Drug Detail:Provera (Medroxyprogesterone (oral) [ me-drox-ee-proe-jes-ter-one ])
Drug Class: Contraceptives Hormones / antineoplastics Progestins
WARNING: CARDIOVASCULAR DISORDERS, BREAST CANCER AND PROBABLE DEMENTIA FOR ESTROGEN PLUS PROGESTIN THERAPY
Provera - Clinical Pharmacology
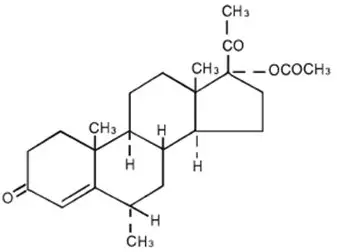
Medroxyprogesterone acetate (MPA) administered orally or parenterally in the recommended doses to women with adequate endogenous estrogen, transforms proliferative into secretory endometrium. Androgenic and anabolic effects have been noted, but the drug is apparently devoid of significant estrogenic activity. While parenterally administered MPA inhibits gonadotropin production, which in turn prevents follicular maturation and ovulation, available data indicate that this does not occur when the usually recommended oral dosage is given as single daily doses.
Pharmacokinetics
The pharmacokinetics of MPA were determined in 20 postmenopausal women following a single-dose administration of eight PROVERA 2.5 mg tablets or a single administration of two PROVERA 10 mg tablets under fasting conditions. In another study, the steady-state pharmacokinetics of MPA were determined under fasting conditions in 30 postmenopausal women following daily administration of one PROVERA 10 mg tablet for 7 days. In both studies, MPA was quantified in serum using a validated gas chromatography-mass spectrometry (GC-MS) method. Estimates of the pharmacokinetic parameters of MPA after single and multiple doses of PROVERA tablets were highly variable and are summarized in Table 1.
| Tablet Strength | C max
(ng/mL) | T max
(h) | Auc 0–(∞)
(ng∙h/mL) | t 1/2
(h) | Vd/f (L) | CL/f (mL/min) |
|---|---|---|---|---|---|---|
|
||||||
| Single Dose | ||||||
| 2 × 10 mg | 1.01 (0.599) | 2.65 (1.41) | 6.95 (3.39) | 12.1 (3.49) | 78024 (47220) | 64110 (42662) |
| 8 × 2.5 mg | 0.805 (0.413) | 2.22 (1.39) | 5.62 (2.79) | 11.6 (2.81) | 62748 (40146) | 74123 (35126) |
| Multiple Dose | ||||||
| 10 mg * | 0.71 (0.35) | 2.83 (1.83) | 6.01 (3.16) | 16.6 (15.0) | 40564 (38256) | 41963 (38402) |
Clinical Studies
Effects on the Endometrium
In a 3-year, double-blind, placebo-controlled study of 356 nonhysterectomized, postmenopausal women between 45 and 64 years of age randomized to receive placebo (n=119), 0.625 mg conjugated estrogen only (n=119), or 0.625 mg conjugated estrogen plus cyclic PROVERA (n=118), results showed a reduced risk of endometrial hyperplasia in the treatment group receiving 10 mg PROVERA plus 0.625 mg conjugated estrogens compared to the group receiving 0.625 mg conjugated estrogens only. See Table 2.
| Histological Results | Placebo (n=119) | CEE †
(n=119) | PROVERA ‡ + CEE (n=118) |
|---|---|---|---|
|
|||
| Normal/No hyperplasia (%) | 116 (97) | 45 (38) | 112 (95) |
| Simple (cystic) hyperplasia (%) | 1 (1) | 33 (28) | 4 (3) |
| Complex (adenomatous) hyperplasia (%) | 1 (1) | 27 (22) | 2 (2) |
| Atypia (%) | 0 | 14 (12) | 0 |
| Adenocarcinoma (%) | 1 (1) | 0 | 0 |
In a second 1-year study, 832 postmenopausal women between 45 and 65 years of age were treated with daily 0.625 mg conjugated estrogen (days 1–28), plus either 5 mg cyclic PROVERA or 10 mg cyclic PROVERA (days 15–28), or daily 0.625 mg conjugated estrogen only. The treatment groups receiving 5 or 10 mg cyclic PROVERA (days 15–28) plus daily conjugated estrogens showed a significantly lower rate of hyperplasia as compared to the conjugated estrogens only group. See Table 3.
| CEE * | MPA † + CEE * | ||
|---|---|---|---|
| (n=283) | MPA 5 mg (n=277) | MPA 10 mg (n=272) |
|
|
|||
| Cystic hyperplasia (%) | 55 (19) | 3 (1) | 0 |
| Adenomatous hyperplasia without atypia | 2 (1) | 0 | 0 |
Women's Health Initiative Studies
The WHI enrolled approximately 27,000 predominantly healthy postmenopausal women in two substudies to assess the risks and benefits of daily oral CE (0.625 mg)-alone or in combination with MPA (2.5 mg) compared to placebo in the prevention of certain chronic diseases. The primary endpoint was the incidence of coronary heart disease (CHD) (defined as nonfatal MI, silent MI and CHD death), with invasive breast cancer as the primary adverse outcome. A "global index" included the earliest occurrence of CHD, invasive breast cancer, stroke, PE, endometrial cancer (only in the CE plus MPA substudy), colorectal cancer, hip fracture, or death due to other cause. These substudies did not evaluate the effects of CE-alone or CE plus MPA on menopausal symptoms.
WHI Estrogen Plus Progestin Substudy
The WHI estrogen plus progestin substudy was stopped early. According to the predefined stopping rule, after an average follow-up of 5.6 years of treatment, the increased risk of invasive breast cancer and cardiovascular events exceeded the specified benefits included in the "global index." The absolute excess risk of events included in the "global index" was 19 per 10,000 women-years.
For those outcomes included in the WHI "global index" that reached statistical significance after 5.6 years of follow-up, the absolute excess risks per 10,000 women-years in the group treated with CE plus MPA were 7 more CHD events, 8 more strokes, 10 more PEs, and 8 more invasive breast cancers, while the absolute risk reduction per 10,000 women-years were 6 fewer colorectal cancers and 5 fewer hip fractures.
Results of the CE plus MPA substudy, which included 16,608 women (average 63 years of age, range 50 to 79; 83.9 percent White, 6.8 percent Black, 5.4 percent Hispanic, 3.9 percent Other) are presented in Table 4. These results reflect centrally adjudicated data after an average follow-up of 5.6 years.
| Event | Relative Risk CE/MPA vs placebo (95%nCI ‡) | CE/MPA n = 8,506 | Placebo n = 8,102 |
|---|---|---|---|
| Absolute Risk per 10,000 Women-Years | |||
|
|||
| CHD events | 1.23 (0.99–1.53) | 41 | 34 |
| Non-fatal MI | 1.28 (1.00–1.63) | 31 | 25 |
| CHD death | 1.10 (0.70–1.75) | 8 | 8 |
| All strokes | 1.31 (1.03–1.68) | 33 | 25 |
| Ischemic stroke | 1.44 (1.09–1.90) | 26 | 18 |
| Deep vein thrombosis§ | 1.95 (1.43–2.67) | 26 | 13 |
| Pulmonary embolism | 2.13 (1.45–3.11) | 18 | 8 |
| Invasive breast cancer¶ | 1.24 (1.01–1.54) | 41 | 33 |
| Colorectal cancer | 0.61 (0.42–0.87) | 10 | 16 |
| Endometrial cancer§ | 0.81 (0.48–1.36) | 6 | 7 |
| Cervical cancer§ | 1.44 (0.47–4.42) | 2 | 1 |
| Hip fracture | 0.67 (0.47–0.96) | 11 | 16 |
| Vertebral fractures§ | 0.65 (0.46–0.92) | 11 | 17 |
| Lower arm/wrist fractures§ | 0.71 (0.59–0.85) | 44 | 62 |
| Total fractures§ | 0.76 (0.69–0.83) | 152 | 199 |
| Overall mortality# | 1.00 (0.83–1.19) | 52 | 52 |
| Global IndexÞ | 1.13 (1.02–1.25) | 184 | 165 |
Timing of the initiation of estrogen plus progestin therapy relative to the start of menopause may affect the overall risk benefit profile. The WHI estrogen plus progestin substudy stratified by age showed in women 50 to 59 years of age a nonsignificant trend toward reduced risk in overall mortality [hazard ration (HR) 0.69 (95 percent CI, 0.44–1.07)].
Indications and Usage for Provera
PROVERA tablets are indicated for the treatment of secondary amenorrhea and abnormal uterine bleeding due to hormonal imbalance in the absence of organic pathology, such as fibroids or uterine cancer. They are also indicated for use in the prevention of endometrial hyperplasia in nonhysterectomized postmenopausal women who are receiving daily oral conjugated estrogens 0.625 mg tablets.
Contraindications
PROVERA is contraindicated in women with any of the following conditions:
- Undiagnosed abnormal genital bleeding.
- Known, suspected, or history of breast cancer.
- Known or suspected estrogen- or progesterone-dependent neoplasia.
- Active DVT, PE, or a history of these conditions
- Active arterial thromboembolic disease (for example, stroke and MI), or a history of these conditions.
- Known anaphylactic reaction or angioedema to PROVERA.
- Known liver impairment or disease.
- Known or suspected pregnancy.
Warnings
See BOXED WARNINGS.
1. Cardiovascular Disorders
An increased risk of PE, DVT, stroke, and MI has been reported with estrogen plus progestin therapy. Should any of these events occur or be suspected, estrogen plus progestin therapy should be discontinued immediately.
Risk factors for arterial vascular disease (for example, hypertension, diabetes mellitus, tobacco use, hypercholesterolemia, and obesity) and/or venous thromboembolism (VTE) (for example, personal history or family history of VTE, obesity, and systemic lupus erythematosus) should be managed appropriately.
2. Malignant Neoplasms
a. Breast Cancer
The most important randomized clinical trial providing information about breast cancer in estrogen plus progestin users is the WHI substudy of daily CE (0.625 mg) plus MPA (2.5 mg). After a mean follow-up of 5.6 years, the estrogen plus progestin substudy reported an increased risk of invasive breast cancer in women who took daily CE plus MPA.
In this substudy, prior use of estrogen-alone or estrogen plus progestin therapy was reported by 26 percent of the women. The relative risk of invasive breast cancer was 1.24, and the absolute risk was 41 versus 33 cases per 10,000 women-years, for CE plus MPA compared with placebo. Among women who reported prior use of hormone therapy, the relative risk of invasive breast cancer was 1.86, and the absolute risk was 46 versus 25 cases per 10,000 women-years, for CE plus MPA compared with placebo. Among women who reported no prior use of hormone therapy, the relative risk of invasive breast cancer was 1.09, and the absolute risk was 40 versus 36 cases per 10,000 women-years, for CE plus MPA compared with placebo. In the same substudy, invasive breast cancers were larger, were more likely to be node positive, and were diagnosed at a more advanced stage in the CE (0.625 mg) plus MPA (2.5 mg) group compared with the placebo group. Metastatic disease was rare with no apparent difference between the two groups. Other prognostic factors such as histologic subtype, grade, and hormone receptor status did not differ between the groups. (See CLINICAL STUDIES.)
Consistent with the WHI clinical trial, observational studies have also reported an increased risk of breast cancer for estrogen plus progestin therapy, and a smaller risk for estrogen-alone therapy, after several years of use. The risk increased with duration of use, and appeared to return to baseline over about 5 years after stopping treatment (only the observational studies have substantial data on risk after stopping). Observational studies also suggest that the risk of breast cancer was greater, and became apparent earlier, with estrogen plus progestin therapy as compared to estrogen-alone therapy. However, these studies have not found significant variation in the risk of breast cancer among different estrogen plus progestin combinations, or routes of administration.
The use of estrogen plus progestin has been reported to result in an increase in abnormal mammograms requiring further evaluation. All women should receive yearly breast examinations by a healthcare provider and perform monthly breast self-examinations. In addition, mammography examinations should be scheduled based on patient age, risk factors, and prior mammogram results.
3. Probable Dementia
In the WHIMS estrogen plus progestin ancillary study of WHI, a population of 4,532 postmenopausal women aged 65 to 79 years was randomized to daily CE (0.625 mg) plus MPA (2.5 mg) or placebo.
After an average follow-up of 4 years, 40 women in the CE plus MPA group and 21 women in the placebo group were diagnosed with probable dementia. The relative risk of probable dementia for CE plus MPA versus placebo was 2.05 (95 percent CI, 1.21–3.48). The absolute risk of probable dementia for CE plus MPA versus placebo was 45 versus 22 cases per 10,000 women-years. It is unknown whether these findings apply to younger postmenopausal women. (See CLINICAL STUDIES and PRECAUTIONS, Geriatric Use.)
4. Visual Abnormalities
Discontinue estrogen plus progestin therapy pending examination if there is sudden partial or complete loss of vision, or a sudden onset of proptosis, diplopia or migraine. If examination reveals papilledema or retinal vascular lesions, estrogen plus progestin therapy should be permanently discontinued.
Precautions
F. Nursing Mothers
PROVERA should not be used during lactation. Detectable amounts of progestin have been identified in the breast milk of nursing mothers receiving progestins.
G. Pediatric Use
PROVERA tablets are not indicated in children. Clinical studies have not been conducted in the pediatric population.
Adverse Reactions/Side Effects
See BOXED WARNINGS, WARNINGS, and PRECAUTIONS.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The following adverse reactions have been reported in women taking PROVERA tablets, without concomitant estrogens treatment:
PATIENT INFORMATION
PROVERA
(pro-VE-rah)
(medroxyprogesterone acetate tablets, USP)
Read this Patient Information before you start taking PROVERA and read what you get each time you refill your PROVERA prescription. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment.
What is PROVERA?
PROVERA is a medicine that contains medroxyprogesterone acetate, a progestin hormone.
What is PROVERA used for?
PROVERA is used to:
- Treat menstrual periods that have stopped or to treat abnormal uterine bleeding. Women with a uterus who are not pregnant, who stop having regular menstrual periods or who begin to have irregular menstrual periods may have a drop in their progesterone level. Talk with your healthcare provider about whether PROVERA is right for you.
- Reduce your chances of getting cancer of the uterus (womb). In postmenopausal women with a uterus who use estrogens, taking progestin in combination with estrogen will reduce your chance of getting cancer of the uterus (womb).
Who should not take PROVERA?
Do not start taking PROVERA if you:
- have unusual vaginal bleeding
-
currently have or have had certain cancers
Estrogen plus progestin may increase your chance of getting certain types of cancers, including cancer of the breast. If you have or have had cancer, talk with your healthcare provider about whether you should use PROVERA. - had a stroke or heart attack
- currently have or have had blood clots
- currently have or have had liver problems
-
are allergic to PROVERA or any of its ingredients
See the list of ingredients in PROVERA at the end of this leaflet. -
think you may be pregnant
PROVERA is not for pregnant women. If you think you may be pregnant, you should have a pregnancy test and know the results. Do not use PROVERA if the test is positive and talk to your healthcare provider. There may be an increased risk of minor birth defects in children whose mothers take PROVERA during the first 4 months of pregnancy.
PROVERA should not be used as a test for pregnancy.
What should I tell my healthcare provider before taking PROVERA? Before you take PROVERA, tell your healthcare provider if you:
-
have any other medical problems
Your healthcare provider may need to check you more carefully if you have certain conditions such as asthma (wheezing), epilepsy (seizures), diabetes, migraine, endometriosis (severe pelvic pain), lupus, or problems with your heart, liver, thyroid, kidneys, or have high calcium in your blood. -
are going to have surgery or will be on bed rest
Your healthcare provider will let you know if you need to stop taking PROVERA. -
are breast feeding
The hormone in PROVERA can pass into your breast milk.
Tell your healthcare provider about all the medicines you take including prescription and nonprescription medicines, vitamins, and herbal supplements. Some medicines may affect how PROVERA works. PROVERA may also affect how other medicines work.
How should I take PROVERA?
Start at the lowest dose and talk to your healthcare provider about how well that dose is working for you. The lowest effective dose of PROVERA has not been determined. You and your healthcare provider should talk regularly (every 3 to 6 months) about the dose you are taking and whether you still need treatment with PROVERA.
- Absence of menstrual period: PROVERA may be given in doses ranging from 5 to 10 mg daily for 5 to 10 days.
- Abnormal Uterine Bleeding: PROVERA may be given in doses ranging from 5 to 10 mg daily for 5 to 10 days.
- Overgrowth of the lining of the uterus: When used in combination with oral conjugated estrogens in postmenopausal women with a uterus, PROVERA may be given in doses ranging from 5 or 10 mg daily for 12 to 14 straight days per month.
What are the possible side effects of PROVERA?
The following side effects have been reported with the use of PROVERA alone:
- breast tenderness
- breast milk secretion
- breakthrough bleeding
- spotting (minor vaginal bleeding)
- irregular periods
- amenorrhea (absence of menstrual periods)
- vaginal secretions
- headaches
- nervousness
- dizziness
- depression
- insomnia, sleepiness, fatigue
- premenstrual syndrome-like symptoms
- thrombophlebitis (inflamed veins)
- blood clot
- itching, hives, skin rash
- acne
- hair loss, hair growth
- abdominal discomfort
- nausea
- bloating
- fever
- increase in weight
- swelling
- changes in vision and sensitivity to contact lenses
Call your healthcare provider right away if you get hives, problems breathing, swelling of the face, mouth, tongue or neck
The following side effects have been reported with the use of PROVERA with an estrogen.
Side effects are grouped by how serious they are and how often they happen when you are treated.
Serious, but less common side effects include:
- heart attack
- stroke
- blood clots
- dementia
- breast cancer
- cancer of the uterus
- cancer of the ovary
- high blood pressure
- high blood sugar
- gallbladder disease
- liver problems
- changes in your thyroid hormone levels
- enlargements of benign tumors ("fibroids")
Call your healthcare provider right away if you get any of the following warning signs or any other unusual symptoms that concern you:
- new breast lumps
- unusual vaginal bleeding
- changes in vision and speech
- sudden new severe headaches
- severe pains in your chest or legs with or without shortness of breath, weakness and fatigue
- memory loss or confusion
Less serious, but common side effects include:
- headache
- breast pain
- irregular vaginal bleeding or spotting
- stomach or abdominal cramps, bloating
- nausea and vomiting
- hair loss
- fluid retention
- vaginal yeast infection
These are not all the possible side effects of PROVERA with or without estrogen. For more information, ask your healthcare provider or pharmacist for advice about side effects. Tell your healthcare provider if you have side effect that bothers you or does not go away. You may report side effects to Pfizer at 1-800-438-1985 or FDA at 1-800-FDA-1088.
What can I do to lower my chances of a serious side effect with PROVERA?
- Talk with your healthcare provider regularly about whether you should continue taking PROVERA. The addition of a progestin is generally recommended for women with a uterus to reduce the chance of getting cancer of the uterus (womb).
- See your healthcare provider right away if you get vaginal bleeding while taking PROVERA.
- Have a pelvic exam, breast exam and mammogram (breast X-ray) every year unless your healthcare provider tells you something else. If members of your family have had breast cancer or if you have ever had breast lumps or an abnormal mammogram, you may need to have breast exams more often.
- If you have high blood pressure, high cholesterol (fat in the blood), diabetes, are overweight, or if you use tobacco, you may have a higher chance of getting heart disease. Ask your healthcare provider for ways to lower your chance of getting heart disease.
General information about safe and effective use of PROVERA
- Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets.
- Do not take PROVERA for conditions for which it was not prescribed.
- Do not give PROVERA to other people, even if they have the same symptoms you have. It may harm them.
Keep PROVERA out of the reach of children.
This leaflet provides a summary of the most important information about PROVERA. If you would like more information, talk with your health care provider or pharmacist. You can ask for information about PROVERA that is written for health professionals. You can get more information by calling the toll-free number, 1-800-438-1985.
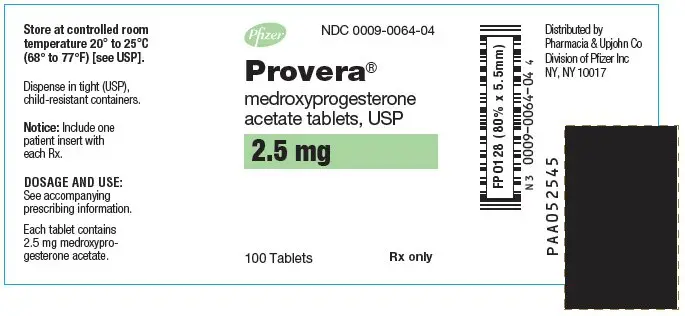
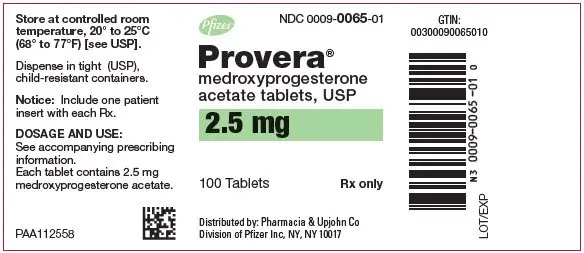
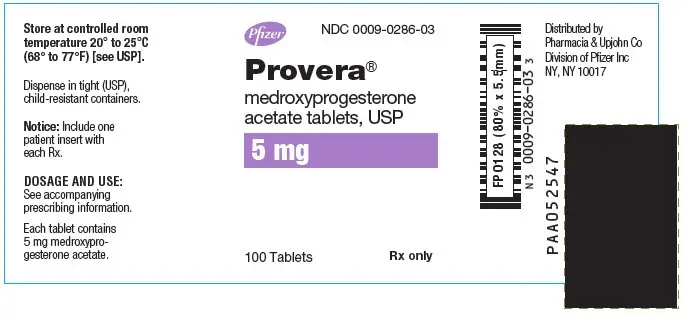
What are the ingredients in PROVERA?
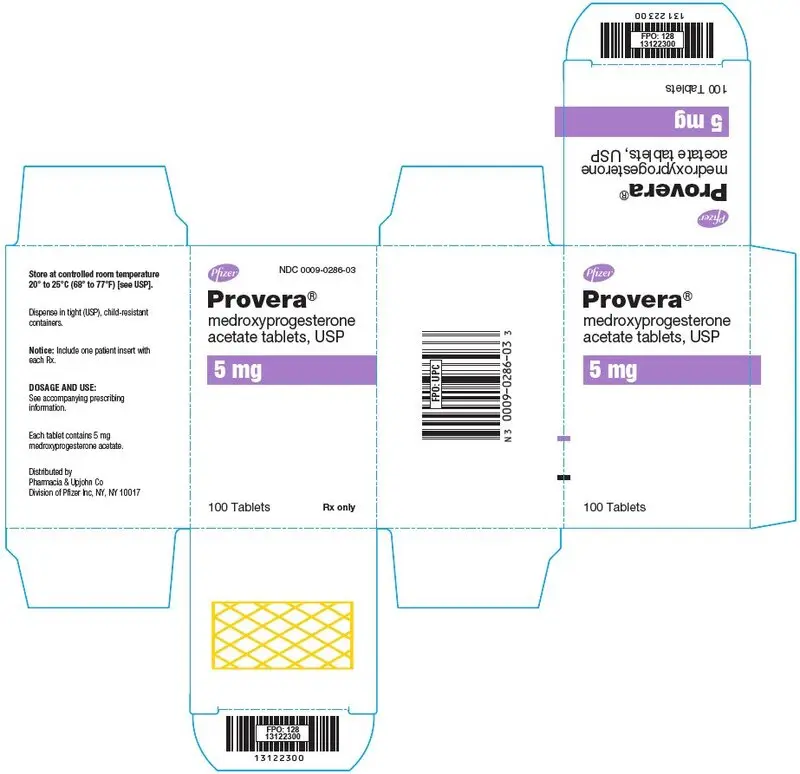
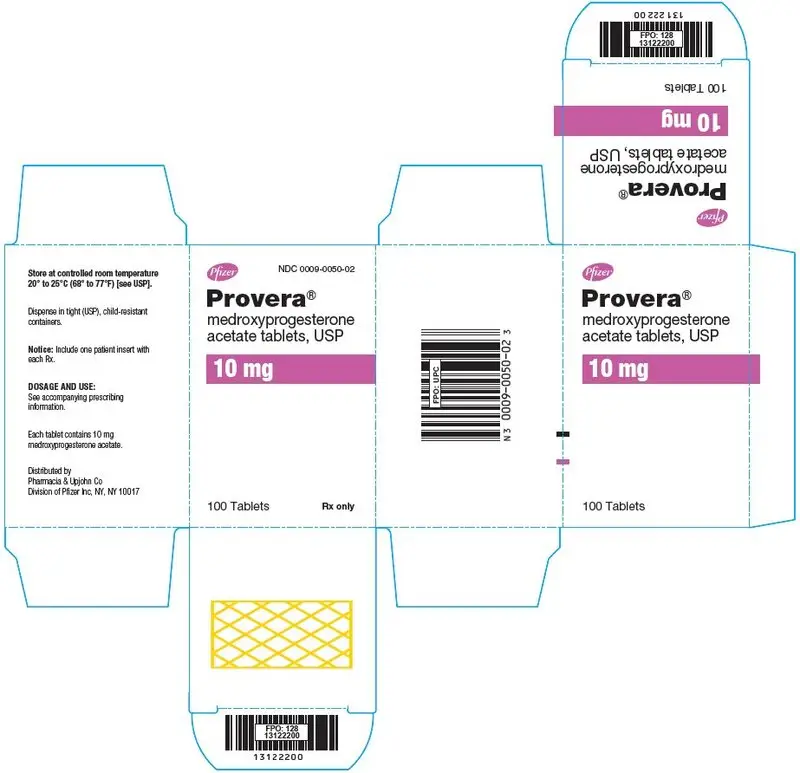
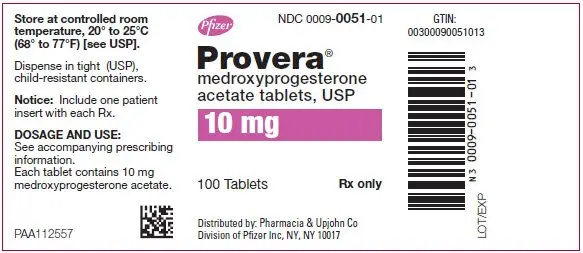
Each PROVERA tablet for oral administration contains 2.5 mg, 5 mg or 10 mg of medroxyprogesterone acetate.
Inactive ingredients:
| 2.5 mg tablets | ||
| calcium stearate, corn starch, lactose, mineral oil, sorbic acid, sucrose, talc, FD&C Yellow No. 6. | OR | calcium stearate, corn starch, lactose, mineral oil, sucrose, talc, FD&C Yellow No. 6. |
| 5 mg tablets | ||
| calcium stearate, corn starch, lactose, mineral oil, sorbic acid, sucrose, talc. | OR | calcium stearate, corn starch, lactose, mineral oil, sucrose, talc, FD&C Blue No.2 – Aluminum Lake. |
| 10 mg tablets | ||
| calcium stearate, corn starch, lactose, mineral oil, sorbic acid, sucrose, talc. | OR | calcium stearate, corn starch, lactose, mineral oil, sucrose, talc. |
This product's label may have been updated. For current full prescribing information, please visit www.pfizer.com
Rx only

LAB-0365-8.0
January 2018
| PROVERA
medroxyprogesterone acetate tablet |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| PROVERA
medroxyprogesterone acetate tablet |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| PROVERA
medroxyprogesterone acetate tablet |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| PROVERA
medroxyprogesterone acetate tablet |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| PROVERA
medroxyprogesterone acetate tablet |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| PROVERA
medroxyprogesterone acetate tablet |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Pharmacia and Upjohn Company (618054084) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pharmacia & Upjohn Company LLC | 618054084 | ANALYSIS(0009-0050, 0009-0051, 0009-0064, 0009-0065, 0009-0286, 0009-0287) , MANUFACTURE(0009-0050, 0009-0051, 0009-0064, 0009-0065, 0009-0286, 0009-0287) , API MANUFACTURE(0009-0050, 0009-0051, 0009-0064, 0009-0065, 0009-0286, 0009-0287) , PACK(0009-0050, 0009-0051, 0009-0064, 0009-0065, 0009-0286, 0009-0287) , LABEL(0009-0050, 0009-0051, 0009-0064, 0009-0065, 0009-0286, 0009-0287) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pfizer Italia S.r.l. | 458521908 | ANALYSIS(0009-0050, 0009-0051, 0009-0064, 0009-0065, 0009-0286, 0009-0287) , MANUFACTURE(0009-0050, 0009-0051, 0009-0064, 0009-0065, 0009-0286, 0009-0287) , PACK(0009-0050, 0009-0051, 0009-0064, 0009-0065, 0009-0286, 0009-0287) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pfizer Inc | 943955690 | ANALYSIS(0009-0050, 0009-0051, 0009-0064, 0009-0065, 0009-0286, 0009-0287) | |