Drug Detail:Otezla (Apremilast [ a-pre-mi-last ])
Drug Class: Antirheumatics
Highlights of Prescribing Information
OTEZLA® (apremilast) tablets, for oral use
Initial U.S. Approval: 2014
Indications and Usage for Otezla
OTEZLA, an inhibitor of phosphodiesterase 4 (PDE4), is indicated for the treatment of:
- Adult patients with active psoriatic arthritis (1.1)
- Adult patients with plaque psoriasis who are candidates for phototherapy or systemic therapy (1.2)
- Adult patients with oral ulcers associated with Behçet's Disease (1.3)
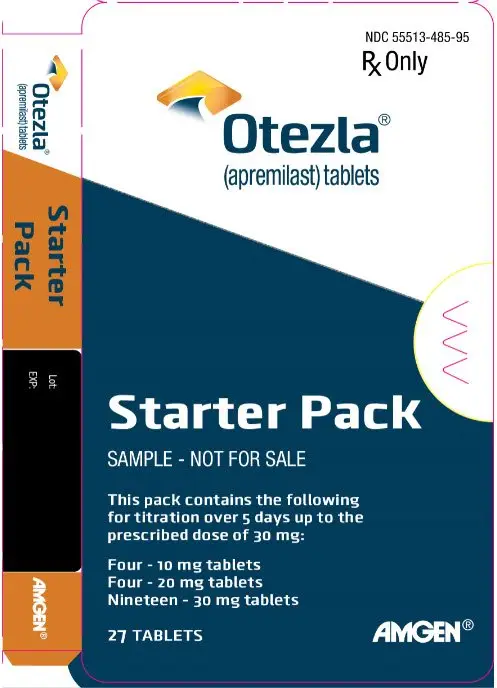
Otezla Dosage and Administration
- To reduce risk of gastrointestinal symptoms, titrate to recommended dosage of 30 mg twice daily according to the following schedule (2.1)
- Day 1: 10 mg in morning
- Day 2: 10 mg in morning and 10 mg in evening
- Day 3: 10 mg in morning and 20 mg in evening
- Day 4: 20 mg in morning and 20 mg in evening
- Day 5: 20 mg in morning and 30 mg in evening
- Day 6 and thereafter: 30 mg twice daily
-
Dosage in Severe Renal Impairment:
- Recommended dosage is 30 mg once daily (2.2)
- For initial dosage titration, titrate using only morning schedule listed in Table 1 and skip afternoon doses (2.2)
Dosage Forms and Strengths
Tablets: 10 mg, 20 mg, 30 mg (3)
Contraindications
Known hypersensitivity to apremilast or to any of the excipients in the formulation (4)
Warnings and Precautions
- Hypersensitivity: Cases of angioedema and anaphylaxis have been reported during post marketing surveillance. Avoid the use of OTEZLA in patients with known hypersensitivity to apremilast or to any of the excipients in the formulation. If signs or symptoms of serious hypersensitivity reactions develop during treatment, discontinue OTEZLA and institute appropriate therapy (5.1).
- Diarrhea, Nausea, and Vomiting: Consider OTEZLA dose reduction or suspension if patients develop severe diarrhea, nausea, or vomiting (5.2)
- Depression: Advise patients, their caregivers, and families to be alert for the emergence or worsening of depression, suicidal thoughts or other mood changes and if such changes occur to contact their healthcare provider. Carefully weigh risks and benefits of treatment with OTEZLA in patients with a history of depression and/or suicidal thoughts or behavior (5.3)
- Weight Decrease: Monitor weight regularly. If unexplained or clinically significant weight loss occurs, evaluate weight loss and consider discontinuation of OTEZLA (5.4)
- Drug Interactions: Use with strong cytochrome P450 enzyme inducers (e.g., rifampin, phenobarbital, carbamazepine, phenytoin) is not recommended because loss of efficacy may occur (5.5, 7.1)
Adverse Reactions/Side Effects
- Psoriatic Arthritis: The most common adverse reactions (≥ 5%) are diarrhea, nausea, and headache (6.1)
- Plaque Psoriasis: The most common adverse reactions (≥ 5%) are diarrhea, nausea, upper respiratory tract infection, and headache, including tension headache (6.1)
- Behçet's Disease: The most common adverse reactions (≥ 10%) are diarrhea, nausea, headache, and upper respiratory tract infection (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Amgen Inc. at 1-800-77-AMGEN (1-800-772-6436) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Use In Specific Populations
Severe Renal Impairment: Increased systemic exposure of OTEZLA has been observed, reduction in dosage to 30 mg once daily is recommended (2.2, 8.6)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 7/2023
Full Prescribing Information
1. Indications and Usage for Otezla
1.1 Psoriatic Arthritis
OTEZLA is indicated for the treatment of adult patients with active psoriatic arthritis.
2. Otezla Dosage and Administration
2.1 Dosage in Psoriatic Arthritis, Plaque Psoriasis, and Behçet's Disease
The recommended initial dosage titration of OTEZLA from Day 1 to Day 5 is shown in Table 1. Following the 5-day titration, the recommended maintenance dosage is 30 mg twice daily taken orally starting on Day 6. This titration is intended to reduce the gastrointestinal symptoms associated with initial therapy.
OTEZLA can be administered without regard to meals. Do not crush, split, or chew the tablets.
| Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 & thereafter | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| AM | AM | PM | AM | PM | AM | PM | AM | PM | AM | PM |
| 10 mg | 10 mg | 10 mg | 10 mg | 20 mg | 20 mg | 20 mg | 20 mg | 30 mg | 30 mg | 30 mg |
2.2 Dosage Adjustment in Patients with Severe Renal Impairment
OTEZLA dosage should be reduced to 30 mg once daily in patients with severe renal impairment (creatinine clearance (CLcr) of less than 30 mL per minute estimated by the Cockcroft–Gault equation) [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)]. For initial dosage titration in this group, it is recommended that OTEZLA be titrated using only the AM schedule listed in Table 1 and the PM doses be skipped.
3. Dosage Forms and Strengths
OTEZLA is available as diamond shaped, film coated tablets in the following dosage strengths:
- 10-mg pink tablet engraved with "APR" on one side and "10" on the other side
- 20-mg brown tablet engraved with "APR" on one side and "20" on the other side
- 30-mg beige tablet engraved with "APR" on one side and "30" on the other side
4. Contraindications
OTEZLA is contraindicated in patients with a known hypersensitivity to apremilast or to any of the excipients in the formulation [see Adverse Reactions (6.1)].
5. Warnings and Precautions
5.1 Hypersensitivity
Hypersensitivity reactions, including cases of angioedema and anaphylaxis, have been reported during post marketing surveillance. Avoid the use of OTEZLA in patients with known hypersensitivity to apremilast or to any of the excipients in the formulation. If signs or symptoms of serious hypersensitivity reactions develop during treatment, discontinue OTEZLA and institute appropriate therapy.
5.2 Diarrhea, Nausea, and Vomiting
There have been reports of severe diarrhea, nausea, and vomiting associated with the use of OTEZLA. Most events occurred within the first few weeks of treatment. In some cases, patients were hospitalized. Patients 65 years of age or older and patients taking medications that can lead to volume depletion or hypotension may be at a higher risk of complications from severe diarrhea, nausea, or vomiting. Monitor patients who are more susceptible to complications of diarrhea or vomiting. Patients who reduced dosage or discontinued OTEZLA generally improved quickly. Consider OTEZLA dose reduction or suspension if patients develop severe diarrhea, nausea, or vomiting.
5.3 Depression
Treatment with OTEZLA is associated with an increased incidence of depression. Before using OTEZLA in patients with a history of depression and/or suicidal thoughts or behavior, prescribers should carefully weigh the risks and benefits of treatment with OTEZLA. Patients, their caregivers, and families should be advised of the need to be alert for the emergence or worsening of depression, suicidal thoughts or other mood changes, and if such changes occur to contact their healthcare provider. Prescribers should carefully evaluate the risks and benefits of continuing treatment with OTEZLA if such events occur.
5.4 Weight Decrease
During the placebo-controlled period of the trials in psoriatic arthritis (PsA), weight decrease between 5%-10% of body weight was reported in 10% (49/497) of subjects treated with OTEZLA 30 mg twice daily compared to 3.3% (16/495) treated with placebo.
During the placebo-controlled period of the trials in moderate to severe plaque psoriasis, weight decrease between 5%-10% of body weight occurred in 12% (96/784) of subjects treated with OTEZLA compared to 5% (19/382) treated with placebo. Weight decrease of ≥ 10% of body weight occurred in 2% (16/784) of subjects treated with OTEZLA 30 mg twice daily compared to 1% (3/382) subjects treated with placebo.
During the placebo-controlled period of the mild to moderate plaque psoriasis clinical trial, weight decrease was similar to what was observed in the moderate to severe plaque psoriasis trials.
During the placebo-controlled period of the phase 3 trial in Behçet's Disease, weight decrease >5% of body weight was reported in 4.9% (5/103) of subjects treated with OTEZLA 30 mg twice daily compared to 3.9% (4/102) subjects treated with placebo.
Patients treated with OTEZLA should have their weight monitored regularly. If unexplained or clinically significant weight loss occurs, weight loss should be evaluated, and discontinuation of OTEZLA should be considered [see Adverse Reactions (6.1)].
5.5 Drug Interactions
Co-administration of strong cytochrome P450 enzyme inducer, rifampin, resulted in a reduction of systemic exposure of apremilast, which may result in a loss of efficacy of OTEZLA. Therefore, the use of cytochrome P450 enzyme inducers (e.g., rifampin, phenobarbital, carbamazepine, phenytoin) with OTEZLA is not recommended [see Drug Interactions (7.1) and Clinical Pharmacology (12.3)].
6. Adverse Reactions/Side Effects
The following adverse reactions are described elsewhere in the labeling:
- Hypersensitivity [see Warnings and Precautions (5.1)]
- Diarrhea, Nausea, and Vomiting [see Warnings and Precautions (5.2)]
- Depression [see Warnings and Precautions (5.3)]
- Weight Decrease [see Warnings and Precautions (5.4)]
- Drug Interactions [see Warnings and Precautions (5.5)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Psoriatic Arthritis Clinical Trials
OTEZLA was evaluated in 3 multicenter, randomized, double-blind, placebo-controlled trials (PsA-1, PsA-2, and PsA-3) of similar design in adult subjects with active psoriatic arthritis [see Clinical Studies (14.1)]. Across the 3 trials, there were 1493 subjects randomized equally to placebo, OTEZLA 20 mg twice daily or OTEZLA 30 mg twice daily. Titration was used over the first 5 days [see Dosage and Administration (2.1)]. Placebo subjects whose tender and swollen joint counts had not improved by at least 20% were re-randomized 1:1 in a blinded fashion to either OTEZLA 20 mg twice daily or 30 mg twice daily at week 16 while OTEZLA subjects remained on their initial treatment. Subjects ranged in age from 18 to 83 years, with an overall median age of 51 years.
The majority of the most common adverse reactions presented in Table 2 occurred within the first 2 weeks of treatment and tended to resolve over time with continued dosing. Diarrhea, headache, and nausea were the most commonly reported adverse reactions. The most common adverse reactions leading to discontinuation for subjects taking OTEZLA were nausea (1.8%), diarrhea (1.8%), and headache (1.2%). The proportion of subjects with psoriatic arthritis who discontinued treatment due to any adverse reaction was 4.6% for subjects taking OTEZLA 30 mg twice daily and 1.2% for placebo-treated subjects.
| Placebo | OTEZLA 30 mg BID* | |||
|---|---|---|---|---|
| Adverse Reactions | Day 1 to 5 (N = 495) n (%)† | Day 6 to Day 112 (N = 490) n (%) | Day 1 to 5 (N = 497) n (%) | Day 6 to Day 112 (N = 493) n (%) |
|
||||
| Diarrhea‡ | 6 (1.2) | 8 (1.6) | 46 (9.3) | 38 (7.7) |
| Nausea‡ | 7 (1.4) | 15 (3.1) | 37 (7.4) | 44 (8.9) |
| Headache‡ | 9 (1.8) | 11 (2.2) | 24 (4.8) | 29 (5.9) |
| Upper respiratory tract infection§ | 3 (0.6) | 9 (1.8) | 3 (0.6) | 19 (3.9) |
| Vomiting‡ | 2 (0.4) | 2 (0.4) | 4 (0.8) | 16 (3.2) |
| Nasopharyngitis§ | 1 (0.2) | 8 (1.6) | 1 (0.2) | 13 (2.6) |
| Abdominal pain upper§ | 0 (0.0) | 1 (0.2) | 3 (0.6) | 10 (2.0) |
Moderate to Severe Plaque Psoriasis Clinical Trials
The safety of OTEZLA was assessed in 1426 subjects in 3 randomized, double-blind, placebo-controlled trials in adult subjects with moderate to severe plaque psoriasis who were candidates for phototherapy or systemic therapy. Subjects were randomized to receive OTEZLA 30 mg twice daily or placebo twice daily. Titration was used over the first 5 days [see Dosage and Administration (2.1)]. Subjects ranged in age from 18 to 83 years, with an overall median age of 46 years.
Diarrhea, nausea, and upper respiratory tract infection were the most commonly reported adverse reactions (see Table 3). The most common adverse reactions leading to discontinuation for subjects taking OTEZLA were nausea (1.6%), diarrhea (1.0%), and headache (0.8%). The proportion of subjects with plaque psoriasis who discontinued treatment due to any adverse reaction was 6.1% for subjects treated with OTEZLA 30 mg twice daily and 4.1% for placebo-treated subjects.
| Adverse Reactions | Placebo (N = 506) n (%) | OTEZLA 30 mg BID* (N = 920) n (%) |
|---|---|---|
|
||
| Diarrhea | 32 (6) | 160 (17) |
| Nausea | 35 (7) | 155 (17) |
| Upper respiratory tract infection | 31 (6) | 84 (9) |
| Tension headache | 21 (4) | 75 (8) |
| Headache | 19 (4) | 55 (6) |
| Abdominal pain† | 11 (2) | 39 (4) |
| Vomiting | 8 (2) | 35 (4) |
| Fatigue | 9 (2) | 29 (3) |
| Dyspepsia | 6 (1) | 29 (3) |
| Decreased appetite | 5 (1) | 26 (3) |
| Insomnia | 4 (1) | 21 (2) |
| Back pain | 4 (1) | 20 (2) |
| Migraine | 5 (1) | 19 (2) |
| Frequent bowel movements | 1 (0) | 17 (2) |
| Depression | 2 (0) | 12 (1) |
| Bronchitis | 2 (0) | 12 (1) |
| Tooth abscess | 0 (0) | 10 (1) |
| Folliculitis | 0 (0) | 9 (1) |
| Sinus headache | 0 (0) | 9 (1) |
Severe worsening of psoriasis (rebound) occurred in 0.3% (4/1184) subjects following discontinuation of treatment with OTEZLA.
OTEZLA was evaluated in a Phase 3, multicenter, randomized, placebo-controlled trial (PSOR-3) in adults with moderate to severe plaque psoriasis of the scalp [see Clinical Studies (14.2)]. A total of 302 subjects were randomized to receive OTEZLA 30 mg twice daily or placebo twice daily. The most commonly reported adverse reactions that occurred at a higher rate in the OTEZLA group than in the placebo group were: diarrhea (31% vs. 11%), nausea (22% vs. 6%), headache (12% vs. 5%), and vomiting (6% vs. 2%). The proportion of subjects who discontinued treatment because of any adverse reaction during the 16-week placebo-controlled period of the trial was 6% for subjects who received OTEZLA 30 mg twice daily and 3% for subjects who received placebo. Gastrointestinal adverse reactions that led to discontinuation of treatment were diarrhea (3% vs. 0%), nausea (1.5% vs. 1%), and vomiting (1.5% vs. 0 %) in the OTEZLA group compared to placebo.
OTEZLA was evaluated in a Phase 3, multicenter, randomized, placebo-controlled trial (PSOR-5) in adults with moderate to severe plaque psoriasis of the genital area [see Clinical Studies (14.2)]. A total of 289 subjects were randomized to receive OTEZLA 30 mg twice daily or placebo twice daily. Overall, the safety profile observed in the OTEZLA group during the placebo-controlled phase was consistent with the safety profile previously established in adult subjects with moderate to severe plaque psoriasis.
Behçet's Disease Clinical Trials
OTEZLA was evaluated in a Phase 3, multicenter, randomized, placebo-controlled trial (BCT-002) in adult subjects with Behçet's Disease (BD) with active oral ulcers [see Clinical Studies (14.4)]. A total of 207 subjects were randomized to receive OTEZLA 30 mg twice daily or placebo twice daily. Titration was used over the first 5 days [see Dosage and Administration (2.1)]. After Week 12, all subjects received treatment with OTEZLA 30 mg twice daily. Subjects ranged in age from 19 to 72, with a mean age of 40 years.
Diarrhea, nausea, headache, and upper respiratory tract infection were the most commonly reported adverse reactions (see Table 4). The proportion of subjects with BD who discontinued treatment due to any adverse reaction during the placebo-controlled period of the trial, was 2.9% for subjects treated with OTEZLA 30 mg twice daily and 4.9% for placebo-treated subjects.
| Adverse Reactions | Placebo (N = 103) n (%) | OTEZLA 30 mg twice daily (N = 104) n (%) |
|---|---|---|
|
||
| Diarrhea* | 21 (20.4) | 43 (41.3) |
| Nausea* | 11 (10.7) | 20 (19.2) |
| Headache | 11 (10.7) | 15 (14.4) |
| Upper respiratory tract infection | 5 (4.9) | 12 (11.5) |
| Abdominal pain upper | 2 (1.9) | 9 (8.7) |
| Vomiting* | 2 (1.9) | 9 (8.7) |
| Back pain | 6 (5.8) | 8 (7.7) |
| Viral upper respiratory tract infection | 5 (4.9) | 7 (6.7) |
| Arthralgia | 3 (2.9) | 6 (5.8) |
8. Use In Specific Populations
8.4 Pediatric Use
The safety and effectiveness of OTEZLA in pediatric patients less than 18 years of age have not been established.
8.5 Geriatric Use
Of the 1493 patients who enrolled in Trials PsA-1, PsA-2, and PsA-3, a total of 146 psoriatic arthritis patients were 65 years of age and older, including 19 patients 75 years and older. No overall differences were observed in the safety profile of geriatric patients ≥ 65 years of age and younger adult patients < 65 years of age in the clinical trials.
Of the 1257 subjects who enrolled in two placebo-controlled plaque psoriasis trials (PSOR 1 and PSOR 2), a total of 108 plaque psoriasis patients were 65 years of age and older, including 9 patients who were 75 years of age and older. No overall differences were observed in the safety or effectiveness in geriatric patients ≥ 65 years of age and younger adult patients < 65 years of age in the clinical trials.
Because patients 65 years of age or older may be at a higher risk of complications such as volume depletion or hypotension from severe diarrhea, nausea, or vomiting, monitor geriatric patients closely for such complications [see Warning and Precautions (5.2)].
8.6 Renal Impairment
Apremilast pharmacokinetics were characterized in subjects with mild, moderate, and severe renal impairment as defined by a creatinine clearance of 60-89, 30-59, and less than 30 mL per minute, respectively, by the Cockcroft–Gault equation. While no dosage adjustment is needed in patients with mild or moderate renal impairment, the dosage of OTEZLA should be reduced to 30 mg once daily in patients with severe renal impairment [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)].
11. Otezla Description
The active ingredient in OTEZLA tablets is apremilast. Apremilast is a phosphodiesterase 4 (PDE4) inhibitor. Apremilast is known chemically as N-[2-[(1S)-1-(3-ethoxy-4-methoxyphenyl)-2-(methylsulfonyl)ethyl]-2,3-dihydro-1,3-dioxo-1H-isoindol-4-yl]acetamide. Its empirical formula is C22H24N2O7S and the molecular weight is 460.5.
The chemical structure is:
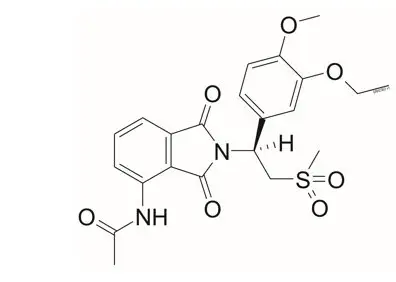
OTEZLA tablets are supplied in 10-, 20-, and 30-mg strengths for oral administration. Each tablet contains apremilast as the active ingredient and the following inactive ingredients: lactose monohydrate, microcrystalline cellulose, croscarmellose sodium, magnesium stearate, polyvinyl alcohol, titanium dioxide, polyethylene glycol, talc, iron oxide red, iron oxide yellow (20 and 30 mg only) and iron oxide black (30 mg only).
12. Otezla - Clinical Pharmacology
12.1 Mechanism of Action
Apremilast is an oral small-molecule inhibitor of phosphodiesterase 4 (PDE4) specific for cyclic adenosine monophosphate (cAMP). PDE4 inhibition results in increased intracellular cAMP levels. The specific mechanism(s) by which apremilast exerts its therapeutic action is not well defined.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies were conducted in mice and rats with apremilast to evaluate its carcinogenic potential. No evidence of apremilast-induced tumors was observed in mice at oral doses up to 8.8-times the Maximum Recommended Human Dose (MRHD) on an AUC basis (1000 mg/kg/day) or in rats at oral doses up to approximately 0.08- and 1.1-times the MRHD, (20 mg/kg/day in males and 3 mg/kg/day in females, respectively).
Apremilast tested negative in the Ames assay, in vitro chromosome aberration assay of human peripheral blood lymphocytes, and the in vivo mouse micronucleus assay.
In a fertility study of male mice, apremilast at oral doses up to approximately 3-times the MRHD based on AUC (up to 50 mg/kg/day) produced no effects on male fertility. In a fertility study of female mice, apremilast was administered at oral doses of 10, 20, 40, or 80 mg/kg/day. At doses ≥ 1.8-times the MRHD (≥ 20 mg/kg/day), estrous cycles were prolonged, due to lengthening of diestrus which resulted in a longer interval until mating. Mice that became pregnant at doses of 20 mg/kg/day and greater also had increased incidences of early postimplantation losses. There was no effect of apremilast approximately 1.0-times the MRHD (10 mg/kg/day).
14. Clinical Studies
14.1 Psoriatic Arthritis
The safety and efficacy of OTEZLA was evaluated in 3 multicenter, randomized, double-blind, placebo-controlled trials (PsA-1 [NCT01172938], PsA-2 [NCT01212757], and PsA-3 [NCT01212770]) of similar design. A total of 1493 adult subjects with active PsA (≥ 3 swollen joints and ≥ 3 tender joints) despite prior or current treatment with disease-modifying antirheumatic drug (DMARD) therapy were randomized. Subjects enrolled in these trials had a diagnosis of PsA for at least 6 months. One qualifying psoriatic skin lesion of at least 2 cm in diameter was required in Trial PsA-3. Previous treatment with a biologic, including TNF-blockers was allowed (up to 10% could be TNF-blocker therapeutic failures). Across the 3 trials, subjects were randomly assigned to placebo (n = 496), OTEZLA 20 mg (n = 500), or OTEZLA 30 mg (n = 497) given orally twice daily. Titration was used over the first 5 days [see Dosage and Administration (2.1)]. Subjects were allowed to receive stable doses of concomitant methotrexate [MTX (≤25 mg/week)], sulfasalazine [SSZ (≤ 2 g/day)], leflunomide [LEF (≤20 mg/day)], low dose oral corticosteroids (equivalent to ≤10 mg of prednisone a day), and/or nonsteroidal anti-inflammatory drugs (NSAIDs) during the trial. Treatment assignments were stratified based on small-molecule DMARD use at baseline in Trials PsA-1, PsA-2 and PsA-3. There was an additional stratification of body surface area (BSA) > 3% with psoriasis in Trial PsA-3. The subjects who were therapeutic failures of > 3 agents for PsA (small molecules or biologics), or > 1 biologic TNF blocker were excluded.
The primary endpoint was the percentage of subjects achieving American College of Rheumatology (ACR) 20 response at Week 16. Placebo-controlled efficacy data were collected and analyzed through Week 24. Subjects whose tender and swollen joint counts had not improved by at least 20% were considered non-responders at Week 16. Placebo non-responders were re-randomized 1:1 in a blinded fashion to either OTEZLA 20 mg twice daily or 30 mg twice daily following the titration schema [see Dosage and Administration (2.1)]. OTEZLA subjects remained on their initial treatment. At Week 24, all remaining placebo subjects were re-randomized to either 20 mg twice daily or 30 mg twice daily.
Subjects with subtypes of PsA were enrolled across the 3 trials, including symmetric polyarthritis (62.0%), asymmetric oligoarthritis (27.0%), distal interphalangeal (DIP) joint arthritis (6.0%), arthritis mutilans (3.0%), and predominant spondylitis (2.1%). The median duration of PsA disease was 5 years. Subjects received concomitant therapy with at least one DMARD (65.0%), MTX (55.0%), SSZ (9.0%), LEF (7.0%), low dose oral corticosteroids (14.0%), and NSAIDs (71.0%). Prior treatment with small-molecule DMARDs only was reported in 76.0% of subjects and prior treatment with biologic DMARDs was reported in 22.0% of subjects, which includes 9.0% who had failed prior biologic DMARD treatment.
Clinical Response in Subjects with Psoriatic Arthritis
The percent of subjects achieving ACR 20, 50 and 70 responses in Trials PsA-1, PsA-2, and PsA-3 are presented in Table 5 below. OTEZLA ± DMARDs, compared with Placebo ± DMARDs resulted in a greater improvement in signs and symptoms of psoriatic arthritis as demonstrated by the proportion of subjects with an ACR 20 response at Week 16.
| PsA-1 | PsA-2 | PsA-3 | ||||
|---|---|---|---|---|---|---|
| N* | Placebo ± DMARDs N = 168 | OTEZLA 30 mg twice daily ± DMARDs N = 168 | Placebo ± DMARDs N = 159 | OTEZLA 30 mg twice daily ± DMARDs N = 162 | Placebo ± DMARDs N = 169 | OTEZLA 30 mg twice daily ± DMARDs N = 167 |
|
||||||
| ACR 20
Week 16 | 19% | 38% † | 19% | 32% † | 18% | 41% † |
| ACR 50
Week 16 | 6% | 16% | 5% | 11% | 8% | 15% |
| ACR 70
Week 16 | 1% | 4% | 1% | 1% | 2% | 4% |
OTEZLA 30 mg twice daily resulted in improvement for each ACR component, compared to placebo at Week 16 in Trial PsA-1 (Table 6). Consistent results were observed in Trials PsA-2 and PsA-3.
| Placebo (N* = 168) | OTEZLA 30 mg twice daily (N* = 168) |
|
|---|---|---|
| Mean changes from baseline are least square means from analyses of covariance. | ||
|
||
| Number of tender joints† | ||
| Sample Size | 166 | 164 |
| Baseline | 23 | 23 |
| Mean Change at Week 16 | -2 | -7 |
| Number of swollen joints‡ | ||
| Sample Size | 166 | 164 |
| Baseline | 13 | 13 |
| Mean Change at Week 16 | -2 | -5 |
| Patient's assessment of pain§ | ||
| Sample Size | 165 | 159 |
| Baseline | 61 | 58 |
| Mean Change at Week 16 | -6 | -14 |
| Patient's global assessment of disease activity§ | ||
| Sample Size | 165 | 159 |
| Baseline | 59 | 56 |
| Mean Change at Week 16 | -3 | -10 |
| Physician's global assessment of disease activity§ | ||
| Sample Size | 158 | 159 |
| Baseline | 55 | 56 |
| Mean Change at Week 16 | -8 | -19 |
| HAQ-DI¶ score | ||
| Sample Size | 165 | 159 |
| Baseline | 1.2 | 1.2 |
| Mean Change at Week 16 | -0.09 | -0.2 |
| CRP# | ||
| Sample Size | 166 | 167 |
| Baseline | 1.1 | 0.8 |
| Mean Change at Week 16 | 0.1 | -0.1 |
Treatment with OTEZLA resulted in improvement in dactylitis and enthesitis in subjects with pre-existing dactylitis or enthesitis.
14.2 Moderate to Severe Plaque Psoriasis
Two multicenter, randomized, double-blind, placebo-controlled trials (PSOR-1 [NCT01194219] and PSOR-2 [NCT01232283]) enrolled a total of 1257 subjects 18 years of age and older with moderate to severe plaque psoriasis [body surface area (BSA) involvement of ≥ 10%, static Physician Global Assessment (sPGA) of ≥ 3 (moderate or severe disease), Psoriasis Area and Severity Index (PASI) score ≥ 12, candidates for phototherapy or systemic therapy]. Subjects were allowed to use low-potency topical corticosteroids on the face, axilla and groin. Subjects with plaque psoriasis of the scalp were allowed to use coal tar shampoo and/or salicylic acid scalp preparations on scalp lesions.
Trial PSOR-1 enrolled 844 subjects and Trial PSOR-2 enrolled 413 subjects. In both trials, subjects were randomized 2:1 to OTEZLA 30 mg twice daily (BID) or placebo for 16 weeks. Both trials assessed the proportion of subjects who achieved PASI-75 at Week 16 and the proportion of subjects who achieved an sPGA score of clear (0) or almost clear (1) at Week 16. Across both trials, subjects ranged in age from 18 to 83 years, with an overall median age of 46 years. The mean baseline BSA involvement was 25.2% (median 21.0%), the mean baseline PASI score was 19.1 (median 16.8), and the proportion of subjects with an sPGA score of 3 (moderate) and 4 (severe) at baseline were 70.0% and 29.8%, respectively. Approximately 30% of all subjects had received prior phototherapy and 54% had received prior conventional systemic and/or biologic therapy for the treatment of psoriasis with 37% receiving prior conventional systemic therapy and 30% receiving prior biologic therapy. Approximately one-third of subjects had not received prior phototherapy, conventional systemic nor biologic therapy. A total of 18% of subjects had a history of psoriatic arthritis.
Clinical Response in Subjects with Moderate to Severe Plaque Psoriasis
The proportion of subjects who achieved PASI-75 responses, and an sPGA score of clear (0) or almost clear (1), are presented in Table 7.
| Trial PSOR-1 | Trial PSOR-2 | |||
|---|---|---|---|---|
| Placebo | OTEZLA 30 mg BID | Placebo | OTEZLA 30 mg BID* |
|
| N† | N = 282 | N = 562 | N = 137 | N = 274 |
|
||||
| PASI‡ -75, n (%) | 15 (5.3) | 186 (33.1) | 8 (5.8) | 79 (28.8) |
| sPGA§ of Clear or Almost Clear, n (%) | 11 (3.9) | 122 (21.7) | 6 (4.4) | 56 (20.4) |
The median time to loss of PASI-75 response among the subjects re-randomized to placebo at Week 32 during the Randomized Treatment Withdrawal Phase was 5.1 weeks.
Plaque Psoriasis Involving the Scalp Area
A randomized, double-blind, placebo-controlled trial (PSOR-3 [NCT03123471]) was conducted in 303 adult subjects with moderate to severe plaque psoriasis of the scalp. Enrolled subjects had a Scalp Physician Global Assessment (ScPGA) score of ≥ 3, Scalp Surface Area (SSA) involvement of ≥ 20%, an inadequate response or intolerance to at least one topical therapy for plaque psoriasis of the scalp, and moderate to severe plaque psoriasis (BSA involvement of ≥ 10%, sPGA of ≥ 3 [moderate or severe disease], and PASI score ≥ 12).
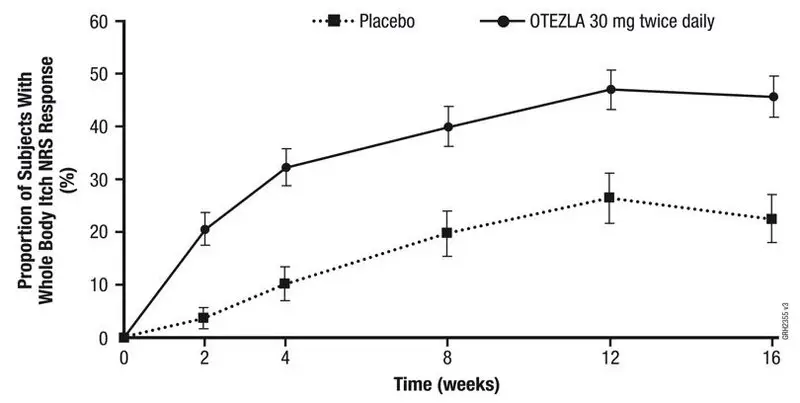
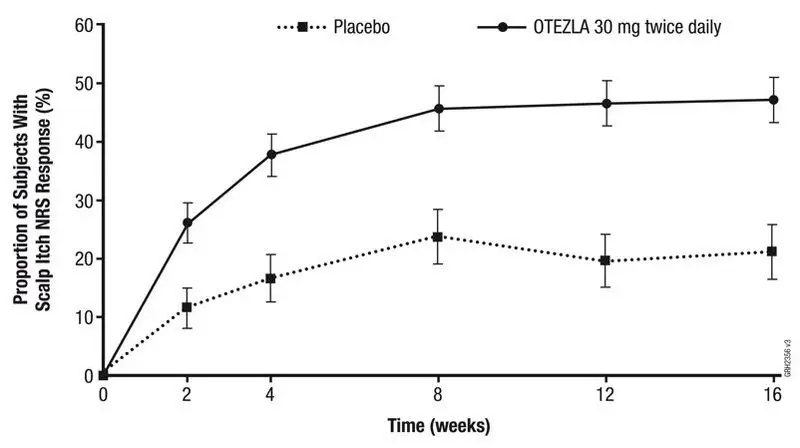
Subjects were randomized 2:1 to receive either OTEZLA 30 mg twice daily (n =201) or placebo twice daily (n = 102) for 16 weeks. The primary endpoint was the proportion of subjects who achieved an ScPGA response at Week 16 (defined as ScPGA score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline at Week 16). Secondary endpoints included the proportion of subjects with Whole Body Itch Numeric Rating Scale (NRS) response (defined as ≥ 4-point reduction from baseline) and the proportion of subjects with a Scalp Itch NRS response (defined as ≥ 4-point reduction from baseline).
Subjects had a mean age of 46.9 years, 61.7% were men and 75.6 % were white. At baseline, 76.9% of subjects had moderate plaque psoriasis of the scalp (ScPGA of 3), 23.1% had severe plaque psoriasis of the scalp (ScPGA of 4), 71.6% of subjects were biologic naïve, and 58.8% had failed 1 or 2 topical treatments. At baseline, the mean Whole Body Itch NRS score was 7.2 and the mean Scalp Itch NRS score was 6.7 with the scales ranging from 0 to 10. The mean baseline SSA involvement was 60.6% and the mean baseline BSA involvement was 19.8%.
The proportion of subjects who achieved an ScPGA response, Whole Body Itch NRS response, and Scalp Itch NRS response at Week 16 are presented in Table 8.
Figure 1 displays the proportion of subjects achieving Whole Body Itch NRS response at each visit, while Figure 2 displays the proportion of subjects achieving Scalp Itch NRS response at each visit.
| Trial PSOR-3 | |||
|---|---|---|---|
| Placebo | OTEZLA 30 mg twice daily | Treatment Difference*,†
(95% CI‡) |
|
|
|||
| Number of subjects randomized | N = 102 | N = 201 | |
| ScPGA response§ | 13.7% | 43.3% | 29.6% (19.5%, 39.7%) |
| Number of subjects with baseline Whole Body Itch NRS Score ≥4 | N = 94 | N = 185 | |
| Whole Body Itch NRS response | 22.5% | 45.5% | 23.0% (11.5%, 34.6%) |
| Number of subjects with baseline Scalp Itch NRS Score ≥4 | N = 90 | N = 175 | |
| Scalp Itch NRS response | 21.1% | 47.1% | 26.2% (13.9%, 38.5%) |
| NRS = Numeric Rating Scale; SE = standard error |
| Figure 1: Proportion (± SE) of Subjects Achieving Whole Body Itch NRS Response through Week 16 |
 |
| NRS = Numeric Rating Scale; SE = standard error |
| Figure 2: Proportion (± SE) of Subjects Achieving Scalp Itch NRS Response through Week 16 |
 |
Plaque Psoriasis Involving the Genital Area
A randomized, double-blind, placebo-controlled trial (PSOR-5 [NCT03777436]) was conducted in 289 adult subjects with moderate to severe plaque psoriasis of the genital area. Subjects had a modified static Physician Global Assessment of Genitalia (sPGA-G) score of ≥ 3 (moderate or severe), sPGA score of ≥ 3 (moderate or severe), and had an inadequate response or were intolerant to topical therapy for the treatment of plaque psoriasis of the genital area.
Subjects were randomized 1:1 to receive either apremilast 30 mg twice daily (n = 143) or placebo twice daily (n = 146) for 16 weeks. At Week 16, the placebo group was switched to receive OTEZLA and the OTEZLA group remained on drug through Week 32. The primary endpoint was the proportion of subjects who achieved a modified sPGA-G response (defined as a score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline) at Week 16. Secondary endpoints included the proportion of subjects who achieved an sPGA response (defined as a score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline) at Week 16 and the proportion of subjects who achieved at least a 4-point improvement in the 11-point Genital Psoriasis Itch Numeric Rating Scale (GPI-NRS) item score within the Genital Psoriasis Symptoms Scale (GPSS) at Week 16, among subjects with a baseline GPI-NRS score of ≥ 4.
Subjects ranged in age from 18-81 years, with a median age of 44 years. The proportions of subjects with a modified sPGA-G score of 3 (moderate) and 4 (severe) at baseline were 86.9% and 13.1%, respectively. The proportions of subjects with a sPGA score of 3 (moderate) and 4 (severe) at baseline were 88.6% and 11.1%, respectively. Baseline BSA involvement was < 10% for 57.4% of the subjects and ≥ 10% for 42.6% of the subjects. The mean baseline GPI-NRS score was 6.5. Of the enrolled subjects, 78.9% did not receive prior conventional systemic therapy and 84.4% were biologic-naïve.
The proportions of subjects who achieved a modified sPGA-G response, sPGA response, and GPI-NRS response are presented in Table 9.
| Trial PSOR-5 | |||
|---|---|---|---|
| Placebo | OTEZLA 30 mg twice daily | Treatment Difference*,†
(95% CI)‡ |
|
|
|||
| Number of Subjects Randomized | N = 146 | N = 143 | |
| Modified sPGA-G Response§ | 19.5% | 39.6% | 20.1% (9.2%, 30.9%) |
| sPGA Response¶ | 6.9% | 22.2% | 15.2% (6.9%, 23.6%) |
| Number of Subjects with Baseline GPI-NRS Score ≥ 4 | N = 121 | N = 122 | |
| GPI-NRS Response# | 19.6% | 47.3% | 27.4% (15.4%, 39.3%) |
14.3 Mild to Moderate Plaque Psoriasis
A multicenter, randomized, double-blind, placebo-controlled trial (PSOR-4 [NCT03721172]) was conducted in 595 adult subjects with mild to moderate plaque psoriasis (BSA involvement of 2-15%, sPGA score of 2-3 [mild or moderate disease], and PASI score of 2–15). Enrolled subjects had an inadequate response or were intolerant to at least one topical therapy and had not received prior biologic therapy. Subjects were allowed to use unmedicated emollients for lesions on non-scalp areas of the body and non-medicated shampoos for lesions on the scalp.
Subjects were randomized 1:1 to receive either OTEZLA 30 mg twice daily (n = 297) or placebo twice daily (n = 298) for 16 weeks. At Week 16, the placebo group was switched to receive OTEZLA and the OTEZLA group remained on drug through Week 32. The primary endpoint was the proportion of subjects who achieved an sPGA response (defined as an sPGA score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline) at Week 16. Subjects with mild disease (sPGA = 2 at baseline) were required to be clear (sPGA = 0) to achieve an sPGA response. Other evaluated endpoints include the proportion of subjects with a Whole Body Itch NRS response (defined as a ≥ 4-point reduction from baseline) at Week 16 among subjects with a baseline Whole Body Itch NRS ≥ 4 and the proportion of subjects with an ScPGA response (defined as an ScPGA score of clear [0] or almost clear [1] with at least a 2-point reduction from baseline) at Week 16 among subjects with a baseline ScPGA score ≥ 2.
Subjects ranged in age from 18 to 85 years, with an overall median age of 50 years. The mean baseline BSA involvement was 6.4%, the mean baseline PASI score was 6.5, and the proportions of subjects with an sPGA score of 2 (mild) and 3 (moderate) at baseline were 30.6% and 69.4%, respectively.
Clinical Response in Subjects with Mild to Moderate Plaque Psoriasis
The proportions of subjects who achieved an sPGA response, Whole Body Itch NRS response, and an ScPGA response at Week 16 are presented in Table 10.
| Trial PSOR-4 | |||
|---|---|---|---|
| Placebo | OTEZLA 30 mg twice daily | Treatment Difference*,†
(95% CI‡) |
|
|
|||
| Number of Subjects Randomized | N = 298 | N = 297 | |
| sPGA Response§ | 4.1% | 21.6% | 17.5% (12.2%, 22.8%) |
| Number of Subjects with Baseline Whole Body Itch NRS Score ≥ 4 | N = 249 | N = 253 | |
| Whole Body Itch NRS Response¶ | 18.6% | 43.2% | 24.7% (16.5%, 32.8%) |
| Number of Subjects with Baseline ScPGA Score ≥ 2 | N = 199 | N = 212 | |
| ScPGA Response# | 16.6% | 44.0% | 27.4% (18.6%, 36.3%) |
14.4 Oral Ulcers Associated with Behçet's Disease
A multicenter, randomized, placebo-controlled trial (BCT-002 [NCT02307513]) enrolled a total of 207 adult subjects with BD with active oral ulcers. Subjects were previously treated with at least one nonbiologic BD medication and were candidates for systemic therapy. Subjects met the International Study Group (ISG) Criteria for BD. Subjects had at least 2 oral ulcers at screening and at least 2 oral ulcers at randomization and without currently active major organ involvement. Concomitant treatment for BD was not allowed.
Subjects were randomized 1:1 to receive either OTEZLA 30 mg twice daily (n = 104) or placebo (n = 103) for 12 weeks. After Week 12, all subjects received OTEZLA 30 mg twice daily.
Efficacy was assessed based on the number and pain of oral ulcers.
Subjects ranged in age from 19 to 72 years, with a mean age of 40 years. The mean duration of BD was 6.84 years. All subjects had a history of recurrent oral ulcers that were currently active. Subjects had a history of skin lesions (98.6%), genital ulcers (90.3%), musculoskeletal manifestations (72.5%), ocular manifestations (17.4%), central nervous system (9.7%), gastrointestinal (GI) manifestations (9.2%) and vascular involvement (1.4%). The mean baseline oral ulcer counts were 4.2 and 3.9 in the OTEZLA and placebo groups, respectively.
Measures of Oral Ulcers
Improvements in measures of oral ulcers at Week 12 are presented in Table 11.
| Endpoint | Placebo N = 103 | OTEZLA 30 mg twice daily N = 104 | Treatment Difference†
(95% CI‡) |
|---|---|---|---|
|
|||
| Change§ from baseline in the pain of oral ulcers as measured by VAS¶ at Week 12 | −18.7 | −42.7 | −24.1 (−32.4, −15.7) |
| Proportion# of subjects achieving oral ulcer complete response (oral ulcer-free) at Week 12 | 22.3% | 52.9% | 30.6%Þ
(18.1%, 43.1%) |
| Proportion# of subjects achieving oral ulcer complete response (oral ulcer-free) by Week 6, and who remained oral ulcer-free for at least 6 additional weeks during the 12-week Placebo-controlled Treatment Phase | 4.9% | 29.8% | 25.1%Þ
(15.5%, 34.6%) |
| Daily averageß,à number of oral ulcers during the 12-week Placebo-controlled Treatment Phase | 2.6 | 1.5 | −1.1 (−1.6, −0.7) |
Figure 3 displays the mean number of oral ulcers for each treatment group at each visit, while Figure 4 displays the mean oral ulcer pain on a visual analog scale for each treatment group at each visit.
| ITT = intent-to-treat; SE = standard error | ||||||||
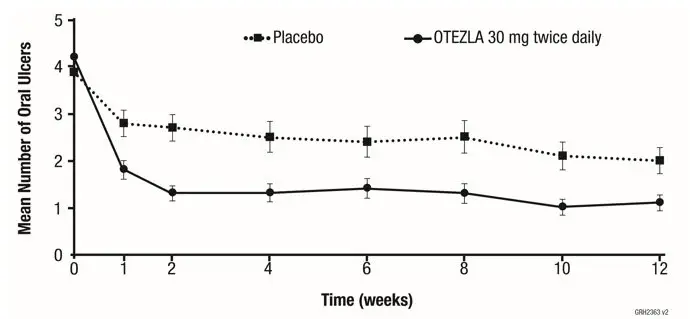 |
||||||||
| Weeks | 0 | 1 | 2 | 4 | 6 | 8 | 10 | 12 |
| Placebo, n | 103 | 98 | 97 | 93 | 91 | 86 | 83 | 82 |
| OTEZLA 30 mg twice daily, n | 104 | 101 | 101 | 101 | 98 | 94 | 94 | 97 |
| ITT = intent-to-treat; SE = standard error. Oral ulcer pain was assessed on a 100-mm Visual Analog Scale with 0 = no pain and 100 = worst possible pain. Mean baseline Visual Analog Scale pain scores were 61.2 and 60.8 in the OTEZLA 30 mg twice daily treatment group and placebo treatment group, respectively. |
||||||||
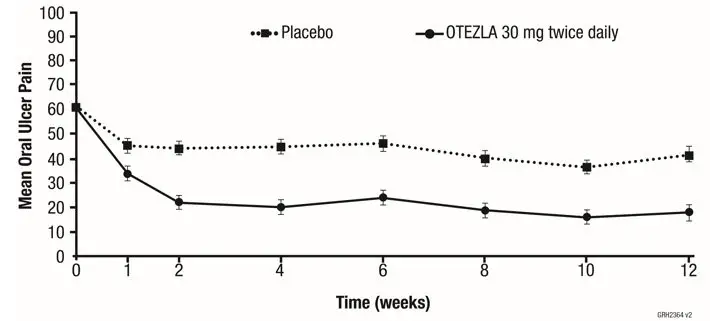 |
||||||||
| Weeks | 0 | 1 | 2 | 4 | 6 | 8 | 10 | 12 |
| Placebo, n | 101 | 95 | 96 | 91 | 90 | 85 | 82 | 81 |
| OTEZLA 30 mg twice daily, n | 102 | 95 | 97 | 99 | 97 | 92 | 93 | 95 |
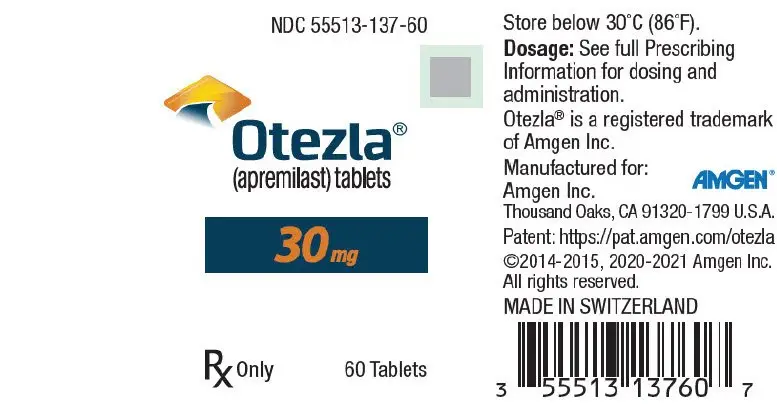
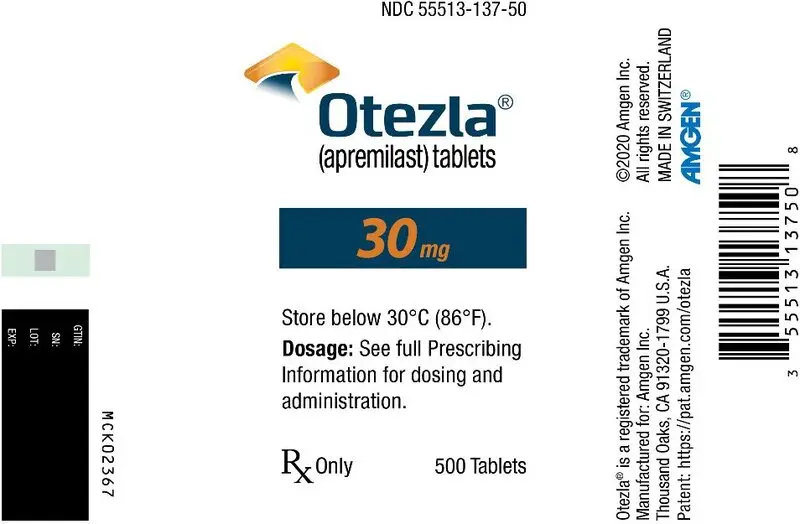
16. How is Otezla supplied
OTEZLA is available as diamond-shaped, film-coated tablets in the following dosage strengths: 10-mg pink tablet engraved with "APR" on one side and "10" on the other side; 20-mg brown tablet engraved with "APR" on one side and "20" on the other side; 30-mg beige tablet engraved with "APR" on one side and "30" on the other side.
Tablets are supplied in the following strengths and package configurations:
| Package configuration | Tablet strength | NDC number |
|---|---|---|
| Bottles of 60 | 30 mg | 55513-137-60 |
| 28-day starter pack | 13-tablet blister titration pack containing: (4) 10-mg, (4) 20-mg, and (5) 30-mg tablets with an additional (42) 30-mg tablets | 55513-369-55 |
| OTEZLA
apremilast tablet, film coated |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| OTEZLA
apremilast kit |
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
| OTEZLA
apremilast kit |
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
| Labeler - Amgen Inc (039976196) |