Drug Detail:Pazeo (Olopatadine ophthalmic [ oh-loe-pat-a-deen ])
Drug Class: Ophthalmic antihistamines and decongestants
Highlights of Prescribing Information
PAZEO (olopatadine hydrochloride ophthalmic solution) 0.7%
For topical ophthalmic administration.
Initial U.S. Approval: 1996
Indications and Usage for Pazeo
PAZEO is a mast cell stabilizer indicated for the treatment of ocular itching associated with allergic conjunctivitis. (1).
Pazeo Dosage and Administration
The recommended dose is one drop in each affected eye once a day. (2)
Dosage Forms and Strengths
Ophthalmic solution: 7.76 mg of olopatadine hydrochloride in one mL of solution (0.7%) in a four mL bottle. (3)
Contraindications
None. (4)
Warnings and Precautions
Contamination of Tip and Solution. To prevent contaminating the dropper tip and solution, do not touch the eyelids or surrounding areas with the dropper tip of the bottle. (5.1)
Adverse Reactions/Side Effects
The most common adverse reactions (2-5%) were blurred vision, superficial punctate keratitis, dry eye, abnormal sensation in eye, and dysgeusia. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Alcon Laboratories, Inc. at 1-800-757-9195 or FDA at
1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 4/2017
Related/similar drugs
ketorolac ophthalmic, Pataday, olopatadine ophthalmic, Lotemax, Patanol, AlrexFull Prescribing Information
1. Indications and Usage for Pazeo
PAZEO is indicated for the treatment of ocular itching associated with allergic conjunctivitis.
2. Pazeo Dosage and Administration
The recommended dosage of PAZEO is to instill one drop in each affected eye once a day.
3. Dosage Forms and Strengths
Ophthalmic solution: 7.76 mg of olopatadine hydrochloride in one mL solution (0.7%) in a 4 mL bottle.
5. Warnings and Precautions
5.1 CONTAMINATION OF TIP AND SOLUTION
As with any eye drop, care should be taken not to touch the eyelids or surrounding areas with the dropper tip of the bottle to prevent contaminating the tip and solution. Keep bottle tightly closed when not in use.
5.2 CONTACT LENS USE
Patients should not wear a contact lens if their eye is red. The preservative in PAZEO solution, benzalkonium chloride, may be absorbed by soft contact lenses. Patients who wear soft contact lenses and whose eyes are not red, should be instructed to wait at least five minutes after instilling PAZEO before they insert their contact lenses.
6. Adverse Reactions/Side Effects
6.1 CLINICAL TRIALS EXPERIENCE
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In a randomized, double-masked, vehicle-controlled trial, patients at risk for developing allergic conjunctivitis received one drop of either PAZEO (N=330) or vehicle (N=169) in both eyes for 6 weeks. The mean age of the population was 32 years (range 2 to 74 years). Thirty-five percent were male. Fifty-three percent had brown iris color and 23% had blue iris color. The most commonly reported adverse reactions occurred in 2-5% of patients treated with either PAZEO or vehicle. These events were blurred vision, dry eye, superficial punctate keratitis, dysgeusia and abnormal sensation in eye.
8. Use In Specific Populations
8.1 PREGNANCY
Risk Summary
There are no adequate or well-controlled studies with PAZEO in pregnant women. Olopatadine caused maternal toxicity and embryofetal toxicity in rats at levels 1,080 to 14,400 times the maximum recommended human ophthalmic dose (MRHOD). There was no toxicity in rat offspring at exposures estimated to be 45 to 150 times that at MRHOD. Olopatadine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Animal Data
In a rabbit embryofetal study, rabbits treated orally at 400 mg/kg/day during organogenesis showed a decrease in live fetuses. This dose is 14,400 times the MRHOD, on a mg/m2 basis.
An oral dose of 600 mg/kg/day olopatadine (10,800 times the MRHOD) was shown to be maternally toxic in rats, producing death and reduced maternal body weight gain. When administered to rats throughout organogenesis, olopatadine produced cleft palate at 60 mg/kg/day (1080 times the MRHOD) and decreased embryofetal viability and reduced fetal weight in rats at 600 mg/kg/day. When administered to rats during late gestation and throughout the lactation period, olopatadine produced decreased neonatal survival at 60 mg/kg/day and reduced body weight gain in offspring at 4 mg/kg/day. A dose of 2 mg/kg/day olopatadine produced no toxicity in rat offspring. An oral dose of 1 mg/kg olopatadine in rats resulted in a range of systemic plasma area under the curve (AUC) levels that were 45 to 150 times higher than the observed human exposure [9.7 ng∙hr/mL] following administration of the recommended human ophthalmic dose.
8.3 NURSING MOTHERS
Olopatadine has been identified in the milk of nursing rats following oral administration. Oral administration of olopatadine doses at or above 4 mg/kg/day throughout the lactation period produced decreased body weight gain in rat offspring; a dose of 2 mg/kg/day olopatadine produced no toxicity. An oral dose of 1 mg/kg olopatadine in rats resulted in a range of systemic plasma area under the curve (AUC) levels that were 45 to 150 times higher than the observed human exposure [9.7 ng∙hr/mL] following administration of the recommended human ophthalmic dose. It is not known whether topical ocular administration could result in sufficient systemic absorption to produce detectable quantities in the human breast milk. Nevertheless, caution should be exercised when PAZEO is administered to a nursing mother.
8.4 PEDIATRIC USE
The safety and effectiveness of PAZEO have been established in pediatric patients two years of age and older. Use of PAZEO in these pediatric patients is supported by evidence from adequate and well-controlled studies of PAZEO in adults and an adequate and well controlled study evaluating the safety of PAZEO in pediatric and adult patients.
11. Pazeo Description
PAZEO is a sterile ophthalmic solution containing olopatadine, which is a mast cell stabilizer, for topical administration to the eyes. Olopatadine hydrochloride is a white, crystalline, water‑soluble powder with a molecular weight of 373.88 and a molecular formula of C21H23NO3•HCl.
The chemical structure is presented below:
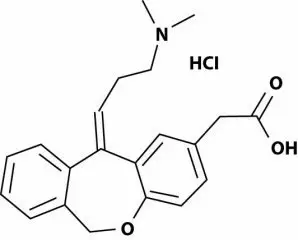
Chemical Name: 11-[(Z)-3(dimethylamino) propylidene]-6-11dihydrodibenz[b,e] oxepin-2-acetic acid, hydrochloride.
Each mL of PAZEO solution contains an active ingredient [7.76 mg of olopatadine hydrochloride (7 mg olopatadine)] and the following inactive ingredients: povidone; hydroxypropyl-gamma-cyclodextrin; polyethylene glycol 400; hypromellose; boric acid; mannitol; benzalkonium chloride 0.015% (preservative); hydrochloric acid/sodium hydroxide (to adjust pH); and purified water.
PAZEO solution has a pH of approximately 7.2 and an osmolality of approximately 300 mOsm/kg.
12. Pazeo - Clinical Pharmacology
12.1 MECHANISM OF ACTION
Olopatadine is a mast cell stabilizer and a histamine H1 antagonist. Decreased chemotaxis and inhibition of eosinophil activation has also been demonstrated.
12.3 PHARMACOKINETICS
In healthy subjects, topical ocular dosing of 1 drop of PAZEO once daily for 7 days into both eyes resulted in mean ± SD (range) steady state plasma olopatadine Cmax and AUC0-12 of 1.6 ± 0.9 ng/mL (0.6 to 4.5 ng/mL) and 9.7 ± 4.4 ng*h/mL (3.7 to 21.2 ng*h/mL), respectively. The olopatadine Cmax and AUC0-12 after the first dose were similar to those measured on day 7 in these subjects, suggesting that there was no systemic accumulation of olopatadine after repeated topical ocular dosing with PAZEO. The median (range) time to achieve peak olopatadine concentrations (Tmax) was 2.0 hours (0.25 to 4 hours). The mean ± SD (range) elimination half‑life of olopatadine was 3.4 ± 1.2 hours (2 to 8 hours). N-oxide olopatadine (M3) was detected during the first 4 hours after bilateral topical ocular dosing of PAZEO in approximately half of the subjects and in less than 10% of the total plasma samples collected, at concentrations not exceeding 0.121 ng/mL on day 1 and 0.174 ng/mL on day 7. None of the plasma samples from these subjects had mono-desmethyl olopatadine (M1) concentrations that were above the lower limit of quantitation (0.05 ng/mL) of the PK assay.
13. Nonclinical Toxicology
13.1 CARCINOGENESIS, MUTAGENESIS, IMPAIRMENT OF FERTILITY
Carcinogenicity
Olopatadine administered orally was not carcinogenic in mice and rats in doses up to 500 mg/kg/day and 200 mg/kg/day, respectively. Based on a 35 μL drop size and a 60 kg person, these doses are approximately 4,500 and 3,600 times the MRHOD, on a mg/m2 basis.
Mutagenesis
No mutagenic potential was observed when olopatadine was tested in an in vitro bacterial reverse mutation (Ames) test, an in vitro mammalian chromosome aberration assay or an in vivo mouse micronucleus test.
Impairment of fertility
Olopatadine administered at an oral dose of 400 mg/kg/day (approximately 7,200 times the MRHOD) produced toxicity in male and female rats, and resulted in a decrease in the fertility index and reduced implantation rate. No effects on reproductive function were observed at 50 mg/kg/day (approximately 900 times the MRHOD).
14. Clinical Studies
The efficacy of PAZEO was established in two randomized, double-masked, placebo-controlled, conjunctival allergen challenge (CAC) clinical studies in patients with a history of allergic conjunctivitis (Studies 1 and 2).
In Study 1, patients were randomized to receive one of the following study treatments: PAZEO, PATADAY, or vehicle ophthalmic solutions. In Study 2, patients were randomized to receive one of the following study treatments: PAZEO, PATADAY, PATANOL, or vehicle ophthalmic solutions.
Patients were evaluated with an ocular itching severity score ranging from 0 (no itching) to 4 (incapacitating itch) at several time points after CAC administration. Table 1 displays the mean ocular itching severity scores after ocular administration of a specific antigen using the CAC model in Studies 1 and 2, respectively. A one unit difference compared to vehicle is considered a clinically meaningful change in the ocular itching severity score.
PAZEO demonstrated statistically significantly improved relief of ocular itching compared to vehicle at 30-34 minutes, 16 hours, and 24 hours after study treatment. PAZEO demonstrated statistically significantly improved relief of ocular itching compared to PATADAY at 24 hours after study treatment, but not at 30-34 minutes after study treatment.
| Time Point | PAZEO (Olopatadine, 0.7%) | PATADAY (Olopatadine, 0.2%) | Vehicle | |||
|---|---|---|---|---|---|---|
| Study 1 | (N = 66) | (N = 68) | (N = 68) | |||
| Mean | Mean | Difference (95% CI) | Mean | Difference (95% CI) |
||
| Onset | 3 mins | 0.36 | 0.39 |
-0.02 | 1.90 |
-1.54 |
| 5 mins | 0.53 | 0.61 | -0.08 (-0.39, 0.22) | 2.06 | -1.53 (-1.84, -1.22) |
|
| 7 mins | 0.48 | 0.61 | -0.13 (-0.44, 0.17) | 1.97 | -1.49 (-1.80, -1.18) |
|
| 16h | 3 mins | 0.70 | 0.87 | -0.17 (-0.44, 0.11) | 2.20 | -1.50 (-1.77, -1.23) |
| 5 mins | 0.79 | 1.04 | -0.24 (-0.55, 0.07) | 2.27 | -1.48 (-1.79, -1.16) |
|
| 7 mins | 0.75 | 0.98 | -0.23 (-0.54, 0.08) | 2.13 | -1.38 (-1.69, -1.07) |
|
| 24h | 3 mins | 0.93 | 1.41 | -0.48 (-0.76, -0.20) | 2.54 | -1.61 (-1.88, -1.33) |
| 5 mins | 1.10 | 1.52 | -0.42 (-0.72, -0.12) | 2.62 | -1.51 (-1.81, -1.21) |
|
| 7 mins | 1.09 | 1.50 |
-0.41 | 2.50 | -1.41 (-1.72, -1.11) |
|
| Study 2 | (N = 98) | (N = 99) | (N = 49) | |||
| Onset | 3 mins | 0.38 | 0.47 | -0.09 (-0.28, 0.09) | 1.91 | -1.53 (-1.76, -1.30) |
| 5 mins | 0.53 | 0.61 | -0.08 (-0.29, 0.12) | 1.99 | -1.46 (-1.71, -1.22) |
|
| 7 mins | 0.65 | 0.61 | 0.04 (-0.18, 0.26) | 1.82 | -1.17 (-1.45, -0.90) |
|
| 24h | 3 mins | 1.01 | 1.33 | -0.31 (-0.57, -0.06) | 2.30 | -1.29 (-1.60, -0.97) |
| 5 mins | 1.22 | 1.48 | -0.26 (-0.51, -0.01) | 2.37 | -1.15 (-1.46, -0.84) |
|
| 7 mins | 1.25 | 1.41 | -0.16 (-0.42, 0.11) | 2.14 | -0.89 (-1.22, -0.57) |
|
*Mean score estimates, treatment differences and corresponding 95% confidence intervals (CIs) were based on analysis of repeated measures using a mixed model with itching scores from each eye (left or right) as the dependent variable and fixed effect terms for investigator, treatment, eye-type (left or right), time, and treatment-by-time interaction;
The ocular itching score range is 0-4, where 0 is none and 4 is incapacitating itch.
16. How is Pazeo supplied
PAZEO (olopatadine hydrochloride ophthalmic solution) 0.7% is supplied in a white, oval, low density polyethylene DROP-TAINER*dispenser with a natural low density polyethylene dispensing plug and a white polypropylene cap. Tamper evidence is provided with a shrink band around the closure and neck area of the package. PAZEO is supplied in a 4 mL bottle that contains 2.5 mL of olopatadine hydrochloride ophthalmic solution [7.76 mg of olopatadine hydrochloride in one mL of solution (0.7%)].
NDC 0065-4273-25
Storage: Store at 2°C to 25°C (36°F to 77°F). Keep bottle tightly closed when not in use.
17. Patient Counseling Information
-
Risk of Contamination: Advise patients to not touch dropper tip to eyelids or surrounding areas, as this may contaminate the dropper tip and ophthalmic solution.
- Concomitant Use of Contact Lenses: Advise patients not to wear contact lenses if their eyes are red. Advise patients that PAZEO should not be used to treat contact lens‑related irritation. Advise patients to remove contact lenses prior to instillation of PAZEO. The preservative in PAZEO solution, benzalkonium chloride, may be absorbed by soft contact lenses. Lenses may be reinserted 5 minutes following administration of PAZEO.
U.S. Pat.:www.alconpatents.com
ALCON®
ALCON LABORATORIES, INC.
Fort Worth, Texas 76134 USA
© 2015, 2016 Novartis.
* a Trademark of Novartis
| PAZEO
olopatadine hydrochloride solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - Alcon Laboratories, Inc. (008018525) |





