Drug Detail:Remodulin (injection) (Treprostinil (injection) [ tre-pros-ti-nil ])
Drug Class: Agents for pulmonary hypertension
Highlights of Prescribing Information
REMODULIN® (treprostinil) Injection, for subcutaneous or intravenous use
Initial U.S. Approval: May 2002
Indications and Usage for Remodulin
Remodulin is a prostacyclin mimetic indicated for:
- Treatment of pulmonary arterial hypertension (PAH; WHO Group 1) to diminish symptoms associated with exercise. Studies establishing effectiveness included patients with NYHA Functional Class II-IV symptoms and etiologies of idiopathic or heritable PAH (58%), PAH associated with congenital systemic-to-pulmonary shunts (23%), or PAH associated with connective tissue diseases (19%). (1.1)
- Patients who require transition from epoprostenol, to reduce the rate of clinical deterioration. The risks and benefits of each drug should be carefully considered prior to transition. (1.2)
Remodulin Dosage and Administration
PAH WHO Group 1 in patients with NYHA Class II-IV symptoms:
- Initial dose for patients new to prostacyclin infusion therapy: 1.25 ng/kg/min; increase based on clinical response (increments of 1.25 ng/kg/min per week for the first 4 weeks of treatment, later 2.5 ng/kg/min per week). Avoid abrupt cessation. (2.2, 2.4)
- Mild to moderate hepatic insufficiency: Decrease initial dose to 0.625 ng/kg/min.
Severe hepatic insufficiency: No studies performed. (2.5)
Transition from Epoprostenol:
Increase the Remodulin dose gradually as the epoprostenol dose is decreased, based on constant observation of response. (2.7)
Administration:
Continuous subcutaneous infusion is the preferred mode. Use intravenous (IV) infusion if subcutaneous infusion is not tolerated. (2.1, 2.6)
Dosage Forms and Strengths
- Remodulin is supplied in 20-mL vials containing 20, 50, 100, 200, or 400 mg of treprostinil (1, 2.5, 5, 10, or 20 mg/mL). (3)
Contraindications
None (4)
Warnings and Precautions
- Chronic intravenous infusions delivered using an external infusion pump with an indwelling central venous catheter are associated with the risk of blood stream infections (BSIs) and sepsis, which may be fatal. (5.1)
- Do not abruptly lower the dose or withdraw dosing. (5.2)
- Remodulin may cause symptomatic hypotension. (5.4)
- Remodulin inhibits platelet aggregation and increases the risk of bleeding. (5.5)
Adverse Reactions/Side Effects
Most common adverse reactions (incidence >3%) reported in clinical studies with Remodulin: subcutaneous infusion site pain and reaction, headache, diarrhea, nausea, jaw pain, vasodilatation, edema, and hypotension. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact United Therapeutics Corp. at 1-866-458-6479 or contact FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Remodulin dosage adjustment may be necessary if inhibitors or inducers of CYP2C8 are added or withdrawn. (7.1)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 7/2021
Related/similar drugs
sildenafil, tadalafil, Adcirca, Revatio, Opsumit, ambrisentanFull Prescribing Information
1. Indications and Usage for Remodulin
1.1 Pulmonary Arterial Hypertension
Remodulin is indicated for the treatment of pulmonary arterial hypertension (PAH; WHO Group 1) to diminish symptoms associated with exercise. Studies establishing effectiveness included patients with NYHA Functional Class II-IV symptoms and etiologies of idiopathic or heritable PAH (58%), PAH associated with congenital systemic-to-pulmonary shunts (23%), or PAH associated with connective tissue diseases (19%) [see Clinical Studies (14.1)].
2. Remodulin Dosage and Administration
2.1 General
Remodulin can be administered with or without further dilution with Sterile Diluent for Remodulin or similar approved high-pH glycine diluent (e.g., Sterile Diluent for Flolan or Sterile Diluent for Epoprostenol), Sterile Water for Injection, or 0.9% Sodium Chloride Injection prior to administration. See Table 1 below for storage and administration time limits for the different diluents.
Diluted Remodulin has been shown to be stable at ambient temperature when stored for up to 14 days using high-pH glycine diluent at concentrations as low as 0.004 mg/mL (4,000 ng/mL).
| Diluent | Storage Limits | Administration Limits |
|---|---|---|
| None | See Section 16 | 16 weeks at 40°C |
| Sterile Diluents for Remodulin, Flolan, or Epoprostenol | 14 days at room temperature | 48 hours at 40°C |
| Sterile Water for Injection 0.9% Sodium Chloride for Injection | 4 hours at room temperature or 24 hours refrigerated | 48 hours at 40°C |
2.2 Initial Dose for Patients New to Prostacyclin Infusion Therapy
Remodulin is indicated for subcutaneous (SC) or intravenous (IV) use only as a continuous infusion. Remodulin is preferably infused subcutaneously, but can be administered by a central intravenous line if the subcutaneous route is not tolerated because of severe site pain or reaction. The infusion rate is initiated at 1.25 ng/kg/min. If this initial dose cannot be tolerated because of systemic effects, reduce the infusion rate to 0.625 ng/kg/min.
2.3 Initial Dose for Patients Transitioning to an Implantable Intravenous Infusion Pump
The initial dose of Remodulin should be the same as the current dose the patient is receiving using the external infusion pump at the time of transition.
2.4 Dosage Adjustments
The goal of chronic dosage adjustments is to establish a dose at which PAH symptoms are improved, while minimizing excessive pharmacologic effects of Remodulin (headache, nausea, emesis, restlessness, anxiety, and infusion site pain or reaction).
The infusion rate should be increased in increments of 1.25 ng/kg/min per week for the first four weeks of treatment and then 2.5 ng/kg/min per week for the remaining duration of infusion, depending on clinical response. Dosage adjustments may be undertaken more often if tolerated. Avoid abrupt cessation of infusion [see Warnings and Precautions (5.2)]. Restarting a Remodulin infusion within a few hours after an interruption can be done using the same dose rate. Interruptions for longer periods may require the dose of Remodulin to be re-titrated.
2.5 Patients with Hepatic Insufficiency
In patients with mild or moderate hepatic insufficiency, decrease the initial dose of Remodulin to 0.625 ng/kg/min ideal body weight. Remodulin has not been studied in patients with severe hepatic insufficiency [see Warnings and Precautions (5.3), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)].
2.6 Administration
Inspect parenteral drug products for particulate matter and discoloration prior to administration whenever solution and container permit. If either particulate matter or discoloration is noted, do not use.
2.7 Patients Requiring Transition from Epoprostenol
Transition from epoprostenol to Remodulin is accomplished by initiating the infusion of Remodulin and increasing it, while simultaneously reducing the dose of intravenous epoprostenol. The transition to Remodulin should take place in a hospital with constant observation of response (e.g., walk distance and signs and symptoms of disease progression). Initiate Remodulin at a recommended dose of 10% of the current epoprostenol dose, and then escalate as the epoprostenol dose is decreased (see Table 2 for recommended dose titrations).
Patients are individually titrated to a dose that allows transition from epoprostenol therapy to Remodulin while balancing prostacyclin-limiting adverse events. Treat increases in the patient's symptoms of PAH first with increases in the dose of Remodulin. Treat side effects normally associated with prostacyclin and prostacyclin analogs first by decreasing the dose of epoprostenol.
| Step | Epoprostenol Dose | Remodulin Dose |
|---|---|---|
| 1 | Unchanged | 10% Starting Epoprostenol Dose |
| 2 | 80% Starting Epoprostenol Dose | 30% Starting Epoprostenol Dose |
| 3 | 60% Starting Epoprostenol Dose | 50% Starting Epoprostenol Dose |
| 4 | 40% Starting Epoprostenol Dose | 70% Starting Epoprostenol Dose |
| 5 | 20% Starting Epoprostenol Dose | 90% Starting Epoprostenol Dose |
| 6 | 5% Starting Epoprostenol Dose | 110% Starting Epoprostenol Dose |
| 7 | 0 | 110% Starting Epoprostenol Dose + additional 5-10% increments as needed |
3. Dosage Forms and Strengths
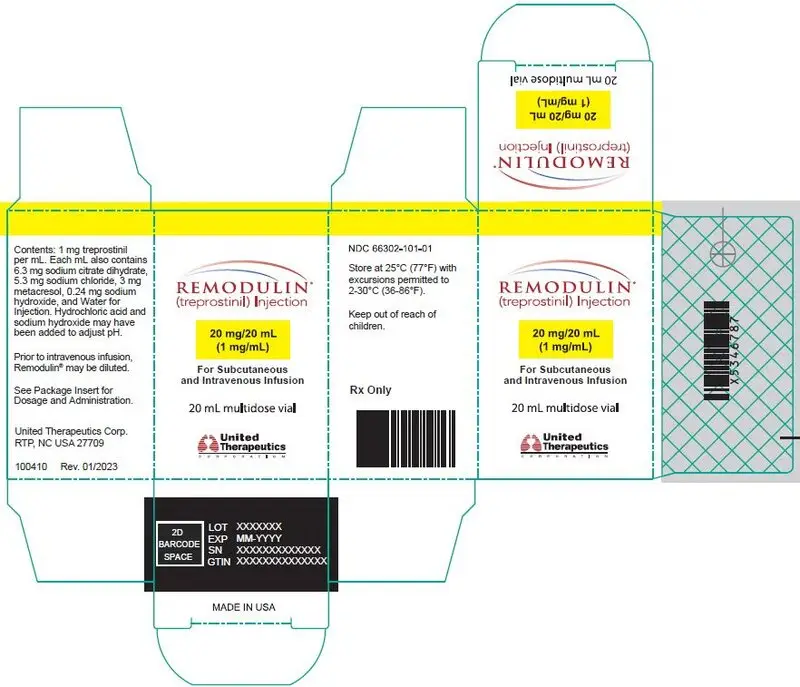
20-mL vial containing 20 mg treprostinil (1 mg per mL).
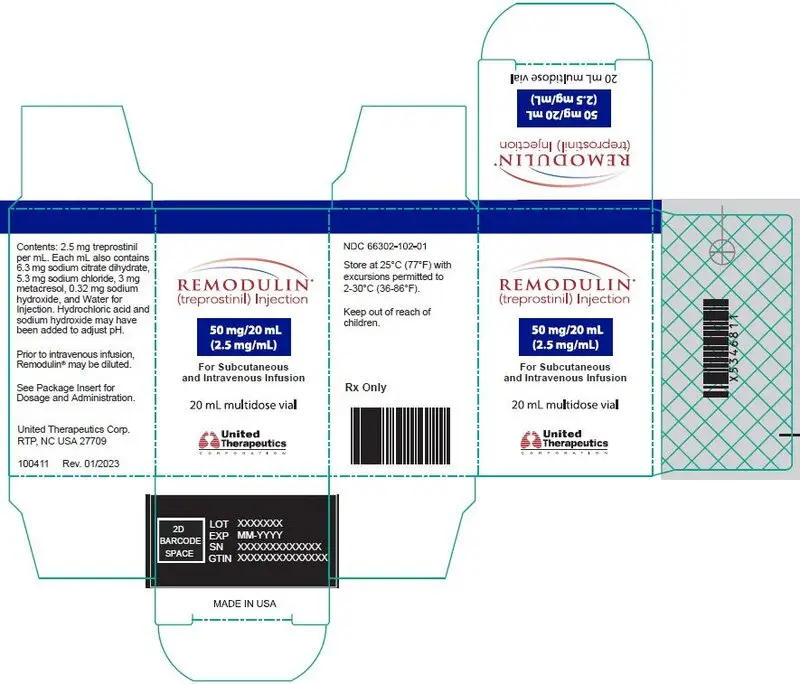
20-mL vial containing 50 mg treprostinil (2.5 mg per mL).
20-mL vial containing 100 mg treprostinil (5 mg per mL).
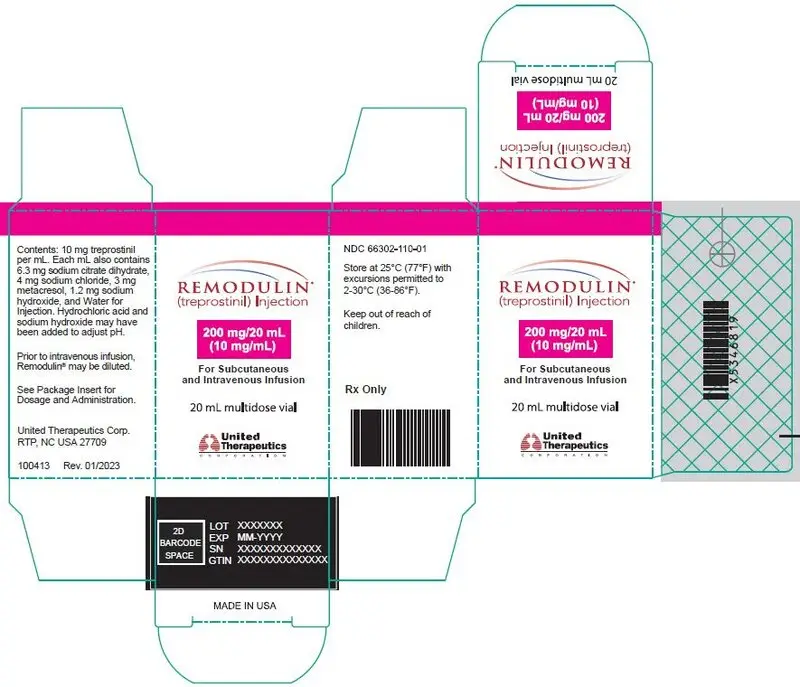
20-mL vial containing 200 mg treprostinil (10 mg per mL).
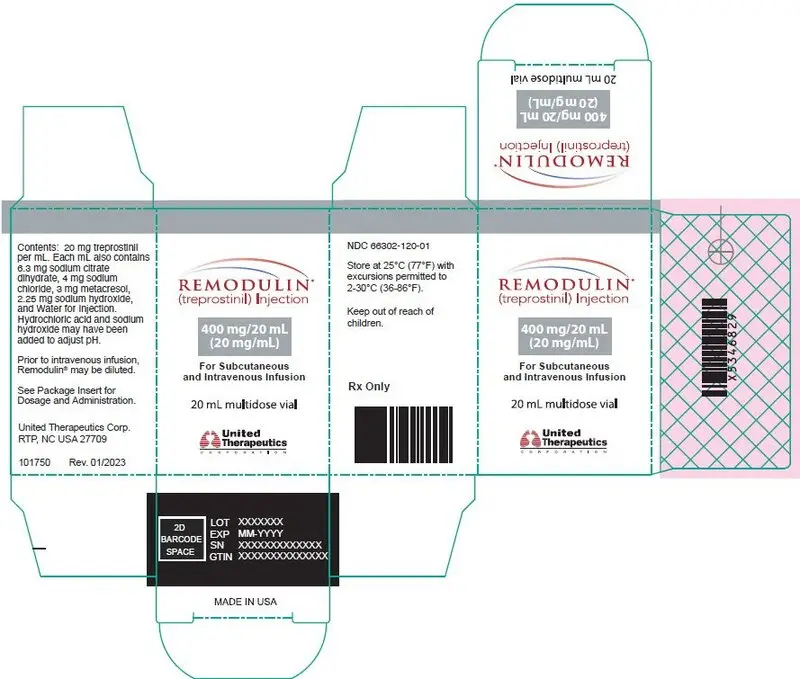
20-mL vial containing 400 mg treprostinil (20 mg per mL).
5. Warnings and Precautions
5.1 Risk of Catheter-Related Bloodstream Infection
Chronic intravenous infusions of Remodulin delivered using an external infusion pump with an indwelling central venous catheter are associated with the risk of blood stream infections (BSIs) and sepsis, which may be fatal. Therefore, continuous subcutaneous infusion is the preferred mode of administration.
In an open-label study of IV treprostinil (n=47) using an external infusion pump, there were seven catheter-related line infections during approximately 35 patient years, or about 1 BSI event per 5 years of use. A CDC survey of seven sites that used IV treprostinil for the treatment of PAH found approximately 1 BSI (defined as any positive blood culture) event per 3 years of use. Administration of IV Remodulin with a high pH glycine diluent has been associated with a lower incidence of BSIs when compared to neutral diluents (sterile water, 0.9% sodium chloride) when used along with catheter care guidelines.
In an open-label study of an implantable pump (n=60), there were two blood stream infections (BSIs) related to the implant procedure during approximately 265 patient years.
5.2 Worsening PAH upon Abrupt Withdrawal or Sudden Large Dose Reduction
Avoid abrupt withdrawal or sudden large reductions in dosage of Remodulin, which may result in worsening of PAH symptoms.
5.3 Patients with Hepatic Insufficiency
Titrate Remodulin slowly in patients with hepatic insufficiency, because such patients will likely be exposed to greater systemic concentrations relative to patients with normal hepatic function [see Dosage and Administration (2.5), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)].
6. Adverse Reactions/Side Effects
The following adverse reactions are discussed elsewhere in labeling: Infections associated with intravenous administration [see Warnings and Precautions (5.1)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
6.2 Post-Marketing Experience
In addition to adverse reactions reported from clinical trials, the following events have been identified during post-approval use of Remodulin. Because they are reported voluntarily from a population of unknown size, estimates of frequency cannot be made. The following events have been chosen for inclusion because of a combination of their seriousness, frequency of reporting, and potential connection to Remodulin. These events are thrombophlebitis associated with peripheral intravenous infusion, thrombocytopenia, bone pain, pruritus, dizziness, arthralgia, myalgia/muscle spasm, and pain in extremity. In addition, generalized rashes, sometimes macular or papular in nature, and cellulitis have been infrequently reported.
7. Drug Interactions
7.1 Effect of CYP2C8 Inhibitors and Inducers on Treprostinil
Dose adjustment of treprostinil may be necessary when co-administered with CYP2C8 inducers or inhibitors. Human pharmacokinetic studies with an oral formulation of treprostinil (treprostinil diolamine) indicated that co-administration of the cytochrome P450 (CYP) 2C8 enzyme inhibitor gemfibrozil increases exposure (both Cmax and AUC) to treprostinil. Co-administration of the CYP2C8 enzyme inducer rifampin decreases exposure to treprostinil. It has not been determined if the changes in exposure of treprostinil with inhibitors or inducers of CYP2C8 observed for the oral administration of treprostinil would be similar for treprostinil administered via the parenteral route [see Clinical Pharmacology (12.3)].
8. Use In Specific Populations
8.1 Pregnancy
Data
Animal reproduction studies have been conducted with treprostinil via continuous subcutaneous administration and with treprostinil diolamine administered orally. In pregnant rats, continuous subcutaneous infusions of treprostinil during organogenesis and late gestational development, at doses as high as 900 ng treprostinil/kg/min (about 117 times the starting human subcutaneous infusion rate, on a ng/m2 basis and about 16 times the average rate achieved in clinical trials), resulted in no evidence of harm to the fetus. In pregnant rabbits, effects of continuous subcutaneous infusions of treprostinil during organogenesis were limited to an increased incidence of fetal skeletal variations (bilateral full rib or right rudimentary rib on lumbar 1) associated with maternal toxicity (reduction in body weight and food consumption) at a dose of 150 ng treprostinil/kg/min (about 41 times the starting human subcutaneous infusion rate, on a ng/m2 basis, and 5 times the average rate used in clinical trials). In rats, continuous subcutaneous infusion of treprostinil from implantation to the end of lactation, at doses of up to 450 ng treprostinil/kg/min, did not affect the growth and development of offspring. In studies with orally administered treprostinil diolamine, no adverse effect doses for fetal viability/growth, fetal development (teratogenicity), and postnatal development were determined in rats. In pregnant rats, no evidence of harm to the fetus was observed following oral administration of treprostinil diolamine at the highest dose tested (20 mg/kg/day), which represents about 123 and 48 times the human exposure, when based on Cmax and AUC of the average subcutaneous infusion rate achieved in clinical trials, respectively. In pregnant rabbits, external fetal and soft tissue malformations and fetal skeletal malformation occurred. The dose at which no adverse effects were seen (0.5 mg/kg/day) represents about 7 and 5 times the human exposure, when based on Cmax and AUC of the average subcutaneous infusion rate achieved in clinical trials, respectively. No treprostinil treatment-related effects on labor and delivery were seen in animal studies. Animal reproduction studies are not always predictive of human response.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients have not been established. Clinical studies of Remodulin did not include sufficient numbers of patients aged ≤16 years to determine whether they respond differently from older patients.
8.5 Geriatric Use
Clinical studies of Remodulin did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from younger patients. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Patients with Hepatic Insufficiency
Remodulin clearance is reduced in patients with hepatic insufficiency. In patients with mild or moderate hepatic insufficiency, decrease the initial dose of Remodulin to 0.625 ng/kg/min ideal body weight, and monitor closely. Remodulin has not been studied in patients with severe hepatic insufficiency [see Dosage and Administration (2.5), Warnings and Precautions (5.3), and Clinical Pharmacology (12.3)].
10. Overdosage
Signs and symptoms of overdose with Remodulin during clinical trials are extensions of its dose-limiting pharmacologic effects and include flushing, headache, hypotension, nausea, vomiting, and diarrhea. Most events were self-limiting and resolved with reduction or withholding of Remodulin.
In controlled clinical trials using an external infusion pump, seven patients received some level of overdose and in open-label follow-on treatment seven additional patients received an overdose; these occurrences resulted from accidental bolus administration of Remodulin, errors in pump programmed rate of administration, and prescription of an incorrect dose. In only two cases did excess delivery of Remodulin produce an event of substantial hemodynamic concern (hypotension, near-syncope).
One pediatric patient was accidentally administered 7.5 mg of Remodulin via a central venous catheter. Symptoms included flushing, headache, nausea, vomiting, hypotension, and seizure-like activity with loss of consciousness lasting several minutes. The patient subsequently recovered.
11. Remodulin Description
Remodulin (treprostinil) Injection is a sterile solution of treprostinil, a prostacyclin mimetic, formulated for subcutaneous or intravenous administration. Remodulin is supplied in 20-mL multidose vials in five strengths, containing 20 mg, 50 mg, 100 mg, 200 mg, or 400 mg (1 mg/mL, 2.5 mg/mL, 5 mg/mL, 10 mg/mL, or 20 mg/mL) of treprostinil. Each mL also contains 5.3 mg sodium chloride (except for the 10 mg/mL and 20 mg/mL strengths, which contain 4.0 mg sodium chloride), 3 mg metacresol, 6.3 mg sodium citrate dihydrate, and water for injection. Sodium hydroxide and hydrochloric acid may be added to adjust pH between 6.0 and 7.2.
Treprostinil is chemically stable at room temperature and neutral pH.
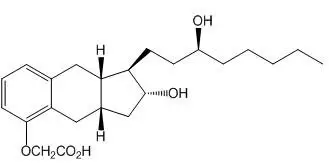
Treprostinil is (1R,2R,3aS,9aS)-[[2,3,3a,4,9,9a-hexahydro-2-hydroxy-1-[(3S)-3-hydroxyoctyl]-1H-benz[f]inden-5-yl]oxy]acetic acid. Treprostinil has a molecular weight of 390.52 and a molecular formula of C23H34O5.
The structural formula of treprostinil is:
Sterile Diluent for Remodulin is a high-pH (pH~10.4) glycine diluent supplied in a 50-mL vial containing 50 mL of Sterile Diluent for Remodulin. Each vial contains 94 mg glycine, 73.3 mg sodium chloride, sodium hydroxide (to adjust pH), and water for injection.
12. Remodulin - Clinical Pharmacology
12.1 Mechanism of Action
The major pharmacologic actions of treprostinil are direct vasodilation of pulmonary and systemic arterial vascular beds, and inhibition of platelet aggregation.
12.2 Pharmacodynamics
In animals, the vasodilatory effects reduce right and left ventricular afterload and increase cardiac output and stroke volume. Other studies have shown that treprostinil causes a dose-related negative inotropic and lusitropic effect. No major effects on cardiac conduction have been observed.
Treprostinil produces vasodilation and tachycardia. Single doses of treprostinil up to 84 mcg by inhalation produce modest and short-lasting effects on QTc, but this is apt to be an artifact of the rapidly changing heart rate. Treprostinil administered by the subcutaneous or intravenous routes has the potential to generate concentrations many-fold greater than those generated via the inhaled route; the effect on the QTc interval when treprostinil is administered parenterally has not been established.
12.3 Pharmacokinetics
The pharmacokinetics of continuous subcutaneous Remodulin are linear over the dose range of 2.5 to 125 ng/kg/min (corresponding to plasma concentrations of about 260 pg/mL to 18,250 pg/mL) and can be described by a two-compartment model. Dose proportionality at infusion rates greater than 125 ng/kg/min has not been studied.
Subcutaneous and intravenous administration of Remodulin demonstrated bioequivalence at steady state at a dose of 10 ng/kg/min.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
A two-year rat carcinogenicity study was performed with treprostinil inhalation at target doses of 5.26, 10.6, and 34.1 mcg/kg/day. There was no evidence for carcinogenic potential associated with treprostinil inhalation in rats at systemic exposure levels up to about 34 and 1 times the human exposure, when based on Cmax and AUC of the average subcutaneous infusion rate achieved in clinical trials, respectively. In vitro and in vivo genetic toxicology studies did not demonstrate any mutagenic or clastogenic effects of treprostinil. Treprostinil sodium did not affect fertility or mating performance of male or female rats given continuous subcutaneous (sc) infusions at rates of up to 450 ng treprostinil/kg/min [about 59 times the recommended starting human sc infusion rate (1.25 ng/kg/min) and 8 times the average rate (9.3 ng/kg/min) achieved in clinical trials, on a ng/m2 basis]. In this study, males were dosed from 10 weeks prior to mating and through the 2-week mating period. Females were dosed from 2 weeks prior to mating until gestational day 6.
Treprostinil diolamine did not demonstrate any carcinogenic effects in mouse or rat carcinogenicity studies. Oral administration of treprostinil diolamine to Tg.rasH2 mice at 0, 5, 10, and 20 mg/kg/day in males and 0, 3, 7.5, and 15 mg/kg/day in females daily for 26 weeks did not significantly increase the incidence of tumors. The exposures, when based on AUC, obtained at the highest dose levels used in males and females are about 7- and 15-fold, respectively, the human exposure of the average subcutaneous infusion rate achieved in clinical trials. Oral administration of treprostinil diolamine to Sprague Dawley rats at 0, 1, 3, and 10 mg/kg/day daily for 104 weeks did not significantly increase the incidence of tumors. The exposures obtained at the highest dose levels used in males and females are about 18- and 26-fold, respectively, the human exposure of the average subcutaneous infusion rate achieved in clinical trials.
Treprostinil diolamine was tested in vivo in a rat micronucleus assay and did not induce an increased incidence of micronucleated polychromatic erythrocytes.
14. Clinical Studies
14.1 Clinical Trials in Pulmonary Arterial Hypertension (PAH)
Two 12-week, multicenter, randomized, double-blind studies compared continuous subcutaneous infusion of Remodulin to placebo in a total of 470 patients with NYHA Class II (11%), III (81%), or IV (7%) PAH. PAH was idiopathic/heritable in 58% of patients, associated with connective tissue diseases in 19%, and the result of congenital systemic-to-pulmonary shunts in 23%. The mean age was 45 (range 9 to 75 years). About 81% were female and 84% were Caucasian. Pulmonary hypertension had been diagnosed for a mean of 3.8 years. The primary endpoint of the studies was change in 6-minute walking distance, a standard measure of exercise capacity. There were many assessments of symptoms related to heart failure, but local discomfort and pain associated with Remodulin may have substantially unblinded those assessments. The 6-minute walking distance and an associated subjective measurement of shortness of breath during the walk (Borg dyspnea score) were administered by a person not participating in other aspects of the study. Remodulin was administered as a subcutaneous infusion, described in Section 2, DOSAGE AND ADMINISTRATION, and the dose averaged 9.3 ng/kg/min at Week 12. Few subjects received doses greater than 40 ng/kg/min. Background therapy, determined by the investigators, could include anticoagulants, oral vasodilators, diuretics, digoxin, and oxygen, but not an endothelin receptor antagonist or epoprostenol. The two studies were identical in design and conducted simultaneously, and the results were analyzed both pooled and individually.
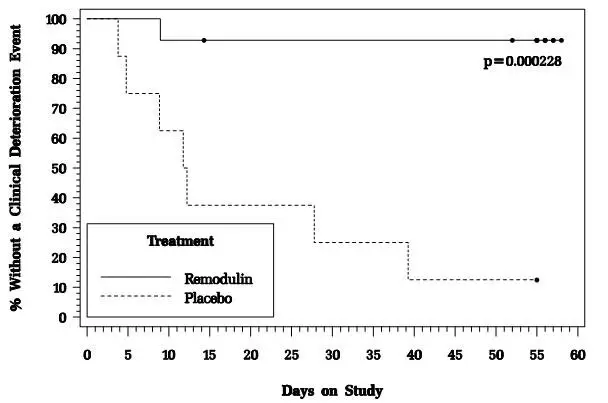
14.2 Flolan-To-Remodulin Transition Study
In an 8-week, multicenter, randomized, double-blind, placebo-controlled study, patients on stable doses of Flolan were randomly withdrawn from Flolan to placebo or Remodulin. Fourteen Remodulin and 8 placebo patients completed the study. The primary endpoint of the study was the time to clinical deterioration, defined as either an increase in Flolan dose, hospitalization due to PAH, or death. No patients died during the study.
During the study period, Remodulin effectively prevented clinical deterioration in patients transitioning from Flolan therapy compared to placebo (Figure 1). Thirteen of 14 patients in the Remodulin arm were able to transition from Flolan successfully, compared to only 1 of 8 patients in the placebo arm (p=0.0002).
Figure 1: Time to Clinical Deterioration for PAH Patients Transitioned from Flolan to Remodulin or Placebo in an 8-Week Study
16. How is Remodulin supplied
Remodulin is supplied in 20-mL multidose vials as sterile solutions in water for injection, individually packaged in cartons. Unopened vials of Remodulin are stable until the date indicated when stored at 25°C (77°F), with excursions permitted to 2-30°C (36-86°F). A single vial of Remodulin should be used for no more than 30 days after the initial introduction into the vial.
Remodulin Injection is supplied as:
| Remodulin | Concentration | NDC |
|---|---|---|
| 20 mg / 20 mL | 1 mg/mL | 66302-101-01 |
| 50 mg / 20 mL | 2.5 mg/mL | 66302-102-01 |
| 100 mg / 20 mL | 5 mg/mL | 66302-105-01 |
| 200 mg / 20 mL | 10 mg/mL | 66302-110-01 |
| 400 mg / 20 mL | 20 mg/mL | 66302-120-01 |
| REMODULIN
treprostinil injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| REMODULIN
treprostinil injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| REMODULIN
treprostinil injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| REMODULIN
treprostinil injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| REMODULIN
treprostinil injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| STERILE DILUENT FOR REMODULIN
water injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - United Therapeutics Corporation (965460025) |