Drug Detail:Omnitrope (Somatropin [ soe-ma-troe-pin ])
Drug Class: Growth hormones
Highlights of Prescribing Information
OMNITROPE® (somatropin) injection, for subcutaneous use
Initial U.S. Approval: 1987
Indications and Usage for Omnitrope
OMNITROPE is a recombinant human growth hormone indicated for:
- •
- Pediatric: Treatment of children with growth failure due to growth hormone deficiency (GHD), Prader-Willi Syndrome, Small for Gestational Age, Turner syndrome, and Idiopathic Short Stature (1.1)
- •
- Adult: Treatment of adults with either adult onset or childhood onset GHD (1.2)
Omnitrope Dosage and Administration
OMNITROPE should be administered subcutaneously (2).
- •
- Pediatric GHD: 0.16 to 0.24 mg/kg/week, divided into 6 to 7 daily injections (2.1)
- •
- Prader-Willi Syndrome: 0.24 mg/kg/week, divided into 6 to 7 daily injections (2.1)
- •
- Small for Gestational Age: Up to 0.48 mg/kg/week, divided into 6 to 7 daily injections (2.1)
- •
- Turner Syndrome: 0.33 mg/kg/week, divided into 6 to 7 daily injections (2.1)
- •
- Idiopathic Short Stature: Up to 0.47 mg/kg/week, divided into 6 to 7 daily injections (2.1)
- •
- Adult GHD: not more than 0.04 mg/kg/week (divided into daily injections) to be increased as tolerated to not more than 0.08 mg/kg/week); to be increased gradually every 1 to 2 months (2.2)
- •
- OMNITROPE Cartridges 5 mg/1.5 mL and 10 mg/1.5 mL must be used with the corresponding OMNITROPE Pen 5 and Pen 10 delivery system, respectively (2.3)
- •
- Injection sites should always be rotated to avoid lipoatrophy (2.3)
Dosage Forms and Strengths
- •
- OMNITROPE Cartridge 5 mg/1.5 mL is a prefilled sterile solution in a glass cartridge ready to be administered with the Omnitrope Pen 5 (3)
- •
- OMNITROPE Cartridge 10 mg/1.5 mL is a prefilled sterile solution in a glass cartridge ready to be administered with the Omnitrope Pen 10 (3)
- •
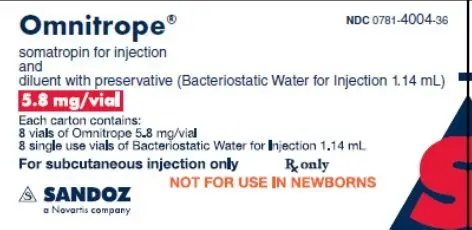
- OMNITROPE for injection 5.8 mg/vial is supplied with two vials, one containing somatropin as a powder and the other vial containing diluent (3)
Contraindications
- •
- Acute Critical Illness (4)
- •
- Children with Prader-Willi Syndrome who are severely obese or have severe respiratory impairment - reports of sudden death (4)
- •
- Active Malignancy (4)
- •
- Hypersensitivity to somatropin or its excipients (4)
- •
- Active Proliferative or Severe Non-Proliferative Diabetic Retinopathy (4)
- •
- Children with closed epiphyses (4)
- •
- Known hypersensitivity to somatropin or excipients (4)
Warnings and Precautions
- •
- Acute Critical Illness: Potential benefit of treatment continuation should be weighed against the potential risk (5.1)
- •
- Prader-Willi Syndrome in children: Evaluate for signs of upper airway obstruction and sleep apnea before initiation of treatment. Discontinue treatment if these signs occur (5.2)
- •
- Neoplasm: Monitor patients with preexisting tumors for progression or recurrence. Increased risk of a second neoplasm in childhood cancer survivors treated with somatropin - in particular meningiomas in patients treated with radiation to the head for their first neoplasm (5.3)
- •
- Impaired Glucose Tolerance and Diabetes Mellitus: May be unmasked. Periodically monitor glucose levels in all patients. Doses of concurrent antihyperglycemic drugs in diabetics may require adjustment (5.4)
- •
- Intracranial Hypertension: Exclude preexisting papilledema. May develop and is usually reversible after discontinuation or dose reduction (5.5)
- •
- Hypersensitivity: Serious hypersensitivity reactions may occur. In the event of an allergic reaction, seek prompt medical attention (5.6)
- •
- Fluid Retention (i.e., edema, arthralgia, carpal tunnel syndrome - especially in adults): May occur frequently. Reduce dose as necessary (5.7)
- •
- Hypoadrenalism: Monitor patients for reduced serum cortisol levels and/or need for glucocorticoid dose increases in those with known hypoadrenalism (5.8)
- •
- Hypothyroidism: May first become evident or worsen (5.9)
- •
- Slipped Capital Femoral Epiphysis: May develop. Evaluate children with the onset of a limp or hip/knee pain (5.10)
- •
- Progression of Preexisting Scoliosis: May develop (5.11)
- •
- Pancreatitis: Consider pancreatitis in patients with persistent severe abdominal pain (5.16)
Adverse Reactions/Side Effects
Other common somatropin-related adverse reactions include injection site reactions/rashes and lipoatrophy (6.1) and headaches (6.2).
To report SUSPECTED ADVERSE REACTIONS, contact Sandoz Inc. at 1-800-525-8747 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- •
- 11β-Hydroxysteroid Dehydrogenase Type 1: May require the initiation of glucocorticoid replacement therapy. Patients treated with glucocorticoid replacement for previously diagnosed hypoadrenalism may require an increase in their maintenance doses (7.1, 7.2)
- •
- Pharmacologic Glucocorticoid Therapy and Supraphysiologic Glucocorticoid Treatment: Should be carefully adjusted (7.2)
- •
- Cytochrome P450-Metabolized Drugs: Monitor carefully if used with somatropin (7.3)
- •
- Oral Estrogen: Larger doses of somatropin may be required in women (7.4)
- •
- Insulin and/or Oral Hypoglycemic Agents: May require adjustment (7.5)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 6/2019
Full Prescribing Information
1. Indications and Usage for Omnitrope
1.1 Pediatric Patients
Omnitrope (somatropin) injection is indicated for the treatment of children with growth failure due to inadequate secretion of endogenous growth hormone (GH).
Omnitrope (somatropin) injection is indicated for the treatment of pediatric patients who have growth failure due to Prader-Willi Syndrome (PWS). The diagnosis of PWS should be confirmed by appropriate genetic testing [see Contraindications (4) and Warnings and Precautions (5.2)].
Omnitrope (somatropin) injection is indicated for the treatment of growth failure in children born small for gestational age (SGA) who fail to manifest catch-up growth by age 2 years.
Omnitrope (somatropin) injection is indicated for the treatment of growth failure associated with Turner syndrome.
Omnitrope (somatropin) injection is indicated for the treatment of idiopathic short stature (ISS), also called non-growth hormone-deficient short stature, defined by height standard deviation score (SDS) ≤ -2.25, and associated with growth rates unlikely to permit attainment of adult height in the normal range, in pediatric patients whose epiphyses are not closed and for whom diagnostic evaluation excludes other causes associated with short stature that should be observed or treated by other means.
1.2 Adult Patients
Omnitrope (somatropin) injection is indicated for the replacement of endogenous GH in adults with growth hormone deficiency (GHD) who meet either of the following two criteria:
- •
- Adult Onset (AO): Patients who have GHD, either alone or associated with multiple hormone deficiencies (hypopituitarism), as a result of pituitary disease, hypothalamic disease, surgery, radiation therapy, or trauma; or
- •
- Childhood Onset (CO): Patients who were GH deficient during childhood as a result of congenital, genetic, acquired, or idiopathic causes.
Patients who were treated with somatropin for growth hormone deficiency in childhood and whose epiphyses are closed should be reevaluated before continuation of somatropin therapy at the reduced dose level recommended for growth hormone deficient adults. Confirmation of the diagnosis of adult growth hormone deficiency in both groups involves an appropriate growth hormone provocative test with two exceptions: (1) patients with multiple other pituitary hormone deficiencies due to organic disease; and (2) patients with congenital/genetic growth hormone deficiency.
2. Omnitrope Dosage and Administration
The weekly dose should be divided over 6 or 7 days of subcutaneous injections.
Therapy with Omnitrope should be supervised by a physician who is experienced in the diagnosis and management of pediatric patients with short stature associated with GHD, Prader-Willi Syndrome (PWS), Turner syndrome (TS), those who were born small for gestational age (SGA), Idiopathic Short Stature (ISS) and adult patients with either childhood onset or adult onset GHD.
2.1 Dosing of Pediatric Patients
General Pediatric Dosing Information
The Omnitrope dosage and administration schedule should be individualized based on the growth response of each patient.
Response to somatropin therapy in pediatric patients tends to decrease with time. However, in pediatric patients, the failure to increase growth rate, particularly during the first year of therapy, indicates the need for close assessment of compliance and evaluation for other causes of growth failure, such as hypothyroidism, undernutrition, advanced bone age and antibodies to recombinant human GH (rhGH).
Treatment with Omnitrope for short stature should be discontinued when the epiphyses are fused.
Pediatric Growth Hormone Deficiency (GHD)
Generally, a dosage of 0.16 to 0.24 mg/kg body weight /week is recommended. The weekly dose should be divided over 6 or 7 days of subcutaneous injections.
Prader-Willi Syndrome (PWS)
Generally, a dosage of 0.24 mg/kg body weight/week is recommended. The weekly dose should be divided over 6 or 7 days of subcutaneous injections.
Small for Gestational Age (SGA)
Generally, a dosage of up to 0.48 mg/kg body weight/week is recommended. The weekly dose should be divided over 6 or 7 days of subcutaneous injections.
2.2 Dosing of Adult Patients
Adult Growth Hormone Deficiency (GHD)
Based on the weight-based dosing utilized in clinical studies with another somatropin product, the recommended dosage at the start of therapy is not more than 0.04 mg/kg/week given as a daily subcutaneous injection. The dose may be increased at 4- to 8-week intervals according to individual patient requirements to not more than 0.08 mg/kg/week. Clinical response, side effects, and determination of age- and gender-adjusted serum IGF-I levels may be used as guidance in dose titration.
Alternatively, taking into account recent literature, a starting dose of approximately 0.2 mg/day (range, 0.15-0.30 mg/day) may be used without consideration of body weight. This dose can be increased gradually every 1-2 months by increments of approximately 0.1 to 0.2 mg/day, according to individual patient requirements based on the clinical response and serum IGF-I concentrations. During therapy, the dose should be decreased if required by the occurrence of adverse events and/or serum IGF-I levels above the age- and gender-specific normal range. Maintenance dosages vary considerably from person to person.
A lower starting dose and smaller dose increments should be considered for older patients, who are more prone to the adverse effects of somatropin than younger individuals. In addition, obese individuals are more likely to manifest adverse effects when treated with a weight-based regimen. In order to reach the defined treatment goal, estrogen-replete women may need higher doses than men. Oral estrogen administration may increase the dose requirements in women.
2.3 Preparation and Administration
Omnitrope Cartridge 5 mg/1.5 mL and Cartridge 10 mg/1.5 mL
Each cartridge of Omnitrope must be inserted into its corresponding Omnitrope Pen 5 or Omnitrope Pen 10 delivery system. Instructions for delivering the dosage are provided in the Omnitrope INSTRUCTIONS FOR USE booklet enclosed with the Omnitrope drug and the Omnitrope Pens.
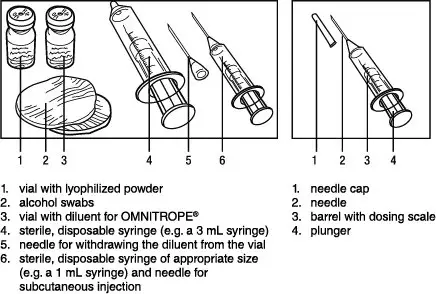
Omnitrope for injection 5.8 mg/vial
Instructions for delivering the dosage are provided in the INSTRUCTIONS FOR USE leaflets enclosed with the Omnitrope drug.
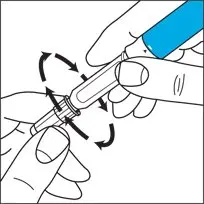
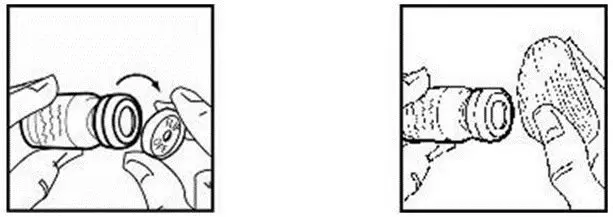
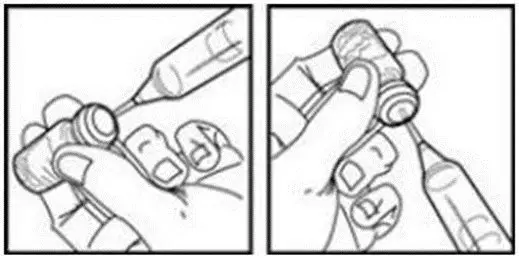
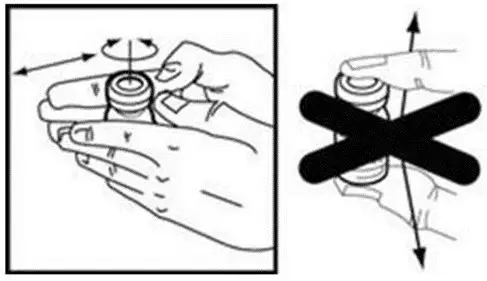
Once the diluent is added to the lyophilized powder, swirl gently; do not shake. Shaking may cause denaturation of the active ingredient.
Parenteral drug products should always be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Omnitrope MUST NOT BE INJECTED if the solution is cloudy or contains particulate matter. Use it only if it is clear and colorless. Omnitrope must be refrigerated at 2° to 8°C (36° to 46°F).
Patients and caregivers who will administer Omnitrope in medically unsupervised situations should receive appropriate training and instruction on the proper use of Omnitrope from the physician or other suitably qualified health professional.
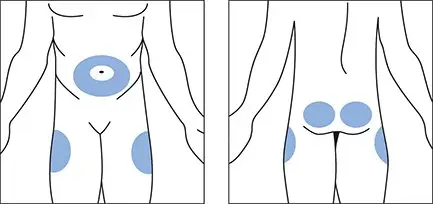
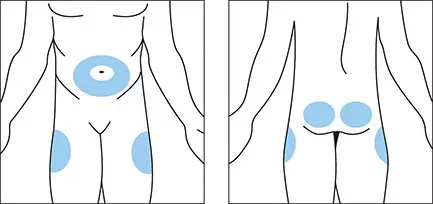
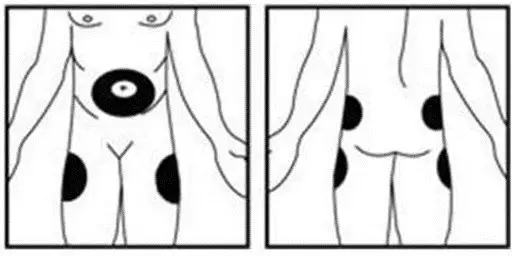
The dosage of Omnitrope must be adjusted for the individual patient. The dose should be given daily by subcutaneous injections (administered preferably in the evening). Omnitrope may be given in the thigh, buttocks, or abdomen.
Injection sites should always be rotated to avoid lipoatrophy.
3. Dosage Forms and Strengths
Omnitrope Cartridges and vials (for injection) are available:
- •
- 5 mg/1.5 mL Cartridge is a prefilled sterile somatropin solution containing benzyl alcohol in a glass cartridge ready to be administered with the Omnitrope Pen 5.
- •
- 10 mg/1.5 mL Cartridge is a prefilled sterile somatropin solution in a glass cartridge ready to be administered with the Omnitrope Pen 10.
- •
- 5.8 mg/vial is supplied with two vials, one containing somatropin as a powder and the other vial containing diluent (Bacteriostatic Water for Injection containing benzyl alcohol as a preservative).
4. Contraindications
- •
- Acute Critical Illness
Treatment with pharmacologic amounts of somatropin is contraindicated in patients with acute critical illness due to complications following open heart surgery, abdominal surgery or multiple accidental trauma, or those with acute respiratory failure [see Warnings and Precautions (5.1)].
- •
- Prader-Willi Syndrome in Children
Somatropin is contraindicated in patients with Prader-Willi Syndrome who are severely obese, have a history of upper airway obstruction or sleep apnea, or have severe respiratory impairment. There have been reports of sudden death when somatropin was used in such patients [see Warnings and Precautions (5.2)].
- •
- Active Malignancy
In general, somatropin is contraindicated in the presence of active malignancy. Any preexisting malignancy should be inactive and its treatment complete prior to instituting therapy with somatropin. Somatropin should be discontinued if there is evidence of recurrent activity. Since GHD may be an early sign of the presence of a pituitary tumor (or, rarely, other brain tumors), the presence of such tumors should be ruled out prior to initiation of treatment. Somatropin should not be used in patients with any evidence of progression or recurrence of an underlying intracranial tumor [see Warnings and Precautions (5.3)].
- •
- Hypersensitivity
Omnitrope is contraindicated in patients with a known hypersensitivity to somatropin or any of its excipients. Systemic hypersensitivity reactions have been reported with postmarketing use of somatropin products [see Warnings and Precautions (5.6)].
- •
- Diabetic Retinopathy
Somatropin is contraindicated in patients with active proliferative or severe non-proliferative diabetic retinopathy.
- •
- Closed Epiphyses
Somatropin should not be used for growth promotion in pediatric patients with closed epiphyses.
5. Warnings and Precautions
5.1 Acute Critical Illness
Increased mortality in patients with acute critical illness due to complications following open heart surgery, abdominal surgery or multiple accidental trauma, or those with acute respiratory failure has been reported after treatment with pharmacologic amounts of somatropin [see Contraindications (4)]. Two placebo-controlled clinical trials in non-growth hormone deficient adult patients (n=522) with these conditions in intensive care units revealed a significant increase in mortality (42% vs. 19%) among somatropin-treated patients (doses 5.3-8 mg/day) compared to those receiving placebo. The safety of continuing somatropin treatment in patients receiving replacement doses for approved indications who concurrently develop these illnesses has not been established. Therefore, the potential benefit of treatment continuation with somatropin in patients experiencing acute critical illnesses should be weighed against the potential risk.
5.2 Prader-Willi Syndrome in Children
There have been reports of fatalities after initiating therapy with somatropin in pediatric patients with Prader-Willi Syndrome who had one or more of the following risk factors: severe obesity, history of upper airway obstruction or sleep apnea, or unidentified respiratory infection. Male patients with one or more of these factors may be at greater risk than females. Patients with Prader-Willi Syndrome should be evaluated for signs of upper airway obstruction (including onset of or increased snoring) and sleep apnea before initiation of treatment with somatropin. If, during treatment with somatropin, patients show signs of upper airway obstruction (including onset of or increased snoring) and/or new onset sleep apnea, treatment should be interrupted. All patients with Prader-Willi Syndrome treated with somatropin should also have effective weight control and be monitored for signs of respiratory infection, which should be diagnosed as early as possible and treated aggressively [see Contraindications (4)].
5.3 Neoplasms
In childhood cancer survivors who were treated with radiation to the brain/head for their first neoplasm and who developed subsequent GHD and were treated with somatropin, an increased risk of a second neoplasm has been reported. Intracranial tumors, in particular meningiomas, were the most common of these second neoplasms. In adults, it is unknown whether there is any relationship between somatropin replacement therapy and CNS tumor recurrence [see Contraindications (4)]. Monitor all patients with a history of GHD secondary to an intracranial neoplasm routinely while on somatropin therapy for progression or recurrence of the tumor [see Contraindications (4)].
Because children with certain rare genetic causes of short stature have an increased risk of developing malignancies, practitioners should thoroughly consider the risks and benefits of starting somatropin in these patients. If treatment with somatropin is initiated, these patients should be carefully monitored for development of neoplasms.
Monitor patients on somatropin therapy carefully for increased growth, or potential malignant changes, of preexisting nevi.
5.4 Impaired Glucose Tolerance and Diabetes Mellitus
Treatment with somatropin may decrease insulin sensitivity, particularly at higher doses in susceptible patients. As a result, previously undiagnosed impaired glucose tolerance and overt diabetes mellitus may be unmasked, and new onset type 2 diabetes mellitus has been reported in patients taking somatropin. Therefore, glucose levels should be monitored periodically in all patients treated with somatropin, especially in those with risk factors for diabetes mellitus, such as obesity, Turner Syndrome, or a family history of diabetes mellitus. Patients with preexisting type 1 or type 2 diabetes mellitus or impaired glucose tolerance should be monitored closely during somatropin therapy. The doses of antihyperglycemic drugs (i.e., insulin or oral agents) may require adjustment when somatropin therapy is instituted in these patients. [See Drug Interactions (7.5)]
5.5 Intracranial Hypertension (IH)
Intracranial hypertension (IH) with papilledema, visual changes, headache, nausea, and/or vomiting has been reported in a small number of patients treated with somatropin products. Symptoms usually occurred within the first eight (8) weeks after the initiation of somatropin therapy. In all reported cases, IH-associated signs and symptoms rapidly resolved after cessation of therapy or a reduction of the somatropin dose.
Funduscopic examination should be performed routinely before initiating treatment with somatropin to exclude preexisting papilledema, and periodically during the course of somatropin therapy. If papilledema is observed by funduscopy during somatropin treatment, treatment should be stopped. If somatropin-induced IH is diagnosed, treatment with somatropin can be restarted at a lower dose after IH-associated signs and symptoms have resolved. Patients with Turner syndrome and Prader-Willi Syndrome may be at increased risk for the development of IH.
5.6 Hypersensitivity
Serious systemic hypersensitivity reactions including anaphylactic reactions and angioedema have been reported with postmarketing use of somatropin products. Patients and caregivers should be informed that such reactions are possible and that prompt medical attention should be sought if an allergic reaction occurs [see Contraindications (4)].
5.7 Fluid Retention
Fluid retention during somatropin replacement therapy in adults may frequently occur. Clinical manifestations of fluid retention (e.g. edema, arthralgia, myalgia, nerve compression syndromes including carpal tunnel syndrome/paraesthesias) are usually transient and dose dependent.
5.8 Hypoadrenalism
Patients receiving somatropin therapy who have or are at risk for pituitary hormone deficiency(s) may be at risk for reduced serum cortisol levels and/or unmasking of central (secondary) hypoadrenalism. In addition, patients treated with glucocorticoid replacement for previously diagnosed hypoadrenalism may require an increase in their maintenance or stress doses following initiation of somatropin treatment [see Section 7.1, 11-β Hydroxysteroid Dehydrogenase Type 1].
5.9 Hypothyroidism
Undiagnosed/untreated hypothyroidism may prevent an optimal response to somatropin, in particular, the growth response in children. Patients with Turner syndrome have an inherently increased risk of developing autoimmune thyroid disease and primary hypothyroidism and should have their thyroid function checked prior to initiation of somatropin therapy. In patients with GHD, central (secondary) hypothyroidism may first become evident or worsen during somatropin treatment. Therefore, patients treated with somatropin should have periodic thyroid function tests and thyroid hormone replacement therapy should be initiated or appropriately adjusted when indicated.
5.10 Slipped Capital Femoral Epiphysis in Pediatric Patients
Slipped capital femoral epiphysis may occur more frequently in patients with endocrine disorders (including GHD and Turner syndrome) or in patients undergoing rapid growth. Any pediatric patient with the onset of a limp or complaints of hip or knee pain during somatropin therapy should be carefully evaluated.
5.11 Progression of Preexisting Scoliosis in Pediatric Patients
Progression of scoliosis can occur in patients who experience rapid growth. Because somatropin increases growth rate, patients with a history of scoliosis who are treated with somatropin should be monitored for progression of scoliosis. However, somatropin has not been shown to increase the occurrence of scoliosis. Skeletal abnormalities including scoliosis are commonly seen in untreated Turner syndrome patients. Scoliosis is also commonly seen in untreated patients with Prader-Willi Syndrome. Physicians should be alert to these abnormalities, which may manifest during somatropin therapy.
5.12 Confirmation of Childhood Onset Adult GHD
Patients with epiphyseal closure who were treated with somatropin replacement therapy in childhood should be reevaluated according to the criteria in Indications and Usage (1.2) before continuation of somatropin therapy at the reduced dose level recommended for GH deficient adults.
5.13 Otitis Media and Cardiovascular Disorders in Turner Syndrome
Patients with Turner syndrome should be evaluated carefully for otitis media and other ear disorders since these patients have an increased risk of ear and hearing disorders. Somatropin treatment may increase the occurrence of otitis media in patients with Turner syndrome. In addition, patients with Turner syndrome should be monitored closely for cardiovascular disorders (e.g., stroke, aortic aneurysm/dissection, hypertension) as these patients are also at risk for these conditions.
5.14 Lipoatrophy
When somatropin is administered subcutaneously at the same site over a long period of time, tissue atrophy may result. This can be avoided by rotating the injection site [see Dosage and Administration (2.3)].
5.15 Laboratory Tests
Serum levels of inorganic phosphorus, alkaline phosphatase, parathyroid hormone (PTH) and IGF-I may increase after somatropin therapy.
5.16 Pancreatitis
Cases of pancreatitis have been reported rarely in children and adults receiving somatropin treatment, with some evidence supporting a greater risk in children compared with adults. Published literature indicates that girls who have Turner syndrome may be at greater risk than other somatropin-treated children. Pancreatitis should be considered in any somatropin treated patient, especially a child, who develops persistent severe abdominal pain.
5.17 Benzyl Alcohol
Benzyl alcohol, a component of Omnitrope Cartridge 5 mg/1.5 mL and the diluent for Omnitrope for injection 5.8 mg/vial, has been associated with serious adverse events and death, particularly in pediatric patients. The “gasping syndrome,” (characterized by central nervous system depression, metabolic acidosis, gasping respirations, and high levels of benzyl alcohol and its metabolites found in the blood and urine) has been associated with benzyl alcohol dosages >99 mg/kg/day in neonates and low-birth weight neonates. Additional symptoms may include gradual neurological deterioration, seizures, intracranial hemorrhage, hematologic abnormalities, skin breakdown, hepatic and renal failure, hypotension, bradycardia, and cardiovascular collapse. Practitioners administering this and other medications containing benzyl alcohol should consider the combined daily metabolic load of benzyl alcohol from all sources.
6. Adverse Reactions/Side Effects
The following important adverse reactions area also described elsewhere in labeling:
- •
- Increased mortality in patients with acute critical illness [see Warnings and Precautions (5.1)]
- •
- Fatalities in children with Prader-Willi Syndrome [see Warnings and Precautions (5.2)]
- •
- Neoplasms [see Warnings and Precautions (5.3)]
- •
- aGlucose intolerance and diabetes mellitus [Warnings and Precautions (5.4)]
- •
- Intracranial hypertension [see Warnings and Precautions (5.5)]
- •
- Severe hypersensitivity [see Warnings and Precautions (5.6)]
- •
- Fluid retention [see Warnings and Precautions (5.7)]
- •
- Hypoadrenalism [see Warnings and Precautions (5.8)]
- •
- Hypothyroidism [see Warnings and Precautions (5.9)]
- •
- Slipped capital femoral epiphysis in pediatric patients [see Warnings and Precautions (5.10)]
- •
- Progression of preexisting scoliosis in pediatric patients [see Warnings and Precautions (5.11)]
- •
- Otitis media and cardiovascular disorders in patients with Turner syndrome [see Warnings and Precautions (5.13)]
- •
- Lipoatrophy [see Warnings and Precautions (5.14)]
- •
- Pancreatitis [see Warnings and Precautions (5.16)]
- •
- Benzyl Alcohol [see Warnings and Precautions (5.17)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under varying conditions, adverse reaction rates observed during the clinical trials performed with one somatropin formulation cannot always be directly compared to the rates observed during the clinical trials performed with a second somatropin formulation, and may not reflect the adverse reaction rates observed in practice.
Clinical Trials in Pediatric GHD Patients
The following events were observed during clinical studies with Omnitrope Cartridge conducted in children with GHD:
| Adverse Event | n (%) |
|---|---|
| N=number of patients receiving treatment n=number of patients who reported the event during study period %=percentage of patients who reported the event during study period |
|
|
Elevated HbA1c |
12 (14%) |
|
Eosinophilia |
10 (12%) |
|
Hematoma |
8 (9%) |
The following events were observed during clinical studies with Omnitrope for injection conducted in children with GHD:
| Adverse Event | n (%) | ||
|---|---|---|---|
| N=number of patients receiving treatment n=number of patients who reported the event during study period %= percentage of patients who reported the event during study period |
|||
|
Hypothyroidism |
7 (16%) |
||
|
Eosinophilia |
5 (11%) |
||
|
Elevated HbA1c |
4 (9%) |
||
|
Hematoma |
4 (9%) |
||
|
Headache |
3 (7%) |
||
|
Hypertriglyceridemia |
2 (5%) |
||
|
Leg Pain |
2 (5%) |
||
Clinical Trials in PWS
In two clinical studies in pediatric patients with Prader-Willi Syndrome carried out with another somatropin product, the following drug-related events were reported: edema, aggressiveness, arthralgia, benign intracranial hypertension, hair loss, headache, and myalgia.
Clinical Trials in Children with SGA
In clinical studies of 273 pediatric patients born small for gestational age treated with another somatropin product, the following clinically significant events were reported: mild transient hyperglycemia, one patient with benign intracranial hypertension, two patients with central precocious puberty, two patients with jaw prominence, and several patients with aggravation of preexisting scoliosis, injection site reactions, and self-limited progression of pigmented nevi.
Clinical Trials in Children with Idiopathic Short Stature
In two open-label clinical studies conducted with another somatropin product in pediatric patients with ISS, the most commonly encountered adverse events were upper respiratory tract infections, influenza, tonsillitis, nasopharyngitis, gastroenteritis, headaches, increased appetite, pyrexia, fracture, altered mood, and arthralgia. In one of the two studies during treatment with this other somatropin product, the mean IGF-1 standard deviation (SD) scores were maintained in the normal range. IGF-1 SD scores above +2 SD were observed as follows: 1 subject (3%), 10 subjects (30%) and 16 subjects (38%) in the untreated control, 0.23 and the 0.47 mg/kg/week groups respectively, had at least one measurement; while 0 subjects (0%), 2 subjects (7%) and 6 subjects (14%) had two or more consecutive IGF-1 measurements above +2 SD.
Clinical Trials in Children with Turner Syndrome
In two clinical studies with another somatropin product in pediatric patients with Turner syndrome, the most frequently reported adverse events were respiratory illnesses (influenza, tonsillitis, otitis, sinusitis), joint pain, and urinary tract infection. The only treatment-related adverse event that occurred in more than 1 patient was joint pain.
Clinical Trials in Adults with GHD
In clinical trials with another somatropin product in 1,145 GHD adults, the majority of the adverse events consisted of mild to moderate symptoms of fluid retention, including peripheral swelling, arthralgia, pain and stiffness of the extremities, peripheral edema, myalgia, paresthesia, and hypoesthesia. These events were reported early during therapy, and tended to be transient and/or responsive to dosage reduction.
Table 3 displays the adverse events reported by 5% or more of adult GHD patients in clinical trials after various durations of treatment with another somatropin product. Also presented are the corresponding incidence rates of these adverse events in placebo patients during the 6-month double-blind portion of the clinical trials.
|
Double Blind Phase | Open Label Phase
Another Somatropin Product |
||||
|---|---|---|---|---|---|
|
Adverse Event |
Placebo 0–6 mo. (n = 572) % Patients | Another
Somatropin Product 0–6 mo. (n = 573) % Patients |
6–12 mo. (n = 504) % Patients |
12–18 mo. (n = 63) % Patients |
18–24 mo. (n = 60) % Patients |
| n=number of patients receiving treatment during the indicated period %=percentage of patients who reported the event during the indicated period |
|||||
|
|||||
|
Swelling, peripheral |
5.1 |
17.5* |
5.6 |
0 |
1.7 |
|
Arthralgia |
4.2 |
17.3* |
6.9 |
6.3 |
3.3 |
|
Upper respiratory infection |
14.5 |
15.5 |
13.1 |
15.9 |
13.3 |
|
Pain, extremities |
5.9 |
14.7* |
6.7 |
1.6 |
3.3 |
|
Edema, peripheral |
2.6 |
10.8* |
3.0 |
0 |
0 |
|
Paresthesia |
1.9 |
9.6* |
2.2 |
3.2 |
0 |
|
Headache |
7.7 |
9.9 |
6.2 |
0 |
0 |
|
Stiffness of extremities |
1.6 |
7.9* |
2.4 |
1.6 |
0 |
|
Fatigue |
3.8 |
5.8 |
4.6 |
6.3 |
1.7 |
|
Myalgia |
1.6 |
4.9* |
2.0 |
4.8 |
6.7 |
|
Back pain |
4.4 |
2.8 |
3.4 |
4.8 |
5.0 |
Post-Trial Extension Studies in Adults
In expanded post-trial extension studies, diabetes mellitus developed in 12 of 3,031 patients (0.4%) during treatment with another somatropin product. All 12 patients had predisposing factors, e.g., elevated glycated hemoglobin levels and/or marked obesity, prior to receiving this other somatropin product. Of the 3,031 patients receiving this other somatropin product, 61 (2%) developed symptoms of carpal tunnel syndrome, which lessened after dosage reduction or treatment interruption (52) or surgery (9). Other adverse events that have been reported include generalized edema and hypoesthesia.
As with all therapeutic proteins, there is potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to Omnitrope with the incidence of antibodies to other products may be misleading. In the case of growth hormone, antibodies with binding capacities lower than 2 mg/mL have not been associated with growth attenuation. In a very small number of patients treated with somatropin, when binding capacity was greater than 2 mg/mL, interference with the growth response was observed.
6.2 Post-Marketing Experience
Because these adverse events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The adverse events reported during post-marketing surveillance do not differ from those listed/discussed above in Sections 6.1 and 6.2 in children and adults.
Serious systemic hypersensitivity reactions including anaphylactic reactions and angioedema have been reported with postmarketing use of somatropin products [see Warnings and Precautions (5.6)].
Leukemia has been reported in a small number of GH deficient children treated with somatropin, somatrem (methionylated rhGH) and GH of pituitary origin. It is uncertain whether these cases of leukemia are related to GH therapy, the pathology of GHD itself, or other associated treatments such as radiation therapy. On the basis of current evidence, experts have not been able to conclude that GH therapy per se was responsible for these cases of leukemia. The risk for children with GHD, if any, remains to be established [see Contraindications (4) and Warnings and Precautions (5.3)].
The following additional adverse reactions have been observed during the use of somatropin: headaches (children and adults), gynecomastia (children), and pancreatitis (children and adults) [see Warnings and Precautions (5.16)].
New-onset type 2 diabetes mellitus has been reported.
7. Drug Interactions
7.1 11β-Hydroxysteroid Dehydrogenase Type 1 (11βHSD-1)
The microsomal enzyme 11β-hydroxysteroid dehydrogenase type 1 (11βHSD-1) is required for conversion of cortisone to its active metabolite, cortisol, in hepatic and adipose tissue. GH and somatropin inhibit 11βHSD-1. Consequently, individuals with untreated GH deficiency have relative increases in 11βHSD-1 and serum cortisol. Introduction of somatropin treatment may result in inhibition of 11βHSD-1 and reduced serum cortisol concentrations. As a consequence, previously undiagnosed central (secondary) hypoadrenalism may be unmasked and glucocorticoid replacement may be required in patients treated with somatropin. In addition, patients treated with glucocorticoid replacement for previously diagnosed hypoadrenalism may require an increase in their maintenance or stress doses following initiation of somatropin treatment; this may be especially true for patients treated with cortisone acetate and prednisone since conversion of these drugs to their biologically active metabolites is dependent on the activity of 11βHSD-1 [see Warnings and Precautions(5.8)].
7.2 Pharmacologic Glucocorticoid Therapy and Supraphysiologic Glucocorticoid Treatment
Pharmacologic glucocorticoid therapy and supraphysiologic glucocorticoid treatment may attenuate the growth promoting effects of somatropin in children. Therefore, glucocorticoid replacement dosing should be carefully adjusted in children receiving concomitant somatropin and glucocorticoid treatments to avoid both hypoadrenalism and an inhibitory effect on growth.
7.3 Cytochrome P450-Metabolized Drugs
Limited published data indicate that somatropin treatment increases cytochrome P450 (CYP450)-mediated antipyrine clearance in man. These data suggest that somatropin administration may alter the clearance of compounds known to be metabolized by CYP450 liver enzymes (e.g., corticosteroids, sex steroids, anticonvulsants, cyclosporine). Careful monitoring is advisable when somatropin is administered in combination with other drugs known to be metabolized by CYP450 liver enzymes. However, formal drug interaction studies have not been conducted.
8. Use In Specific Populations
8.1 Pregnancy
Pregnancy Category B
Animal reproduction studies have not been conducted with Omnitrope. It is not known whether Omnitrope can cause fetal harm when administered to a pregnant woman or can affect reproductive capacity.
Reproduction studies carried out with another somatropin product at doses of 0.3, 1, and 3.3 mg/kg/day administered subcutaneously in the rat and 0.08, 0.3, and 1.3 mg/kg/day administered intramuscularly in the rabbit (highest doses approximately 24 times and 19 times the recommended human therapeutic levels, respectively, based on body surface area) resulted in decreased maternal body weight gains but were not teratogenic. In rats receiving subcutaneous doses during gametogenesis and up to 7 days of pregnancy, 3.3 mg/kg/day (approximately 24 times human dose) produced anestrus or extended estrus cycles in females and fewer and less motile sperm in males. When given to pregnant female rats (days 1 to 7 of gestation) at 3.3 mg/kg/day a very slight increase in fetal deaths was observed. At 1 mg/kg/day (approximately seven times human dose) rats showed slightly extended estrus cycles, whereas at 0.3 mg/kg/day no effects were noted.
In perinatal and postnatal studies in rats, doses of 0.3, 1, and 3.3 mg/kg/day of this other somatropin product produced growth-promoting effects in the dams but not in the fetuses. Young rats at the highest dose showed increased weight gain during suckling but the effect was not apparent by 10 weeks of age. No adverse effects were observed on gestation, morphogenesis, parturition, lactation, postnatal development, or reproductive capacity of the offspring due to this other somatropin product. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
8.3 Nursing Mothers
It is not known whether Omnitrope is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Omnitrope is administered to a nursing woman.
8.5 Geriatric Use
The safety and effectiveness of Omnitrope in patients aged 65 and over have not been evaluated in clinical studies. Elderly patients may be more sensitive to the action of somatropin, and therefore may be more prone to develop adverse reactions. A lower starting dose and smaller dose increments should be considered for older patients [see Dosage and Administration (2.2)].
10. Overdosage
11. Omnitrope Description
Omnitrope (somatropin) is a polypeptide hormone of recombinant DNA origin. It has 191 amino acid residues and a molecular weight of 22,125 daltons. The amino acid sequence of the product is identical to that of human growth hormone of pituitary origin (somatropin). Omnitrope is synthesized in a strain of Escherichia coli that has been modified by the addition of the gene for human growth hormone. Omnitrope Cartridge is a clear, colorless, sterile solution for subcutaneous injection. Omnitrope for Injection is a lyophilized powder that is reconstituted for subcutaneous injection.
Figure 1. Schematic amino acid sequence of human growth hormone including the disulfide bonds
Each Omnitrope Cartridge or vial contains the following (see Table 4):
|
|
|
|
For
|
|
Component | |||
|
Somatropin |
5 mg |
10 mg |
5.8 mg |
|
Disodium hydrogen |
1.15 mg |
1.34 mg |
1.88 mg |
|
Sodium dihydrogen |
1.67 mg |
1.56 mg |
0.68 mg |
|
Poloxamer 188 |
3.0 mg |
3.0 mg |
- |
|
Mannitol |
52.5 mg |
- |
- |
|
Glycine |
- |
27.75 mg |
27.6 mg |
|
Benzyl alcohol |
13.5 mg |
- |
- |
|
Phenol |
- |
4.50 mg |
- |
|
Water for Injection |
to make |
to make |
- |
|
Diluent (vials only) |
Bacteriostatic
|
||
|
Water for injection |
to make |
||
|
Benzyl alcohol |
17 mg |
12. Omnitrope - Clinical Pharmacology
12.1 Mechanism of Action
Somatropin (as well as endogenous GH) binds to a dimeric GH receptor in the cell membrane of target cells resulting in intracellular signal transduction and a host of pharmacodynamic effects. Some of these pharmacodynamic effects are primarily mediated by IGF-1 produced in the liver and also locally (e.g., skeletal growth, protein synthesis), while others are primarily a consequence of the direct effects of somatropin (e.g., lipolysis) [see Pharmacodynamics (12.2)].
12.2 Pharmacodynamics
Tissue Growth
The primary and most intensively studied action of somatropin is the stimulation of linear growth. This effect is demonstrated in children with GHD and children who have PWS, were born SGA, have TS or have ISS.
Skeletal Growth
The measurable increase in bone length after administration of somatropin results from its effect on the cartilaginous growth areas of long bones. Studies in vitro have shown that the incorporation of sulfate into proteoglycans is not due to a direct effect of somatropin, but rather is mediated by the somatomedins or insulin-like growth factors (IGFs). The somatomedins, among them IGF-1, are polypeptide hormones which are synthesized in the liver, kidney, and various other tissues. IGF-1 levels are low in the serum of hypopituitary dwarfs and hypophysectomized humans or animals, and increase after treatment with somatropin.
Cell Growth
It has been shown that the total number of skeletal muscle cells is markedly decreased in children with short stature lacking endogenous GH compared with normal children, and that treatment with somatropin results in an increase in both the number and size of muscle cells.
Organ Growth
Somatropin influences the size of internal organs, and it also increases red cell mass.
Protein Metabolism
Linear growth is facilitated in part by increased cellular protein synthesis. This synthesis and growth are reflected by nitrogen retention which can be quantitated by observing the decline in urinary nitrogen excretion and blood urea nitrogen following the initiation of somatropin therapy.
Carbohydrate Metabolism
Hypopituitary children sometimes experience fasting hypoglycemia that may be improved by treatment with somatropin. In healthy subjects, large doses of somatropin may impair glucose tolerance. Although the precise mechanism of the diabetogenic effect of somatropin is not known, it is attributed to blocking the action of insulin rather than blocking insulin secretion. Insulin levels in serum actually increase as somatropin levels increase. Administration of human growth hormone to normal adults and patients with growth hormone deficiency results in increases in mean serum fasting and postprandial insulin levels, although mean values remain in the normal range. In addition, mean fasting and postprandial glucose and hemoglobin A1C levels remain in the normal range.
Lipid Metabolism
Somatropin stimulates intracellular lipolysis, and administration of somatropin leads to an increase in plasma free fatty acids and triglycerides. Untreated GHD is associated with increased body fat stores, including increased abdominal visceral and subcutaneous adipose tissue. Treatment of growth hormone deficient patients with somatropin results in a general reduction of fat stores, and decreased serum levels of low density lipoprotein (LDL) cholesterol.
Mineral Metabolism
Administration of somatropin results in an increase in total body potassium and phosphorus and to a lesser extent sodium. This retention is thought to be the result of cell growth. Serum levels of phosphate increase in children with GHD after somatropin therapy due to metabolic activity associated with bone growth. Serum calcium levels are not altered. Although calcium excretion in the urine is increased, there is a simultaneous increase in calcium absorption from the intestine. Negative calcium balance, however, may occasionally occur during somatropin treatment.
12.3 Pharmacokinetics
There are no pharmacokinetic studies using Omnitrope Cartridges in patients with growth hormone deficiency.
Absorption
Following a subcutaneous injection of single dose of 5 mg Omnitrope 5 mg/1.5 mL Cartridge or 5 mg Omnitrope 10 mg/1.5 mL Cartridge in healthy male and female adults, the peak concentration (Cmax) was 72-74 mcg/L. The time to reach Cmax (tmax) for Omnitrope was 4.0 hours.
The aqueous formulations of 5 mg/1.5 mL Omnitrope cartridge and 10 mg/mL Omnitrope cartridge are bioequivalent to the lyophilized 5.8 mg/vial Omnitrope formulation.
Metabolism
Somatropin is metabolized in both the liver and kidneys by proteolytic degradation. In renal cells, at least a portion of the breakdown products are returned to the systemic circulation.
Excretion
The mean terminal half-life of somatropin after subcutaneous administration of Omnitrope Cartridge in healthy adults is 2.5-2.8 hours. The mean clearance of subcutaneously administered Omnitrope Cartridge in healthy adults was about 0.14 L/hr·kg.
Specific Populations
Pediatric: No pharmacokinetic studies of Omnitrope have been conducted in pediatric patients.
Gender: The effect of gender on pharmacokinetics of Omnitrope has not been evaluated in pediatric patients.
Race: No studies have been conducted with Omnitrope to assess pharmacokinetic differences among races.
Renal or hepatic impairment: No pharmacokinetic studies have been conducted with Omnitrope in patients with renal or hepatic impairment.
14. Clinical Studies
14.1 Pediatric Growth Hormone Deficiency (GHD)
The efficacy and safety of Omnitrope were compared with another somatropin product approved for growth hormone deficiency (GHD) in pediatric patients. In sequential clinical trials involving a total of 89 GHD children, 44 patients received Omnitrope for Injection (lyophilized powder) 5.8 mg/vial and 45 patients received the comparator somatropin product for 9 months. After 9 months of treatment patients who had received the comparator somatropin product were switched to Omnitrope Cartridge (liquid) 5 mg/1.5 mL. After 15 months of treatment, all patients were switched to Omnitrope Cartridge to collect long-term efficacy and safety data.
In both groups, somatropin was administered as a daily subcutaneous injection at a dose of 0.03 mg/kg. Similar effects on growth were observed between Omnitrope for Injection and the comparator somatropin product during the initial 9 months of treatment.
The efficacy results after 9 months of treatment (Omnitrope for Injection vs. the comparator somatropin product) and after 15 months (Omnitrope Cartridge) are summarized in Table 5.
|
||
|
|
Treatment
|
Treatment
|
|
0 - 9 months |
Omnitrope
|
Another Somatropin
(n=45) |
|
9 - 15 months |
Omnitrope
|
Omnitrope |
|
Treatment Parameter |
Mean (SD) |
Mean (SD) |
|
Height velocity (cm/yr) | ||
|
Pre-treatment |
3.8 (1.2) |
4.0 (0.8) |
|
Month 9 |
10.7 ( 2.6) |
10.7 (2.9) |
|
Month 15 |
8.5 (1.8) |
8.6 (2.0) |
|
Height velocity SDS | ||
|
Pre-treatment |
-2.4 (1.3) |
-2.3 (1.1) |
|
Month 9 |
6.1 (3.7) |
5.4 (3.2) |
|
Month 15 |
3.4 (2.6) |
3.2 (2.9) |
|
Height SDS | ||
|
Pre-treatment |
-3.0 (0.7) |
-3.1 (0.9) |
|
Month 9 |
-2.3 (0.7) |
-2.5 (0.7) |
|
Month 15 |
-2.0 (0.7) |
-2.2 (0.7) |
|
IGF-1* | ||
|
Pre-treatment |
159 (92) |
158 (43) |
|
Month 9 |
291 (174) |
302 (183) |
|
Month 15 |
300 (225) |
323 (189) |
|
IGFBP-3* | ||
|
Pre-treatment |
3.5 (1.3) |
3.5 (1.0) |
|
Month 9 |
4.6 (3.0) |
4.0 (1.5) |
|
Month 15 |
4.6 (1.3) |
4.9 (1.4) |
14.2 Adult Growth Hormone Deficiency (GHD)
Another somatropin product was compared with placebo in six randomized clinical trials involving a total of 172 adult GHD patients. These trials included a 6-month double-blind treatment period, during which 85 patients received this other somatropin product and 87 patients received placebo, followed by an open-label treatment period in which participating patients received this other somatropin product for up to a total of 24 months. This other somatropin product was administered as a daily SC injection at a dose of 0.04 mg/kg/week for the first month of treatment and 0.08 mg/kg/week for subsequent months.
Beneficial changes in body composition were observed at the end of the 6-month treatment period for the patients receiving this other somatropin product as compared with the placebo patients. Lean body mass, total body water, and lean/fat ratio increased while total body fat mass and waist circumference decreased. These effects on body composition were maintained when treatment was continued beyond 6 months. Bone mineral density declined after 6 months of treatment but returned to baseline values after 12 months of treatment.
14.3 Prader-Willi Syndrome (PWS)
The safety and efficacy of another somatropin product in the treatment of pediatric patients with Prader-Willi Syndrome (PWS) were evaluated in two randomized, open-label, controlled clinical trials. Patients received either this other somatropin product or no treatment for the first year of the studies, while all patients received this other somatropin product during the second year. This other somatropin product was administered as a daily SC injection, and the dose was calculated for each patient every 3 months. In Study 1, the treatment group received this other somatropin product at a dose of 0.24 mg/kg/week during the entire study. During the second year, the control group received this other somatropin product at a dose of 0.48 mg/kg/week. In Study 2, the treatment group received this other somatropin product at a dose of 0.36 mg/kg/week during the entire study. During the second year, the control group received this other somatropin product at a dose of 0.36 mg/kg/week.
Patients who received this other somatropin product showed significant increases in linear growth during the first year of study, compared with patients who received no treatment (see Table 6). Linear growth continued to increase in the second year, when both groups received treatment with this other somatropin product.
| Study 1 | Study 2 | |||
|---|---|---|---|---|
| Another
Somatropin Product (0.24 mg/kg/week) (n=15) |
Untreated Control (n=12) | Another
Somatropin Product (0.36 mg/kg/week) (n=7) |
Untreated Control (n=9) |
|
|
||||
|
Linear growth (cm)
|
112.7 ± 14.9 |
109.5 ± 12.0 |
120.3 ± 17.5 |
120.5 ± 11.2 |
|
Growth from months 0 to 12 |
11.6* ± 2.3 |
5.0 ± 1.2 |
10.7* ± 2.3 |
4.3 ± 1.5 |
|
Baseline SDS |
-1.6 ± 1.3 |
-1.8 ± 1.5 |
-2.6 ± 1.7 |
-2.1 ± 1.4 |
|
SDS at 12 months |
-0.5† ± 1.3 |
-1.9 ± 1.4 |
-1.4† ± 1.5 |
-2.2 ± 1.4 |
Changes in body composition were also observed in the patients receiving this other somatropin product (see Table 7). These changes included a decrease in the amount of fat mass, and increases in the amount of lean body mass and the ratio of lean-to-fat tissue, while changes in body weight were similar to those seen in patients who received no treatment. Treatment with this other somatropin product did not accelerate bone age, compared with patients who received no treatment.
| Another
Somatropin Product (n=14) |
Untreated Control (n=10) |
|
|---|---|---|
|
||
|
Fat mass (kg)
|
|
|
|
Change from months 0 to 12 |
-0.9* ± 2.2 |
2.3 ± 2.4 |
|
Lean body mass (kg)
|
|
|
|
Change from months 0 to 12 |
4.7* ± 1.9 |
0.7 ± 2.4 |
|
Lean body mass/Fat mass
|
|
|
|
Change from months 0 to 12 |
1.0* ± 1.4 |
-0.1 ± 0.6 |
|
Body weight (kg)†
|
|
|
|
Change from months 0 to 12 |
3.7‡ ± 2.0 |
3.5 ± 1.9 |
14.4 Pediatric Patients Born Small for Gestational Age (SGA) Who Fail to Manifest Catch-up Growth by Age 2
The safety and efficacy of another somatropin product in the treatment of children born small for gestational age (SGA) were evaluated in 4 randomized, open-label, controlled clinical trials. Patients (age range of 2 to 8 years) were observed for 12 months before being randomized to receive either this other somatropin product (two doses per study, most often 0.24 and 0.48 mg/kg/week) as a daily SC injection or no treatment for the first 24 months of the studies. After 24 months in the studies, all patients received this other somatropin product.
Patients who received any dose of this other somatropin product showed significant increases in growth during the first 24 months of study, compared with patients who received no treatment (see Table 8). Children receiving 0.48 mg/kg/week demonstrated a significant improvement in height standard deviation score (SDS) compared with children treated with 0.24 mg/kg/week. Both of these doses resulted in a slower but constant increase in growth between months 24 to 72 (data not shown).
| Another
Somatropin Product (0.24 mg/kg/week) (n=76) | Another
Somatropin Product (0.48 mg/kg/week) (n=93) |
Untreated Control (n=40) |
|
|---|---|---|---|
|
|||
|
Height Standard Deviation Score (SDS) | |||
|
Baseline SDS |
-3.2 ± 0.8 |
-3.4 ± 1.0 |
-3.1 ± 0.9 |
|
SDS at 24 months |
-2.0 ± 0.8 |
-1.7 ± 1.0 |
-2.9 ± 0.9 |
|
Change in SDS from baseline to month 24 |
1.2* ± 0.5 |
1.7*,† ± 0.6 |
0.1 ± 0.3 |
14.5 Idiopathic Short Stature (ISS)
The long-term efficacy and safety of another somatropin product in patients with idiopathic short stature (ISS) were evaluated in one randomized, open-label, clinical trial that enrolled 177 children. Patients were enrolled on the basis of short stature, stimulated GH secretion > 10 ng/mL, and prepubertal status (criteria for idiopathic short stature were retrospectively applied and included 126 patients). All patients were observed for height progression for 12 months and were subsequently randomized to this other somatropin product or observation only and followed to final height. Two somatropin doses were evaluated in this trial: 0.23 mg/kg/week (0.033 mg/kg/day) and 0.47mg/kg/week (0.067 mg/kg/day). Baseline patient characteristics for the ISS patients who remained prepubertal at randomization (n= 105) were: mean (± SD): chronological age 11.4 (1.3) years, height SDS -2.4 (0.4), height velocity SDS -1.1 (0.8), and height velocity 4.4 (0.9) cm/yr, IGF-1 SDS -0.8 (1.4). Patients were treated for a median duration of 5.7 years. Results for final height SDS are displayed by treatment arm in Table 9. Therapy with this other somatropin product improved final height in ISS children relative to untreated controls. The observed mean gain in final height was 9.8 cm for females and 5.0 cm for males for both doses combined compared to untreated control subjects. A height gain of 1 SDS was observed in 10 % of untreated subjects, 50% of subjects receiving 0.23 mg/kg/week and 69% of subjects receiving 0.47 mg/kg/week.
|
Untreated (n=30) | Another
Somatropin Product 0.033 mg/kg/day (n=30) | Another
Somatropin Product 0.067 mg/kg/day (n=42) | Another
Somatropin Product 0.033 vs. Untreated (95% CI) | Another
Somatropin Product 0.067 vs. Untreated (95% CI) |
|
|---|---|---|---|---|---|
| Least square means based on ANCOVA (final height SDS and final height SDS minus baseline predicted height SDS were adjusted for baseline height SDS) | |||||
|
|||||
|
Baseline height |
0.41 |
0.95 (0.75) |
1.36 (0.64) |
+0.53 (0.20, 0.87) |
+0.94 (0.63, 1.26) |
|
Baseline |
0.23 (0.66) |
0.73 (0.63) |
1.05 (0.83) |
+0.60 (0.09, 1.11) |
+0.90 (0.42, 1.39) |
14.6 Turner Syndrome
Two randomized, open-label, clinical trials were conducted that evaluated the efficacy and safety of another somatropin product in Turner syndrome patients with short stature. Turner syndrome patients were treated with this other somatropin product alone or this other somatropin product plus adjunctive hormonal therapy (ethinylestradiol or oxandrolone). A total of 38 patients were treated with this other somatropin product alone in the two studies. In Study 1, 22 patients were treated for 12 months, and in Study 2, 16 patients were treated for 12 months. Patients received this other somatropin product at a dose between 0.13 to 0.33 mg/kg/week.
SDS for height velocity and height are expressed using either the Tanner (Study 1) or Sempé (Study 2) standards for age-matched normal children as well as the Ranke standard (both studies) for age-matched, untreated Turner syndrome patients. As seen in Table 10, height velocity SDS and height SDS values were smaller at baseline and after treatment with this other somatropin product when the normative standards were utilized as opposed to the Turner syndrome standard.
Both studies demonstrated statistically significant increases from baseline in all of the linear growth variables (i.e., mean height velocity, height velocity SDS, and height SDS) after treatment with this other somatropin product (see Table 10). The linear growth response was greater in Study 1 wherein patients were treated with a larger dose of this other somatropin product.
| Another somatropin
product 0.33 mg/kg/week Study 1* n=22 | Another somatropin
product 0.13-0.23 mg/kg/week Study 2† n=16 |
|
|---|---|---|
| SDS = Standard Deviation Score Ranke standard based on age-matched, untreated Turner syndrome patients Tanner*/Sempé† standards based on age-matched normal children p<0.05, for all changes from baseline |
||
|
Height Velocity (cm/yr) | ||
|
Baseline |
4.1 ± 1.5 |
3.9 ± 1.0 |
|
Month 12 |
7.8 ± 1.6 |
6.1 ± 0.9 |
|
Change from baseline (95% CI) |
3.7 (3.0, 4.3) |
2.2 (1.5, 2.9) |
|
Height Velocity SDS | ||
|
Baseline |
-2.3 ± 1.4 |
-1.6 ± 0.6 |
|
Month 12 |
2.2 ± 2.3 |
0.7 ± 1.3 |
|
Change from baseline (95% CI) |
4.6 (3.5, 5.6) |
2.2 (1.4, 3.0) |
|
Height Velocity SDS (Ranke | ||
|
Baseline |
-0.1 ± 1.2 |
-0.4 ± 0.6 |
|
Month 12 |
4.2 ± 1.2 |
2.3 ± 1.2 |
|
Change from baseline (95% CI) |
4.3 (3.5, 5.0) |
2.7 (1.8, 3.5) |
|
Height SDS (Tanner*/Sempé† | ||
|
Baseline |
-3.1 ± 1.0 |
-3.2 ± 1.0 |
|
Month 12 |
-2.7 ± 1.1 |
-2.9 ± 1.0 |
|
Change from baseline (95% CI) |
0.4 (0.3, 0.6) |
0.3 (0.1, 0.4) |
|
Height SDS (Ranke Standard) | ||
|
Baseline |
-0.2 ± 0.8 |
-0.3 ± 0.8 |
|
Month 12 |
0.6 ± 0.9 |
0.1 ± 0.8 |
|
Change from baseline (95% CI) |
0.8 (0.7, 0.9) |
0.5 (0.4, 0.5) |
16. How is Omnitrope supplied
Storage
Store Omnitrope refrigerated at 2° to 8°C (36° to 46°F).
Do not freeze.
Omnitrope is light sensitive and should be stored in the carton.
16.1 OMNITROPE Cartridge 5 mg/1.5 mL
Omnitrope Cartridge (somatropin) 5 mg/1.5 mL is supplied in the following package sizes:
- •
- One cartridge (NDC 0781-3001-07)
- •
- Five cartridges (NDC 0781-3001-26)
For use only with the Omnitrope Pen 5 delivery system, which is sold separately After the first use the cartridge should remain in the pen and has to be kept in a refrigerator at 2° to 8°C (36° to 46°F) for a maximum of 28 days (see Table 11).
16.2 OMNITROPE Cartridge 10 mg/1.5 mL
Omnitrope Cartridge (somatropin) injection 10 mg/1.5 mL is supplied in the following package sizes:
- •
- One cartridge (NDC 0781-3004-07)
- •
- Five cartridges (NDC 0781-3004-26)
For use only with the Omnitrope Pen 10 delivery system, which is sold separately. After the first use the cartridge should remain in the pen and has to be kept in a refrigerator at 2° to 8°C (36° to 46°F) for a maximum of 28 days (see Table 11).
16.3 OMNITROPE (somatropin) for injection 5.8 mg/vial
After reconstitution, the concentration is 5 mg/mL.
- •
- Carton contains 8 vials of Omnitrope 5.8 mg and 8 vials of diluent (Bacteriostatic Water for injection containing 1.5% benzyl alcohol as a preservative.)
NDC 0781-4004-36
Omnitrope 5.8 mg is supplied with a diluent containing benzyl alcohol as a preservative. After reconstitution, the contents of the vial must be used within 3 weeks. After the first injection, the vial should be stored in the carton in a refrigerator at 2° to 8°C (36° to 46°F) (see Table 11).
|
Omnitrope
|
Storage Requirement |
|
|
|
In-use
|
|
|
5 mg/1.5 mL
|
2-8ºC/ |
2-8 ºC/36-46 ºF |
|
10 mg/1.5 mL
|
2-8 ºC/36-46 ºF |
|
|
5.8 mg/vial |
2-8 ºC/36-46 ºF |
|
17. Patient Counseling Information
See FDA-approved patient labeling (Instructions For Use: Omnitrope Pen 5 Instructions For Use, Omnitrope Pen 10 Instructions For Use, Instructions For Omnitrope 5.8 mg/Vial).
Patients being treated with Omnitrope (and/or their parents) should be informed about the potential risks and benefits associated with somatropin treatment. This information is intended to better educate patients (and caregivers); it is not a disclosure of all possible adverse or intended effects.
Patients and caregivers who will administer Omnitrope should receive appropriate training and instruction on the proper use of Omnitrope from the physician or other suitably qualified health care professional. A puncture-resistant container for the disposal of used syringes and needles should be strongly recommended. Patients and/or parents should be thoroughly instructed in the importance of proper disposal, and cautioned against any reuse of needles and syringes. Counsel patients and parents that they should never share an Omnitrope Pen with another person, even if the needle is changed. Sharing of the pen between patients may pose a risk of transmission of infection.
If patients are prescribed Omnitrope Cartridge 5 mg/1.5 mL or 10 mg/1.5 mL (to be inserted into Omnitrope Pen 5 or Pen 10 delivery systems), physicians should instruct patients to read the corresponding Instructions For Use provided with the Omnitrope Pens delivery systems and the Omnitrope Cartridges.
If patients are prescribed Omnitrope for injection, physicians should instruct patients to read the Instructions For Use leaflets provided with the Omnitrope for injection 5.8 mg/vial.
Omnitrope is a registered trademark of Novartis AG.
Manufactured in Austria by Sandoz GmbH
Distributed by Sandoz Inc., Princeton, NJ 08540
Rev. June 2019
INSTRUCTIONS FOR USE
OMNITROPE® PEN 5 INSTRUCTIONS FOR USE
Omnitrope (om-KNEE-trope)
(somatropin) injection, for subcutaneous use
5 mg/1.5 mL cartridges for use with
Omnitrope Pen 5
Read these Instructions for Use before you start using Omnitrope Pen 5 and each time you get a refill. There may be new information. This information does not take the place of talking to the healthcare provider about the medical condition or the treatment.
Note:
- •
- Omnitrope is for use under the skin only (subcutaneous).
- •
- Do not share your Omnitrope Pen or needles with anyone else. You may give an infection to them or get an infection from them.
- •
- The “Start use by no later than” date, presented in year, month and day on the outer carton, indicates the date after which therapy should not be initiated with this pen.
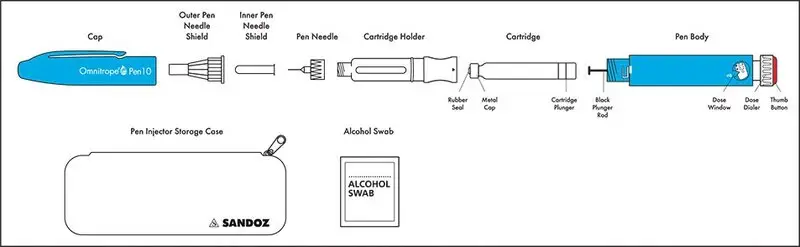
Omnitrope Pen 5, cartridge containing Omnitrope, needle, alcohol swab and storage case:
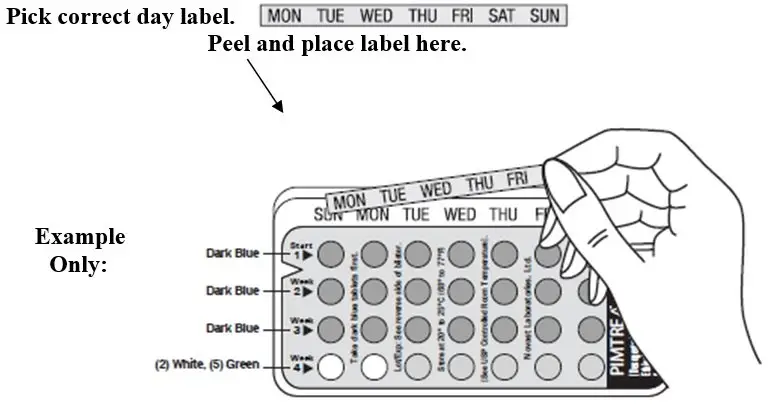
Supplies you will need to give an Omnitrope Injection. See Figure A.
- •
- Omnitrope Pen 5
- •
- 5 mg/1.5 mL cartridge containing Omnitrope
- •
- 1 new BD™ Pen needle (29G x 12.7 mm or 31G x 8 mm or 31G x 5 mm). Needles are not included with the Pen.
- •
- 1 alcohol swab
- •
- flat surface like a table
- •
- a sharps disposal container. See Step 6 for information on how to dispose of used needles and syringes.
Steps you should follow to give an Omnitrope injection:
Step 1. Placing the cartridge in the Omnitrope Pen 5
Step 2. Attaching the needle to the Omnitrope Pen 5
Step 3. Priming a new cartridge
Step 4. Selecting the correct dose of Omnitrope
Step 5. Selecting the injection site and injecting the dose of Omnitrope
Step 6. Removing and throwing away the needle and empty cartridge
Step 1. Placing the cartridge in the Omnitrope Pen 5
- •
- Take an Omnitrope cartridge out of the refrigerator and leave at room temperature for about 30 minutes. Wash and dry your hands while you wait.
- •
- Assemble all of the supplies needed on a flat surface. Remove the Pen and cartridge from their cartons if you are preparing the injection for the first time.
- •
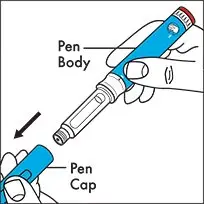
- Hold the body of the Pen with 1 hand and pull off the Pen cap with the other hand. See Figure B.
- •
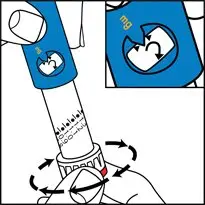
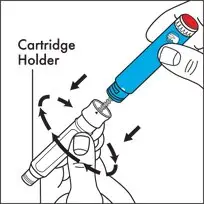
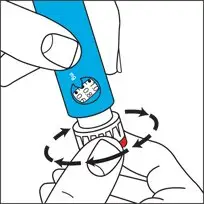
- Hold the body of the Pen with 1 hand and unscrew the cartridge holder in a clockwise direction until the Pen and cartridge holder are completely separated. See Figure C.
- •
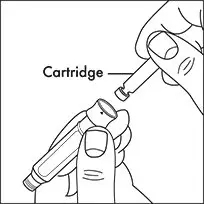
- Hold the cartridge in 1 hand with the metal cap end pointing down. Insert the cartridge into the cartridge holder. See Figure D.
- •
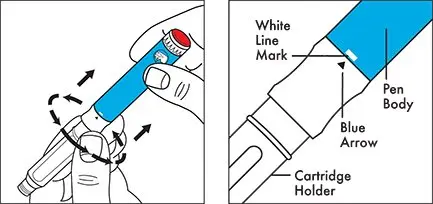
- Lower the Pen body onto the cartridge holder so that the black rod presses against the cartridge plunger. Screw the cartridge holder onto the Pen body in a counterclockwise direction until the cartridge holder will not turn anymore. One of the blue arrows on the cartridge holder must line up with the yellow line mark on the Pen body. Do not over tighten the cartridge holder. See Figure E.
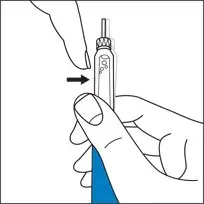
Step 2. Attaching the needle to the Omnitrope Pen 5
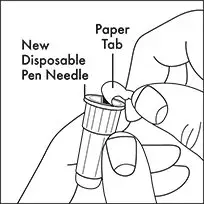
- •
- Take a new disposable needle and tear off the paper tab. Do not touch the needle or lay it on a surface. See Figure F.
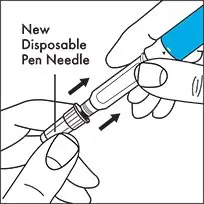
- •
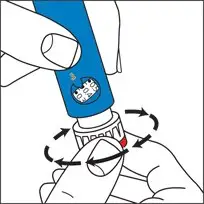
- Holding the cartridge holder with 1 hand, firmly press the needle onto the cartridge holder end of the Pen. See Figure G. Screw the threaded hub of the needle onto the cartridge holder in a counterclockwise direction until the needle will not turn anymore. See Figure H.
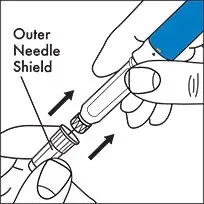
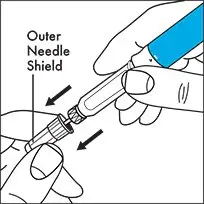
- •
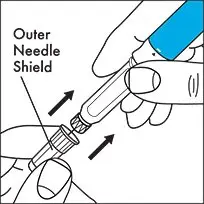
- Gently pull off the outer needle shield and put it on a flat surface. You will use the outer needle shield later to remove the needle from the Pen after the injection is finished. See Figure I.
Note: Check that the cartridge holder is attached to the Pen body before each injection. One of the blue arrows on the cartridge should be lined up with the yellow mark on the Pen body. After you attach the needle, you may see a few drops of medicine at the tip of the needle.
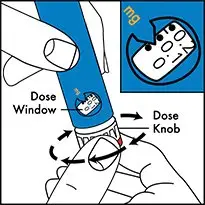
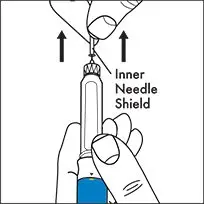
Step 3. Priming a new cartridge
- •
- Priming is not needed for a cartridge you have used before. If the cartridge has already been primed, go to Step 4.
- •
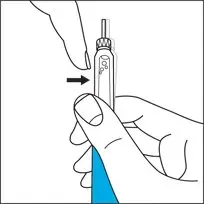
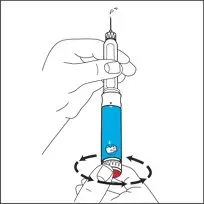
- Before you use a new cartridge you must first prepare it for use. Hold the Pen with the needle pointing upwards. Gently tap the cartridge holder with your finger to help air bubbles rise to the top of the cartridge. See Figure J.
- •
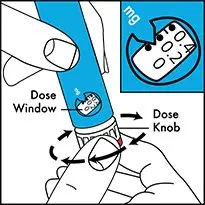
- Hold the pen with the needle pointing up and the dose window facing you and you will see the numbers in the dose window at the bottom of the Pen body. Using the dose knob on the bottom of the Pen, slowly turn the dose knob in a clockwise direction as shown in Figure K until you hear 1 “click”. The arrow on the Pen body will then be lined up with the small line between “0” and “0.1” (0.05 mg). See Figure K.
- •
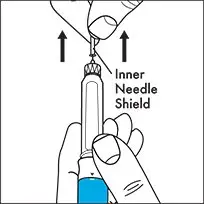
- Remove the inner needle shield. See Figure L.
- •
- With the needle pointing up, firmly turn the dose knob in a counterclockwise direction and back to the “0” position.
At least 2 drops of medicine must flow out of the needle for the Pen to be properly primed. See Figure M.
- •
- If at least 2 drops of medicine do not flow out, set the dose to 0.05 mg and repeat this step until at least 2 drops of medicine appear at the tip of the needle.
- •
- When you see 2 drops of medicine flow out of the needle, the Pen is correctly primed and ready to use.
Step 4. Selecting the correct dose of Omnitrope
- •
- Hold the pen with the needle pointing up and the dose window facing you and turn (dial) the dose knob in a clockwise direction until you see the number of mg for the prescribed dose in the middle of the dose window. The dose should be lined up with the arrow on the Pen body. You will hear 1 click for every single unit you dial. See Figure N.
Do not count the clicks to measure the correct dose of medicine.
- •
- If you turn the dose knob past the correct dose, do not dial counterclockwise.
Instead, hold the Pen body with the needle pointing up and turn the dose knob in a clockwise direction until you see a bent arrow (
 ) in the dose dialing window. See Figure O. Now continue to turn the dose knob in a clockwise direction until you hear a click and the entire Pen body is fully extended.
) in the dose dialing window. See Figure O. Now continue to turn the dose knob in a clockwise direction until you hear a click and the entire Pen body is fully extended.
The injection button can now be fully pressed, resetting the dial to “0” without giving medicine. The correct dose can now be redialed.
- •
- Check that the cartridge holder is still attached to the Pen body, with the blue arrow lined up with the yellow mark on the Pen body.
Step 5. Selecting the injection site and injecting the dose of Omnitrope
Change the injection site every day. See Figure P.
- •
- Select the injection site and wipe the skin with an alcohol pad as your healthcare provider showed you.
- •
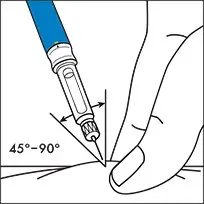
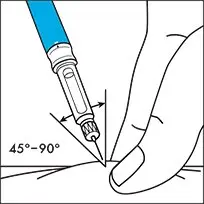
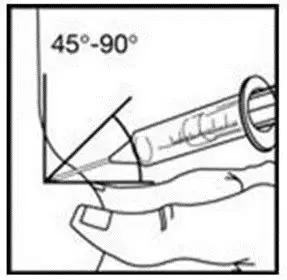
- Insert the needle under the skin as your healthcare provider showed you. See Figure Q.
- •
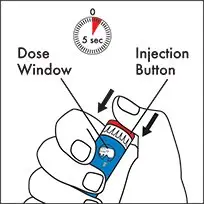
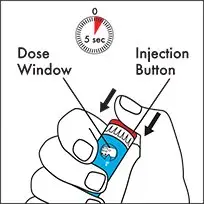
- After inserting the needle into the skin, push the injection button as far in as it will go and press the button firmly. A clicking sound will be heard while the dose is being injected. Continue to press firmly on the injection button for 5 seconds before you remove the needle from the skin. See Figure R.
- •
- Stop pressing the injection button before you carefully remove the needle from the skin.
- •
- If the injection button cannot be pushed in completely or stops during the injection, and the cartridge is empty, then the full dose has not been given. The dose indicator window will show the amount of medicine still needed. Reset the dose knob to “0” as described in Step 4. Remove the needle as described in Step 6. Replace the empty cartridge with a new cartridge as described in Step 1. Prime the new cartridge as described in Step 3. Set the dose, which you noted, and inject. This completes your dose.
Step 6. Removing and throwing away the needle and empty cartridge
- •
- Carefully replace the outer needle shield. See Figure S.
- •
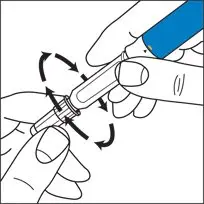
- Hold the Pen by the cartridge holder and carefully remove the needle from the Pen by turning the needle in a clockwise direction. See Figure T. Recap the pen.
- •
- Put your used needles and cartridges in a FDA-cleared sharps disposal container right away after use. Do not throw away (dispose of) loose needles and cartridges in your household trash.
- •
- If you do not have a FDA-cleared sharps disposal container, you may use a household container that is:
- o
- made of a heavy-duty plastic,
- o
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out,
- o
- upright and stable during use,
- o
- leak-resistant, and
- o
- properly labeled to warn of hazardous waste inside the container.
- •
- When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and cartridges. For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA’s website at: http://www.fda.gov/safesharpsdisposal.
- •
- Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container.
How should I store Omnitrope Pen 5?
- •
- Store Omnitrope cartridges in the refrigerator between 36°F and 46°F (2°C and 8°C).
- •
- When the Omnitrope Pen 5 contains a cartridge, do not remove the cartridge from the Pen in between injections. Store the Pen containing the cartridge in the storage case provided and place in the refrigerator.
- •
- When the Pen does not contain a cartridge, you may store the Pen at room temperature.
- •
- Do not freeze Omnitrope cartridges.
- •
- Protect the Omnitrope Pen 5 and cartridge from light by storing in their cartons or the storage case.
- •
- The Omnitrope cartridge must be thrown away 28 days after the first injection. The Omnitrope Pen 5 can be reloaded with a new cartridge and can be used multiple times.
Important information about possible problems you may have with the Omnitrope Pen 5
| Problem | Possible cause | How to fix |
|---|---|---|
|
Dial unit does not turn easily. |
Dust or dirt |
Turn the dial beyond the highest setting on the scale. Wipe all exposed surfaces with a clean, damp cloth. |
|
The injection button cannot be pushed or stops during injection. The dose knob does not return to “0”. |
Cartridge is empty and full dose has not been given. |
Remove the needle as described in Step 6. Replace the empty cartridge with a new cartridge as described in Step 1. Prime the new cartridge as described in Step 3. |
|
Clogged needle. |
Remove the needle as described in Step 6. Replace with a new needle as described in Step 2. |
|
|
No clicking is heard during the injection and dose knob moves freely. |
Pen is in dose correction mode. |
Remove the needle from skin. Press injection button all the way in so the dial returns to zero and repeat Step 2, Step 4 and Step 5 to give the injection. |
|
Medicine continues to drip from the needle before injection. |
Cartridge holder is not properly attached to the Pen body. |
Line up blue arrow on cartridge holder with yellow mark on Pen body. |
|
Medicine continues to drip from the needle after injection. |
Needle was removed from the skin too early. |
Hold the needle in the skin for 5 seconds to complete the injection, before you carefully remove the needle from the skin. For the next injection, make sure that you hold the needle in the skin for 5 seconds. |
|
Cartridge holder is not properly attached to the Pen body. |
Line up blue arrow on cartridge holder with yellow mark on Pen body. |
|
|
The needle is left on the Pen after injection. |
Carefully remove the needle from the Pen right after the injection. |
If the Omnitrope Pen 5 is damaged or does not work, call the pharmacy where you got the Omnitrope Pen 5. If you got your Omnitrope Pen 5 from OmniSource, call 1-877-456-6794.
For other questions or additional information, call OmniSource at 1-877-456-6794. Do not try to repair the Pen yourself.
Your Omnitrope Pen 5 is covered by a 2 year guarantee. Contact your Omnitrope Pen 5 provider after you have used the pen for 2 years to have it replaced by a new one.
This guarantee is invalid if your Omnitrope Pen 5 has not been used in accordance with the manufacturer’s instruction leaflet or if the defect has been caused by neglect, misuse or accident.
These Instructions for Use have been approved by the U.S. Food and Drug Administration.
Omnitrope is a trademark of Novartis.
BD and BD Logo are trademarks of Becton, Dickinson and Company © 2016 BD
Manufactured for
Sandoz GmbH, Kundl, Austria
Product of Taiwan
Distributed by
Sandoz Inc., Princeton, NJ 08540
12-2017
46170948
OMNITROPE® PEN 10 INSTRUCTIONS FOR USE
Omnitrope (om-KNEE-trope)
(somatropin) injection, for subcutaneous use
10 mg/1.5 mL cartridges for use with
Omnitrope Pen 10
Read these Instructions for Use before you start using Omnitrope Pen 10 and each time you get a refill. There may be new information. This information does not take the place of talking to the healthcare provider about the medical condition or the treatment.
Note:
- •
- Omnitrope is for use under the skin only (subcutaneous).
- •
- Do not share your Omnitrope Pen or needles with anyone else. You may give an infection to them or get an infection from them.
- •
- The “Start use by no later than” date, presented in year, month and day on the outer carton, indicates the date after which therapy should not be initiated with this pen.
Omnitrope Pen 10, cartridge containing Omnitrope, needle, alcohol swab and storage case:
Supplies you will need to give an Omnitrope Injection. See Figure A.
- •
- Omnitrope Pen 10
- •
- 10 mg/1.5 mL cartridge containing Omnitrope
- •
- 1 new BD™ Pen needle (29G x 12.7 mm or 31G x 8 mm or 31G x 5 mm). Needles are not included with the Pen.
- •
- 1 alcohol swab
- •
- flat surface like a table
- •
- a sharps disposal container. See Step 6 for information on how to dispose of used needles and syringes.
Steps you should follow to give an Omnitrope injection:
Step 1. Placing the cartridge in the Omnitrope Pen 10
Step 2. Attaching the needle to the Omnitrope Pen 10
Step 3. Priming a new cartridge
Step 4. Selecting the correct dose of Omnitrope
Step 5. Selecting the injection site and injecting the dose of Omnitrope
Step 6. Removing and throwing away the needle and empty cartridge
Step 1. Placing the cartridge in the Omnitrope Pen 10
- •
- Take an Omnitrope cartridge out of the refrigerator and leave at room temperature for about 30 minutes. Wash and dry your hands while you wait.
- •
- Assemble all of the supplies needed on a flat surface. Remove the Pen and cartridge from their cartons if you are preparing the injection for the first time.
- •
- Hold the body of the Pen with 1 hand and pull off the Pen cap with the other hand. See Figure B.
- •
- Hold the body of the Pen with 1 hand and unscrew the cartridge holder in a clockwise direction until the Pen and cartridge holder are completely separated. See Figure C.
- •
- Hold the cartridge in 1 hand with the metal cap end pointing down. Insert the cartridge into the cartridge holder. See Figure D.
- •
- Lower the Pen body onto the cartridge holder so that the black rod presses against the cartridge plunger. Screw the cartridge holder onto the Pen body in a counterclockwise direction until the cartridge holder will not turn anymore. One of the blue arrows on the cartridge holder must line up with the white line mark on the Pen body. Do not over tighten the cartridge holder. See Figure E.
Step 2. Attaching the needle to the Omnitrope Pen 10
- •
- Take a new disposable needle and tear off the paper tab. Do not touch the needle or lay it on a surface. See Figure F.
- •
- Holding the cartridge holder with 1 hand, firmly press the needle onto the cartridge holder end of the Pen. See Figure G. Screw the threaded hub of the needle onto the cartridge holder in a counterclockwise direction until the needle will not turn anymore. See Figure H.
- •
- Gently pull off the outer needle shield and put it on a flat surface. You will use the outer needle shield later to remove the needle from the Pen after the injection is finished. See Figure I.
Note: Check that the cartridge holder is attached to the Pen body before each injection. One of the blue arrows on the cartridge should be lined up with the white mark on the Pen body. After you attach the needle, you may see a few drops of medicine at the tip of the needle.
Step 3. Priming a new cartridge
- •
- Priming is not needed for a cartridge you have used before. If the cartridge has already been primed, go to Step 4.
- •
- Before you use a new cartridge you must first prepare it for use. Hold the Pen with the needle pointing upwards. Gently tap the cartridge holder with your finger to help air bubbles rise to the top of the cartridge. See Figure J.
- •
- Hold the pen with the needle pointing up and the dose window facing you and you will see the numbers in the dose window at the bottom of the Pen body. Using the dose knob on the bottom of the Pen, slowly turn the dose knob in a clockwise direction as shown in Figure K until you hear 1 “click”. The arrow on the Pen body will then be lined up with the small line between “0” and “0.2” (0.1 mg). See Figure K.
- •
- Remove the inner needle shield. See Figure L.
- •
- With the needle pointing up, firmly turn the dose knob in a counterclockwise direction and back to the “0” position.
At least 2 drops of medicine must flow out of the needle for the Pen to be properly primed. See Figure M.
- •
- If at least 2 drops of medicine do not flow out, set the dose to 0.1 mg and repeat this step until at least 2 drops of medicine appear at the tip of the needle.
- •
- When you see 2 drops of medicine flow out of the needle, the Pen is correctly primed and ready to use.
Step 4. Selecting the correct dose of Omnitrope
- •
- Hold the pen with the needle pointing up and the dose window facing you and turn (dial) the dose knob in a clockwise direction until you see the number of mg for the prescribed dose in the middle of the dose window. The dose should be lined up with the arrow on the Pen body. You will hear 1 click for every single unit you dial. See Figure N.
Do not count the clicks to measure the correct dose of medicine.
- •
- If you turn the dose knob past the correct dose, do not dial counterclockwise.
Instead, hold the Pen body with the needle pointing up and turn the dose knob in a clockwise direction until you see a bent arrow ( ) in the dose dialing window. See Figure O. Now continue to turn the dose knob in a clockwise direction until you hear a click and the entire Pen body is fully extended.
) in the dose dialing window. See Figure O. Now continue to turn the dose knob in a clockwise direction until you hear a click and the entire Pen body is fully extended.
The injection button can now be fully pressed, resetting the dial to “0” without giving medicine. The correct dose can now be redialed.
- •
- Check that the cartridge holder is still attached to the Pen body, with the blue arrow lined up with the white mark on the Pen body.
Step 5. Selecting the injection site and injecting the dose of Omnitrope
Change the injection site every day. See Figure P.
- •
- Select the injection site and wipe the skin with an alcohol pad as your healthcare provider showed you.
- •
- Insert the needle under the skin as your healthcare provider showed you. See Figure Q.
- •
- After inserting the needle into the skin, push the injection button as far in as it will go and press the button firmly. A clicking sound will be heard while the dose is being injected. Continue to press firmly on the injection button for 5 seconds before you remove the needle from the skin. See Figure R.
- •
- Stop pressing the injection button before you carefully remove the needle from the skin.
- •
- If the injection button cannot be pushed in completely or stops during the injection, and the cartridge is empty, then the full dose has not been given. The dose indicator window will show the amount of medicine still needed. Reset the dose knob to “0” as described in Step 4. Remove the needle as described in Step 6. Replace the empty cartridge with a new cartridge as described in Step 1. Prime the new cartridge as described in Step 3. Set the dose, which you noted, and inject. This completes your dose.
Step 6. Removing and throwing away the needle and empty cartridge
- •
- Carefully replace the outer needle shield. See Figure S.
- •
- Hold the Pen by the cartridge holder and carefully remove the needle from the Pen by turning the needle in a clockwise direction. See Figure T. Recap the pen.
- •
- Put your used needles and cartridges in a FDA-cleared sharps disposal container right away after use. Do not throw away (dispose of) loose needles and cartridges in your household trash.
- •
- If you do not have a FDA-cleared sharps disposal container, you may use a household container that is:
- o
- made of a heavy-duty plastic,
- o
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out,
- o
- upright and stable during use,
- o
- leak-resistant, and
- o
- properly labeled to warn of hazardous waste inside the container.
- •
- When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and cartridges. For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA’s website at: http://www.fda.gov/safesharpsdisposal.
- •
- Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container.
How should I store Omnitrope Pen 10?
- •
- Store Omnitrope cartridges in the refrigerator between 36°F and 46°F (2°C and 8°C).
- •
- When the Omnitrope Pen 10 contains a cartridge, do not remove the cartridge from the Pen in between injections. Store the Pen containing the cartridge in the storage case provided and place in the refrigerator.
- •
- When the Pen does not contain a cartridge, you may store the Pen at room temperature.
- •
- Do not freeze Omnitrope cartridges.
- •
- Protect the Omnitrope Pen 10 and cartridge from light by storing in their cartons or the storage case.
- •
- The Omnitrope cartridge must be thrown away 28 days after the first injection. The Omnitrope Pen 10 can be reloaded with a new cartridge and can be used multiple times.
Important information about possible problems you may have with the Omnitrope Pen 10
| Problem | Possible cause | How to fix |
|---|---|---|
|
Dial unit does not turn easily. |
Dust or dirt |
Turn the dial beyond the highest setting on the scale. Wipe all exposed surfaces with a clean, damp cloth. |
|
The injection button cannot be pushed or stops during injection. The dose knob does not return to “0”. |
Cartridge is empty and full dose has not been given. |
Remove the needle as described in Step 6. Replace the empty cartridge with a new cartridge as described in Step 1. Prime the new cartridge as described in Step 3. |
|
Clogged needle. |
Remove the needle as described in Step 6. Replace with a new needle as described in Step 2. |
|
|
No clicking is heard during the injection and dose knob moves freely. |
Pen is in dose correction mode. |
Remove the needle from skin. Press injection button all the way in so the dial returns to zero and repeat Step 2, Step 4 and Step 5 to give the injection. |
|
Medicine continues to drip from the needle before injection. |
Cartridge holder is not properly attached to the Pen body. |
Line up blue arrow on cartridge holder with white mark on Pen body. |
|
Medicine continues to drip from the needle after injection. |
Needle was removed from the skin too early. |
Hold the needle in the skin for 5 seconds to complete the injection, before you carefully remove the needle from the skin. For the next injection, make sure that you hold the needle in the skin for 5 seconds. |
|
Cartridge holder is not properly attached to the Pen body. |
Line up blue arrow on cartridge holder with white mark on Pen body. |
|
|
The needle is left on the Pen after injection. |
Carefully remove the needle from the Pen right after the injection. |
If the Omnitrope Pen 10 is damaged or does not work, call the pharmacy where you got the Omnitrope Pen 10. If you got your Omnitrope Pen 10 from OmniSource, call 1-877-456-6794.
For other questions or additional information, call OmniSource at 1-877-456-6794. Do not try to repair the Pen yourself.
Your Omnitrope Pen 10 is covered by a 2 year guarantee. Contact your Omnitrope Pen 10 provider after you have used the pen for 2 years to have it replaced by a new one.
This guarantee is invalid if your Omnitrope Pen 10 has not been used in accordance with the manufacturer’s instruction leaflet or if the defect has been caused by neglect, misuse or accident.
These Instructions for Use have been approved by the U.S. Food and Drug Administration.
Omnitrope is a trademark of Novartis.
BD and BD Logo are trademarks of Becton, Dickinson and Company © 2016 BD
Manufactured for
Sandoz GmbH, Kundl, Austria
Product of Taiwan
Distributed by
Sandoz Inc., Princeton, NJ 08540
12-2017
46170949
INSTRUCTIONS FOR OMNITROPE® 5.8 MG/VIAL
The following instructions explain how to inject OMNITROPE 5.8 mg. Do not inject OMNITROPE yourself until your healthcare provider has taught you and you understand the instructions. Ask your healthcare provider or pharmacist if you have any questions about injecting OMNITROPE.
- •
- OMNITROPE 5.8 mg is for multiple uses.
- •
- The concentration of OMNITROPE after mixing is 5 mg/mL.
- •
- After mixing, OMNITROPE 5.8 mg contains a preservative and should not be used in newborns.
Preparation
Collect necessary items before you begin:
- •
- a vial with OMNITROPE 5.8 mg
- •
- a vial with diluent (mixing liquid - Bacteriostatic Water for Injection containing benzyl alcohol as preservative) for OMNITROPE 5.8 mg
- •
- a sterile, disposable 3 mL syringe and needle for withdrawing the diluent from the vial (not supplied in the pack)
- •
- sterile disposable 1 mL syringes and needles for under the skin (subcutaneous) injection (not supplied in the pack)
- •
- 2 alcohol swabs (not supplied in the pack)
Wash your hands before you start with the next steps.
Mixing OMNITROPE 5.8 mg
- •
- Remove the protective caps from the two vials. With one alcohol swab, clean both the rubber top of the vial that contains the powder and the rubber top of the vial that contains diluent.
- •
- Use next the sterile diluent vial, the disposal 3 mL syringe and a needle.
- •
- Attach the needle to the syringe (if not attached already). Pull back the syringe plunger and fill the syringe with air. Push the needle fitted to the syringe through the rubber top of the diluent vial, push all the air from the syringe into the vial, turn the vial upside down, and withdraw all the diluent from the vial into the syringe. Remove the syringe and needle.
- •
- Next take the syringe with the diluent in it and push the needle through the rubber stopper of the vial that contains the white powder. Inject the diluent slowly. Aim the stream of liquid against the glass wall in order to avoid foam. Remove the syringe and needle and dispose of them.
- •
- Gently swirl the vial until the content is completely dissolved. Do not shake.
- •
- If the medicine is cloudy or contains particles, it should not be used. The medicine must be clear and colorless after mixing.
- •
- After mixing the medicine, the medicine in the vial must be used within 3 weeks. Store the vial in a refrigerator at 2° to 8°C (36° to 46°F) after mixing and using it each time.
Measuring the Dose of OMNITROPE 5.8 mg to Be Injected
- •
- Next use the sterile, disposable 1 mL (or similar) syringe and needle for subcutaneous injection. Push the needle through the rubber top of the vial that contains the medicine that you have just mixed.
- •
- Turn the vial and the syringe upside down.
- •
- Be sure the tip of the syringe is in the OMNITROPE mixed medicine.
- •
- Pull back on the plunger slowly and withdraw the dose prescribed by your doctor into the syringe.
- •
- Hold the syringe with the needle in the vial pointing up and remove the syringe from the vial.
- •
- Check for air bubbles in the syringe. If you see any bubbles, pull the plunger slightly back; tap the syringe gently, with the needle pointing upwards, until the bubble disappears. Push the plunger slowly back up to the correct dose. If there is not enough medicine in the syringe after removing the air bubbles, draw more medicine into the syringe from the mixed medicine vial and repeat checking for bubbles.
- •
- Look at the mixed medicine in the syringe before using. Do not use if discolored or particles are present. You are now ready to inject the dose.
Injecting OMNITROPE 5.8 mg
- •
- Choose the site of injection on your body. The best sites for injection are tissues with a layer of fat between skin and muscle such as the upper leg (thigh), buttocks, or stomach area (abdomen) as in the picture shown below. Do not inject near your belly button (navel) or waistline.
- •
- Make sure you rotate the injection sites on your body. Inject at least 1/2 inch from the last injection. Change the places on your body where you inject, as you have been taught.
- •
- Before you make an injection, clean your skin well with an alcohol swab. Wait for the area to air dry.
- •
- With one hand, pinch a fold of loose skin at the injection site. With your other hand, hold the syringe as you would a pencil. Insert the needle into the pinched skin straight in or at a slight angle (an angle of 45° to 90°). After the needle is in, remove the hand used to pinch the skin and use it to hold the syringe barrel. Pull back the plunger very slightly with one hand. If blood comes into the syringe, the needle has entered a blood vessel. Do not inject into this site; withdraw the needle and repeat the procedure at a different site. If no blood comes into the syringe, inject the solution by pushing the plunger all the way down gently.
- •
- Pull the needle straight out of the skin. After injection, press the injection site with a small bandage or sterile gauze if needed for bleeding, for several seconds. Do not massage or rub the injection site.
After Injecting OMNITROPE 5.8 mg
- •
- Discard the injection materials.
- •
- Dispose the syringes safely in a closed container. You can ask your healthcare provider or pharmacist for a “sharps” container. A sharps container is a special container to put used needles and syringes in. You can return a full sharps container to your pharmacist or healthcare provider for disposal.
- •
- The vial of mixed medicine must be stored in the refrigerator in its carton at 2° to 8°C (36° to 46°F) and used within 3 weeks.
- •
- The solution should be clear after removal from the refrigerator. If the solution is cloudy or contains particles, discard the vial. Do not inject the medicine from this vial. Start over with a new vial of OMNITROPE 5.8 mg. Call your pharmacist if you need a replacement.
- •
- Before each use disinfect the rubber top of the reconstituted vial with an alcohol swab. You must use a new disposable 1 mL syringe and needle for each injection.
Omnitrope is a trademark of Novartis.
Manufactured in Austria by Sandoz GmbH
Distributed by Sandoz Inc., Princeton, NJ 08540
02-2016M
46170948
46170949
46171070
5 mg/1.5 mL Carton
NDC 0781-3001-07
Omnitrope®
Somatropin
injection
5 mg/1.5 mL
For subcutaneous injection only
Rx only
Each cartridge contains
somatropin 5 mg/1.5 mL
1 cartridge
SANDOZ
a Novartis company
10 mg/1.5 mL Carton
NDC 0781-3004-07
Omnitrope®
Somatropin
injection
10 mg/1.5 mL
For subcutaneous injection only
Rx only
Each cartridge contains
somatropin 10 mg/1.5 mL
1 cartridge
SANDOZ
a Novartis company
5.8 mg Carton
NDC 0781-4004-36
Omnitrope®
somatropin for injection
and
diluent with preservative (Bacteriostatic Water for Injection 1.14 mL)
5.8 mg/vial
Each carton contains:
8 vials of Omnitrope 5.8 mg/vial
8 single use vials of Bacteriostatic Water for Injection 1.14 mL
For subcutaneous injection only
NOT FOR USE IN NEWBORNS Rx only
SANDOZ
a Novartis company
| OMNITROPE
somatropin injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| OMNITROPE
somatropin injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| OMNITROPE
somatropin kit |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| Labeler - Sandoz Inc (005387188) |