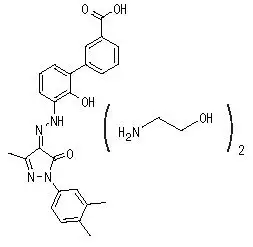
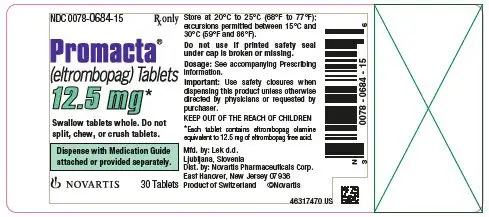
Drug Detail:Promacta (Eltrombopag [ el-trom-boe-pag ])
Drug Class: Platelet-stimulating agents
Highlights of Prescribing Information
PROMACTA® (eltrombopag) tablets, for oral use
PROMACTA® (eltrombopag) for oral suspension
Initial U.S. Approval: 2008
WARNING: RISK FOR HEPATIC DECOMPENSATION IN PATIENTS WITH CHRONIC HEPATITIS C and RISK OF HEPATOTOXICITY
See full prescribing information for complete boxed warning.
In patients with chronic hepatitis C, PROMACTA in combination with interferon and ribavirin may increase the risk of hepatic decompensation. (5.1)
PROMACTA may increase the risk of severe and potentially life-threatening hepatotoxicity. Monitor hepatic function and discontinue dosing as recommended. (5.2)
Indications and Usage for Promacta
PROMACTA is a thrombopoietin receptor agonist indicated:
- for the treatment of thrombocytopenia in adult and pediatric patients 1 year and older with persistent or chronic immune thrombocytopenia (ITP) who have had an insufficient response to corticosteroids, immunoglobulins, or splenectomy. PROMACTA should be used only in patients with ITP whose degree of thrombocytopenia and clinical condition increase the risk for bleeding. (1.1)
- for the treatment of thrombocytopenia in patients with chronic hepatitis C to allow the initiation and maintenance of interferon-based therapy. PROMACTA should be used only in patients with chronic hepatitis C whose degree of thrombocytopenia prevents the initiation of interferon-based therapy or limits the ability to maintain interferon-based therapy. (1.2)
- in combination with standard immunosuppressive therapy for the first-line treatment of adult and pediatric patients 2 years and older with severe aplastic anemia. (1.3)
- for the treatment of patients with severe aplastic anemia who have had an insufficient response to immunosuppressive therapy. (1.3)
Limitations of Use:
- PROMACTA is not indicated for the treatment of patients with myelodysplastic syndrome (MDS). (1.4)
- Safety and efficacy have not been established in combination with direct-acting antiviral agents used without interferon for treatment of chronic hepatitis C infection. (1.4)
Promacta Dosage and Administration
- Take PROMACTA without a meal or with a meal low in calcium (≤ 50 mg). Take PROMACTA at least 2 hours before or 4 hours after any medications or products containing polyvalent cations, such as antacids, calcium-rich foods, and mineral supplements. (2.4, 7.1, 12.3)
- Persistent or Chronic ITP: Initiate PROMACTA at 50 mg once daily for most adult and pediatric patients 6 years and older, and at 25 mg once daily for pediatric patients aged 1 to 5 years. Dose reductions are needed for patients with hepatic impairment and some patients of East-/Southeast-Asian ancestry. Adjust to maintain platelet count greater than or equal to 50 x 109/L. Do not exceed 75 mg per day. (2.1, 8.6, 8.7)
- Chronic Hepatitis C-associated Thrombocytopenia: Initiate PROMACTA at 25 mg once daily for all patients. Adjust to achieve target platelet count required to initiate antiviral therapy. Do not exceed a daily dose of 100 mg. (2.2)
- First-line Severe Aplastic Anemia: Initiate PROMACTA once daily at 2.5 mg/kg (in pediatric patients aged 2 to 5 years old), 75 mg (pediatric patients aged 6 to 11 years old), or 150 mg for patients aged 12 years and older concurrently with standard immunosuppressive therapy. Reduce initial dose in patients of East-/Southeast-Asian ancestry. Modify dosage for toxicity or elevated platelet counts. (2.3, 8.7)
- Refractory Severe Aplastic Anemia: Initiate PROMACTA at 50 mg once daily. Reduce initial dose in patients with hepatic impairment or patients of East-/Southeast-Asian ancestry. Adjust to maintain platelet count greater than 50 x 109/L. Do not exceed 150 mg per day. (2.3, 8.6, 8.7)
Dosage Forms and Strengths
- Tablets: 12.5 mg, 25 mg, 50 mg, and 75 mg (3)
- For oral suspension: 12.5 mg and 25 mg (3)
Contraindications
None. (4)
Warnings and Precautions
- Hepatotoxicity: Monitor liver function before and during therapy. (5.2)
- Increased Risk of Death and Progression of Myelodysplastic Syndromes to Acute Myeloid Leukemia. (5.3)
- Thrombotic/Thromboembolic Complications: Portal vein thrombosis has been reported in patients with chronic liver disease receiving PROMACTA. Monitor platelet counts regularly. (5.4)
Adverse Reactions/Side Effects
Across all indications, the most common adverse reactions (≥ 20% in any indication) were: anemia, nausea, pyrexia, alanine aminotransferase increased, cough, fatigue, headache, and diarrhea. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Novartis Pharmaceuticals Corporation at 1-888-669-6682 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Use In Specific Populations
- Lactation: Advise women not to breastfeed during treatment. (8.2)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 3/2023
Related/similar drugs
prednisone, dexamethasone, triamcinolone, Decadron, Deltasone, Kenalog-40, DopteletFull Prescribing Information
1. Indications and Usage for Promacta
1.1 Treatment of Thrombocytopenia in Patients With Persistent or Chronic Immune Thrombocytopenia
PROMACTA is indicated for the treatment of thrombocytopenia in adult and pediatric patients 1 year and older with persistent or chronic immune thrombocytopenia (ITP) who have had an insufficient response to corticosteroids, immunoglobulins, or splenectomy. PROMACTA should be used only in patients with ITP whose degree of thrombocytopenia and clinical condition increase the risk for bleeding.
1.2 Treatment of Thrombocytopenia in Patients With Hepatitis C Infection
PROMACTA is indicated for the treatment of thrombocytopenia in patients with chronic hepatitis C to allow the initiation and maintenance of interferon-based therapy. PROMACTA should be used only in patients with chronic hepatitis C whose degree of thrombocytopenia prevents the initiation of interferon-based therapy or limits the ability to maintain interferon-based therapy.
1.3 Treatment of Severe Aplastic Anemia
- PROMACTA is indicated in combination with standard immunosuppressive therapy (IST) for the first-line treatment of adult and pediatric patients 2 years and older with severe aplastic anemia.
- PROMACTA is indicated for the treatment of patients with severe aplastic anemia who have had an insufficient response to immunosuppressive therapy.
1.4 Limitations of Use
- PROMACTA is not indicated for the treatment of patients with myelodysplastic syndromes (MDS) [see Warnings and Precautions (5.3)].
- Safety and efficacy have not been established in combination with direct-acting antiviral agents used without interferon for treatment of chronic hepatitis C infection.
2. Promacta Dosage and Administration
2.1 Persistent or Chronic Immune Thrombocytopenia
Use the lowest dose of PROMACTA to achieve and maintain a platelet count greater than or equal to 50 x 109/L as necessary to reduce the risk for bleeding. Dose adjustments are based upon the platelet count response. Do not use PROMACTA to normalize platelet counts [see Warnings and Precautions (5.4)]. In clinical trials, platelet counts generally increased within 1 to 2 weeks after starting PROMACTA and decreased within 1 to 2 weeks after discontinuing PROMACTA [see Clinical Studies (14.1)].
Initial Dose Regimen:
Adult and Pediatric Patients 6 Years and Older with ITP: Initiate PROMACTA at a dose of 50 mg once daily, except in patients who are of East-/Southeast-Asian ancestry or who have mild to severe hepatic impairment (Child-Pugh class A, B, C).
For patients of East-/Southeast-Asian ancestry with ITP, initiate PROMACTA at a reduced dose of 25 mg once daily [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)].
For patients with ITP and mild, moderate, or severe hepatic impairment (Child-Pugh class A, B, C), initiate PROMACTA at a reduced dose of 25 mg once daily [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)].
For patients of East-/Southeast-Asian ancestry with ITP and hepatic impairment (Child-Pugh class A, B, C), consider initiating PROMACTA at a reduced dose of 12.5 mg once daily [see Clinical Pharmacology (12.3)].
Pediatric Patients with ITP Aged 1 to 5 Years: Initiate PROMACTA at a dose of 25 mg once daily [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)].
Monitoring and Dose Adjustment: After initiating PROMACTA, adjust the dose to achieve and maintain a platelet count greater than or equal to 50 x 109/L as necessary to reduce the risk for bleeding. Do not exceed a dose of 75 mg daily. Monitor clinical hematology and liver tests regularly throughout therapy with PROMACTA and modify the dosage regimen of PROMACTA based on platelet counts as outlined in Table 1. During therapy with PROMACTA, assess complete blood counts (CBCs) with differentials, including platelet counts, weekly until a stable platelet count has been achieved. Obtain CBCs with differentials, including platelet counts, monthly thereafter.
When switching between the oral suspension and tablet, assess platelet counts weekly for 2 weeks, and then follow standard monthly monitoring.
|
Platelet count result |
Dose adjustment or response |
|
< 50 x 109/L following at least 2 weeks of PROMACTA |
Increase daily dose by 25 mg to a maximum of 75 mg/day. For patients taking 12.5 mg once daily, increase the dose to 25 mg daily before increasing the dose amount by 25 mg. |
|
≥ 200 x 109/L to ≤ 400 x 109/L at any time |
Decrease the daily dose by 25 mg. Wait 2 weeks to assess the effects of this and any subsequent dose adjustments. For patients taking 25 mg once daily, decrease the dose to 12.5 mg once daily. |
|
> 400 x 109/L |
Stop PROMACTA; increase the frequency of platelet monitoring to twice weekly. Once the platelet count is < 150 x 109/L, reinitiate therapy at a daily dose reduced by 25 mg. For patients taking 25 mg once daily, reinitiate therapy at a daily dose of 12.5 mg. |
|
> 400 x 109/L after 2 weeks of therapy at lowest dose of PROMACTA |
Discontinue PROMACTA. |
In patients with ITP and hepatic impairment (Child-Pugh class A, B, C), after initiating PROMACTA or after any subsequent dosing increase, wait 3 weeks before increasing the dose.
Modify the dosage regimen of concomitant ITP medications, as medically appropriate, to avoid excessive increases in platelet counts during therapy with PROMACTA. Do not administer more than one dose of PROMACTA within any 24-hour period.
Discontinuation: Discontinue PROMACTA if the platelet count does not increase to a level sufficient to avoid clinically important bleeding after 4 weeks of therapy with PROMACTA at the maximum daily dose of 75 mg. Excessive platelet count responses, as outlined in Table 1, or important liver test abnormalities also necessitate discontinuation of PROMACTA [see Warnings and Precautions (5.2)]. Obtain CBCs with differentials, including platelet counts, weekly for at least 4 weeks following discontinuation of PROMACTA.
2.2 Chronic Hepatitis C-Associated Thrombocytopenia
Use the lowest dose of PROMACTA to achieve and maintain a platelet count necessary to initiate and maintain antiviral therapy with pegylated interferon and ribavirin. Dose adjustments are based upon the platelet count response. Do not use PROMACTA to normalize platelet counts [see Warnings and Precautions (5.4)]. In clinical trials, platelet counts generally began to rise within the first week of treatment with PROMACTA [see Clinical Studies (14.2)].
Initial Dose Regimen: Initiate PROMACTA at a dose of 25 mg once daily.
Monitoring and Dose Adjustment: Adjust the dose of PROMACTA in 25-mg increments every 2 weeks as necessary to achieve the target platelet count required to initiate antiviral therapy. Monitor platelet counts every week prior to starting antiviral therapy.
During antiviral therapy, adjust the dose of PROMACTA to avoid dose reductions of peginterferon. Monitor CBCs with differentials, including platelet counts, weekly during antiviral therapy until a stable platelet count is achieved. Monitor platelet counts monthly thereafter. Do not exceed a dose of 100 mg daily. Monitor clinical hematology and liver tests regularly throughout therapy with PROMACTA.
For specific dosage instructions for peginterferon or ribavirin, refer to their respective prescribing information.
|
Platelet count result |
Dose adjustment or response |
|
< 50 x 109/L following at least 2 weeks of PROMACTA |
Increase daily dose by 25 mg to a maximum of 100 mg/day. |
|
≥ 200 x 109/L to ≤ 400 x 109/L at any time |
Decrease the daily dose by 25 mg. Wait 2 weeks to assess the effects of this and any subsequent dose adjustments. |
|
> 400 x 109/L |
Stop PROMACTA; increase the frequency of platelet monitoring to twice weekly. Once the platelet count is < 150 x 109/L, reinitiate therapy at a daily dose reduced by 25 mg. For patients taking 25 mg once daily, reinitiate therapy at a daily dose of 12.5 mg. |
|
> 400 x 109/L after 2 weeks of therapy at lowest dose of PROMACTA |
Discontinue PROMACTA. |
Discontinuation: The prescribing information for pegylated interferon and ribavirin include recommendations for antiviral treatment discontinuation for treatment futility. Refer to pegylated interferon and ribavirin prescribing information for discontinuation recommendations for antiviral treatment futility.
PROMACTA should be discontinued when antiviral therapy is discontinued. Excessive platelet count responses, as outlined in Table 2, or important liver test abnormalities also necessitate discontinuation of PROMACTA [see Warnings and Precautions (5.2)].
2.3 Severe Aplastic Anemia
First-Line Severe Aplastic Anemia
Initiate PROMACTA concurrently with standard immunosuppressive therapy [see Clinical Studies (14.3)].
Initial Dose Regimen
The recommended initial dose regimen is listed in Table 3. Do not exceed the initial dose of PROMACTA.
|
Age |
Dose regimen |
|
Patients 12 years and older |
150 mg once daily for 6 months |
|
Pediatric patients 6 to 11 years |
75 mg once daily for 6 months |
|
Pediatric patients 2 to 5 years |
2.5 mg/kg once daily for 6 months |
For patients with severe aplastic anemia of East-/Southeast-Asian ancestry or those with mild, moderate, or severe hepatic impairment (Child-Pugh class A, B, C), decrease the initial PROMACTA dose by 50% as listed in Table 4 [see Use in Specific Populations (8.6, 8.7), Clinical Pharmacology (12.3)].
If baseline alanine aminotransferase (ALT) or aspartate aminotransferase (AST) levels are > 6 x upper limit of normal (ULN), do not initiate PROMACTA until transaminase levels are < 5 x ULN. Determine the initial dose for these patients based on Table 3 or Table 4.
|
Age |
Dose regimen |
|
Patients 12 years and older |
75 mg once daily for 6 months |
|
Pediatric patients 6 to 11 years |
37.5 mg once daily for 6 months |
|
Pediatric patients 2 to 5 years |
1.25 mg/kg once daily for 6 months |
Monitoring and Dose Adjustment for PROMACTA: Perform clinical hematology and liver tests regularly throughout therapy with PROMACTA [see Warnings and Precautions (5.2)].
Modify the dosage regimen of PROMACTA based on platelet counts as outlined in Table 5.
|
Platelet count result |
Dose adjustment or response |
|
> 200 x 109/L to ≤ 400 x 109/L |
Decrease the daily dose by 25 mg every 2 weeks to lowest dose that maintains platelet count ≥ 50 x 109/L. |
|
> 400 x 109/L |
Discontinue PROMACTA for one week. Once the platelet count is < 200 x 109/L, reinitiate PROMACTA at a daily dose reduced by 25 mg (or 12.5 mg in pediatric patients under 12 years of age). |
Table 6 summarizes the recommendations for dose interruption, reduction, or discontinuation of PROMACTA in the management of elevated liver transaminase levels and thromboembolic events.
| Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; ULN, upper limit of normal. | |
|
Event |
Recommendation |
|
ALT or AST elevations |
Increase in ALT or AST > 6 x ULN
Increase in ALT or AST > 6 x ULN after reinitiating PROMACTA
If ALT or AST returns to > 6 x ULN on the reduced dose
In pediatric patients under 12 years of age, reduce the daily dose by at least 15% to the nearest dose that can be administered. |
|
Thromboembolic events (e.g., deep vein thrombosis, pulmonary embolus, stroke, myocardial infarction) |
Discontinue PROMACTA but remain on horse antithymocyte globulin (h-ATG) and cyclosporine. |
The total duration of PROMACTA treatment is 6 months.
Refractory Severe Aplastic Anemia
Use the lowest dose of PROMACTA to achieve and maintain a hematologic response. Dose adjustments are based upon the platelet count. Hematologic response requires dose titration, generally up to 150 mg, and may take up to 16 weeks after starting PROMACTA [see Clinical Studies (14.3)].
Initial Dose Regimen: Initiate PROMACTA at a dose of 50 mg once daily.
For patients with severe aplastic anemia of East-/Southeast-Asian ancestry or those with mild, moderate, or severe hepatic impairment (Child-Pugh class A, B, C), initiate PROMACTA at a reduced dose of 25 mg once daily [see Use in Specific Populations (8.6, 8.7), Clinical Pharmacology (12.3)].
Monitoring and Dose Adjustment: Adjust the dose of PROMACTA in 50-mg increments every 2 weeks as necessary to achieve the target platelet count greater than or equal to 50 x 109/L as necessary. Do not exceed a dose of 150 mg daily. Monitor clinical hematology and liver tests regularly throughout therapy with PROMACTA and modify the dosage regimen of PROMACTA based on platelet counts as outlined in Table 7.
|
Platelet count result |
Dose adjustment or response |
|
< 50 x 109/L following at least 2 weeks of PROMACTA |
Increase daily dose by 50 mg to a maximum of 150 mg/day. For patients taking 25 mg once daily, increase the dose to 50 mg daily before increasing the dose amount by 50 mg. |
|
≥ 200 x 109/L to ≤ 400 x 109/L at any time |
Decrease the daily dose by 50 mg. Wait 2 weeks to assess the effects of this and any subsequent dose adjustments. |
|
> 400 x 109/L |
Stop PROMACTA for 1 week. Once the platelet count is < 150 x 109/L, reinitiate therapy at a dose reduced by 50 mg. |
|
> 400 x 109/L after 2 weeks of therapy at lowest dose of PROMACTA |
Discontinue PROMACTA. |
For patients who achieve tri-lineage response, including transfusion independence, lasting at least 8 weeks: the dose of PROMACTA may be reduced by 50% [see Clinical Studies (14.3)]. If counts remain stable after 8 weeks at the reduced dose, then discontinue PROMACTA and monitor blood counts. If platelet counts drop to less than 30 x 109/L, hemoglobin to less than 9 g/dL, or absolute neutrophil count (ANC) to less than 0.5 x 109/L, PROMACTA may be reinitiated at the previous effective dose.
Discontinuation: If no hematologic response has occurred after 16 weeks of therapy with PROMACTA, discontinue therapy. If new cytogenetic abnormalities are observed, consider discontinuation of PROMACTA [see Adverse Reactions (6.1)]. Excessive platelet count responses (as outlined in Table 7) or important liver test abnormalities also necessitate discontinuation of PROMACTA [see Warnings and Precautions (5.2)].
2.4 Administration
Administration of Tablets and Oral Suspension: Take PROMACTA without a meal or with a meal low in calcium (≤ 50 mg). Take PROMACTA at least 2 hours before or 4 hours after other medications (e.g., antacids), calcium-rich foods (containing > 50 mg calcium e.g., dairy products, calcium-fortified juices, and certain fruits and vegetables), or supplements containing polyvalent cations, such as iron, calcium, aluminum, magnesium, selenium, and zinc [see Drug Interactions (7.1), Clinical Pharmacology (12.3)].
Do not split, chew, or crush tablets and mix with food or liquids.
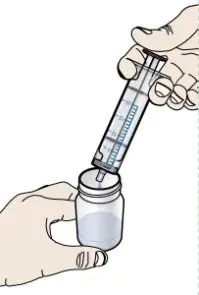
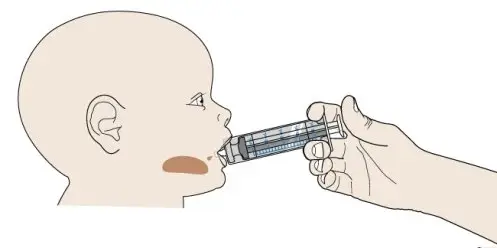
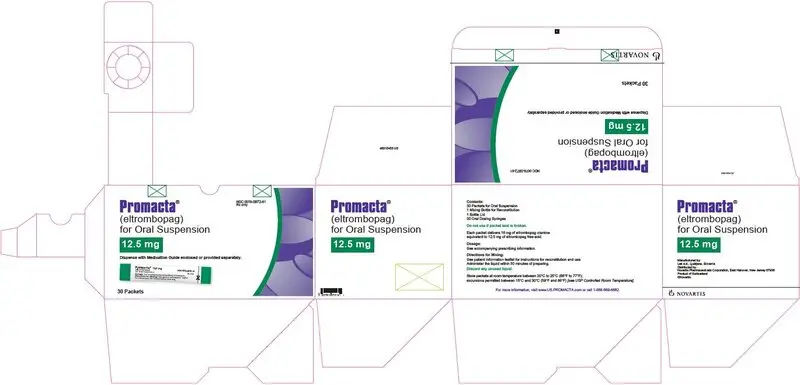
Preparation of the Oral Suspension: Prior to use of the oral suspension, ensure patients or caregivers receive training on proper dosing, preparation, and administration of PROMACTA for oral suspension.
Administer the oral suspension immediately after preparation. Discard any suspension not administered within 30 minutes after preparation.
Prepare the suspension with water only. NOTE: Do not use hot water to prepare the suspension.
For details on preparation and administration of the suspension, including the recommended duration of use of each oral dosing syringe, [see Instructions for Use].
3. Dosage Forms and Strengths
Tablets
- 12.5-mg tablets —– round, biconvex, white, film-coated tablets debossed with “GS MZ1” and 12.5 on one side. Each tablet, for oral administration, contains eltrombopag olamine, equivalent to 12.5 mg of eltrombopag free acid.
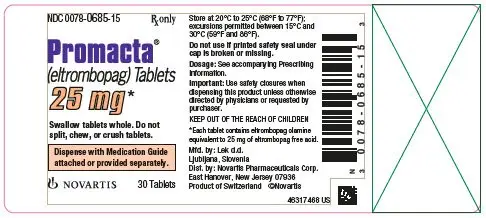
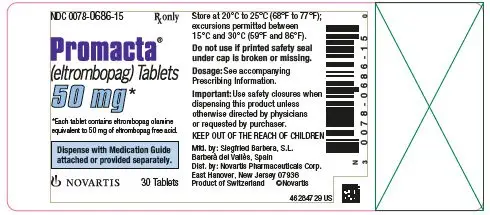
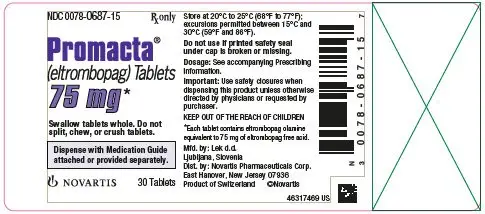
- 25-mg tablets —– round, biconvex, orange, film-coated tablets debossed with “GS NX3” and 25 on one side. Each tablet, for oral administration, contains eltrombopag olamine, equivalent to 25 mg of eltrombopag free acid.
- 50-mg tablets —– round, biconvex, blue, film-coated tablets debossed with “GS UFU” and 50 on one side. Each tablet, for oral administration, contains eltrombopag olamine, equivalent to 50 mg of eltrombopag free acid.
- 75-mg tablets —– round, biconvex, pink, film-coated tablets debossed with “GS FFS” and 75 on one side. Each tablet, for oral administration, contains eltrombopag olamine, equivalent to 75 mg of eltrombopag free acid.
For Oral Suspension
- 12.5-mg packet —– contains a reddish-brown to yellow powder for reconstitution.
- 25-mg packet —– contains a reddish-brown to yellow powder for reconstitution.
5. Warnings and Precautions
5.1 Hepatic Decompensation in Patients With Chronic Hepatitis C
In patients with chronic hepatitis C, PROMACTA in combination with interferon and ribavirin may increase the risk of hepatic decompensation. In two controlled clinical trials in patients with chronic hepatitis C and thrombocytopenia, ascites and encephalopathy occurred more frequently on the arm receiving treatment with PROMACTA plus antivirals (7%) than the placebo plus antivirals arm (4%). Patients with low albumin levels (less than 3.5 g/dL) or Model for End-Stage Liver Disease (MELD) score greater than or equal to 10 at baseline had a greater risk for hepatic decompensation on the arm receiving treatment with PROMACTA plus antivirals. Discontinue PROMACTA if antiviral therapy is discontinued.
5.2 Hepatotoxicity
PROMACTA may increase the risk of severe and potentially life-threatening hepatotoxicity [see Adverse Reactions (6.1)]. One patient (< 1%) with ITP treated with PROMACTA in clinical trials experienced drug-induced liver injury. Eleven patients (1%) with chronic hepatitis C treated with PROMACTA in clinical trials experienced drug-induced liver injury.
Treatment of ITP, Chronic Hepatitis C-associated Thrombocytopenia, and Refractory Severe Aplastic Anemia
Measure serum ALT, AST, and bilirubin prior to initiation of PROMACTA, every 2 weeks during the dose adjustment phase, and monthly following establishment of a stable dose. PROMACTA inhibits UDP-glucuronosyltransferase (UGT)1A1 and organic anion-transporting polypeptide (OATP)1B1, which may lead to indirect hyperbilirubinemia. If bilirubin is elevated, perform fractionation. Evaluate abnormal serum liver tests with repeat testing within 3 to 5 days. If the abnormalities are confirmed, monitor serum liver tests weekly until resolved or stabilized. Discontinue PROMACTA if ALT levels increase to greater than or equal to 3 x ULN in patients with normal liver function or greater than or equal to 3 x baseline (or greater than 5 x ULN, whichever is the lower) in patients with pre-treatment elevations in transaminases and are:
- progressively increasing, or
- persistent for greater than or equal to 4 weeks, or
- accompanied by increased direct bilirubin, or
- accompanied by clinical symptoms of liver injury or evidence for hepatic decompensation.
If the potential benefit for reinitiating treatment with PROMACTA is considered to outweigh the risk for hepatotoxicity, then consider cautiously reintroducing PROMACTA and measure serum liver tests weekly during the dose adjustment phase. Hepatotoxicity may reoccur if PROMACTA is reinitiated. If liver test abnormalities persist, worsen, or recur, then permanently discontinue PROMACTA.
First-Line Treatment of Severe Aplastic Anemia
Measure ALT, AST, and bilirubin prior to initiation of PROMACTA, every other day while hospitalized for h-ATG therapy, and then every 2 weeks during treatment. During treatment, manage increases in ALT or AST levels as recommended in Table 6.
5.3 Increased Risk of Death and Progression of Myelodysplastic Syndromes to Acute Myeloid Leukemia
A randomized, double-blind, placebo-controlled, multicenter trial in patients with International Prognostic Scoring System (IPSS) intermediate-1, intermediate-2 or high risk MDS with thrombocytopenia, receiving azacitidine in combination with either PROMACTA (n = 179) or placebo (n = 177) was terminated due to lack of efficacy and safety reasons, including increased progression to acute myeloid leukemia (AML). Patients received PROMACTA or placebo at a starting dose of 200 mg once daily, up to a maximum of 300 mg once daily, in combination with azacitidine for at least six cycles. The incidence of death (overall survival) was 32% (57/179) in the PROMACTA arm versus 29% (51/177) in the placebo arm (HR [95% CI] = 1.42 [0.97, 2.08], showing an increased relative risk of death in this trial by 42% in the PROMACTA arm). The incidence of progression to AML was 12% (21/179) in the PROMACTA arm versus 6% (10/177) in the placebo arm (HR [95% CI] = 2.66 [1.31, 5.41], showing an increased relative risk of progression to AML in this trial by 166% in the PROMACTA arm).
5.4 Thrombotic/Thromboembolic Complications
Thrombotic/thromboembolic complications may result from increases in platelet counts with PROMACTA. Reported thrombotic/thromboembolic complications included both venous and arterial events and were observed at low and at normal platelet counts.
Consider the potential for an increased risk of thromboembolism when administering PROMACTA to patients with known risk factors for thromboembolism (e.g., Factor V Leiden, ATIII deficiency, antiphospholipid syndrome, chronic liver disease). To minimize the risk for thrombotic/thromboembolic complications, do not use PROMACTA in an attempt to normalize platelet counts. Follow the dose adjustment guidelines to achieve and maintain target platelet counts [see Dosage and Administration (2.1, 2.2, 2.3)].
In two controlled clinical trials in patients with chronic hepatitis C and thrombocytopenia, 3% (31/955) treated with PROMACTA experienced a thrombotic event compared with 1% (5/484) on placebo. The majority of events were of the portal venous system (1% in patients treated with PROMACTA versus less than 1% for placebo).
In a controlled trial in patients with chronic liver disease and thrombocytopenia not related to ITP undergoing elective invasive procedures (N = 292), the risk of thrombotic events was increased in patients treated with 75 mg of PROMACTA once daily. Seven thrombotic complications (six patients) were reported in the group that received PROMACTA and three thrombotic complications were reported in the placebo group (two patients). All of the thrombotic complications reported in the group that received PROMACTA were portal vein thrombosis (PVT). Symptoms of PVT included abdominal pain, nausea, vomiting, and diarrhea. Five of the six patients in the group that received PROMACTA experienced a thrombotic complication within 30 days of completing treatment with PROMACTA and at a platelet count above 200 x 109/L. The risk of portal venous thrombosis was increased in thrombocytopenic patients with chronic liver disease treated with 75 mg of PROMACTA once daily for 2 weeks in preparation for invasive procedures.
5.5 Cataracts
In the three controlled clinical trials in adults with persistent or chronic ITP, cataracts developed or worsened in 15 (7%) patients who received 50 mg of PROMACTA daily and 8 (7%) placebo-group patients. In the extension trial, cataracts developed or worsened in 11% of patients who underwent ocular examination prior to therapy with PROMACTA. In the two controlled clinical trials in patients with chronic hepatitis C and thrombocytopenia, cataracts developed or worsened in 8% of patients treated with PROMACTA and 5% of patients treated with placebo.
Cataracts were observed in toxicology studies of eltrombopag in rodents [see Nonclinical Toxicology (13.2)]. Perform a baseline ocular examination prior to administration of PROMACTA and, during therapy with PROMACTA, regularly monitor patients for signs and symptoms of cataracts.
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions associated with PROMACTA are described in other sections.
- Hepatic Decompensation in Patients with Chronic Hepatitis C [see Warnings and Precautions (5.1)]
- Hepatotoxicity [see Warnings and Precautions (5.2)]
- Increased Risk of Death and Progression of Myelodysplastic Syndromes to Acute Myeloid Leukemia [see Warnings and Precautions (5.3)]
- Thrombotic/Thromboembolic Complications [see Warnings and Precautions (5.4)]
- Cataracts [see Warnings and Precautions (5.5)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Persistent or Chronic Immune Thrombocytopenia
Adults: In clinical trials, hemorrhage was the most common serious adverse reaction and most hemorrhagic reactions followed discontinuation of PROMACTA. Other serious adverse reactions included thrombotic/thromboembolic complications [see Warnings and Precautions (5.4)]. The data described below reflect exposure of PROMACTA to patients with persistent or chronic ITP aged 18 to 85 years, of whom 66% were female, in three placebo-controlled trials and one open-label extension trial [see Clinical Studies (14.1)]. PROMACTA was administered to 330 patients for at least 6 months and 218 patients for at least 1 year.
Table 8 presents the most common adverse drug reactions (experienced by greater than or equal to 3% of patients receiving PROMACTA) from the three placebo-controlled trials, with a higher incidence in PROMACTA versus placebo.
| Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase. aIncludes PTs of urinary tract infection, cystitis, urinary tract infection bacterial, and bacteriuria. |
||
|
Adverse reaction |
PROMACTA 50 mg n = 241 (%) |
Placebo n = 128 (%) |
|
Nausea |
9 |
3 |
|
Diarrhea |
9 |
7 |
|
Upper respiratory tract infection |
7 |
6 |
|
Vomiting |
6 |
< 1 |
|
Urinary tract infectiona |
5 |
4 |
|
Increased ALT |
5 |
3 |
|
Myalgia |
5 |
2 |
|
Oropharyngeal pain |
4 |
3 |
|
Increased AST |
4 |
2 |
|
Pharyngitis |
4 |
2 |
|
Back pain |
3 |
2 |
|
Influenza |
3 |
2 |
|
Paresthesia |
3 |
2 |
|
Rash |
3 |
2 |
In the three controlled clinical persistent or chronic ITP trials, alopecia, musculoskeletal pain, blood alkaline phosphatase increased, and dry mouth were the adverse reactions reported in 2% of patients treated with PROMACTA and in no patients who received placebo.
Among 302 patients with persistent or chronic ITP who received PROMACTA in the single-arm extension trial, the adverse reactions occurred in a pattern similar to that seen in the placebo-controlled trials. Table 9 presents the most common treatment-related adverse reactions (experienced by greater than or equal to 3% of patients receiving PROMACTA) from the extension trial.
| Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase. | |
|
Adverse reaction |
PROMACTA 50 mg n = 302 (%) |
|
Headache |
10 |
|
ALT increased |
5 |
|
AST increased |
5 |
|
Cataract |
5 |
|
Fatigue |
5 |
|
Blood bilirubin increased |
4 |
|
Nausea |
4 |
|
Hyperbilirubinemia |
3 |
|
Diarrhea |
3 |
In the three controlled persistent or chronic ITP trials, serum liver test abnormalities (predominantly Grade 2 or less in severity) were reported in 11% and 7% of patients for PROMACTA and placebo, respectively. Four patients (1%) treated with PROMACTA and three patients in the placebo group (2%) discontinued treatment due to hepatobiliary laboratory abnormalities. Seventeen of the patients treated with PROMACTA in the controlled trials with hepatobiliary laboratory abnormalities were re-exposed to PROMACTA in the extension trial. Eight of these patients again experienced liver test abnormalities (less than or equal to Grade 3) resulting in discontinuation of PROMACTA in one patient. In the extension persistent or chronic ITP trial, six additional patients had PROMACTA discontinued due to liver test abnormalities (less than or equal to Grade 3).
In the three controlled persistent or chronic ITP trials, cataracts developed or worsened in 7% of patients treated with PROMACTA and 7% of patients in the placebo group. All patients had documented, preexisting risk factors for cataractogenesis, including corticosteroid use. In the extension trial, cataracts developed or worsened in 11% of patients who underwent ocular examination prior to therapy with PROMACTA. Seventy-two percent of patients had preexisting risk factors, including corticosteroid use.
The safety of PROMACTA was also assessed in all patients treated in 7 adult persistent or chronic ITP clinical trials (N = 763 PROMACTA-treated patients and 179 placebo-treated patients). Thromboembolic events were reported in 6% of PROMACTA-treated patients versus 0% of placebo-treated patients and thrombotic microangiopathy with acute renal failure was reported in < 1% of PROMACTA-treated patients versus 0% of placebo-treated patients.
In a placebo-controlled trial of PROMACTA in patients with chronic liver disease and thrombocytopenia not related to ITP, six patients treated with PROMACTA and one patient in the placebo group developed portal vein thromboses [see Warnings and Precautions (5.4)].
Pediatric Patients: The data described below reflect median exposure to PROMACTA of 91 days for 107 pediatric patients (aged 1 to 17 years) with persistent or chronic ITP, of whom 53% were female, across the randomized phase of two placebo-controlled trials.
Table 10 presents the most common adverse drug reactions (experienced by greater than or equal to 3% of pediatric patients 1 year and older receiving PROMACTA) across the two placebo-controlled trials, with a higher incidence for PROMACTA versus placebo.
| Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase. aIncludes adverse reactions or laboratory abnormalities > 3 x ULN. |
||
|
PROMACTA |
Placebo |
|
|
n = 107 |
n = 50 |
|
|
Adverse reaction |
(%) |
(%) |
|
Upper respiratory tract infection |
17 |
6 |
|
Nasopharyngitis |
12 |
4 |
|
Cough |
9 |
0 |
|
Diarrhea |
9 |
2 |
|
Pyrexia |
9 |
8 |
|
Abdominal pain |
8 |
4 |
|
Oropharyngeal pain |
8 |
2 |
|
Toothache |
6 |
0 |
|
ALT increaseda |
6 |
0 |
|
Rash |
5 |
2 |
|
AST increased |
4 |
0 |
|
Rhinorrhea |
4 |
0 |
In the two controlled clinical persistent or chronic ITP trials, cataracts developed or worsened in 2 (1%) patients treated with PROMACTA. Both patients had received chronic oral corticosteroids, a risk factor for cataractogenesis.
Chronic Hepatitis C-associated Thrombocytopenia: In the two placebo-controlled trials, 955 patients with chronic hepatitis C-associated thrombocytopenia received PROMACTA. Table 11 presents the most common adverse drug reactions (experienced by greater than or equal to 10% of patients receiving PROMACTA compared with placebo).
| aIncludes PTs of insomnia, initial insomnia, and poor quality sleep. | ||
|
Adverse reaction |
PROMACTA + Peginterferon/Ribavirin n = 955 (%) |
Placebo + Peginterferon/Ribavirin n = 484 (%) |
|
Anemia |
40 |
35 |
|
Pyrexia |
30 |
24 |
|
Fatigue |
28 |
23 |
|
Headache |
21 |
20 |
|
Nausea |
19 |
14 |
|
Diarrhea |
19 |
11 |
|
Decreased appetite |
18 |
14 |
|
Influenza-like illness |
18 |
16 |
|
Insomniaa |
16 |
15 |
|
Asthenia |
16 |
13 |
|
Cough |
15 |
12 |
|
Pruritus |
15 |
13 |
|
Chills |
14 |
9 |
|
Myalgia |
12 |
10 |
|
Alopecia |
10 |
6 |
|
Peripheral edema |
10 |
5 |
Rash was reported in 9% and 7% of patients receiving PROMACTA and placebo, respectively.
In the two controlled clinical trials in patients with chronic hepatitis C, hyperbilirubinemia was reported in 8% of patients receiving PROMACTA compared with 3% for placebo. Total bilirubin greater than or equal to 1.5 x ULN was reported in 76% and 50% of patients receiving PROMACTA and placebo, respectively. ALT or AST greater than or equal to 3 x ULN was reported in 34% and 38% of patients for PROMACTA and placebo, respectively.
In the two controlled clinical trials in patients with chronic hepatitis C, cataracts developed or worsened in 8% of patients treated with PROMACTA and 5% of patients treated with placebo.
The safety of PROMACTA was also assessed in all patients treated with PROMACTA in the two controlled trials, including patients who initially received PROMACTA in the pre-antiviral treatment phase of the trial and were later randomized to the placebo arm (N = 1520 PROMACTA-treated patients). Hepatic failure was reported in 0.8% of PROMACTA-treated patients and 0.4% of placebo-treated patients.
Severe Aplastic Anemia
First-Line Treatment of Severe Aplastic Anemia
The safety of PROMACTA was established based upon a single-arm trial of 153 patients with severe aplastic anemia who had not received prior definitive immunosuppressive therapy. In this trial, PROMACTA was administered in combination with horse antithymocyte globulin (h-ATG) and cyclosporine [see Clinical Studies (14.3)]. Among the 153 patients who were dosed in this trial, 92 patients were evaluable for safety of the concurrent use of PROMACTA, h-ATG, and cyclosporine at the recommended dose and schedule.
In this cohort, PROMACTA was administered at up to 150 mg once daily on Day 1 to Month 6 (D1-M6) in combination with h-ATG on Days 1 to 4 and cyclosporine for 6 months, followed by low dose of cyclosporine (maintenance dose) for an additional 18 months for patients who achieved a hematologic response at 6 months. The median duration of exposure to PROMACTA in this cohort was 183 days with 70% of patients exposed for > 24 weeks.
Table 12 presents the most common adverse reactions (experienced by greater than or equal to 5% of patients) associated with PROMACTA in the D1-M6 cohort.
| Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase. | |
|
Adverse reaction |
PROMACTA |
|
ALT increased |
29 |
|
AST increased |
17 |
|
Blood bilirubin increased |
17 |
|
Rash |
8 |
|
Skin discoloration, including hyperpigmentation |
5 |
In the PROMACTA D1-M6 cohort, ALT increased (29%), AST increased (17%), and blood bilirubin increased (17%) were reported more frequently than in patients with refractory severe aplastic anemia (see Table 13).
New or worsening liver function laboratory abnormalities (CTCAE Grade 3 and Grade 4) in the PROMACTA D1-M6 cohort were 15% and 2% for AST, 26% and 4% for ALT, and 12% and 1% for bilirubin, respectively.
In this single-arm open-label clinical trial, ALT or AST > 3 x ULN with total bilirubin > 1.5 x ULN and ALT or AST > 3 x ULN with total bilirubin > 2 x ULN were reported in 44% and 32% of patients, respectively, in the PROMACTA D1-M6 cohort.
Pediatric Patients
A total of 34 pediatric patients (2 patients 2 to 5 years of age, 12 patients 6 to 11 years of age, and 20 patients 12 to 16 years of age) were enrolled in this single-arm trial of which 26 pediatric patients were enrolled in the PROMACTA D1-M6 cohort. In this cohort, the most frequent serious adverse reactions (experienced by ≥ 10% of patients) were upper respiratory tract infection (12% in patients age 2 to 16 years compared to 5% in patients 17 years of age and older, respectively) and rash (12% compared to 2%). The most common adverse reactions (experienced by ≥ 10% of patients) associated with PROMACTA were ALT increased (23% in patients age 2 to 16 years compared to 32% in patients 17 years of age and older, respectively), blood bilirubin increased (12% compared to 20%), AST increased (12% compared to 20%), and rash (12% compared to 6%).
Cytogenetic Abnormalities
In this trial, patients had bone marrow aspirates evaluated for cytogenetic abnormalities. Seven patients in the PROMACTA D1-M6 cohort had a new cytogenetic abnormality reported of which 4 had the loss of chromosome 7; these 4 occurred within 6.1 months. Across all cohorts, clonal cytogenetic evolution occurred in 15 out of 153 (10%) patients. Of the 15 patients who experienced a cytogenetic abnormality: 7 patients had the loss of chromosome 7, 6 of which occurred within 6.1 months; 4 patients had chromosomal aberrations which were of unclear significance; 3 patients had a deletion of chromosome 13; and 1 patient had a follow-up bone marrow assessment at 5 years with features of dysplasia with hypercellularity concerning for potential development of MDS. It is unclear whether these findings occurred due to the underlying disease, the immunosuppressive therapy, and/or treatment with PROMACTA.
Refractory Severe Aplastic Anemia
In the single-arm, open-label trial, 43 patients with refractory severe aplastic anemia received PROMACTA. Eleven patients (26%) were treated for greater than 6 months and 7 patients (16%) were treated for greater than 1 year. The most common adverse reactions (greater than or equal to 20%) were nausea, fatigue, cough, diarrhea, and headache.
|
Adverse reaction |
PROMACTA n = 43 (%) |
|
Nausea |
33 |
|
Fatigue |
28 |
|
Cough |
23 |
|
Diarrhea |
21 |
|
Headache |
21 |
|
Pain in extremity |
19 |
|
Pyrexia |
14 |
|
Dizziness |
14 |
|
Oropharyngeal pain |
14 |
|
Abdominal pain |
12 |
|
Muscle spasms |
12 |
|
Transaminases increased |
12 |
|
Arthralgia |
12 |
|
Rhinorrhea |
12 |
Rash and hyperbilirubinemia were reported in 7% of patients; cataract was reported in 2% of patients.
In this trial, concurrent ALT or AST greater than 3 x ULN with total bilirubin greater than 1.5 x ULN were reported in 5% of patients. Total bilirubin greater than 1.5 x ULN occurred in 14% of patients.
In this trial, patients had bone marrow aspirates evaluated for cytogenetic abnormalities. Eight patients had a new cytogenetic abnormality reported on therapy, including 5 patients who had complex changes in chromosome 7.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of PROMACTA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate the frequency or establish a causal relationship to drug exposure.
Skin and Subcutaneous Tissue Disorders: Skin discoloration, including hyperpigmentation and skin yellowing.
7. Drug Interactions
7.1 Polyvalent Cations (Chelation)
Eltrombopag chelates polyvalent cations (such as iron, calcium, aluminum, magnesium, selenium, and zinc) in foods, mineral supplements, and antacids.
Take PROMACTA at least 2 hours before or 4 hours after any medications or products containing polyvalent cations, such as antacids, dairy products, and mineral supplements to avoid significant reduction in absorption of PROMACTA due to chelation [see Dosage and Administration (2.4), Clinical Pharmacology (12.3)].
7.2 Transporters
Use caution when concomitantly administering PROMACTA and drugs that are substrates of OATP1B1 (e.g., atorvastatin, bosentan, ezetimibe, fluvastatin, glyburide, olmesartan, pitavastatin, pravastatin, rosuvastatin, repaglinide, rifampin, simvastatin acid, SN-38 [active metabolite of irinotecan], valsartan) or breast cancer resistance protein (BCRP) (e.g., imatinib, irinotecan, lapatinib, methotrexate, mitoxantrone, rosuvastatin, sulfasalazine, topotecan). Monitor patients closely for signs and symptoms of excessive exposure to the drugs that are substrates of OATP1B1 or BCRP and consider reduction of the dose of these drugs, if appropriate. In clinical trials with PROMACTA, a dose reduction of rosuvastatin by 50% was recommended.
7.3 Protease Inhibitors
HIV Protease Inhibitors: No dose adjustment is recommended when PROMACTA is coadministered with lopinavir/ritonavir (LPV/RTV). Drug interactions with other HIV protease inhibitors have not been evaluated.
Hepatitis C Virus Protease Inhibitors: No dose adjustments are recommended when PROMACTA is coadministered with boceprevir or telaprevir. Drug interactions with other hepatitis C virus (HCV) protease inhibitors have not been evaluated.
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
Available data from a small number of published case reports and postmarketing experience with PROMACTA use in pregnant women are insufficient to assess any drug-associated risks for major birth defects, miscarriage, or adverse maternal or fetal outcomes. In animal reproduction and developmental toxicity studies, oral administration of eltrombopag to pregnant rats during organogenesis resulted in embryolethality and reduced fetal weights at maternally toxic doses. These effects were observed at doses resulting in exposures that were six times the human clinical exposure based on area under the curve (AUC) in patients with persistent or chronic ITP at 75 mg/day, and three times the AUC in patients with chronic hepatitis C at 100 mg/day (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and of miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal Data
In an early embryonic development study, female rats received oral eltrombopag at doses of 10, 20, or 60 mg/kg/day (0.8, 2, and 6 times, respectively, the human clinical exposure based on AUC in patients with ITP at 75 mg/day and 0.3, 1, and 3 times, respectively, the human clinical exposure based on AUC in patients with chronic hepatitis C at 100 mg/day). Increased pre- and post-implantation loss and reduced fetal weight were observed at the highest dose which also caused maternal toxicity.
In an embryo-fetal development study eltrombopag was administered orally to pregnant rats during the period of organogenesis at doses of 10, 20, or 60 mg/kg/day (0.8, 2, and 6 times, respectively, the human clinical exposure based on AUC in patients with ITP at 75 mg/day and 0.3, 1, and 3 times, respectively, the human clinical exposure based on AUC in patients with chronic hepatitis C at 100 mg/day). Decreased fetal weights (6% to 7%) and a slight increase in the presence of cervical ribs were observed at the highest dose which also caused maternal toxicity. However, no evidence of major structural malformations was observed.
In an embryo-fetal development study eltrombopag was administered orally to pregnant rabbits during the period of organogenesis at doses of 30, 80, or 150 mg/kg/day (0.04, 0.3, and 0.5 times, respectively, the human clinical exposure based on AUC in patients with ITP at 75 mg/day and 0.02, 0.1, and 0.3 times, respectively, the human clinical exposure based on AUC in patients with chronic hepatitis C at 100 mg/day). No evidence of fetotoxicity, embryolethality, or teratogenicity was observed.
In a pre- and post-natal developmental toxicity study in pregnant rats (F0), oral eltrombopag was administered from gestation Day 6 through lactation Day 20. No adverse effects on maternal reproductive function or on the development of the offspring (F1) were observed at doses up to 20 mg/kg/day (2 times the human clinical exposure based on AUC in patients with ITP at 75 mg/day and similar to the human clinical exposure based on AUC in patients with chronic hepatitis C at 100 mg/day). Eltrombopag was detected in the plasma of offspring (F1). The plasma concentrations in pups increased with dose following administration of drug to the F0 dams.
8.2 Lactation
Risk Summary
There are no data regarding the presence of eltrombopag or its metabolites in human milk, the effects on the breastfed child, or the effects on milk production. However, eltrombopag was detected in the pups of lactating rats 10 days postpartum suggesting the potential for transfer during lactation. Due to the potential for serious adverse reactions in a breastfed child from PROMACTA, breastfeeding is not recommended during treatment.
8.3 Females and Males of Reproductive Potential
Contraception
Based on animal reproduction studies, PROMACTA can cause fetal harm when administered to a pregnant woman. Sexually-active females of reproductive potential should use effective contraception (methods that result in less than 1% pregnancy rates) when using PROMACTA during treatment and for at least 7 days after stopping treatment with PROMACTA.
8.4 Pediatric Use
The safety and efficacy of PROMACTA have been established in pediatric patients 1 year and older with persistent or chronic ITP and in pediatric patients 2 years and older with IST-naïve severe aplastic anemia (in combination with h-ATG and cyclosporine). Safety and efficacy in pediatric patients below the age of 1 year with ITP have not been established. Safety and efficacy in pediatric patients with thrombocytopenia associated with chronic hepatitis C and refractory severe aplastic anemia have not been established.
The safety and efficacy of PROMACTA in pediatric patients 1 year and older with persistent or chronic ITP were evaluated in two double-blind, placebo-controlled trials [see Adverse Reactions (6.1), Clinical Studies (14.1)]. The pharmacokinetics of eltrombopag have been evaluated in 168 pediatric patients 1 year and older with ITP dosed once daily [see Clinical Pharmacology (12.3)]. See Dosage and Administration (2.1) for dosing recommendations for pediatric patients 1 year and older.
The safety and efficacy of PROMACTA in combination with h-ATG and cyclosporine for the first-line treatment of severe aplastic anemia in pediatric patients 2 years and older were evaluated in a single-arm, open-label trial [see Adverse Reactions (6.1), Clinical Studies (14.3)]. A total of 26 pediatric patients (ages 2 to < 17 years) were evaluated; 12 children (aged 2 to < 12 years) and 14 adolescents (aged 12 to < 17). See Dosage and Administration (2.3) for dosing recommendations for pediatric patients 2 years and older. The safety and efficacy of PROMACTA in combination with h-ATG and cyclosporine in pediatric patients younger than 2 years for the first-line treatment of severe aplastic anemia have not yet been established. In patients 2 to 16 years of age, 69% of patients experienced serious adverse events compared to 42% in patients 17 years and older. Among the 12 patients who were 2 to 11 years of age in the PROMACTA D1-M6 cohort and reached the 6-month assessment or withdrew earlier, the complete response rate at Month 6 was 8% versus 46% in patients age 12 to 16 years and 50% in patients 17 years of age and older.
8.5 Geriatric Use
Of the 106 patients in two randomized clinical trials of PROMACTA 50 mg in persistent or chronic ITP, 22% were 65 years of age and over, while 9% were 75 years of age and over. Of the 1439 patients in two randomized clinical trials of PROMACTA in patients with chronic hepatitis C and thrombocytopenia, 7% were 65 years of age and over, while < 1% were 75 years of age and over. Of the 196 patients who received PROMACTA for the treatment of severe aplastic anemia, 18% were 65 years of age and over, while 3% were 75 years of age and over. No overall differences in safety or effectiveness were observed between these patients and younger patients.
8.6 Hepatic Impairment
Patients With Persistent or Chronic ITP and Severe Aplastic Anemia
Reduce the initial dose of PROMACTA in patients with persistent or chronic ITP (adult and pediatric patients 6 years and older only) or refractory severe aplastic anemia who also have hepatic impairment (Child-Pugh class A, B, C) [see Dosage and Administration (2.1, 2.3), Warnings and Precautions (5.2), Clinical Pharmacology (12.3)].
In a clinical trial in patients with severe aplastic anemia who had not received prior definitive immunosuppressive therapy, patients with baseline ALT or AST > 5 x ULN were ineligible to participate. If a patient with hepatic impairment (Child-Pugh class A, B, C) initiates therapy with PROMACTA for the first-line treatment of severe aplastic anemia, reduce the initial dose [see Dosage and Administration (2.3), Warnings and Precautions (5.2), Clinical Pharmacology (12.3)].
Patients With Chronic Hepatitis C
No dosage adjustment is recommended in patients with chronic hepatitis C and hepatic impairment [see Clinical Pharmacology (12.3)].
8.7 Ethnicity
Reduce the initial dose of PROMACTA for patients of East-/Southeast-Asian ancestry with ITP (adult and pediatric patients 6 years and older only) or severe aplastic anemia [see Dosage and Administration (2.1, 2.3), Clinical Pharmacology (12.3)]. No reduction in the initial dose of PROMACTA is recommended in patients of East-/Southeast-Asian ancestry with chronic hepatitis C [see Clinical Pharmacology (12.3)].
10. Overdosage
In the event of overdose, platelet counts may increase excessively and result in thrombotic/thromboembolic complications.
In one report, a subject who ingested 5000 mg of PROMACTA had a platelet count increase to a maximum of 929 x 109/L at 13 days following the ingestion. The patient also experienced rash, bradycardia, ALT/AST elevations, and fatigue. The patient was treated with gastric lavage, oral lactulose, intravenous fluids, omeprazole, atropine, furosemide, calcium, dexamethasone, and plasmapheresis; however, the abnormal platelet count and liver test abnormalities persisted for 3 weeks. After 2 months’ follow-up, all events had resolved without sequelae.
In case of an overdose, consider oral administration of a metal cation-containing preparation, such as calcium, aluminum, or magnesium preparations to chelate eltrombopag and thus limit absorption. Closely monitor platelet counts. Reinitiate treatment with PROMACTA in accordance with dosing and administration recommendations [see Dosage and Administration (2.1, 2.2)].
12. Promacta - Clinical Pharmacology
12.2 Pharmacodynamics
In clinical trials, treatment with PROMACTA resulted in dose-dependent increases in platelet counts following repeated (daily) dosing. The increase in platelet counts reached a maximum approximately two weeks after the initiation of dosing, and returned to baseline within approximately two weeks after the last dose of PROMACTA.
Cardiac Electrophysiology
At doses up to 150 mg (the maximum recommended dose) daily for 5 days, PROMACTA did not prolong the QT/QTc interval to any relevant extent.
12.3 Pharmacokinetics
Eltrombopag demonstrated a dose-proportional increase in exposure between doses of 50 to 150 mg/day in healthy adult subjects. Eltrombopag AUC was approximately 1.7-fold higher in patients with persistent or chronic ITP and approximately 2.8-fold higher in patients with HCV compared to healthy subjects. Steady-state was achieved after approximately 1 week of once daily treatment, with geometric mean accumulation ratio of 1.56 (90% confidence interval 1.20, 1.63) at 75 mg/day. Eltrombopag AUC was approximately 3.2-fold higher in patients with definitive immunosuppressive therapy-naïve severe aplastic anemia compared to healthy subjects suggesting higher relative exposure compared to healthy subjects or patients with ITP and similar exposure compared to patients with chronic hepatitis C. Eltrombopag for oral suspension delivered 22% higher plasma AUC0-INF than the tablet formulation.
Absorption
Eltrombopag is absorbed with a peak concentration occurring 2 to 6 hours after oral administration. Oral absorption of drug-related material following administration of a single 75-mg solution dose was estimated to be at least 52%.
Effect of Food
A standard high-fat breakfast (876 calories, 52 g fat, 71 g carbohydrate, 34 g protein, and 427 mg calcium) significantly decreased plasma eltrombopag AUC0-INF by approximately 59% and Cmax by 65% and delayed Tmax by 1 hour. The decrease in exposure is primarily due to the high calcium content.
A meal low in calcium (≤ 50 mg calcium) did not significantly impact plasma eltrombopag exposure, regardless of calorie and fat content.
The effect of administration of a single 25-mg dose of eltrombopag for oral suspension with a high-calcium, moderate-fat, moderate calorie meal on AUC0-INF and Cmax in healthy adult subjects is presented in Table 14.
| a372 calories, 9 g fat, and 448 mg calcium. | ||
| Timing of eltrombopag for oral suspension dose | Mean (90% CI) reduction in plasma eltrombopag AUC0-INF | Mean (90% CI) reduction in plasma eltrombopag Cmax |
| With a high-calcium, moderate-fat, moderate-calorie meal | 75% (71%, 88%) | 79% (76%, 82%) |
| 2 hours after the high-calcium, moderate-fat, moderate-calorie meal | 47% (40%, 53%) | 48% (40%, 54%) |
| 2 hours before the high-calcium, moderate-fat, moderate-calorie meal | 20% (9%, 29%) | 14% (2%, 25%) |
Distribution
The concentration of eltrombopag in blood cells is approximately 50% to 79% of plasma concentrations based on a radiolabel study. In vitro studies suggest that eltrombopag is highly bound to human plasma proteins (greater than 99%). Eltrombopag is a substrate of BCRP, but is not a substrate for P-glycoprotein (P-gp) or OATP1B1.
Elimination
The plasma elimination half-life of eltrombopag is approximately 21 to 32 hours in healthy subjects and 26 to 35 hours in patients with ITP.
Metabolism: Absorbed eltrombopag is extensively metabolized, predominantly through pathways, including cleavage, oxidation, and conjugation with glucuronic acid, glutathione, or cysteine. In vitro studies suggest that CYP1A2 and CYP2C8 are responsible for the oxidative metabolism of eltrombopag. UGT1A1 and UGT1A3 are responsible for the glucuronidation of eltrombopag.
Excretion: The predominant route of eltrombopag excretion is via feces (59%), and 31% of the dose is found in the urine. Unchanged eltrombopag in feces accounts for approximately 20% of the dose; unchanged eltrombopag is not detectable in urine.
Specific Populations
Ethnicity
Eltrombopag concentrations in East-/Southeast-Asian ancestry patients with ITP or chronic hepatitis C, were 50% to 55% higher compared with non-Asian subjects [see Dosage and Administration (2.1, 2.3)].
Eltrombopag exposure in healthy African-American subjects was approximately 40% higher than that observed in Caucasian subjects in one clinical pharmacology trial and similar in three other clinical pharmacology trials. The effect of African-American ethnicity on exposure and related safety and efficacy of eltrombopag has not been established.
Hepatic Impairment
Following a single dose of PROMACTA (50 mg), plasma eltrombopag AUC0-INF was 41% higher in patients with mild hepatic impairment (Child-Pugh class A) compared with subjects with normal hepatic function. Plasma eltrombopag AUC0-INF was approximately 2-fold higher in patients with moderate (Child-Pugh class B) and severe hepatic impairment (Child-Pugh class C) compared with subjects with normal hepatic function. The half-life of eltrombopag was prolonged 2-fold in these patients. This clinical trial did not evaluate protein-binding effects.
Chronic Liver Disease
Following repeat doses of eltrombopag in patients with thrombocytopenia and with chronic liver disease, mild hepatic impairment resulted in an 87% to 110% higher plasma eltrombopag AUC(0-τ) and moderate hepatic impairment resulted in approximately 141% to 240% higher plasma eltrombopag AUC(0-τ) values compared with patients with normal hepatic function. The half-life of eltrombopag was prolonged 3-fold in patients with mild hepatic impairment and 4-fold in patients with moderate hepatic impairment. This clinical trial did not evaluate protein-binding effects.
Chronic Hepatitis C
Patients with chronic hepatitis C treated with PROMACTA had higher plasma AUC(0-τ) values as compared with healthy subjects, and AUC(0-τ) increased with increasing Child-Pugh score. Patients with chronic hepatitis C and mild hepatic impairment had approximately 100% to 144% higher plasma AUC(0-τ) compared with healthy subjects. This clinical trial did not evaluate protein-binding effects.
Renal Impairment
Following a single dose of PROMACTA (50 mg), the average total plasma eltrombopag AUC0-INF was 32% to 36% lower in subjects with mild (estimated creatinine clearance (CLCr) by Cockcroft-Gault equation: 50 to 80 mL/min), to moderate (CLCr of 30 to 49 mL/min) renal impairment and 60% lower in subjects with severe (CLCr less than 30 mL/min) renal impairment compared with healthy subjects. The effect of renal impairment on unbound (active) eltrombopag exposure has not been assessed.
Pediatric Patients
The pharmacokinetics of eltrombopag have been evaluated in 168 pediatric patients 1 year and older with ITP dosed once daily in two trials. Plasma eltrombopag apparent clearance following oral administration (CL/F) increased with increasing body weight. East-/Southeast-Asian pediatric patients with ITP had approximately 43% higher plasma eltrombopag AUC(0-τ) values as compared with non-Asian patients.
Plasma eltrombopag AUC(0-τ) and Cmax in pediatric patients aged 12 to 17 years was similar to that observed in adults. The pharmacokinetic parameters of eltrombopag in pediatric patients with ITP are shown in Table 15.
| aPK parameters presented as geometric mean (95% CI).
bBased on population PK post-hoc estimates. |
||
|
Cmaxb |
AUC(0-τ)b |
|
|
Age |
(mcg/mL) |
(mcg·hr/mL) |
|
Adults (n = 108) |
7.03 |
101 |
|
(6.44, 7.68) |
(91.4, 113) |
|
|
12 to 17 years (n = 62) |
6.80 |
103 |
|
(6.17, 7.50) |
(91.1, 116) |
|
|
6 to 11 years (n = 68) |
10.3 |
153 |
|
(9.42, 11.2) |
(137, 170) |
|
|
1 to 5 years (n = 38) |
11.6 |
162 |
|
(10.4, 12.9) |
(139, 187) |
|
Drug Interaction Studies
Clinical Studies
Effect of Drugs on Eltrombopag
Effect of Polyvalent Cation-containing Antacids on Eltrombopag:
The coadministration of a single dose of PROMACTA (75 mg) with a polyvalent cation-containing antacid (1,524 mg aluminum hydroxide, 1,425 mg magnesium carbonate, and sodium alginate) decreased plasma eltrombopag AUC0-INF and Cmax by approximately 70%. The contribution of sodium alginate to this interaction is not known.
Effect of HIV Protease Inhibitors on Eltrombopag:
The coadministration of repeat-dose lopinavir 400 mg/ritonavir 100 mg (twice daily) with a single dose of PROMACTA (100 mg) decreased plasma eltrombopag AUC0-INF by 17%.
Effect of HCV Protease Inhibitors on Eltrombopag:
The coadministration of repeat-dose telaprevir (750 mg every 8 hours) or boceprevir (800 mg every 8 hours) with a single dose of PROMACTA (200 mg) to healthy adult subjects in a clinical trial did not alter plasma eltrombopag AUC0-INF or Cmax to a significant extent.
Effect of Cyclosporine on Eltrombopag:
The coadministration of a single dose of PROMACTA (50 mg) with a single dose of an OATP and BCRP inhibitor cyclosporine (200 mg or 600 mg) decreased plasma eltrombopag AUC0-INF by 18% to 24% and Cmax by 25% to 39%.
Effect of Pegylated Interferon alfa-2a + Ribavirin and Pegylated Interferon alfa-2b + Ribavirin on Eltrombopag:
The presence of pegylated interferon alfa + ribavirin therapy did not significantly affect the clearance of eltrombopag.
Effect of Eltrombopag on Other Drugs
Effect of Eltrombopag on Cytochrome P450 Enzymes Substrates:
The coadministration of multiple doses of PROMACTA (75 mg once daily for 7 days) did not result in the inhibition or induction of the metabolism of a combination of probe substrates for CYP1A2 (caffeine), CYP2C19 (omeprazole), CYP2C9 (flurbiprofen), or CYP3A4 (midazolam) in humans.
Effect of Eltrombopag on Rosuvastatin:
The coadministration of multiple doses of PROMACTA (75 mg once daily for 5 days) with a single dose of rosuvastatin (OATP1B1 and BCRP substrate; 10 mg) increased plasma rosuvastatin AUC0-INF by 55% and Cmax by 103%.
Effect of Eltrombopag on HCV Protease Inhibitors:
The coadministration of repeat-dose telaprevir (750 mg every 8 hours) or boceprevir (800 mg every 8 hours) with a single dose of PROMACTA (200 mg) to healthy adult subjects in a clinical trial did not alter plasma telaprevir or boceprevir AUC0-INF or Cmax to a significant extent.
In vitro Studies
Eltrombopag Effect on Metabolic Enzymes
Eltrombopag has demonstrated the potential to inhibit CYP2C8, CYP2C9, UGT1A1, UGT1A3, UGT1A4, UGT1A6, UGT1A9, UGT2B7, and UGT2B15.
Eltrombopag Effect on Transporters
Eltrombopag has demonstrated the potential to inhibit OATP1B1 and BCRP.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Eltrombopag does not stimulate platelet production in rats, mice, or dogs because of unique TPO receptor specificity. Data from these animals do not fully model effects in humans.
Eltrombopag was not carcinogenic in mice at doses up to 75 mg/kg/day or in rats at doses up to 40 mg/kg/day (exposures up to 4 times the human clinical exposure based on AUC in patients with ITP at 75 mg/day and 2 times the human clinical exposure based on AUC in patients with chronic hepatitis C at 100 mg/day).
Eltrombopag was not mutagenic or clastogenic in a bacterial mutation assay or in two in vivo assays in rats (micronucleus and unscheduled DNA synthesis, 10 times the human clinical exposure based on Cmax in patients with ITP at 75 mg/day and 7 times the human clinical exposure based on Cmax in patients with chronic hepatitis C at 100 mg/day). In the in vitro mouse lymphoma assay, eltrombopag was marginally positive (less than 3-fold increase in mutation frequency).
Eltrombopag did not affect female fertility in rats at doses up to 20 mg/kg/day (2 times the human clinical exposure based on AUC in patients with ITP at 75 mg/day and similar to the human clinical exposure based on AUC in patients with chronic hepatitis C at 100 mg/day). Eltrombopag did not affect male fertility in rats at doses up to 40 mg/kg/day, the highest dose tested (3 times the human clinical exposure based on AUC in patients with ITP at 75 mg/day and 2 times the human clinical exposure based on AUC in patients with chronic hepatitis C at 100 mg/day).
13.2 Animal Pharmacology and/or Toxicology
Treatment-related cataracts were detected in rodents in a dose- and time-dependent manner. At greater than or equal to 6 times the human clinical exposure based on AUC in patients with ITP at 75 mg/day and 3 times the human clinical exposure based on AUC in patients with chronic hepatitis C at 100 mg/day, cataracts were observed in mice after 6 weeks and in rats after 28 weeks of dosing. At greater than or equal to 4 times the human clinical exposure based on AUC in patients with ITP at 75 mg/day and 2 times the human clinical exposure based on AUC in patients with chronic hepatitis C at 100 mg/day, cataracts were observed in mice after 13 weeks and in rats after 39 weeks of dosing [see Warnings and Precautions (5.5)].
Renal tubular toxicity was observed in studies up to 14 days in duration in mice and rats at exposures that were generally associated with morbidity and mortality. Tubular toxicity was also observed in a 2-year oral carcinogenicity study in mice at doses of 25, 75, and 150 mg/kg/day. The exposure at the lowest dose was 1.2 times the human clinical exposure based on AUC in patients with ITP at 75 mg/day and 0.6 times the human clinical exposure based on AUC in patients with chronic hepatitis C at 100 mg/day. No similar effects were observed in mice after 13 weeks at exposures greater than those associated with renal changes in the 2-year study, suggesting that this effect is both dose- and time-dependent.
| This Medication Guide has been approved by the U.S. Food and Drug Administration | Revised: March 2023 |
| MEDICATION GUIDE | |
| PROMACTA® (pro-MAC-ta) (eltrombopag) tablets | PROMACTA® (pro-MAC-ta) (eltrombopag) for oral suspension |
| What is the most important information I should know about PROMACTA?
PROMACTA can cause serious side effects, including: Liver problems:
Tell your healthcare provider right away if you have any of these signs and symptoms of liver problems: |
|
|
|
| See “What are the possible side effects of PROMACTA?” for other side effects of PROMACTA. | |
| What is PROMACTA?
PROMACTA is a prescription medicine used to treat adults and children 1 year of age and older with low blood platelet counts due to persistent or chronic immune thrombocytopenia (ITP), when other medicines to treat ITP or surgery to remove the spleen have not worked well enough. PROMACTA is also used to treat people with:
PROMACTA is used to try to raise platelet counts in order to lower your risk for bleeding. PROMACTA is not used to make platelet counts normal. PROMACTA is not for use in people with a pre-cancerous condition called myelodysplastic syndrome (MDS), or in people with low platelet counts caused by certain other medical conditions or diseases. It is not known if PROMACTA is safe and effective when used with other antiviral medicines to treat chronic hepatitis C. It is not known if PROMACTA is safe and effective in children:
|
|
Before you take PROMACTA, tell your healthcare provider about all of your medical conditions, including if you:
Especially tell your healthcare provider if you take:
Certain medicines may keep PROMACTA from working correctly. Take PROMACTA at least 2 hours before or 4 hours after taking these products:
Ask your healthcare provider if you are not sure if your medicine is one that is listed above. |
|
How should I take PROMACTA?
|
|
| What should I avoid while taking PROMACTA?
Avoid situations and medicines that may increase your risk of bleeding. |
|
| What are the possible side effects of PROMACTA?
PROMACTA may cause serious side effects, including:
The most common side effects of PROMACTA in adults and children include: |
|
|
|
| Laboratory tests may show abnormal changes to the cells in your bone marrow. Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all of the possible side effects of PROMACTA. For more information, ask your healthcare provider or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
|
| How should I store PROMACTA tablets and PROMACTA for oral suspension?
Tablets:
For oral suspension:
Keep PROMACTA and all medicines out of the reach of children. |
|
| General information about the safe and effective use of PROMACTA
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use PROMACTA for a condition for which it was not prescribed. Do not give PROMACTA to other people, even if they have the same symptoms that you have. It may harm them. You can ask your healthcare provider or pharmacist for information about PROMACTA that is written for health professionals. |
|
| What are the ingredients in PROMACTA?
Tablets Active ingredient: eltrombopag olamine Inactive ingredients:
For oral suspension Active ingredient: eltrombopag olamine Inactive ingredients: mannitol, sucralose, and xanthan gum Distributed by: Novartis Pharmaceuticals Corporation, East Hanover, New Jersey 07936 © Novartis For more information about PROMACTA, go to www.PROMACTA.com or call 1-888-669-6682. |
|
T2023-14
INSTRUCTIONS FOR USE
PROMACTA® [pro-MAC-ta]
(eltrombopag)
for oral suspension
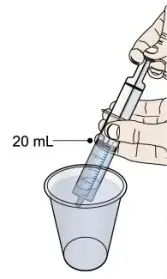
Read all the Instructions for Use and follow the steps below to mix and give a dose of PROMACTA for oral suspension.
Important information you need to know before taking PROMACTA for oral suspension:
- Do not take PROMACTA for oral suspension or give it to someone else until you have been shown how to properly mix and give a dose of PROMACTA for oral suspension. Your healthcare provider or nurse will show you how to mix and give a dose of PROMACTA for oral suspension properly.
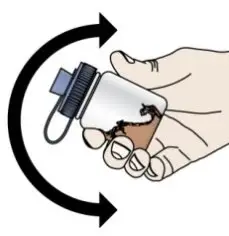
- PROMACTA for oral suspension must be mixed with cool or cold water only. Do not use hot water to prepare the oral suspension.
- Give the dose of suspension right away after mixing with water. If the medicine is not given within 30 minutes, you will have to mix a new dose. Throw away (discard) the unused mixture into the trash. Do not pour it down the drain.
- If PROMACTA for oral suspension comes in contact with your skin, wash the skin right away with soap and water. Call your healthcare provider if you have a skin reaction or if you have any questions. If you spill any powder or liquid, follow the clean-up instructions in Step 12.
- Contact your healthcare provider or pharmacist if you have any questions about how to mix or give PROMACTA to your child, or if you damage or lose any of the supplies in your kit.
- Do not re-use the oral dosing syringe. Use a new single-use oral dosing syringe to prepare each dose of PROMACTA for oral suspension.
- After you have used all 30 packets, throw all the remaining supplies (mixing bottle, lid with cap, and oral dosing syringe) away in the trash.
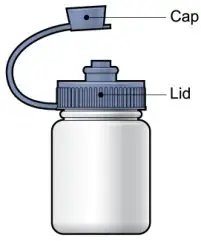
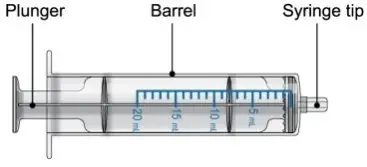
Each PROMACTA for oral suspension kit contains the following supplies:
You will need the following to give a dose of PROMACTA for oral suspension.
From the kit:
- prescribed number of packets
- 1 reusable mixing bottle with lid and cap. Note: Due to its small size, the cap may pose a danger of choking to small children.
- 1 single-use 20-mL oral dosing syringe (Use a new (single-use) oral dosing syringe to prepare each dose of PROMACTA for oral suspension)
Not included in the kit:
- 1 clean glass or cup filled with drinking water
- scissors to cut packet
- paper towels or disposable cloth
- disposable gloves (optional)
T2020-61
| PROMACTA
eltrombopag olamine tablet, film coated |
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| PROMACTA
eltrombopag olamine tablet, film coated |
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| PROMACTA
eltrombopag olamine tablet, film coated |
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
| PROMACTA
eltrombopag olamine tablet, film coated |
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| PROMACTA
eltrombopag olamine powder, for suspension |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| PROMACTA
eltrombopag olamine powder, for suspension |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| Labeler - Novartis Pharmaceuticals Corporation (002147023) |