Drug Detail:Ocaliva (Obeticholic acid [ oh-bet-i-koe-lik-as-id ])
Drug Class: Miscellaneous GI agents
Highlights of Prescribing Information
OCALIVA® (obeticholic acid) tablets, for oral use
Initial U.S. Approval: 2016
WARNING: HEPATIC DECOMPENSATION AND FAILURE IN PRIMARY BILIARY CHOLANGITIS PATIENTS WITH CIRRHOSIS
See full prescribing information for complete boxed warning
- Hepatic decompensation and failure, sometimes fatal or resulting in liver transplant, have been reported with OCALIVA treatment in primary biliary cholangitis (PBC) patients with either compensated or decompensated cirrhosis. (5.1)
- OCALIVA is contraindicated in PBC patients with decompensated cirrhosis, a prior decompensation event, or with compensated cirrhosis who have evidence of portal hypertension. (4)
- Permanently discontinue OCALIVA in patients who develop laboratory or clinical evidence of hepatic decompensation, have compensated cirrhosis and develop evidence of portal hypertension, or experience clinically significant hepatic adverse reactions while on treatment. (2.3, 5.1)
Indications and Usage for Ocaliva
OCALIVA, a farnesoid X receptor (FXR) agonist, is indicated for the treatment of adult patients with primary biliary cholangitis (PBC)
- without cirrhosis or
- with compensated cirrhosis who do not have evidence of portal hypertension,
either in combination with ursodeoxycholic acid (UDCA) with an inadequate response to UDCA or as monotherapy in patients unable to tolerate UDCA.
This indication is approved under accelerated approval based on a reduction in alkaline phosphatase (ALP). An improvement in survival or disease-related symptoms has not been established. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials. (1)
Ocaliva Dosage and Administration
Recommended Dosage Regimen
The recommended starting dosage of OCALIVA, for PBC patients without cirrhosis or with compensated cirrhosis who do not have evidence of portal hypertension, who have not achieved an adequate biochemical response to an appropriate dosage of UDCA for at least 1 year or who are intolerant to UDCA follows below:
- Start with a dosage of 5 mg once daily for the first 3 months.
- After the first 3 months, for patients who have not achieved an adequate reduction in ALP and/or total bilirubin and who are tolerating OCALIVA, increase to a maximum dosage of 10 mg once daily. (2.2)
Routinely monitor patients during OCALIVA treatment for biochemical response, tolerability, and progression of PBC. (2.3)
Management of Patients with Intolerable Pruritus
- See full prescribing information for management options. (2.4)
Administration Instructions
- Take with or without food. (2.5)
- For patients taking bile acid binding resins, take OCALIVA at least 4 hours before or 4 hours after taking a bile acid binding resin, or at as great an interval as possible. (7.1)
Dosage Forms and Strengths
Tablets: 5 mg, 10 mg (3)
Contraindications
- decompensated cirrhosis (e.g., Child-Pugh Class B or C) or a prior decompensation event (4)
- compensated cirrhosis with evidence of portal hypertension (e.g., ascites, gastroesophageal varices, persistent thrombocytopenia) (4)
- complete biliary obstruction (4)
Warnings and Precautions
- Hepatic Decompensation and Failure in PBC Patients with Cirrhosis: Routinely monitor patients for progression of PBC, including hepatic adverse reactions, with laboratory and clinical assessments. Closely monitor patients at risk of hepatic decompensation. Permanently discontinue in patients who develop laboratory or clinical evidence of hepatic decompensation; have compensated cirrhosis and develop evidence of portal hypertension; experience clinically significant hepatic adverse reactions; or develop complete biliary obstruction. Interrupt treatment in patients with severe intercurrent illness. (2.3, 4, 5.1)
- Severe Pruritus: Management strategies include the addition of bile acid binding resins or antihistamines; OCALIVA dosage reduction and/or temporary dosing interruption. (2.4, 5.2)
- Reduction in HDL-C: Monitor for changes in serum lipid levels during treatment. (5.3)
Adverse Reactions/Side Effects
Most common adverse reactions (≥ 5%) are: pruritus, fatigue, abdominal pain and discomfort, rash, oropharyngeal pain, dizziness, constipation, arthralgia, thyroid function abnormality, and eczema. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Intercept Pharmaceuticals at 1-844-782-ICPT or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Warfarin: Potential for decreased INR; monitor INR and adjust the dosage of warfarin, as needed, to maintain the target INR range. (7.2)
- CYP1A2 Substrates with Narrow Therapeutic Index (e.g., theophylline and tizanidine): Potential for increased exposure to CYP1A2 substrates; monitor drug concentrations of CYP1A2 substrates with narrow therapeutic index. (7.3)
- Inhibitors of Bile Salt Efflux Pump (e.g., cyclosporine): Avoid use. If concomitant use is necessary, monitor serum transaminases and bilirubin. (7.4)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 5/2022
Full Prescribing Information
WARNING: HEPATIC DECOMPENSATION AND FAILURE IN PRIMARY BILIARY CHOLANGITIS PATIENTS WITH CIRRHOSIS
- Hepatic decompensation and failure, sometimes fatal or resulting in liver transplant, have been reported with OCALIVA treatment in primary biliary cholangitis (PBC) patients with either compensated or decompensated cirrhosis [see Warnings and Precautions (5.1)].
- OCALIVA is contraindicated in PBC patients with decompensated cirrhosis, a prior decompensation event, or with compensated cirrhosis who have evidence of portal hypertension [see Contraindications (4)].
- Permanently discontinue OCALIVA in patients who develop laboratory or clinical evidence of hepatic decompensation; have compensated cirrhosis and develop evidence of portal hypertension; or experience clinically significant hepatic adverse reactions while on treatment [see Dosage and Administration (2.3), Warnings and Precautions (5.1)].
1. Indications and Usage for Ocaliva
OCALIVA® is indicated for the treatment of adult patients with primary biliary cholangitis (PBC)
- without cirrhosis or
- with compensated cirrhosis who do not have evidence of portal hypertension,
either in combination with ursodeoxycholic acid (UDCA) with an inadequate response to UDCA or as monotherapy in patients unable to tolerate UDCA.
This indication is approved under accelerated approval based on a reduction in alkaline phosphatase (ALP) [see Clinical Studies (14)]. An improvement in survival or disease-related symptoms has not been established. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
2. Ocaliva Dosage and Administration
2.1 Important Dosage and Administration Instructions
Prior to the initiation of OCALIVA, healthcare providers should determine whether the patient has decompensated cirrhosis (e.g., Child-Pugh Class B or C), has had a prior decompensation event, or has compensated cirrhosis with evidence of portal hypertension (e.g., ascites, gastroesophageal varices, persistent thrombocytopenia) because OCALIVA is contraindicated in these patients [see Contraindications (4), Warnings and Precautions (5.1)].
2.2 Recommended Dosage Regimen
The recommended dosage of OCALIVA for PBC patients without cirrhosis or with compensated cirrhosis who do not have evidence of portal hypertension, who have not achieved an adequate biochemical response to an appropriate dosage of UDCA for at least 1 year or are intolerant to UDCA [see Clinical Studies (14)] follows below:
- Start with a dosage of 5 mg once daily for the first 3 months.
- After the first 3 months, for patients who have not achieved an adequate reduction in ALP and/or total bilirubin and who are tolerating OCALIVA, increase to a maximum dosage of 10 mg once daily.
2.3 Monitoring to Assess Safety, Need for OCALIVA Discontinuation
Routinely monitor patients during OCALIVA treatment for biochemical response, tolerability, and progression of PBC. Closely monitor patients with compensated cirrhosis, concomitant hepatic disease (e.g., autoimmune hepatitis, alcoholic liver disease), and/or severe intercurrent illness for new evidence of portal hypertension (e.g., ascites, gastroesophageal varices, persistent thrombocytopenia) or increases above the upper limit of normal in total bilirubin, direct bilirubin, or prothrombin time. Permanently discontinue OCALIVA in patients who develop laboratory or clinical evidence of hepatic decompensation, have compensated cirrhosis and develop evidence of portal hypertension, experience clinically significant hepatic adverse reactions, or develop complete biliary obstruction [see Contraindications (4), Warnings and Precautions (5.1)].
2.4 Management of Patients with Intolerable Pruritus on OCALIVA
For patients with intolerable pruritus on OCALIVA, consider one or more of the following management strategies:
- Add an antihistamine or bile acid binding resin [see Dosage and Administration (2.5), Clinical Studies (14)].
- Reduce the dosage of OCALIVA to:
- 5 mg every other day, for patients intolerant to 5 mg once daily.
- 5 mg once daily, for patients intolerant to 10 mg once daily.
- Temporarily interrupt OCALIVA dosing for up to 2 weeks. Restart at a reduced dosage.
For patients whose dosage is reduced or interrupted, titrate the dosage based on biochemical response and tolerability [see Dosage and Administration (2.2)].
Consider discontinuing OCALIVA treatment in patients who continue to experience persistent, intolerable pruritus despite management strategies [see Warnings and Precautions (5.2)].
3. Dosage Forms and Strengths
OCALIVA is available as:
- 5 mg tablet: Off white to yellow, round tablet debossed with "INT" on one side and "5" on the other side.
- 10 mg tablet: Off white to yellow, triangular tablet debossed with "INT" on one side and "10" on the other side.
4. Contraindications
OCALIVA is contraindicated in patients with:
- decompensated cirrhosis (e.g., Child-Pugh Class B or C) or a prior decompensation event [see Warnings and Precautions (5.1)].
- compensated cirrhosis who have evidence of portal hypertension (e.g., ascites, gastroesophageal varices, persistent thrombocytopenia) [see Warnings and Precautions (5.1)].
- complete biliary obstruction.
5. Warnings and Precautions
5.1 Hepatic Decompensation and Failure in PBC Patients with Cirrhosis
Hepatic decompensation and failure, sometimes fatal or resulting in liver transplant, have been reported with OCALIVA treatment in PBC patients with cirrhosis, either compensated or decompensated. Among postmarketing cases reporting it, median time to hepatic decompensation (e.g., new onset ascites) was 4 months for patients with compensated cirrhosis; median time to a new decompensation event (e.g., hepatic encephalopathy) was 2.5 months for patients with decompensated cirrhosis.
Some of these cases occurred in patients with decompensated cirrhosis when they were treated with higher than the recommended dosage for that patient population; however, cases of hepatic decompensation and failure have continued to be reported in patients with decompensated cirrhosis even when they received the recommended dosage.
Hepatotoxicity was observed in the OCALIVA clinical trials. A dose-response relationship was observed for the occurrence of hepatic adverse reactions including jaundice, worsening ascites, and primary biliary cholangitis flare with dosages of OCALIVA of 10 mg once daily to 50 mg once daily (up to 5-times the highest recommended dosage), as early as one month after starting treatment with OCALIVA in two 3-month, placebo-controlled clinical trials in patients with primarily early stage PBC [see Overdosage (10)].
In a pooled analysis of three placebo-controlled clinical trials in patients with primarily early stage PBC, the exposure-adjusted incidence rates for all serious and otherwise clinically significant hepatic adverse reactions, and isolated elevations in liver biochemical tests, per 100 patient exposure years (PEY) were: 5.2 in the OCALIVA 10 mg group (highest recommended dosage), 19.8 in the OCALIVA 25 mg group (2.5-times the highest recommended dosage) and 54.5 in the OCALIVA 50 mg group (5-times the highest recommended dosage) compared to 2.4 in the placebo group.
5.2 Severe Pruritus
Severe pruritus was reported in 23% of patients in the OCALIVA 10 mg arm, 19% of patients in the OCALIVA titration arm, and 7% of patients in the placebo arm in Trial 1, a 12-month double-blind randomized controlled clinical trial of 216 patients [see Adverse Reactions (6.1)]. Severe pruritus was defined as intense or widespread itching, interfering with activities of daily living, or causing severe sleep disturbance, or intolerable discomfort, and typically requiring medical interventions. In the subgroup of patients in the OCALIVA titration arm who increased their dosage from 5 mg once daily to 10 mg once daily after 6 months of treatment (n=33), the incidence of severe pruritus was 0% from Months 0 to 6 and 15% from Months 6 to 12. The median time to onset of severe pruritus was 11, 158, and 75 days for patients in the OCALIVA 10 mg, OCALIVA titration, and placebo arms, respectively.
Consider clinical evaluation of patients with new onset or worsening severe pruritus. Management strategies include the addition of bile acid binding resins or antihistamines, OCALIVA dosage reduction, and/or temporary interruption of OCALIVA dosing [see Dosage and Administration (2.4)].
5.3 Reduction in HDL-C
Patients with PBC generally exhibit hyperlipidemia characterized by a significant elevation in total cholesterol primarily due to increased levels of high-density lipoprotein-cholesterol (HDL-C). In Trial 1, dose-dependent reductions from baseline in mean HDL-C levels were observed at 2 weeks in OCALIVA-treated patients, 20% and 9% in the 10 mg and titration arms, respectively, compared to 2% in the placebo arm. At Month 12, the reduction from baseline in mean HDL-C level was 19% in the OCALIVA 10 mg arm, 12% in the OCALIVA titration arm, and 2% in the placebo arm. Nine patients in the OCALIVA 10 mg arm, 6 patients in the OCALIVA titration arm, versus 3 patients in the placebo arm had reductions in HDL-C to less than 40 mg/dL.
Monitor patients for changes in serum lipid levels during treatment. For patients who do not respond to OCALIVA after 1 year at the highest recommended dosage that can be tolerated (maximum of 10 mg once daily), and who experience a reduction in HDL-C, weigh the potential risks against the benefits of continuing treatment.
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions are described elsewhere in labeling:
- Hepatic Decompensation and Failure in PBC Patients with Cirrhosis [see Warnings and Precautions (5.1)]
- Severe Pruritus [see Warnings and Precautions (5.2)]
- Reduction in HDL-C [see Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
A total of 432 patients with PBC were studied in three double-blind, placebo-controlled clinical trials. Of these patients, 290 were treated with OCALIVA for at least 6 months, 232 were treated for at least 12 months, and 70 were treated for at least 2 years. There were 131 patients who received OCALIVA 10 mg once daily and 70 who received OCALIVA 5 mg once daily.
In Trial 1, 216 patients were randomized (1:1:1) to receive either:
- OCALIVA 10 mg once daily for the entire 12 months of the trial (n=73)
- OCALIVA titration (5 mg once daily for the initial 6 months, with the option to increase to 10 mg once daily for the last 6 months, in patients who were tolerating OCALIVA, but had ALP 1.67-times ULN or greater, and/or total bilirubin greater than ULN, or less than 15% ALP reduction) (n=70); or
- placebo (n=73).
During the trial, OCALIVA or placebo was administered in combination with UDCA in 93% of patients and as monotherapy in 7% of patients who were unable to tolerate UDCA. The overall discontinuation rate was 12% in the OCALIVA 10 mg arm, 10% in the OCALIVA titration arm, and 4% in the placebo arm.
The recommended starting dosage of OCALIVA is 5 mg orally once daily for 3 months with titration to 10 mg once daily based upon tolerability and response [see Dosage and Administration (2.2)]. Initiation of therapy with OCALIVA 10 mg once daily is not recommended due to an increased risk of pruritus.
The most common adverse reactions in Trial 1 occurring in at least 5% of patients in either OCALIVA treatment arm and at an incidence at least 1% higher than the placebo treatment arm are shown in Table 1.
| Placebo N=73 % |
|||
|---|---|---|---|
| Adverse Reaction† | OCALIVA 10 mg N=73 % | OCALIVA Titration‡ N=70 % |
|
|
|||
| Pruritus§ | 70 | 56 | 38 |
| Fatigue¶ | 25 | 19 | 15 |
| Abdominal pain and discomfort# | 10 | 19 | 14 |
| RashÞ | 10 | 7 | 8 |
| Arthralgia | 10 | 6 | 4 |
| Oropharyngeal pain | 8 | 7 | 1 |
| Dizzinessß | 7 | 7 | 5 |
| Constipation | 7 | 7 | 5 |
| Peripheral Edema | 7 | 3 | 3 |
| Palpitations | 7 | 3 | 1 |
| Pyrexia | 7 | 0 | 1 |
| Thyroid function abnormalityà | 4 | 6 | 3 |
| Eczema | 3 | 6 | 0 |
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of OCALIVA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure, particularly in PBC patients who have progressive liver disease.
7. Drug Interactions
7.1 Bile Acid Binding Resins
Bile acid binding resins such as cholestyramine, colestipol, or colesevelam adsorb and reduce bile acid absorption and may reduce the absorption, systemic exposure, and efficacy of OCALIVA. If taking a bile acid binding resin, take OCALIVA at least 4 hours before or 4 hours after taking the bile acid binding resin, or at as great an interval as possible [see Dosage and Administration (2.5)].
7.2 Warfarin
The International Normalized Ratio (INR) decreased following coadministration of warfarin and OCALIVA [see Clinical Pharmacology (12.3)]. Monitor INR and adjust the dosage of warfarin, as needed, to maintain the target INR range when co-administering OCALIVA and warfarin.
7.3 CYP1A2 Substrates with Narrow Therapeutic Index
Obeticholic acid may increase the exposure to concomitant drugs that are CYP1A2 substrates [see Clinical Pharmacology (12.3)]. Therapeutic monitoring of CYP1A2 substrates with a narrow therapeutic index (e.g., theophylline and tizanidine) is recommended when co-administered with OCALIVA.
7.4 Inhibitors of Bile Salt Efflux Pump
Avoid concomitant use of inhibitors of the bile salt efflux pump (BSEP) such as cyclosporine [see Clinical Pharmacology (12.3)]. Concomitant medications that inhibit canalicular membrane bile acid transporters such as the BSEP may exacerbate accumulation of conjugated bile salts including taurine conjugate of obeticholic acid in the liver and result in clinical symptoms. If concomitant use is deemed necessary, monitor serum transaminases and bilirubin.
8. Use In Specific Populations
8.4 Pediatric Use
The safety and effectiveness of OCALIVA in pediatric patients have not been established.
8.5 Geriatric Use
Of the 201 patients in clinical trials of OCALIVA who received the recommended dosage (5 mg or 10 mg once daily), 41 (20%) were 65 years of age and older, while 9 (4%) were 75 years of age and older. No overall differences in safety or effectiveness were observed between these patients and patients less than 65 years of age, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Hepatic Impairment
Hepatic decompensation and failure, sometimes fatal or resulting in liver transplant, have been reported with OCALIVA treatment in PBC patients with cirrhosis, either compensated or decompensated [see Warnings and Precautions (5.1)]. OCALIVA is contraindicated in patients with decompensated cirrhosis (e.g., Child-Pugh Class B or C), in those with a prior decompensation event, or with compensated cirrhosis who have evidence of portal hypertension (e.g., ascites, gastroesophageal varices, persistent thrombocytopenia) [see Contraindications (4)].
In PBC clinical trials, a dose-response relationship was observed for the occurrence of hepatic adverse reactions with OCALIVA [see Warnings and Precautions (5.1)].
Plasma exposure to obeticholic acid and its active conjugates, increases significantly in patients with moderate to severe hepatic impairment [see Clinical Pharmacology (12.3)].
Routinely monitor patients for progression of PBC with laboratory and clinical assessments. Closely monitor patients with compensated cirrhosis, concomitant hepatic disease, and/or severe intercurrent illness for new evidence of portal hypertension (e.g., ascites, gastroesophageal varices, persistent thrombocytopenia) or increases above the upper limit of normal in total bilirubin, direct bilirubin, or prothrombin time to determine whether drug discontinuation is needed. Permanently discontinue OCALIVA in patients who develop laboratory or clinical evidence of hepatic decompensation, have compensated cirrhosis and develop evidence of portal hypertension, or experience clinically significant hepatic adverse reactions while on treatment. Interrupt treatment during severe intercurrent illness [see Dosage and Administration (2.3), Warnings and Precautions (5.1)].
10. Overdosage
In the clinical trials, PBC patients who received OCALIVA 25 mg once daily (2.5-times the highest recommended dosage) or 50 mg once daily (5-times the highest recommended dosage) experienced a dose-dependent increase in the incidence of hepatic adverse reactions, including elevations in liver biochemical tests, ascites, jaundice, portal hypertension, and primary biliary cholangitis flares.
Serious hepatic adverse reactions have been reported postmarketing in PBC patients with decompensated cirrhosis when OCALIVA was dosed more frequently than the recommended dosage; these adverse reactions were also reported in some patients who received the recommended dosage [see Contraindications (4), Warnings and Precautions (5.1)].
In the case of overdosage, patients should be carefully observed, and supportive care administered, as appropriate.
11. Ocaliva Description
OCALIVA is a farnesoid X receptor (FXR) agonist. Chemically, obeticholic acid is 3α,7α-dihydroxy-6α-ethyl-5β-cholan-24-oic acid. It is a white to off-white powder. It is soluble in methanol, acetone and ethyl acetate. Its solubility in water is pH dependent. It is slightly soluble at low pH and very soluble at high pH. Its chemical formula is C26H44O4, the molecular weight is 420.63 g/mol, and the chemical structure is:
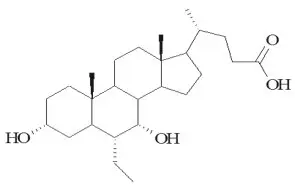
OCALIVA tablets are supplied in 5 mg and 10 mg strengths for oral administration. Each tablet contains obeticholic acid as the active ingredient and the following inactive ingredients: microcrystalline cellulose, sodium starch glycolate, and magnesium stearate. The film coating is Opadry II (Yellow) containing polyvinyl alcohol-part hydrolyzed, titanium dioxide, macrogol (polyethylene glycol 3350), talc, and iron oxide yellow.
12. Ocaliva - Clinical Pharmacology
12.1 Mechanism of Action
Obeticholic acid is an agonist for FXR, a nuclear receptor expressed in the liver and intestine. FXR is a key regulator of bile acid, inflammatory, fibrotic, and metabolic pathways. FXR activation decreases the intracellular hepatocyte concentrations of bile acids by suppressing de novo synthesis from cholesterol as well as by increased transport of bile acids out of the hepatocytes. These mechanisms limit the overall size of the circulating bile acid pool while promoting choleresis, thus reducing hepatic exposure to bile acids.
12.3 Pharmacokinetics
Drug Interaction Studies
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenic potential of obeticholic acid was assessed in carcinogenicity studies of up to 2 years in duration in mice and rats. In mice, there were no drug-related neoplastic findings at doses up to 25 mg/kg/day obeticholic acid, a dose that produced systemic exposures approximately 12-times those in humans at the MRHD of 10 mg. In rats, obeticholic acid was administered at doses of 2, 7, and 20 mg/kg/day. At 20 mg/kg/day (approximately 12-times the human exposure at the MRHD), obeticholic acid caused an increase in the incidence of benign granulosa cell tumors in the ovaries and benign granular cell tumors in the cervix and vagina of female rats. There were no drug-related neoplastic findings in male rats.
Obeticholic acid was not genotoxic in the Ames test, a human peripheral blood lymphocyte chromosomal aberration test, and a mouse micronucleus test. The glycine conjugate of obeticholic acid was also not genotoxic in an Ames test and human peripheral blood lymphocyte chromosome aberration test. The taurine conjugate of obeticholic acid was not genotoxic in an Ames test, and was negative in a human peripheral blood lymphocyte chromosomal aberration test in the presence of metabolic activation; the findings of the chromosomal aberration assay in the absence of metabolic activation were inconclusive.
Obeticholic acid, administered at oral doses of 5, 25, and 50 mg/kg/day to male rats for 28 days before mating and throughout the mating period, and to female rats from 14 days before mating through mating and until gestation day 7, did not alter male or female fertility or early embryonic development at any dose (the 50 mg/kg/day dose is approximately 13-times the human exposure at the MRHD).
14. Clinical Studies
The recommended starting dosage of OCALIVA is 5 mg orally once daily for 3 months with titration to 10 mg once daily based upon tolerability and response [see Dosage and Administration (2.2)]. Initiation of therapy with a starting dosage OCALIVA 10 mg once daily is not recommended due to an increased risk of pruritus [see Adverse Reactions (6.1)].
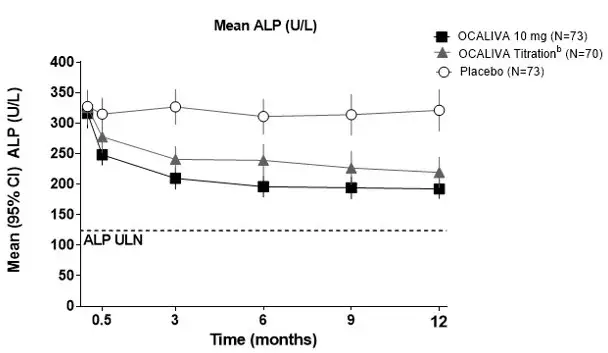
Trial 1 was a randomized, double-blind, placebo-controlled, 12-month clinical trial which evaluated the safety and efficacy of OCALIVA in 216 patients with PBC who were taking UDCA for at least 12 months (on a stable dosage for at least 3 months), or who were unable to tolerate UDCA and did not receive UDCA for at least 3 months. Patients were included in the trial if the ALP was 1.67-times upper limit of normal (ULN) or greater and/or if total bilirubin was greater than 1-times ULN but less than 2-times ULN. Patients were excluded from the trial if they had other liver disease, presence of clinically significant hepatic decompensation events (i.e., portal hypertension and its complications, cirrhosis with complications, or hepato-renal syndrome), severe pruritus, or Model for End Stage Liver Disease (MELD) score of 15 or greater.
Patients were randomized (1:1:1) to receive either OCALIVA 10 mg once daily for the entire 12 months of the trial, (n=73); OCALIVA titration (5 mg once daily for the initial 6 months, with the option to increase to 10 mg once daily for the last 6 months if the patient was tolerating OCALIVA but had ALP 1.67-times ULN or greater, and/or total bilirubin greater than ULN, or less than 15% ALP reduction) (n=70); or placebo (n=73). OCALIVA or placebo was administered in combination with UDCA in 93% of patients during the trial and as monotherapy in 7% of patients who were unable to tolerate UDCA.
The primary endpoint was a responder analysis at Month 12, where response was defined as a composite of three criteria: ALP less than 1.67-times the ULN, total bilirubin less than or equal to ULN, and an ALP decrease of at least 15%. The ULN for ALP was defined as 118 U/L for females and 124 U/L for males. The ULN for total bilirubin was defined as 1.1 mg/dL for females and 1.5 mg/dL for males.
The study population was 91% female and 94% white. The mean age was 56 years (range 29 to 86 years). The mean baseline ALP concentration was 323.2 U/L, corresponding to 2.74-times ULN. Approximately 29% of the patients had ALP concentration levels greater than 3-times the ULN. The mean baseline total bilirubin concentration was 0.65 mg/dL and was less than or equal to the ULN in 92% of the enrolled patients. Distribution of patients by Rotterdam disease stage criteria at baseline is shown in Table 2. Cirrhosis was present at baseline in 4 patients (5%) in the OCALIVA 10 mg arm, 7 patients (10%) in the OCALIVA titration arm, and 9 patients (12%) in the placebo arm.
| Disease Stage† | OCALIVA 10 mg (N=73) | OCALIVA Titration (N=70) | Placebo (N=73) |
|---|---|---|---|
| Percentages are based on non-missing values for each time point. | |||
|
|||
| Early, n (%) | 66 (90) | 64 (91) | 65 (89) |
| Moderately Advanced, n (%) | 7 (10) | 6 (9) | 8 (11) |
| Advanced, n (%) | 0 (0) | 0 (0) | 0 (0) |
Table 3 shows the percentage of patients by treatment arm in Trial 1 who achieved a response to the primary composite endpoint at Month 12, and to the individual components of the primary endpoint (i.e., ALP less than 1.67-times the ULN, total bilirubin less than or equal to ULN, and an ALP decrease of at least 15%). A total of 33 patients in the OCALIVA titration arm, who did not achieve a response at 6 months and tolerated OCALIVA, had their dosage increased from 5 mg once daily to 10 mg once daily. Of these 33 patients, 13 (39%) achieved the primary composite endpoint at 12 months.
| OCALIVA 10 mg (N=73) | OCALIVA Titration† (N=70) | Placebo (N=73) |
|
|---|---|---|---|
|
|||
| Primary Composite Endpoint‡ | |||
| Responder rate, (%)§ | 48 | 46 | 10 |
| [95% CI] | [36, 60] | [34, 58] | [4, 19] |
| Components of Primary Endpoint¶ | |||
| ALP less than 1.67-times ULN, n (%) | 40 (55) | 33 (47) | 12 (16) |
| Decrease in ALP of at least 15%, n (%) | 57 (78) | 54 (77) | 21 (29) |
| Total bilirubin less than or equal to ULN#, n (%) | 60 (82) | 62 (89) | 57 (78) |
16. How is Ocaliva supplied
OCALIVA tablets are packaged in a 40 mL high density polyethylene bottle closed with a 33 mm polypropylene child resistant cap containing an induction seal. Each bottle contains 30 tablets.
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised: April 2022 | |||
| MEDICATION GUIDE OCALIVA® (o-CAL-eh-vah) (obeticholic acid) tablets |
||||
What is the most important information I should know about OCALIVA?
Worsening of liver problems or liver failure, in some cases leading to liver transplant or death, has happened in people with primary biliary cholangitis (PBC) with liver cirrhosis when taking OCALIVA.
|
||||
|
|
|||
|
||||
|
|
|||
| What is OCALIVA?
OCALIVA is a prescription medicine used to treat primary biliary cholangitis (PBC) in combination with ursodeoxycholic acid (UDCA) in adults who have not responded well enough to UDCA, or alone in adults who cannot tolerate UDCA. It is not known if taking OCALIVA will improve your chance of survival or improve your symptoms of PBC. It is not known if OCALIVA is safe and effective in children. |
||||
Do not take OCALIVA if you:
|
||||
Before taking OCALIVA, tell your healthcare provider about all of your medical conditions, including if you:
|
||||
How should I take OCALIVA?
|
||||
| What are the possible side effects of OCALIVA? OCALIVA can cause serious side effects, including:
|
||||
|
|
|
||
| These are not all the possible side effects of OCALIVA. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. | ||||
How should I store OCALIVA?
|
||||
| General information about the safe and effective use of OCALIVA.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use OCALIVA for a condition for which it was not prescribed. Do not give OCALIVA to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about OCALIVA that is written for health professionals. |
||||
| What are the ingredients in OCALIVA? Active ingredient: obeticholic acid Inactive ingredients: microcrystalline cellulose, sodium starch glycolate, magnesium stearate Film coating: Opadry II (Yellow) containing polyvinyl alcohol-part hydrolyzed, titanium dioxide, macrogol (polyethylene glycol 3350), talc, iron oxide yellow Distributed by: Intercept Pharmaceuticals, Inc., Morristown, NJ 07960 OCALIVA is a registered trademark of Intercept Pharmaceuticals, Inc. For more information, go to www.OCALIVA.com or call 1-844-782-4278. |
||||
| OCALIVA
obeticholic acid tablet, film coated |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| OCALIVA
obeticholic acid tablet, film coated |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Intercept Pharmaceuticals Inc (966658416) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pharmacia & Upjohn Company LLC | 618054084 | ANALYSIS(69516-005, 69516-010) , API MANUFACTURE(69516-005, 69516-010) | |