 cm (p = 0.001).
In summary, patients with TS (total n = 181 from the 4 studies above) treated to adult height achieved statistically significant average height gains ranging from 5.0–8.3 cm.
| Study | Group | Study Design† | N at Adult Height | GH Age (yr) | Estrogen Age (yr) | GH Duration (yr) | Adult Height Gain (cm)‡ |
|---|---|---|---|---|---|---|---|
|
|||||||
| US 1 | MHT | 17 | 9.1 | 15.2 | 7.6 | 7.4 | |
| US 2 | A§ | MHT | 29 | 9.4 | 15.0 | 6.1 | 8.3 |
| B§ | 26 | 9.6 | 12.3 | 5.6 | 5.9 | ||
| C§ | 51 | 12.7 | 13.7 | 3.8 | 5.0 | ||
| US 3 | RDT | 31 | 11.1 | 8–13.5 | 5.3 | ~5¶ | |
| Canadian | RCT | 27 | 11.7 | 13 | 4.7 | 5.4 | |
14.4 Pediatric Patient with Idiopathic Short Stature (ISS)
A long-term, open-label, multicenter study was conducted to examine the safety and efficacy of Nutropin in pediatric patients with ISS, also called non-growth hormone deficient short stature. For the first year, 122 pre-pubertal subjects over the age of 5 years with stimulated serum GH ≥ 10 ng/mL were randomized into two treatment groups of approximately equal size; one group was treated with Nutropin 0.3 mg/kg weekly divided into three doses per week and the other group served as untreated controls. For the second and subsequent years of the study, all subjects were re-randomized to receive the same total weekly dose of Nutropin (0.3 mg/kg weekly) administered either daily or three times weekly. Treatment with Nutropin was continued until a subject's bone age was > 15.0 years (boys) or > 14.0 years (girls) and the growth rate was < 2 cm/yr, after which subjects were followed until adult height was achieved. The mean baseline values were: height SDS–2.8, IGF-I SDS -0.9, age 9.4 years, bone age 7.8 years, growth rate 4.4 cm/yr, mid-parental target height SDS –0.7, and Bayley-Pinneau predicted adult height SDS –2.3. Nearly all subjects had predicted adult height that was less than mid-parental target height.
During the one-year controlled phase of the study, the mean height velocity increased by 0.5 ± 1.8 cm (mean ± SD) in the no-treatment control group and by 3.1 ± 1.7 cm in the Nutropin group (p < 0.0001). For the same period of treatment the mean height SDS increased by 0.4 ± 0.2 and remained unchanged (0.0 ± 0.2) in the control group (p < 0.001).
Of the 118 subjects who were treated with Nutropin (70%) reached near-adult height (hereafter called adult height) after 2–10 years of Nutropin therapy. Their last measured height, including post-treatment follow-up, was obtained at a mean age of 18.3 years in males and 17.3 years in females. The mean duration of therapy was 6.2 and 5.5 years, respectively. Adult height was greater than pretreatment predicted adult height in 49 of 60 males (82%) and 19 of 23 females (83%). The mean difference between adult height and pretreatment predicted adult height was 5.2 cm (2.0 inches) in males and 6.0 cm (2.4 inches) in females (p < 0.0001 for both). The table (below) summarizes the efficacy data.
| Characteristic | Males (n = 60) | Females (n = 23) |
|---|---|---|
|
||
| Adult height (cm) | 166.3 ± 5.8 | 153.1 ± 4.8 |
| Pretreatment predicted adult height (cm) | 161.1 ± 5.5 | 147.1 ± 5.1 |
| Adult height minus pretreatment predicted adult height (cm) | + 5.2 ± 5.0* | + 6.0 ± 5.0* |
| Adult height SDS | –1.5 ± 0.8 | –1.6 ± 0.7 |
| Pretreatment predicted adult height SDS | –2.2 ± 0.8 | –2.5 ± 0.8 |
| Adult height minus pretreatment predicted adult height SDS | + 0.7 ± 0.7* | + 0.9 ± 0.8* |
Nutropin therapy resulted in an increase in mean IGF-I SDS from –0.9 ± 1.0 to –0.2 ± 0.9 in Treatment Year 1. During continued treatment, mean IGF-I levels remained close to the normal mean. IGF-I SDS above + 2 occurred sporadically in 14 subjects.
14.5 Adult Growth Hormone Deficiency
Two multicenter, double-blind, placebo-controlled clinical trials were conducted in growth hormone-deficient adults. Study 1 was conducted in subjects with adult-onset GHD (n = 166), mean age 48.3 years, at doses of 0.0125 or 0.00625 mg/kg/day; doses of 0.025 mg/kg/day were not tolerated in these subjects. Study 2 was conducted in previously treated subjects with childhood-onset GHD (n = 64), mean age 23.8 years, at randomly assigned doses of 0.025 or 0.0125 mg/kg/day. The studies were designed to assess the effects of replacement therapy with Nutropin on body composition.
Significant changes from baseline to Month 12 of treatment in body composition (i.e., total body % fat mass, trunk % fat mass, and total body % lean mass by DEXA scan) were seen in all Nutropin groups in both studies (p < 0.0001 for change from baseline and vs. placebo), whereas no statistically significant changes were seen in either of the placebo groups. In the adult-onset study, the Nutropin group improved mean total body fat from 35.0% to 31.5%, mean trunk fat from 33.9% to 29.5%, and mean lean body mass from 62.2% to 65.7%, whereas the placebo group had mean changes of 0.2% or less (p = not significant). Due to the possible effect of GH-induced fluid retention on DEXA measurements of lean body mass, DEXA scans were repeated approximately 3 weeks after completion of therapy; mean % lean body mass in the Nutropin group was 65.0%, a change of 2.8% from baseline, compared with a change of 0.4% in the placebo group (p < 0.0001 between groups).
In the childhood-onset study, the high-dose Nutropin group improved mean total body fat from 38.4% to 32.1%, mean trunk fat from 36.7% to 29.0%, and mean lean body mass from 59.1% to 65.5%; the low-dose Nutropin group improved mean total body fat from 37.1% to 31.3%, mean trunk fat from 37.9% to 30.6%, and mean lean body mass from 60.0% to 66.0%; the placebo group had mean changes of 0.6% or less (p = not significant).
| Adult Onset (Study 1) | Childhood Onset (Study 2) |
||||||
|---|---|---|---|---|---|---|---|
| Proportion | Placebo (n = 62) | Nutropin (n = 63) | Between-Groups t-test p-value | Placebo (n = 13) | Nutropin 0.0125 mg/kg/day (n = 15) | Nutropin 0.025 mg/kg/day (n = 15) | Placebo vs. Pooled Nutropin t-test p-value |
| NA = not available | |||||||
| Total body percent fat | |||||||
| Baseline | 36.8 | 35.0 | 0.38 | 35.0 | 37.1 | 38.4 | 0.45 |
| Month 12 | 36.8 | 31.5 | — | 35.2 | 31.3 | 32.1 | — |
| Baseline to Month 12 change | -0.1 | -3.6 | < 0.0001 | + 0.2 | -5.8 | -6.3 | < 0.0001 |
| Post-washout | 36.4 | 32.2 | — | NA | NA | NA | — |
| Baseline to post-washout change | -0.4 | -2.8 | < 0.0001 | NA | NA | NA | — |
| Trunk percent fat | |||||||
| Baseline | 35.3 | 33.9 | 0.50 | 32.5 | 37.9 | 36.7 | 0.23 |
| Month 12 | 35.4 | 29.5 | — | 33.1 | 30.6 | 29.0 | — |
| Baseline to Month 12 change | 0.0 | -4.3 | < 0.0001 | + 0.6 | -7.3 | -7.6 | < 0.0001 |
| Post-washout | 34.9 | 30.5 | — | NA | NA | NA | — |
| Baseline to post-washout change | -0.3 | -3.4 | — | NA | NA | NA | — |
| Total body percent lean | |||||||
| Baseline | 60.4 | 62.2 | 0.37 | 62.0 | 60.0 | 59.1 | 0.48 |
| Month 12 | 60.5 | 65.7 | — | 61.8 | 66.0 | 65.5 | — |
| Baseline to Month 12 change | + 0.2 | + 3.6 | < 0.0001 | -0.2 | + 6.0 | + 6.4 | < 0.0001 |
| Post-washout | 60.9 | 65.0 | — | NA | NA | NA | — |
| Baseline to post-washout change | + 0.4 | + 2.8 | < 0.0001 | NA | NA | NA | — |
In the adult-onset study, significant decreases from baseline to Month 12 in low-density lipoprotein (LDL) cholesterol and LDL:high-density lipoprotein (HDL) ratio were seen in the Nutropin group compared to the placebo group, p < 0.02; there were no statistically significant between-group differences in change from baseline to Month 12 in total cholesterol, HDL cholesterol, or triglycerides. In the childhood-onset study significant decreases from baseline to Month 12 in total cholesterol, LDL cholesterol, and LDL:HDL ratio were seen in the high-dose Nutropin group only, compared to the placebo group, p < 0.05. There were no statistically significant between-group differences in HDL cholesterol or triglycerides from baseline to Month 12.
In the childhood-onset study, 55% of the patients had decreased spine BMD (z-score < –1) at baseline. The administration of Nutropin (n = 16) (0.025 mg/kg/day) for two years resulted in increased spine BMD from baseline when compared to placebo (n = 13) (4.6% vs. 1.0%, respectively, p < 0.03); a transient decrease in spine BMD was seen at six months in the Nutropin-treated patients. Thirty-five percent of subjects treated with this dose had supraphysiological levels of IGF-I at some point during the study, which may carry unknown risks. No significant improvement in total body BMD was found when compared to placebo. A lower GH dose (0.0125 mg/kg/day) did not show significant increments in either of these bone parameters when compared to placebo. No statistically significant effects on BMD were seen in the adult-onset study where patients received GH (0.0125 mg/kg/day) for one year.
Muscle strength, physical endurance, and quality of life measurements were not markedly abnormal at baseline, and no statistically significant effects of Nutropin therapy were observed in the two studies.
A subsequent 32-week, multicenter, open-label, controlled clinical trial was conducted using Nutropin AQ, Nutropin Depot, or no treatment in adults with both adult-onset and childhood-onset GHD. Subjects were randomized into the three groups to evaluate effects on body composition, including change in visceral adipose tissue (VAT) as determined by computed tomography (CT) scan.
For subjects evaluable for change in VAT in the Nutropin AQ (n = 44) and untreated (n = 19) groups, the mean age was 46.2 years and 78% had adult-onset GHD. Subjects in the Nutropin AQ group were treated at doses up to 0.012 mg/kg per day in women (all of whom received estrogen replacement therapy) and men under age 35 years, and up to 0.006 mg/kg per day in men over age 35 years.
The mean absolute change in VAT from baseline to Week 32 was –10.7 cm2 in the Nutropin AQ group and + 8.4 cm2 in the untreated group (p = 0.013 between groups). There was a 6.7% VAT loss in the Nutropin AQ group (mean percent change from baseline to Week 32) compared with a 7.5% increase in the untreated group (p = 0.012 between groups). The effect of reducing VAT in adult GHD patients with Nutropin AQ on long-term cardiovascular morbidity and mortality has not been determined.
| Nutropin AQ (n = 44) | Untreated (n = 19) | Treatment Difference (adjusted mean) | p-value | |
|---|---|---|---|---|
| VAT = visceral adipose tissue. | ||||
|
||||
| Baseline VAT (cm2) (mean) | 126.2 | 123.3 | ||
| Change in VAT (cm2) (adjusted mean) | – 10.7 | + 8.4 | – 19.1 | 0.013* |
| Percent change in VAT (adjusted mean) | – 6.7 | + 7.5 | – 14.2 | 0.012* |
16. How is Nutropin AQ supplied
| Pen Cartridge (2 mL): | 10 mg 20 mg | NDC 50242-043-14 NDC 50242-073-01 |
| Nutropin AQ NuSpin (2 mL): | 5 mg 10 mg 20 mg | NDC 50242-075-01 NDC 50242-074-01 NDC 50242-076-01 |
17. Patient Counseling Information
Patients being treated with Nutropin AQ (and/or their parents) should be informed about the potential benefits and risks associated with Nutropin AQ treatment, including a review of the contents of the INSTRUCTIONS FOR USE. This information is intended to better educate patients (and caregivers); it is not a disclosure of all possible adverse or intended effects.
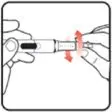
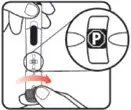
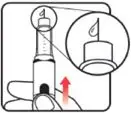
Patients and caregivers who will administer Nutropin AQ should receive appropriate training and instruction on the proper use of Nutropin AQ from the physician or other suitably qualified health care professional. A puncture-resistant container for the disposal of used syringes and needles should be strongly recommended. Patients and/or parents should be thoroughly instructed in the importance of proper disposal, and cautioned against any reuse of needles and syringes. This information is intended to aid in the safe and effective administration of the medication.
Please see the accompanying directions for use of the delivery device.
| NUTROPIN AQ NUSPIN 5
somatropin injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| NUTROPIN AQ NUSPIN 10
somatropin injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| NUTROPIN AQ NUSPIN 20
somatropin injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Genentech, Inc. (080129000) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Genentech, Inc. | 080129000 | ANALYSIS(50242-074, 50242-075, 50242-076) , API MANUFACTURE(50242-074, 50242-075, 50242-076) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Genentech, Inc. | 833220176 | PACK(50242-074, 50242-075, 50242-076) | |




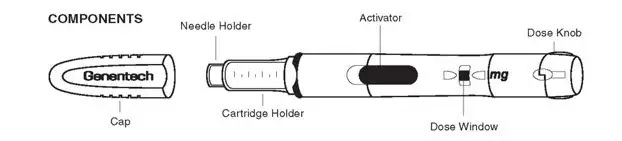




 .
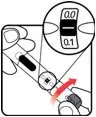
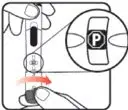
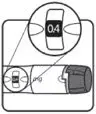
. between those two numbers indicates your dose. Turn the dose knob to
between those two numbers indicates your dose. Turn the dose knob to  .
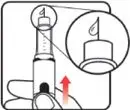
. ).
). and continue to
and continue to  , you have received your full dose.
, you have received your full dose. , your Nutropin AQ NuSpin 5 is empty and you have not received your full dose.
, your Nutropin AQ NuSpin 5 is empty and you have not received your full dose.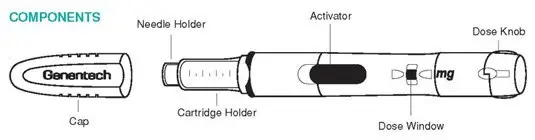








 .
. between those two numbers indicates your dose. Turn the dose knob to
between those two numbers indicates your dose. Turn the dose knob to  .
. ).
). and continue to
and continue to  , you have received your full dose.
, you have received your full dose. , your Nutropin AQ NuSpin 10 is empty and you have not received your full dose.
, your Nutropin AQ NuSpin 10 is empty and you have not received your full dose.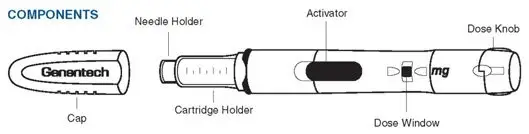






 .
. between those two numbers indicates your dose. Turn the dose knob to
between those two numbers indicates your dose. Turn the dose knob to  .
. ).
). and continue to
and continue to  , you have received your full dose.
, you have received your full dose. , your Nutropin AQ NuSpin 20 is empty and you have not received your full dose.
, your Nutropin AQ NuSpin 20 is empty and you have not received your full dose.